Abstract
Background
Aspirin and heparin are widely used as preventive strategy to reduce the high risk of recurrent pregnancy loss in women with antiphospholipid antibodies (aPL).
This review supersedes a previous, out‐of‐date review that evaluated all potential therapies for preventing recurrent pregnancy loss in women with aPL. The current review focusses on a narrower scope because current clinical practice is restricted to using aspirin or heparins, or both for women with aPL in an attempt to reduce pregnancy complications.
Objectives
To assess the effects of aspirin or heparin, or both for improving pregnancy outcomes in women with persistent (on two separate occasions) aPL, either lupus anticoagulant (LAC), anticardiolipin (aCL) or aβ2‐glycoprotein‐I antibodies (aβ2GPI) or a combination, and recurrent pregnancy loss (two or more, which do not have to be consecutive).
Search methods
We searched Cochrane Pregnancy and Childbirth’s Trials Register, ClinicalTrials.gov, the WHO International Clinical Trials Registry Platform (ICTRP) (3 June 2019), and reference lists of retrieved studies. Where necessary, we attempted to contact trial authors.
Selection criteria
Randomised, cluster‐randomised and quasi‐randomised controlled trials that assess the effects of aspirin, heparin (either low‐molecular‐weight heparin (LMWH) or unfractionated heparin (UFH]), or a combination of aspirin and heparin compared with no treatment, placebo or another, on pregnancy outcomes in women with persistent aPL and recurrent pregnancy loss were eligible. All treatment regimens were considered.
Data collection and analysis
Two review authors independently assessed trials for inclusion criteria and risk of bias. Two review authors independently extracted data and checked them for accuracy and the certainty of the evidence was assessed using the GRADE approach.
Main results
Eleven studies (1672 women) met the inclusion criteria; nine randomised controlled trials and two quasi‐RCTs. The studies were conducted in the USA, Canada, UK, China, New Zealand, Iraq and Egypt. One included trial involved 1015 women, all other included trials had considerably lower numbers of participants (i.e. 141 women or fewer).
Some studies had high risk of selection and attrition bias, and many did not include sufficient information to judge the risk of reporting bias. Overall, the certainty of evidence is low to very low due to the small numbers of women in the studies and to the risk of bias.
The dose and type of heparin and aspirin varied among studies. One study compared aspirin alone with placebo; no studies compared heparin alone with placebo and there were no trials that had a no treatment comparator arm during pregnancy; five studies explored the efficacy of heparin (either UFH or LMWH) combined with aspirin compared with aspirin alone; one trial compared LMWH with aspirin; two trials compared the combination of LMWH plus aspirin with the combination of UFH plus aspirin; two studies evaluated the combination of different doses of heparin combined with aspirin. All trials used aspirin at a low dose.
Aspirin versus placebo
We are very uncertain if aspirin has any effect on live birth compared to placebo (risk ratio (RR) 0.94, 95% confidence interval (CI) 0.71 to 1.25, 1 trial, 40 women, very low‐certainty evidence).
We are very uncertain if aspirin has any effect on the risk of pre‐eclampsia, pregnancy loss, preterm delivery of a live infant, intrauterine growth restriction or adverse events in the child, compared to placebo. We are very uncertain if aspirin has any effect on adverse events (bleeding) in the mother compared with placebo (RR 1.29, 95% CI 0.60 to 2.77, 1 study, 40 women). The certainty of evidence for these outcomes is very low because of imprecision, due to the low numbers of women involved and the wide 95% CIs, and also because of risk of bias.
Venous thromboembolism and arterial thromboembolism were not reported in the included studies.
Heparin plus aspirin versus aspirin alone
Heparin plus aspirin may increase the number of live births (RR 1.27, 95% CI 1.09 to 1.49, 5 studies, 1295 women, low‐certainty evidence).
We are uncertain if heparin plus aspirin has any effect on the risk of pre‐eclampsia, preterm delivery of a live infant, or intrauterine growth restriction, compared with aspirin alone because of risk of bias and imprecision due to the low numbers of women involved and the wide 95% CIs. We are very uncertain if heparin plus aspirin has any effect on adverse events (bleeding) in the mother compared with aspirin alone (RR 1.65, 95% CI 0.19 to 14.03, 1 study, 31 women).
No women in either the heparin plus aspirin group or the aspirin alone group had heparin‐induced thrombocytopenia, allergic reactions, or venous or arterial thromboembolism. Similarly, no infants had congenital malformations.
Heparin plus aspirin may reduce the risk of pregnancy loss (RR 0.48, 95% CI 0.32 to 0.71, 5 studies, 1295 women, low‐certainty evidence).
When comparing LMWH plus aspirin versus aspirin alone the pooled RR for live birth was 1.20 (95% CI 1.04 to 1.38, 3 trials, 1155 women). In the comparison of UFH plus aspirin versus aspirin alone, the RR for live birth was 1.74 (95% CI 1.28 to 2.35, 2 trials, 140 women).
Authors' conclusions
The combination of heparin (UFH or LMWH) plus aspirin during the course of pregnancy may increase live birth rate in women with persistent aPL when compared with aspirin treatment alone. The observed beneficial effect of heparin was driven by one large study in which LMWH plus aspirin was compared with aspirin alone. Adverse events were frequently not, or not uniformly, reported in the included studies. More research is needed in this area in order to further evaluate potential risks and benefits of this treatment strategy, especially among women with aPL and recurrent pregnancy loss, to gain consensus on the ideal prevention for recurrent pregnancy loss, based on a risk profile.
Plain language summary
Anticoagulant drugs for the prevention of recurrent miscarriage in women with antiphospholipid antibodies
We set out to determine if antithrombotic drugs improve pregnancy outcomes for women with persistent antiphospholipid antibody levels who have had a number of miscarriages.
What is the issue?
Phospholipid molecules help form the cell membranes and are critical to a cell's ability to function. The immune system can develop antibodies that are directed against proteins attached to the phospholipids. Different types of antiphospholipid antibodies exist. Presence of these antibodies can lead to the development of blood clots in either veins or arteries, but also repeated pregnancy losses.
Why is this important?
Antiphospholipid antibodies are associated with a higher risk of pregnancy complications, including the risk of pregnancy loss. Use of antithrombotic drugs during pregnancy may help prevent pregnancy loss for women who have had recurrent miscarriages. Aspirin is an anti‐inflammatory drug that reduces platelet aggregation and blood clotting. Heparin is a potent anticoagulant that prevents blood clot formation. Aspirin and heparin may reduce the risk of miscarriage associated with antiphospholipid antibodies. Low‐molecular‐weight heparin is easier to use and causes less side effects for the mother than undivided or unfractionated heparin.
What evidence did we find?
We searched the medical literature for evidence from randomised controlled trials up to June 2019. We identified 11 studies involving 1672 women who had previously experienced at least two pregnancy losses and had persistent antiphospholipid antibodies in their blood. Most studies started eligible women on aspirin before conception with women randomly assigned to receive additional heparin, or not, once pregnancy was confirmed. The dose and type of heparin varied among studies, as did timing for when treatment was started and the length of time women were treated.
The evidence we identified is low certainty due to the small numbers of women in the studies and to the risk of bias in the studies.
Compared to placebo, we are very uncertain if aspirin has any effect on live birth, pre‐eclampsia, pregnancy loss, preterm delivery of a live infant, intrauterine growth restriction or adverse events in the child or in the mother. Venous thromboembolism and arterial thromboembolism were not reported in the studies investigating aspirin compared with placebo.
Heparin plus aspirin may increase the number of live births and may reduce the risk of pregnancy loss.
Compared with aspirin alone, we are uncertain if heparin plus aspirin has any effect on the risk of pre‐eclampsia, preterm delivery of a live infant, intrauterine growth restriction, or bleeding in the mother.
No women in either the heparin plus aspirin group or the aspirin alone group had heparin‐induced thrombocytopenia, allergic reactions, or venous or arterial thromboembolism. Similarly, no infants had congenital malformations.
What does this mean?
The combination of heparin with aspirin during the course of pregnancy for women with persistent antiphospholipid antibodies may lead to a higher number of live births than treatment with aspirin alone. We are uncertain about the safety of heparin and aspirin for mothers and infants because of the lack of reporting of adverse events. Future trials should recruit adequate numbers of women and to fully evaluate the risks and benefits of this treatment strategy.
Summary of findings
Background
Description of the condition
Antiphospholipid antibodies (aPL) are directed against phospholipids and include lupus anticoagulant (LAC), immunoglobulin G (IgG) or immunoglobulin M (IgM) anticardiolipin (aCL) and IgG or IgM anti‐β2‐glycoprotein‐I (aβ2GPI) antibodies. The presence of aPL is associated with a hypercoagulable state (Harris 1983), which is an abnormally increased tendency toward clotting of the blood. aPL are predominantly known for their role in antiphospholipid syndrome (APS), also known as antiphospholipid antibody syndrome or Hughes syndrome. APS is an autoimmune disorder characterised by the occurrence of a clinical event (recurrent pregnancy loss and/or thrombosis) in the persistent presence of aPL. Currently, the diagnosis of APS is made according to the Sydney criteria established in 2006 (also known as the revised Sapporo criteria), and is based on both clinical and biochemical findings (Miyakis 2006). The clinical criteria include venous and/or arterial thrombosis and well‐defined pregnancy complications such as (recurrent) pregnancy loss (miscarriage or fetal loss) and pre‐eclampsia, whereas the biochemical criteria include persistent (after a 12‐week window) presence of aPL. The diagnosis of APS is made if a woman meets at least one of the clinical criteria and at least one of the biochemical criteria.
Antiphospholipid antibodies are reported to be present in 1% to 5.6% of healthy individuals, with prevalence increasing with age (Durcan 2016). In women with recurrent first trimester pregnancy losses, the presence of these antibodies has been detected in 15% (Rai 1995). Presence of antibodies without clinical events does not indicate treatment, as only a minority of individuals with aPL will develop APS (Ruiz‐Irastorza 2010). The prevalence of APS is estimated to range from 40 to 50 per 100,000 individuals, and is especially increased in women with autoimmune and rheumatic diseases, such as systemic lupus erythematosus (SLE) (Gómez‐Puerta 2014; Love 1990).
Knowledge on the mechanisms and triggers inducing the development and persistence of aPL and the different clinical manifestations are poorly understood. It is thought that beside the presence of the antibodies, a trigger such as pregnancy, hormonal therapy, malignancy, smoking or infection, plays a key role in disease initiation (Meroni 2018). As for APS, knowledge and understanding of the disorder evolve constantly, but uncertainty regarding pathogenesis, diagnosis, as well as optimal treatment remains (Schreiber 2018).
Recently it has been suggested that women with different disease manifestations may represent different subgroups with subsequently, a different course of disease in terms of recurrence risk and type of events. For example, women presenting with thrombotic events may represent a different subgroup from women presenting with pregnancy complications, or women presenting with venous events might be a different subgroup again from women presenting with arterial events (Meroni 2012; Lockshin 2013). Moreover, it has been suggested that the risk of (recurrent) pregnancy complications may differ between groups of women. For example, the risk of pregnancy complications (and type of complication) may differ in women with previous complications compared with women with no previous complication, women with high and low aPL titres, and women with positive versus negative LAC antibodies (Erkan 2002; Ioannou 2010; Lockshin 2012).
Description of the intervention
Aspirin and heparins, either unfractionated heparin (UFH) or low‐molecular‐weight heparin (LMWH), are antithrombotic drugs, often prescribed with the intention to prevent excessive clotting of the blood. Aspirin, also known as acetylsalicylic acid, prevents the formation of thromboxane A2, and inhibits platelet aggregation (Vane 1971; Vane 2003). Heparins inhibit thrombus formation by binding to the natural anticoagulant antithrombin, which results in a potent activation of this enzyme (Chaung 2001). The preferred route of UFH administration is either by a continuous intravenous administration or by subcutaneous injection, whereas LMWH is administered by subcutaneous injection. Important side effects of heparin therapy include haemorrhage, heparin‐induced thrombocytopenia and osteoporosis. Heparins do not cross the placenta and are considered safe for the fetus. Treatment with therapeutic doses of UFH requires frequent monitoring, which LMWH treatment does not. For several indications, when studied in the non‐pregnant population, LMWH was found to have similar efficacy and a superior safety profile (Green 1994; Nurmohamed 1992). The antithrombotic effects in pregnant women may not be alike, due to differences in protein binding. Inconsistent findings have been reported and a direct comparison in a large clinical trial has not yet been made (Ensom 2004; Pariente 2016).
How the intervention might work
Antithrombotic therapy has been found to reduce the risk of recurrent (either venous or arterial) thrombosis in APS (ACOG 2012). Traditionally it is hypothesised that pregnancy complications in APS are also the result of a hypercoagulable state, partially by thrombosis of the placental vasculature. Recent hypotheses describe a more intertwined pathophysiological mechanism in which both the coagulation system, as well as inflammation are involved (Meroni 2018; Redecha 2008; Samarkos 2012). Aspirin and heparin may both have a beneficial effect on coagulation and inflammation (Kozlowski 2011; Vane 2003; Vignoli 2006), and are thought to reduce the risk of pregnancy loss in APS. Antiphospholipid antibodies directly inhibit trophoblast proliferation and differentiation, which can lead to defective placentation (Meroni 2018). This inhibitory effect of aPL on proliferation of trophoblasts has been proposed as the pathogenic mechanism in early pregnancy loss, whereas late obstetrical complications have been attributed to a dysfunctional placenta (Burton 2009; Di Simone 2000; Derksen 2008). The effects of UFH on trophoblast proliferation have not been evaluated, but LMWH has the capacity to stimulate proliferation and protect against apoptosis (cell death) of trophoblasts (Shomer 2016). For this reason, if LMWH administration had a beneficial effect in prevention of early miscarriage, the effects would be observed early during pregnancy. Moreover, it has been suggested that aPLs affect the production of several chemokines and angiogenic factors by human endometrial endothelial cells, which may contribute to impaired placentation and vascular transformation. Noticeably, one recent study demonstrated that LMWH and aspirin, alone or in combination, exacerbated the changes in human endometrial endothelial function mediated by aPL, rather than protecting against them (Quao 2018).
Why it is important to do this review
This is a new review which will supersede the previous, out‐of‐date review by Empson and colleagues (Empson 2005), which included all potential therapies for preventing recurrent pregnancy loss in women with aPL. This new review has a narrower scope than Empson 2005, as currently in clinical practice only aspirin or heparins, or both are used in women with aPL in an attempt to reduce pregnancy complications. However, it is uncertain whether these antithrombotic therapies improve pregnancy outcome and reduce the risk of pregnancy complications in women with persistent (on two occasions) aPL.
Objectives
To assess the effects of aspirin or heparin, or both for improving pregnancy outcomes in women with persistent (on two separate occasions) antiphospholipid antibodies (aPL), either lupus anticoagulant (LAC), anticardiolipin (aCL) or aβ2‐glycoprotein‐I antibodies (aβ2GPI), or a combination, and recurrent pregnancy loss (two or more, which do not have to be consecutive).
Methods
Criteria for considering studies for this review
Types of studies
All randomised controlled trials (RCTs), cluster‐randomised trials and quasi‐randomised controlled trials evaluating aspirin or heparin, or both for improving pregnancy outcome in women with recurrent pregnancy loss and persistent antiphospholipid antibodies (aPL). Cross‐over trials were excluded due to the nature of outcomes considered. Studies published in abstract form only were included if sufficient data were available to determine eligibility.
Types of participants
This review includes women with recurrent (two or more, which do not have to be consecutive) pregnancy loss in the presence of persistent (on two separate occasions) aPL. Pregnancy loss entailed any miscarriage or fetal loss, however defined by the trial authors. aPL presence was determined by either positive LAC, aCL or aβ2 antibodies, or a combination.
Types of interventions
Any comparison of aspirin, heparin (either low‐molecular‐weight heparin (LMWH) or unfractionated heparin (UFH)) or a combination of aspirin and heparin with no treatment, placebo or another was included. Any treatment regimen was considered.
Types of outcome measures
Primary outcomes
Live birth
Secondary outcomes
For the mother
Pre‐eclampsia (definition according to original study)
Adverse events in the mother (definitions according to original study: (A) bleeding, (B) heparin‐induced thrombocytopenia, (C) allergic reactions)
Venous thromboembolism
Arterial thromboembolism
Pregnancy loss
For the child
Preterm delivery of a live infant (before 37 weeks, 24 to 28 weeks, 28 to 32 weeks and 32 to 37 weeks)
