Abstract
Female sex workers (FSW) are a marginalized and vulnerable population at high risk of gender-based violence within and outside of their occupation. However, FSW remain underrepresented in the trauma and mental health literature. The aims of this study were to: (1) Characterize exposure to violence among street-based FSW, including violence type, patterns over the life course, and key perpetrator groups; (2) Examine the multivariate associations between PTSD symptom severity and two constructs (revictimization across life stages and cumulative violence). Data were drawn from the SAPPHIRE study, an observational community-based cohort of street-based FSW recruited through targeted sampling across Baltimore, Maryland, USA in 2016–2017. PTSD symptom severity was measured using the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5). At baseline, 61% of FSW screened positive for PTSD symptoms. The mean PCL-5 score was 38.6. We documented extensive histories of sexual and physical violence (lifetime: 81.8%; childhood and adult revictimization: 15.0% for sexual and 37.7% for physical). The vast majority of perpetrators were male and included paying clients, police officers, family members, and intimate partners. Exposure to childhood and adult sexual violence were independently associated with higher PTSD severity (p<0.05), with marginal associations observed for physical violence. Data supported a cumulative violence model of PTSD severity (p<0.05). Binge drinking also appeared to be a contributing factor (p<0.05). The levels of PTSD observed among our sample were comparable to that reported among treatment-seeking war veterans. Our findings underscore the urgent need for tailored trauma-informed interventions and policies to address violence among urban street-based FSW, a population experiencing extremely high levels of violence, PTSD and substance use.
Keywords: sex work, trauma, mental health
Introduction
Violence against women and girls remains a pressing public health issue globally. More than one in three women have been exposed to sexual or physical violence in their lifetime, mostly perpetrated by male intimate partners (World Health Organization, 2013b). Exposure to violence often starts early; among U.S. women, 42% have been exposed to sexual violence during childhood (Black et al., 2011). One in four U.S. women have experienced intimate partner violence (IPV), some as minors, and about half develop symptoms of posttraumatic stress disorder (PTSD) (Black et al., 2011). Population-level studies show that women are more likely to be exposed to sexual violence and are twice as likely to develop PTSD compared to men (Breslau et al., 1998; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995). Sex differences in physiological and cognitive responses to stress, as well as social gender roles (e.g. reliance on passive coping styles) may explain the higher observed burden of PTSD among women (Olff, Langeland, Draijer, & Gersons, 2007).
Female sex workers (FSW) are a population defined by the United Nations as women “who receive money or goods in exchange for sexual services.” Sex work may be formal or informal, voluntary or coerced (Joint United Nations Programme on HIV/AIDS, 2012); the latter meets U.S. definition of sex trafficking alongside entering sex work as a minor. Violence is pervasive in the lives of these women. Globally, between 40–90% of FSW have been exposed to sexual or physical violence in their lifetime (Deering et al., 2014). While many of the deleterious socio-cultural factors affecting all women play a role in increasing FSW vulnerability to gender-based violence (Connell & Pearse, 2014; Heise & Kotsadam, 2015), sex work poses unique occupational challenges to health and safety. In most settings, sex work remains illegal and highly stigmatized, which render FSW vulnerable to violence and coercion, and pose major barriers when seeking health and social services, legal protection and justice following victimization (Decker et al., 2015). For example, FSW frequently report being robbed, beaten up or thrown out of moving cars by clients while working (Lim et al., 2015; Shannon et al., 2009; Wirtz et al., 2015). Gender-based power dynamics, social expectations and stigma towards women in sex work are also strong forces that reverberate in FSW interactions with paying clients and police officers, who are often exclusively male, and frequently perpetrate sexual coercion, bribery and violence against FSW (Erausquin, Reed, & Blankenship, 2011; Footer et al., 2019; Rhodes, Simic, Baros, Platt, & Zikic, 2008; Shannon et al., 2009; Wirtz et al., 2015). Many FSW are also exposed to childhood abuse and IPV prior to entering sex work (Deering et al., 2014; Surratt, Kurtz, Weaver, & Inciardi, 2005). Unsurprisingly, the prevalence of mental health issues among FSW are high, with PTSD symptom prevalence often greater than 50% where studied, although studies are rare (Farley et al., 2004; Roxburgh, Degenhardt, & Copeland, 2006).
A common reason for entering and remaining in sex work among street-based FSW is the need to financially support an active drug addiction, as reviewed previously (Vanwesenbeeck, 2001). Others have suggested that sex work can precede specific forms of substance use, such as injection drug use (Morris et al., 2013) and negative coping, including drug use to chemically dissociate from the hardships of sex work (Romero-Daza, Weeks, & Singer, 2003). Violence, mental health and substance use can serve as mutually reinforcing conditions; survivors with a history of trauma may use drugs/alcohol as an avoidant coping mechanism, which in turn may increase the risk of future victimization (Kilpatrick, Acierno, Resnick, Saunders, & Best, 1997; Krause, Kaltman, Goodman, & Dutton, 2008; Ullman, Relyea, Peter-Hagene, & Vasquez, 2013). While drug use may dampen PTSD symptoms in the short term, drug withdrawal may elevate PTSD symptoms and prolonged drug use may increase the risk of chronic PTSD (Jacobsen, Southwick, & Kosten, 2001).
Only a small subset of trauma-exposed individuals develop PTSD (Breslau, 2002). To better understand the etiology of PTSD stemming from interpersonal violence, a cumulative model of abuse has been proposed by Scott-Storey whereby all lifetime exposures are taken into consideration when modeling their relationship to PTSD (Scott-Storey, 2011). National studies have shown that recurrent violence is associated with higher odds of PTSD in the past 6 months (Walsh et al., 2012) however studies examining accumulated forms of abuse across the life course, especially those that incorporate other types of life stress and co-morbidities, are less common (Finkelhor, Ormrod, & Turner, 2007; Scott-Storey, 2011). Examining the impact of interpersonal violence on PTSD severity alongside “chronic strain” factors (i.e. daily or recurring life stress associated with financial, housing, workplace and interpersonal difficulties) that have been demonstrated to be important in the etiology of depression and substance use, may enhance our understanding of PTSD among women (Scott-Storey, 2011; Thoits, 2010; Turner, Wheaton, & Lloyd, 1995). One previous study on the correlates of incident violence among FSW revealed homelessness, inability to access drug treatment, and police encounters to be significant (Shannon et al., 2009).
Given the high burden of violence among FSW, the aims of this study were to characterize the dimensions of lifetime exposure to violence (i.e. type, lifetime patterns and perpetrators) and to examine the independent relationships between PTSD severity, revictimization across life stages and cumulative violence, both in the context of co-occurring chronic strain and substance use among urban street-based FSW.
