Abstract
On February 19, 2020, the first case of a patient infected with Coronavirus Disease-2019 (COVID-19) was announced in Iran. The number of infected patients increased rapidly, and all health care centers faced an extremely challenging situation in Iran. The centers had to adopt new regulations and approaches to keep their patients and staff safe while providing service to society. Patients diagnosed with a malignancy are at a higher risk for infection with COVID-19 with a poorer prognosis. The Pardis Noor Radiology-Oncology center is a private center in Tehran composed of different departments, including radiation therapy and chemotherapy. Soon after the outbreak, we changed our rules and regulations for patients and staff. This is a report from a private radiology-oncology center in Tehran during the COVID-19 outbreak.
Introduction
On February 19, 2020, the Ministry of Health of Iran1,2 announced the first case of a patient infected with Coronavirus Disease-2019 (COVID-19). On March 11, the World Health Organization declared COVID-19 a pandemic and public health emergency. The number of infected patients increased dramatically in Iran and throughout the world.
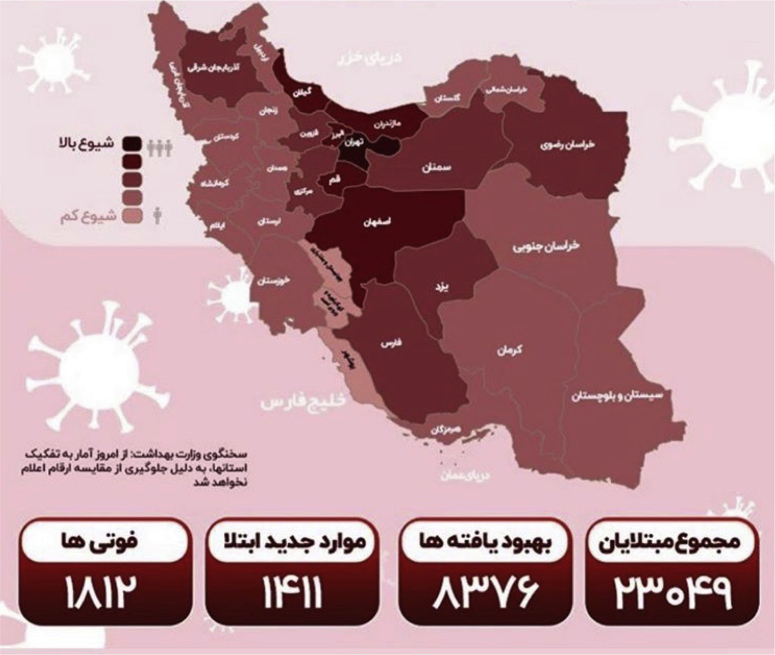
The infection chain rapidly progressed through almost all provinces of Iran.1,2 The most affected provinces were Gilan (northern province along the Caspian Sea), Tehran, and Qom. During the first month of the outbreak, there were 18,407 confirmed cases, 1284 mortalities, and >5979 recovered cases in Iran.1 Schools and universities were ordered closed soon after the detection of the first cases in Qom,1 and major restrictions for intercity trips were put in place. As of March 23, a total of 23,049 infected patients, 1812 deaths, and 8376 patients who recovered from COVID-19 infection have been recorded in Iran (Fig 1).1
Figure 1.
Total Coronavirus infections (23,049) in Iran as of March 23, 2020 (deaths = 1812, recovered = 8376). Printed with permission from https://behdasht.gov.ir/.
In this challenging time, all health care centers in Iran face an emergency. Tehran is the capital of Iran, and is a metropolitan city with an area of 730 km2. Tehran’s population is approximately 13 million in the city and 23 million in the larger metropolitan area of greater Tehran.3 There are 13 radiation therapy centers in Tehran (6 in the public and 7 in the private sector), located all over the city, and these centers cover different geographic areas of Tehran. There are also a total of 22 linear accelerators in Tehran. Each health center has to implement major changes in its organization. Herein, we present our policy and recommendations at a private radiology-oncology center.