Intrauterine growth restriction (definition according to original study)
Adverse events in the child (definitions according to original study: (A) congenital malformations, (B) neonatal bleeding)
Search methods for identification of studies
The following search methods section was based on a standard template used by Cochrane Pregnancy and Childbirth.
Electronic searches
We searched Cochrane Pregnancy and Childbirth’s Trials Register by contacting their Information Specialist (3 June 2019).
The Register is a database containing over 25,000 reports of controlled trials in the field of pregnancy and childbirth. It represents over 30 years of searching. For full current search methods used to populate Pregnancy and Childbirth’s Trials Register including the detailed search strategies for CENTRAL, MEDLINE, Embase and CINAHL; the list of handsearched journals and conference proceedings, and the list of journals reviewed via the current awareness service, please follow this link.
Briefly, Cochrane Pregnancy and Childbirth’s Trials Register is maintained by their Information Specialist and contains trials identified from:
monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL);
weekly searches of MEDLINE (Ovid);
weekly searches of Embase (Ovid);
monthly searches of CINAHL (EBSCO);
handsearches of 30 journals and the proceedings of major conferences;
weekly current awareness alerts for a further 44 journals plus monthly BioMed Central email alerts.
Search results are screened by two people and the full text of all relevant trial reports identified through the searching activities described above is reviewed. Based on the intervention described, each trial report is assigned a number that corresponds to a specific Pregnancy and Childbirth review topic (or topics), and is then added to the Register. The Information Specialist searches the Register for each review using this topic number rather than keywords. This results in a more specific search set that has been fully accounted for in the relevant review sections (Included studies; Excluded studies; Ongoing studies).
In addition, we searched ClinicalTrials.gov and the WHO International Clinical Trials Registry Platform (ICTRP) (3 June 2019) for unpublished, planned and ongoing trial reports using the search methods detailed in Appendix 1.
Searching other resources
We handsearched the reference lists of retrieved studies and relevant review articles. We did not apply any language or date restrictions.
Data collection and analysis
The following methods section was based on a standard template used by Cochrane Pregnancy and Childbirth.
Selection of studies
Two review authors independently assessed for inclusion all potential studies identified as a result of the search strategy. All disagreements were resolved through discussion and if necessary a third author was involved to have the final vote.
We created a study flow diagram to map out the number of records identified, included and excluded (Moher 2009).
Data extraction and management
We designed a form to extract data. Two review authors independently extracted data for every eligible study using the agreed form. A consensus meeting was held to deal with differences in the extracted data, and if necessary a third review author was involved to have the final vote.
All extracted data were entered into the Review Manager 5 (RevMan 5) software (RevMan 2014) and checked for accuracy. In case of uncertainties regarding the study data, we contacted authors of the specific study for additional information.
Assessment of risk of bias in included studies
Two review authors independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017). Any disagreement was resolved by discussion or by involving a third assessor.
(1) Random sequence generation (checking for possible selection bias)
We described for each included study the method used to generate the allocation sequence in sufficient detail to allow an assessment of whether it should produce comparable groups.
We assessed the method as:
low risk of bias (any truly random process, e.g. random number table; computer random‐number generator);
high risk of bias (any non‐random process, e.g. odd or even date of birth; hospital or clinic record number);
unclear risk of bias.
(2) Allocation concealment (checking for possible selection bias)
We described for each included study the method used to conceal allocation to interventions prior to assignment and assessed whether intervention allocation could have been foreseen in advance of, or during recruitment, or changed after assignment.
We assessed the methods as:
low risk of bias (e.g. telephone or central randomisation; consecutively‐numbered, sealed, opaque envelopes);
high risk of bias (open random allocation; unsealed or non‐opaque envelopes, alternation; date of birth);
unclear risk of bias.
(3.1) Blinding of participants and personnel (checking for possible performance bias)
We described for each included study the methods used, if any, to blind study participants and personnel from knowledge of which intervention a participant received. We considered that studies were at low risk of bias if they were blinded, or if we judged that the lack of blinding was unlikely to affect results. We assessed risk of bias by blinding separately for different outcomes or classes of outcomes.
We assessed the methods as:
low, high or unclear risk of bias for participants;
low, high or unclear risk of bias for personnel.
(3.2) Blinding of outcome assessment (checking for possible detection bias)
We described for each included study the methods used, if any, to blind outcome assessors from knowledge of which intervention a participant received. We assessed blinding separately for different outcomes or classes of outcomes.
We assessed methods used to blind outcome assessment as:
low, high or unclear risk of bias.
(4) Incomplete outcome data (checking for possible attrition bias due to the amount, nature and handling of incomplete outcome data)
We described for each included study, and for each outcome or class of outcomes, the completeness of data including attrition and exclusions from the analysis. We stated whether attrition and exclusions were reported and the numbers included in the analysis at each stage (compared with the total randomised participants), reasons for attrition or exclusion where reported, and whether missing data were balanced across groups or were related to outcomes. Where sufficient information was reported, or could be supplied by the trial authors, we planned to re‐include missing data in the analyses that we undertook.
We assessed the methods as:
low risk of bias (e.g. no missing outcome data; missing outcome data balanced across groups);
high risk of bias (e.g. numbers or reasons for missing data imbalanced across groups; ‘as‐treated’ analysis done with substantial departure of intervention received from that assigned at randomisation);
unclear risk of bias.
(5) Selective reporting (checking for reporting bias)
We described for each included study how we investigated the possibility of selective outcome reporting bias and what we found.
We assessed the methods as:
low risk of bias (where it is clear that all of the study’s pre‐specified outcomes and all expected outcomes of interest to the review have been reported);
high risk of bias (where not all the study’s pre‐specified outcomes have been reported; one or more reported primary outcomes were not pre‐specified; outcomes of interest have been reported incompletely and so cannot be used; study failed to include results of a key outcome that would have been expected to have been reported);
unclear risk of bias.
(6) Other bias (checking for bias due to problems not covered by (1) to (5) above)
We described for each included study any important concerns we had about other possible sources of bias.
We assessed whether each study was free of other problems that could put it at risk of bias:
low risk of other bias;
high risk of other bias;
unclear whether there is risk of other bias.
(7) Overall risk of bias
We made explicit judgements about whether studies are at high risk of bias, according to the criteria given in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017). With reference to (1) to (6) above, we planned to assess the likely magnitude and direction of the bias and whether we considered it is likely to impact on the findings. We explored the impact of the level of bias through undertaking sensitivity analyses ‐ see Sensitivity analysis.
Measures of treatment effect
Dichotomous data
For dichotomous data, we presented results as summary risk ratio with 95% confidence intervals.
Continuous data
We did not include any continuous outcome data in the current review. In future updates, we will use the mean difference if outcomes are measured in the same way between trials. We will use the standardised mean difference to combine trials that measure the same outcome, but used different methods.
Unit of analysis issues
Cluster‐randomised trials
There were no cluster‐randomised trials identified to date for inclusion; we will however include them in future updates in the analyses along with individually‐randomised trials. We will adjust for sample sizes, guided by the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2017). If possible, we will use the estimate of the intra‐cluster correlation coefficient (ICC) derived from the study, from a similar study or from a study with a similar population. When we use ICCs from external sources, we will mention it explicitly in the review, and we will conduct appropriate sensitivity analyses. When both cluster‐randomised trials and individually‐randomised trials are encountered, we will use relevant data for the review. We will combine results from both cluster‐randomised trials and individually‐randomised trials if little heterogeneity is observed between study designs, provided that the interaction between the effect of intervention and choice of randomisation unit is considered to be unlikely. Heterogeneity will be acknowledged in the randomisation unit and we will conduct a sensitivity analysis to explore the effects of this randomisation unit.
Multiple‐arm studies
There were no multi‐arm trials identified to date for inclusion. For future updates, all intervention arms will be reported and described in the Characteristics of included studies table, including the number of women randomised to each arm. We will combine groups, to create a single pair‐wise comparison if possible. Appropriate pair‐wise comparisons will then be selected for the meta‐analysis, in order to avoid double‐counting of one of the arms. We will declare in the Characteristics of included studies table if a trial has an intervention arm that is not applicable or relevant to our review question. We will only include the intervention and control groups that meet the eligibility criteria in the analyses.
Cross‐over trials
We considered cross‐over trials an inappropriate design for this intervention.
Dealing with missing data
For every individual included study, we determined the level of attrition. We evaluated the impact on the overall assessment of the intervention of including studies with high proportions of missing data by conducting a sensitivity analysis without these studies.
For all outcomes, analyses were carried out, as far as possible, on an intention‐to‐treat basis; we attempted to include all participants randomised in the analyses, and analysed these participants according to their allocated treatment assignment, regardless of whether the allocated intervention was received. For each outcome in every trial, the denominator was the number of randomised participants minus the participants whose outcomes are missing. In studies with more than 5% loss to follow‐up, we planned to perform a best‐case scenario analysis (losses to follow‐up assumed to have a positive outcome, e.g. primary outcome) and a worst‐case scenario analysis (losses to follow‐up assumed to have a negative outcome, e.g. no primary outcome) ‐ we did not need to perform best case/worst case analyses because the primary outcome was available for all women.
Assessment of heterogeneity
In all meta‐analyses we assessed statistical heterogeneity using the Tau², I² (Higgins 2003) and Chi² statistics (Deeks 2011). We regarded heterogeneity as substantial if Tau² was greater than zero and either the I² statistic was greater than 30%, or there was a P value equal to or less than 0.10 in the Chi² test for heterogeneity.
Assessment of reporting biases
None of the meta‐analyses in the current review concerned 10 or more studies. If in future updates, if the meta‐analysis includes 10 or more studies, we will explore potential reporting bias (mainly publication bias) using funnel plots and visually assess them. We will prepare funnel plots and visually assess them for asymmetry. If visual assessment leads us to suspect asymmetry, we will conduct additional analyses to explore these potential biases.
Data synthesis
We carried out statistical analysis using RevMan 5 software (RevMan 2014). We used fixed‐effect meta‐analysis for combining data where it was reasonable to assume that studies were estimating the same underlying treatment effect: that is, where trials were examining the same intervention, and the trials’ populations and methods were judged sufficiently similar. Where there was clinical heterogeneity sufficient to expect that the underlying treatment effects differed between trials, or if we detected substantial statistical heterogeneity, we used random‐effects meta‐analysis to produce an overall summary, if an average treatment effect across trials was considered clinically meaningful. We treated the random‐effects summary as the average of the range of possible treatment effects and we discussed the clinical implications of treatment effects differing between trials. If the average treatment effect was not clinically meaningful, we did not combine trials.
Where we used random‐effects analyses, we presented the results as the average treatment effect with 95% confidence intervals, and the estimates of Tau² and I² statistic.
Subgroup analysis and investigation of heterogeneity
For the comparison 'heparin with or without aspirin versus aspirin alone', we did subgroup analysis per type of heparin, as follows:
UFH plus aspirin versus aspirin alone
LMWH plus aspirin versus aspirin alone
Over the last two decades or so, clinical practice with regard to heparin treatment has changed from using UFH subcutaneously to the current standard of care of LMWH. For this reason, we consider reporting the subgroup results for both UFH and LMWH to be a more detailed description of the evidence and highly relevant for current clinical practice.
Where we identified substantial heterogeneity, we planned to investigate it using subgroup analyses and sensitivity analyses. We planned to consider whether an overall summary was meaningful, and if it was, used random‐effects analysis to produce it.
The risk of (recurrent) pregnancy complications may differ between different subgroups of women, such as previous placenta‐mediated complications, number of pregnancy losses, high‐ or low‐titre antibodies and positive or negative lupus anticoagulant (LAC) antibodies. For this reason, the following subgroup analyses were pre‐specified.
Previous placenta‐mediated complication (pre‐eclampsia; intrauterine growth restriction or placental abruption, or both) versus no previous placenta‐mediated complication
Two versus three or more pregnancy losses (which do not have to be consecutive)
High‐titre antibodies versus low‐titre antibodies
Positive lupus anticoagulant (LAC) antibodies versus negative LAC antibodies
We planned to use the primary outcome (live birth) in subgroup analyses.
We planned to assess subgroup differences by interaction tests available within RevMan 5 (RevMan 2014). We planned to report the results of subgroup analyses quoting the Chi² statistic and P value, and the interaction test I² statistic value.
Sensitivity analysis
Where possible, we carried out sensitivity analyses to explore the effect of use of the full Sapporo criteria for APS, with studies not using the full criteria excluded from the analyses; and trial quality (including quasi‐randomised trials), assessed by random sequence generation and concealment of allocation, with studies assessed as high risk of bias on these domains being excluded from the analyses. Sensitivity analyses were limited to the primary outcome.
In future updates, where cluster‐randomised trials are included, we plan to carry out sensitivity analyses to explore the effects of variation in intra‐cluster correlation coefficient (ICC) values and in the randomisation unit (i.e. individual versus cluster trials).
Summary of findings and assessment of the certainty of the evidence
The certainty of evidence was assessed using the GRADE approach as outlined in the GRADE handbook in order to assess the certainty of the body of evidence relating to the following outcomes for the two main comparisons.
Aspirin versus placebo
Heparin plus aspirin versus aspirin alone
Primary outcomes
Live birth
Secondary outcomes
For the mother
Pre‐eclampsia (definition according to original study)
Adverse events in the mother (definitions according to original study: (A) bleeding, (B) heparin‐induced thrombocytopenia, (C) allergic reactions)
Venous thromboembolism
Arterial thromboembolism
Pregnancy loss
For the child
Preterm delivery of a live infant (before 37 weeks, 24 to 28 weeks, 28 to 32 weeks and 32 to 37 weeks)
Intrauterine growth restriction (definition according to original study)
Adverse events in the child (definitions according to original study: (A) congenital malformations, (B) neonatal bleeding)
We used the GRADEpro Guideline Development Tool to import data from RevMan 5 (RevMan 2014) in order to create 'Summary of findings' tables for comparison 1 (aspirin versus placebo) and comparison 2 (heparin plus aspirin versus aspirin alone). A summary of the intervention effect and a measure of certainty for each of the above outcomes in these comparisons was produced using the GRADE approach. The GRADE approach uses five considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the certainty of the body of evidence for each outcome. The evidence can be downgraded from 'high certainty' by one level for serious (or by two levels for very serious) limitations, depending on assessments for risk of bias, indirectness of evidence, serious inconsistency, imprecision of effect estimates or potential publication bias.
Results
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies.
Results of the search
See: Figure 1
1.
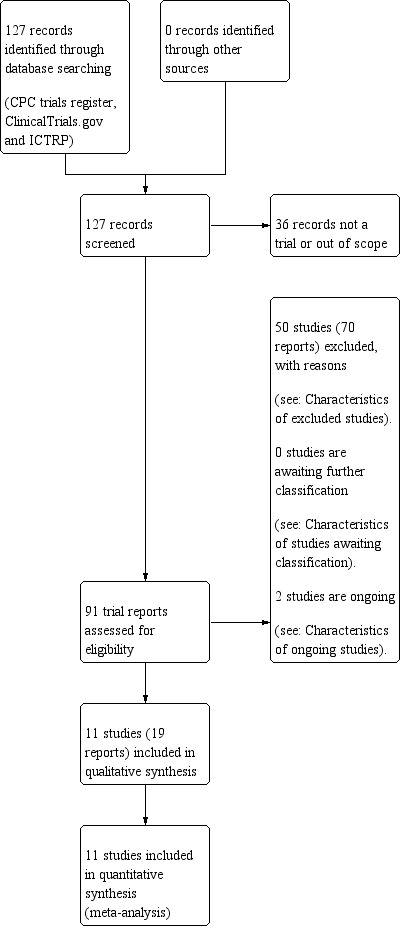
Study flow diagram.
