Highlights
-
•
SARS-CoV-2 may impair host antiviral response, causing subsequent hyperinflammation.
-
•
SARS-CoV-2 likely deranges the renin angiotensin aldosterone system (RAAS).
-
•
Hyperinflammation and RAAS imbalance may drive acute lung injury and coagulopathy.
-
•
RAAS imbalance impairs fibrinolysis, which can result in relative hypofibrinolysis.
-
•
This can lead widespread immunothrombosis, contributing to multi-organ damage.
Keywords: Thrombosis, Endothelial dysfunction, Coagulation, Coronavirus, COVID-19
Abstract
Early clinical evidence suggests that severe cases of coronavirus disease 2019 (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), are frequently characterized by hyperinflammation, imbalance of renin-angiotensin-aldosterone system, and a particular form of vasculopathy, thrombotic microangiopathy, and intravascular coagulopathy. In this paper, we present an immunothrombosis model of COVID-19. We discuss the underlying pathogenesis and the interaction between multiple systems, resulting in propagation of immunothrombosis, which through investigation in the coming weeks, may lead to both an improved understanding of COVID-19 pathophysiology and identification of innovative and efficient therapeutic targets to reverse the otherwise unfavorable clinical outcome of many of these patients.
1. Introduction
Early clinical evidence suggests that severe cases of coronavirus disease 2019 (COVID-19), the new pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) are frequently characterized by hyperinflammation, renin-angiotensin-aldosterone system imbalance, and a particular form of vasculopathy, thrombotic microangiopathy, and intravascular coagulopathy. In previous studies we have identified admission D-dimer [1], prothrombin time (PT) [2], and thrombocytopenia [3] as prognostic markers of severe disease and/or mortality in COVID-19. We suspect that elevated D-dimer values at hospital admission and during further disease progression may be reflective of COVID-19-induced pulmonary inflammation with local activation of platelets and blood coagulation, accompanied by relative hypofibrinolysis, which later spills into systemic circulation [4]. Moreover, we have also reported elevated values of lactate dehydrogenase (LDH) and bilirubin, frequently associated with decreased hemoglobin concentration, in patients with severe and fatal COVID-19 [2] which, given all the above and combined with clinical observations, suggests the potential of hyperinflammation, leading to a thrombotic microangiopathy-like phenomenon.
The occurrence of this thrombotic phenomenon in COVID-19 is supported by a recent autopsy report, which described multiple occlusions and microthrombi in pulmonary vasculature.[5] In a Dutch cohort of critically ill patients receiving prophylaxis with low molecular weight heparin (LMWH; standard or increased dosage), diagnostic imaging in patients with symptoms suggestive of thromboembolism, found venous thrombotic events in 27% of severe cases, and arterial thrombotic events in in 3.7% of COVID-19 patients [6]. The development of multiple and likely primary microthrombi within the pulmonary vasculature may explain the rapid deterioration and pulmonary collapse that is observed in patients who suddenly progress to acute respiratory distress syndrome (ARDS) with significant pulmonary edema, hypoxemia, V/Q mismatch and shunting. With progressive hyperinflammation, a systemic microangiopathy may lead to multiple organ dysfunction syndrome (MODS), encompassing cardiomyopathy, acute kidney and liver failure, mesenteric ischemia, and neurological insults.
Hemostasis is intrinsically tied to inflammatory and immunologic responses. We proffer, based on animal models and in vitro studies of SARS-CoV-1, as well as reported data thus far on COVID-19, that SARS-CoV-2 impairs innate and adaptive antiviral responses, triggers hyperinflammation, and deranges the renin-angiotensin-aldosterone system (RAAS), all culminating to promote detrimental hypercoagulability and immunothrombosis. SARS-CoV-1 and SARS-CoV-2 share up to 85% genomic identity, and both utilize the same primary human host receptor, angiotensin converting enzyme 2 (ACE2), to enter target cells [7]. Due to their homology, similar clinical and immunopathologic aspects are expected to occur, but differences may also exist, and caution is needed when extrapolating data from SARS to COVID-19. For example, the binding affinity for ACE2 of the spike surface glycoprotein of SARS-CoV-2 is considerably higher than that of the homologous protein on SARS-CoV-1, thus potentially magnifying virulence and pathogenicity in vivo of the more recent SARS-CoV-2 coronavirus.
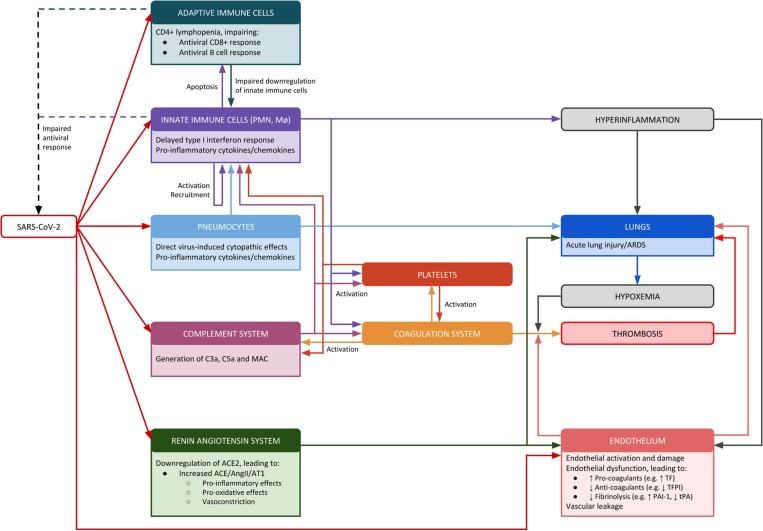
In this paper, we present an immunothrombosis model of COVID-19, as shown in Fig. 1 . We discuss the underlying pathogenesis and the interaction between multiple systems, resulting in propagation of hyperinflammation and immunothrombosis which, through investigation in the coming weeks, may lead to both improved understanding of COVID-19 pathophysiology and identification of novel therapeutic targets.
Fig. 1.
Pathophysiologic Model of Immunothrombisis in COVID-19. SARS-CoV-2 is associated with an impaired antiviral host response, leading to rapid viral replication and a subsequent hyperinflammatory state. The hyperinflammation and virus-induced dysregulation of the renin angiotensin aldosterone system (RAAS) induces acute lung injury, leading to hypoxemia. Together, hyperinflammation, RAAS and hypoxemia induces endothelial dysfunction and a hypercoagulable state leading to widespread immunothrombosis which further propagates organ damage. ACE = angiotensin converting enzyme, ACE2 = angiotensin converting enzyme 2, AngII = angiotensin II, ARDS = acute respiratory distress syndrome, AT1 = angiotensin II receptor type 1, MAC = membrane attack complex, Mø = monocytes/macrophages, PAI-1 = plasminogen activator inhibitor-1, PMN = polymorphonuclear neutrophils, SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2, TF = tissue factor, TFPI = tissue factor pathway inhibitor, tPA = tissue plasminogen activator.