Description and Perspectives
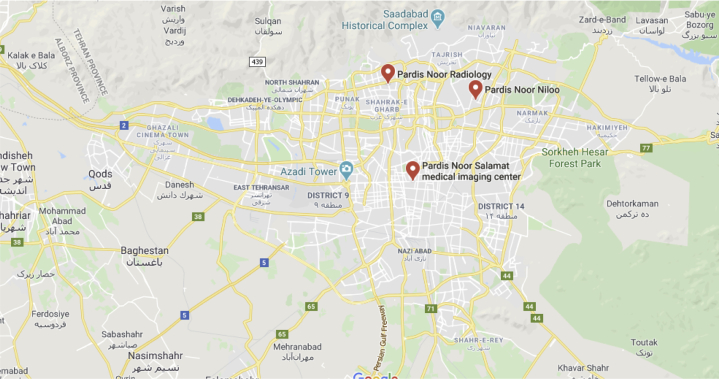
Pardis Noor Radiology-Oncology Center is a private cancer center located in Tehran. The center opened in 2009, and has 3 main branches in Tehran (Table 1). The center consists of the Departments of Diagnostic Radiology, Interventional Radiology, and Nuclear Medicine, in addition to a Radiation Therapy Unit and Chemotherapy Ward. Figure 2 shows the locations of these 3 branches on the map in the city of Tehran.
Table 1.
Names, locations, and departments of each branch of Pardis Noor Radiology-Oncology Center
| Branch name | Location | Area of the city served | Departments |
|---|---|---|---|
| Pardis Noor Radiology | Northwest | West | Diagnostic and interventional radiology, nuclear medicine |
| Pardis Noor Salamat | Center | Central area and South | Diagnostic and interventional radiology, medical laboratory |
| Pardis Noor Niloo | North | North and East | Diagnostic and interventional radiology, radiation therapy, chemotherapy |
Figure 2.
Locations of the 3 branches of Pardis Noor Radiation-Oncology Centre.
Immediately after the announcement of the COVID-19 outbreak in Iran, we decided to implement new rules and principles for our personnel and visitors. As a health care center, we have the responsibility to maintain service as well as to keep our staff and patients safe. We are also responsible to give awareness and education to our society about the outbreak in this challenging time.
One of the highest risk groups for COVID-19 infection are patients who are diagnosed with a malignancy and who have received treatment for cancer or who are under treatment for cancer, such as chemotherapy or radiation therapy.3 We decided to develop policies to maintain the best service possible for our patients diagnosed with malignant disease, and we defined our major goals for actions as follows: (1) decrease the chance of exposure of the clinic’s staff; (2) assure the accurate and sustained delivery of radiation therapy to patients; (3) decrease the chance of exposure of patients and visitors who visit the clinic; (4) educate patients and visitors for signs and symptoms of COVID-19 and general screening of the population visiting the clinic; and (5) guide and give appropriate recommendations and treatment if a person is found to be infected. The target populations for the changing policies were patients, staff and personnel, and visitors (ie, patients’ family members and companions).
Soon after the announcement of the COVID-19 outbreak, our center faced increasing requests for chest computed tomography (CT) scans, which raised the concern of exposure to COVID-19 for our high-risk patients. Hence, we decided to dedicate one branch (Pardis Noor Salamat, located in the center of Tehran) to suspected COVID-19 cases and spare the two other branches. This first move was followed by other plans and actions to prepare our oncology wards in this challenging situation.
Pardis Noor Niloo Radiology-Oncology Center
We developed multiple policies for the Pardis Noor Niloo Center and radiation therapy and chemotherapy wards in addition to the diagnostic and interventional radiology departments. Table 2 shows the different divisions of the Pardis Noor Niloo Radiology-Oncology branch. We reduced the working hours of the radiology department staff members in this branch to 2 days per week. Table 3 shows the number of patients who visited the Pardis Noor Niloo branch within the first week before the outbreak (week –1), the first week after the outbreak, and the third week after the outbreak (week +3)
Table 2.
