Highlights
-
•
A community quarantine strategy against coronavirus disease 2019 (COVID-19) was adopted in all urban populations in Anhui.
-
•
Community quarantine strategy influenced the injuries distributions in trauma centers.
-
•
Community quarantine strategy was effectively implemented and significantly slowed the outbreak of COVID-19 in Anhui.
-
•
The implementation and maintenance of the strategy is costly and requires the participation of the entire population.
Keywords: COVID-19, SARS-CoV-2, Traffic injury, Community quarantine
Abstract
Objective
The objective of our study was to introduce community quarantine strategy against coronavirus disease 2019 (COVID-19) in Anhui and evaluate the effectiveness of community quarantine based on trauma center (TC) patients.
Method
The structure of community quarantine strategy was illustrated. Distribution of injuries among patients in two TCs between January 24, 2020 and February 24, 2020 was described. Multiple linear regression was used to analyze the correlation between the distribution of Injuries in TCs and the number of COVID-19-associated cases.
Results
A total of 757 TC patients in the two hospitals were enrolled. The number of traffic injuries and outdoor injuries showed a significant decrease in the early stage and began to increase on February 17. The number of indoor injuries neither decreased nor increased. Multiple linear regression analysis revealed a significant correlation between COVID-19-associated cases and traffic and outdoor injuries.
Conclusion
From the perspective of the injuries in TCs, community quarantine strategy was effectively implemented and significantly slowed the outbreak of COVID-19 in Anhui. However, the implementation and maintenance of the strategy is costly and requires the participation of the entire population.
1. Introduction
In December 2019, a group of patients with pneumonia of unknown cause were tested positive for a novel coronavirus in Wuhan, China (Sohrabi et al., 2020, Zhu et al., 2020a). The virus spread rapidly in the city and showed strong infectivity and pathogenicity. As this novel coronavirus shared over 79% of its genome sequence with the coronavirus that causes severe acute respiratory syndrome (SARS-CoV), it was subsequently named SARS-CoV-2 (Lu et al., 2020). The pneumonia caused by SARS-CoV-2 was subsequently identified as a novel acute respiratory infectious disease and was named coronavirus disease 2019 (COVID-19). Following outbreaks in China and Asia, COVID-19 spread widely in Europe and the Americas. On March 11, 2020, 40 days after COVID-19 gained the tag “public health emergency of international concern,” The World Health Organization (WHO) declared COVID-19 a pandemic. As of April 2, 2020, SARS-CoV-2 has infected greater than one million people worldwide. European countries including Italy and Spain have adopted a state of emergency in response to the outbreak (Albarello et al., 2020).
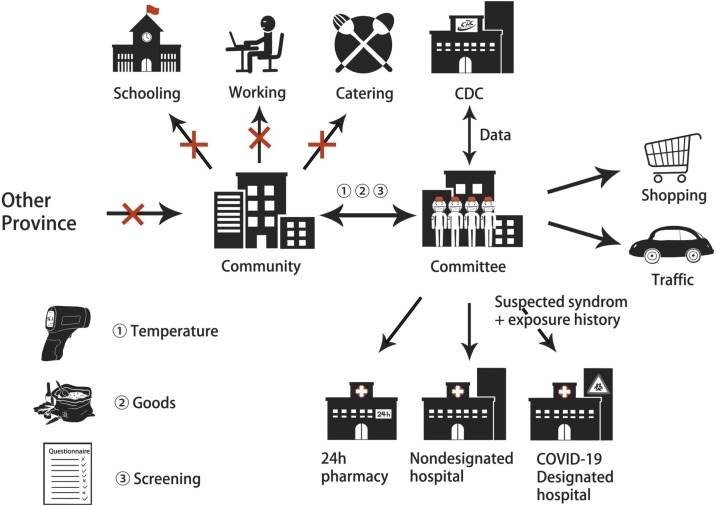
Confirmed cases in China accounted for the majority of infected patients in the early stages of the COVID-19 outbreak. The initial rapid increase in the number of cases had a huge impact on China's medical and public health institutions (Li et al., 2020; Zhu Wanbo et al., 2020). Subsequently, the government took a series of measures to respond to the outbreak, including the establishment of new hospitals for infected patients and square cabin hospitals to quarantine suspected patients. A strategy of community quarantine was also widely adopted in urban populations for medical observation (Lin et al., 2020). The strategy, led by community committees dominated by public servants, aimed to screen the densely populated urban population for potential and latent infections and quarantine residents with definite exposure history. The community committee in China is supported by the community administrative department and all community members. It is administered by a working group recommended by the government and elected by members of the community. During this outbreak, all community members received the committee's standardized questionnaire on temperature, symptoms, and exposure history for a certain period of time. As part of the extended Spring