Highlights
-
•
Diabetes mellitus is a frequent comorbidity in patients with COVID-19 infection
-
•
Diabetic patients with COVID-19 infection are at higher risk to be admitted to intensive care unit
-
•
Diabetic patients with COVID-19 infection have an higher mortality risk
Keywords: Diabetes, COVID-19, ICUM, Ortality
Abstract
Background
The prognostic significance of diabetes mellitus (DM) in patients with coronavirus 2019 disease (COVID-19) remains unknown.
Objectives
To assess the risk of ICU admission and morality risk in diabetic COVID-19 patients.
Study desing
A database search was conducted to identify studies comparing diabetic COVID-19 patients hospitalized in intensive care unit (ICU) and those reporting the overall mortality of these patients published up to March 25, 2020 within MEDLINE, Scopus and Web of Science.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed in abstracting data and assessing validity. Quality assessment was performed using the Newcastle-Ottawa quality assessment scale. The main outcome was the risk of ICU admission in diabetic patients with COVID-19 infection while the second was the mortality risk in overall diabetic COVID-19 patients. Data were pooled using the Mantel-Haenszel random effects models with odds ratio (OR) as the effect measure with the related 95 % confidence interval (CI). Statistical heterogeneity between groups was measured using the Higgins I2 statistic.
Results
Among 1382 patients (mean age 51.5 years, 798 males), DM resulted to be the second more frequent comorbidities. Diabetic patients resulted to have a significant increased risk of ICU admission (OR: 2.79, 95 % CI 1.85–4.22, p < 0.0001, I2 = 46 %). In 471 patients (mean age 56.6 years, 294 males) analysed for the secondary outcome diabetic subjects resulted to be at higher mortality risk (OR 3.21, 95 % CI 1.82–5.64, p < 0.0001, I2 = 16 %).
Conclusions
Diabetic patients with COVID-19 patients are at higher risk of ICU admission and show an higher mortality risk.
1. Introduction
The coronavirus 2019 disease (COVID-19) currently represents a serious public health issue worldwide. As well known, diabetic patients are at higher risk of infection especially during period of poor glycaemic controls [1]. Recent investigations have reported that in COVID-19 infection, diabetes mellitus (DM) is one of the most common comorbidities [2,3]. Moreover, some studies have suggested that these subjects seem to have a higher mortality risk during the infection [[4], [5], [6]]. Unfortunately, data regarding the prognostic impact of diabetes in COVID-19 patients are scant. Aim of the present manuscript is to perform a systematic review and meta-analysis in the effort to assess the risk of ICU admission and the mortality risk in diabetic patients with COVID-19 infection.
1.1. Study desing
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) reporting guideline (Supplementary file 1) [7].
1.2. Eligibility criteria
Data were obtained searching in MEDLINE, Scopus and Web of Science all investigations in English language published any time to March 23, 2020, reporting data of COVID-19 patients admitted to ICU or not and comparing the clinical feature between survivors and not survivors.
The risk for diabetic subjects to be admitted in ICU was chosen as the primary outcome. Conversely, the mortality risk of diabetic COVID-19 patients was selected as the secondary outcome.
1.3. Search strategy
The selection of studies to be included in our analysis was independently conducted by 2 authors (LR and GR) in a blinded fashion. Any discrepancies in study selection was resolved consulting a third author (MZ).The following MeSH terms were used for the search: “COVID-19″ AND “Mortality” OR “ICU” OR “Diabetes mellitus”. Moreover, we searched the bibliographies of target studies for additional references. Case reports review articles, abstracts, editorials/letters, and case series with less than 10 participants were excluded. Data extraction was independently conducted by 2 of us (GR and MZ). Studies were excluded from the meta-analysis if they did not have present a comparison between patients hospitalized in ICU or not, did not report a comparison between survivors or not survivors, did not present data regarding diabetic patients or if they not were written in English language. For each study we extracted the number of patients, mean age, male gender, prevalence of DM, arterial hypertension (HT) and cardiovascular disease (CVD), the number of diabetic subjects admitted o not to the ICU as well as the number of diabetic survivors or not.
1.4. Risk of bias assessment
The quality of included studies was graded using the Newcastle-Ottawa quality assessment scale (NOS) [8]. In this regard, investigations were classified as having low (< 5 stars), moderate (5–7 stars) and high quality (> 7 stars).
