The coronavirus disease 2019 (COVID-19) pandemic has resulted in large-scale social distancing, working from home, prohibiting large group gatherings,1 and staying at home.2 These public health measures have been shown to be effective in the influenza pandemic of 19183 and continue to hold a place in today’s scenario. Social distancing requires one to maintain a distance of at least 2 m or 6 feet between individuals in public spaces4 whereas stay at home orders require an individual to remain confined to one’s home with the provision to leave for essential errands (ie, groceries, medicine, and health care).2 Although these measures are necessary to curb the widespread transmission of respiratory infection disease, their implementation makes the delivery of traditional, centre-based cardiac rehabilitation (CBCR; ie, face-to-face, 12 weeks, 36 sessions) virtually impossible, because CBCR services have been suspended because of their nonessential designation during the COVID-19 pandemic. Essentially, because of the COVID-19 pandemic, the participation rate has decreased to virtually 0%. Before the COVID-19 outbreak, CBCR participation in many jurisdictions, including Canada and the United States was already a long-standing concern, with less than a quarter of eligible American patients participating in traditional cardiac rehabilitation (CR).5 Although many factors are associated with these sobering participation rates, limited access to CBCR is a prominent contributor within the United States and other countries.6 To increase participation, key CR stakeholders (eg, physicians, allied health professionals, scientists, professional organizations, etc) have been calling for alternate delivery models to increase access and participation. These trends and limitations in accepted alternate delivery models are issues around the world.7 For example, a global survey showed that the most frequent methods of reimbursement for CR included: government coverage, paying out of pocket, private insurance companies, and shared methods (ie, between patient and another source), with a portion of the respondents indicating coverage for abbreviated CR services.7 Considering the unprecedented closure of CBCR programs because of the COVID-19 pandemic, the need for covered alternative CR delivery models has never been more important.8 , 9
A recent global survey showed that most countries have the capacity to implement alternate models of CR. Among all of the countries offering CR (N = 85), all offered CBCR and 51 offered some alternative model (ie, home- or community-based CR).10 Across the world, different forms of communication (ie, paper, telephone/mobile, smartphone apps, e-mail, text message, Internet Web pages, webcams, and direct contact) have been used with varying frequencies (see Supplemental Figs. S1-S6, elsewhere10). These methods have been widely used in the delivery of home-based CR (HBCR), but do require the attention and time of service providers to deliver education, counselling, and monitoring. During the current COVID-19 crisis, CBCR practitioners are being called in to help care for patients affected by this pandemic, and CR programs need to operate in a mindful and efficient manner with limited utilization of manpower. This need to limit manpower and abide by shelter in place and social distancing guidelines highlights the need to upscale effective digital health and telerehabilitation models.
The implementation of HBCR options has served as an invaluable resource for delivering CR to patients facing various barriers that prevent participation in a traditional CBCR program. Evidence suggests that the cost effectiveness of the delivery of CR through telerehabilitation is similar to a centre-based program.11 The simple implementation of regular telephone calls to interact with an existing member of a CR program has been successfully used in home-based exercise studies in patients with cardiovascular disease (CVD), including heart failure and pulmonary hypertension.12 , 13 Additionally, the creation of social support groups via social media could lead to successful delivery of HBCR by allowing engagement among peers and health care professionals and promoting healthy behaviours.14 It is important to note that the typical HBCR exercise prescription of ≥ 30 minutes of moderate-intensity exercise, 3-5 sessions per week8 will have to be modified during strict stay at home orders for individuals without exercise equipment (ie, treadmill, stationary bike) who relied on walking/running outside. Instead, other forms of physical activity, such as calisthenics, chair-based exercises, and resistance and balance exercises should be explored. Furthermore, the use of yoga in CR could hold potential for use among individuals with CVD to further expand the scope of CR,15 provided adequate training is provided before initiation.16 Accordingly, for those already in a CR program, HBCR would be a viable option during the COVID-19 pandemic.17 If CR program administrators are able to take measures to implement and master the delivery of HBCR during this time, it is conceivable that CR participation rates might increase when facilities progress to resuming normal CBCR operations by having the option to integrate HBCR within CBCR. The need for implementing the core components of HBCR still requires patient assessment—which poses a challenge to new recruits into CR that requires additional refinement before broad clinical implementation. Specifically, the inclusion of new patients into CR will be challenging with respect to assessments, goal-setting, and prescriptions as per current guidelines8 considering the need for social distancing. Therefore, keeping in mind the continuous evolution of CR to “rebrand and reinvigorate,”18 we hereby propose “technology-driven CR” (TDCR) as a potential model of delivery.
