Dear Editor,
Tang JW, et al. and colleagues have written to this Journal describing the emergence of 2019 novel coronavirus disease (COVID-19).1 We have had an opportunity to examine in detail the chest computed tomography (CT) findings in cases with microbiologically confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection, to familiarize radiologists and clinicians with the imaging manifestations of this new outbreak. Meanwhile, we also studied the clinical characteristics of the cases, combined with CT manifestations, to provide more clues for the correct diagnosis of the disease.
Fourteen patients (P1-P14) aged from 10 to 75 years were referred to the fever clinic of our hospital, 7 of them (P8-P14) were from Hui-Ya branch of our hospital. P9 and P14 had diabetes and other patients had no underlying diseases. Among the 14 cases, 10 of them had a history of exposure to Wuhan or Hubei, while, P6 and P7 had no clear epidemiological history. P3/P4, P10/P11 were family clustering disease. All the patients performed oropharyngeal swabs test and confirmed as COVID-19. Common respiratory viruses, mycoplasma and chlamydia were negative. For patients’ venous blood tests at disease onset, as given in (Table 1 ), we found that leucocytes and lymphocytes were slightly decreased or normal, eosinophil count were slightly decreased in 12 cases and normal in 2 cases. Neutrophil counts were normal for all the patients, and CRP was increased in 6 cases. PCT was normal or slightly elevated.
Table 1.
Clinical characteristics of the 14 patients infected with 2019-nCoV.
| Patient | Gender | Age, years | Epidemiology | 2019-nCoV-RNA test results of oropharyngeal swabs | Chief complaint | CRP, mg/L, 0.00-10.00 | WBC#, x10^9/L, 4.00-10.00 | NEUT#, x10^9/L, 1.80-6.40 | LY#, x10^9/L, 1.00-3.30 | EO#, x10^9/L, 0.05-0.50 | PCT, ng/mL, 0.00-0.05 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| P1 | F | 27 | Went to Wuhan 17 days ago | The second test was positive | Fever (<38°) | 5.78 | 3.77 | 2.55 | 0.98 | 0.01 | NA |
| P2 | F | 32 | Went to Wuhan 12 days ago | Two tests were positive | Fever for 1 day (<38°) | 1.47 | 3.40 | 2.22 | 0.80 | 0.01 | NA |
| P3 | F | 56 | Went to Hubei 1 day ago | The first test was positive | Fatigue and fever for 1 day (<38°) | 6.40 | 5.69 | 3.45 | 1.42 | 0.20 | 0.04 |
| P4 | F | 32 | Family cluster with P3 | The second test was positive | Fever for 1 hour (<38°) | 1.60 | 6.87 | 5.30 | 1.01 | 0.12 | 0.04 |
| P5 | F | 63 | Went to Wuhan 2 days ago | Two tests were positive | Fever (<38°) | 2.85 | 4.08 | 3.13 | 0.55 | 0.01 | NA |
| P6 | F | 54 | No clear history related to Wuhan | The first test was positive | Fever (40°C) | 63.79 | 5.89 | 4.15 | 1.31 | 0.01 | NA |
| P7 | F | 49 | No clear history related to Wuhan | The first test was positive | Fever | 10.36 | 3.76 | 2.56 | 0.94 | 0.00 | NA |
| P8 | F | 35 | Went to Wuhan 14 days ago | The first test was positive, the second test was negative | Fever for half day (37.5°C) | 6.50 | 3.25 | 1.93 | 1.10 | 0.00 | 0.027 |
| P9 | F | 63 | Went to Wuhan 7 days ago | The fourth test was positive | Fever for 2 days (37.1°C) | 88.20 | 5.92 | 5.20 | 0.55 | 0.00 | 0.208 |
| P10 | M | 41 | Contacted with person from Wuhan 25 days ago | The first test was positive | Fever for 2 days (37.8°C) | 15.90 | 6.13 | 3.43 | 1.99 | 0.00 | 0.028 |
| P11 | F | 10 | Family cluster with P10 | Two tests were positive | Asymptomatic (37.1°C) | 0.00 | 6.92 | 5.11 | 1.59 | 0.00 | 0.020 |
| P12 | F | 66 | Went to Wuhan 4 days ago | The first test was positive | Dizziness, vomiturition, fever (38.9°C) and myalgia for more than 1 day | 25.80 | 6.84 | 4.99 | 1.56 | 0.00 | 0.065 |
| P13 | F | 54 | Went to Wuhan 3 days ago | The first test was positive | Chills and headache for 3 days, fever (37.6°C) for 1 day | 9.70 | 3.38 | 2.34 | 0.61 | 0.01 | 0.050 |
| P14 | M | 75 | From Wuhan | The first test was positive | Cough and fever 1 week (38.9°C) | 78.70 | 5.36 | 4.28 | 0.93 | 0.00 | 0.105 |
Abbreviations: F, female; M, male; CRP, C-reactive protein; WBC, white blood cells; NEUT, neutrophil; LY, lymphocyte; EO, eosnophils; #: cell count; NA, not applicable. Note: The normal reference value range is listed behind the blood test index.