Departments of Pardis Noor Niloo (North Eastern Branch of Pardis Noor Radiology-Oncology Center)
| Radiation therapy ward | Outpatient clinic | Treatment unit | Physics and dosimetry group | |
|---|---|---|---|---|
| Chemotherapy ward | Outpatient Clinic | Transfusion unit | ||
| Diagnostic radiology | Magnetic resonance imaging | Computed tomography scan | Ultrasound | Conventional radiology |
| Interventional radiology |
Table 3.
Number of visits at Pardis Noor Niloo Radiology-Oncology center (Northeast branch) within weeks –1, +1, and +3
| Week | Total patient visits at the center | Chest CT scan | All CT scans except chest | MRI | Interventional radiology | Bone mineral density | Ultrasound | Mammogram | Conventional radiology | Radiation treatments |
|---|---|---|---|---|---|---|---|---|---|---|
| –1 | 499 | 6 | 91 | 127 | 10 | 9 | 121 | 25 | 13 | 103 |
| +1 | 394 | 27 | 76 | 71 | 13 | 4 | 60 | 12 | 33 | 98 |
| +3 | 191 | 18 | 48 | 18 | 9 | 1 | 23 | 3 | 6 | 65 |
CT = computed tomography; MRI = magnetic resonance imaging; week –1 = week before the outbreak; week +1 = first week after the outbreak; week +3 = third week after the outbreak
The center rules were implemented at the end of the first week. The number of patients visiting this center in week +3 is reduced by 50% compared with week –1.
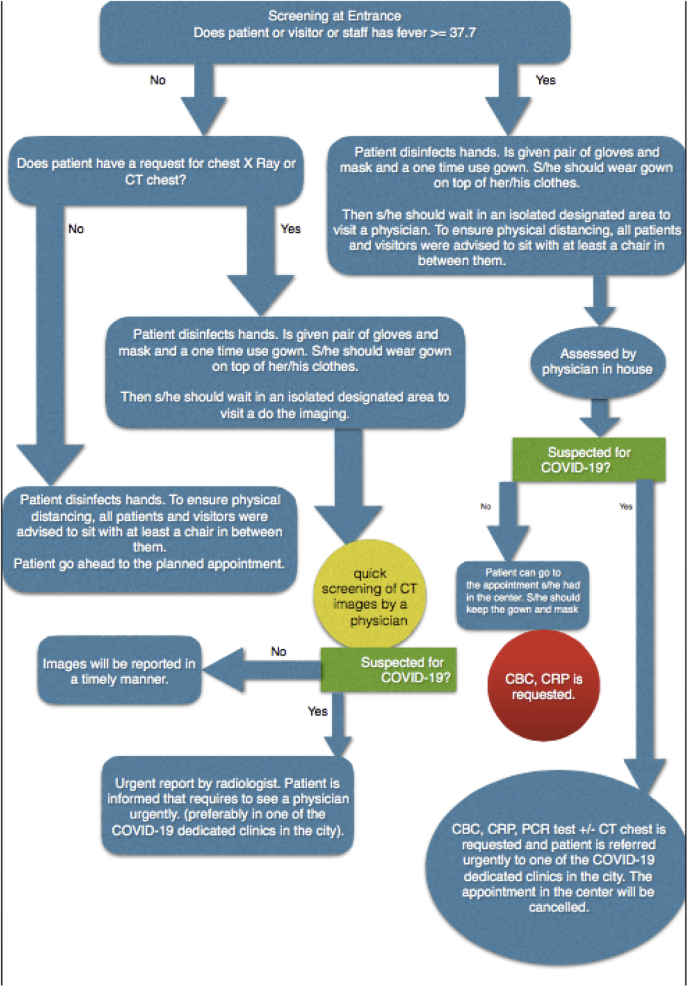
We started fever screenings for all visitors and patients at the entrance of the center, and if anyone had a body temperature of ≥37.7°C, they were placed in a designated isolated waiting area and had to be seen by a physician before going to their appointment. The physician was responsible for deciding whether the suspected cases were able to receive the service that they had initially planned to receive or if the patient should be referred for additional testing, such as virology polymerase chain reaction testing, blood panels, or chest CT scans. If necessary, the patient was referred to an external COVID-19-dedicated clinic. The Iranian Ministry of Health has published a list of dedicated clinics for suspected cases of COVID-19 infection.1 If patients were deemed eligible to receive any service at the center, they were required to wear a gown on top of their clothes, as well as masks and gloves.
