Abstract
The emergence of mental health (MH) problems during a pandemic is extremely common, though difficult to address due to the complexities of pandemics and the scarcity of evidence about the epidemiology of pandemic-related MH problems and the potential interventions to tackle them. Little attention has been devoted so far to this topic from policymakers, stakeholders and researchers, resulting in a lack of replicable, scalable and applicable frameworks to help plan, develop and deliver MH care during pandemics. As a response, we have attempted to develop a conceptual framework (CF) that could guide the development, implementation, and evaluation of MH interventions during the ongoing COVID-19 pandemic. This CF was developed by early career psychiatrists from 16 countries that cover all the WHO regions. Their opinions were elicited via a semi-structured questionnaire. They were asked to provide their views about the current MH situation in their countries and to elaborate on existing 'myths' and misinformation. They were also asked to name the resources available and to propose solutions and approaches to provide accessible and affordable care. The CF was prepared based on the extant literature and the views discussed in this group; it illustrates the epidemiology of MH problems, preparedness plans, stage-specific plans or innovative solutions, opportunities to integrate those plans and possible outcomes at policy level. This CF can serve as a technical guide for future research regarding pandemics. It can be used to monitor trends and to optimize efforts, and to develop evidence based MH interventions. Still, further research focusing on the individual components of this framework is needed.
Keywords: COVID-19, Pandemic, Mental health, Framework, Interventions
1. Introduction
The outbreak of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-Cov2) virus and its associated illness, termed COVID-19, have led to a global health crisis of unparalleled proportions (Wang et al., 2020b). Deemed by the World Health Organization (WHO) as a pandemic on March 11th, 2020, COVID-19 has led to a plethora of follow-on effects, with one country after another coming under lockdown so as to bring the spread under control (Iacobucci, 2020; Lau et al., 2020; Pulla, 2020). The outbreak and the attendant measures to limit its spread have resulted in many countries reporting increased mortality and morbidity rates whilst facing huge economic losses, social disruption and physical distancing. Importantly, it has also raised concerns about the potential for a widespread increase in mental health issues (Dong and Bouey, 2020; Ho et al., 2020; Torales et al., 2020).
So far, there is a lack of evidence based guidelines and clear intervention plans, which may have limited the effectiveness and accessibility of interventions in this pandemic (Jung and Jun, 2020; Lima et al., 2020). Many mental health professionals have attempted to provide primary mental health care (advisories, psychotherapy or counseling and pharmacological treatment) through their professional organization or as volunteers (Dong and Bouey, 2020; Jung and Jun, 2020). These efforts have thus far not been well organized, stage-specific or directed towards the specific needs of the general population and health care workers (HCW) (Dong and Bouey, 2020; Lima et al., 2020; Xiang et al., 2020).
A pandemic, as a form of a disaster is a complex and unpredictable situation that, may leave limited opportunities to conduct well planned, organized and controlled clinical trials (Benight and McFarlane, 2007). Most of the published studies are cross-sectional in nature, phase-specific (i.e. either first phase of disaster or post-disaster phase) and limited to certain populations (e.g. health care workers) (Brooks et al., 2020; Lai et al., 2020; Makwana, 2019; Math et al., 2015; Wang et al., 2020a), which has limited value to develop comprehensive strategies to address the mental health issues during a pandemic. This could be due to the current theoretical framework or recommendation that fails to address the mental health needs of the affected population (Math et al., 2015; Ornell et al., 2020; Purgato et al., 2018). The Young's theoretical framework is one of the commonly used frameworks for disaster research. It includes the heroic, honeymoon, disillusionment and restoration phases of a disaster, with preventive interventions, curative interventions and preparedness as treatment strategies (Math et al., 2015, 2008). However, it is not disaster-specific (e.g. earthquake, terrorist attack, infectious disease), so it may have limited value in the current pandemic. In addition, most national and international recommendations for mental health care during disasters are vertical in nature. These recommendations or frameworks do not consider the use of recently available digital technology and global plans for mental health (Math et al., 2015). There is thus a need to reconsider the current theoretical frameworks and provide alternative approaches (Benight and McFarlane, 2007; Dong and Bouey, 2020). However, thus far, limited attempts have been made to provide new or alternative frameworks for global and national disaster preparedness.
To address the limitations of previous theoretical or conceptual frameworks and to develop global evidence-based measures, we attempted to develop a conceptual framework to address mental health care during pandemics from an early career psychiatrists' perspective.