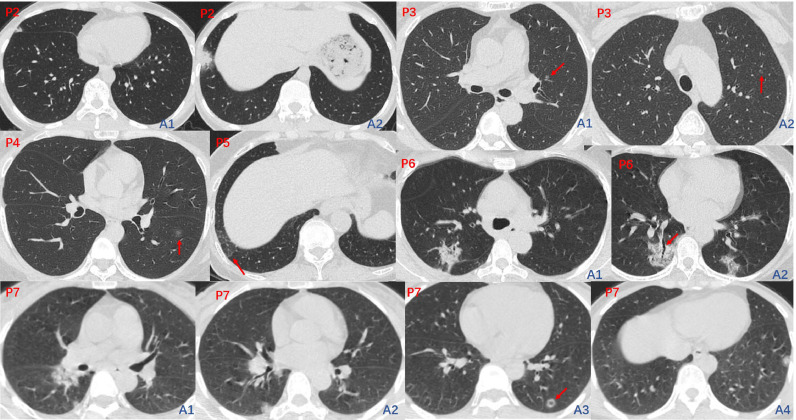
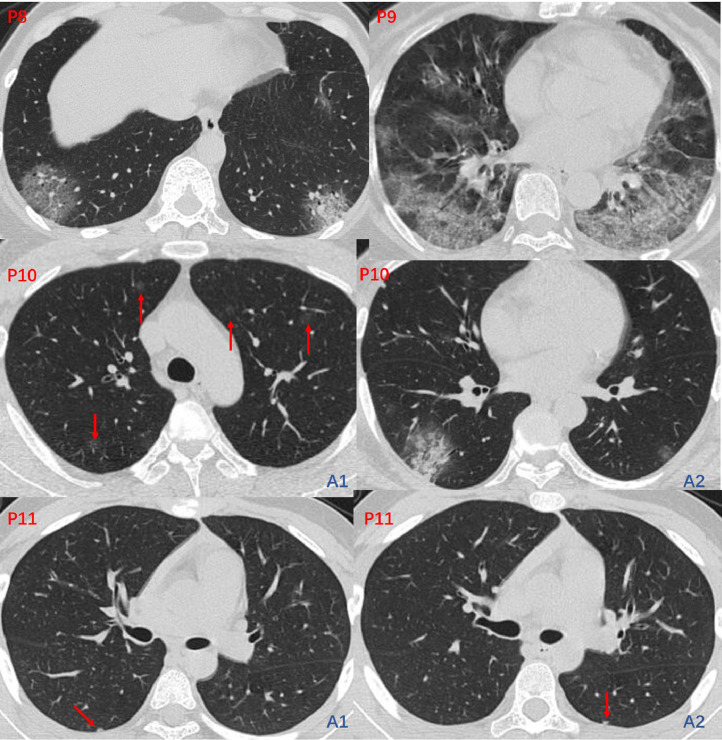
On admission, 11 patients (P1–P11) underwent high resolution chest CT examination and their manifestations were shown in (Table 2 ). P1 (Fig. 1, F0, A1–A4): CT images showed patchy-like pure ground glass opacity (GGO) involving subpleural regions of the right middle lobe (Fig. 1, F0, A3, arrow) and the right lower lobe. The slightly thickened interlobular septa within the lesion makes it appear the crazy paving sign (Fig. 1, F0, A2, arrowhead). P2 (Fig. 2, P2, A1-A2): CT images showed mixed GGO and consolidation that appeared at subpleural area of the right middle lobe and the right lower lobe. The lesion presented as patchy-like morphology. P3 (Fig. 2, P3, A1-A2): CT images showed two well circumscribed, round nodular-like GGO lesions (Fig. 2, P3, arrow) located in the central area of the left upper lobe. P4 (Fig. 2, P4): CT images showed a small nodular-like pure GGO (Fig. 2, P4, arrow) located in the central area of the left lower lobe. P5 (Fig. 2, P5): CT images showed a slight of irregular pure GGO (Fig. 2, P5, arrow) located in the subpleural region of the right lower lobe. P6 (Fig. 2, P6, A1-A2): CT images showed bilateral multi-focal mixed GGO and consolidation appeared at subpleural area of lung. Mild bronchiectasis (Fig. 2, P6, A2, arrow) can also be observed within the lesion. P7 (Fig. 2, P7, A1–A4): CT images showed bilateral subpleural lesions, among which the lesion in the left lower lobe was nodular-like with pseudocavitary sign (Fig. 2, P7, A3, arrow). P8 (Fig. 3, P8) and P9 (Fig. 3, P9): CT images showed bilateral subpleural lesions with crazy paving sign. P10 (Fig. 3, P10, A1-A2): CT images showed bilateral multiple lesions, some of them were pure GGO located in the central region of the lung. P11 (Fig. 3, P11, A1-A2): CT images showed bilateral subpleural small nodular-like lesions.