2. Hyperinflammation
Innate immune cells express pattern recognition receptors (PRRs) which can recognize molecular patterns associated with pathogens (PAMPs) or danger (DAMPs). RNA viruses (like SARS-CoV-2) can be recognized by endosomal and cytoplasmic PRRs (including TLR3, TLR7, RIG-I and MDA-5), leading to production of type I interferons (IFNs) [8]. Type I IFNs (IFN-α and IFN-β) are key players in the host response against viral infections, as they block viral replication and augment antiviral effector mechanisms [8]. SARS-CoV-1 (and likely the homologous SARS-CoV-2) express proteins that inhibit type I IFN production (e.g. through inhibition of TLR3 and TLR7 signaling pathways), which delays the antiviral response and facilitates rapid viral replication and extensive virus-induced direct cytopathic effects in early stages of disease [9], [10], [11]. A subsequent dysregulated, delayed and persistent type I IFN response will, together with cytokines, chemokines and DAMPs released from infected pneumocytes, may orchestrate excessive infiltration of monocyte/macrophages (Mø) and neutrophils (PMNs) in lung parenchyma [12]. These Mø and PMNs can in turn produce high levels of pro-inflammatory cytokines (including interleukin (IL) 1β, IL-6 and tumor necrosis factor alpha (TNFα)) and chemokines, which further amplify the recruitment of innate immune cells, potentially culminating in hyperinflammation and the observed cytokine storm that characterizes the most severe cases of COVID-19 [13]. The association between timing of type I IFN response and disease severity has been demonstrated in a mouse model of SARS [12]. Early administration of recombinant IFN-β protected mice from clinical disease, while an aberrant delayed and persistent type I IFN response was associated with severe lung damage, with massive immune cell infiltration, high levels of pro-inflammatory cytokines, vascular leakage and alveolar edema [12]. Importantly, mice lacking type I IFN receptors (Ifnar-/-) had a mild disease, with markedly reduced pulmonary immunopathology [12]. This illustrates that antiviral type I IFNs may contribute to pulmonary immune cell infiltration and detrimental hyperinflammation if their expression is dysregulated. Furthermore, the same animal model of SARS confirmed that excessive Mø recruitment and activation plays a central role in pulmonary immunopathology, as Mø depletion ameliorated lung damage, without significantly affecting the viral load [12].
COVID-19 is associated with CD4+ and CD8+ T-cell lymphopenia, which may result from a combination of virus-induced direct cytopathic effects, as well as enhanced T-cell apoptosis due to a dysregulated cytokine milieu [14], [15]. CD4+ T-cells are important for modulating the immune response, and the CD4+ T-lymphopenia observed in SARS was thought to contribute to hyperinflammation through impaired downregulation of the inflammatory process [16], [17]. Furthermore, CD4+ T-lymphopenia may impair the adaptive antiviral response through inadequate T-cell help to virus-specific CD8+ cytotoxic T-cells and B-cells.
Data from China and Italy show that approximately 64–71% of deceased COVID-19 patients are male [18], [19], which has largely been attributed to gender differences in some risk factors (e.g., comorbidities) [20]. However, immunobiological sex differences may also contribute. The TLR7 gene is located on chromosome X, and escapes X chromosome inactivation, resulting in enhanced expression in females [21]. TLR7 agonists induce more pronounced IFN-α release from cells in females [22], and estradiol enhances type I IFN release following TLR7 agonism [23]. Biallelic TLR7 expression and estradiol signaling may potentially render females less prone to the viral type I IFN antagonism, which may lead to a more substantial type I IFN response in early stages of disease. This may potentially improve the initial antiviral response and prevent the subsequent aberrant hyperinflammation, in part explaining increased disease severity in males. However, this theory requires additional studies.
Taken together, viral type I IFN antagonism may trigger a cascade of events leading to extensive virus-induced direct cytopathic effects (with release of DAMPs and cytokines from infected cells) and dysregulated type I IFN response. This contributes to excessive Mø and PMN infiltration and T-cell apoptosis, resulting in a gradually increasing hyperinflammatory state. As explained next, hyperinflammation may contribute to development of various forms of intravascular coagulopathy, which in turn fosters the inflammatory response.
3. Immunothrombosis
The hyperinflammatory profile promotes endothelial cell activation and endothelial dysfunction, which may induce a prothrombotic state. There is extensive interplay between the hemostasis and innate immune systems. During infection, platelets, coagulation factors and innate immune effector systems (such as Mø, PMNs and the complement system) interact to form clots in a process termed immunothrombosis (also known as thromboinflammation) [24], [25], [26]. While this is inherently beneficial via inhibiting spread of the pathogen, providing structural support for the endothelium and a site for activation of innate immune cells, uncontrolled and widespread immunothrombosis may result in a potentially devastating microangiopathy, which can contribute to progression to general and COVID-19-induced ARDS [26], [27].
The concept of immunothrombosis requires a basic understanding of the involved processes and their interactions. The coagulation system is activated through the tissue factor (’extrinsic’) pathway, is amplified by the formerly known ‘intrinsic’ pathway (now called “thrombin burst”), which finally converges to activate the ‘common’ pathway, where Factor Va (FVa) and FXa converts prothrombin into thrombin [28]. Thrombin then converts fibrinogen into fibrin, which is stabilized into the clot by FXIIIa activity. Clots are broken down by plasmin, in a process called fibrinolysis, initiated by two proteins that convert plasminogen to plasmin, tissue plasminogen activator (tPA) and urokinase plasminogen activator (uPA). tPA is more specific to the breakdown of fibrin, while uPA is involved in acute inflammation, wound healing and tissue repair [29]. Both tPA and uPA are inhibited by plasminogen activator inhibitor-1 (PAI-1). The balance between tPA/uPA and PAI-1 ensures balanced homeostasis. However, in general ARDS (and likely COVID-19 induced ARDS), this balance is disturbed, with excessive PAI-1 resulting in relative hypofibrinolysis leading to fibrin deposition in the alveoli and perialveolar capillary microthrombosis [29].
During inflammation, it has been convincingly shown that both the extrinsic (i.e., tissue factor; TF) and intrinsic (i.e., FXII) coagulation pathways can be activated. The extrinsic pathway is initiated by TF, which in inflammatory states is expressed by activated endothelial cells and Mø [26]. Furthermore, PMNs can release neutrophil extracellular traps (NETs) containing DAMPs and various other bioactive molecules in a process called NETosis. NETs stimulate the intrinsic pathway through activation of FXII. NETs also activate endothelial cells, platelets and complement system, and contain proteases which inactivates endogenous anticoagulants, thus propagating the pro-coagulant state [30]. While NETosis is typically associated with responses against extracellular pathogens, increasing evidence show that NETosis also occurs in viral infections [31]. Excessive NETs contribute to acute lung injury in influenza pneumonitis [32], but further studies are needed to determine their contribution in COVID-19.