2. Material and methods
For this study, we invited early career psychiatrists (at least one) from each WHO region to share information related to their country and the COVID-19 situation in each of their nations. This team, connected through the Early Career Psychiatrist (ECP) Section of the World Psychiatric Association (WPA) (Pinto da Costa, 2020), held group discussions via online messaging and conferencing platforms (email, WhatsApp and Zoom).
2.1. Phase-1: Preliminary assessment
This phase was directed towards assessing the current scenario of mental health and approaches (preventive and therapeutic, if any) adopted. The ECPs were requested to share information about their country (economic status, number of cases and deaths from COVID-19 at the time of writing), preparatory plans, measures (e.g. innovative, replicable or scalable) adopted or available for the future, as well as to discuss pre-existing infrastructure, ongoing training, and funding.
2.2. Phase-2: Development of an a priori conceptual framework
The lead (RR) and co-lead (FA) started developing a preliminary conceptual framework (epidemiology, interventions and outcomes) based on a comprehensive review of existing literature and the responses submitted by all the co-authors (acting as country representatives). The literature review was focused on identifying relevant existing information related to epidemiology, interventions, opinions, and recommendations. This information formed the basis of a preliminary conceptual model which we attempted to categorize as per the WHO’s pandemic preparedness plan (Droogers et al., 2019).
2.3. Phase -3: Mental health preparedness and action framework (MHPAF)
An a Priori Conceptual Framework was shared with the country representatives for comments, suggestions and modifications and was modified iteratively based on consensus and feedback. The modified delphi method (i.e. consensus decision making (>70% representative agreeable)) was adopted for final inclusion.
2.4. Ethics
As there was no direct involvement of human participants or utilization of identifiable data, ethical approval from local institutional review boards was not necessary.
3. Results
3.1. Baseline characteristics
All WHO regions were represented in this sample of early career psychiatrists. This sample included colleagues from five lower-middle-income countries (India, Nigeria, Indonesia, Egypt and Tunisia), four upper-middle-income countries (Colombia, Brazil, Iran and Lebanon), and six high-income countries (Italy, Spain, United States of America, Portugal, Singapore and New Zealand); one came from a country not recognized by the United Nations (Kosovo). All countries were in stage 5–6 as per WHO- global influenza preparedness plan (WHO-GIPP) and were reporting local transmission, except Nigeria (mainly imported) and Italy (mixed) (WHO, 2020). The countries differed from each other in terms of the occurrence of the first case, number of confirmed cases, rates of mortality and measures adopted (WHO, 2020).
3.2. A Conceptual Model of the Emotional Epidemic Curve
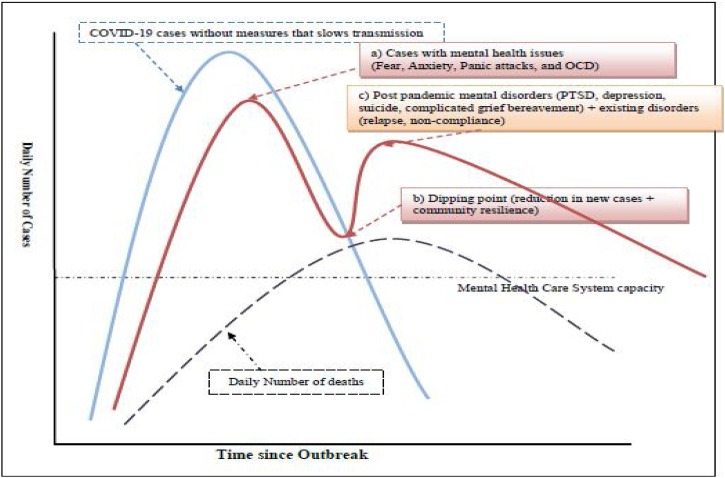
We attempted to construct a conceptual model (Emotional Epidemic Curve - EEC) to depict the possible change in emotional behaviour in different phases (Fig. 1 ). To understand the emotional epidemiology of the pandemic, we should understand the transmission dynamics of COVID-19 (serial interval-3.96 days, doubling time and extent to control the epidemic) .(Svensson, 2007).
Fig. 1.
Emotional Epidemic Curve of the COVID-19 Pandemic in acountrywithoutadequatemeasures (mitigation) (A double peak phenomenon).