Table 2.
Imaging characteristics during the first visit.
| Imaging characteristics | P1 | P2 | P3 | P4 | P5 | P6 | P7 | P8 | P9 | P10 | P11 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lobar location | |||||||||||
| RUL | √ | √ | √ | √ | |||||||
| RML | √ | √ | √ | √ | |||||||
| RLL | √ | √ | √ | √ | √ | √ | √ | √ | √ | ||
| LUL | √ | √ | √ | √ | |||||||
| LLL | √ | √ | √ | √ | √ | √ | |||||
| Distribution | |||||||||||
| Subpleural | √ | √ | √ | √ | √ | √ | √ | √ | |||
| Random or diffuse | √ | √ | √ | ||||||||
| Morphology | |||||||||||
| Patchy-like | √ | √ | √ | √ | √ | √ | |||||
| Nodular-like | √ | √ | √ | ||||||||
| Both | √ | √ | |||||||||
| Contour | |||||||||||
| Clear | √ | √ | √ | ||||||||
| Blurry | √ | √ | √ | √ | √ | √ | √ | √ | |||
| Attenuation | |||||||||||
| GGO only | √ | √ | √ | √ | √ | ||||||
| Mixed GGO and consolidation | √ | √ | √ | √ | √ | √ | |||||
| Consolidation only | |||||||||||
| Other signs | |||||||||||
| Reticulation | √ | ||||||||||
| crazy paving | √ | √ | √ | √ | |||||||
| Cavitation | |||||||||||
| Bronchiectasis | √ | ||||||||||
| Pleural effusion | |||||||||||
| Lymphadenopathy | |||||||||||
Abbreviations: RUL-right upper lobe, RML-right middle lobe; RLL-right lower lobe, LUL-left upper lobe, LLL-left lower lobe; GGO, ground glass opacity. "P#" represents one patient. Note: Check mark (√) indicate the appearance of the corresponding sign.
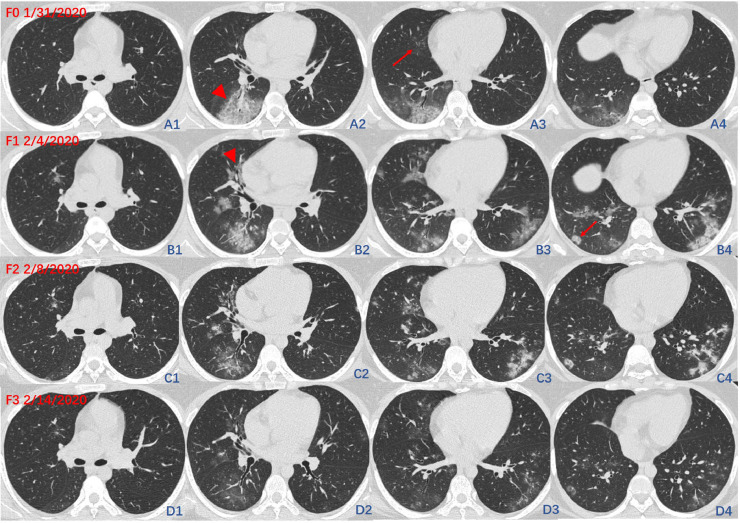
Fig. 1.