Platelets have well-known roles in coagulation, but they also exert pro-inflammatory effects [33]. Platelet activation leads to changes in their shape and release of their stored granules. Platelet alpha granules contain immunostimulatory molecules which are involved in activation and recruitment of PMNs and Mø, including platelet factor 4 (CXCL4), proplatelet basic protein, neutrophil-activating peptide-2 (CXCL7) and stromal cell-derived factor [33]. Activated platelets are also an important source of pro-inflammatory IL-1β [33], underlying their role in the immunothrombotic process. P-selectin from stored granules is upregulated at the surface of activated platelets, and this facilitates interactions with recruited PMNs, thus resulting in platelet-neutrophil complexes [34]. Furthermore, activated platelets can stimulate the recruited PMNs to undergo NETosis, which in turn activates platelets, creating a feedback loop [34]. Though this may be preliminarily beneficial by helping to sequester the spread of infection, accumulation of platelet-neutrophil complexes may result in vaso-occlusive thrombi and MODS [27].
Platelets can activate the coagulation pathway and vice versa, and the interaction between platelet and coagulation proteins plays an intrinsic role in the regulation of both these active players. Activated platelets provide an exposed surface (especially phospholipids) for assembly of enzyme-cofactor-substrate complexes throughout the coagulation cascade.[35] Platelets help sequester coagulation to the site of the hemostatic thrombus. This protects the coagulation proteins from inactivation by both plasma and platelet inhibitors and prevents disseminated intravascular coagulopathy (DIC) [35].
The concept of immunothrombosis is further highlighted by the intricate cross talk between the coagulation system and the complement system [30]. The complement system is composed of circulating proteins and is part of the innate immune system [36]. The complement system can be activated through three pathways (classical pathway, alternative pathway, lectin pathway), which converge on the proteolytic cleavage of complement protein C3 [36]. Complement activation induces a cascade of events, culminating in generation of pleiotropic bioactive molecules, such as C3a, C5a and membrane attack complex (MAC) [36]. A mouse model of SARS demonstrated that dysregulated complement activation contributed to immunopathology, as C3 knock out mice (C3–/-) demonstrated less lung damage and systemic inflammation with similar viral loads as compared to control mice [37]. C3a and C5a exert a multitude of pro-inflammatory effects, including mast cell degranulation and Mø and PMN recruitment [36]. However, they also exert pro-thrombotic effects through activation of platelets and endothelial cells, as well as increasing tissue factor and von Willebrand factor (VWF) expression [30]. Other proteins of the complement system (MASP-1 and MASP-2) also contribute to the generation of a hypercoagulable state, by converting prothrombin to thrombin and fibrinogen to fibrin [30]. Activated components of the coagulation cascade (including thrombin) can in turn activate C3 and C5 [30], thereby augmenting the immunothrombotic interplay between the coagulation and complement systems.
Since vascular endothelium actively expresses ACE2, and was shown to be an active site of SARS-CoV-1 infection [38], it is obviously plausible that SARS-CoV-2 is capable of directly infecting these cells, as also recently argued by Nicin et al [39]. A recently published histopathology report demonstrated endothelial cell infection and endotheliitis in 3 patients with COVID-19 [40]. Notwithstanding direct viral cytopathic effects, as hyperinflammation drives forward local and systemic endothelial dysfunction and injury, this results in increased vascular permeability, excess thrombin generation (also a major activator of platelets) and inhibition of fibrinolysis [27]. In patients with non-specific ARDS, plasma levels of TF and PAI-1 are significantly elevated compared to non-ARDS patients, leading to a lung coagulopathy driven by increased thrombin generation and bronchoalveolar depression of fibrinolysis [41], [42]. Moreover, we proffer that the increased risk of severe and fatal COVID-19 in patients with comorbidities such as diabetes, hypertension, and obesity may in part be due to the underlying endothelial dysfunction, which is common in these conditions.
Upregulation of pro-coagulants is driven by pro-inflammatory cytokines, in particular, IL-1β, IL-6, and TNFα, which we have identified to be significantly elevated in patients with COVID-19 [2]. These cytokines promote release of ultralarge VWF multimers, production of TF and FVII/FVIIa leading to increased thrombin generation, and decrease levels of endogenous anticoagulants such as tissue factor pathway inhibitor (TFPI), antithrombin, and activated protein C [43]. The extensive interplay between endothelial cells, platelets, Mø, PMNs, the complement system and the coagulation system results in a hypercoagulable state with increased levels of procoagulants, decreased levels of anticoagulants, and depressed fibrinolysis. Though elevated D-dimers are reported in patients with severe COVID-19, we suspect this reflects the significant imbalance in thrombin generation and fibrinolysis, especially in the pulmonary vasculature. In both general ARDS and sepsis, significant evidence supports a procoagulatory state characterized by massive thrombin production [44]. More specific to coronaviruses, SARS-CoV-1 was shown to upregulate hfgl2 prothrombinase gene, which may further contribute to thrombin generation and hypercoagulable state in COVID-19 [45].
Overall, as hyperinflammation progresses systematically, these processes may culminate in widespread immunothrombosis, contributing to organ dysfunction. The hypercoagulable state may potentially be further enhanced by other clinical factors including hypoxemia (secondary to ALI/ARDS), hyperthermia (which may activate platelets and coagulation), and/or hypovolemia (secondary to gastrointestinal fluid loss and/or negative fluid balance in the ARDS treatment protocol) [46]. Hypoxemia triggers increased expression of hypoxia inducible factors (HIF). This may promote further inflammation, thus augmenting blood viscosity and contributing to worsen hypercoagulability. Moreover, HIFs may directly activate platelets and coagulation factors, increasing TF expression, increasing PAI-1, and inhibiting the endogenous anticoagulant protein S [44].
An early study suggested that anticoagulation with LMWH may be associated with better prognosis in patients with severe COVID-19 [47]. Heparin, in addition to acting as an anticoagulant, has some anti-inflammatory properties that may be beneficial in COVID-19.[4] In general ARDS, a meta-analysis reported that LMWH administration during the initial first week of onset was associated with 37% reduction of 28-day mortality [48]. In a small recent case series of 3 COVID-19 patients, administration of tPA resulted in a transient improvement in pulmonary function [49]. However, the use of anti-coagulants and fibrinolytics in COVID-19 requires further study, including identification of components most deranged in order to enable effective targeted therapy.
A recent study showed the presence of antiphospholipid (aPL) antibodies in patients with COVID-19 [50]. Antiphospholipid syndrome (APS) is defined by arterial and/or venous thrombosis (or relevant pregnancy morbidity in the case of obstetric APS) plus positive aPL IgG and/or IgM antibodies (anticardiolipin (aCL) and/or β2glycoprotein I (aβ2GPI)) and/or lupus anticoagulant (LAC). In order to diagnose APS in the setting of thrombosis, the aPL and/or LAC positivity must be present on two occasions, with a minimum 12-week interval. Importantly, transient aPL antibody positivity is frequently seen in infection, and this does not necessarily confer clinical significance. In the abovementioned study, positive aCL IgA and aβ2GPI IgA/IgG were described (titers and assay method not provided). LAC was negative, and repeat aPL antibody testing was unavailable [50]. Hence this finding may very well represent non-specific (and clinically insignificant) transient infection related aPL antibody positivity (in the setting of COVID-19 induced non-APS immunothrombosis) rather than true APS.