As of June 2019, the search strategy identified 127 records through database screening. The title and abstract screening identified 91 potentially eligible citations. The full‐text screening of these 91 citations identified 11 eligible randomised controlled trials published as full reports (Alalaf 2012; Bao 2017; Farquharson 2002; Fouda 2010; Fouda 2011; Kutteh 1996a; Kutteh 1996b; Laskin 2009; Pattison 2000; Rai 1997; Stephenson 2004. We identified two registered, but unpublished trials (Abdelhafez 2014; Rodger 2017). We did not identify any cluster‐randomised trials that met our inclusion criteria. None of the studies only published as abstracts were included, as insufficient data were available to determine eligibility.
Included studies
A total of 1672 women were enrolled in the 11 included trials; nine were randomised controlled trials and two were quasi‐randomised controlled trials (Kutteh 1996a; Kutteh 1996b). The study designs, inclusion and exclusion criteria and interventions are shown in the Characteristics of included studies tables. The studies were conducted in the USA, Canada, the UK, China, New Zealand, Iraq and Egypt. One included trial involved 1015 women (Bao 2017), all other included trials had considerably lower numbers of participants (i.e. 141 women or fewer).
One study compared aspirin with placebo (n = 40) (Pattison 2000). No study compared heparin alone with placebo and we did not identify trials with a no treatment comparator arm during pregnancy. Five studies explored the efficacy of heparin plus aspirin with aspirin alone; two studies evaluated the combination of unfractionated heparin (UFH) plus aspirin in comparison with aspirin alone (n = 140) (Kutteh 1996a; Rai 1997), three studies used low‐molecular weight heparin (LWMH) plus aspirin and compared this to aspirin alone (n = 1155) (Bao 2017; Farquharson 2002; Laskin 2009). One trial compared LMWH with aspirin (n = 141) (Alalaf 2012). Two trials compared LMWH with UFH, both combined with aspirin (n = 86) (Fouda 2011; Stephenson 2004). Two studies investigated the combination of different doses of heparin plus aspirin; one compared high‐dose UFH with low‐dose UFH, both combined with aspirin (n = 50) (Kutteh 1996b), whereas the other study compared high‐dose LMWH with low‐dose LWMH, both combined with aspirin (n = 60) (Fouda 2010).
Characteristics of participants
The characteristics of the trial participants are summarised in Table 3, though these were not completely reported in all studies. One trial also included participants who did not have antiphospholipid antibodies (aPL) (Laskin 2009) and we included only data from the subgroup of participants with aPL from this study (n = 42/88) (Laskin 2009); we contacted the authors to provide data on the secondary outcomes for the subgroup of aPL‐positive participants, but we did not receive a reply.
1. Summary of participants in the studies.
|
Total No. |
Participants per group |
Mean age (years) |
Mean total prior miscarriages/woman |
aCL IgM | aCL IgG | LAC | aCL and LAC | aβ2GPI | |||||||||
| Studies | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | B | |
| Alalaf 2012 | 141 | 80 | 61 | 31.4 ± 5.8 | 30.6 ± 6.3 | 3.3 ± 1.7 | 3.4 ± 1.8 | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Bao 2017 | 1015 | 497 | 518 | median 35 (25‐47) | median 34 (24‐43) | median 4 (2‐11) | median 3 (2‐8) | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Farquharson 2002 | 98 | 51 | 47 | 33 ± 4.8 | 33 ± 4.9 | 3 ± 0.8 | 3 ± 0.9 | 3/51 | 5/47 | 6/51 | 2/47 | 23/51 | 18/47 | 18/51 | 22/47 | NA | NA |
| Fouda 2010 | 60 | 30 | 30 | 27.1 ± 3.7 | 28.9 ± 4.2 | 4.0 ± 1.2 | 4.1 ± 1.1 | 4/30 | 5/30 | 8/30 | 6/30 | 10/30 | 9/30 | 8/30 | 10/30 | NA | NA |
| Fouda 2011 | 60 | 30 | 30 | 27.5 ± 3.2 | 28.6 ± 3.5 | 4.4 ± 1.2 | 4.2 ± 1.2 | 5/30 | 8/30 | 7/30 | 5/30 | 12/30 | 10/30 | 6/30 | 7/30 | NA | NA |
| Kutteh 1996a | 50 | 25 | 25 | 33.2 ± 4.2 | 33.5 ± 5.8 | 3.9 ± 1.4 | 3.7 ± 1.0 | 6/25 | 5/25 | NR | NR | NA | NA | NA | NA | NA | NA |
| Kutteh 1996b | 50 | 25 | 25 | 33.3 ± 4.2 | 33.2 ± 3.9 | 3.9 ± 1.4 | 3.6 ± 1.0 | NR | NR | NR | NR | NA | NA | NA | NA | NA | NA |
| Laskin 2009* | 42 | 22 | 20 | 34.6 ± 3.9 | 33.8 ± 4.1* | NR | NR | NR | NR | NR | NR | NR | NR | NR | NR | NA | NA |
| Pattison 2000 | 40 | 20 | 20 | 31 ± 4.5 | 30.9 ± 3.9 | NR | NR | 6/20 | 3/20 | 6/20 | 9/20 | 4/20 | 5/20 | 3/20 | 3/20 | NA | NA |
| Rai 1997 | 90 | 45 | 45 | median 32 (23‐40) |
median 34 (22‐44) |
median 4 (3‐15) |
median 4 (3‐8) |
0/45 | 1/45 | 3/45 | 4/45 | 40/45 | 34/45 | 6/45 | 2/45 | NA | NA |
| Stephenson 2004** | 26 | 13 | 13 | 34 (27‐40) | 34 (28‐43) | 3.8 (3‐7) | 3.9 (3‐7) | 4/14 | 11/14 | 11/14 | 7/14 | 6/14 | 3/14 | 4/14 | 2/14 | NA | NA |
aβ2GPI: anti‐β2‐glycoprotein‐I antibodies; aCL: anticardiolipin antibodies,aPL: antiphospholipid antibodies; LAC: lupus anticoagulant,.LMWH: low‐molecular weight heparin; NA: outcome not assessed;NR: outcome not reported,UFH: unfractionated heparin
* mean age in years for the entire study population (N = 88), not separately reported for the subgroup with positive aPL specifically.
** aPL profiles given for entire study population (N = 28), not separately reported the subgroup of patients who conceived and were subsequently randomised.
- Alalaf 2012: group A = LMWH, group B = aspirin
- Bao 2017: group A = LMWH + aspirin, group B = aspirin
- Farquharson 2002: group A = LMWH + aspirin, group B = aspirin
- Fouda 2010: group A = high‐dose LMWH plus aspirin, group B = low‐dose LMWH plus aspirin;
- Fouda 2011: group A = LMWH + aspirin, group B = UFH + aspirin
- Kutteh 1996a: group A = UFH + aspirin, group B = aspirin
- Kutteh 1996b: group A = high‐dose UFH plus aspirin, group B = low‐dose UFH + aspirin
- Laskin 2009: group A = LMWH + aspirin, group B = aspirin
- Pattison 2000: group A = aspirin, group B = placebo
- Rai 1997: group A = UFH + aspirin, group B = aspirin
- Stephenson 2004: group A = LMWH + aspirin, group B = UFH + aspirin
Prior pregnancy losses
The mean number of previous pregnancy losses in the studies ranged from 3 to 4.3 (Alalaf 2012; Farquharson 2002; Fouda 2010;Fouda 2011; Kutteh 1996a; Kutteh 1996b; Rai 1997; Stephenson 2004). In eight trials, participants met the clinical criteria for antiphospholipid syndrome (APS) with three or more early miscarriages. Three trials included women with two or more consecutive pregnancy losses (Alalaf 2012; Bao 2017; Laskin 2009). Previous pregnancy losses concerned mostly early pregnancy losses, but less than half of the included studies specified this (Kutteh 1996a; Kutteh 1996b; Laskin 2009; Pattison 2000; Rai 1997). Full details on pregnancy losses are provided in the characteristics of included studies (Included studies).
Presence of antiphospholipid antibodies (aPL)
All trials included participants with persistent presence of aPL, but the time‐frame between tests differed per study. Two trials included patients with aPL tested at least six weeks apart (Farquharson 2002; Stephenson 2004); three trials with tests at least eight weeks apart (Alalaf 2012; Laskin 2009; Rai 1997); three trials with tests at least 12 weeks apart (Bao 2017; Fouda 2010; Fouda 2011); and three trials did not mention the time‐frame (Kutteh 1996a; Kutteh 1996b; Pattison 2000). None of the included trials reported women with aβ2‐GPI antibodies. Table 3 lists the aPL‐profiles for trial participants.
Dose and type of aspirin and heparin
Low‐dose aspirin was used in all trials. In six trials a dose of aspirin of 75 mg/day was used (Bao 2017; Farquharson 2002; Fouda 2010; Fouda 2011; Pattison 2000; Rai 1997), in four trials the dose was 81 mg/day (Kutteh 1996a; Kutteh 1996b; Laskin 2009; Stephenson 2004), and in one trial the dose used was 100 mg/day (Alalaf 2012). The types of LMWH included bemiparin in a dose of 2500 IU/day (Alalaf 2012), enoxaparin in a dose of 20 mg or 40 mg per day (Fouda 2010, Fouda 2011), dalteparin in a dose of 5000 IU/day (Laskin 2009) or 2500 IU/day (Stephenson 2004), nadroparin in a dose of 4100 IU/day (Bao 2017), and in one trial the type of LMWH was not mentioned, but administered in a dose of 5000 IU/day (Farquharson 2002). The dose of UFH was 5000 IU twice daily in both the trial of Kutteh 1996a and the trial of Stephenson 2004, with the latter with increasing the dose of administered heparin (LMWH or UFH) during the trial. One trial compared a lower and a higher dose of UFH (Kutteh 1996b); in the high‐dose UFH group, the doses of heparin were adjusted to maintain 1.2 to 1.5 times the baseline partial thromboplastin time (PTT) and were increased by 1000 U/dose weekly until the desired range was achieved, whereas in the low‐dose UFH group the dose of heparin was adjusted to maintain the PTT at the upper limits of the normal range in the reference laboratory.
Initiation and duration of treatment
There was a wide variation in treatment initiation and duration between trials. One trial randomised women to aspirin, which was started preconceptionally and continued upon pregnancy confirmation or to LMWH commencing at the confirmation of pregnancy, continuing either treatment until 36 weeks of gestation (Alalaf 2012). In one trial, participants were randomised before 12 weeks of gestation, with a mean gestation age of 6.7 weeks at randomisation, and received treatment until delivery (Farquharson 2002). In two trials, aspirin was started preconceptionally up to 36 gestational weeks, with a heparin (LMWH or UFH) started when the serum pregnancy test became positive until delivery, when it was switched to twice‐daily UFH (Fouda 2010; Fouda 2011). Two trials initiated aspirin preconceptionally in all participants and at the first confirmed pregnancy test, patients were instructed to continue aspirin alone or to add subcutaneous injections of heparin twice‐daily (Kutteh 1996a), or all participants were started on heparin injections (Kutteh 1996b) until full term. Four trials initiated treatment at the first confirmation of pregnancy and treatment was continued until 34 weeks of gestation (Rai 1997), 35 weeks of gestation (Bao 2017; Laskin 2009) or study duration (Pattison 2000). One trial started aspirin before conception, with heparin (LMWH or UFH) started in the luteal phase for a maximum of three cycles until delivery and continued postpartum in a prophylactic dose (Stephenson 2004).
Placebo
One trial randomised between aspirin and placebo (Pattison 2000). No studies were identified that compared heparin with placebo or aspirin and/or heparin with no treatment.
Outcomes reported
The reported outcomes per included trial are summarised in Table 4. Our primary outcome live birth was reported in all studies, in contrast to the secondary outcomes that were only reported in a subset of included trials. All included trials contributed data to at least one comparison in the meta‐analysis.
2. Summary of reported outcomes.
| Live birth | Pre‐eclampsia | Maternal bleeding |
Thrombo cytopenia |
Allergic Reactions |
VTE ATE | Preterm delivery | IUGR |
Congenital Malformations |
Neonatal Bleeding |
|||||||||||
| Studies | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | B | A | B |
| Alalaf 2012 | 69/80 | 44/61 | 1/69 | 0/44 | 5/81 | NA | NA | NA | NA | NA | 0/80 | 0/61 | 3/69 | 2/44 | NA | NA | NA | NA | NA | NA |
| Bao 2017 | 449/497 | 363/518 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Farquharson 2002 | 40/51 | 34/47 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | 2/40 | 4/34 | NA | NA | NA | NA | NA | NA |
| Fouda 2010 | 23/30 | 21/30 | 3/30 | 2/30 | 0/30 | 0/30 | 0/30 | 0/30 | NA | NA | 0/30 | 0/30 | 3/23 | 2/21 | 2/30 | 1/30 | 0/23 | 0/21 | 0/23 | 0/21 |
| Fouda 2011* | 24/30 | 20/30 | 2/24 | 1/20 | 0/30 3/30 |
0/30 3/30 |
0/30 | 0/30 | 0/30 | 1/30 | 0/30 | 0/30 | 3/24 | 2/20 | 1/24 | 2/20 | 0/24 | 0/20 | 0/24 | 0/20 |
| Kutteh 1996a** | 20/25 | 11/25 | 2/20 | 1/11 | 0/20 3/20 |
0/11 1/11 |
0/25 | 0/25 | NA | NA | 0/25 | 0/25 | 3/20 | 1/11 | 3/20 | 1/11 | NA | NA | NA | NA |
| Kutteh 1996b** | 20/25 | 19/25 | 2/20 | 1/19 | 0/20 3/20 |
0/19 4/19 |
0/25 | 0/25 | NA | NA | NA | NA | 3/20 | 1/19 | 3/20 | 0/19 | NA | NA | NA | NA |
| Laskin 2009 | 17/22 | 15/20 | NA | NA | NA | NA | NA | NA | NA | NA | 0/22 | 0/20 | NA | NA | NA | NA | NA | NA | NA | NA |
| Pattison 2000 | 16/20 | 17/20 | 3/16 | 3/17 | 9/20 | 7/20 | NA | NA | NA | NA | NA | NA | 2/16 | 0/17 | 1/16 | 4/17 | 1/16 | 1/17 | NA | NA |
| Rai 1997 | 32/45 | 19/45 | 0/32 | 1/19 | 0/45 | NA | 0/45 | NA | 0/45 | NA | 0/45 | 0/45 | 8/32 | 4/19 | 3/32 | 1/19 | 0/32 | 0/19 | NA | NA |
| Stephenson 2004 | 9/13 | 4/13 | 1/13 | 0/13 | 0/13 | 0/13 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
ATE: arterial thromboembolism;LMWH: low‐molecular weight heparin; NA: outcome not assessed; UFH: unfractionated heparin; VTE: venous thromboembolism.
- Alalaf 2012: group A = LMWH, group B = aspirin
- Bao 2017: group A = LMWH + aspirin, group B = aspirin
- Farquharson 2002: group A = LMWH + aspirin, group B = aspirin
- Fouda 2010: group A = high‐dose LMWH plus aspirin, group B = low‐dose LMWH plus aspirin
- Fouda 2011: group A = LMWH + aspirin, group B = UFH + aspirin, *no bleeding in either group, subcutaneous bruising 3/30 in both group
- Kutteh 1996a: group A = UFH + aspirin, group B = aspirin; **no major bleeding, reports are minor bleeding events
- Kutteh 1996b: group A = high‐dose UFH plus aspirin, group B = low‐dose UFH + aspirin; **no major bleeding events, reports are minor bleeding events
- Laskin 2009: group A = LMWH + aspirin, group B = aspirin
- Pattison 2000: group A = aspirin, group B = placebo
- Rai 1997: group A = UFH + aspirin, group B = aspirin
- Stephenson 2004: group A = LMWH + aspirin, group B = UFH + aspirin
Live birth rate: all 11 included trials reported our primary outcome live birth.
Pre‐eclampsia: eight trials reported on pre‐eclampsia (Alalaf 2012; Fouda 2010; Fouda 2011; Kutteh 1996a; Kutteh 1996b; Pattison 2000; Rai 1997; Stephenson 2004).
Maternal bleeding: eight trials mentioned maternal bleeding rates; three trials reported on postpartum haemorrhage or vaginal bleeding during pregnancy (Fouda 2010; Fouda 2011; Stephenson 2004), two trials reported on both major and minor maternal bleeding (Kutteh 1996a; Kutteh 1996b), one trial reported any maternal bleeding without specification (Pattison 2000) and two trials reported bruising at injection site in case of heparin use (Alalaf 2012, Fouda 2010).
Heparin‐induced thrombocytopenia (HIT): 10 of 11 trials had heparin as an intervention arm and five trials reported on thrombocytopenia (Fouda 2010; Fouda 2011; Kutteh 1996a; Kutteh 1996b; Rai 1997).
Allergic reactions: one trial reported allergic reactions to study medication (Fouda 2011).
Venous thromboembolism (VTE): six trials reported on thromboembolic events, without discerning arterial or venous origin (Alalaf 2012; Fouda 2010; Fouda 2011; Kutteh 1996a; Laskin 2009; Rai 1997).
Arterial thromboembolism (ATE): six trials reported on thromboembolic events, without discerning arterial or venous origin (Alalaf 2012; Fouda 2010; Fouda 2011; Kutteh 1996a; Laskin 2009; Rai 1997).
Preterm delivery of a live infant: eight of 11 trials reported on preterm delivery of a live infant, defined as delivery between 32 to 37 weeks of gestation (Alalaf 2012), between 30 to 36 weeks or before 30 weeks (Farquharson 2002), between 24 to 37 weeks (Pattison 2000) or preterm was not specifically defined (Fouda 2010; Fouda 2011; Kutteh 1996a; Kutteh 1996b; Rai 1997).
Intrauterine growth restriction (IUGR): IUGR was reported in six of 11 studies (Fouda 2010; Fouda 2011; Kutteh 1996a; Kutteh 1996b; Pattison 2000; Rai 1997).
Congenital malformations: four trials reported on congenital malformations (Fouda 2010; Fouda 2011; Pattison 2000; Rai 1997).
Neonatal bleeding: two trials reported on neonatal bleeding (Fouda 2010; Fouda 2011).
Trial registries and dates
Only two of 11 trials had registered their study in a clinical trials registry (Laskin 2009; Fouda 2011), as at the time of publication for most of the other studies clinical trials registries were not operational. Three relatively more recent trials were published, but had not registered their study in a trials registry (Alalaf 2012; Bao 2017; Fouda 2010). More than half of the included studies were published before 2005. Three studies did not report on the recruitment period (Kutteh 1996a; Kutteh 1996b; Rai 1997), with one study only mentioning the overall recruitment time being 39 months (Pattison 2000).
Funding sources
Two trials were funded by governmental and non‐governmental research grants from the UK (Farquharson 2002; Rai 1997), and two by governmental and non‐governmental grants from Canada (Laskin 2009; Stephenson 2004). One study reported supply of study medication and sponsorship from a pharmaceutical company (Laskin 2009). One trial reported financial support by governmental research grants from China (Bao 2017). One study specifically thanked a pharmaceutical company for donation of study medication, but did not clarify the relationship (Stephenson 2004). Four trials did not mention any support (Fouda 2010; Kutteh 1996a; Kutteh 1996b; Pattison 2000).
Declarations of Interest
Five trials explicitly declared no conflict of interest (Alalaf 2012; Fouda 2010; Fouda 2011; Rai 1997; Stephenson 2004) and the other six trials did not state if any interests existed (Bao 2017; Farquharson 2002; Kutteh 1996a; Kutteh 1996b; Pattison 2000; Laskin 2009).
Excluded studies
Reasons for exclusion are stated in the Characteristics of excluded studies table. Eight studies were excluded based on abstract only, as full text could not be retrieved and information in the abstract was insufficient to critically evaluate if inclusion criteria were met (Bu 2009; Dendrinos 2007; Guo 2013; Malathi 2011; Malinowski 2003; Mankuta 1999; Quenby 1992; Zhou 2012). On obtaining the full papers, three trials were found to be non‐randomised (Mohamed 2014; Noble 2005; Shefras 1995) and three trials had a different study design (Gibbins 2018; De Veciana 2001; Kahwa 2006). Eighteen trials considered a different study population, such as women without recurrent miscarriage or no persistent presence of aPL (Agarwal 2018; Cowchock 1997; De Vries 2012; Goel 2006; Golding 1998; Gris 1995; Ismail 2016; Kaaja 1993; Kaandorp 2010; Kahwa 2006; Mahmoud 2004; Radin 2017; Saad 2014; Tulppala 1997; Schisterman 2014; Vahid 1999; van Hoorn 2016; Visser 2011). Sixteen trials evaluated a different intervention or aspirin and/or heparin in combination with for instance intravenous immunoglobulin (IVIG) or prednisone (Branch 2000; Carta 2005; Christiansen 1995; Cowchock 1992; Dendrinos 2009; Eid 2019; Fu 2004; Geva 1998; Laskin 1997; Rai 2005; Shu 2002; Silver 1993; Tang 2012; Triolo 2003; Vaquero 2001; Xiao 2013). Two studies investigated a different outcome; thrombotic sequelae after 20 years (Clark 2009) and drug exposure throughout pregnancy (Ensom 2004), respectively.
Risk of bias in included studies
See Figure 2; Figure 3 for a summary of risk of bias in the included trials.
2.