1.5. Data synthesis and analysis
Continues variables were expressed as mean while categorical variables, were presented as proportions. Data were pooled using the Mantel-Haenszel random effects models with odds ratio (OR) as the effect measure with the related 95 % confidence interval (CI). Statistical heterogeneity between groups was measured using the Higgins I2 statistic. Specifically, a I2 = 0 indicated no heterogeneity while we considered low, moderate, and high degrees of heterogeneity based on the values of I2 as <25 %, 25–75 % and above 75 % respectively. To evaluate the publication bias concerning for both outcomes, Egger’s test further performed to assess the asymmetry of the funnel plot. Analyses were carried out using Review Manager 5.2 (The Cochrane Collaboration, Oxford, England).
2. Results
2.1. Study selection and characteristics
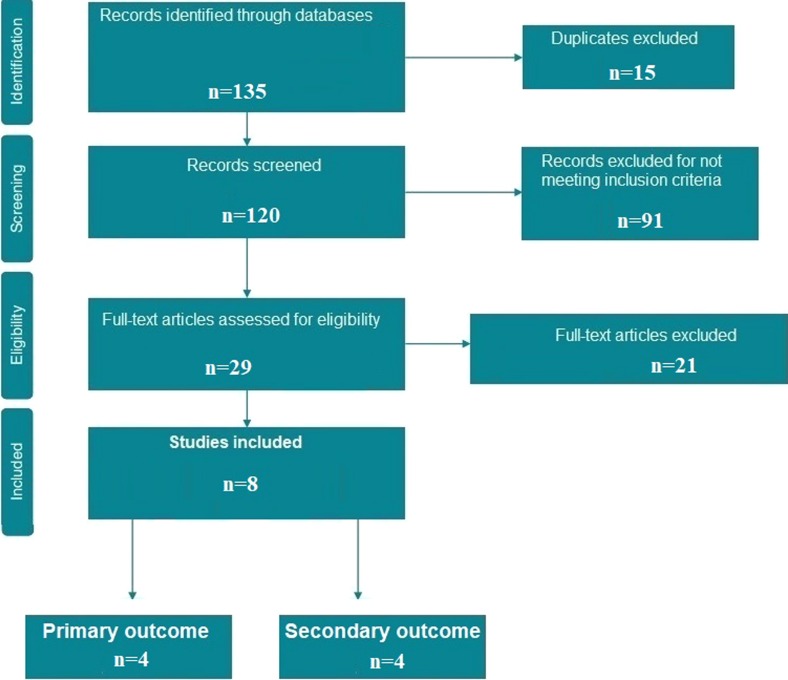
The initial search identified 135 potentially relevant citations (Fig. 1 ). After screening titles and abstracts, 29 articles remained for full-text assessment while 21 were subsequently excluded. Eight studies (summarized in Table 1 and Table 2 ) met the meta-analysis inclusion criteria. Specifically, 4 for the primary [[9], [10], [11], [12]] and four for the secondary study outcome [[13], [14], [15], [16]], respectively, were included. Of these, seven to be of high quality while one of moderate quality according to the NOS.
Fig. 1.
Flow diagram of selected studies for the meta-analysis according to the Preferred reporting items for systematic reviews and meta-analyses (PRISMA).
Table 1.
General characteristics of studies considered for the first study outcome (i.e. risk of ICU admission for diabetic patients). DM: Diabetes mellitus; CVD: Cardiovascular disease; HT: Arterial Hypertension: NOS: Newcastle-Ottawa quality assessment scale. *Patients defined as “Severe”.
| Authors | N° of patients | Mean Age (years) |
Males N, (%) |
DM | CVD N (%) |
HT N (%) |
NOS |
|---|---|---|---|---|---|---|---|
| Cao et al. [9] | 102 | 54 | 53 (52) | 11 (11) | 5 (5) | 28 (28) | High |
| Huang et al. [10] | 43 | 49 | 30 (73) | 8 (20) | 6 (15) | 8 (20) | High |
| Wang et al. [11] | 138 | 56 | 75 (54) | 14 (10) | 20 (14.5) | 43 (31) | High |
| Guan et al. [12] * | 1099 | 47 | 640 (58) | 81 (7.4) | 27 (2.5) | 165 (15) | High |
Table 2.
