Abstract
Since the outbreak of novel coronavirus disease (COVID-19) in December 2019, it has spread to various regions and countries, forming a global pandemic. Reducing nosocomial infection is a new issue and challenge for all healthcare systems. Otolaryngology is a high-risk specialty as it close contact with upper respiratory tract mucous, secretions, droplets and aerosols during procedures and surgery. Therefore, infection prevention and control measures for this specialty are essential. Literatures on the epidemiology, clinical characteristics and infection control measures of COVID-19 were reviewed, practical knowledge from first-line otolaryngologists in China, the United States, and Brazil were reviewed and collated. It was recommended that otolaryngology professionals should improve screening in suspected patients with relevant nasal and pharyngeal symptoms and signs, suspend non-emergency consultations and examinations in clinics, and rearrange the working procedures in operating rooms. The guidelines of personal protective equipment for swab sampling, endoscopy and surgery were listed. Indications for tracheotomy during the pandemic should be carefully considered to avoid unnecessary airway opening and aerosol-generation; precautions during surgery to reduce the risk of exposure and infection were illustrated. This review aimed to provide recommendations for otolaryngologists to enhance personal protection against COVID-19 and reduce the risk of nosocomial infection.
Keywords: COVID-19, SARS-CoV-2, Otolaryngology, Infection control, Tracheotomy
1. Introduction
In December 2019, a novel coronavirus infection broke out in Wuhan, China [1]. This virus has spread rapidly across the country and is now a global pandemic [2,3]. The virus is named SARS-CoV-2, and the disease caused by the virus is called 2019 novel coronavirus disease (COVID-19) [4]. SARS-CoV-2 belongs to lineage B of genus Betacoronavirus [5], shares 96% homology to a bat coronavirus and 79.6% homology to SARS-CoV at the whole genome level [6], but is less similar to the MERS-CoV [7]. By March 2020, COVID-19 caused by SARS-CoV-2 has more than 82,000 cases in China and more than 1,347,000 all around the world [8]. Pneumonia is its main manifestation, although most cases are mild, but 14% of cases present severe symptoms such as dyspnea, reduced blood oxygen saturation, 5% turn to critical with acute respiratory distress syndrome (ARDS) and shock [2], 1.4–4.3% to death [9,10]. However, due to the abruptness of COVID-19, its rapid increase in the number of infected populations has placed a heavy load on local healthcare systems, due especially to the high requirement for intensive care unit (ICU) and invasive ventilation [11]. As a result, the mortality rate at the center of the national epidemic storm tends to be more severe (7.2–15%) [1,12]. After the outbreak, the specialties that usually need to be in close contact with patients or to deal with the airway management, such as ophthalmology [13], stomatology [14], anesthesiology [15], have issued relevant infection control and prevention measures for COVID-19. Therefore, this review summarized the experiences in China, the United States, and Brazil, thus providing practical guidance for otolaryngologists under this pandemic.
2. Risk for otolaryngologic professionals
Human to human transmission of SARS-CoV-2 has been confirmed [16], and the infection is highly contagious with about 2.2–3.6 basic reproductive number that is slightly higher than SARS-CoV, but lower than MERS-CoV [[17], [18], [19]]. Direct contact, airborne and droplet are the most common transmission routes. Although SARS-CoV-2 mainly invades the lower respiratory tract, nasopharynx and oropharynx have been proved to have virus shedding [20,21]. For otolaryngologists, most examinations and treatments require inevitable contact with upper airway mucosa and face to face position, and any reflex coughing or sneezing during procedures will cause a direct contamination to medical staffs. Some aerosol generating procedures such as nasal endoscopy and laryngoscopy will increase virus infectivity and contribute to working environment contamination up to several days [[22], [23], [24]]. Generally, otolaryngology is in a high-risk level during this pandemic. Since nosocomial transmission has been confirmed and more than 3000 health care personnel have been infected in China during the epidemic [10], it is important for otolaryngologic staffs to enhance personal protection against nosocomial infections based on current experience and lessons learned from SARS epidemic [25].