'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.

'Risk of bias' summary: review authors' judgements about each risk of bias item for each included study.
Allocation
Eight of 11 included trials, had low risk of bias for random sequence generation; seven trials used a computer‐generated list of study numbers or other adequate methods of randomisation (Bao 2017; Farquharson 2002; Fouda 2010; Fouda 2011; Laskin 2009; Pattison 2000; Rai 1997) and one trial used a random numbers table with block of 12 (Stephenson 2004). One trial used some form of alternation, but the method of randomisation, or what treatment allocation was based on (e.g. date of birth or medical record number) was not described and therefore risk of bias is regarded as high (Alalaf 2012). Two quasi‐randomised controlled trials used non‐random alternative assignment to treatment groups (Kutteh 1996a) or a sequential block of 25 allocated to one treatment group and a second sequential block of 25 allocated to the other treatment group (Kutteh 1996b) ‐ both trials were assessed as high risk of bias.
Allocation concealment was considered adequate and thus at low risk of bias in eight of 11 studies (Bao 2017; Farquharson 2002; Fouda 2010; Fouda 2011; Laskin 2009; Pattison 2000; Rai 1997; Stephenson 2004) that used central or telephone randomisation or sealed, opaque envelopes. Three trials were assessed as high risk of bias ‐ two quasi‐randomised controlled trials did not conceal allocation of treatment (Kutteh 1996a; Kutteh 1996b), and one trial did not report methods to conceal allocation (Alalaf 2012).
Blinding
In only one trial both participant and treating physician were unaware of the treatment allocation (Pattison 2000). All other trials did not blind or did not report on blinding participants and treatment providers. Few trials stated explicitly who performed the outcome assessment and whether outcome assessors were blinded to treatment allocation. However, the primary outcome live birth was considered unlikely to be influenced by knowledge of treatment allocation, therefore these trials were assessed as low risk of bias, as suggested in the Cochrane Handbook for Systematic Reviews for Interventions (Higgins 2017).
Incomplete outcome data
The majority of trials had low rates of attrition and reasons for exclusion or the numbers of participants included in each stage of the analysis were clearly reported. Three trials were considered to be at high risk of attrition bias (Alalaf 2012; Bao 2017; Pattison 2000). Alalaf 2012 did not report on exclusions, reasons for exclusions, numbers included in the analysis at each stage or loss to‐follow‐up. Bao 2017, did a per‐protocol analysis; 37 of the 1052 women receiving treatment failed to follow up or could not continue the trial due to change of intervention or specific allergies and outcomes of these censored participants were not reported; we assessed this trial as high risk of bias. In the trial by Pattison 2000, in each arm 5/25 (20%) of participants were excluded because of inappropriate inclusion. Analyses were performed with and without these participants but results from included participants only were published, not an analysis by intent‐to‐treat.
We assessed Kutteh 1996a and Kutteh 1996b as having an unclear risk of attrition bias; in those trials, exclusions, reasons for exclusion and numbers included in the analysis at each stage were not reported and it was unclear whether all evaluated participants started low‐dose aspirin before conception, prior to randomisation. Also, analysis by intent‐to‐treat and losses to follow‐up were unclear.
Selective reporting
Only a minority of trials were registered in a clinical trials registry and had a published study protocol (Fouda 2011; Laskin 2009), and we judged these trials to have a low risk of selective reporting. A clinical trial registry did not exist at the time of publication of some of the included studies (and for those more recently published studies, trial protocols were not available), and we therefore assessed reporting bias as unclear in eight unregistered studies, (Alalaf 2012; Bao 2017; Farquharson 2002; Fouda 2010; Kutteh 1996a; Kutteh 1996b; Rai 1997;Stephenson 2004). One trial excluded 20% of included participants due to inappropriate inclusion and performed analyses with and without these participants, but only provided results from included participants; we did not have sufficient information to assess whether all outcomes were reported and thus judged this trial to be at an unclear risk of reporting bias (Pattison 2000).
Other potential sources of bias
All of the included trials were assessed as low risk of other potential sources of bias.
Effects of interventions
Summary of findings 1. Aspirin compared to placebo for improving pregnancy outcomes in women with persistent antiphospholipid antibodies and recurrent pregnancy loss.
| Aspirin compared to placebo for improving pregnancy outcomes in women with persistent antiphospholipid antibodies and recurrent pregnancy loss | ||||||
| Patient or population: improving pregnancy outcomes in women with persistent antiphospholipid antibodies and recurrent pregnancy loss Setting: Intervention: aspirin Comparison: placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with Aspirin | |||||
| Live birth | Study population | RR 0.94 (0.71 to 1.25) | 40 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 1 2 | ||
| 850 per 1,000 | 799 per 1,000 (603 to 1,000) | |||||
| Pre‐eclampsia | Study population | RR 1.06 (0.25 to 4.52) | 33 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 1 2 | ||
| 176 per 1,000 | 187 per 1,000 (44 to 798) | |||||
| Adverse events in the mother ‐ Bleeding | Study population | RR 1.29 (0.60 to 2.77) | 40 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 1 2 | ||
| 350 per 1,000 | 451 per 1,000 (210 to 969) | |||||
| Venous thromboembolism | Not reported | |||||
| Arterial thromboembolism | Not reported | |||||
| Pregnancy loss | Study population | RR 1.33 (0.34 to 5.21) | 40 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 1 2 | ||
| 150 per 1,000 | 200 per 1,000 (51 to 782) | |||||
| Preterm delivery of a live infant | 2/16 in the aspirin group and 0/17 in the placebo group had a preterm delivery of a live infant | RR 5.29 (0.27 to 102.49) | 33 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 1 2 | ||
| Intrauterine growth restriction | Study population | RR 0.27 (0.03 to 2.13) | 33 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 1 2 | ||
| 235 per 1,000 | 64 per 1,000 (7 to 501) | |||||
| Adverse events in the child ‐ Congenital malformations | Study population | RR 1.06 (0.07 to 15.60) | 33 (1 RCT) | ⊕⊝⊝⊝ VERY LOW 1 2 | ||
| 59 per 1,000 | 62 per 1,000 (4 to 918) | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RCT: randomised controlled trial; RR: Risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1 Downgraded one level due to serious risk of selection and attrition bias
2 Downgraded two levels due to very serious imprecision: few participants and wide confidence intervals crossing the line of no effect
Summary of findings 2. Heparin plus aspirin compared to aspirin for improving pregnancy outcomes in women with persistent antiphospholipid antibodies and recurrent pregnancy loss.
| Heparin plus aspirin compared to aspirin for improving pregnancy outcomes in women with persistent antiphospholipid antibodies and recurrent pregnancy loss | ||||||
| Patient or population: women with persistent antiphospholipid antibodies and recurrent pregnancy loss Setting: mix of multicentre and single‐centre trials, based in the UK, the USA, Canada and China Intervention: heparin (UFH or LMWH) and aspirin Comparison: aspirin | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with Aspirin | Risk with Heparin (UFH or LMWH) and aspirin | |||||
| Live birth | Study population | RR 1.27 (1.09 to 1.49) | 1295 (5 RCTs) | ⊕⊕⊝⊝ LOW 1 2 | Subgroup analysis: UFH + aspirin v aspirin: RR 1.74 (1.28 to 2.35) LMWH + aspirin v aspirin: RR 1.20 (1.04 to 1.38) |
|
| 675 per 1.000 | 857 per 1.000 (736 to 1.000) | |||||
| Pre‐eclampsia | Study population | RR 0.57 (0.10 to 3.14) |
82 (2 RCTs) | ⊕⊕⊝⊝ LOW 3 4 | ||
| 67 per 1.000 | 48 per 1.000 (7 to 209) | |||||
| Adverse events in the mother ‐ Bleeding | Study population | RR 1.65 (0.19 to 14.03) | 31 (1 RCT) | ⊕⊕⊝⊝ LOW 45 | ||
| 91 per 1.000 | 150 per 1.000 (17 to 1.000) | |||||
| Adverse events in the mother ‐ Heparin‐induced thrombocytopenia | 0/70 women in the heparin plus aspirin group had heparin‐induced thrombocytopenia, compared with 0/70 in the aspirin only group. | 140 (2 RCTs) |
‐ | |||
| Adverse events in the mother ‐ Allergic reactions | 0/45 women in the heparin plus aspirin group had allergic reactions, compared with 0/45 in the aspirin only group. | 90 (1 RCT) | ‐ | |||
| Venous thromboembolism | 0/92 women in the heparin plus aspirin group had venous thromboembolism, compared with 0/90 in the aspirin only group. | 182 (3 RCTs) |
‐ | |||
| Arterial thromboembolism | 0/92 women in the heparin plus aspirin group had venous thromboembolism, compared with 0/90 in the aspirin only group. | 182 (3 RCTs) |
‐ | |||
| Pregnancy loss | Study population | RR 0.48 (0.32 to 0.71) | 1295 (5 RCTs) | ⊕⊕⊝⊝ LOW 2 5 | ||
| 325 per 1.000 | 156 per 1.000 (104 to 231) | |||||
| Preterm delivery of a live infant | Study population | RR 0.93 (0.42 to 2.07 |
156 (3 RCTs) | ⊕⊝⊝⊝ VERY LOW 3 6 | ||
| 141 per 1.000 | 131 per 1.000 (59 to 291) | |||||
| Intrauterine growth restriction | Study population | RR 0.85 (0.33 to 2.19) |
151 (3 RCTs) | ⊕⊝⊝⊝ VERY LOW 3 6 | ||
| 125 per 1.000 | 106 per 1.000 (41 to 274) | |||||
| Adverse events in the child ‐ Congenital malformations | 0/32 infants the heparin plus aspirin group had congenital malformations, compared with 0/19 in the aspirin only group. | 51 (1 RCT) | ‐ | |||
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; LMWH: low‐molecular weight heparin; RR: Risk ratio; UFH: unfractionated heparin. | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
1 Downgraded one level due to serious risk of bias for limitations (selection and attrition bias)
2 Downgraded one level due to serious inconsistency: heterogeneity in interventions (I² > 45%)
3 Downgraded one level due to serious risk of bias for limitations (selection and reporting bias)
4 Downgraded one level due to serious imprecision: few participants and wide confidence interval crossing the line of no effect
5 Downgraded one level due to serious risk of bias for limitations (selection, attrition and reporting bias)
6 Downgraded two levels due to very serious imprecision: few participants and wide confidence interval crossing the line of not effect
Eleven trials (1672 women) met the inclusion criteria and all trials contributed data to our analyses. We present five different comparisons, with meta‐analysis only possible in three of our comparisons; comparison 2 (heparin [UFH or LMWH] plus aspirin versus aspirin alone), comparison 4 (LMWH plus aspirin versus UFH plus aspirin) and comparison 5 (higher dose heparin [LMWH or UFH] plus aspirin versus lower dose heparin [LMWH or UFH] plus aspirin).
Comparison 1: Aspirin versus placebo
Primary outcome ‐ Live birth
We are uncertain if there is any difference in live birth rates when comparing aspirin with placebo (risk ratio (RR) of 0.94, 95% confidence interval (CI) 0.71 to 1.25, 1 trial, 40 women; very low‐certainty evidence; Analysis 1.1; Table 1). In one small trial (Pattison 2000) there were similar numbers of live births in the aspirin group (16/20) and the placebo group (17/20).
1.1. Analysis.