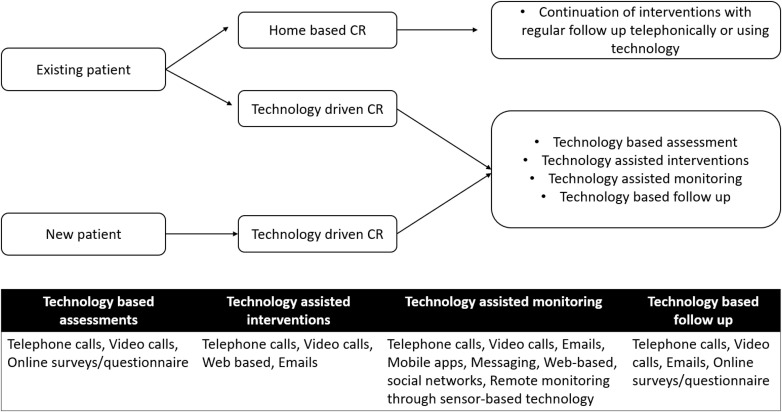
We propose that TDCR is a nonsupervised delivery of CR with the assistance of any form of technology, including but not limited to smartphones, mobile apps, Internet, messaging, e-mail, Web sites, webcams, and use of wearable sensors. Technology-based CR has been shown to be beneficial related to reduction of risk factors, while also cost effective.9 Irrespective of the technology used, TDCR should ensure that appropriate precautions are taken in light of COVID-19 risks, while performing any type of physical activity or exercise.19 A proposed model for the use of TDCR is given in Figure 1 .
Figure 1.
Model for technology-driven cardiac rehabilitation (CR).
At this time, the transition from traditional models of CR to TDCR is not only challenging but daunting. The utilization of resources required for establishing various network and virtual connections with individuals currently enrolled and for new cases requires the development of new standard operating procedures. These newer models will be even more challenging in resource-limited settings, especially because the delivery of CR is still not sufficient across many low- and middle-income countries.20 , 21 Limited availability of stable and powerful internet and telephone signals might continue to hamper delivery of TDCR in rural areas. Nevertheless, in the current pandemic, all of these options should be explored to ensure that delivery of CR is sustained and patients with CVD can continue to gain the associated benefits,22 , 23 and potentially get better traction, not just for coronary heart disease but also for eligible patients with heart failure and peripheral arterial disease. Furthermore, the use of TDCR might increase accessibility to CR in jurisdictions where services have been challenging to provide.24 This might be another case in which creative solutions to a temporary problem provide long-term unanticipated benefits for long-standing challenges.
Funding Sources
The authors have no funding sources to declare.
Disclosures
The authors have no conflicts of interest to disclose.
Footnotes
See page 793 for disclosure information.
References
- 1.Hartley DM, Reisinger HS, Perencevich EN. When infection prevention enters the temple: intergenerational social distancing and COVID-19 [e-pub ahead of print]. Infect Control Hosp Epidemiol doi:10.1017/ice.2020.100. Accessed April 1, 2020. [DOI] [PMC free article] [PubMed]
- 2.Schwiegershausen E. Shelter-in-Place and Stay-at-Home Orders: What They Mean. https://www.thecut.com/article/what-does-shelter-in-place-mean.html Available at: Accessed April 6, 2020.
- 3.Hatchett R.J., Mecher C.E., Lipsitch M. Public health interventions and epidemic intensity during the 1918 influenza pandemic. Proc Natl Acad Sci U S A. 2007;104:7582–7587. doi: 10.1073/pnas.0610941104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization Coronavirus Disease (COVID-19) Advice for the Public. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public Available at: Accessed April 7, 2020.