Festival holiday, most jobs, schools, and public places were shut down. Going outdoors was mainly for grocery shopping and to visit the hospital. Members of the community were free to leave and enter the community after the committee ruled out potential infections each day; however, multiple daily outings were recommended against. After daily screening of all community members, the committee shared the data with the Center for Disease Control (CDC). This date sharing mainly included three ways: (1) the information platform would update the vital signs of suspected infected and medical observation patients in all the communities, as well as the information about the recent population migration in communities, especially the areas with high incidence of infection; (2) information of patients requiring medical quarantine who need to be transferring in the community today; (3) telemedicine to guide the community in epidemic prevention and medical resource allocation. For members with suspected syndromes and a clear exposure history, the CDC or designated COVID-19 hospital quarantined the member for medical observation and performed the nucleic acid affirmatory test for the virus. For patients who required treatment for non-COVID-19 diseases, the committee contacted non-designated hospitals for admission. For members in need of drugs, the committee extended help via a 24-h contactless pharmacy. Meanwhile, during the period of community quarantine, community members communicated with the committee in a timely manner, including on social platforms and door-to-door (Rao and Vazquez, 2020). The committee also provided delivery services of goods to members unwilling to go outdoors. The health of committee workers was guaranteed by the CDC. This strategy of community quarantine in Anhui is illustrated in Fig. 1 .
Fig. 1.
Illustration of the strategy of community quarantine adopted in Anhui. Community members were screened for COVID-19 by the community committee. The screening data were sharing between committee and the CDC. Suspected patients would be sent to designated hospitals for further treatment. The committee also responsible for traffic regulation and goods delivery during community quarantine.
Anhui is adjacent to the Hubei, whose capital is Wuhan. With the adoption of the strategy of community quarantine on January 23, 2020, there was almost no increase in confirmed or suspected cases in Anhui as of February 22, and all positively tested patients were discharged on March 7. Previously, we reported that there was a plunge in traffic injuries based on information from a trauma center (TC) in Anhui after January 23 (Zhu et al., 2020b, Zhu et al., 2020c). In this study, the relationship between the distribution of patients in two TCs and the daily number of new COVID-19-associated cases was studied, while attempting to evaluate the role of community quarantine during the COVID-19 outbreak in Anhui.
2. Materials and methods
2.1. Patients data collection
This retrospective study describes the distribution of injuries among patients in TCs of the First Affiliated Hospital of University of Science and Technology of China and the Southern branch of the Anhui Provincial Hospital between January 24, 2020 and February 24, 2020. The injuries were generally divided into traffic injuries, indoor injuries, and outdoor injuries excluding traffic injuries. Traffic injuries included motor vehicle accidents and non-motor vehicle accidents. Indoor injuries included falls, joint dislocations, fractures, soft tissue and ligament injuries, and open injuries and associated emerging infections that occurred indoors. Outdoor injuries included outdoor falls, joint dislocations, fractures, soft tissue and ligament injuries, and open injuries and associated new infections. Exclusion criteria were chronic injury and other non-injury diseases. All patient data were stored in the hospital's medical records management system, and the patient's diagnosis at the trauma center was performed by two or more trauma doctors. Patient data were collected by two volunteers. This study was approved by the ethics committees of the First Affiliated Hospital of USTC and the Southern branch of the Anhui Provincial Hospital.