3. Preventive measures
3.1. Patients' screening
Identifying infected or suspicious patients is the first step that will help both medical staffs and patients to quickly enter standard COVID-19 infection prevent and control management procedures and avoid unnecessary risks of nosocomial transmission [26]. Otolaryngologists should pay attention to symptoms. Although common discomforts in COVID-19 patients are fever, cough, shortness of breath and sometimes associated with sputum, fatigue, myalgia, some patients also have regular ENT complaints such as sore throat (13.9–60%), rhinorrhea (4–6%) and nasal obstruction (4.8%) [1,9,12,27], 2.1% has tonsil swelling and 1.7% has throat congestion [9]. In other countries, such as Brazil, the USA and Europe, COVID-19 has also been associated with other changes such as anosmia and dysgeusia [28,29]. These symptoms in an isolated form also constitute criteria for quarantine. Abdominal pain and skin rash have also been reported, and can be confusing symptoms in countries where dengue, chikungunya and measles are already epidemic [30]. Epidemiological contact history in about 7 days is another key to assess a suspicious infection [17]. Early in China's experience, 72.3% patients had had contact with people in the original city, Wuhan, and 31.3% had shown travel history [9]. However, with rapid global widespread and infection increase in communities, not only travel history but also any contact or staying in an enclosed environment with people who have been confirmed or suspected with respiratory illness in the previous 14 days should be noted. In China, many people have been infected while caring for sick family members, thus infections transmission in families cannot be ignored [16].
3.2. Examination suggestion
Asymptomatic transmission is an important characteristic of COVID-19 [31,32], there is 1.8% potential infectivity among population with negative symptoms screening result [33]. Therefore, for suspected patients without typical symptoms, necessary examinations should be performed to exclude potential infection. Chest X-radiography or CT is recommended firstly, and pulmonary ground-glass opacity (GGO) and bilateral infiltration manifestation usually indicate SARS-CoV-2 related infection [34]. Blood test will provide additional support for diagnosis, confirmed patients often have lymphopenia and elevated CRP level, or leukopenia or thrombocytopenia [10]. SARS-CoV-2 real-time reverse transcriptase–polymerase chain reaction (RT-PCR) test is the clinical diagnostic criteria [35]. Recently, antibody test was applied and elevated IgM after 5 days of symptom indicated early infection [36]. But the clinical use of the latter two depends on the detection capability of local healthcare system.
3.3. Medical service management
Given the severity of virus transmission and the rapid growth in the number of infected patients, healthcare services should be adjusted accordingly to reduce the accumulation of patients in hospitals, reduce the risk of nosocomial transmission to staffs and other patients, and ensure enough medical services and supplies to respond outbreaks of respiratory infective disease [37]. In the Chinese experience, during the early outbreak, ENT clinic, routine endoscopy and surgeries were suspended, only emergency cases were seen and surgeries were performed until the epidemic was well controlled. Elderly medical staff or with co-morbidities such as cardiovascular disease, hypertension, diabetes and cancer, who are susceptible to more severe infection and worse prognosis [2,38], were suggested to avoid engaging with high infection risk medical procedures.
We also suggest the restriction in the necessary number of assistants during procedures and segregate into smaller teams or individuals to cover entire services, with the goal to keep as many physicians and residents home each day as possible, to minimize the chance of transmission between providers if someone gets exposed or infected.
In the author's (C.Z) hospital, telemedicine has been implemented during pandemic. Patients can make appointments through a mobile app and have text consultation with doctors. After an initial evaluation, the doctor can decide if an in presence consultation is needed and permitted to visit in hospital. Meanwhile, most postoperative patients can get remote recovery instructions. The service is currently free during the outbreak.