Methods
Participants
Data for this cross-sectional analysis were drawn from the baseline visit of the Sex Workers and Police Promoting Health in Risky Environments (SAPPHIRE) study, a prospective cohort study of street-based FSW recruited through targeted sampling in Baltimore City, Maryland, USA (Allen et al., 2019; Sherman et al., 2019). Baseline data were collected in 2016 through 2017. Eligibility criteria were: not identifying as male/man; aged ≥ 15 years; sold or traded oral, vaginal or anal sex “for money or things like food, drugs or favors”; picked up clients on the street or at public places ≥ 3 times in the past 3 months, and willing to undergo HIV and sexually transmitted infection testing. The baseline visit consisted of a 50-minute computer assisted personal interview (CAPI) with a trained interviewer. At the end of the survey, the interviewer offered referrals to local health and social service organizations as appropriate. Respondents were compensated with a pre-paid $70 USD VISA gift card for completing the baseline visit. The study was approved by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board and holds a Certificate of Confidentiality.
Measures
i. PTSD symptoms
PTSD symptoms were measured using the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5), a 20-item self-reported scale that asks about symptoms in the past month, with responses for each symptom coded using a 5-point Likert scale (not at all, a little bit, moderately, quite a bit, extremely); overall score can range from 0 to 80 (Weathers et al., 2013). Total PCL-5 scores indicating “PTSD symptom severity” were computed. The mean, standard deviation (SD), median and interquartile range (IQR) were calculated. Internal consistency of the PCL-5 was high in this sample (Cronbach’s Alpha=0.96).
ii. Sexual and physical violence, revictimization and cumulative violence
A series of questions on lifetime sexual and physical violence experiences during childhood (<18 years) and adulthood (≥18 years) were asked. Violence items were adapted from the Revised Conflict Tactics Scale (Straus, Hamby, Boney-McCoy, & Sugarman, 1996), a widely used scale designed for capturing IPV that has been used in previous sex work research (Brantley, Kerrigan, German, Lim, & Sherman, 2017). Childhood sexual violence (CSV) was defined as ever being pressured or forced sexual intercourse or sexual touching. Childhood physical violence (CPV) was defined as ever being hit, punched, slapped or otherwise physically hurt by someone causing marks or injury. Respondents who had experienced violence during childhood were also asked to select their relation to the perpetrator(s) from a list of options. Those who selected the “other” option were asked to specify their relationship to the perpetrator.
Adulthood exposures to violence were measured separately for four types of perpetrators found to be most common in the literature (Decker et al., 2015; Deering et al., 2014): (1) intimate partners; (2) sex work clients; (3) police officers; and (4) pimps/managers (if applicable). Adult sexual violence (ASV) was defined as ever being physically forced to have sexual intercourse by a given type of perpetrator, and adult physical violence (APV) was defined as ever being hit, punched, slapped or otherwise physically hurt, or ever being threatened or hurt with a weapon, by a given type of perpetrator. We also created four variables for each category of violence indicating if two or more perpetrator types were selected.
A binary variable (“any lifetime violence”; yes/no) was constructed using responses to CSV, CPV, ASV and APV. Further, binary variables representing sexual and physical violence exposures by life stage were constructed (e.g. sexual violence during childhood only, sexual violence during adulthood only, sexual violence during childhood and adulthood; yes/no).
Sexual revictimization across life stages was defined as responding yes to CSV and ASV. Physical revictimization was defined comparably. Cumulative violence was constructed using the sum of the number of lifetime violence types (i.e. from CSV, CPV, ASV, APV), resulting in a possible range of 0 to 4; this variable was based on prior operationalizations of cumulative violence among FSW (Peitzmeier et al., 2019), female college students (Briere, Kaltman, & Green, 2008) and women (Follette, Polusny, Bechtle, & Naugle, 1996)
iii. Chronic strain
The survey included items on three types of chronic strain: homelessness (self-reported), financial insecurity (defined as having no monthly savings), and food insecurity (defined as going to sleep at night hungry due to not having enough food); we included any experience in the past 3 months. We also included currently having a criminal record for personal drug possession or engaging in sex work as an indicator of chronic strain. The number of chronic strain items endorsed was used to construct a cumulative strain score (0–4).
iv. Drug use
Other survey measures were developed from previous work (Brantley, Footer, Lim, Kerrigan, & Sherman, 2017; Brantley, Kerrigan, et al., 2017; Decker et al., 2017). Frequency of substance use in the past 12 months was measured using pre-defined drug type categories, which included daily as the most frequent use option. Binary (yes/no) variables for daily opioid use and daily cocaine use were constructed given high rates of drug use expected in this population based on prior work (Vanwesenbeeck, 2001) as well as the popularity of speedball use (concomitant use of heroin and cocaine) among drug-using women in Baltimore (Park, Weir, Allen, Chaulk, & Sherman, 2018). Opioids were defined as heroin use (injected/snorted/smoked) or misuse of “prescription pain killers such as Percocet, Morphine, OxyContin, Codeine, Fentanyl but not over the counter pills.” Cocaine included use of smoking crack cocaine or snorting/injecting powder cocaine.
v. Binge drinking
The Alcohol Use Disorders Identification Test (AUDIT-C) is a validated brief three-item screening scale developed by the World Health Organization for assessing alcohol disorders (Bush, Kivlahan, McDonell, Fihn, & Bradley, 1998). Scores range from 0 to 16. An “at least weekly binge drinking” binary variable was constructed from the item “How often did you have four or more drinks on one occasion in the past year?” by collapsing the daily and almost daily response options.
Data analysis
This analysis only included baseline data from FSW who were assigned as female at birth (i.e. cisgender women) in the SAPPHIRE cohort, and who completed the PCL-5 scale and violence measures (N=220). The dependent variable was PTSD severity (PCL-5 score), modeled as a continuous outcome. Age-adjusted linear regressions were used to model associations between PTSD severity and a range of covariates specified a priori (i.e., all four violence indicators, cumulative violence, chronic strain factors and substance use). Lowess plots were used to visually inspect the linearity of the relationships. Variance clustering was applied to account for recruitment zone. Linear combinations of the levels of cumulative violence were computed to test for statistically significant differences between each level.
Two multivariate linear regression models of PTSD severity were examined. The “revictimization across life stages model”, included all four types of violence as independent covariates as well as interaction terms for CSV × ASV, and CPV × APV. The “cumulative violence” model included the total number of lifetime violence types (ranging from 0 to 4) as a covariate, which was modeled categorically since the relationship was not linear during exploratory data analysis as expected. We tested several models by adding all possible combinations of the three chronic strain variables (homelessness, financial insecurity and food insecurity; and the total number), as well as substance use variables (opioid use, stimulant use, binge drinking). Models were age-adjusted and accounted for variance clustering for recruitment zone. The lowest value of the Akaike information criterion was used to select the final model. The distribution of PTSD severity was visualized using a violin plot, which overlays the Kernel density of the sample distribution over a traditional boxplot (vioplot package in Stata). All analyses were conducted in Stata/SE 14.2 (College Station, Texas).