4. Renin-Angiotensin-Aldosterone-System (RAAS) derangement
RAAS dysfunction plays a significant role in the pathophysiology of general ARDS [51], [52]. The SARS-CoV-2 host receptor, ACE2, is a major component of RAAS [7]. Thus, we hypothesize that RAAS aberrations significantly contribute to the likelihood of developing severe COVID-19 [53], [54].
ACE converts angiotensin I (AngI) to angiotensin II (AngII), while ACE2 converts AngII to angiotensin 1–7 (Ang1-7). AngII binds AngII receptor type 1 (AT1) and exerts pro-inflammatory, pro-oxidative, vasoconstrictive and even fibrotic effects.[53] In opposition, Ang1-7 binds to the Mas receptor (MasR) and mediates anti-inflammatory, anti-oxidative and vasodilatory effects [53]. We postulate that SARS-CoV-2 binding to ACE2 attenuates ACE2 activity via internalization, skewing the ACE/ACE2 balance to a state predominated by high levels of AngII, which causes pulmonary vasoconstriction and inflammatory, oxidative and fibrotic organ damage, ultimately progressing towards ALI/ARDS.
COVID-19 appears more severe in patients with hypertension, cardiovascular disease, and diabetes [55]. These disorders are associated with reduced baseline levels of ACE2 expression, which we proffer makes them more susceptible to SARS-CoV-2 mediated ACE/ACE2 imbalance [56].
In an animal model with SARS-CoV-1, the spike protein induced acute lung injury, which was improved with AT1 blocker (angiotensin receptor blocker, ARB) [57]. Liu et al. observed in a small sample of COVID-19 patients that plasma concentrations of AngII in COVID-19 infected patients were significantly higher than in healthy individuals [58]. Moreover, they observed that AngII levels in COVID-19 patients were correlated with viral load and lung injury, suggesting that COVID-19 induces an imbalanced RAAS and predominant ACE/AngII signaling may be a major driver of ARDS. Pulmonary vasoconstriction due to increased AngII may also increase hypoxemia which can influence hypercoagulability as previously described.
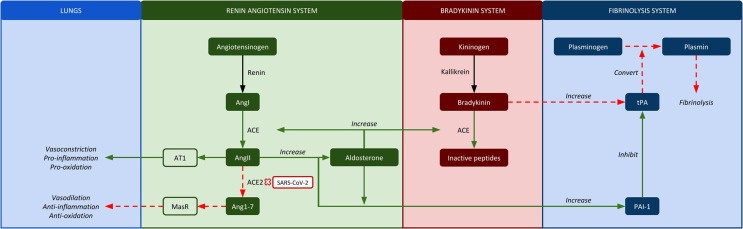
The RAAS system is intrinsically linked to the coagulation cascade and may exacerbate the processes of immunothrombosis, further driving microthrombi formation in COVID-19 (Fig. 2 ). First, AngII induces TF and PAI-1 expression by endothelial cells via the AT1 receptor, contributing to a PAI-1/tPA imbalance and a hypercoagulable state [59], [60]. This may explain why unresolved fibrin deposits are observed in the alveoli of patients with general ARDS, a feature that has also been observed in lungs of both SARS and COVID-19 victims [29], [37], [61]. Interestingly, AngII also stimulates PAI-1 release from adipocytes via AT1 receptors, and may in part account for the increased severity observed in those with high BMI [62].
Fig. 2.
Potential interactions between renin angiotensin system, bradykinin system and fibrinolysis in severe COVID-19. Arrows demonstrate interactions. Italic script depicts the function of the molecule/enzyme in a normal state. The color of the arrows demonstrate how SARS-CoV-2 may influence their function. Green solid arrow means that the process (in italics) is enhanced in COVID-19, while red dashed arrow means that the process (in italics) is suppressed in COVID-19. As an example, in COVID-19 decreased ACE2 increases AngII, which increases aldosterone, which augments ACE expression, causing increased breakdown of bradykinin, thereby preventing the normal bradykinin-mediated increase in tPA). ACE = angiotensin converting enzyme, ACE2 = angiotensin converting enzyme 2, AngI = angiotensin I, AngII = angiotensin II, Ang1-7 = angiotensin 1–7, AT1 = angiotensin II receptor type 1, MasR = Mas receptor, PAI-1 = plasminogen activator inhibitor-1, SARS-CoV-2 = severe acute respiratory syndrome coronavirus 2, tPA = tissue plasminogen activator. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Secondly, ACE metabolizes bradykinin. Bradykinin can stimulate vasodilation and release of tissue plasminogen activator (tPA) from endothelial cells [63]. How the kallikrein-bradykinin pathway would be altered by COVID-19 induced RAAS derangement is unclear. It can be assumed that an inflammatory response to COVID-19 would lead to increased bradykinin production (and hence increased tPA expression). However, elevated AngII would lead to increased aldosterone that may further enhance ACE activity, which converts bradykinin to inactive peptides, blunting the bradykinin-mediated tPA increase [64]. A hyperaldosterone state is suspected in severe COID-19 based on observations of hypokalemia [65]. Aldosterone levels have been shown to correlate with PAI-1 levels [66]. Moreover, aldosterone has also been shown to directly increase PAI-1 expression, especially in renal tissue [67], [68], [69].
Hence, while bradykinin (and hence tPA) may be increased, the increased ACE, AngII and aldosterone (and hence PAI-1) is likely to be of greater magnitude, leading to a decreased tPA to PAI-1 ratio, promoting hypofibrinolysis. In addition to the microthrombi, this imbalance (low tPA and low uPA to high PAI-1 ratio) may lead to poor resolution of alveolar lesions and explain the significant degree of fibrosis observed in COVID-19 patients [29], [61].
Overall, high levels of AngII may exacerbate any active or underlying endothelial dysfunction, and significantly contribute to lung injury in COVID-19. ACE inhibitors (ACEi) have been shown to improve endothelial function and have been suggested to be associated with less severe COVID-19 disease [54], [70]. Interestingly, ACEi have been shown to lower PAI-1 levels and increase release of tPA via elevated bradykinin [71], [72], [73], [74], [75]. On the other hand, AT1 receptor blockers (ARBs) have been shown to have a variable effect on PAI-1 (increase [76], decrease [77], or no change [78], [79]) and do not increase levels of tPA [74]. Spironolactone, an aldosterone receptor blocker, has been shown to decrease PAI-1 levels [66], [80]. In a one week study, spironolactone (aldosterone receptor blocker) treatment in hypertensive patients significantly reduced PAI-1 levels and increased tPA levels compared to baseline [80]. However, other studies found no significant changes [81]. The differences between these studies highlight the complexity of the RAAS, with differences in volume status and the degree of RAAS activation as contributing factors [80], [81]. The combined effects of RAAS on both the pulmonary system and hemostasis make it a tantalizing target in COVID-19, but requires urgent further investigation to confirm these hypotheses and identify optimal therapeutic targets [53], [54].