Footnote: Illustrative simulations of an Emotional Epidemic Curve of the COVID-19 (red), Number of confirmed cases of COVID-19 (blue) & Number of deaths due to COVID-19 (black dotted curve), both curves may be the potential predictor of peak [i.e first peak (a) and second peak (c)] This is a qualitative illustration only, not a quantitative estimation.
3.2.1. Components of the Emotional Epidemic Curve
The EEC may have two-peaks as described below.
-
a)
First peak: It may be associated with inadequate communication, misinformation, myths and fake news. Rapid or exponential growth of COVID-19 cases may cause fear, distress, anxiety, depression, sleep disorders, panic attacks, adjustment disorders, and suicidal ideation and/or behavior (Ho et al., 2020; Li et al., 2020; Lima et al., 2020).
-
b)
Dipping point: Some countries may show a dipping point, indicative of community resilience, with a rapid reduction of distress after the first peak.
-
c)
Second peak: This can be unpredicted and complex, occurring due to the death of loved ones, economic damage and marked social disruption. The predominant effects may be post-traumatic stress disorder, grief, depression and relapse of pre-existing mental health conditions (Liu et al., 2020; Neria et al., 2008).
3.3. Mental Health Preparedness and Action Framework (MHPAF)
The WHO-Global Influenza Preparedness Plan (WHO-GIPP) neither mentions nor recommends the inclusion of a mental health component in the management of pandemics despite evidence that the mental health of the general population and health care workers is at risk (WHO, 2005). The recently published report on pandemic preparedness in WHO Member States has not taken into account the need for a mental health response (WHO, 2020). Therefore, we considered the opinions of different country representatives to develop stage-specific measures (Fig. 2 ) pertaining to the emotional epidemic curve mentioned above. The framework was prepared in line with the WHO-GIPP (WHO, 2005).
Fig. 2.
Mental Health Preparedness and Action Framework (MHPAF).
Footnote : a) Color of text box is similar to color of Phases on time line, b) Text color is similar to component (legend 2)Abbreviation: MHSS-Mental health surveillance system, HCW-health care worker (modified and developed as per WHO-GIPP Plan).
3.3.1. Brief summary of the WHO-GIPP
This includes the description of the stages of the pandemic, the role of the WHO and the recommendations for before and during a pandemic (WHO, 2005, 2009). It classifies the pandemic in six phases and includes a post-peak and post-pandemic period. The phase 1–3 measures are directed towards increasing the health care capacity through training, development of infrastructure and a surveillance system, while phase 4–6 includes the coordination, support, response and community mitigation efforts. Community mitigation efforts are vital public response measures aimed to halt transmission of the influenza virus. They include social distancing (e.g. travel restriction, working from home, closing of school, city or country lockdown), masks, respiratory and hand washing hygiene (WHO, 2005).
3.3.2. Components of MHPAF
The MHPAF is mainly focused on the development of a Mental Health Surveillance System (MHSS) to understand the epidemiology of mental disorders during the pandemic, as well as to develop possible measures directed towards reducing the burden of mental disorders and the use of appropriate technology. We have discussed these components in depth subsequently.
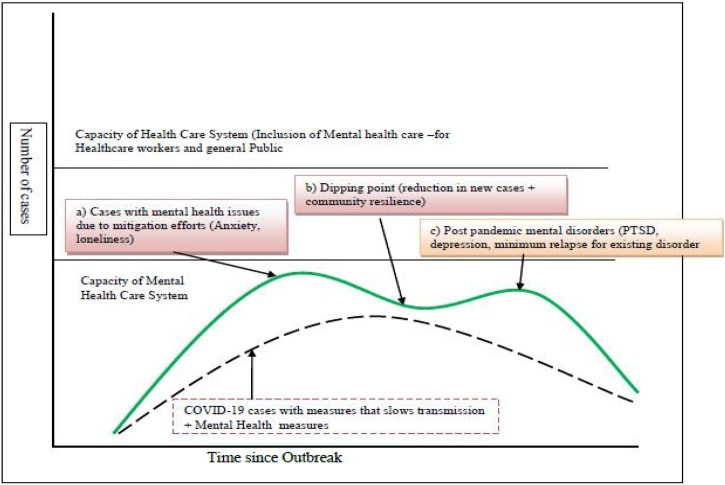
3.4. Probable Effect of MHPAF on the Emotional Epidemic Curve
In our opinion, MHPAF can address mental health issues more effectively than existing approaches. Real time data obtained through MHSS can help to prioritize interventions (e.g. population at risk, HCW), with dynamic modifications being made based on the changing needs of the population.