Results
Demographics and drug use
The mean age of FSW (n=220) was 35.7 years (SD=8.9) with age ranging from 18–61 years. Women were mostly Non-Hispanic White (68.2%), with others being Non-Hispanic Black (21.8%), Hispanic (3.2%) or multiracial/other races (6.8%). Half of the sample (51%) did not complete high school, 89.1% were financially insecure, 74.1% were food insecure, and 61.8% were homeless. Daily drug use was common (opioids: 73.2%; stimulants: 63.2%; both: 50.9%), and 8.6% engaged in binge drinking more than once a week (data not shown).
Violence and PTSD symptoms
The baseline prevalence of lifetime violence was high at 81.8% (see Table 1 & Figure 1). The majority of FSW exhibited high levels of PTSD; 61.4% screened positive for PTSD symptoms (PCL-5≥33), mean PCL-5 score was 39 (SD=22), and the median PCL-5 was 41 (interquartile range [IQR]=21–57). Many women had been revictimized as a child and adult (sexually: 15.0%; physically: 37.7%). Perpetrators of CSV (Table 2) were almost exclusively male; many were family including their father/step-father (22.1%) or other male relatives (33.8%). One in five (19.2%) reported multiple perpetrator types. CPV was most commonly perpetrated by a father/step-father (49.5%), followed by a mother/step-mother (27.4%) or an intimate partner (26.3%), and 26.3% of the women had multiple perpetrators during childhood.
Table 1.
Prevalence of Violence and PTSD among Street-Based Female Sex Workers (n = 220) in Baltimore, Maryland
| Variable | n | % |
|---|---|---|
| Violence | ||
| Lifetime | 180 | 81.8 |
| Childhood sexual violence1 | 77 | 35.0 |
| Adulthood sexual violence2 | 87 | 39.6 |
| Sexual revictimization across life stages | 33 | 15.0 |
| Childhood physical violence3 | 94 | 42.7 |
| Adulthood physical violence4 | 159 | 72.3 |
| Physical revictimization across life stages | 83 | 37.7 |
| Lifetime number of violence types (0–4), Mean (SD) | 1.9 | (1.3) |
| PTSD | ||
| Screened positive (PCL-5≥33) | 135 | 61.4 |
| PCL-5 score, Mean (SD) | 38.7 | (21.9) |
Note. Denominators vary due to data missingness
Pressured or forced to have sexual contact including sexual touching or sexual intercourse before age of 18.
Forced to have sexual intercourse by clients, pimps/managers, intimate partners or police officers
Hit, punched, slapped or otherwise physically hurt before age of 18.
Hit, punched, slapped or otherwise physically hurt or threatened with a weapon by clients, pimps/managers, intimate partners or police officers
Figure 1.
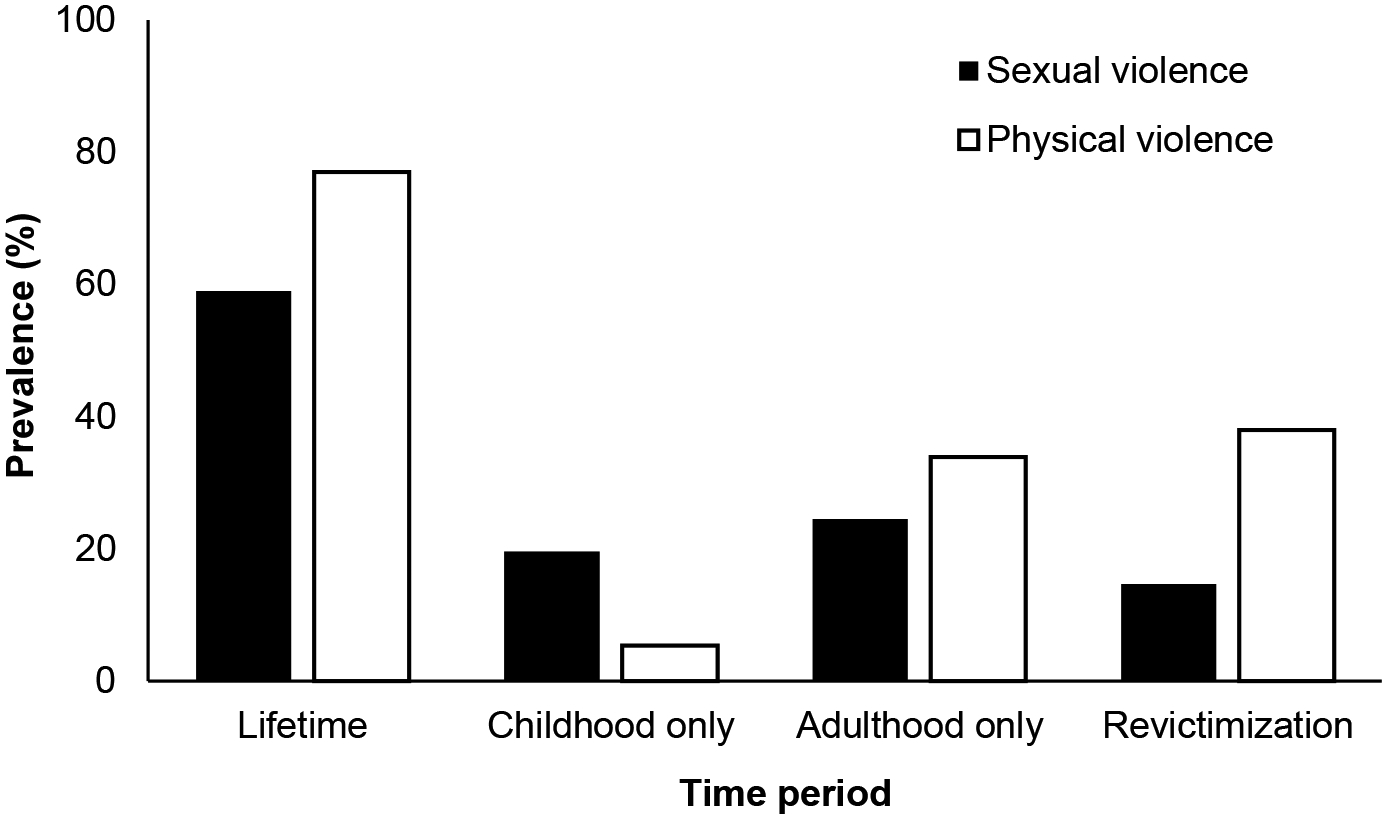
Lifetime Exposure to Sexual Violence, Physical Violence, and Revictimization across life stages among Street-Based Female Sex Workers (n = 220) in Baltimore, Maryland
Table 2.