2.2. COVID-19-associated cases
Data of COVID-19-associated cases in Anhui were collected based on the daily report of the COVID-19 outbreak issued by the National Health Commission of the People's Republic of China (China, 2020). New confirmed and suspected cases were identified according to guidelines for the diagnosis and treatment of pneumonia caused by novel coronavirus infection published by the National Health Commission. New medical observation cases were members who came in close contact with the above cases. The daily new confirmed cases, new suspected cases, and new medical observation cases in Anhui from January 24, 2020 to February 24, 2020 were recorded by two people.
2.3. Statistical analysis
SPSS Statistics 20 (IBM Corp, Armonk, New York) was used for statistical analysis. Count data are expressed as number of cases. Multiple linear regression was used to analyze the correlation between the distribution of patients in TCs and the number of COVID-19-associated cases. P < 0.05 was considered statistically significant.
3. Results
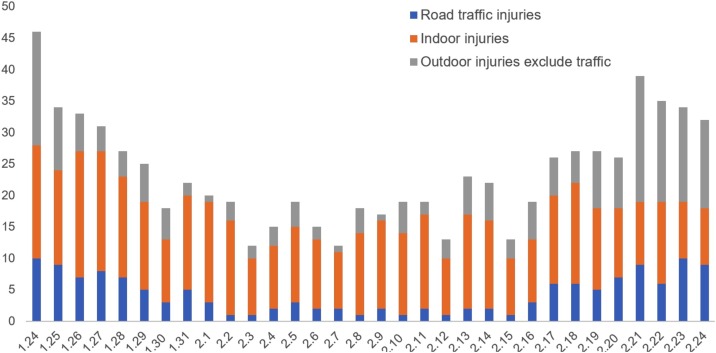
A total of 757 TC patients in the two hospitals were enrolled in the study. Daily patient descriptions are shown in Supplemental Table 1. The numbers of patients with traffic injuries, indoor injuries, and outdoor injury excluding traffic injury were 141, 416, and 200 respectively. Daily distribution is shown as a schematic (Fig. 2 ). The number of traffic injuries and outdoor injuries showed a significant decrease in the early stage and began to increase on February 17. The number of indoor injuries neither decreased nor increased.
Fig. 2.
Distribution of injuries in trauma centers. The daily injuries distribution in TCs include traffic injuries, indoor and outdoor injuries excluding traffic injuries from January 24 to February 24.
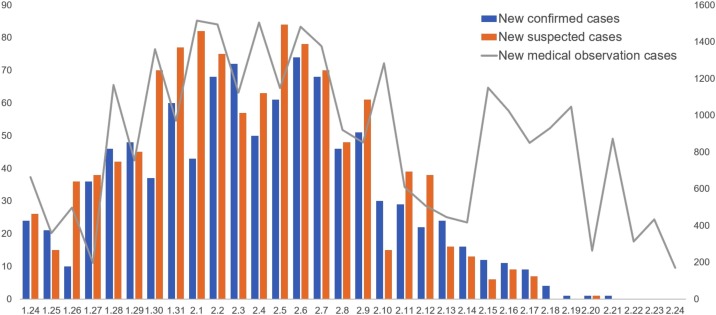
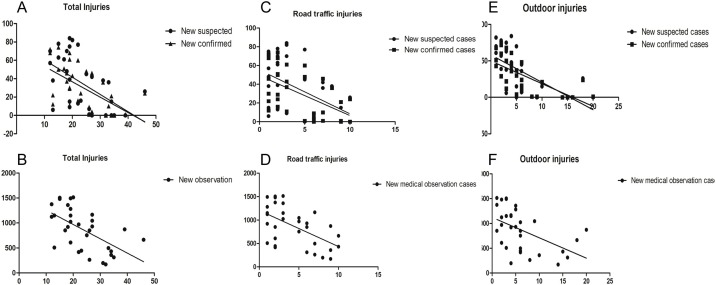
A total of 975 confirmed cases, 1,111 suspected cases, and 27,696 medical observation cases were reported during this period as shown in Fig. 3 and Supplemental Table 2. The number of all cases increased significantly in the first 15 days and gradually peaked. On February 10, there was a marked decline, and on the 27th day there were almost no confirmed and suspected cases. New medical observation cases began to decline on February 6. However, on February 14, there was a marked recovery. Multiple linear regression analysis revealed a significant correlation between COVID-19-associated cases and traffic and outdoor injuries (Table 1 ). Total injuries were significantly correlated with COVID-19-associated cases. However, indoor injuries were not related to the new confirmed, suspected, or medical observation cases, respectively. Fig. 4 shows the correlational analysis of distribution of injuries and COVID-19-associated cases.