A detailed flowchart shows how we make decisions at the time of screening (Fig 3). This flowchart is based on the Iranian Ministry of Health recommendation booklet for outpatient clinics at the time of the outbreak. This booklet was published on March 8, 2020 and is available online.1 Hand sanitizers are available at the entrance and at all stations, and the cleaning of hands is mandatory before entrance and exit. Frequent (every half hour) disinfecting of all the surfaces, chairs, and floors is also in place, and staff members have to change their clothes after coming to work and before leaving the building.
Figure 3.
Flowchart of decision-making after screening patients, visitors, and staff at the entrance.
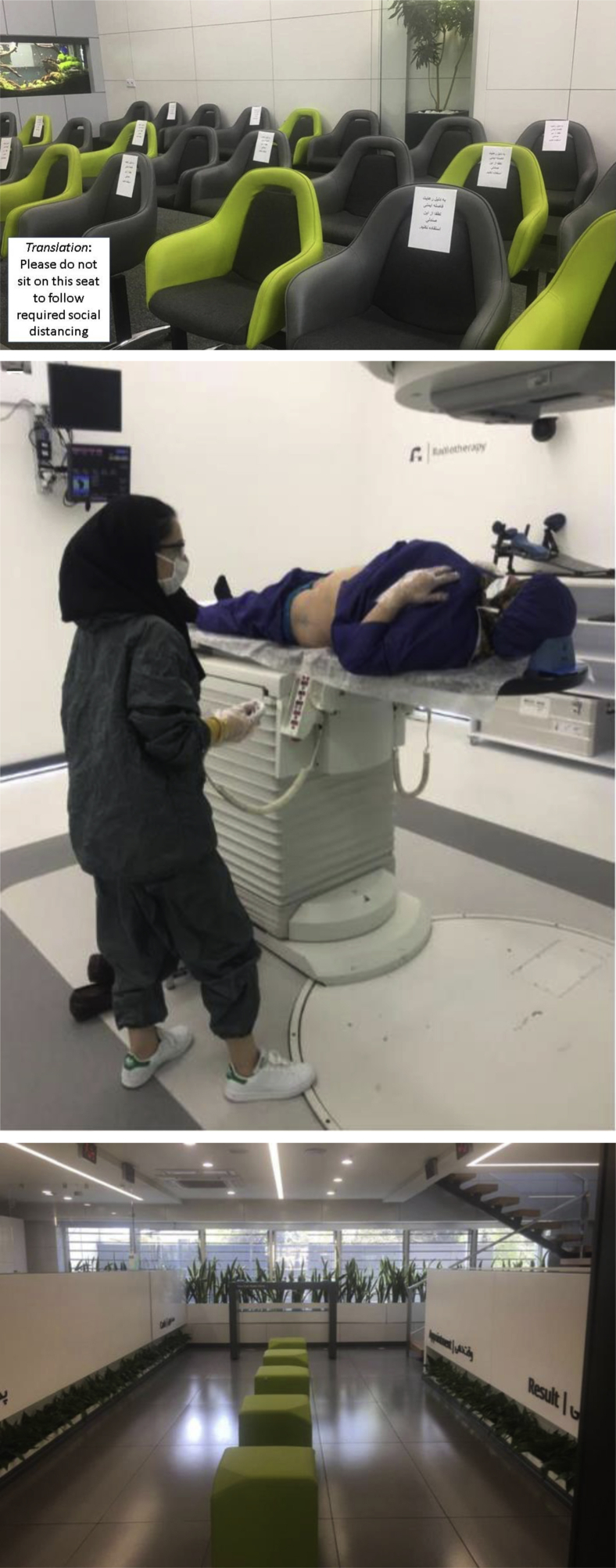
To ensure physical distancing, all patients and visitors are advised to sit with at least 1 chair in between them. If we face limits in the capacity of our waiting area, we advise visitors and patient family members to stay in the car or outside the building. We provide an isolated waiting area for anyone who is found to have a fever (before seeing the physician or administration staff) or who reports a cough or unexpected malaise or myalgia. All suspected cases have to wear a mask and gown on top of their clothes.