Lifetime Perpetrators of Sexual and Physical Violence against Street-Based Female Sex Workers in Baltimore, Maryland
| Childhood sexual violence1 (n = 77) | Childhood physical violence2 (n = 97) | |||
|---|---|---|---|---|
| Variable | n | % | n | % |
| Family | ||||
| Father/step-father | 17 | 22.1 | 47 | 49.5 |
| Mother/step-mother | 0 | 0.0 | 26 | 27.4 |
| Sibling | 4 | 5.2 | 8 | 8.4 |
| Male relative | 26 | 33.8 | 9 | 9.5 |
| Female relative | 2 | 2.6 | 7 | 7.4 |
| Intimate partner | 7 | 9.1 | 25 | 26.3 |
| Client | 1 | 1.3 | 2 | 2.1 |
| Someone else | 18 | 23.4 | 10 | 10.5 |
| Don’t know | 8 | 10.4 | 0 | 0.0 |
| ≥2 perpetrator types reported^ | 14 | 19.2 | 25 | 26.3 |
| Adulthood sexual violence3,5 (n = 91) | Adulthood physical violence4,5 (n = 166) | |||
| Variable | n | % | n | % |
| Intimate partner | 39 | 42.9 | 113 | 69.3 |
| Client | 75 | 82.4 | 108 | 65.5 |
| Police officer | 10 | 11.0 | 59 | 35.5 |
| Pimps/manager | 1 | 1.1 | 2 | 1.2 |
| ≥2 perpetrator types reported^ | 30 | 33.0 | 90 | 54.2 |
Note. Multiple perpetrators could be reported
Pressured or forced to have sexual contact including sexual touching or sexual intercourse before age of 18.
Hit, punched, slapped or otherwise physically hurt before age of 18.
Forced to have sexual intercourse.
Hit, punched, slapped or otherwise physically hurt or threatened with a weapon.
The measure of adulthood violence did not include other types of perpetrators such as family or strangers.
denominator excludes those who refused to answer
A small proportion (7.7%) entered sex work as a victim of force, coercion, threats pressure or trickery, and one in five (21.4%) entered as a minor (age < 18). Most (65.0%) engaged in sex work daily and virtually all recent clients were male (99.1%). Clients (82.4%) and intimate partners (42.9%) perpetrated the vast majority of ASV (Table 2). The proportion of APV perpetrated by clients and intimate partners were similarly high (65.1% and 69.3% respectively) however police-perpetrated APV was also substantial (35.5%).
Age-adjusted associations
Results of age-adjusted linear regression models of the association between violence and PTSD severity were as follows: CSV (β=14.43, 95% CI: 9.56, 19.31), ASV (β=14.04, 95% CI: 5.02, 23.06), CPV (β=12.35, 95% CI: 0.26–24.44) and APV (β=11.02, 95% CI: 1.74–20.29) were all associated with PTSD severity when modeled separately (data not shown). Compared to no reported lifetime violence, exposure to one (β=6.02, 95% CI: 1.82, 10.21), two (β=16.96, 95% CI: 8.75, 25.16), three (β=18.32, 95% CI: 12.91, 23.73) or four (β=31.65, 95% CI: 24.48, 38.81) types of violence substantially increased PTSD severity; differences between two versus one (β=10.94, 95% CI: 3.68–18.21) and 4 versus 3 (13.33, 95% CI: 9.22–17.43) types were also significant (data not shown). Low education (β=-8.77, 95% CI: −14.7, −2.85) and food insecurity (β=6.73, 95% CI: 0.85, 12.62) were two chronic strain factors associated with PTSD severity at the p<0.05 level. Homelessness (β=5.62, 95% CI: −0.53, 11.78) and financial insecurity (β=7.03, 95% CI: −0.77, 14.84) were marginally associated (p<0.1). Having a criminal record (β=-0.16, 95% CI: −3.77, 3.44) and cumulative strain (β=0.84, 95% CI: −0.80–2.48) were not significantly associated with PTSD severity. Daily opioid use (β=2.05, 95% CI: −7.24, 11.34) and daily stimulant use (β=0.82, 95% CI: −4.4, 6.04) were not significantly associated with PTSD severity while daily/almost daily binge drinking (β=10.8, 95% CI: −2.02, 23.62) was marginally (p<0.1) associated.
Age-adjusted multivariate associations
No significant age-adjusted multivariate regression associations between revictimization across life stages and PTSD severity emerged (Table 3, Model A). Multivariate modeling revealed support for a cumulative violence model (Table 3, Model B). Compared to FSW with no lifetime exposure to violence, FSW with one (β=6.83, 95% CI: 2.63, 11.02), two (β=17.98, 95% CI: 9.81, 26.16), three (β=18.81, 95% CI: 12.52, 25.1), or four (β=31.89, 95% CI: 22.00, 41.79) violence types exhibited significantly higher PTSD severity. Binge drinking was also associated with PTSD severity in this model (β=13.04, 95% CI: 3.98, 22.09). Chronic strain factors were not significantly associated with PTSD severity in the presence of other covariates and subsequently removed from the final model. The dose-response relationship between cumulative violence and PTSD severity is depicted in Figure 2.
Table 3.
Multivariate Associations between PTSD Symptom Severity and Revictimization and Cumulative Violence among Street-Based Female Sex Workers (n = 220) in Baltimore, Maryland
| Median PCL-5 by violence indicator | Revictimization across life stages (Model A) | Cumulative violence (Model B) | ||
|---|---|---|---|---|
| Yes | No | β (95% CI) | β (95% CI) | |
| Childhood sexual violence | 48 | 32 | 11.33 (5.84, 16.82)** | |
| Adulthood sexual violence | 50 | 32 | 11.08 (1.10, 21.06)* | |
| Revict: Sexual × Sexual | 57 | 37 | 0.12 (-9.73, 9.96) | |
| Childhood physical violence | 46 | 36 | 9.30 (-0.51, 19.10) | |
| Adulthood physical violence | 44 | 27 | 7.10 (-1.71, 15.91) | |
| Revict: Physical × Physical | 47 | 36 | −7.94 (−20.76, 4.87) | |
| >Weekly binge drinking | 53 | 40 | 12.13 (3.18, 21.08)* | 13.04 (3.98, 22.09)* |
| Cumulative violence1 | ||||
| 0 | 21 | ref (1.0) | ||
| 1 | 25 | 6.83 (2.63, 11.02)** | ||
| 2 | 43 | 17.98 (9.81, 26.16)** | ||
| 3 | 44 | 18.81 (12.52, 25.1)*** | ||
| 4 | 61 | 31.89 (22.00, 41.79)*** | ||
Note. Age-adjusted multivariate linear regression with robust variance to account for clustering by recruitment zone. Revictimization model includes two interaction terms (sexual and physical revictimization).
lifetime number of violence types endorsed
p < .05.
p < .01.
p < .001.
Figure 2.