3.4. Personal protective equipment (PPE) for otolaryngology
In addition to strict airborne and contact precautions, PPE is necessity for health care staff against SARS-CoV-2 [39,40]. Otolaryngologists should choose appropriate protective equipment based on medical operations, respectively. Routine inquiry or simple examination, such as anterior rhinoscopy and oropharyngeal inspection, require basic protection, including surgical cap, NIOSH-certified disposable N95 filtering respirator, goggles, gown and gloves. If the procedures is likely to have close contact with respiratory droplets or aerosols caused by involuntary coughing, sneezing and deeply breathing, such as throat swabs, endoscopy for nose and larynx, treatment for nasal bleeding and foreign body in pharynx, in our experience more protection should be utilized, including wearing coveralls inside the gown, water-resistant boot covers, face shield outside the goggle (Fig. 1a), aiming to minimize skin exposure. Double-layer gloves are recommended in case of a tearing accident, while the inner layer can provide greater security while putting off the external equipment. Invasive airway procedures such as tracheotomy are at the highest risk and require powered air purifying respirator (PAPR) to provide seamless resistance to aerosols (Fig. 1b).
Fig. 1.
(a) Personal protection with surgical mask, N95 filtering respirator (under facial mask), goggle, face shield, coveralls, gown, gloves, water-resistant boot covers as high risk operation will be performed, such as throat swab, endoscopy. (b) Powered air purifying respirator (PAPR) substitute for face shield to provide more sufficient protection for invasive airway operation such as tracheotomy.
On the one hand, it should be noted that most nosocomial infections do not occur with careful protection, but when protective equipment is removed while hands, eyes, nose accidentally touch the contaminated surface of the protective equipment. On the other hand, unlike the department of infectious disease, emergency, intensive care medicine, otolaryngology has less knowledge and training on how to use PPE, which increases the risk of nosocomial infections. Practical training and exercises prior to clinical use should be conducted.
4. Treatment
Regarding treatment, there is still no concrete information. There are reports about the use of hydroxychloroquine and azithromycin in severe cases [41], for rescue, in the hospital environment. However, there are records of indiscriminate use of hydroxychloroquine by the population, without any form of risk control. Reports of cardiovascular toxic manifestations (hypotension, suppression of myocardial function, cardiac arrhythmias and cardiac arrest) have been recorded among these patients in indiscriminate use. Hydroxychloroquine is used to treat rheumatoid arthritis, systemic lupus erythematosus, malaria, among other diseases. The use of topical and systemic corticosteroids has been contraindicated. Use of vasoconstrictors to control nasal symptoms and nasal lavage with small volumes to avoid swallowing. Antipyretics, oxygen supplementation and, in cases with severe dyspnea, use of respiratory ventilators.
4.1. Tracheotomy consideration during pandemic
Tracheotomy is a routine operation to otolaryngologist [42], but it is an invasive open airway surgery with aerosolization [43]. When patients infected by SARS-CoV-2 undergo the procedure, aerosol mixed with secretions and blood will constitute a high risk to medical staffs, therefore it should be decided and performed with caution. During this epidemic, tracheostomy is most likely to be performed to severe or critical patients who have undergone endotracheal intubation and mechanical ventilation because of unsustainable blood oxygen saturation and long ICU stay. Whether tracheotomy is needed and when is the optimal timing are still controversial issues. Some studies suggest that early tracheotomy (usually 5-7 days after intubation), in patients with respiratory failure can reduce ventilation dead space, airway resistance, sedation usage [44], decrease the incidence of sepsis and mechanical ventilation-related pneumonia [45], reduce duration of mechanical ventilation and ICU stay [46], increase the chance of discharge [47,48]. However, other studies show that early tracheotomy is only beneficial for some selected ICU patients [49], especially for traumatized patients [50,51]. Pneumonia and consequent ARDS are the main problems for COVID-19 patients with intubation [52,53]. For pneumonia, several meta-analyses demonstrate that there is insufficient evidence for early tracheotomy to reduce incidence of mechanical ventilation-associated pneumonia [54,55]. For ARDS, early tracheostomy should not be performed or only performed to limited patients according to some clinical guidelines [56,57]. Once ventilation for more than 2 weeks, the mortality and disability will eventually increase with or without tracheotomy [58]. Therefore, tracheotomy should be evaluated carefully in intubated COVID-19 patients and only be performed with exact benefit expectation. Patients with apparent intolerance to transoral intubation or high muscle load due to increased airway resistance maybe an appropriate indication [59].