Radiation therapy department
Radiation treatment is an integral part of cancer treatment. Approximately 50% of all patients who are diagnosed with cancer will require radiation treatment at some point in their treatment.4 Radiation therapy is a complex multidisciplinary treatment that requires close coordination between different groups of health care workers, including radiation oncologists, medical physicists, radiation technicians, and dosimetrists.
Pardis Noor Niloo is the oncology branch of the Pardis Noor Radiology-Oncology Complex, and is located in the northeast of Tehran. The branch is divided into 11 floors with an area of 2500 m2 and has a single unit of ARTIST Siemens Linear Accelerator with dual high-energy photons (6 MV and 18 MV). The unit is customized with multileaf collimator, electronic portal imaging and cone beam CT. We implemented new rules and regulations to decrease the chance of exposure for our patients and staff while delivering accurate and sustained radiation treatment to our patients (Fig. 4 A-C).
Figure 4.
Pardis Noor Radiology Oncology Center through Covid-19 outbreak.
Outpatient clinics
Outpatient clinics are open during the outbreak. Radiation oncologists have to wear a surgical mask during visits and physical examinations, and physical distancing in the waiting area and clinic are met. However, several modifications were implemented to decrease the chance of spreading the COVID-19 virus.
New consultations
Many radiation therapy centers started modifying the indications and scheduling of radiation treatment.5, 6, 7 To have a systematic approach to make decisions for new patients, we developed a structured table so that the decision making in clinics can be more homogenous (Table 4). We started using and referring to the guidelines recently published.8
Table 4.
Systematic approach to decision making
| Goals of treatment | Types of treatment | Examples of treatment | Decision making for radiation therapy |
|---|---|---|---|
| Curative | Radical | Head and neck cancer, cervical cancer | ∗ |
| Adjuvant | Breast cancer, sarcoma, head and neck cancer, moderate- and high-risk prostate cancer, endometrial cancer | † | |
| Neoadjuvant | Rectal cancer, sarcoma | † | |
| Palliative | Emergency | Cord compression, superior vena cava obstruction, life-threatening bleeding | ∗ |
| Pain control | Bone metastasis, multiple brain metastasis | ‡ |
Note: Stereotactic ablative body radiation or stereotactic radiosurgery for brain lesions is not available in Iran.
Do not defer treatment unless a reasonable alternative exists (eg, start hormone therapy for intermediate- and high-risk prostate cancer and defer radiation treatment for a couple of weeks). If decision is made to start radiation therapy (eg, nasopharyngeal cancer), extensive education on hand hygiene and physical distancing is given directly by the radiation oncologist. All patients have access to hotline to ask questions and report symptoms. Whenever possible, hypofractionated regimen is used.
Categorize evidence behind the indication of radiation therapy and absolute benefit of the treatment. Categorize if there is survival benefit from radiation therapy versus local control benefit (eg, boost in breast radiation therapy can be omitted). Assess whether alternative exists to defer or replace radiation therapy. Prioritize by age and other comorbidities of the patient. Radiation treatment can be deferred for some time (eg, radiation treatment might be canceled for elderly patients with early stage breast cancer). Some cases will be deferred or cancelled in this category.
Defer the treatment and try to use alternative options, such as medical treatment for pain control or use steroidal drugs for multiple brain metastasis.
Radiation treatment is avoided in our patient population whenever possible. If treatment cannot be avoided, it is deferred or shortened when possible. All palliative treatments are and will be delivered through a hypofractionated regimen (either 1 or 5 fractions) until the outbreak is over. Breast cancer adjuvant radiation therapy treatment is one example that is planned to be delivered through a hypofractionated regimen. At the time of the COVID-19 outbreak, we are treating all patients with breast cancer with 40 Gy in 15 fractions (adopted from the UK Consensus Statement).9
Follow-up patients
Most follow-up visits are performed through phone and video calls, unless the physician feels that the patient needs to be seen, and then a visit is be arranged. This includes any new complaint, sign, or symptom that warrants a detailed physical examination, such as a new lump in the breast for patients with a history of breast cancer or a new lump in the neck for patients with a history of head and neck cancer.