5. Conclusions
Hyperinflammation and detrimental immunothrombosis may be central to the pathophysiology of COVID-19. Platelet hyper-reactivity, hypercoagulability, hypofibrinolysis, complement overactivation, and RAAS derangement in the presence of underlying inflammatory-induced endothelial dysfunction likely lead to a state of COVID-induced coagulopathy. Fortunately, modern medicine has left us with a multitude of therapeutic options for targeting all of the pathways discussed, if the components driving disease can be identified. Immunomodulation (including cytokine inhibitors and complement inhibitors), RAAS inhibitors, anticoagulants, antiplatelets and fibrinolytics may all serve potential roles in COVID-19 therapy. As such, rapid investigation is required to determine which pathways and components are deranged and most contributory to morbidity and mortality in COVID-19. Through multi-center studies and international collaboration, we aim to quickly answer these questions and enable targeted therapeutic monitoring and intervention.
References
- 1.Lippi G., Favaloro E.J. D-dimer is associated with severity of coronavirus disease 2019: a pooled analysis. Thromb. Haemost. 2020 doi: 10.1055/s-0040-1709650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Henry B.M., de Oliveira M.H.S., Benoit S., Plebani M., Lippi G. Hematologic, biochemical and immune biomarker abnormalities associated with severe illness and mortality in coronavirus disease 2019 (COVID-19): a meta-analysis. Clin. Chem. Lab. Med. (CCLM). 2020;1 doi: 10.1515/cclm-2020-0369. [DOI] [PubMed] [Google Scholar]
- 3.G. Lippi, M. Plebani, B.M. Henry, Thrombocytopenia is associated with severe coronavirus disease 2019 (COVID-19) infections: A meta-analysis, Clin. Chim. Acta. 506 (2020) 145–148. https://doi.org/10.1016/j.cca.2020.03.022. [DOI] [PMC free article] [PubMed]
- 4.Thachil J. The versatile heparin in COVID-19. J. Thromb. Haemost. 2020 doi: 10.1111/jth.14821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.W. Luo, H. Yu, J. Gou, X. Li, Y. Sun, J. Li, L. Liu, Clinical Pathology of Critical Patient with Novel Coronavirus Pneumonia (COVID-19), (2020). https://www.preprints.org/manuscript/202002.0407/v1 (accessed April 5, 2020).
- 6.Klok F.A., Kruip M.J.H.A., van der Meer N.J.M., Arbous M.S., Gommers D.A.M.P.J., Kant K.M., Kaptein F.H.J., van Paassen J., Stals M.A.M., Huisman M.V., Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb. Res. 2020 doi: 10.1016/j.thromres.2020.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhou P., Yang X.-L., Wang X.-G., Hu B., Zhang L., Zhang W., Si H.-R., Zhu Y., Li B., Huang C.-L., Chen H.-D., Chen J., Luo Y., Guo H., Jiang R.-D., Liu M.-Q., Chen Y., Shen X.-R., Wang X., Zheng X.-S., Zhao K., Chen Q.-J., Deng F., Liu L.-L., Yan B., Zhan F.-X., Wang Y.-Y., Xiao G.-F., Shi Z.-L. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jensen S., Thomsen A.R. Sensing of RNA viruses: a review of innate immune receptors involved in recognizing RNA virus invasion. J. Virol. 2012;86:2900–2910. doi: 10.1128/JVI.05738-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siu K.-L., Kok K.-H., Ng M.-H.J., Poon V.K.M., Yuen K.-Y., Zheng B.-J., Jin D.-Y. Severe acute respiratory syndrome coronavirus M protein inhibits type I interferon production by impeding the formation of TRAF3.TANK.TBK1/IKKepsilon complex. J. Biol. Chem. 2009;284:16202–16209. doi: 10.1074/jbc.M109.008227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen X., Yang X., Zheng Y., Yang Y., Xing Y., Chen Z. SARS coronavirus papain-like protease inhibits the type I interferon signaling pathway through interaction with the STING-TRAF3-TBK1 complex. Protein Cell. 2014;5:369–381. doi: 10.1007/s13238-014-0026-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li S.-W., Wang C.-Y., Jou Y.-J., Huang S.-H., Hsiao L.-H., Wan L., Lin Y.-J., Kung S.-H., Lin C.-W. SARS Coronavirus Papain-Like Protease Inhibits the TLR7 Signaling Pathway through Removing Lys63-Linked Polyubiquitination of TRAF3 and TRAF6. Int. J. Mol. Sci. 2016;17 doi: 10.3390/ijms17050678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Channappanavar R., Fehr A.R., Vijay R., Mack M., Zhao J., Meyerholz D.K., Perlman S. Dysregulated Type I Interferon and Inflammatory Monocyte-Macrophage Responses Cause Lethal Pneumonia in SARS-CoV-Infected Mice. Cell Host Microbe. 2016;19:181–193. doi: 10.1016/j.chom.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mehta P., McAuley D.F., Brown M., Sanchez E., Tattersall R.S., Manson J.J. COVID-19: consider cytokine storm syndromes and immunosuppression. The Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang X., Xu W., Hu G., Xia S., Sun Z., Liu Z., Xie Y., Zhang R., Jiang S., Lu L. SARS-CoV-2 infects T lymphocytes through its spike protein-mediated membrane fusion. Cell. Mol. Immunol. 2020:1–3. doi: 10.1038/s41423-020-0424-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tan L., Wang Q., Zhang D., Ding J., Huang Q., Tang Y.-Q., Wang Q., Miao H. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Transduct. Targeted Therapy. 2020;5:1–3. doi: 10.1038/s41392-020-0148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen J., Lau Y.F., Lamirande E.W., Paddock C.D., Bartlett J.H., Zaki S.R., Subbarao K. Cellular immune responses to severe acute respiratory syndrome coronavirus (SARS-CoV) infection in senescent BALB/c mice: CD4+ T cells are important in control of SARS-CoV infection. J. Virol. 2010;84:1289–1301. doi: 10.1128/JVI.01281-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Channappanavar R., Perlman S. Pathogenic human coronavirus infections: causes and consequences of cytokine storm and immunopathology. Semin Immunopathol. 2017;39:529–539. doi: 10.1007/s00281-017-0629-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team, The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19) — China, 2020, CCDCW. 2 (2020) 113–122. [PMC free article] [PubMed]
- 19.Italian National Institute of Health, Report on the characteristics of COVID-19 positive patients deceased in Italy (2020).