Fig. 3.
Description of daily new COVID-19-associated cases. The COVID-19-associated cases include new infected, suspected and medical observation cases from January 24 to February 24.
Table 1.
Pearson correlation analysis between injuries in TC and patients
| Injuries | New confirmed cases |
New suspected cases |
New medical observation cases |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Pearson coefficients | R squared | P value | Pearson coefficients | R squared | P value | Pearson coefficients | R squared | P value | |
| Total injuries | −0.5846 | 0.3418 | 0.0004 | −0.5371 | 0.2885 | 0.0015 | −0.5772 | 0.3331 | 0.0005 |
| Road traffic injuries | −0.5340 | 0.2851 | 0.0016 | −0.4806 | 0.2310 | 0.0054 | −0.5560 | 0.3091 | 0.0010 |
| Indoor injuries | 0.00384 | <0.0001 | 0.9834 | 0.0699 | 0.0049 | 0.7038 | −0.2093 | 0.04382 | 0.2502 |
| Outdoor injuries exclude traffic | −0.6545 | 0.4284 | <0.0001 | −0.6478 | 0.4197 | <0.0001 | −0.4985 | 0.2485 | 0.0037 |
Fig. 4.
Correlation analysis of injuries and daily new COVID-19-associated cases. A and B, correlation analysis of total injuries and daily new COVID-19-associated cases; C and D, correlation analysis of traffic injuries and daily new COVID-19 associated cases; E and F, correlation analysis of outdoor injuries and daily new COVID-19-associated cases.
4. Discussion
In this study, a strategy for community quarantine was described for urban populations during the outbreak of COVID-19 in the Anhui province of China. The correlation between daily injury distribution in two TCs and new COVID-19-associated cases was studied. The study revealed that the number of traffic injuries and outdoor injuries in TCs decreased significantly after community quarantine was implemented. Moreover, the number of traffic injuries and outdoor injuries during the implementation of community quarantine was correlated with daily new confirmed and suspected cases of COVID-19.
Since the outbreak of COVID-19 in Wuhan at the end of 2019, most cities in China have quickly experienced outbreaks owing to the accelerated population migration during the Spring Festival travel rush and the early limited understanding of SARS-CoV-2 (Zhong et al., 2020). Four months later, the outbreak is still not under control globally and the rapidly increasing number of cases has already made a huge impact on medical and public health institutions. As of March 16, 2020, COVID-19 has infected more than 170,000 people worldwide and was deemed a pandemic by the WHO. Due to the presence of latent and asymptomatic infections, as well as the lack of a complete understanding of the transmission route of the SARS-CoV-2, effectively controlling the source of infection in the population, cutting off the transmission route, and protecting vulnerable people has proved to be difficult for public health policy makers (Wang et al., 2020). Although epidemiological analyses and data models provide references for controlling further expansion of the outbreak, there is no consensus on a unified approach.