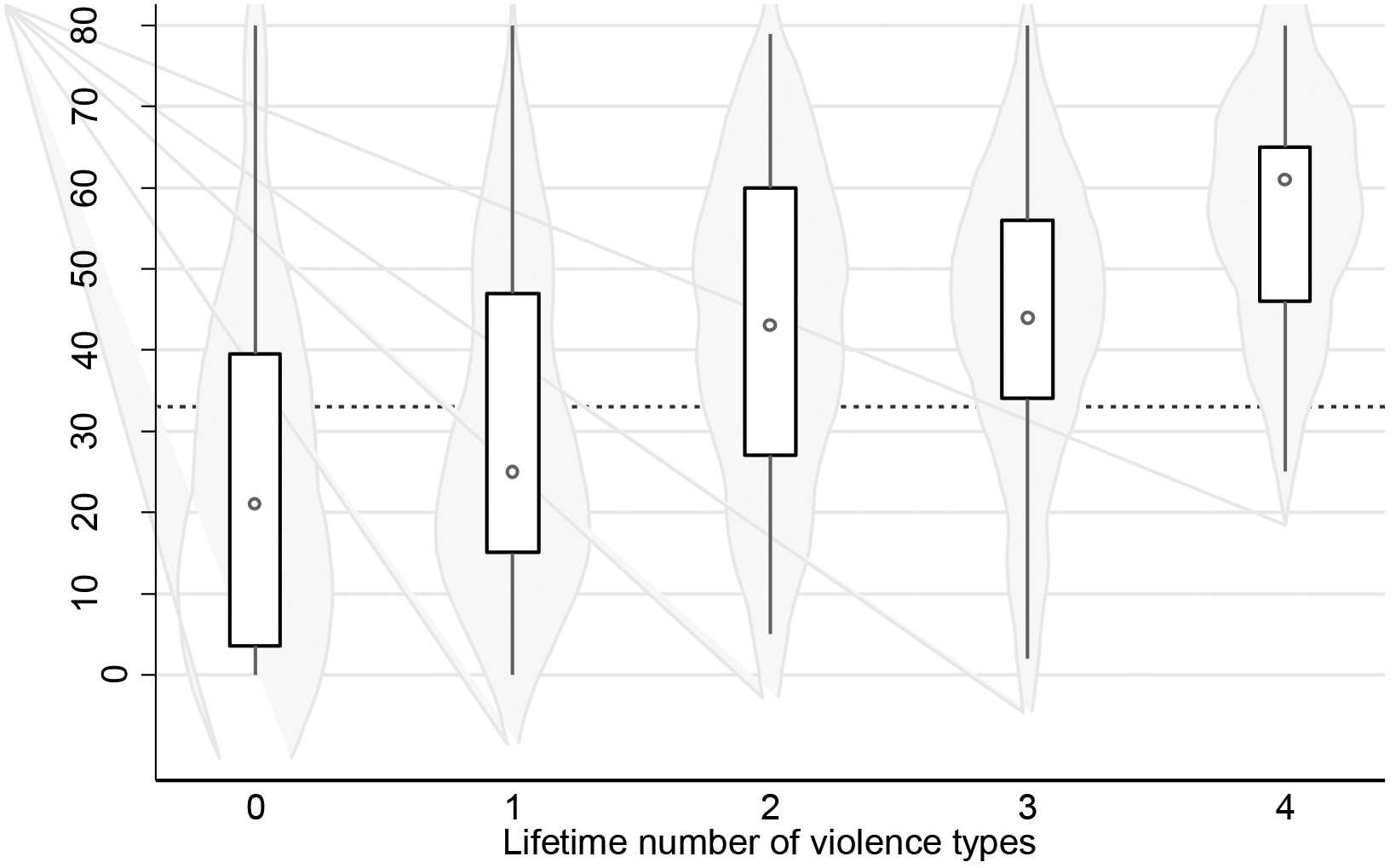
Violin Plot of the Dose-Response Relationship between Cumulative Violence and PTSD Symptom Severity among Street-Based Female Sex Workers (n = 220) in Baltimore, Maryland
Note. Dashed line indicates the cut-off score for a positive PTSD screen (≥33).
*p < .05. **p < .01. ***p < .001.
Discussion
Street-based FSW are one of the most marginalized and vulnerable groups among society, and a population disproportionately impacted by trauma. This study, which was conducted in an urban US setting, documented extremely high rates of sexual and physical violence and PTSD symptoms. The average PTSD score among these women was comparable to treatment-seeking war veterans (Wortmann et al., 2016). Multivariate analyses supported a cumulative violence model; the lifetime number of violence categories held a dose-response relationship with PTSD severity with the largest increases in severity observed between 1 to 2 types and 3 to 4 types of violence. Binge drinking was independently associated with higher PTSD severity whereas chronic strain indicators were not significantly associated in adjusted models. This study is one of the first to document the relationships between accumulated violence, substance use and PTSD severity among street-based FSW, a uniquely vulnerable population of women worldwide.
Violence and PTSD Severity
Levels of sexual and physical revictimization across life stages were exceedingly high at 15% and 38% respectively. Interestingly, lifetime revictimization did not hold significant associations with PTSD symptom severity, after adjusting for the independent effects of violence. While this may appear to contradict some findings in the revictimization literature, the revictimization measure used in this study notably differed from previous studies that define revictimization simply as repeated events rather than exposure over life stages, or do not restrict events solely to violent encounters (Scott-Storey, 2011; Walsh et al., 2012).
However, we observed a clear dose-response relationship between cumulative violence and PTSD symptom severity, which complements findings in other populations that a dose-response relationship exists with greater lifetime frequency of abuse (Scott-Storey, 2011). This was clearly indicated by the lower levels of PTSD symptoms among women in our study who had experienced none or one violence type (median PCL-5 scores: 21 and 25) compared to women who were exposed to 2, 3 or 4 categories of violence in their lifetime (median PCL-5 scores: 43, 44 and 61 respectively). The findings supported a cumulative violence model of the effects of interpersonal violence (Scott-Storey, 2011).
Sexual violence has been given more attention in the FSW literature with physical violence often combined into a global binary sexual/physical violence indicator during analysis (Scott-Storey, 2011; Surratt et al., 2005; Ulibarri et al., 2009). Our study highlights four considerations when understanding the impact of trauma among this vulnerable population: levels of sexual and physical violence among street-based FSW are likely high throughout the life course; the burden of interpersonal violence is not solely due to engagement in sex work; physical violence is a more common occurrence during both life stages; there are key differences in the types of perpetrators across life stage and violence type. These findings affirm to researchers as well as healthcare and other service providers who encounter FSW seeking services to screen for and respond to sexual and physical violence occurring in childhood and adulthood, both within and outside the context of sex work.