- 20.Wenham C., Smith J., Morgan R. COVID-19: the gendered impacts of the outbreak. The Lancet. 2020;395:846–848. doi: 10.1016/S0140-6736(20)30526-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Souyris M., Cenac C., Azar P., Daviaud D., Canivet A., Grunenwald S., Pienkowski C., Chaumeil J., Mejía J.E., Guéry J.-C. TLR7 escapes X chromosome inactivation in immune cells. Sci. Immunol. 2018;3 doi: 10.1126/sciimmunol.aap8855. [DOI] [PubMed] [Google Scholar]
- 22.Berghöfer B., Frommer T., Haley G., Fink L., Bein G., Hackstein H. TLR7 ligands induce higher IFN-alpha production in females. J. Immunol. 2006;177:2088–2096. doi: 10.4049/jimmunol.177.4.2088. [DOI] [PubMed] [Google Scholar]
- 23.Seillet C., Laffont S., Trémollières F., Rouquié N., Ribot C., Arnal J.-F., Douin-Echinard V., Gourdy P., Guéry J.-C. The TLR-mediated response of plasmacytoid dendritic cells is positively regulated by estradiol in vivo through cell-intrinsic estrogen receptor α signaling. Blood. 2012;119:454–464. doi: 10.1182/blood-2011-08-371831. [DOI] [PubMed] [Google Scholar]
- 24.Guo L., Rondina M.T. The Era of Thromboinflammation: Platelets Are Dynamic Sensors and Effector Cells During Infectious Diseases. Front. Immunol. 2019;10 doi: 10.3389/fimmu.2019.02204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gaertner F., Massberg S. Blood coagulation in immunothrombosis-At the frontline of intravascular immunity. Semin. Immunol. 2016;28:561–569. doi: 10.1016/j.smim.2016.10.010. [DOI] [PubMed] [Google Scholar]
- 26.Jackson S.P., Darbousset R., Schoenwaelder S.M. Thromboinflammation: challenges of therapeutically targeting coagulation and other host defense mechanisms. Blood. 2019;133:906–918. doi: 10.1182/blood-2018-11-882993. [DOI] [PubMed] [Google Scholar]
- 27.Frantzeskaki F., Armaganidis A., Orfanos S.E. Immunothrombosis in Acute Respiratory Distress Syndrome: Cross Talks between Inflammation and Coagulation. Res. 2017;93:212–225. doi: 10.1159/000453002. [DOI] [PubMed] [Google Scholar]
- 28.Lippi G., Adcock D., Favaloro E.J. Understanding the “philosophy” of laboratory hemostasis. Diagnosis (Berl). 2019;6:223–226. doi: 10.1515/dx-2018-0099. [DOI] [PubMed] [Google Scholar]
- 29.Kwaan H. Coronavirus Disease 2019: The Role of the Fibrinolytic System from Transmission to Organ Injury and Sequalae. Semin. Thromb. Hemost. 2020 doi: 10.1055/s-0040-1709996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Keragala C.B., Draxler D.F., McQuilten Z.K., Medcalf R.L. Haemostasis and innate immunity - a complementary relationship: A review of the intricate relationship between coagulation and complement pathways. Br. J. Haematol. 2018;180:782–798. doi: 10.1111/bjh.15062. [DOI] [PubMed] [Google Scholar]
- 31.Schönrich G., Raftery M.J. Neutrophil Extracellular Traps Go Viral. Front. Immunol. 2016;7:366. doi: 10.3389/fimmu.2016.00366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Narasaraju T., Yang E., Samy R.P., Ng H.H., Poh W.P., Liew A.-A., Phoon M.C., van Rooijen N., Chow V.T. Excessive neutrophils and neutrophil extracellular traps contribute to acute lung injury of influenza pneumonitis. Am. J. Pathol. 2011;179:199–210. doi: 10.1016/j.ajpath.2011.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morrell C.N., Aggrey A.A., Chapman L.M., Modjeski K.L. Emerging roles for platelets as immune and inflammatory cells. Blood. 2014;123:2759–2767. doi: 10.1182/blood-2013-11-462432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zucoloto A.Z., Jenne C.N. Platelet-Neutrophil Interplay: Insights Into Neutrophil Extracellular Trap (NET)-Driven Coagulation in Infection. Front Cardiovasc Med. 2019;6 doi: 10.3389/fcvm.2019.00085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Walsh P.N. Platelet coagulation-protein interactions. Semin. Thromb. Hemost. 2004;30:461–471. doi: 10.1055/s-2004-833481. [DOI] [PubMed] [Google Scholar]
- 36.Sarma J.V., Ward P.A. The complement system. Cell Tissue Res. 2011;343:227–235. doi: 10.1007/s00441-010-1034-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gralinski L.E., Sheahan T.P., Morrison T.E., Menachery V.D., Jensen K., Leist S.R., Whitmore A., Heise M.T., Baric R.S. Complement Activation Contributes to Severe Acute Respiratory Syndrome Coronavirus Pathogenesis. MBio. 2018;9 doi: 10.1128/mBio.01753-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ye J., Zhang B., Xu J., Chang Q., McNutt M.A., Korteweg C., Gong E., Gu J. Molecular pathology in the lungs of severe acute respiratory syndrome patients. Am. J. Pathol. 2007;170:538–545. doi: 10.2353/ajpath.2007.060469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.L. Nicin, W.T. Abplanalp, H. Mellentin, B. Kattih, L. Tombor, D. John, J.D. Schmitto, J. Heineke, F. Emrich, M. Arsalan, T. Holubec, T. Walther, A.M. Zeiher, S. Dimmeler, Cell type-specific expression of the putative SARS-CoV-2 receptor ACE2 in human hearts, Eur Heart J. (n.d.). https://doi.org/10.1093/eurheartj/ehaa311. [DOI] [PMC free article] [PubMed]
- 40.Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A.S., Mehra M.R., Schuepbach R.A., Ruschitzka F., Moch H. Endothelial cell infection and endotheliitis in COVID-19. The Lancet. 2020 doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ozolina A., Sarkele M., Sabelnikovs O., Skesters A., Jaunalksne I., Serova J., Ievins T., Bjertnaes L.J., Vanags I. Activation of Coagulation and Fibrinolysis in Acute Respiratory Distress Syndrome: A Prospective Pilot Study. Front Med (Lausanne). 2016;3 doi: 10.3389/fmed.2016.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Glas G.J., Van Der Sluijs K.F., Schultz M.J., Hofstra J.-J.H., Van Der Poll T., Levi M. Bronchoalveolar hemostasis in lung injury and acute respiratory distress syndrome. J. Thromb. Haemost. 2013;11:17–25. doi: 10.1111/jth.12047. [DOI] [PubMed] [Google Scholar]