Comparison 1: Aspirin versus placebo, Outcome 1: Live birth
Secondary outcomes (maternal)
Pre‐eclampsia
We are uncertain if there is any difference in the risk of pre‐eclampsia between aspirin and placebo (Pattison 2000; RR 1.06, 95% CI 0.25 to 4.52; 1 trial, 33 women; very low‐certainty evidence; Analysis 1.2; Table 1).
1.2. Analysis.

Comparison 1: Aspirin versus placebo, Outcome 2: Pre‐eclampsia
Adverse events in the mother (definitions according to original study: (A) bleeding, (B) heparin‐induced thrombocytopenia, (C) allergic reactions)
It is uncertain if there is any difference in the risk of bleeding events during pregnancy when aspirin was compared with placebo (Pattison 2000; RR 1.29, 95% CI 0.60 to 2.77; 1 trial, 40 women; very low‐certainty evidence; Analysis 1.3; Table 1). Heparin‐induced thrombocytopenia was not reported, as heparin was not evaluated in this trial; allergic reactions to aspirin or placebo were not reported either.
1.3. Analysis.

Comparison 1: Aspirin versus placebo, Outcome 3: Adverse events in the mother
Venous thromboembolism
Not reported.
Arterial thromboembolism
Not reported
Pregnancy loss
We are very uncertain if there is any difference in the risk of pregnancy loss when comparing aspirin with placebo (RR 1.33, 95% CI 0.34 to 5.21; 40 women; 1 study; very low‐certainty evidence; Table 1; Analysis 1.7).
1.7. Analysis.

Comparison 1: Aspirin versus placebo, Outcome 7: Pregnancy loss
Secondary outcomes (for the child)
Preterm delivery of a live infant
It is uncertain if there is any difference between aspirin and placebo in the risk of preterm delivery did not occur in the 17 placebo‐treated women and in two of 16 women receiving aspirin (Pattison 2000; RR 5.29, 95% CI 0.27 to 102.49; 1 trial, 33 children; very low‐certainty evidence; Analysis 1.4; Table 1).
1.4. Analysis.

Comparison 1: Aspirin versus placebo, Outcome 4: Preterm delivery of a live infant
Intrauterine growth restriction (IUGR)
It is uncertain if there is any difference in the risk of IUGR between women receiving placebo or aspirin during pregnancy, the RR for IUGR was 0.27 (95% CI 0.03 to 2.13; 1 trial, 33 children; very low‐certainty evidence; Analysis 1.5; Table 1),
1.5. Analysis.

Comparison 1: Aspirin versus placebo, Outcome 5: Intrauterine growth restriction
Adverse events in the child (definitions according to original study: (A) congenital malformations, (B) neonatal bleeding)
It is uncertain if there is any difference between aspirin and placebo in the risk of adverse events. One child in both treatment groups was diagnosed with a congenital malformation in the trial of Pattison 2000, but malformations were not specified (RR 1.06; 95% CI 0.07 to 15.60; 1 trial, 33 children; very low‐certainty evidence; Analysis 1.6; Table 1). Neonatal bleeding was not reported.
1.6. Analysis.

Comparison 1: Aspirin versus placebo, Outcome 6: Adverse events in the child
Comparison 2: Heparin plus aspirin versus aspirin alone
Primary outcome ‐ Live birth
Five studies (1295 women) which compared heparin (either UFH or LMWH) combined with aspirin to aspirin alone, were included in a random‐effects meta‐analysis for the primary outcome live birth. Heparin plus aspirin may increase the number of live births compared with aspirin alone (RR 1.27; 95% CI 1.09 to 1.49; Tau² = 0.01; Chi² = 7.71, df = 4 (P = 0.10); I² = 48%; low‐certainty evidence; Analysis 2.1; Table 2).
2.1. Analysis.

Comparison 2: Heparin + aspirin versus aspirin, Outcome 1: Live birth
Subgroup analysis
We carried out a non‐pre‐specified subgroup analysis comparing trials that used LMWH and those that used UFH. There was evidence of a subgroup difference, as indicated by the subgroup interaction test (test for subgroup differences: Chi² = 4.74, df = 1 (P = 0.03), I² = 78.9%), possibly suggesting a larger treatment effect (benefit) with the use of UFH compared with LMWH. Both subgroups demonstrated higher rates of live birth when heparin was combined with aspirin as compared to aspirin alone (trials with LMWH: RR 1.20, 95% CI 1.04 to 1.38, 3 trials, 1155 women; trials with UFH: RR 1.74, 95% CI 1.28 to 2.35, 2 trials, 140 women; Analysis 2.1).
Farquharson 2002 reported 92.3% (12/13) pregnancy losses < 24 weeks of gestation and 7.7% (1/13) ≥ 24 weeks of gestation in the aspirin group, compared with all pregnancy losses in the LMWH plus aspirin group occurring before 24 weeks of gestation. All other included trials only reported total numbers of live birth.
We were not able to perform a subgroup analysis based on history of previous miscarriages, as three trials only included women with three or more recurrent pregnancy losses (Farquharson 2002; Kutteh 1996a; Rai 1997) and one trial explicitly stated that live birth did not differ between those with a history of two versus three pregnancy losses, without reporting numbers of participants (Laskin 2009). The largest trial did not report the numbers of previous miscarriages for participants in either group, but described that this number (two versus three versus more than four) had no significant association with live birth (Bao 2017). Subgroup analyses based on previous placenta‐mediated complications and positivity of lupus anticoagulant (LAC) antibodies were also not possible, since these were not specified for the primary outcome live birth, if reported at all. This also applied to a subgroup analysis based on aPL titers, with only one trial (Kutteh 1996a) reporting and no specification for live birth.
Sensitivity analysis
A sensitivity analysis excluding one quasi‐randomised trial with a higher risk of bias (Kutteh 1996a) did not materially change the treatment effect. We did not carry out a sensitivity analysis to explore the effect of the full Sydney criteria for antiphospholipid syndrome (APS). Technically none of the participants in four trials met the current laboratory criteria for APS (positivity on two separate occasions, tested at least 12 weeks apart; Miyakis 2006), as the time between testing varied between six weeks (Farquharson 2002) and eight weeks (Laskin 2009; Rai 1997), or was undefined (Kutteh 1996a). The participants in the largest trial met the laboratory criteria, but it was unclear if the clinical criteria were met, as the trial did not differentiate between previous early and late pregnancy loss (Bao 2017).
Secondary outcomes (maternal)
Pre‐eclampsia
It is uncertain if there is any difference in the risk of pre‐eclampsia comparing UFH plus aspirin with aspirin alone (RR 0.57 95% CI 0.10 to 3.14; 2 trials, 82 women; low‐certainty evidence; Analysis 2.2; Table 2).
2.2. Analysis.

Comparison 2: Heparin + aspirin versus aspirin, Outcome 2: Pre‐eclampsia
Adverse events in the mother (definitions according to original study: (A) bleeding, (B) heparin‐induced thrombocytopenia, (C) allergic reactions)
Major maternal bleeding was reported in one quasi‐randomised controlled trial, but did not occur in any participant (Kutteh 1996a). It is uncertain if there is any difference in the risk of minor bleeding in the mother (RR 1.65; 95% CI, 0.19 to 14.03; 1 trial, 31 women; low‐certainty evidence; Analysis 2.3), but this point estimate may not be reproduced in a larger sample size as implied by the wide confidence interval. Minor bleeding events, not further specified, did occur in 3/20 in the UFH and aspirin treated group, versus 1/11 in the aspirin only group. Data on heparin‐induced thrombocytopenia and allergic reactions were collected, but none of the participating women reported either.
2.3. Analysis.

Comparison 2: Heparin + aspirin versus aspirin, Outcome 3: Adverse events in the mother
Venous thromboembolism
Three trials reported venous thromboembolism but none of the study participants was diagnosed with a new event during study participation (Kutteh 1996a; Rai 1997; Laskin 2009) (Analysis 2.4)..
2.4. Analysis.

Comparison 2: Heparin + aspirin versus aspirin, Outcome 4: Venous thromboembolism
Arterial thromboembolism
Three trials reported venous thromboembolism but none of the study participants was diagnosed with a new event during study participation (Kutteh 1996a; Rai 1997; Laskin 2009) (Analysis 2.5)
2.5. Analysis.

Comparison 2: Heparin + aspirin versus aspirin, Outcome 5: Arterial thromboembolism
Pregnancy loss
Heparin plus aspirin may reduce the risk of pregnancy loss compared with aspirin alone (RR 0.48, 95% CI 0.32, 0.71; 1295 women; 5 studies; low‐certainty evidence; Table 2) (Analysis 2.9).
2.9. Analysis.

Comparison 2: Heparin + aspirin versus aspirin, Outcome 9: Pregnancy loss
Secondary outcomes (for the child)
Preterm delivery of a live infant
It is uncertain if there is any difference in the risk of preterm delivery comparing heparin plus aspirin to aspirin alone (RR 0.93, 95% CI 0.42 to 2.07; 3 trials, 156 women; very low‐certainty of evidence; Table 2; Farquharson 2002; Kutteh 1996a, Rai 1997; Analysis 2.6). Farquharson 2002 specified preterm delivery at gestational age between 30 to 36 weeks (1/40 and 3/34 in the heparin plus aspirin and aspirin alone groups, respectively) and delivery before 30 weeks (1/40 and 1/34 in the heparin plus aspirin and aspirin alone groups respectively).
2.6. Analysis.

Comparison 2: Heparin + aspirin versus aspirin, Outcome 6: Preterm delivery of a live infant
Intrauterine growth restriction
It is uncertain if there is any difference in the risk comparing heparin plus aspirin to aspirin alone (RR 0.85; 95% CI 0.33 to 2.19; 3 trials, 151 women; very low‐certainty of evidence; Table 2; Analysis 2.7).
2.7. Analysis.

Comparison 2: Heparin + aspirin versus aspirin, Outcome 7: Intrauterine growth restriction
Adverse events in the child (definitions according to original study: (A) congenital malformations, (B) neonatal bleeding)
The study of Rai 1997 comparing UFH plus aspirin with aspirin alone found no congenital malformations in either treatment group (Analysis 2.8). Neonatal bleeding was not reported in any of the trials comparing a combination of heparin and aspirin with aspirin treatment alone.
2.8. Analysis.

Comparison 2: Heparin + aspirin versus aspirin, Outcome 8: Adverse events in the child
Comparison 3: LMWH versus aspirin
Primary outcome ‐ Live birth
We identified one study in which LMWH was compared with aspirin (Alalaf 2012). Women in the group treated with LMWH had a higher live birth rate of 86.3%, compared with a 72.1% live birth rate in the women treated with aspirin (RR 1.20, 95% CI 1.00 to 1.43, 1 trial, 141 women; Analysis 3.1).
3.1. Analysis.

Comparison 3: LMWH versus aspirin, Outcome 1: Live birth
Secondary outcomes (maternal)
Pre‐eclampsia
One case of pre‐eclampsia occurred in the LMWH‐treated group, compared with none in the aspirin group (RR 1.93, 95% CI 0.08 to 46.31; Analysis 3.2).
3.2. Analysis.

Comparison 3: LMWH versus aspirin, Outcome 2: Pre‐eclampsia
Adverse events in the mother (definitions according to original study: (A) bleeding, (B) heparin‐induced thrombocytopenia, (C) allergic reactions)
Alalaf 2012 reported ecchymosis at injection site in 5 of 80 participants in the LMWH‐treated group (RR 8.42, 95% CI 0.47 to 149.41; Analysis 3.3, 1 trial, 141 women). Heparin‐induced thrombocytopenia and allergic reactions to either LMWH or aspirin were not reported.
3.3. Analysis.

Comparison 3: LMWH versus aspirin, Outcome 3: Adverse events in the mother
Venous thromboembolism
One trial reported zero events in both arms (Alalaf 2012) (Analysis 3.4).
3.4. Analysis.

Comparison 3: LMWH versus aspirin, Outcome 4: Venous thromboembolism
Arterial thromboembolism
One trial reported zero events in both arms (Alalaf 2012) (Analysis 3.5).
3.5. Analysis.

Comparison 3: LMWH versus aspirin, Outcome 5: Arterial thromboembolism
Pregnancy loss
In one trial there were 11/80 pregnancy losses in the LMHW arm compared to 17/61 in the aspirin arm (RR 0.49, 95% CI 0.25, 0.98; Analysis 3.7).
3.7. Analysis.

Comparison 3: LMWH versus aspirin, Outcome 7: Pregnancy loss
Secondary outcomes (for the child)
Preterm delivery of a live infant
The rate of preterm delivery was low and no clear difference was observed between treatment groups in the trial that compared heparin alone to aspirin alone (Alalaf 2012; RR 0.96, 95% CI 0.17 to 5.50, 1 trial, 113 women; Analysis 3.6).
3.6. Analysis.

Comparison 3: LMWH versus aspirin, Outcome 6: Preterm delivery of a live infant
Intrauterine growth restriction (IUGR)
IUGR was not reported as an outcome in the trial that compared heparin alone to aspirin alone (Alalaf 2012).
Adverse events in the child (definitions according to original study: (A) congenital malformations, (B) neonatal bleeding)
Neither congenital malformations nor neonatal bleeding were assessed in the trial by Alalaf 2012.
Comparison 4: LMWH plus aspirin versus UFH plus aspirin
Primary outcome ‐ Live birth
There was no clear difference between LMWH and aspirin versus UFH and aspirin for the outcome live birth (RR 1.44, 95% CI 0.80 to 2.62, 2 trials, 86 women; Tau² = 0.11; Chi² = 1.91, df = 1 (P = 0.17); I² = 48%; Analysis 4.1) (Fouda 2011; Stephenson 2004).
4.1. Analysis.

Comparison 4: LMWH+ aspirin versus UFH + aspirin, Outcome 1: Live birth
Secondary outcomes (maternal)
Pre‐eclampsia
Pre‐eclampsia occurred in three of 37 women in the LMWH plus aspirin treated group versus one woman of 33 in the UFH plus aspirin treated group (RR 2.09, 95% CI 0.33 to 13.22; Analysis 4.2; Fouda 2011; Stephenson 2004).
4.2. Analysis.

Comparison 4: LMWH+ aspirin versus UFH + aspirin, Outcome 2: Pre‐eclampsia
Adverse events in the mother (definitions according to original study: (A) bleeding, (B) heparin‐induced thrombocytopenia, (C) allergic reactions)
Both the trials by Fouda 2011 and Stephenson 2004 did not establish any major bleeding events in either treatment group, but three of 30 women in each treatment arm in the trial by Fouda 2011 reported subcutaneous bruises (RR 1.00, 95% CI 0.22 to 4.56, 2 trials, 206 women; Analysis 4.3; Fouda 2011; Stephenson 2004). Data on heparin‐induced thrombocytopenia and allergic reactions were collected, but none of the participating women reported in the studies by Fouda 2010;Fouda 2011 reported either.
4.3. Analysis.

Comparison 4: LMWH+ aspirin versus UFH + aspirin, Outcome 3: Adverse events in the mother
Venous thromboembolism
One trial reported zero venous thromboembolism events in both arms (Fouda 2011), whereas the trial by Stephenson 2004 did not assess these (Analysis 4.4).
4.4. Analysis.

Comparison 4: LMWH+ aspirin versus UFH + aspirin, Outcome 4: Venous thromboembolism
Arterial thromboembolism
One trial reported zero arterial thromboembolism events in both arms (Fouda 2011), whereas the trial by Stephenson 2004 did not assess these (Analysis 4.5).
4.5. Analysis.

Comparison 4: LMWH+ aspirin versus UFH + aspirin, Outcome 5: Arterial thromboembolism
Pregnancy loss
Based on two studies, there may be a lower risk of pregnancy loss with LMWH plus aspirin compared to UFH plus aspirin (RR 0.53, 95% CI 0.28, 0.99; 83 women; Analysis 4.9).
4.9. Analysis.

Comparison 4: LMWH+ aspirin versus UFH + aspirin, Outcome 9: Pregnancy loss
Secondary outcomes (for the child)
Preterm delivery of a live infant
No clear difference in the risk of preterm delivery was observed with a higher compared with a lower dose of LMWH (Analysis 4.6; Fouda 2011). This outcome could not be evaluated for different doses of UFH, as data were lacking.
4.6. Analysis.