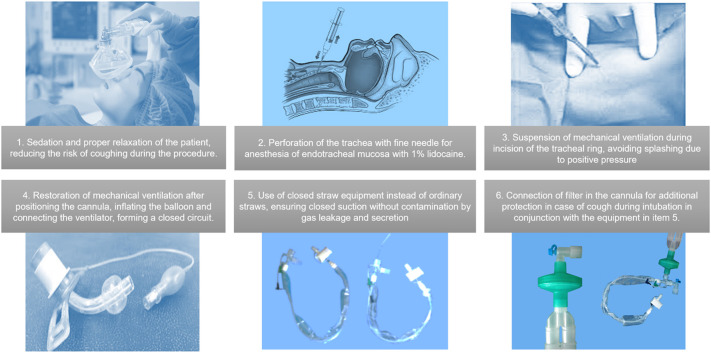
However, in practical terms, ENT surgeons seldom decide whether to perform a tracheotomy to COVID-19 patients, instead, they usually act in concert with the plan decided by ICU, infectious disease and respiratory specialists. Therefore, otolaryngologists should be prepared for the procedure, including the highest level of personal protection, as described above, and operating skills to reduce aerosol infection (Fig. 2 ). For experienced surgeons, tracheostomy in COVID-19 patients receiving extracorporeal membrane oxygenation (ECMO) does not significantly increase the risk of bleeding and death, the use of anticoagulants is not a contraindication [60].
Fig. 2.
1. Communicating with the anesthesiologist to ensure adequately sedated and relaxed to reduce coughing. 2. Performing extra endotracheal mucosal anesthesia. 3. Suspending mechanical ventilation while trachea ring is incised. 4. Restoring mechanical ventilation until forming a closed circuit. 5. Using enclosed straws equipment instead of ordinary straws. 6. Attaching a filter to provide additional protection.
5. Conclusions
The epidemic of COVID-19 has spread globally and the pandemic situation is very grim. Otolaryngology medical staff, as high-risk exposed professionals, should enhance protection awareness. Screening patients carefully, conducting advanced training on PPE, preparing appropriate personal protection while performing high-risk operations will help reduce the incidence of nosocomial infections. With the progression of the disease to other populations, new clinical changes have been registered and deserve the constant attention of professionals.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and materials
Not applicable.
Funding
Not applicable.
Authors' contributions
CZ, AV, YW, HQW, AHY, RC collected and analyzed the material. CZ and AV were major contributors in writing the manuscript. RC was major supervision. All authors read and approved the final manuscript.
Declaration of competing interest
The authors declare that they have no competing interests.
Acknowledgements
Not applicable.