- 43.Beristain-Covarrubias N., Perez-Toledo M., Thomas M.R., Henderson I.R., Watson S.P., Cunningham A.F. Understanding Infection-Induced Thrombosis: Lessons Learned From Animal Models. Front. Immunol. 2019;10:2569. doi: 10.3389/fimmu.2019.02569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schulman S. COVID-19, prothrombotic factors and venous thromboembolism. Semin. Thromb. Hemost. 2020 doi: 10.1055/s-0040-1710337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Han M., Yan W., Huang Y., Yao H., Wang Z., Xi D., Li W., Zhou Y., Hou J., Luo X., Ning Q. The nucleocapsid protein of SARS-CoV induces transcription of hfgl2 prothrombinase gene dependent on C/EBP alpha. J. Biochem. 2008;144:51–62. doi: 10.1093/jb/mvn042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Meyer M.A.S., Ostrowski S.R., Overgaard A., Ganio M.S., Secher N.H., Crandall C.G., Johansson P.I. Hypercoagulability in response to elevated body temperature and central hypovolemia. J. Surg. Res. 2013;185:e93–e100. doi: 10.1016/j.jss.2013.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tang N., Bai H., Chen X., Gong J., Li D., Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J. Thromb. Haemost. 2020 doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Li J., Li Y., Yang B., Wang H., Li L. Low-molecular-weight heparin treatment for acute lung injury/acute respiratory distress syndrome: a meta-analysis of randomized controlled trials. Int. J. Clin. Exp. Med. 2020;11:414–422. [Google Scholar]
- 49.J. Wang, N. Hajizadeh, E.E. Moore, R.C. McIntyre, P.K. Moore, L.A. Veress, M.B. Yaffe, H.B. Moore, C.D. Barrett, Tissue Plasminogen Activator (tPA) Treatment for COVID-19 Associated Acute Respiratory Distress Syndrome (ARDS): A Case Series, Journal of Thrombosis and Haemostasis. n/a (n.d.). https://doi.org/10.1111/jth.14828. [DOI] [PMC free article] [PubMed]
- 50.Zhang Y., Xiao M., Zhang S., Xia P., Cao W., Jiang W., Chen H., Ding X., Zhao H., Zhang H., Wang C., Zhao J., Sun X., Tian R., Wu W., Wu D., Ma J., Chen Y., Zhang D., Xie J., Yan X., Zhou X., Liu Z., Wang J., Du B., Qin Y., Gao P., Qin X., Xu Y., Zhang W., Li T., Zhang F., Zhao Y., Li Y., Zhang S. Coagulopathy and Antiphospholipid Antibodies in Patients with Covid-19. N. Engl. J. Med. 2020 doi: 10.1056/NEJMc2007575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Vrigkou E., Tsangaris I., Bonovas S., Tsantes A., Kopterides P. The evolving role of the renin–angiotensin system in ARDS. Crit. Care. 2017;21 doi: 10.1186/s13054-017-1917-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang H., Baker A. Recombinant human ACE2: acing out angiotensin II in ARDS therapy. Crit. Care. 2017;21 doi: 10.1186/s13054-017-1882-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Henry B.M., Vikse J. Clinical Characteristics of Covid-19 in China. N. Engl. J. Med. 2020;382 doi: 10.1056/NEJMc2005203. [DOI] [PubMed] [Google Scholar]
- 54.F. Sanchis-Gomar, C.J. Lavie, C. Perez-Quilis, B.M. Henry, G. Lippi, Angiotensin-Converting Enzyme 2 and Anti-Hypertensives (Angiotensin Receptor Blockers and Angiotensin Converting Enzyme Inhibitors) in Coronavirus Disease 2019 (COVID-19), Mayo Clinic Proceedings. (2020) 19. [DOI] [PMC free article] [PubMed]
- 55.Guan W.-J., Ni Z.-Y., Hu Y., Liang W.-H., Ou C.-Q., He J.-X., Liu L., Shan H., Lei C.-L., Hui D.S.C., Du B., Li L.-J., Zeng G., Yuen K.-Y., Chen R.-C., Tang C.-L., Wang T., Chen P.-Y., Xiang J., Li S.-Y., Wang J.-L., Liang Z.-J., Peng Y.-X., Wei L., Liu Y., Hu Y.-H., Peng P., Wang J.-M., Liu J.-Y., Chen Z., Li G., Zheng Z.-J., Qiu S.-Q., Luo J., Ye C.-J., Zhu S.-Y., Zhong N.-S. China Medical Treatment Expert Group for Covid-19, Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tikellis C., Thomas M.C. Angiotensin-Converting Enzyme 2 (ACE2) Is a Key Modulator of the Renin Angiotensin System in Health and Disease. Int J Pept. 2012;2012 doi: 10.1155/2012/256294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kuba K., Imai Y., Rao S., Gao H., Guo F., Guan B., Huan Y., Yang P., Zhang Y., Deng W., Bao L., Zhang B., Liu G., Wang Z., Chappell M., Liu Y., Zheng D., Leibbrandt A., Wada T., Slutsky A.S., Liu D., Qin C., Jiang C., Penninger J.M. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat. Med. 2005;11:875–879. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Liu Y., Yang Y., Zhang C., Huang F., Wang F., Yuan J., Wang Z., Li J., Li J., Feng C., Zhang Z., Wang L., Peng L., Chen L., Qin Y., Zhao D., Tan S., Yin L., Xu J., Zhou C., Jiang C., Liu L. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci. China Life Sci. 2020;63:364–374. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Vaughan D.E., Lazos S.A., Tong K. Angiotensin II regulates the expression of plasminogen activator inhibitor-1 in cultured endothelial cells. A potential link between the renin-angiotensin system and thrombosis. J. Clin. Invest. 1995;95:995–1001. doi: 10.1172/JCI117809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nakamura S., Nakamura I., Ma L., Vaughan D.E., Fogo A.B. Plasminogen activator inhibitor-1 expression is regulated by the angiotensin type 1 receptor in vivo1. Kidney Int. 2000;58:251–259. doi: 10.1046/j.1523-1755.2000.00160.x. [DOI] [PubMed] [Google Scholar]
- 61.Yao X.H., Li T.Y., He Z.C., Ping Y.F., Liu H.W., Yu S.C., Mou H.M., Wang L.H., Zhang H.R., Fu W.J., Luo T., Liu F., Chen C., Xiao H.L., Guo H.T., Lin S., Xiang D.F., Shi Y., Li Q.R., Huang X., Cui Y., Li X.Z., Tang W., Pan P.F., Huang X.Q., Ding Y.Q., Bian X.W. A pathological report of three COVID-19 cases by minimally invasive autopsies. Zhonghua Bing Li Xue Za Zhi. 2020;49:E009. doi: 10.3760/cma.j.cn112151-20200312-00193. [DOI] [PubMed] [Google Scholar]