Previous studies have found that despite the presence of individual cases, the incubation period of SARS-CoV-2 is around 14 days (Lauer et al., 2020). The urban population density is conducive to the clustering effect of virus transmission. To prevent people from being exposed to asymptomatic and latent infections, as well as infections of unknown routes of transmission, a strategy of community quarantine was developed and widely adopted in the urban populations in China. The strategy aimed to screen urban populations based on committees in their communities to ensure that all confirmed and suspected cases in the city are detected in a timely manner. Subsequently, the CDC provided effective nucleic acid tests for the virus in all suspected cases by sharing data with the committee. Members of the community excluded by the committee from suspected infection were encouraged to complete a period of medical observation at home to avoid potential exposure and infection. Due to the continuation of the Spring Festival holiday, most offices, schools, and public areas have not yet been opened, which provides a realistic background for the implementation of community quarantine.
Although community members deemed uninfected by the committee and CDC were not restricted to going outdoors, the impact of the strategy on injuries was noted in our study. The reduction in traffic and outdoor injuries in TCs reflects the effectiveness of the strategy. Moreover, this pattern of injuries reduction was relevant to the change in the COVID-19-associated cases in Anhui after the implementation of the strategy of community quarantine. The logical explanation is that as community screening continues, members of the community are encouraged to stay home and travel outdoors less. Confirmed and suspected cases were found and sent to designated hospitals for treatment. However, with the end of the incubation period, the number of cases began to decline rapidly due to the full admission of confirmed patients and the community quarantine of the entire urban population. The number of people going outdoors gradually increased subsequently, resulting in an increase in traffic injuries and outdoor injuries.
The community quarantine strategy was phased out in March as the outbreak was brought under control in Anhui. Recent studies suggest that transmission control measures have yielded satisfactory results in controlling the spread of the disease in Wuhan, averting hundreds of thousands of cases (Tian et al., 2020). As a potential part of the control measures, the community quarantine strategy provides an idea of medical and basic living support for community members. Researchers, including in Singapore, have suggested deployment of the strategy to response to this global public health incident (Koo et al., 2020).
The shortcomings of this strategy are equally obvious. Because of the presence of asymptomatic infections, community members quarantined at home cannot avoid familial cluster infection (Chan et al., 2020, Pan et al., 2020). In our study, new confirmed and suspected cases did not begin to decline significantly until the middle of the second incubation period. Moreover, in the second incubation period, the number of new medical observation cases experienced a significant recovery, which may be related to the screening of delayed familial cluster infection (Lauer et al., 2020). It is important to note that the implementation and maintenance of this strategy are expensive. Community quarantine in a province containing more than ten million people requires a large number of committee members and volunteers, while no more than a thousand people were eventually diagnosed. Daily disease screenings, contact with the CDC, and community services are costly in terms of human effort and economically. The closure of work places, schools, and public areas; the domiciliary of the urban population; and the shutdown of social services have had a huge impact on the functioning of the society and the social economy. In addition, the possible psychological effects on quarantined members of the community need to be evaluated in the long term.
Our study has several limitations. First, although these hospitals are the two main TCs in the Anhui province, they still cannot cover all patients with injuries. Admission bias is unavoidable. Second, we only studied the relationship between the number of injury patients and the number of COVID-19-associated cases in Anhui, which may not represent the implementation of strategies in other regions. Finally, we mainly described the correlation between injuries and COVID-19-associated cases to attempt to evaluate the strategy of community quarantine; more rigorous multicenter statistical analysis of the strategy on the impact of outbreaks and injuries are needed in the future.
5. Conclusion
We described a strategy of community quarantine adopted for the outbreak of COVID-19 in Anhui, where nearly 1000 confirmed cases were cured within 40 days. From the perspective of the differential distribution of injuries in TCs, this strategy was effectively implemented and significantly slowed the outbreak of COVID-19 in Anhui. However, the implementation and maintenance of the strategy of community quarantine is costly and requires the participation of the entire population.