If there is no concerning symptom or new complaint, follow-up procedures (eg, colonoscopy for patients with colorectal cancer, endoscopic physical examination for patients with a history of head and neck cancer) and imaging requests (eg, brain magnetic resonance imaging for patients with a history of glioblastoma multiforme or a chest CT scan for patients with a history of lung cancer) are all deferred.
Patients under treatment
Unless patients have a major side effect (eg, from head and neck cancer radiation treatment), they are advised to leave the building after treatment. Hence, almost all weekly visits for patients under treatment were cancelled. A direct line, in addition to a direct WhatsApp line, to a radiation oncologist was provided for all patients so that they can report any complication. WhatsApp is a common messaging service in Iran, and most people are familiar with its use. We have not experienced any issue using these measures.
Treatment unit
We reduced the number of CT simulation sessions to 2 days per week. We kept, at maximum, 2 radiation technicians (RTs) at the time of each patient’s treatment appointment to work the treatment machines. RTs must wear airtight, waterproof clothes provided by the center. Before and after each patient, all immobilization devices, in addition to the RT’s hands, top clothes, and sleeves are disinfected using an alcohol-based solution. The treatment machine coach is always covered with a 1-time use cover sheet, which is changed after each patient.
All patients are asked if they have any symptoms of cough, myalgia, malaise, and fever. This is an extra screening on top of the screening at the entrance. If the answer to any of these questions is positive, the patient is treated with a mask and a gown on top of their clothes. Then, arrangements are made for the patient to visit the inhouse physician. A thorough history review of possible exposure, signs, and symptoms for COVID-19 infection is performed, and any required test (eg, polymerase chain reaction test for COVID-19, complete blood count, c-reactive protein, or chest CT scan) is ordered.10
If a patient is confirmed to have COVID-19 by virology testing or CT scan findings (in addition to clinical symptoms) at any time during treatment, the radiation treatment is ceased, and the patient is referred to a dedicated clinic for assessment and quarantine. The Iranian Ministry of Health has published a list of dedicated clinics for suspected cases of COVID-19 infection.1 Radiation treatment is restarted after the patient’s virology test is negative. The decision to continue treatment after completion of the quarantine is made by the radiation oncologist based on the type of cancer, the number of days left, and the number of days of interruption. For some patients, changes to their treatment plan to account for missed days may be made, which is decided by the radiation oncologist and responsible physicist.
Physics and dosimetry
Physicians can review CT images of patients from home. If needed, a consultation with a radiologist or other specialists can be done through phone or video call. External access to treatment planning and contouring is still not available at our center. However, to practice physical and social distancing, different rooms are dedicated to physicians for contouring and to physicists for treatment planning.
In the medical physics department, we also tried to find ways to practice physical distancing of at least 1.5 m. The staff is distributed in separate (long) working shifts to minimize exposure in an enclosed space in the planning room. All staff members are required to change clothes after coming to work and before going out of the building. Special strategies are taken to decrease the workload and decrease staff stay at the center. The annual quality assurance check of our center is presently postponed for 2 months. The monthly mechanical tests for the linear accelerators, lasers, and treatment couch are all performed by a single medical physicist. We stopped using physical wedges to decrease treatment time and the presence of RTs in the treatment room. Virtual wedges continue to be used.
Chemotherapy department
We adopted a few strategies in the chemotherapy ward during the COVID-19 outbreak. The distance between all beds in the chemotherapy unit is set to be at least 1.5 m. We limit the number of patient companions to a maximum of 1 person and preferably none. We also started refusing to accept patients from other cities and instead refer them to the nearest facility to their home city. Outpatient regimens are now preferred to reduce the time of hospitalization. In cases that are eligible for upfront surgery, such as breast cancer or sarcoma, neoadjuvant chemotherapy is omitted. For patients with a history of neutropenia, dose adjustment are made. Because of the shortage in blood supply, dose adjustment are made in the patients with borderline levels of serum hemoglobin (≤9 g/dL).