Comparison 4: LMWH+ aspirin versus UFH + aspirin, Outcome 6: Preterm delivery of a live infant
Intrauterine growth restriction
The rates of IUGR in the trial by Fouda and colleagues were low, 1 of 24 in the higher dose of LMWH treatment arm versus 2 of 20 in the lower dose of LMWH treated group respectively (RR 0.42, 95% CI 0.04 to 4.27; Analysis 4.7; Fouda 2011).
4.7. Analysis.

Comparison 4: LMWH+ aspirin versus UFH + aspirin, Outcome 7: Intrauterine growth restriction
Adverse events in the child (definitions according to original study: (A) congenital malformations, (B) neonatal bleeding)
Both congenital malformations and neonatal bleeding were reported as an outcome, but the trial by Fouda 2011 had no cases in either treatment arm (Analysis 4.8).
4.8. Analysis.

Comparison 4: LMWH+ aspirin versus UFH + aspirin, Outcome 8: Adverse events in the child
Comparison 5: Higher dose heparin plus aspirin versus lower dose heparin plus aspirin
Primary outcome ‐ Live birth
A higher dose of LMWH did not improve the live birth rate (RR 1.10, 95% CI 0.81 to 1.49, 1 trial, 60 women; Analysis 5.1), similar to the effects of a higher dose of UFH (RR 1.05, 95% CI 0.78 to 1.41, 1 trial, 50 women; Analysis 5.1).
5.1. Analysis.

Comparison 5: Higher dose heparin + aspirin versus lower dose heparin + aspirin, Outcome 1: Live birth
Secondary outcomes (maternal)
Pre‐eclampsia
The incidence of pre‐eclampsia did not clearly differ in the groups treated with a higher or a lower dose of either heparin (RR 1.64, 95% CI 0.41 to 6.48; Analysis 5.2. 2 trials, 90 women; Fouda 2010; Kutteh 1996b).
5.2. Analysis.

Comparison 5: Higher dose heparin + aspirin versus lower dose heparin + aspirin, Outcome 2: Pre‐eclampsia
Adverse events in the mother (definitions according to original study: (A) bleeding, (B) heparin‐induced thrombocytopenia, (C) allergic reactions)
Major maternal bleeding events did not occur in any participant, whereas the rate of minor bleeding events was similar in the high‐dose UFH group (3/20) compared with the low‐dose UFH group (4/19) (RR 0.71, 95% CI 0.18 to 2.77. 2 trials, 99 women; Analysis 5.3; Kutteh 1996b). The incidence of postpartum haemorrhage was evaluated in one trial, but was not diagnosed (Fouda 2010). Heparin‐induced thrombocytopenia was not reported in either trial, while allergic reactions were not assessed (Fouda 2010; Kutteh 1996b).
5.3. Analysis.

Comparison 5: Higher dose heparin + aspirin versus lower dose heparin + aspirin, Outcome 3: Adverse events in the mother
Venous thromboembolism
Fouda 2010 reported no events in any of the participants during study participation (Fouda 2010; Analysis 5.4).
5.4. Analysis.

Comparison 5: Higher dose heparin + aspirin versus lower dose heparin + aspirin, Outcome 4: Venous thromboembolism
Arterial thromboembolism
Fouda 2010 reported no events in any of the participants during study participation (Fouda 2010; Analysis 5.5).
5.5. Analysis.

Comparison 5: Higher dose heparin + aspirin versus lower dose heparin + aspirin, Outcome 5: Arterial thromboembolism
Pregnancy loss
Based on two studies, there may be a lower risk of pregnancy loss with LMWH plus aspirin compared to UFH plus aspirin (RR 0.80, 95% CI 0.41, 1.55; 110 women; Analysis 5.9).
5.9. Analysis.

Comparison 5: Higher dose heparin + aspirin versus lower dose heparin + aspirin, Outcome 9: Pregnancy loss
Secondary outcomes (for the child)
Preterm delivery of a live infant
The rate of preterm delivery was low and the difference between treatment groups was not clear in the trials that compared a higher‐dose heparin (LMWH or UFH) plus aspirin versus lower‐dose heparin (LMWH or UFH) plus aspirin (RR 1.96, 95% CI 0.52 to 7.32; Analysis 5.6; Fouda 2010; Kutteh 1996b).
5.6. Analysis.

Comparison 5: Higher dose heparin + aspirin versus lower dose heparin + aspirin, Outcome 6: Preterm delivery of a live infant
Intrauterine growth restriction
IUGR was reported in a small minority of cases and rates with no clear difference between interventions; 2/30 and 3/20 in the respective groups treated with a higher dose heparin (LMWH or UFH) versus 1/30 and 0/19 in the groups treated with a lower dose of heparin (Fouda 2010; Kutteh 1996b; Analysis 5.7).
5.7. Analysis.