References
- 1.Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020 doi: 10.1001/jama.2020.2648. Feb 24. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization . World Health Organization; Geneva: 2020. 2020 coronavirus disease (COVID-2019) situation reports.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports [Google Scholar]
- 4.World Health Organization WHO Director General's remarks at the media briefing on 2019 nCoV on 11 February 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-2019-ncov-on-11-february-2020
- 5.Lu R., Zhao X., Li J., Niu P., Yang B., Wu H. Genomic characterization and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou P., Yang X.L., Wang X.G., Hu B., Zhang L., Zhang W. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579(7798):270–273. doi: 10.1038/s41586-020-2012-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu A., Peng Y., Huang B., Ding X., Wang X., Niu P. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe. 2020;27(3):325–328. doi: 10.1016/j.chom.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.John'’s Hopkins University Medicine Coronavirus resource center. https://coronavirus.jhu.edu/map.html
- 9.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Qu C.Q., He J.X. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 Feb 28 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 Feb 7 doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H. Clinical course and outcomes of critically ill patients withSARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30079-5. Feb 24. pii: S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Onder G., Rezza G., Brusaferro S. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA. 2020 doi: 10.1001/jama.2020.4683. Mar 23. [DOI] [PubMed] [Google Scholar]
- 13.Lai T.H.T., Tang E.W.H., Chau S.K.Y., Fung K.S.C., Li K.K.W. Stepping up infection control measures in ophthalmology during the novel coronavirus outbreak: an experience from Hong Kong. Graefes Arch Clin Exp Ophthalmol. 2020 doi: 10.1007/s00417-020-04641-8. Mar 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Peng X., Xu X., Li Y., Cheng L., Zhou X., Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12(1):9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wax R.S., Christian M.D. Practical recommendations for critical care and anesthesiology teams caring for novel coronavirus (2019-nCoV) patients. Can J Anaesth. 2020 doi: 10.1007/s12630-020-01591-x. Feb 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chan J.F., Yuan S., Kok K.H., To K.K., Chu H., Yang J. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li Q., Guan X., Wu P., Wang X.Y., Zhou L., Tong Y.Q. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382(13):1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zhao S., Lin Q., Ran J., Musa S.S., Yang G., Wang W. Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: a data-driven analysis in the early phase of the outbreak. Int J Infect Dis. 2020;92:214–217. doi: 10.1016/j.ijid.2020.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou T., Liu Q., Yang Z., Liao J., Yang K., Bai W. Preliminary prediction of the basic reproduction number of the Wuhan novel coronavirus 2019-nCoV. J Evid Based Med. 2020;13(1):3–7. doi: 10.1111/jebm.12376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zou L., Ruan F., Huang M., Liang L., Huang H., Hong Z. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382(12):1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang W., Xu Y., Gao R., Lu R., Han K., Wu G. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020 doi: 10.1001/jama.2020.3786. Mar 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020 doi: 10.1056/NEJMc2004973. March 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ong S.W.X., Tan Y.K., Chia P.Y., Lee T.H., Ng O.T., Wong M.S.Y. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA. 2020 Mar 4 doi: 10.1001/jama.2020.3227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kampf G., Todt D., Pfaender S., Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104(3):246–251. doi: 10.1016/j.jhin.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chan J.Y.K., Wong E.W.Y., Lam W. Practical aspects of otolaryngologic clinical services during the 2019 novel coronavirus epidemic: an experience in Hong Kong. JAMA Otolaryngol Head Neck Surg. 2020 doi: 10.1001/jamaoto.2020.0488. Mar 20. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization Interim guidance: infection prevention and control during health care when novel coronavirus (nCoV) infection is suspected. https://www.who.int/publications-detail/infection-prevention-and-control-during-health-care-when-novel-coronavirus-(ncov)-infection-is-suspected-20200125