The initial CT images (F0) and three times of follow-up CT images (F1–F3) of P1. F0 showed patchy-like pure GGO located in the subpleural regions of the right middle lobe (F0, A3, arrow) and the right lower lobe, accompanied by crazy paving sign (F0, A2, arrowhead). Follow-up 1(F1, B1–B4): CT images showed diseases progression. The lesions manifested as coexisted nodular-like (F1, B4, arrow) and patchy-like lesions as well as peribronchial (F1, B2, arrowhead), central and subpleural distribution. The lesions are migratory manifested as the absorption of the primary lesions and the emergence of new lesions. CT images of Follow-up 2 (F2, C1–C4) and Follow-up 3 (F3, D1–D4) showed lesion absorption.
Fig. 2.
The initial CT images of P2-P7. CT images of P2 (Fig. 2, P2, A1-A2), P5 (Fig. 2, P5), P6 (Fig. 2, P6, A1-A2) and P7 (Fig. 2, P7, A1–A4) showed subpleural lesions, a nodular-like lesion with pseudocavitary sign (Fig. 2, P7, A3, arrow) and mild bronchiectasis (Fig. 2, P6, A2, arrow) were also observed within the lesion. CT images of P3 (Fig. 2, P3, A1-A2) and P4 (Fig. 2, P4) showed round nodular-like GGO lesions (P3 and P4, arrow) located in the central area of the lung.
Fig. 3.
The initial CT images of P8-P11. CT images of P8 (Fig. 3, P8) and P9 (Fig. 3, P9) showed bilateral subpleural lesions with crazy paving sign. CT images of P10 (Fig. 3, P10, A1-A2) showed bilateral multiple lesions, some of them were pure GGO located in the central region of the lung. CT images of P11 (Fig. 3, P11, A1-A2) showed bilateral subpleural small nodular-like lesions.
P1 had three follow-up CTs (Fig. 1, F1–F3). The time interval between initial chest CT and follow-up were 4, 8, 14 days. Follow-up 1(Fig. 1, F1, B1–B4): CT images showed diseases progression. The lesions showed diversified morphology and distribution, appearing as coexisted nodular-like (Fig. 1, F1, B4, arrow) and patchy-like lesions as well as peribronchial (Fig. 1, F1, B2, arrowhead), central and subpleural distribution. CT images of F1 showed the that lesions were migratory manifested as the absorption of the primary lesions and the emergence of new lesions. CT images of Follow-up 2 (Fig. 1, F2, C1-C4) and Follow-up 3 (Fig. 1, F3, D1–D4) showed the diseases were obviously absorbed.
In the current study, we investigated the detailed information including clinical features and CT imaging characteristics of 6 patients with COVID-19. Our research has some new findings on the basis of previous study: (1) The decrease of eosinophil count may be helpful for the early diagnosis of the disease. Nevertheless, till now, there is no study refer to blood tests2 , 3 mentioned eosinophil, which is worthy of further study. (2) Our CT study found that COVID-19 has a variety of manifestations. In the early stage of the disease, the lesion can manifest as round nodular-like GGO in the central area of the lung lobe, which is different from the common imaging manifestations that are patchy-like lesion in subpleural region.4, 5, 6 (3) The follow-up CT images showed the lesions are migratory manifested as the absorption of the primary lesions and the emergence of new lesions, which had not been reported yet. (4) The false negative rate of oropharyngeal swabs seems high. As we know that, oropharyngeal swabs are the recommended upper respiratory tract specimen types for SARS-CoV-2 diagnostic testing,7 , 8 so a new detection technique should be developed as soon as possible.
Declaration of Competing Interest
The authors declare that they have no competing interests.
References
- 1.Tang J.W., Tambyah P.A., Hui D.S.C. Emergence of a novel coronavirus causing respiratory illness from Wuhan, China. J Infect. 2020 Jan 28 doi: 10.1016/j.jinf.2020.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223) doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang D., Hu B., Hu C. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Song F., Shi N., Shan F. Emerging Coronavirus 2019-nCoV Pneumonia. Radiology. 2020 doi: 10.1148/radiol.2020200274. [DOI] [Google Scholar]
- 5.Xie X., Zhong Z., Zhao W. Chest CT for Typical 2019-nCoV Pneumonia: Relationship to Negative RT-PCR Testing. Radiology. 2020 doi: 10.1148/radiol.2020200343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pan Y., Guan H., Zhou S. Initial CT findings and temporal changes in patients with the novel coronavirus pneumonia (2019-nCoV): a study of 63 patients in Wuhan, China. Eur Radiol. 2020 doi: 10.1007/s00330-020-06731-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan J.F., Yuan S., Kok K.H. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223) doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.To K.K., Tsang O.T., Chik-Yan Yip C. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa149. [DOI] [PMC free article] [PubMed] [Google Scholar]