- 62.Thomas Skurk, Yu-Mi Lee, Hans Hauner. Angiotensin II and Its Metabolites Stimulate PAI-1 Protein Release From Human Adipocytes in Primary Culture. Hypertension. 2001;37:1336–1340. doi: 10.1161/01.HYP.37.5.1336. [DOI] [PubMed] [Google Scholar]
- 63.Brown N.J., Nadeau J.H., Vaughan D.E. Selective stimulation of tissue-type plasminogen activator (t-PA) in vivo by infusion of bradykinin. Thromb. Haemost. 1997;77:522–525. [PubMed] [Google Scholar]
- 64.Stoll D., Yokota R., Sanches Aragão D., Casarini D.E. Both aldosterone and spironolactone can modulate the intracellular ACE/ANG II/AT1 and ACE2/ANG (1–7)/MAS receptor axes in human mesangial cells. Physiol Rep. 7. 2019 doi: 10.14814/phy2.14105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.G. Lippi, A.M. South, B.M. Henry, ANNALS EXPRESS: Electrolyte Imbalances in Patients with Severe Coronavirus Disease 2019 (COVID-19), Ann Clin Biochem. (2020) 0004563220922255. https://doi.org/10.1177/0004563220922255. [DOI] [PMC free article] [PubMed]
- 66.Sawathiparnich P., Kumar S., Vaughan D.E., Brown N.J. Spironolactone abolishes the relationship between aldosterone and plasminogen activator inhibitor-1 in humans. J. Clin. Endocrinol. Metab. 2002;87:448–452. doi: 10.1210/jcem.87.2.7980. [DOI] [PubMed] [Google Scholar]
- 67.Ma J., Weisberg A., Griffin J.P., Vaughan D.E., Fogo A.B., Brown N.J. Plasminogen activator inhibitor-1 deficiency protects against aldosterone-induced glomerular injury. Kidney Int. 2006;69:1064–1072. doi: 10.1038/sj.ki.5000201. [DOI] [PubMed] [Google Scholar]
- 68.Brown N.J., Nakamura S., Ma L., Nakamura I., Donnert E., Freeman M., Vaughan D.E., Fogo A.B. Aldosterone modulates plasminogen activator inhibitor-1 and glomerulosclerosis in vivo. Kidney Int. 2000;58:1219–1227. doi: 10.1046/j.1523-1755.2000.00277.x. [DOI] [PubMed] [Google Scholar]
- 69.Yuan J., Jia R., Bao Y. Aldosterone up-regulates production of plasminogen activator inhibitor-1 by renal mesangial cells. J. Biochem. Mol. Biol. 2007;40:180–188. doi: 10.5483/bmbrep.2007.40.2.180. [DOI] [PubMed] [Google Scholar]
- 70.Sanjay Rajagopalan. Harrison David G., Reversing Endothelial Dysfunction With ACE Inhibitors. Circulation. 1996;94:240–243. doi: 10.1161/01.CIR.94.3.240. [DOI] [PubMed] [Google Scholar]
- 71.Brown N.J., Kim K.S., Chen Y.Q., Blevins L.S., Nadeau J.H., Meranze S.G., Vaughan D.E. Synergistic effect of adrenal steroids and angiotensin II on plasminogen activator inhibitor-1 production. J. Clin. Endocrinol. Metab. 2000;85:336–344. doi: 10.1210/jcem.85.1.6305. [DOI] [PubMed] [Google Scholar]
- 72.Brown Nancy J., Agirbasli Mehmet A., Williams Gordon H., Litchfield W. Reid, Vaughan Douglas E. Effect of Activation and Inhibition of the Renin-Angiotensin System on Plasma PAI-1. Hypertension. 1998;32(6):965–971. doi: 10.1161/01.HYP.32.6.965. [DOI] [PubMed] [Google Scholar]
- 73.Vaughan D.E., Rouleau J.L., Ridker P.M., Arnold J.M., Menapace F.J., Pfeffer M.A. Effects of ramipril on plasma fibrinolytic balance in patients with acute anterior myocardial infarction. HEART Study Investigators, Circulation. 1997;96:442–447. doi: 10.1161/01.cir.96.2.442. [DOI] [PubMed] [Google Scholar]
- 74.Matsumoto T., Minai K., Horie H., Ohira N., Takashima H., Tarutani Y., Yasuda Y., Ozawa T., Matsuo S., Kinoshita M., Horie M. Angiotensin-converting enzyme inhibition but not angiotensin II type 1 receptor antagonism augments coronary release of tissue plasminogen activator in hypertensive patients. J. Am. Coll. Cardiol. 2003;41:1373–1379. doi: 10.1016/s0735-1097(03)00162-1. [DOI] [PubMed] [Google Scholar]
- 75.Minai K., Matsumoto T., Horie H., Ohira N., Takashima H., Yokohama H., Kinoshita M. Bradykinin stimulates the release of tissue plasminogen activator in human coronary circulation: effects of angiotensin-converting enzyme inhibitors. J. Am. Coll. Cardiol. 2001;37:1565–1570. doi: 10.1016/s0735-1097(01)01202-5. [DOI] [PubMed] [Google Scholar]
- 76.Fogari R., Zoppi A., Mugellini A., Maffioli P., Lazzari P., Derosa G. Role of angiotensin II in plasma PAI-1 changes induced by imidapril or candesartan in hypertensive patients with metabolic syndrome. Hypertens. Res. 2011;34:1321–1326. doi: 10.1038/hr.2011.137. [DOI] [PubMed] [Google Scholar]
- 77.Liu L., Zhao S.-P., Zhou H.-N., Li Q.-Z., Li J.-X. Effect of fluvastatin and valsartan, alone and in combination, on postprandial vascular inflammation and fibrinolytic activity in patients with essential hypertension. J. Cardiovasc. Pharmacol. 2007;50:50–55. doi: 10.1097/FJC.0b013e31805751d3. [DOI] [PubMed] [Google Scholar]
- 78.Lin T.-H., Voon W.-C., Yen H.-W., Huang C.-H., Su H.-M., Lai W.-T., Sheu S.-H. Lercanidipine and losartan effects on blood pressure and fibrinolytic parameters. Kaohsiung J. Med. Sci. 2006;22:177–183. doi: 10.1016/S1607-551X(09)70304-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Skurk T., Lee Y.-M., Nicuta-Rölfs T.-O., Haastert B., Wirth A., Hauner H. Effect of the angiotensin II receptor blocker candesartan on fibrinolysis in patients with mild hypertension. Diabetes Obes. Metab. 2004;6:56–62. doi: 10.1111/j.1463-1326.2004.00316.x. [DOI] [PubMed] [Google Scholar]
- 80.Yalcin A.I., Dincer M., Aslan V., Gulbas Z. Effect of spironolactone on impaired fibrinolysis of hypertensive patients. Kidney Blood Press. Res. 2002;25:260–264. doi: 10.1159/000066348. [DOI] [PubMed] [Google Scholar]
- 81.Sawathiparnich P., Murphey L.J., Kumar S., Vaughan D.E., Brown N.J. Effect of Combined AT1 Receptor and Aldosterone Receptor Antagonism on Plasminogen Activator Inhibitor-1. J. Clin. Endocrinol. Metab. 2003;88:3867–3873. doi: 10.1210/jc.2003-030374. [DOI] [PubMed] [Google Scholar]