The effects can be categorized as follows:
COVID-19 Epidemic Curve: MHPAF along with WHO-GIPP may have an additive effect on flattening the epidemic curve, allowing more time to the first response and increasing the capacity or performance of the healthcare system (Fig. 3 ).
Fig. 3.
Effect of MHPAF + WHO-GIPP on Epidemic Curve and Health Care System.
Footnote: Illustrative simulations of Number of confirmed cases of COVID-19 (blue)
Effect of inclusion of MHPAF + Measures to reduce transmission on Epidemic Curve of the COVID-19 (green), Effect of inclusion of only Measures to reduce transmission on Epidemic Curve of the COVID-19 (red) and Incease in overall capacity of health care system (green arrow).
(This is a qualitative illustration only, not a quantitative estimation.).
Emotional Epidemic Curve (EEC): MHPAF integrated with global influenza preparedness may reduce the height of the first and second peak of EEC, and may help in flattening of the epidemic cure, and thus may reduce the prevalence of post-peak or post-pandemic disorders (Fig. 4 ). Together, the performance or capacity of the mental health system can be well preserved.
Fig. 4.
Effect of MHPAF + WHO-GIPP on Emotional epidemic curve.
Footnote: Illustrative simulations of an Emotional Epidemic Curve of the COVID-19 (blue), Number of confirmed cases of COVID-19 (dotted black curve), Additive effect of Mental health measures on both COVID-19 epidemic curve and Mental health curve. Health care system and mental health system can cope with volume of both group patients i.e. COVID-19 and mental health problems due to COVID-19.This is a qualitative illustration only, not a quantitative estimation.
4. Discussion
The paucity of organization, advanced preparation, and a lack of cross-disciplinary collaboration and integration are major hurdles that need to be overcome in creating a comprehensive and effective pandemic related mental health response (Dong and Bouey, 2020; Ornell et al., 2020). In addition, there needs to be a greater consideration of crucial parameters such as the aforementioned emotional epidemic curve. The MHPAF was focused to address most of these – it may thus provide a dedicated, sustainable, accessible, scalable and affordable mental health intervention.
4.1. Conceptual model of emotional epidemic curve of pandemic
It is noted that in the midst of a pandemic, people may experience an ‘emotional contagion’ (i.e., the spread of mood and affect through populations by the direct induction of emotions) (Hatfield et al., 1993). The fear and distress experienced by one person may be unconsciously mirrored by others, thus leading to a spread of these emotions throughout society. In our deeply interconnected and digitalized world, these emotions may spread far more easily, as dire news from one corner of the world can influence people in another distant country by a myriad of news outlets, social media networks, videos and chat rooms (Gao et al., 2020). As a consequence of this, we may expect first peak of EEC in the community. There may also be an increase in the rates of relapse and recurrence of mental disorders in those already living with mental illness (Torales et al., 2020). Furthermore, the stigma against mental health disorders, and inadequate mental health-related infrastructure, serve as additional barriers for those who are distressed to obtain help. This conceptual model is well supported by the existing literature (Ho et al., 2020; Li et al., 2020; Lima et al., 2020; Liu et al., 2020; Neria et al., 2008). The time interval between the two peaks will be dependent on country-specific measures and mitigation efforts. We note however, that in this model, we have not considered the appearance of the second wave of COVID-19 re-infection. In such case, a second wave of EEC may have a more heterogeneous mixture of cases. It is thus imperative that this emotional contagion is prepared for by stakeholders at both national and international levels.
4.2. Conceptual framework for Mental Health Preparedness and Action Framework (MHPAF)
The five components of the preparedness and action framework are closely interlinked with each other; therefore, inadequate preparation of one component can affect the success of mental health interventions before, during and after a pandemic.
4.2.1. Preparation and coordination
In the early phase of a pandemic, this component should be directed towards preparing infrastructure (e.g. Mental Health Surveillance System (MHSS) and telepsychiatry), training of volunteers and health care workers, and creating materials to disseminate during each phase, for example psychological first aid (PFA) materials, which can act as a psychological personal protective equipment (PPE).