- 5.Ritchey M.D., Maresh S., McNeely J. Tracking cardiac rehabilitation participation and completion among medicare beneficiaries to inform the efforts of a national initiative. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.119.005902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ades P.A., Keteyian S.J., Wright J.S. Increasing cardiac rehabilitation participation from 20% to 70%: a road map from the Million Hearts Cardiac Rehabilitation Collaborative. Mayo Clin Proc. 2017;92:234–242. doi: 10.1016/j.mayocp.2016.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Babu A.S., Lopez-Jimenez F., Thomas R.J. Advocacy for outpatient cardiac rehabilitation globally. BMC Health Serv Res. 2016;16:471. doi: 10.1186/s12913-016-1658-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thomas R.J., Beatty A.L., Beckie T.M. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation. 2019;140:e69–89. doi: 10.1161/CIR.0000000000000663. [DOI] [PubMed] [Google Scholar]
- 9.Clark R.A., Conway A., Poulsen V. Alternative models of cardiac rehabilitation: a systematic review. Eur J Prev Cardiol. 2015;22:35–74. doi: 10.1177/2047487313501093. [DOI] [PubMed] [Google Scholar]
- 10.Lima de Melo Ghisi G., Pesah E., Turk-Adawi K. Cardiac rehabilitation models around the globe. J Clin Med. 2018;7:260. doi: 10.3390/jcm7090260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hwang R., Morris N.R., Mandrusiak A. Cost-utility analysis of home-based telerehabilitation compared with centre-based rehabilitation in patients with heart failure. Heart Lung Circ. 2019;28:1795–1803. doi: 10.1016/j.hlc.2018.11.010. [DOI] [PubMed] [Google Scholar]
- 12.O’Connor C.M., Whellan D.J., Lee K.L. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301:1439–1450. doi: 10.1001/jama.2009.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Babu A.S., Padmakumar R., Nayak K. Effects of home-based exercise training on functional outcomes and quality of life in patients with pulmonary hypertension: a randomized clinical trial. Indian Heart J. 2019;71:161–165. doi: 10.1016/j.ihj.2019.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Beatty A.L., Fukuoka Y., Whooley M.A. Using mobile technology for cardiac rehabilitation: a review and framework for development and evaluation. J Am Heart Assoc. 2013;2 doi: 10.1161/JAHA.113.000568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lavie C.J., Pack Q.R., Levine G.N. Expanding traditional cardiac rehabilitation in the 21st century. J Am Coll Cardiol. 2020;75:1562–1564. doi: 10.1016/j.jacc.2020.02.038. [DOI] [PubMed] [Google Scholar]
- 16.Prabhakaran D., Chandrasekaran A.M., Singh K. Yoga-based cardiac rehabilitation after acute myocardial infarction: a randomized trial. J Am Coll Cardiol. 2020;75:1551–1561. doi: 10.1016/j.jacc.2020.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yeo TJ, Wang YL, Low TT. Have a heart during the COVID-19 crisis: making the case for cardiac rehabilitation in the face of an ongoing pandemic [e-pub ahead of print]. Eur J Prev Cardiol doi:10.1177/2047487320915665. Accessed April 6, 2020. [DOI] [PMC free article] [PubMed]
- 18.Sandesara P.B., Lambert C.T., Gordon N.F. Cardiac rehabilitation and risk reduction: time to “rebrand and reinvigorate”. J Am Coll Cardiol. 2015;65:389–395. doi: 10.1016/j.jacc.2014.10.059. [DOI] [PubMed] [Google Scholar]
- 19.Chen P., Mao L., Nassis G.P. Coronavirus disease (COVID-19): the need to maintain regular physical activity while taking precautions. J Sport Health Sci. 2020;9:103–104. doi: 10.1016/j.jshs.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pesah E., Turk-Adawi K., Supervia M. Cardiac rehabilitation delivery in low/middle-income countries. Heart. 2019;105:1806–1812. doi: 10.1136/heartjnl-2018-314486. [DOI] [PubMed] [Google Scholar]
- 21.Babu A.S., Turk-Adawi K., Supervia M. Cardiac rehabilitation in India: results from the International Council of Cardiovascular Prevention and Rehabilitation’s Global Audit of Cardiac Rehabilitation. Global Heart. 2020;15:28. doi: 10.5334/gh.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kachur S., Lavie C.J., Morera R., Ozemek C., Milani R.V. Exercise training and cardiac rehabilitation in cardiovascular disease. Expert Rev Cardiovasc Ther. 2019;17:585–596. doi: 10.1080/14779072.2019.1651198. [DOI] [PubMed] [Google Scholar]
- 23.Jimenez-Pavon D, Carbonell-Baeza A, Lavie CJ. Physical exercise as therapy to fight against the mental and physical consequences of COVID-19 quarantine: special focus in older people [e-pub ahead of print]. Prog Cardiovasc Dis doi:10.1016/j.pcad.2020.03.009. Accessed April 6, 2020 [DOI] [PMC free article] [PubMed]
- 24.Tran M., Pesah E., Turk-Adawi K. Cardiac rehabilitation availability and delivery in Canada: how does it compare with other high-income countries? Can J Cardiol. 2018;34:S252–S262. doi: 10.1016/j.cjca.2018.07.413. [DOI] [PubMed] [Google Scholar]