Comparison 5: Higher dose heparin + aspirin versus lower dose heparin + aspirin, Outcome 7: Intrauterine growth restriction
Adverse events in the child (definitions according to original study: (A) congenital malformations, (B) neonatal bleeding)
Congenital malformations and neonatal bleeding were assessed in the trial by Fouda 2010, but there were no cases in either treatment arm (Fouda 2010; Analysis 5.8).
5.8. Analysis.
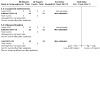
Comparison 5: Higher dose heparin + aspirin versus lower dose heparin + aspirin, Outcome 8: Adverse events in the child
Discussion
Summary of main results
The aim of this review was to assess the effects of aspirin or heparin or both for improving pregnancy outcome in women with persistent antiphospholipid antibodies (aPL) and recurrent pregnancy loss. There were no trials that had a no treatment comparator arm during pregnancy.
It is uncertain if aspirin alone has any effect on live birth when compared to placebo. There were no studies that investigated heparin alone.
The results of the meta‐analyses suggest that the combination of heparin, started after a positive pregnancy test, plus aspirin may slightly improve live birth rates compared with aspirin alone. This result was mostly driven by one large single‐centre trial (n = 1015) using low‐molecular‐weight heparin (LMWH), that found a 90.3% live birth rate in the LMWH plus aspirin group, compared to 70.1% in the group treated with aspirin alone. Two small trials evaluating unfractionated heparin (UFH) also demonstrated the combination of UFH plus aspirin to be superior to aspirin alone.
The pooled risk ratio for live birth in a head‐to‐head comparison of LMWH with UFH, both in combination with aspirin, did not demonstrate a clear benefit of one heparin over the other. Two small trials compared a higher and a lower dose of heparin (LMWH or UFH) both combined with aspirin, but there were insufficient data for meaningful analyses.
It is very uncertain if aspirin compared with placebo has any effect on the risk of pre‐eclampsia, pregnancy loss, preterm delivery of a live infant, intrauterine growth restriction or adverse events in the mother or child.
Similarly, it is very uncertain if heparin plus aspirin compared with aspirin alone has any effect on the risk of pre‐eclampsia, preterm delivery of a live infant, intrauterine growth restriction or adverse events in the mother or child.
Overall completeness and applicability of evidence
Eleven trials met our predefined inclusion criteria, with differences in treatment regimens and types of intervention. The substantial heterogeneity in study populations and numbers of enrolled participants reflect the clinical heterogeneity of antiphospholipid syndrome (APS) and at the same time point out the potential difficulties that can be encountered in conducting research in this population. The current review focused on recurrent pregnancy loss, whereas obstetric APS also has other manifestations. We strictly adhered to the inclusion criteria to maintain uniformity in this review and consequently excluded a large number of trials. Results from these trials may be of equal clinical importance and should not be neglected because they did not exactly meet the set criteria for the current review.
The evidence from this review stems from an overall small number of trials, though largely driven by the results from one trial with a large number of enrolled participants. The predefined criteria for inclusion and exclusion were followed consistently, though we broadened the criteria for persistent antibodies, as only three trials adhered to the time‐frame of at least 12 weeks between aPL‐testing. The heterogeneity in study populations, the variety of inclusion criteria and the interventions in the included trials form limitations in this review, but for the main comparisons findings were consistent.
Currently, suggested and widely employed management strategies to improve pregnancy outcomes in women with recurrent pregnancy loss and positive aPL include antepartum administration of prophylactic‐ or intermediate‐dose UFH or prophylactic‐dosed LMWH combined with aspirin over no treatment, but a risk and benefit evaluation per patient is advised (Bates 2012; Skeith 2018). The pharmacokinetic profiles of UFH and LMWH differ and perhaps their biological effects as well. Possible effects on complement activation may be of more importance and it has been hypothesised that the non‐anticoagulant effects of heparins on inflammatory processes, vascular function or placental pathology may play a role in prevention of pre‐eclampsia, a disorder highly associated with APS (Wat 2018). In a mouse model of the APS, the prevention of fetal loss by both LMWH and UFH was mediated through complement activation inhibition (Girardi 2004). A prophylactic dose of LMWH was sufficient to reduce classical complement activity in pregnant women with a history of venous thromboembolism, but this has not been evaluated for different dosages of heparin, or in presence of aPL (Oberkersch 2010). The role of non‐thrombotic processes involved in the pathogenesis of recurrent miscarriage in presence of aPL has become more clear over the years (Schreiber 2018). As defined in the protocol, we planned to carry out a subgroup analysis based on a history of previous placenta‐mediated complications, such as pre‐eclampsia, intrauterine growth restriction and/or placental abruption. The rationale for this was the different pathogenesis of recurrent early (i.e. first‐trimester) miscarriage associated with presence of aPL from the pathogenesis of aPL‐associated late pregnancy morbidity. A minority of trials reported our predefined secondary outcomes and a subgroup analysis was not possible for this reason.
Clinical criteria for pregnancy morbidity associated with APS include ≥ 1 unexplained fetal death after ≥ 10 weeks of gestation, one or more premature delivery < 34 weeks of gestation due to severe (pre)eclampsia or placental insufficiency or ≥ 3 unexplained consecutive miscarriages < 10 weeks of gestation. Though all participants in the included studies had at least two, and most at least three pregnancy losses and persistent presence of aPL, baseline characteristics differed largely between study populations. A substantial part of the studied population in the current review are not considered to be patients with obstetric APS and it is known that differences exist in risk for obstetric complications in subgroups of patients with APS (Meroni 2012; Lockshin 2013; Schreiber 2018). Most of our studied population differs from women described as being a classic APS case (late fetal death, lupus anticoagulant, history of thrombosis). In obstetric APS, presence of lupus anticoagulant has been identified as the main predictor of adverse pregnancy outcomes and thrombotic events (Buyon 2015, Lockshin 2012). As demonstrated in Table 3, in patients whose aPL antibody profiles were reported, the majority of the studied population was positive for lupus anticoagulant alone or both lupus anticoagulant and anticardiolipin antibodies. Bao 2017 reported results on a large number of women with aPL and recurrent miscarriage, but did not report details on aPL‐profiles in either treatment group; therefore it remains unknown if clinically relevant subgroup differences exist. Attempts to contact the authors of this trial in order to retrieve additional data relevant for the current review, were unfruitful. This trial also did not exclude patients with a previous thrombosis, whereas most other trials explicitly did. We ourselves did not further define miscarriage, as both recurrent early or late pregnancy losses could be included (as long as a history of two miscarriages had been established) and only a minority of the studies reported additional data on gestational age at the time of pregnancy loss. Hence, patients with classic APS may have been included in the studied population. We cannot state that the risk for obstetric complications or thrombotic complications for that matter, is much lower in our studied population, as we simply lack the data to conclude this. As the main predictor for the next pregnancy outcome is the number of previous pregnancy losses (Carp 2007), possibly the trial by Laskin and colleagues (Laskin 2009) would have demonstrated different outcomes for subgroups with ≥ 2 or ≥ 3 previous miscarriages. The largest trial (Bao 2017), which was a large contributor to the pooled effect, included women with a history of at least two consecutive miscarriages, but did not report the number of previous miscarriages per treatment group. It should be noted that the currently employed Sydney classification criteria for APS (Miyakis 2006) form an aid in the diagnosis of APS, but were originally developed for research purposes. In the current review, we were not able to carry out subgroup analyses based on aPL‐profiles, due to the small numbers of included trials and/or limited reporting of aPL‐profiles in correlation to the primary outcome live birth.
Antibody cut‐off levels differed greatly between trials and only one trial explicitly reported aPL‐titres in participants. The association between aPL and recurrent pregnancy loss varies per type of aPL and also differs for early and late pregnancy loss (Opatrny 2006). For this reason, current guidelines recommend testing for aPL ( lupus anticoagulant (LAC) and anticardiolipin (ACA) IgG and IgM) after two pregnancy losses, consecutive or non‐consecutive, whereas testing for aβ2GPI can be considered (Vermeulen 2018). None of the included trials in the current review reported women with aβ2‐GPI antibodies. Clinical studies ideally should report results on women with homogenous aPL‐profiles and women with strongly positive tests or high‐titre antibodies should be analysed separately. As APS is a heterogeneous disease with a wide variation in both clinical presentation and laboratory parameters, an accurate evaluation of two interventions in a homogeneous subset of APS‐patients is challenging.
Uncertainty also remains regarding the ideal timing of initiation and duration of treatment. Most trials included in this review started eligible participants on aspirin preconceptionally, with heparin added once pregnancy was confirmed, in order to compare heparin and/or aspirin with aspirin alone during pregnancy. A recent study by Eid 2019 evaluated early initiation of LMWH, i.e. once positive pregnancy test was established in the fifth week of gestation, and later initiation of LMWH, i.e. after sonographic confirmation of fetal cardiac pulsation in week seven, both regimens combined with aspirin started preconceptionally. Early initiation led to an ongoing pregnancy rate of 81% at 12 weeks' gestation compared to 61% in the later initiation group. However, live birth rates and the incidence of late obstetrical complications were similar in both groups (Eid 2019). In another trial, comparing LMWH and aspirin with placebo given preconceptionally, women in the treatment group had a higher ongoing pregnancy rate within six months after randomisation when compared with women in the placebo group, but live birth overall was not affected. Additionally, the incidence of pre‐eclampsia was higher in the placebo‐treated women; 24% versus 11% in the intervention group (Ismail 2016). Initiation of heparin preconceptionally in all women with APS and recurrent early pregnancy loss would be undesirable from a patients' perspective, but whether heparin can be safely discontinued after the first trimester of pregnancy with regard to pregnancy outcome, requires further investigation.
Women with persistent presence of aPL and a history of thrombosis as well as recurrent miscarriage require thromboprophylaxis during pregnancy, as aspirin only would not be considered sufficient to prevent recurrent thrombosis. However, there are no randomised clinical trials that have evaluated anticoagulant treatment strategies, i.e. between different doses of anticoagulants, in this high‐risk population. In women with obstetric APS without a personal history of venous or arterial thrombosis receiving antepartum anticoagulant prophylaxis continuation postpartum can be considered (Bates 2018). However, the incidence of postpartum thrombosis in this population is unclear, hence the aim of postpartum thromboprophylaxis and duration thereof in this population, cannot be substantiated with the currently available evidence. Further trials should investigate the role of LMWH for prevention of recurrent pregnancy loss and of placenta‐mediated complications in women with APS.
In the trial by Farquharson 2002, a substantial part of the study population was non‐adherent (24/98), which challenges interpretation of the reported results. The authors reported no significant differences in live birth in the non‐adherent group compared to either the adherent group or the whole group. Adherence to therapy may have been higher in women receiving UFH‐ compared to LMWH‐treated women, as the dose of UFH is adjusted per patient through activated partial thromboplastin time (aPTT) monitoring. The optimal dose of LMWH or heparin, with maximal benefit and minimal risks, is unknown. Various doses of aspirin and or heparin were used in the included studies, but we did not account for these differences in the analyses, due to small sizes of the studies and limited data. Studies comparing a high or low dose of either UFH or LMWH in combination with aspirin did not show significant differences between treatment groups, though it should be noted that the quasi‐randomised controlled trial comparing different dosages of UFH lacked the power to detect any significant differences and had methodological limitations (no allocation concealment). Variation in initiation of treatment, in duration of treatment, as well as different doses and agents used, limits the possibilities of a cross‐study comparison. Two included trials continued heparin postpartum.
Noticeably, adverse events associated with heparin therapy, easy bruising at injection site or allergies, did not occur frequently or were not reported. The improvement in pregnancy outcome observed in the UFH‐treated women seemed to be associated with a non‐significant increase in risk of preterm delivery, as assessed in the subgroup of live births. For intrauterine growth restriction a comparison in the subgroup of live births was not possible, as the trial by Laskin at al (Laskin 2009) only reported adverse outcomes for all participants. As we do not know the baseline risk for preterm delivery and intrauterine growth restriction in the subgroups of live birth and this baseline risk likely differs, this comparison is prone to bias.
Important side effects of UFH therapy, such as haemorrhage and heparin‐induced thrombocytopenia did not occur or were not reported and only minor bleeding events and bruising at injection site were mentioned as possible adverse effects of heparin therapy. In the general population (i.e. without anticoagulant use during pregnancy), estimated incidences of bleeding after delivery > 500 mL typically range from 4% to 6% (Scheres 2019). Hence, the possibility of underreporting should be considered in interpreting these figures. Thrombocytopenia occurs in 5% to 10% of all pregnant women, with a slow decrease in platelet counts starting in the second trimester, most likely a consequence of haemodilution (Cines 2017). Osteoporosis is associated with heparin treatment and should be taken into consideration when treatment is long term, but was not evaluated as a secondary outcome in this review. UFH therapy when given in a low dose does not require monitoring and likely is effective in preventing recurrent pregnancy loss, though the unexpectedly low live birth rates in the comparator arms in the UFH studies may have led to an overestimation of the effect. LMWH, which has a similar efficacy and a superior safety profile compared with UFH, is a reasonable alternative treatment and currently most often used in clinical practice.
Quality of the evidence
Most of the trials were judged to be at low risk of bias for most categories. Two quasi‐randomised trials were at high risk of selection bias due to lack of allocation concealment (Kutteh 1996a; Kutteh 1996b),and in one trial, allocation concealment was unclear, therefore considered as at high risk of selection bias as well (Alalaf 2012). Three trials reported incomplete outcome data (attrition bias), including one trial at high risk for reporting bias as well (Alalaf 2012; Bao 2017; Pattison 2000).
Additonally, a majority of trials were not registered in a clinical trial registry nor had published a study protocol. For this reason, it remains unclear whether selective reporting occurred in these trials and we assessed reporting bias as unclear in unregistered studies published in the last 10 years.
Though in only two trials participants and personnel both were made unaware of treatment allocation, we assessed all trials at low risk for performance bias, since live birth is an unequivocal outcome and knowledge of treatment allocation is unlikely to influence this.
Certainty of the evidence
The certainty of evidence is low to very low. We downgraded the evidence for imprecision (due to low numbers of women participating in the studies and wide 95% confidence intervals, which are consistent with appreciable harms and benefits) and for risk of bias limitations.
Potential biases in the review process
We minimised the risk of bias in the selection of studies, with an extensive search strategy and no language or publication date restriction, to identify all relevant studies. Two review authors independently assessed study eligibility, performed data extraction and GRADE assessments. There was no funding provided for this review. Lastly, none of the review authors were involved in any of the trials evaluated for this review. We were unaware of any potential bias by focusing specifically on aspirin and/or heparin versus placebo or another for prevention of recurrent pregnancy loss in women with persistent aPL in this revision of the previous review. Formal assessment of reporting bias by means of a funnel plot, was not possible due to the small number of trials in the meta‐analyses for the main comparisons.
Agreements and disagreements with other studies or reviews
For aspirin, we only identified one study which investigated the effect of aspirin alone by comparing it with placebo (Pattison 2000). However, due to its small sample size and considerable limitations, no conclusions could be drawn based on this single study. In studies with women with recurrent pregnancy loss without persistent aPL, aspirin does not seem to improve live birth rates (De Jong 2014). Aspirin has been studied extensively in the context of reduction of the risk of pre‐eclampsia. Here, also outside of the population with persistent aPL, aspirin reduces the risk of pre‐eclampsia (Askie 2007; Rolnik 2017). Based on the lack of direct evidence and available indirect evidence, it is reasonable to suggest aspirin for prevention of pre‐eclampsia in women with recurrent pregnancy loss and persistent aPL.
A cohort study of 693 women with recurrent miscarriage evaluated live birth rates in aPL‐positive women and in women with unexplained recurrent miscarriage; overall live birth rates were 69% in aPL‐positive women and 63% in women with unexplained recurrent miscarriage. Stratification by treatment demonstrated 79% live birth in the group with aPL‐positive women treated with aspirin and heparin compared to 62% in the group treated with aspirin alone. Stratification by treatment did not show differences in outcome in the group of women with recurrent miscarriage (Cohn 2010). In non‐aPL populations evidence from an individual‐patient level meta‐analysis suggests no role for LMWH in a prophylactic dose during pregnancy to prevent recurrent placenta‐mediated pregnancy complications (Rodger 2014). Another recent meta‐analysis including eight trials involving 483 women with inherited thrombophilia and recurrent miscarriage found no significant difference in live birth rates with LMWH use compared to no LMWH (RR 0.81, 95% CI 0.55 to 1.19) (Skeith 2016).
Authors' conclusions
Implications for practice.
Heparin (low‐molecular‐weight heparin (LMWH) or unfractionated heparin (UFH)) combined with aspirin may lead to more live births in women with recurrent pregnancy loss with antiphospholipid antibodies (aPL) than treatment with aspirin alone (low‐certainty evidence). The observed beneficial effect of heparins is mainly driven by one large single‐centre trial using LMWH. The effect of aspirin on live birth rates remains uncertain.
Implications for research.
A large multicentre randomised controlled trial with clearly defined inclusion and exclusion criteria for subgroups of patients with aPL and recurrent pregnancy loss, is needed in order to evaluate risks and benefits of current treatment strategies and to gain consensus on the ideal prevention for recurrent pregnancy loss, based on a risk profile. Additionally, further research involving women with obstetric antiphospholipid syndrome (APS) without a history of venous or arterial thrombosis, is needed to determine whether LMWH can be safely discontinued after the first trimester of pregnancy, with regard to adverse pregnancy outcomes.
History
Protocol first published: Issue 11, 2017 Review first published: Issue 5, 2020
Acknowledgements
The review authors would like to thank Lynn Hampson for her search of the Cochrane Pregnancy and Childbirth Trials Register.
LJJ Scheres is a PhD‐candidate of the CREW project (2013T083) supported by the Netherlands Heart Foundation. Saskia Middeldorp is supported by a VIDI grant from The Netherlands Organisation for Health Research and Development (016.126.364).
As part of the pre‐publication editorial process, this review has been commented on by four peers (an editor and three referees who are external to the editorial team), and the Group's Statistical Adviser. The authors are grateful to the following peer reviewers for their time and comments: Professor Fionnuala Ní Áinle, Depts of Haematology, Mater Misericordiae University Hospital and Rotunda Hospital, Dublin, University College Dublin School of Medicine; Bob Silver, University of Utah; and also to an another who wishes to remain anonymous.
This project was supported by the National Institute for Health Research, via Cochrane Infrastructure funding to Cochrane Pregnancy and Childbirth. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
The review authors would like to thank Fiona Stewart, Cochrane Children and Families' Network Support Fellow for her assistance and guidance in finalising the review.
Appendices
Appendix 1. Search strategies
ICTRP and ClinicalTrials.gov search terms (up to 26 November 2018)
Each line was run separately
ICTRP
antiphospholipid AND miscarriage
anti‐phospholipid AND miscarriage
antiphospholipid AND pregnancy
anti‐phospholipid AND pregnancy
hughes syndrome AND pregnancy
hughes syndrome AND miscarriage
heparin AND miscarriage
aspirin AND miscarriage
anticoagulant(s) AND miscarriage
ClinicalTrials.gov
Advanced search
Types of study: Interventional
Condition: Antiphospholipid in pregnancy; recurrent miscarriage; Hughes syndrome
Data and analyses
Comparison 1. Aspirin versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Live birth | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.94 [0.71, 1.25] |
| 1.2 Pre‐eclampsia | 1 | 33 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.25, 4.52] |
| 1.3 Adverse events in the mother | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.3.1 Bleeding | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.29 [0.60, 2.77] |
| 1.4 Preterm delivery of a live infant | 1 | 33 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.29 [0.27, 102.49] |
| 1.5 Intrauterine growth restriction | 1 | 33 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.27 [0.03, 2.13] |
| 1.6 Adverse events in the child | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 1.6.1 Congenital malformations | 1 | 33 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.07, 15.60] |
| 1.7 Pregnancy loss | 1 | 40 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.34, 5.21] |
Comparison 2. Heparin + aspirin versus aspirin.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Live birth | 5 | 1295 | Risk Ratio (M‐H, Random, 95% CI) | 1.27 [1.09, 1.49] |
| 2.1.1 UFH + aspirin versus aspirin | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 1.74 [1.28, 2.35] |
| 2.1.2 LMWH + aspirin versus aspirin | 3 | 1155 | Risk Ratio (M‐H, Random, 95% CI) | 1.20 [1.04, 1.38] |
| 2.2 Pre‐eclampsia | 2 | 82 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.57 [0.10, 3.14] |
| 2.3 Adverse events in the mother | 2 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2.3.1 Bleeding | 1 | 31 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.65 [0.19, 14.03] |
| 2.3.2 Heparin‐induced thrombocytopenia | 2 | 140 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 2.3.3 Allergic reactions | 1 | 90 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 2.4 Venous thromboembolism | 3 | 182 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 2.5 Arterial thromboembolism | 3 | 182 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 2.6 Preterm delivery of a live infant | 3 | 156 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.93 [0.42, 2.07] |