Substance Use
Almost all FSW in our study were daily substance users, which is a common reason for entering sex work among street-based FSW (Vanwesenbeeck, 2001). Compared to daily opioid or stimulant use, which affected the majority of FSW in our study, daily binge drinking was less prevalent, affecting one in ten FSW, but strongly associated with PTSD severity. Unlike other substance use disorders, alcohol use disorders are characterized by memory impairment, which may be a factor that could help explain this finding particularly among FSW who are using alcohol to “self-medicate” i.e., suppress trauma intrusion symptoms (American Psychiatric Association, 2013). Access to alcohol use disorder treatment among this small yet high-risk population are warranted (Ullman et al., 2013). While evidence shows that reductions in PTSD severity can be achieved with reductions in substance use frequency (Hien et al., 2009; Manhapra, Stefanovics, & Rosenheck, 2015), care must be taken when treating women who are actively using substances to cope with PTSD symptoms; alcohol or drug withdrawal may trigger PTSD and drug relapse (Jacobsen et al., 2001). By treating substance use disorder and PTSD concurrently, rather than consecutively, the two conditions can be managed safely and effectively (Roberts et al., 2015)
Chronic strain and the Sex Work Context
Sex work has been described as a high demand and low control occupation; these types of jobs are linked to chronic strain and poorer mental health outcomes (Spector, 2002; Wingood & DiClemente, 2000). Street-based sex work is particularly demanding and risky due to risks present in the work environment (e.g. violent and coercive behaviors of clients and police officers), which are shaped by broader social and structural forces (e.g. sex work criminalization and stigma). The health needs of street-based FSW are great, though resources that are tailored to meet the needs of this population are scarce due to socio-political factors, particularly in the U.S. context (Decker, Beyrer, & Sherman, 2014). Despite being a multi-billion-dollar industry, sex work is not recognized as a legal occupation in many countries including the U.S., except in some parts of Nevada. A negative consequence of criminalization policy environments is that FSW are often not afforded any legal protections, even when sexually or physically assaulted (Decker et al., 2015). Decriminalizing sex work will likely improve FSW access to care, protection and justice (Decker et al., 2015; UNAIDS, 2012).
Although the chronic strain variables (homelessness, financial insecurity and food insecurity) were not independently associated with PTSD severity, the high levels observed posed a challenge to modeling associations. Their role requires further research given their prominence and persistence in the lives of FSW. For example, food insecurity held a bivariate association with PTSD as observed previously (Hadley et al., 2008) and can be traumatic depending on severity (e.g. food deprivation could be used as a form of control).
Limitations
There are limitations to consider when interpreting these findings. PTSD severity has been linked to violence severity, frequency, perception of life threat during the assault, self-blame and delayed disclosure of the assault, which are important unmeasured factors (Brewin, Andrews, & Valentine, 2000; Ullman, Filipas, Townsend, & Starzynski, 2007). We observed relatively high residual PTSD in the “no violence” group; while violence exposures from the most common perpetrators established in the literature were measured (i.e., clients, police, pimps and intimate partners), there were other perpetrators of adult violence who were not included. Unmeasured confounding due to other forms of trauma (e.g. witnessing violence, car accidents) may have also confounded the associations with PTSD, though it is known that among all sources of trauma, sexual and physical violence results in the highest risk of PTSD (Breslau et al., 1998). The operationalization of cumulative violence using a summed score has its merits but does not account for severity, duration, and frequency of victimization within each time frame assessed, which are known to elevate the risk of PTSD (Scott-Storey, 2011). Given the high rates of substance use in this population, future studies should include a validated scale to measure drug use to examine the prevalence of substance use disorders among FSW. The data may be subject to social desirability bias. The cross-sectional nature of the study limits establishment of temporality of the relationships; longitudinal studies would certainly help to overcome this limitation and bolster the small body of literature on this topic.
Conclusions
This study is one of the first to examine the role of cumulative violence in the etiology of PTSD among FSW, a population with exceedingly high burden of violence throughout the life course and PTSD levels comparable to treatment-seeking military veterans. The broader social and structural context surrounding sex work and gender-based violence remain major barriers to delivering appropriate healthcare, safety and justice. Trauma-informed mental health interventions and violence prevention strategies that are non-stigmatizing and tailored to the needs of FSW (e.g., that account for non-traditional work hours and respect their agency) are urgently required (World Health Organization, 2013a). Substance use is a major issue among this population that need to be addressed concurrently. Active engagement of current and former FSW in these responses will be critical in shaping these interventions.
Acknowledgments
We thank the sex workers who participated in the study. We are grateful to the SAPPHIRE field team, especially to Steve Huettner, Sean Allen, Brad Silberzahn, Eddie Poole, Orline Johnson, Jackie Toppins, Suzanne Lebovit, Miles Morris and Katelyn Riegger for their contributions to data collection.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the National Institute on Drug Abuse (R01DA038499). Additional support for this work was provided by the Johns Hopkins University Center for AIDS Research (1P30AI094189). JNP was partially supported by the Charlotte Silverman Award. The content is solely the responsibility of the authors and does not necessarily reflect the official views of the National Institutes of Health.
Author Biographies
Ju Nyeong Park, PhD, MHS, is an assistant scientist in the Bloomberg School of Public Health at Johns Hopkins University. Her research focuses on trauma, substance use, and infectious disease among marginalized populations, including female sex workers and people who inject drugs. She actively works on developing and evaluating interventions to improve health outcomes in clinical and community-based settings.
Michele R. Decker, ScD, MPH, is an associate professor in the Bloomberg School of Public Health at Johns Hopkins University. Her research focuses on the social determinants of women’s health and gender equity with an emphasis on gender-based violence (e.g., sexual assault, intimate partner violence, sex trafficking), its prevention, and its implications for sexual and reproductive health (e.g., sexually transmitted infections, HIV, and unintended pregnancy).
Judith K. Bass, PhD, MPH, MIA, is an associate professor in the Bloomberg School of Public Health at Johns Hopkins University. Her major area of interest is designing and evaluating methods for assessing mental health and mental illness in non-Western cultures with the intention for using these assessments to investigate the effectiveness of innovative prevention and intervention strategies.
Noya Galai, PhD, is an associate professor in the Bloomberg School of Public Health at Johns Hopkins University and a biostatistician with extensive experience in the design and analysis of epidemiological studies and intervention evaluation among key populations.
Catherine Tomko, MHS, is a doctoral candidate in the Bloomberg School of Public Health at Johns Hopkins University. Her research focuses on examining social and structural factors in health access and mental health disparities among marginalized women populations, including female sex workers and women who use drugs.
Kriti M. Jain, MSPH, PhD (at the time of writing), was a doctoral candidate at the Bloomberg School of Public Health at Johns Hopkins University. Her dissertation research focused on the intersection of HIV and posttraumatic stress disorder (PTSD). She is the lead author of Improving Access to HIV Care: Lessons Learned From Five U.S. Sites (JHU Press, 2016).
Katherine H.A. Footer, LLB, MSc, is an assistant scientist in the Bloomberg School of Public Health at Johns Hopkins University, and Barrister at Law in England and Wales. Her research focus is on the intersection of public health, human rights, and social justice with a specific focus on key populations.