- 27.Young B.E., Ong S.W.X., Kalimuddin S., Low J.G., Tan S.Y., Loh J. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA. 2020 doi: 10.1001/jama.2020.3204. Mar 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.AAO-HNS Anosmia, hyposmia, and dysgeusia symptoms of coronavirus disease. https://www.entnet.org/content/aao-hns-anosmia-hyposmia-and-dysgeusia-symptoms-coronavirus-disease
- 29.Baig A.M., Khaleeq A., Ali U., Syeda H. Evidence of the COVID-19 virus targeting the CNS: tissue distribution, host-virus interaction, and proposed neurotropic mechanisms. ACS Chem Nerosci. 2020 doi: 10.1021/acschemneuro.0c00122. Mar 13. [DOI] [PubMed] [Google Scholar]
- 30.Joob B., Wiwanitkit V. COVID-19 can present with a rash and be mistaken for Dengue. J Am Acad Dermatol. 2020 doi: 10.1016/j.jaad.2020.03.036. Mar 22. pii: S0190-9622 (20)30454-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bai Y., Yao L., Wei T., Tian F., Jin D.Y., Chen L. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020 doi: 10.1001/jama.2020.2565. February 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rothe C., Schunk M., Sothmann P., Bretzel G., Froeschl G., Wallrauch C. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N Engl J Med. 2020;382(10):970–971. doi: 10.1056/NEJMc2001468. Mar 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hoehl S., Rabenau H., Berger A., Kortenbusch M., Cinatl J., Bojkova D. Evidence of SARS-CoV-2 infection in returning travelers from Wuhan, China. N Engl J Med. 2020;382(13):1278–1280. doi: 10.1056/NEJMc2001899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bernheim A., Mei X., Huang M., Yang Y., Fayad Z.A., Zhang N. Chest CT findings in coronavirus disease-19 (COVID-19): relationship to duration of infection. Radiology. 2020 doi: 10.1148/radiol.2020200463. doi: 10.1148/radiol.2020200463. Feb 20. 200463. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Corman V.M., Landt O., Kaiser M., Molenkamp R., Meijer A., Chu D.K.W. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25(3) doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guo L., Ren L., Yang S., Chang Xiao M., Yang F. Profiling early humoral response to diagnose novel coronavirus disease (COVID-19) Clin Infect Dis. 2020 Mar 21 doi: 10.1093/cid/ciaa310. pii: ciaa 310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Megan L.R., Valerie G., Ashish K.J. Critical supply shortages-the need for ventilators and personal protective equipment during the Covid-19 pandemic. N Engl J Med. 2020 doi: 10.1056/NEJMp2006141. March 25. [DOI] [PubMed] [Google Scholar]
- 38.Liang W., Guan W., Chen R., Wang W., Li J., Xu K. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention Interim infection prevention and control recommendations for patients with known or patients under investigation for 2019 novel coronavirus (2019-nCoV) in a healthcare setting. https://www.cdc.gov/coronavirus/2019-nCoV/hcp/infection-control.html Updated February 21, 2020.
- 40.World Health Organization Infection prevention and control of epidemic- and pandemic-prone acute respiratory infections in health care: WHO guidelines. http://apps.who.int/iris/10665/112656 [PubMed]
- 41.Gautret P., Lagier J.C., Parola P., Hoang V.T., Meddeb L., Mailhe M. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020 doi: 10.1016/j.ijantimicag.2020.105949. Mar 20. 105949. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 42.de Kleijn B.J., Wedman J., Zijlstra J.G., Dikkers F.G., van der Laan B.F.A.M. Short- and long-term complications of surgical and percutaneous dilatation tracheotomies: a large single-centre retrospective cohort study. Eur Arch Otorhinolaryngol. 2019;276(6):1823–1828. doi: 10.1007/s00405-019-05394-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tran K., Cimon K., Severn M., Pessoa-Silva C.L., Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7(4) doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaese S., Zander M.C., Lebiedz P. Successful use of early percutaneous dilatational tracheotomy and the no sedation concept in respiratory failure in critically ill obese subjects. Respir Care. 2016;61(5):615–620. doi: 10.4187/respcare.04333. [DOI] [PubMed] [Google Scholar]