General characteristics of studies considered for the second study outcome (i.e. Risk of mortality in diabetic patients). DM: Diabetes mellitus; CVD: Cardiovascular disease; HT: Arterial Hypertension: NOS: Newcastle-Ottawa quality assessment scale.
| Authors | N° of patients | Mean Age (years) |
Males N, (%) |
DM | CVD N (%) |
HT N (%) |
NOS |
|---|---|---|---|---|---|---|---|
| Wu et al. [13] | 201 | 51 | 128 (64) | 22 (11) | 8 (4.0) | 39 (19.4) | High |
| Yang et al. [14] | 52 | 59.7 | 35 (67) | 9 (17) | 5 (10) | NR | Moderate |
| Yuan et al. [15] | 27 | 60 | 12 (45) | 6 (22) | 3 (11) | 5 (19) | High |
| Zhou et al. [16] | 191 | 56 | 119 (62) | 36 (19) | 15 (8) | 58 (30) | High |
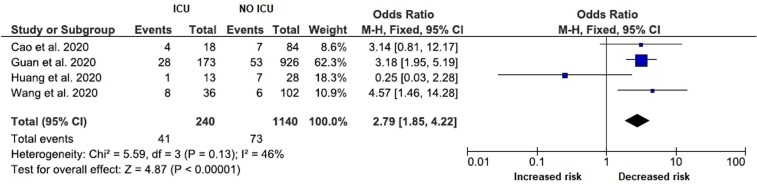
2.2. Risk of ICU admission
Regarding the risk of ICU admission for diabetic patients with COVID-19 infection, the general characteristics of the study reviewed are showed in Table 1. Among 1382 patients (mean age 51.5 years, 798 males), DM resulted to be the second more frequent comorbidities. Diabetic patients resulted to have a significant increased risk of ICU admission (OR: 2.79, 95 % CI 1.85–4.22, p < 0.0001, I2 = 46 %), as showed in Fig. 2 .
Fig. 2.
Forest plot of studies investigating ICU admission in relation to diabetes mellitus.
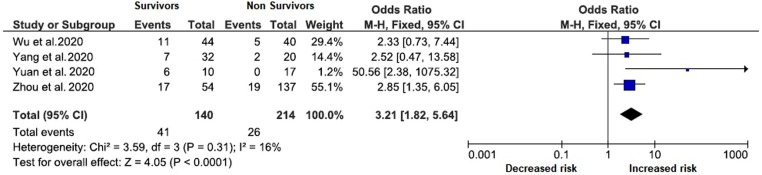
2.3. Mortality risk
Table 2 represent the general characteristics of patients considered for the secondary outcome of the study. Specifically, 4 investigations fulfilled in the inclusion criteria presenting the survival for 471 patients (mean age 56.6 years, 294 males). Again, DM represented the second more frequent comorbidities after arterial hypertension (HT). Diabetic patients resulted to be at higher mortality risk (OR 3.21, 95 % CI 1.82–5.64, p < 0.0001, I2 = 16 %) as demonstrated by the forest plot in Fig. 3 .
Fig. 3.
Forest plot of studies investigating survival in relation to diabetes mellitus.
2.4. Publication Bias
The Egger’s regression test for the primary (p = 0.303) and for the secondary (p = 0.451) outcome, respectively, confirmed that there were no statistically evidence of publication bias.