4.2.1.1. Mental Health Surveillance System (MHSS)
A MHSS enables systematic data collection, analysis, interpretation and the timely dissemination of the data to those responsible for prevention and control of the epidemic (Nsubuga et al., 2020). Unfortunately, at present, there is no active MHSS in the sampled countries, except in Iran, Italy and Tunisia. This MHSS must be strengthened to increase the likelihood of early detection and the tracking of mental health issues. Continued virtual support and other innovative surveillance strategies (e.g., mobile app trackers and other mobile apps, screening tools) will benefit the public during a pandemic (considering the varying degrees of movement restriction and social distancing enforced) (Keesara et al., 2020; Li et al., 2020a; Xiang et al., 2020).
In the absence of a MHSS, countries will limit their opportunities to integrate and collaborate for global response and assistance, making it difficult to manage mental illnesses in the community. We recommend the establishment of a MHSS with teams (psychiatrist, psychologist and other mental health professionals) at different levels of service administration. The teams should coordinate public health, medical and emergency responses to enable the effective detection and management of common mental illnesses (Banerjee, 2020).
4.2.1.2. Psychological first aid (PFA)
The PFA (developed by WHO) has been used in many countries as the primary psychological intervention of choice (WHO, 2011). However, most HCW are inadequately trained in the intervention. In addition, the WHO-PFA does not address the primary mental health needs of the people under quarantine, those facing COVID-19 related social stigma, and those affected by national mitigation measures (social distancing, lockdowns, etc.). Furthermore, the WHO-PFA provides little attention to managing myths, misinformation and fake news, the impact of the digital world on pandemic-related distress and the effects of the epidemic curve on mental health. Thus, it does not address the first peak of the EEC nor the second. It may also have poor face- and content-validity, all of which limits its use in practice. As such, we suggest the following modifications in the WHO-PFA (Ref. Box 1 ) to address core mental health issues. Further tailoring of the PFA to the socio-cultural aspects of various nations may be required.
Box 1. Psychological first aid for COVID-19 Pandemic.
-
1
COVID-19 Pandemic: Brief overview, etiology, and mode of transmission.
-
2
Self and family care: Identifying safe areas and constructive behaviors to protect.
-
3
Primary information about COVID-19, preventive mental health, mental health promotion, and mental health surveillance.
-
4
Information regarding official websites or mobile apps, radio, television, or printed material.
-
5
Learning the calming skills and maintenance of biological functions (e.g., nutrition, sleep, rest, exercise).
-
6
Maximizing and facilitating connectedness to family and other social support systems to the extent possible (through electronic media rather than physical presence).
-
7
Fostering hope and optimism.
-
8
Identification of stage specific red flag signs of deteriorating mental health.
Alt-text: Box 1
4.2.1.3. Special cells or clinics for mental health
Major alterations to existing mental health care services have been reported in all countries during this pandemic. We noted that most countries, except Iran, had yet to create COVID 19-specific mental health services. Special clinics should be created for COVID-19 patients. The possibility of telepsychiatry or a remote clinic can provide an opportunity to limit the attendance in outpatient services.
4.2.1.4. Training
The ECPs noted that primary health care workers could do with more training in conducting PFA. We recommend that frontline health workers should be trained in PFA and they must assume a leadership position in the dissemination of updated knowledge. This can be done digitally through webinars and video-conferencing.
4.2.2. Monitoring and Assessment
4.2.2.1. Identification and monitoring of the population at risk population
The MHSS team should prepare a well-circulated and written pandemic mental health emergency plan with special attention to the population at risk (HCW, pre-existing mental illness and quarantined or isolated population). In Italy, Brazil, Lebanon and Colombia such efforts have been undertaken.
4.2.2.2. Health care technology for assessment and monitoring
Telepsychiatry, digital platforms, dedicated hotlines and mental health apps have the potential to reduce the treatment gap (Xiang et al., 2020; Yao et al., 2020). These tools were used in Italy, which were aimed at assessing, evaluating and providing psychological and psychiatric support to vulnerable people. MHSS should be equipped with such tools for monitoring and assessment in all phases of pandemic.
4.2.3. Reducing the mental distress due to misinformation and ‘myths’
In many countries, there is no well-defined approach to address the circulation of misinformation, fake news and myths related to the pandemic. Most of these myths seem religious in nature (e.g. COVID-19 can be treated by religious practices or faith healers), particularly in low-income countries. The myths, fakes and misinformation were similar to those usually referring to psychiatric disorders. Some myths can be easily predicted based on previous experiences and these should be addressed at an early phase of the pandemic.