Susan G. Sherman, PhD, MPH, is a professor in the Bloomberg School of Public Health at Johns Hopkins University who focuses on improving the health of marginalized populations. She is interested in the structural drivers of health and risk and has worked for almost two decades on developing and evaluating HIV, substance use, and microenterprise interventions in Baltimore, Pakistan, Thailand, and India.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Allen ST, Footer KH, Galai N, Park JN, Silberzahn B, & Sherman SG (2019). Implementing targeted sampling: lessons learned from recruiting female sex workers in Baltimore, MD. Journal of Urban Health, 96(3), 442–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (DSM-5®): American Psychiatric Pub. [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, … Stevens MR (2011). The national intimate partner and sexual violence survey (NISVS): 2010 summary report. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, 25. [Google Scholar]
- Brantley ML, Footer KHA, Lim S, Kerrigan D, & Sherman SG (2017). Experiences of structural vulnerability among exotic dancers in Baltimore, Maryland: Co-occurring social and economic antecedents of HIV/STI risk. Int J Drug Policy, 50, 74–81. doi: 10.1016/j.drugpo.2017.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brantley ML, Kerrigan D, German D, Lim S, & Sherman SG (2017). Identifying Patterns of Social and Economic Hardship Among Structurally Vulnerable Women: A Latent Class Analysis of HIV/STI Risk. AIDS Behav, 21(10), 3047–3056. doi: 10.1007/s10461-017-1673-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N (2002). Epidemiologic studies of trauma, posttraumatic stress disorder, and other psychiatric disorders. In: SAGE Publications Sage CA: Los Angeles, CA. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, & Andreski P (1998). Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Archives of general psychiatry, 55(7), 626–632. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, & Valentine JD (2000). Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol, 68(5), 748–766. [DOI] [PubMed] [Google Scholar]
- Briere J, Kaltman S, & Green BL (2008). Accumulated childhood trauma and symptom complexity. J Trauma Stress, 21(2), 223–226. doi: 10.1002/jts.20317 [DOI] [PubMed] [Google Scholar]
- Bush K, Kivlahan DR, McDonell MB, Fihn SD, & Bradley KA (1998). The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Archives of internal medicine, 158(16), 1789–1795. [DOI] [PubMed] [Google Scholar]
- Connell R, & Pearse R (2014). Gender: In World Perspective. (3rd edition ed.): Polity. [Google Scholar]
- Decker MR, Beyrer C, & Sherman SG (2014). Ending the invisibility of sex workers in the US HIV/AIDS surveillance and prevention strategy. AIDS, 28(15), 2325–2327. doi: 10.1097/QAD.000000000000041100002030-201409240-00018 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker MR, Crago AL, Chu SK, Sherman SG, Seshu MS, Buthelezi K, … Beyrer C (2015). Human rights violations against sex workers: burden and effect on HIV. Lancet, 385(9963), 186–199. doi: 10.1016/S0140-6736(14)60800-XS0140-6736(14)60800-X [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker MR, Nail JE, Lim S, Footer K, Davis W, & Sherman SG (2017). Client and Partner Violence Among Urban Female Exotic Dancers and Intentions for Seeking Support and Justice. J Urban Health, 94(5), 637–647. doi: 10.1007/s11524-017-0195-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deering KN, Amin A, Shoveller J, Nesbitt A, Garcia-Moreno C, Duff P, … Shannon K (2014). A systematic review of the correlates of violence against sex workers. Am J Public Health, 104(5), e42–54. doi: 10.2105/AJPH.2014.301909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erausquin JT, Reed E, & Blankenship KM (2011). Police-related experiences and HIV risk among female sex workers in Andhra Pradesh, India. J Infect Dis, 204 Suppl 5, S1223–1228. doi: 10.1093/infdis/jir539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farley M, Cotton A, Lynne J, Zumbeck S, Spiwak F, Reyes ME, … Sezgin U (2004). Prostitution and trafficking in nine countries: An update on violence and posttraumatic stress disorder. Journal of Trauma Practice, 2(3–4), 33–74. [Google Scholar]
- Finkelhor D, Ormrod RK, & Turner HA (2007). Polyvictimization and trauma in a national longitudinal cohort. Development and psychopathology, 19(1), 149–166. [DOI] [PubMed] [Google Scholar]
- Follette VM, Polusny MA, Bechtle AE, & Naugle AE (1996). Cumulative trauma: the impact of child sexual abuse, adult sexual assault, and spouse abuse. J Trauma Stress, 9(1), 25–35. [DOI] [PubMed] [Google Scholar]
- Footer KHA, Park JN, Allen ST, Decker MR, Silberzahn B, Huettner S, … Sherman SG (2019). Police related correlates of client violence among female sex workers in Baltimore City, Maryland, USA. American Journal of Public Health, 109(2), 289–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadley C, Tegegn A, Tessema F, Cowan JA, Asefa M, & Galea S (2008). Food insecurity, stressful life events and symptoms of anxiety and depression in east Africa: evidence from the Gilgel Gibe growth and development study. Journal of Epidemiology & Community Health, 62(11), 980–986. [DOI] [PubMed] [Google Scholar]
- Heise L, & Kotsadam A (2015). Cross-national and multilevel correlates of partner violence: an analysis of data from population-based surveys. The Lancet Global Health, 3(6), e332–e340. [DOI] [PubMed] [Google Scholar]
- Hien DA, Jiang H, Campbell AN, Hu M-C, Miele GM, Cohen LR, … Robinson J (2009). Do treatment improvements in PTSD severity affect substance use outcomes? A secondary analysis from a randomized clinical trial in NIDA’s Clinical Trials Network. American Journal of Psychiatry, 167(1), 95–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobsen LK, Southwick SM, & Kosten TR (2001). Substance use disorders in patients with posttraumatic stress disorder: a review of the literature. American Journal of Psychiatry, 158(8), 1184–1190. [DOI] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. (2012). UNAIDS Guidance Note on HIV and Sex Work. Retrieved from Geneva, Switzerland:
- Kessler RC, Sonnega A, Bromet E, Hughes M, & Nelson CB (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Archives of general psychiatry, 52(12), 1048–1060. [DOI] [PubMed] [Google Scholar]
- Kilpatrick DG, Acierno R, Resnick HS, Saunders BE, & Best CL (1997). A 2-year longitudinal analysis of the relationships between violent assault and substance use in women. Journal of consulting and clinical psychology, 65(5), 834. [DOI] [PubMed] [Google Scholar]
- Krause ED, Kaltman S, Goodman LA, & Dutton MA (2008). Avoidant coping and PTSD symptoms related to domestic violence exposure: A longitudinal study. Journal of Traumatic Stress, 21(1), 83–90. [DOI] [PubMed] [Google Scholar]