3. Discussion
Our brief meta-analysis demonstrated that diabetic patients with COVID-19 infection have an higher risk to be admitted to ICU during the infection. Moreover, DM increased the risk of mortality during the infection. To the best of our knowledge, this is the first meta-analysis considering the DM in COVID-19 infection. Surely, DM s generally associated with a poor prognosis in infective disease [[17], [18], [19], [20]], but a direct demonstration of this aspect in COVID-19 patients, until now, has been only reported in isolated reports [[13], [14], [15], [16]] and never analysed comprehensively. However, whether DM increased the risk of infection due to COVID-SARS-19 remains an unresolved question to date and will require further clarification by specific studies. However, current data seems to indicate that diabetic patients, as would be expected, have an higher risk of complications, as demonstrated by the ore frequent admission to ICU [[9], [10], [11], [12]]. This aspect results confirmed by our preliminary results indicating an increased risk to be admitted to ICU and the poorer outcome of these subgroup of patients. However, published data did not allow us to examine the type of DM, the length of the disease, presence of related complications, type of treatment and glycaemic controls during the infection or in the previous month. However the lack of data in this phase of the pandemia is understandable since in many regions physicians are doing a “frontline” medicine, where the time to collect records is very limited. Recently. some investigations have focused their attention to the risk of infection in diabetic subjects [20,21]. Despite the prevention of the infection remains the primary concern, also the comprehension of the course of the disease has a pivotal role, especially in different subset of patients, as the diabetics. Indeed, if the most critical issues related to the deterioration of the disease will be identify, a potential vulnerability score could be created in order to understand who of these patients will benefit from a more aggressive treatment from the beginning, to limit the complications rate. In this regard, DM resulted the most common comorbidities in most of cohorts presenting data of COVID-19 patients, generally after HT [22,23]. Whether this aspect could be related with baseline characteristics of the population or represents a real “risk factor” will require further investigations in different areas of the world. In the meanwhile, due the absence of a specific viral treatment, diabetic patients should be considered to be at higher risk of poor prognosis and/or need for intensive support. These aspects could be helpful to orient the current clinical approach to COVID-19 patients.
3.1. Limitations
Our study has several limitations related to the observational nature of the studied reviewed with all inherited biases. Secondly, very few investigations on the COVID-19 infection have stratified the cohort into survivors and non survivors as well as in ICU and no-ICU patients, limiting the number of the studies included into the meta-analysis and the related number of patients. Moreover, the inability to compare the outcome in diabetic patients on the basis of different treatment strategy adopted represent an obvious limitation.
4. Conclusions
Our analysis suggests that diabetic patients with COVID-19 infection have an higher risk to be admitted to the ICU and show an higher mortality risk during the disease.
Author contributions
Conception: LR, MZ. Literature search: LR, GR. Selection of studies: LR, GR, MZ,. Full texts search: MZ, GR. Data extraction: MZ, GR. Data synthesis and analysis: LR, MZ. Data interpretation: MZ, GR. Manuscript drafting: LR, MZ,. Manuscript editing and revision: GR, GZ. Manuscript final version approval: LR, GZ. Guarantor of the review: LR
Ethical approval
Not required.
Conflicts of interest
None of the authors have conflicts of interest to declare
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgments
None.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.jcv.2020.104354.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Critchley J.A., Carey I.M., Harris T., DeWilde S., Hosking F.J., Cook D.G. Glycemic control and risk of infections among people with type 1 or type 2 diabetes in a large primary care cohort study. Diabetes Care. 2018;41:2127–2135. doi: 10.2337/dc18-0287. [DOI] [PubMed] [Google Scholar]