4.2.3.1. Interventions
Social media, television and radio are the most frequently used approaches by the government to address misinformation. The MHSS team, public health system and technical team (social media, media) should be well equipped for continuous monitoring and should address myths promptly. We note the innovative concept of Corona Warriors (a team of volunteers to monitor social media sites to check for rumors) and the creation of a chatbot for this purpose (Standard, 2020). The success and sustainability of Corona Warriors will be limited if not integrated as part of a MHSS team. However, mental health preparedness and response were not included in these chatbots. The preventive tips about mental health, nearby surveillance centers and other vital information regarding mental health can be provided through these tools. In addition, global efforts should be attempted to develop technology based interventions with local translations or adaptations. These will bring the uniform approach to address the mental distress and myths.
4.2.4. Sustainability of mental health care services
4.2.4.1. Funding
Funds are critical for strengthening the country’s preparedness and response to a pandemic. Inadequate funding for mental health resources will affect mental health preparedness and the ability to mitigate against a surge of mental health related problems. We thus recommend that substantial funds should be allotted to mental health. It may help to reduce the burden of mental health disorders in both the first and second peak of EEC.
4.2.4.2. Policy
In many countries, early career psychiatrists have been redeployed to provide medical services to COVID-19 patients. This can lead to serious consequences with inadequate preparation for the second wave of EEC, a lack of mental health workers, and a lack of mental health training and support to HCW.
4.2.4.3. Coordination and collaboration
A lack of coordination and collaboration within the healthcare system can affect the delivery of mental health services during a pandemic (Banerjee, 2020). In most of the countries, there were few efforts taken to improve coordination amongst healthcare service providers. A broad, multi-disciplinary approach that sees relationships being established both within, and outside the medical fraternity (e.g. with law enforcement) is crucial to enhancing interventive strategies.
4.2.5. Communication
Communication is a key component in the mental health response during the pandemic. Previous epidemiological reports suggest that the public demands up-to-date information on an ongoing basis throughout the period (Van Bavel et al., 2020; Zandifar and Badrfam, 2020). Factual information presented by trusted public health officials and websites often assist in minimizing fear and hysteria. We opine that one of the key facets of MHSS is to communicate important and accurate information in a timely manner. We note the ongoing efforts by some governments, professional bodies and the WHO to do this – this is a commendable endeavor and we believe that these efforts need to be scaled up and continued.
4.2.5.1. Media
Traditional media (e.g. television), social media (e.g. Facebook), phone calls and official websites are commonly used to disseminate the information about COVID-19. However, this information may not be accessible to those who are illiterate, remote or underprivileged. In such a scenario, caller tunes or recorded phone calls can be used to ensure the information is more widely accessible.
4.2.5.2. Digital support groups
Few countries (e.g. Iran, Colombia and Italy) attempted to provide digital remote support through Whatsapp, Telegram, Skype, Facebook and others. Integrating telepsychiatry with digital support groups may improve the accessibility and affordability of mental health services (Yao et al., 2020).
4.3. Probable effect of MHPAF on emotional epidemiology of pandemic
We expect MHPAF to reduce the impact of the epidemic in mental health, if implemented and suitably resourced. It will help mental health professionals to prepare for the expected surge of serious mental disorders (e.g. suicide, depression). Some countries (e.g. Spain, Italy, Iran) have already initiated the redeployment of early career psychiatrists to units managing COVID-19 patients, and this move may stymie preparations to manage the anticipated mental health surge. We thus recommend that redeployment efforts should be done with caution.
4.4. Strengths and limitations
In this study, early career psychiatrists from a broad swathe of nations were interviewed, which is a strength as these are commonly those who are heavily involved, at ground-level, in the clinical mental health work and can offer key perspectives on the mental health challenges encountered. This is especially important as national level planning may, at times, not percolate down to service providers conducting front-line work. The heterogeneity between the nations from which the early career psychiatrists came, further strengthens the broad applicability of our framework across nations with varying socio-economic situations.
We are mindful, however, that further validation will be needed. Admittedly, it is difficult to conduct well planned studies or controlled trials during pandemics (Benight and McFarlane, 2007). Nonetheless, our conceptual framework can be useful for researchers to develop future studies about this topic. Indeed, MHPAF is a semi-structured framework which provides the opportunity to incorporate evidence-based interventions and the qualitative collection of data related to culture, health systems and other systems (legal, administrative and political).
This framework considers the time frame of interest (starting point of disaster to recovery trajectory). Thus, it can be used to frame various research and policy questions in advance. However, there is a need to define key terms and construct analytic strategies. In subsequent studies, we are planning to explore various components of this framework to evaluate process indicators, challenges and barriers as well as outcome evaluation in selected countries.