Funding
No funding was provided specifically for this project.
Availability of data and materials
Please contact author for data requests.
Authors’ contributions
Xinyuan Li and Li Li conceived and designed the study. Wanbo Zhu and Changqing Xu collected the data. Wanbo Zhu and Xinyuan Li wrote the manuscript. Jiazhao Yang and Shiyuan Fang read, corrected, and approved the final manuscript. All authors read and approved the final manuscript.
Ethics approval and consent to participate
This study was approved by the ethics committee of the First Affiliated Hospital of USTC and Southern Brach of Anhui Provincial Hospital. As for this research, an optout of the informed consent, the information disclosure, and a negative opportunity are guaranteed in the Ethical approval.
Consent for publication
All the patients in this study have given their informed consent for the article to be published.
Competing interests
The authors declare that they have no competing interests.
Acknowledgements
Not applicable.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.ijid.2020.04.016
Appendix A. Supplementary data
The following are the supplementary data to this article:
References
- Albarello F., Pianura E., Di Stefano F., Cristofaro M., Petrone A., Marchioni L. 2019-novel Coronavirus severe adult respiratory distress syndrome in two cases in Italy: an uncommon radiological presentation. Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan J.F.-W., Yuan S., Kok K.-H., To K.K.-W., Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- China NHCotPsRo. Diagnosis and treatment of pneumonia caused by novel coronavirus infection (trial version III). http://wwwnhcgovcn/yzygj/s7653p/202001/f492c9153ea9437bb587ce2ffcbee1fashtml 2020.
- Koo J.R., Cook A.R., Park M., Sun Y., Sun H., Lim J.T. Interventions to mitigate early spread of SARS-CoV-2 in Singapore: a modelling study. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30162-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauer S.A., Grantz K.H., Bi Q., Jones F.K., Zheng Q., Meredith H.R. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Intern Med. 2020 doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin Q., Zhao S., Gao D., Lou Y., Yang S., Musa S.S. A conceptual model for the coronavirus disease 2019 (COVID-19) outbreak in Wuhan, China with individual reaction and governmental action. Int J Infect Dis. 2020;93:211–216. doi: 10.1016/j.ijid.2020.02.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu R., Zhao X., Li J., Niu P., Yang B., Wu H. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan X., Chen D., Xia Y., Wu X., Li T., Ou X. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30114-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao A., Vazquez J.A. Identification of COVID-19 can be quicker through artificial intelligence framework using a mobile phone-based survey in the populations when cities/towns are under quarantine. Infect Control Hosp Epidemiol. 2020:1–18. doi: 10.1017/ice.2020.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohrabi C., Alsafi Z., O’Neill N., Khan M., Kerwan A., Al-Jabir A. World Health Organization declares Global Emergency: a review of the 2019 Novel Coronavirus (COVID-19) Int J Surg. 2020 doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian H., Liu Y., Li Y., Wu C.H., Chen B., Kraemer M.U.G. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020 doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Wang Y., Chen Y., Qin Q. Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID-19) implicate special control measures. J Med Virol. 2020 doi: 10.1002/jmv.25748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong P., Guo S., Chen T. Correlation between travellers departing from Wuhan before the Spring Festival and subsequent spread of COVID-19 to all provinces in China. J Travel Med. 2020 doi: 10.1093/jtm/taaa036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu W., Xie K., Lu H., Xu L., Zhou S., Fang S. Initial clinical features of suspected Coronavirus Disease 2019 in two emergency departments outside of Hubei, China. J Med Virol. 2020 doi: 10.1002/jmv.25763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu W., Yang J., Xu L., Fang S. A plunge in the number of traumatic traffic injuries in an emergency center in Anhui province, China. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Please contact author for data requests.