- Lim S, Peitzmeier S, Cange C, Papworth E, LeBreton M, Tamoufe U, … Njindam I (2015). Violence against female sex workers in Cameroon: accounts of violence, harm reduction, and potential solutions. JAIDS Journal of Acquired Immune Deficiency Syndromes, 68, S241–S247. [DOI] [PubMed] [Google Scholar]
- Manhapra A, Stefanovics E, & Rosenheck R (2015). Treatment outcomes for veterans with PTSD and substance use: Impact of specific substances and achievement of abstinence. Drug & Alcohol Dependence, 156, 70–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris MD, Lemus H, Wagner KD, Martinez G, Lozada R, Gomez RM, & Strathdee SA (2013). Factors associated with pathways toward concurrent sex work and injection drug use among female sex workers who inject drugs in northern Mexico. Addiction, 108(1), 161–170. doi: 10.1111/j.1360-0443.2012.04016.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olff M, Langeland W, Draijer N, & Gersons BP (2007). Gender differences in posttraumatic stress disorder. Psychological bulletin, 133(2), 183. [DOI] [PubMed] [Google Scholar]
- Park JN, Weir BW, Allen ST, Chaulk P, & Sherman SG (2018). Fentanyl-contaminated drugs and non-fatal overdose among people who inject drugs in Baltimore, MD. Harm Reduct J, 15(1), 34. doi: 10.1186/s12954-018-0240-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peitzmeier SM, Wirtz AL, Beyrer C, Peryshkina A, Sherman SG, Colantuoni E, & Decker MR (2019). Polyvictimization Among Russian Sex Workers: Intimate Partner, Police, and Pimp Violence Cluster With Client Violence. J Interpers Violence, 886260519839431. doi: 10.1177/0886260519839431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes T, Simic M, Baros S, Platt L, & Zikic B (2008). Police violence and sexual risk among female and transvestite sex workers in Serbia: qualitative study. BMJ, 337, a811. doi: 10.1136/bmj.a811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts NP, Roberts PA, Jones N, & Bisson JI (2015). Psychological interventions for post-traumatic stress disorder and comorbid substance use disorder: A systematic review and meta-analysis. Clinical psychology review, 38, 25–38. [DOI] [PubMed] [Google Scholar]
- Romero-Daza N, Weeks M, & Singer M (2003). “ Nobody gives a damn if I live or die”: violence, drugs, and street-level prostitution in inner-city Hartford, Connecticut. Medical anthropology, 22(3), 233–259. [DOI] [PubMed] [Google Scholar]
- Roxburgh A, Degenhardt L, & Copeland J (2006). Posttraumatic stress disorder among female street-based sex workers in the greater Sydney area, Australia. BMC Psychiatry, 6, 24. doi:1471–244X-6–24 [pii] 10.1186/1471-244X-6-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott-Storey K (2011). Cumulative abuse: do things add up? An evaluation of the conceptualization, operationalization, and methodological approaches in the study of the phenomenon of cumulative abuse. Trauma, Violence, & Abuse, 12(3), 135–150. [DOI] [PubMed] [Google Scholar]
- Shannon K, Kerr T, Strathdee SA, Shoveller J, Montaner JS, & Tyndall MW (2009). Prevalence and structural correlates of gender based violence among a prospective cohort of female sex workers. BMJ, 339, b2939. doi: 10.1136/bmj.b2939bmj.b2939 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman SG, Park JN, Galai N, Allen ST, Huettner SS, Silberzahn BE, … & Footer KH (2019). Drivers of HIV Infection Among Cisgender and Transgender Female Sex Worker Populations in Baltimore City: Results From the SAPPHIRE Study. JAIDS Journal of Acquired Immune Deficiency Syndromes, 80(5), 513–521. [DOI] [PubMed] [Google Scholar]
- Spector PE (2002). Employee control and occupational stress. Current Directions in Psychological Science, 11(4), 133–136. [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, & Sugarman DB (1996). The revised conflict tactics scales (CTS2) development and preliminary psychometric data. Journal of family issues, 17(3), 283–316. [Google Scholar]
- Surratt HL, Kurtz SP, Weaver JC, & Inciardi JA (2005). The Connections of Mental Health Problems, Violent Life Experiences, and the Social Milieu of the “Stroll” with the HIV Risk Behaviors of Female Street Sex Workers. Journal of Psychology & Human Sexuality, 17(1–2), 23–44. doi: 10.1300/J056v17n01_03 [DOI] [Google Scholar]
- Thoits PA (2010). Stress and health: Major findings and policy implications. Journal of health and social behavior, 51(1_suppl), S41–S53. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Wheaton B, & Lloyd DA (1995). The epidemiology of social stress. American sociological review, 104–125. [Google Scholar]
- Ulibarri MD, Semple SJ, Rao S, Strathdee SA, Fraga-Vallejo MA, Bucardo J, … Patterson TL (2009). History of abuse and psychological distress symptoms among female sex workers in two Mexico-U.S. border cities. Violence Vict, 24(3), 399–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ullman SE, Filipas HH, Townsend SM, & Starzynski LL (2007). Psychosocial correlates of PTSD symptom severity in sexual assault survivors. Journal of Traumatic Stress, 20(5), 821–831. [DOI] [PubMed] [Google Scholar]
- Ullman SE, Relyea M, Peter-Hagene L, & Vasquez AL (2013). Trauma histories, substance use coping, PTSD, and problem substance use among sexual assault victims. Addictive behaviors, 38(6), 2219–2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanwesenbeeck I (2001). Another decade of social scientific work on sex work: a review of research 1990–2000. Annu Rev Sex Res, 12, 242–289. [PubMed] [Google Scholar]
- Walsh K, Danielson CK, McCauley JL, Saunders BE, Kilpatrick DG, & Resnick HS (2012). National prevalence of posttraumatic stress disorder among sexually revictimized adolescent, college, and adult household-residing women. Arch Gen Psychiatry, 69(9), 935–942. doi: 10.1001/archgenpsychiatry.2012.132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). Retrieved from doi:Scale available from the National Center for PTSD at www.ptsd.va.gov.
- Wingood GM, & DiClemente RJ (2000). Application of the theory of gender and power to examine HIV-related exposures, risk factors, and effective interventions for women. Health education & behavior, 27(5), 539–565. [DOI] [PubMed] [Google Scholar]
- Wirtz AL, Schwartz S, Ketende S, Anato S, Nadedjo FD, Ouedraogo HG, … Papworth E (2015). Sexual violence, condom negotiation, and condom use in the context of sex work: results from two West African countries. JAIDS Journal of Acquired Immune Deficiency Syndromes, 68, S171–S179. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2013a). Addressing violence against sex workers. Implementing comprehensive HIV/STI programmes with sex workers: Practical approaches from collaborative interventions, 19–39. [Google Scholar]
- World Health Organization. (2013b). Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence: World Health Organization. [Google Scholar]
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, … Litz BT (2016). Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychol Assess, 28(11), 1392–1403. doi: 10.1037/pas0000260 [DOI] [PubMed] [Google Scholar]