5. Conclusions
This conceptual framework is not a “one-size-fits-all” approach to mental health needs during a pandemic but provides a means by which national health care stakeholders can prepare for a potential rise in mental health issues. Further explorative studies with contemporary literature reviews and analytic strategies are needed to develop an effective preparedness and response plan to strengthen the response to pandemics at both national and global level.
Funding
The authors declare that there was no funding for this work.
Declaration of Competing Interest
The authors declare that they have no conflict of interest.
Acknowledgment
The authors wish to thank the Early Career Psychiatrists Section of the World Psychiatric Association (WPA) for being a supportive network that allowed to connect early career psychiatrists from different countries to work together on this initiative.
References
- Banerjee D. The COVID-19 outbreak: crucial role the psychiatrists can play. Asian J. Psychiatry. 2020;50:102014. doi: 10.1016/j.ajp.2020.102014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benight C., McFarlane A. Challenges for disaster research: recommendations for planning and implementing disaster mental health studies. J. Loss Trauma. 2007;12:419–434. [Google Scholar]
- Brooks S., Webster R., Smith L., Woodland L., Wessely S., Greenberg N., Rubin G. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395 doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong L., Bouey J. Public mental health crisis during COVID-19 pandemic, China. Emerging Infect. Dis. 2020;26 doi: 10.3201/eid2607.200407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Droogers M., Ciotti M., Kreidl P., Melidou A., Penttinen P., Sellwood C., Tsolova S., Snacken R. European pandemic influenza preparedness planning: a review of national plans, July 2016. Disaster Med. Publ. Health Prep. 2019;13:582–592. doi: 10.1017/dmp.2018.60. [DOI] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., Wang Y., Fu H., Dai J. 2020. Mental Health Problems and Social Media Exposure During COVID-19 Outbreak. Available at SSRN 3541120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatfield E., Cacioppo J.T., Rapson R.L. Emotional contagion. Curr. Dir. Psychol. Sci. 1993;2:96–100. [Google Scholar]
- Ho C.S., Chee C.Y., Ho R.C. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann. Acad. Med. Singap. 2020;49:1–3. [PubMed] [Google Scholar]
- Iacobucci G. Covid-19: UK lockdown is "crucial" to saving lives, say doctors and scientists. Bmj. 2020;368:m1204. doi: 10.1136/bmj.m1204. [DOI] [PubMed] [Google Scholar]
- Jung S.J., Jun J.Y. Mental health and psychological intervention amid COVID-19 outbreak: perspectives from South Korea. Yonsei Med. J. 2020;61:271–272. doi: 10.3349/ymj.2020.61.4.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keesara S., Jonas A., Schulman K. Covid-19 and health care’s digital revolution. N. Engl. J. Med. 2020 doi: 10.1056/nejmp2005835. [DOI] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. e203976-e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau H., Khosrawipour V., Kocbach P., Mikolajczyk A., Schubert J., Bania J., Khosrawipour T. The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J. Travel Med. 2020 doi: 10.1093/jtm/taaa037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Ge J., Yang M., Feng J., Qiao M., Jiang R., Bi J., Zhan G., Xu X., Wang L., Zhou Q., Zhou C., Pan Y., Liu S., Zhan G.H., Yang J., Zhu B., Hu Y., Hashimoto K., Jia Y., Wang H., Wang R., Liu C., Yang C. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Yang Y., Liu Z.-H., Zhao Y.-J., Zhang Q., Zhang L., Cheung T., Xiang Y.-T. Progression of mental health services during the COVID-19 outbreak in China. Int. J. Biol. Sci. 2020;16:1732–1738. doi: 10.7150/ijbs.45120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima C.K.T., Carvalho P.M.M., Lima I., Nunes J., Saraiva J.S., de Souza R.I., da Silva C.G.L., Neto M.L.R. The emotional impact of coronavirus 2019-nCoV (new Coronavirus disease) Psychiatry Res. 2020;287:112915. doi: 10.1016/j.psychres.2020.112915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J.J., Bao Y., Huang X., Shi J., Lu L. Mental health considerations for children quarantined because of COVID-19. Lancet Child Adolesc. Health. 