- 2.Fang L., Karakiulakis G., Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir. Med. 2020 doi: 10.1016/S2213-2600(20)30116-8. S2213-2600(20)30116-8. doi: 10.1016/S2213-2600(20)30116-8. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta R., Ghosh A., Singh A.K., Misra A. Clinical considerations for patients with diabetes in times of COVID-19 epidemic. Diabetes Metab. Syndr. 2020;14:211–212. doi: 10.1016/j.dsx.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang J.J., Dong X., Cao Y.Y., Yuan Y.D., Yang Y.B., Yan Y.Q., Akdis C.A., Gao Y.D. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy. 2020 doi: 10.1111/all.14238. doi: 10.1111/all.14238. [ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05991-x. doi: 10.1007/s00134-020-05991-x. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the chinese center for disease control and prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. doi: 10.1001/jama.2020.2648 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.Moher D., Liberati A., Tetzlaff J., Altman DG PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J. Clin. Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 8.Wells G.A., Shea B., O’Connell D., Peterson J., Welch V., Losos M., Tugwell P. 2012. The Newcastle-ottawa Scale (NOS) for Assessing the Quality If Nonrandomized Studies in Meta-analyses.http://wwwohrica/programs/clinical_epidemiology/oxfordasp Available from: [Google Scholar]
- 9.Cao J., Hu X., Cheng W., Yu L., Tu W.J., Liu Q. Clinical features and short-term outcomes of 18 patients with corona virus disease 2019 in intensive care unit. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05987-7. doi: 10.1007/s00134-020-05987-7. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G., Xu J., Gu X., Cheng Z., Yu T., Xia J., Wei Y., Wu W., Xie X., Yin W., Li H., Liu M., Xiao Y., Gao H., Guo L., Xie J., Wang G., Jiang R., Gao Z., Jin Q., Wang J., Cao B. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B., Xiang H., Cheng Z., Xiong Y., Zhao Y., Li Y., Wang X., Peng Z. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. doi: 10.1001/jama.2020.1585. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., Liu L., Shan H., Lei C.L., Hui DSC Du B., Li L.J., Zeng G., Yuen K.Y., Chen R.C., Tang C.L., Wang T., Chen P.Y., Xiang J., Li S.Y., Wang J.L., Liang Z.J., Peng Y.X., Wei L., Liu Y., Hu Y.H., Peng P., Wang J.M., Liu J.Y., Chen Z., Li G., Zheng Z.J., Qiu S.Q., Luo J., Ye C.J., Zhu S.Y., Zhong N.S., China Medical Treatment Expert Group for Covid-19 Characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu C., Chen X., Cai Y., Xia J., Zhou X., Xu S., Huang H., Zhang L., Zhou X., Du C., Zhang Y., Song J., Wang S., Chao Y., Yang Z., Xu J., Zhou X., Chen D., Xiong W., Xu L., Zhou F., Jiang J., Bai C., Zheng J., Song Y. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern. Med. 2020 doi: 10.1001/jamainternmed.2020.0994. doi: 10.1001/jamainternmed.2020.0994. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H., Wu Y., Zhang L., Yu Z., Fang M., Yu T., Wang Y., Pan S., Zou X., Yuan S., Shang Y. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir. Med. 2020 doi: 10.1016/S2213-2600(20)30079-5. S2213-2600(20)30079-5 doi: 10.1016/S2213-2600(20)30079-5. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yuan M., Yin W., Tao Z., Tan W., Hu Y. Association of radiologic findings with mortality of patients infected with 2019 novel coronavirus in Wuhan, China. PLoS One. 2020;15 doi: 10.1371/journal.pone.0230548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L., Wei Y., Li H., Wu X., Xu J., Tu S., Zhang Y., Chen H., Cao B. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30566-3. S0140-6736(20)30566-3 doi:10.1016/S0140-6736(20)30566-3 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pearson-Stuttard J., Blundell S., Harris T., Cook D.G., Critchley J. Diabetes and infection: assessing the association with glycaemic control in population-based studies. Lancet Diabetes Endocrinol. 2016;4:148–158. doi: 10.1016/S2213-8587(15)00379-4. [DOI] [PubMed] [Google Scholar]
- 18.Benfield T., Jensen J.S., Nordestgaard B.G. Influence of diabetes and hyperglycaemia on infectious disease hospitalisation and outcome. Diabetologia. 2007;50:549–554. doi: 10.1007/s00125-006-0570-3. [DOI] [PubMed] [Google Scholar]
- 19.Falcone M., Tiseo G., Russo A. Hospitalization for pneumonia is associated with decreased 1-Year survival in patients with type 2 diabetes: results from a prospective cohort study. Bull. Sch. Med. Md. 2016;95:e2531. doi: 10.1097/MD.0000000000002531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ji M., Chen M., Hong X., Chen T., Zhang N. The effect of diabetes on the risk and mortality of acute lung injury/acute respiratory distress syndrome: a meta-analysis. Bull. Sch. Med. Md. 2019;98 doi: 10.1097/MD.0000000000015095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li B., Yang J., Zhao F., Zhi L., Wang X., Liu L., Bi Z., Zhao Y. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin. Res. Cardiol. 2020 doi: 10.1007/s00392-020-01626-9. doi: 10.1007/s00392-020-01626-9. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q., Ji R., Wang H., Wang Y., Zhou Y. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int. J. Infect. Dis. 2020 doi: 10.1016/j.ijid.2020.03.017. S1201-9712(20)30136-3 doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li B., Yang J., Zhao F., Zhi L., Wang X., Liu L., Bi Z., Zhao Y. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin. Res. Cardiol. 2020 doi: 10.1007/s00392-020-01626-9. doi: 10.1007/s00392-020-01626-9. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.