Radiology department
After day 5 of the outbreak, the team decided to reduce the radiology department working schedule to 2 days per week, including both the CT simulations and diagnostic radiology. We also implemented a policy to disinfect the magnetic resonance imaging and CT scanner. At the end of the day, all surfaces of the diagnostic machines are disinfected with Deconex solution. If Deconex is not available, we use Kodan solution that contains 2 and 1-propanol, biphenyl, hydrogen peroxide, and water.
If a patient is referred for a CT chest scan or chest x-ray regardless of the indication or symptom, they would be seated in an isolated area, and should wear a mask and gown on top of their clothes. The images are all reviewed quickly so if there are suspicious findings, an urgent report by the radiologist can be done. An urgent consultation with a physician can be arranged.
Conclusions
All health care workers face an extremely challenging situation after the announcement of the COVID-19 outbreak in Iran. Emergency medicine specialists, internists, infectious disease specialists, and respirologists, as well as nurses who work with them, experience a huge burden of workload and emotional stress. Many of our colleagues have to isolate themselves at the hospital for a few days before switching shifts to keep their families safe. We have sadly lost many colleagues in different departments, including physicians, nurses, RTs, administration workers, and laboratory technicians.
Patients who are diagnosed with malignant disease or those who receive therapy for cancer are at a higher risk for COVID-19 infection and have a poorer prognosis.4 This is a further challenge for radiation oncologists while taking care of their patients. Radiation therapy is a multidisciplinary treatment, and radiation oncologists are dependent on physicists, RTs, and nurses. We are aware of the limited human resources we face, and are trying diligently to decrease the chance of virus spread at our center.
However, we are dedicated to keep our patients and staff members safe while offering sustaining treatment to our patients. This report is a summary of the approach and precautions taken in the private sector in Tehran to reach this goal. An international guideline for best practices in oncology clinics that face COVID-19 would best serve our patients with cancer all over the world in this challenging time of health history.
Acknowledgments
The authors appreciate the help of all staff members, administration workers, RTs, and physicists in this challenging time. The authors especially thank Drs Soraya Salmanian and Sara Abdollahi for their help, guidance, and contribution in the care of our patients and scheduling our policies.
Footnotes
Disclosures: None.
References
- 1.Iranian Ministry of Health and Medical Education Official website. http://behdasht.gov.ir Available at:
- 2.World Health Organization Official website. www.who.int
- 3.Wikipedia Tehran, Iran. https://en.wikipedia.org/wiki/Tehran Available at:
- 4.Liang W., Guan W., Chen R. Cancer patients in SARS-CoV-2 infection: A nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baskar R., Lee K.A., Yeo R., Yeoh K.W. Cancer and radiation therapy: Current advances and future directions. Int J Med Sci. 2012;9:193–199. doi: 10.7150/ijms.3635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Filippi A.R., Russi E., Magrini S.M., Corvo R. Letter from Italy: First practical indications for radiation therapy departments during COVID-19 outbreak. Int J Radiat Oncol Biol Phys. 2020 doi: 10.1016/j.ijrobp.2020.03.007. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wu S., Zheng D., Liu Y., Hu D., Wei W., Han G. Radiotherapy care during a major outbreak of COVID-19 in Wuhan. Adv Radiat Oncol. 2020 doi: 10.1016/j.adro.2020.03.004. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Simcock R., Thomas T.V., Estes C. COVID-19: Global radiation oncology’s targeted response for pandemic preparedness. Clin Transl Radiat Oncol. 2020;22:55–68. doi: 10.1016/j.ctro.2020.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Royal College of Radiologists, Clinical Oncology Group . The Royal College of Radiologists; London, United Kingdom: 2016. Postoperative radiotherapy for breast cancer: UK consensus statements. [Google Scholar]
- 10.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]