2020 doi: 10.1016/s2352-4642(20)30096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makwana N. Disaster and its impact on mental health: a narrative review. J. Fam. Med. Prim. Care. 2019;8:3090–3095. doi: 10.4103/jfmpc.jfmpc_893_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Math S.B., Tandon S., Girimaji S.C., Benegal V., Kumar U., Hamza A., Jangam K., Nagaraja D. Psychological impact of the tsunami on children and adolescents from the andaman and nicobar islands. Prim. Care Companion J. Clin. Psychiatry. 2008;10:31–37. doi: 10.4088/pcc.v10n0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Math S.B., Nirmala M.C., Moirangthem S., Kumar N.C. Disaster management: mental health perspective. Indian J. Psychol. Med. 2015;37:261–271. doi: 10.4103/0253-7176.162915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neria Y., Nandi A., Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol. Med. 2008;38:467–480. doi: 10.1017/S0033291707001353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nsubuga P., White M.E., Thacker S.B., Anderson M.A., Blount S.B., Broome C.V., Chiller T.M., Espitia V., Imtiaz R., Sosin D., J.D.c.p.i.d.c Public health surveillance: a tool for targeting and monitoring interventions. Dis. Control Priorities Dev. Ctries. 2020;2:997–1018. [Google Scholar]
- Ornell F., Schuch J., Sordi A., Kessler F. “Pandemic fear” and COVID-19: mental health burden and strategies. Braz. J. Psychiatry. 2020 doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto da Costa M. Early career psychiatrists – history, 2020 and beyond. World Psychiatry. 2020;19:127–128. doi: 10.1002/wps.20712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pulla P. Covid-19: India imposes lockdown for 21 days and cases rise. Bmj. 2020;368:m1251. doi: 10.1136/bmj.m1251. [DOI] [PubMed] [Google Scholar]
- Purgato M., Gastaldon C., Papola D., van Ommeren M., Barbui C., Tol W.A. Psychological therapies for the treatment of mental disorders in low- and middle-income countries affected by humanitarian crises. Cochrane Database Syst. Rev. 2018;7:Cd011849. doi: 10.1002/14651858.CD011849.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Standard, B., https://www.business-standard.com/article/news-ani/karnataka-hires-corona-warriors-to-provide-real-time-information-avoid-fake-news-menace-120032100178_1.html.
- Svensson A. A note on generation times in epidemic models. Math. Biosci. 2007;208:300–311. doi: 10.1016/j.mbs.2006.10.010. [DOI] [PubMed] [Google Scholar]
- Torales J., O’Higgins M., Castaldelli-Maia J.M., Ventriglio A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry. 2020 doi: 10.1177/0020764020915212. 20764020915212. [DOI] [PubMed] [Google Scholar]
- Van Bavel J.J., Boggio P., Capraro V., Cichocka A., Cikara M., Crockett M., Crum A., Douglas K., Druckman J., Drury J. 2020. Using Social and Behavioural Science to Support COVID-19 Pandemic Response. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17 doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L.S., Wang Y.R., Ye D.W., Liu Q.Q. A review of the 2019 Novel Coronavirus (COVID-19) based on current evidence. Int. J. Antimicrob. Agents. 2020 doi: 10.1016/j.ijantimicag.2020.106137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Oganization . 2005. Pandemic Influenza Preparedness in WHO Member States: Report of a Member States Survey.https://apps.who.int/iris/bitstream/handle/10665/325411/9789241515962-eng.pdf?ua=1 Available from: [Google Scholar]
- World Health Organization . 2009. WHO Global Influenza Preparedness Plan: The Role of WHO and Recommendations for National Measures Before and During Pandemics.https://www.who.int/csr/resources/publications/influenza/WHO_CDS_CSR_GIP_2005_5.pdf Available from: [Google Scholar]
- World Health Organization . World Health Organization; 2011. Psychological First Aid: Guide for Field Workers. [Google Scholar]
- World Health Organization Coronavirus disease . 2020. World Health Organization Coronavirus Disease 2019 (COVID-19) Situation Report – 73.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200402-sitrep-73-covid-19.pdf?sfvrsn=5ae25bc7_4 [Google Scholar]
- Xiang Y.T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T., Ng C.H. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. 2020;7:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao H., Chen J.-H., Xu Y.-F. Rethinking online mental health services in China during the COVID-19 epidemic. Asian J. Psychiatry. 2020;50 doi: 10.1016/j.ajp.2020.102015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zandifar A., Badrfam R. Iranian mental health during the COVID-19 epidemic. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.101990. [DOI] [PMC free article] [PubMed] [Google Scholar]