- 45.Villwock J., Jones K. Outcomes of early versus late tracheostomy: 2008–2010. Laryngoscope. 2014;124(8):1801–1806. doi: 10.1002/lary.24702. [DOI] [PubMed] [Google Scholar]
- 46.Adly A., Youssef T.A., El-Begermy M.M., Younis H.M. Timing of tracheostomy in patients with prolonged endotracheal intubation: a systematic review. Eur Arch Otorhinolaryngol. 2018;275(3):679–690. doi: 10.1007/s00405-017-4838-7. [DOI] [PubMed] [Google Scholar]
- 47.Mehta A.B., Cooke C.R., Wiener R.S., Walkey A.J. Hospital variation in early tracheostomy in the United States: a population-based study. Crit Care Med. 2016;44(8):1506–1514. doi: 10.1097/CCM.0000000000001674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Patel S.A., Plowman E.K., Halum S., Merati A.L., Sardesai M.G. Late tracheotomy is associated with higher morbidity and mortality in mechanically ventilated patients. Laryngoscope. 2015;125(9):2134–2138. doi: 10.1002/lary.25322. [DOI] [PubMed] [Google Scholar]
- 49.Blot F., Similowski T., Trouillet J.L., Chardon P., Korach J.M., Costa M.A. Early tracheotomy versus prolonged endotracheal intubation in unselected severely ill ICU patients. Intensive Care Med. 2008;34(10):1779–1787. doi: 10.1007/s00134-008-1195-4. [DOI] [PubMed] [Google Scholar]
- 50.Aquino Esperanza J., Pelosi P., Blanch L. What’s new in intensive care: tracheostomy-what is known and what remains to be determined. Intensive Care Med. 2019;45(11):1619–1621. doi: 10.1007/s00134-019-05758-z. [DOI] [PubMed] [Google Scholar]
- 51.Young D., Harrison D.A., Cuthbertson B.H., Rowan K. Effect of early vs late tracheostomy placement on survival in patients receiving mechanical ventilation: the TracMan randomized trial. JAMA. 2013;309(20):2121–2129. doi: 10.1001/jama.2013.5154. [DOI] [PubMed] [Google Scholar]
- 52.Sweeney R.M., McAuley D.F. Acute respiratory distress syndrome. Lancet. 2016;388(10058):2416–2430. doi: 10.1016/S0140-6736(16)00578-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Luks A.M. Ventilatory strategies and supportive care in acute respiratory distress syndrome. Influenza Other Respi Viruses. 2013;7(Suppl. 3):8–17. doi: 10.1111/irv.12178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Andriolo B.N., Andriolo R.B., Saconato H., Atallah Á.N., Valente O. Early versus late tracheostomy for critically ill patients. Cochrane Database Syst Rev. 2015 Jan 12;1 doi: 10.1002/14651858.CD007271.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shan L., Hao P., Xu F., Chen Y.G. Benefits of early tracheotomy: a meta-analysis based on 6 observational studies. Respir Care. 2013;58(11):1856–1862. doi: 10.4187/respcare.02413. [DOI] [PubMed] [Google Scholar]
- 56.Hashimoto S., Sanui M., Egi M., Ohshimo S., Shiotsuka J., Seo R. The clinical practice guideline for the management of ARDS in Japan. J Intensive Care. 2017 Jul 25;5:50. doi: 10.1186/s40560-017-0222-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cho Y.J., Moon J.Y., Shin E.S., Kim J.H., Jung H., Park S.Y. Clinical practice guideline of acute respiratory distress syndrome. Tuberc Respir Dis (Seoul) 2016;79(4):214–233. doi: 10.4046/trd.2016.79.4.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Herridge M.S., Chu L.M., Matte A., Tomlinson G., Chan L., Thomas C. The RECOVER program: disability risk groups and 1-year outcome after 7 or more days of mechanical ventilation. Am J Respir Crit Care Med. 2016;194(7):831–844. doi: 10.1164/rccm.201512-2343OC. [DOI] [PubMed] [Google Scholar]
- 59.MacIntyre N.R., Cook D.J., Ely E.W., Jr., Epstein S.K., Fink J.B., Heffner J.E. Evidence-based guidelines for weaning and discontinuing ventilatory support: a collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest. 2001;120(6 Suppl) doi: 10.1378/chest.120.6_suppl.375s. (375S-95S) [DOI] [PubMed] [Google Scholar]
- 60.Yeo H.J., Yoon S.H., Lee S.E., Jeon D., Kim Y.S., Cho W.H. Safety of surgical tracheostomy during extracorporeal membrane oxygenation. Korean J Crit Care Med. 2017;32(2):197–204. doi: 10.4266/kjccm.2017.00059. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.