| 2.7 Intrauterine growth restriction | 3 | 151 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.85 [0.33, 2.19] |
| 2.8 Adverse events in the child | 1 | 51 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 2.8.1 Congenital malformations | 1 | 51 | Risk Ratio (M‐H, Random, 95% CI) | Not estimable |
| 2.9 Pregnancy loss | 5 | 1295 | Risk Ratio (M‐H, Random, 95% CI) | 0.48 [0.32, 0.71] |
| 2.9.1 UFH + aspirin versus aspirin | 2 | 140 | Risk Ratio (M‐H, Random, 95% CI) | 0.46 [0.29, 0.71] |
| 2.9.2 LMWH + aspirin versus aspirin | 3 | 1155 | Risk Ratio (M‐H, Random, 95% CI) | 0.55 [0.26, 1.16] |
Comparison 3. LMWH versus aspirin.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Live birth | 1 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.20 [1.00, 1.43] |
| 3.2 Pre‐eclampsia | 1 | 113 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.93 [0.08, 46.31] |
| 3.3 Adverse events in the mother | 1 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.42 [0.47, 149.41] |
| 3.3.1 Bleeding | 1 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 8.42 [0.47, 149.41] |
| 3.4 Venous thromboembolism | 1 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 3.5 Arterial thromboembolism | 1 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 3.6 Preterm delivery of a live infant | 1 | 113 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.96 [0.17, 5.50] |
| 3.7 Pregnancy loss | 1 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.49 [0.25, 0.98] |
Comparison 4. LMWH+ aspirin versus UFH + aspirin.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 4.1 Live birth | 2 | 86 | Risk Ratio (M‐H, Random, 95% CI) | 1.44 [0.80, 2.62] |
| 4.2 Pre‐eclampsia | 2 | 70 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.09 [0.33, 13.22] |
| 4.3 Adverse events in the mother | 2 | 206 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.22, 4.56] |
| 4.3.1 Bleeding | 2 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.00 [0.22, 4.56] |
| 4.3.2 Heparin‐induced thrombocytopenia | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 4.3.3 Allergic reactions | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 4.4 Venous thromboembolism | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 4.5 Arterial thromboembolism | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 4.6 Preterm delivery of a live infant | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.25 [0.23, 6.76] |
| 4.7 Intrauterine growth restriction | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.42 [0.04, 4.27] |
| 4.8 Adverse events in the child | 1 | 88 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 4.8.1 Congenital malformations | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 4.8.2 Neonatal bleeding | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 4.9 Pregnancy loss | 2 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.53 [0.28, 0.99] |
Comparison 5. Higher dose heparin + aspirin versus lower dose heparin + aspirin.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 5.1 Live birth | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.08 [0.87, 1.33] |
| 5.1.1 Higher dose UFH versus lower dose UFH | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.05 [0.78, 1.41] |
| 5.1.2 Higher dose LMWH versus lower dose LMWH | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.10 [0.81, 1.49] |
| 5.2 Pre‐eclampsia | 2 | 99 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.41, 6.48] |
| 5.3 Adverse events in the mother | 2 | 198 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.18, 2.77] |
| 5.3.1 Bleeding | 2 | 99 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.71 [0.18, 2.77] |
| 5.3.2 Heparin‐induced thrombocytopenia | 2 | 99 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 5.3.3 Allergic reactions | 0 | 0 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 5.4 Venous thromboembolism | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 5.5 Arterial thromboembolism | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 5.6 Preterm delivery of a live infant | 2 | 81 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.96 [0.52, 7.32] |
| 5.7 Intrauterine growth restriction | 2 | 99 | Risk Ratio (M‐H, Fixed, 95% CI) | 3.58 [0.61, 21.07] |
| 5.8 Adverse events in the child | 1 | 88 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 5.8.1 Congenital malformations | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 5.8.2 Neonatal bleeding | 1 | 44 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 5.9 Pregnancy loss | 2 | 110 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.80 [0.41, 1.55] |
| 5.9.1 Higher dose UFH versus lower dose UFH | 1 | 50 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.83 [0.29, 2.38] |
| 5.9.2 Higher dose LMWH versus lower dose LMWH | 1 | 60 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.78 [0.33, 1.82] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Alalaf 2012.
| Study characteristics | ||
| Methods | Open‐label, randomised controlled trial (N = 141) | |
| Participants |
Inclusion criteria 1) age 18‐42 years at time of interview 2) ≥ 2 unexplained consecutive miscarriages before 20 weeks' gestation 3) persistent presence of aCL antibodies (IgG > 15 GPL or IgM > 25 MPL) or positive LAC on 2 occasions, 8 weeks apart. Exclusion criteria Systemic lupus erythematosus, known peptic ulcer disease, sensitivity to aspirin or heparin depending on patient's history report, previous venous thromboembolic disease requiring ongoing anticoagulant therapy, other causes for recurrent miscarriage (polycystic ovarian syndrome, thyroid dysfunction, anatomical causes), bacterial vaginosis infection and failure to consent to participate. |
|
| Interventions | LMWH (bemiparin) 2500 IU/day sc (N = 80) versus Aspirin 100 mg/day (N = 61) |
|
| Outcomes |
Primary outcome Live birth Secondary outcomes Obstetrical complications, fetal and maternal adverse events |
|
| Notes | Aspirin commenced preconceptionally until 36 weeks of gestation, bemiparin commenced when pregnancy was confirmed until 36 weeks of gestation. Mean number of previous pregnancy losses was 3.28 ± 1.72 in the LMWH group versus 3.41 ± 1.76 in the aspirin group; no specification for previous early and late loss reported. As study outcome total pregnancy loss reported; no specification for early and late loss reported. Trial registry: trial not registered in clinical trial registry. No published study protocol. Dates of study: recruitment period 15 September 2007 to 1 August 2010, publication 2012. Funding sources: not stated Declarations of interest: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Process of randomisation not clearly described. Authors state some form of alternation between treatment groups: the first case was randomised to treatment 1, the second case to treatment 2 and sometimes 2 cases were randomised to treatment 1, followed by one case of treatment 2. |
| Allocation concealment (selection bias) | High risk | Not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Exclusions, reasons for exclusion and numbers included in the analysis at each stage were not reported. Loss‐to‐follow up not reported. |
| Selective reporting (reporting bias) | Unclear risk | Trial not registered in clinical trial registry. No published study protocol. |
| Other bias | Low risk | No indication of other sources of bias |
Bao 2017.
| Study characteristics | ||
| Methods | Randomised study (N = 1096) | |
| Participants |
Inclusion criteria 1) history of ≥ 2 consecutive miscarriages 2) ≥ 2 blood tests taken at an interval of at least 12 weeks apart confirming the presence of either LA (prolongation of the dilute Russell viper venom time ratio greater than 1.09 with at least 20% correction by washed, frozen/thawed platelets) anti‐β2GPI or aCL antibodies (IgG > 40 GPL, IgM > 40 MPL or higher than the 99th percentile of the reference range obtained with normal participants) before pregnancy Exclusion criteria Recent history of major surgery; pregnancy; haemorrhage or trauma; under oral contraception or hormone therapy; partner with an abnormal karyotype |
|
| Interventions | LMWH (nadroparin) 4100 U/day sc + aspirin 75 mg/day (N = 497) versus Aspirin 75 mg/day (N = 518) |
|
| Outcomes | Live birth and pregnancy failure (including ectopic pregnancy and miscarriage) | |
| Notes | At confirmation of pregnancy randomisation to either LWMH + aspirin or aspirin, treatment continued until miscarriage or 35 weeks of gestation. Number of previous pregnancy losses not reported. As study outcome total pregnancy loss reported; no specification for early and late loss reported. Per‐protocol analysis, no intention‐to‐treat analysis. 30/548 in LMWH + aspirin group and 14/548 in aspirin group excluded due to disagreement on assigned treatment. Additionally, 37 (3.3%) women lost to follow‐up (21/518 in LMWH + aspirin group and 16/534 in aspirin group). 497 women in LMWH + aspirin group versus 518 women in aspirin group. Trial registry: trial not registered in clinical trial registry. No published study protocol. Dates of study: recruitment period 2012 to 2015, publication in 2017. Funding sources: Shanghai Committee of Science and Technology, Grant/Number: 14411966600 and 17411967800; The Joint Key Project of New Frontier Technology in Shanghai Municipal Hospitals, Grant/Number: SHDC12014129. Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list. |
| Allocation concealment (selection bias) | Low risk | Adequate allocation concealment, randomisation list kept by independent member of staff not involved in the trial. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | No published study protocol. Exclusions, reasons for exclusion and numbers included in the analysis at each stage were reported; loss to follow‐up reported; per‐protocol analysis, outcomes of censored participants and reasons for censoring unclear. |
| Selective reporting (reporting bias) | Unclear risk | Trial not registered in clinical trial registry. No published study protocol. |
| Other bias | Low risk | No indication of other sources of bias |
Farquharson 2002.
| Study characteristics | ||
| Methods | Single‐centre, randomised non‐blinded, non‐placebo controlled trial (N = 98) | |
| Participants |
Inclusion criteria 1) 18‐41 years 2) ≥ 3 consecutive pregnancy losses or 2 consecutive losses with proven fetal death after 10 weeks 3) 2 positive test for antiphospholipid antibodies more than 6 weeks apart, determined by lupus anticoagulant (dRVVT > 1.09 with > 20% correction with platelets), or aCL antibodies (IgG > 9 U/mL or aCL IgM > 5 U/mL) Exclusion criteria Parental chromosomal abnormality, uterine anomaly, previous arterial of venous thrombosis, use of steroids during pregnancy, systemic lupus erythematosus requiring medication or complicated by nephritis, and other thrombophilia such as activated protein C resistance or protein C/S deficiency. |
|
| Interventions | LMWH 5000 IU/day sc + aspirin 75 mg/day (N = 51) versus Aspirin 75 mg/day (N = 47) |
|
| Outcomes | Embryo loss (no visible crown rump length or fetal heart activity) and fetal loss (loss of fetal heart activity after clear identification on previous scan) | |
| Notes | Randomisation occurred < 12 weeks' gestation, mean 7.1 weeks for LMWH plus aspirin group and 6.3 weeks for the aspirin group Mean number of previous pregnancy losses was 3 ± 0.8 in the LMWH + aspirin group versus 3 ± 0.9 in the aspirin group; no specification for previous early and late loss reported. LMWH plus aspirin or aspirin started at randomisation (before 12 weeks of gestation) and continued until delivery. 11/47 in the aspirin group also took LMWH and 13/51 in the aspirin/LMWH group took aspirin alone Type of LMWH not specified. 11/51 pregnancy losses in the LMWH plus aspirin group (3/11 embryo loss, 8/11 fetal loss) versus 13/47 pregnancy losses in the aspirin group (9/13 embryo loss, 4/13 fetal loss). Trial registry: trial not registered in clinical trial registry, but clinical trial registry at time of publication non‐existing. No published study protocol. Dates of study: recruitment period from January 1997 to January 2000, publication in 2002. Funding sources: LUPUS UK and NHS R&D (NWEST) grant support Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated sequence of random numbers. |
| Allocation concealment (selection bias) | Low risk | Telephone randomisation, adequate allocation concealment. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth Data collection by independent research officer who received copies of randomisation data sheets. Blinding of outcome assessment not explicitly stated. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusions, reasons for exclusion and numbers included in the analysis at each stage were reported; no missing outcome data, no loss to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | All analyses completed on an intention‐to‐treat basis. Trial not registered in clinical trial registry, but clinical trial registry at time of publication non‐existing. No published study protocol. |
| Other bias | Low risk | No indication of other sources of bias |
Fouda 2010.
| Study characteristics | ||
| Methods | 2‐arm prospective, randomised controlled study (N = 60) | |
| Participants |
Inclusion criteria 1) ≥ 3 consecutive pregnancy losses before 10 weeks' gestation 2) positive LAC and/or aCL antibodies (IgG and IgM) on at least 2 occasions, at least 12 weeks apart Exclusion criteria Paternal chromosomal abnormalities or uterine abnormalities, luteal phase defect, abnormal thyroid function tests, hyperprolactinaemia, polycystic ovary syndrome, systemic lupus erythematosus, previous thromboembolism, peptic ulcer, age < 19 years or > 37 years, BMI < 19 or > 30 or sensitivity to aspirin or heparin. |
|
| Interventions | LMWH (enoxaparin) 40 mg/day sc + aspirin 75 mg/day (N = 30) versus LMWH (enoxaparin) 20 mg/day sc + aspirin 75 mg/day (N = 30) |
|
| Outcomes |
Primary outcome Live birth rate Secondary outcome Maternal and obstetric complications during pregnancy or puerperium such as excessive bleeding, thrombocytopenia, intrauterine growth restriction, pre‐eclampsia, intrauterine fetal death, thrombotic event and spontaneous osteoporotic fractures. For the infants preterm delivery, neonatal bleeding and congenital anomalies. |
|
| Notes | All participants were started on aspirin preconceptionally until 36 weeks and LMWH was added with a confirmed positive pregnancy test and continued until delivery. Mean number of previous pregnancy losses was 4.03 ± 1.24 in the LMWH 40 mg + aspirin group versus 4.1 ± 1.12 in the LMWH 20 mg plus aspirin group; no specification for previous early and late loss reported. 7/30 pregnancy losses in the LMWH 40 mg + aspirin group (6/30 first trimester loss, 1/30 second trimester loss) versus 9/30 pregnancy losses in the LMWH 20 mg + aspirin group (8/30 first trimester loss, 1/30 second trimester loss). No intrauterine fetal death in either group. Trial registry: trial not registered in clinical trial registry. No published study protocol. Dates of study: recruitment period December 2008 to May 2010, publication 2010. Funding sources: not stated Declarations of interest: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random numbers. |
| Allocation concealment (selection bias) | Low risk | Opaque envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding not reported, but knowledge of treatment allocation unlikely to influence outcome live birth. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusions, reasons for exclusion and numbers included in the analysis at each stage were reported; no loss to follow‐up, all participants analysed. |
| Selective reporting (reporting bias) | Unclear risk | Trial not registered in clinical trial registry. No published study protocol. |
| Other bias | Low risk | Nothing to indicate any other sources of bias. |
Fouda 2011.
| Study characteristics | ||
| Methods | 2‐arm, prospective, open‐labelled, multicentre, randomised controlled trial (N = 60) | |
| Participants |
Inclusion criteria 1) ≥ 3 consecutive pregnancy losses before 10 weeks' gestation 2) Positive anticardiolipin antibodies IgG (> 40 GPL) and IgM (> 40 MPL) or presence of LAC (aPTT and dilute Russell viper venom test). All of the women with positive LAC and/or anticardiolipin antibodies were retested after at least 12 weeks. Only those with persistently positive tests were included in the study. Exclusion criteria Paternal chromosomal abnormalities; uterine malformation detected by hysterosalpingography or office hysteroscopy; cervical incompetence; luteal‐phase defect; abnormal thyroid function tests; hyperprolactinaemia; polycystic ovary syndrome; hereditary thrombophilia; systemic lupus erythematosus; previous venous or arterial thrombotic episodes; diabetes mellitus; kidney or liver disease; gastric ulcer; and sensitivity to aspirin, UFH, or enoxaparin. |
|
| Interventions | Unfractionated heparin 5000 U sc twice daily + aspirin 75 mg/day (N = 30) versus LMWH (enoxaparin) 40 mg/day sc + aspirin 75 mg/day (N = 30) |
|
| Outcomes |
Primary outcome Live birth rate Secondary outcomes Excessive haemorrhage (defined by a 10% decline in the hematocrit value or the requirement of a blood transfusion), thrombocytopenia (platelet count b100,000/mL), IUGR (birthweight lower than the tenth percentile for gestational age), pre‐eclampsia (blood pressure ≥140/90 mm Hg and proteinuria ≥ 300 mg/day), IUFD, and spontaneous osteoporotic fractures. For the infants, the secondary endpoints were preterm labour (birth of infant at < 37 weeks of gestation), neonatal bleeding, and congenital anomalies. |
|
| Notes | Multicentre trial (2 centres). All women became pregnant after randomisation. Aspirin was started before conception and continued through pregnancy until 36 weeks of gestation. Anticoagulation treatment was started as soon as the serum pregnancy test became positive. Mean number of previous pregnancy losses was 4.37 ± 1.19 in the UFH + aspirin group versus 4.23 ± 1.16 in the LMWH + aspirin group; no specification for previous early and late loss reported. 10/30 pregnancy losses in the UFH + aspirin group (9/30 first trimester loss, 1/30 second trimester loss) versus 6/30 pregnancy losses in the LMWH + aspirin group (6/30 first trimester loss, 0/30 second trimester loss). No intrauterine fetal death in either group. Trial registry: the study was registered at clinicaltrials.gov [NCT01051778]. Dates of study: recruitment period 28 June 2006 to 14 December 2009, publication 2011. Funding sources: not stated Declarations of interest: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated randomisation list. |
| Allocation concealment (selection bias) | Low risk | Sequentially‐numbered, opaque sealed envelopes, each containing the allocation information written on a card. The envelopes were opened sequentially by a staff nurse to assign the women to either treatment group. The computer‐generated randomisation list and the sealed envelopes were prepared by a statistician not involved in the study. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding not reported, but knowledge of treatment allocation unlikely to influence outcome live birth. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusions, reasons for exclusion and numbers included in the analysis at each stage were reported; no loss to follow‐up, all participants analysed. |
| Selective reporting (reporting bias) | Low risk | The study was registered at clinicaltrials.gov [NCT01051778]. All of the study's pre‐specified outcomes and all expected outcomes of interest were reported. |
| Other bias | Low risk | Multicentre trial (2 centres). |
Kutteh 1996a.
| Study characteristics | ||
| Methods | Single‐centre, quasi‐randomised, non‐blinded, non‐placebo controlled trial (N = 50) | |
| Participants |
Inclusion criteria 1) Desire to become pregnant 2) Agreement to be completely evaluated 3) ≥ 3 spontaneous consecutive miscarriages 4) Consent to alternative treatment assignment 5) Presence of antiphospholipid antibodies ≥ 27 IgG or ≥ 23 IgM phospholipid units (> 2.5 multiples of the median) on 2 separate occasions Exclusion criteria Systemic lupus erythematosus, positive for lupus anticoagulant, presence of another abnormal test result that was not corrected either medically or surgically, aspirin allergy, another reason for anticoagulation during pregnancy, refused treatment or assignment to treatment. |
|
| Interventions | Unfractionated heparin 5000 units sc twice daily + aspirin 81 mg/day (N = 25) versus Aspirin 81 mg/day (N = 25) |
|
| Outcomes | Obstetric complications (preterm birth, intrauterine growth retardation and maternal complications (gestational diabetes, major and minor bleeding, thrombocytopenia, pre‐eclampsia) | |
| Notes | Aspirin commenced before conception, heparin commenced at the first confirmed pregnancy test (5.3 weeks post‐gestation). Treatment was continued until delivery and heparin continued for 3 weeks postpartum. Heparin dose increased by 1000 units/dose weekly until PTT was 1.2‐1.5 times baseline. Mean total prior miscarriages per patient was 3.9 ± 1.4 in the UFH + aspirin group (79.1% of these < 12 weeks of gestation, 91.3% < 20 weeks of gestation) versus 3.7 ± 1.0 in the aspirin group (76.6% of these < 12 weeks of gestation, 88.5% < 20 weeks of gestation). As study outcome total pregnancy loss reported; no specification for early and late loss reported. Trial registry: trial not registered in clinical trial registry, but clinical trial registry at time of publication non‐existing. No published study protocol. Dates of study: recruitment period not specified, publication in 1996. Funding sources: not stated Declarations of interest: not stated Authors report that treatment was initiated at the first documented pregnancy test, to eliminate selection bias. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Non‐random alternative assignment of treatment. |
| Allocation concealment (selection bias) | High risk | No concealment of allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | 600 women evaluated, 50 consented to study participation; exclusions, reasons for exclusion and numbers included in the analysis at each stage were not reported. Unclear whether all evaluated participants started low‐dose aspirin before conception, prior to randomisation. Analysis by intent‐to‐treat and loss to follow‐up unclear. |
| Selective reporting (reporting bias) | Unclear risk | Trial not registered in clinical trial registry, but clinical trial registry at time of publication non‐existing, therefore unclear risk. No published study protocol. |
| Other bias | Low risk | No indication of other sources of bias |
Kutteh 1996b.
| Study characteristics | ||
| Methods | Single‐centre, quasi‐randomised, non‐blinded, non‐placebo controlled trial (N = 50) | |
| Participants |
Inclusion criteria 1) Desire to become pregnant 2) Agreement to be completely evaluated 3) ≥ 3 documented pregnancy losses 4) Presence of antiphospholipid antibodies IgG ≥ 27 GPL (> 2.5 multiples of the median) on 2 separate occasions 5) Consent to treatment protocol Exclusion criteria Systemic lupus erythematosus, a positive test for lupus anticoagulant, an allergy to aspirin, a documented bone disorder, another abnormal test result that was not corrected aspirin allergy, refused treatment. |
|
| Interventions | Aspirin 81 mg/day plus heparin 5000 U twice daily sc adjusted to maintain the PTT at 1.2 to 1.5 times the baseline (high dose) (N = 25) versus Aspirin 81 mg/day + heparin 5000 U twice daily sc adjusted to maintain the PTT at the upper limit of normal (low dose) (N = 25) |
|
| Outcomes | Obstetric complications (preterm birth, intrauterine growth retardation and maternal complications (gestational diabetes, major and minor bleeding, thrombocytopenia, pre‐eclampsia) | |
| Notes | Mean daily dose in low‐dose heparin group 8127 ± 2389 U twice daily; mean daily dose in high‐dose heparin group 13300 ± 3500 U twice daily. Aspirin commenced before conception, heparin commenced at the first confirmed pregnancy test. Treatment was continued until delivery and heparin continued for 3 weeks postpartum. Mean total prior miscarriages per patient was 3.6 ± 1.0 in the low‐dose UFH + aspirin group (92.9% of these < 20 weeks of gestation) versus 3.9 ± 1.4 in the aspirin group (91.2% of these < 20 weeks of gestation). As study outcome total pregnancy loss reported; no specification for early and late loss reported. Trial registry: trial not registered in clinical trial registry, but clinical trial registry at time of publication non‐existing. No published study protocol. Dates of study: recruitment period not specified, publication in 1996. Funding sources: not stated Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | The first 25 women had heparin dosages adjusted periodically to maintain the baseline PTT at 1.2 to 1.5 times baseline (HD heparin). The second 25 women had heparin dosages adjusted periodically to maintain the PTT at the allocated to upper limits of the normal range (LD heparin). |
| Allocation concealment (selection bias) | High risk | No concealment of allocation. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding not reported, but knowledge of treatment allocation unlikely to influence outcome live birth. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding not reported, but knowledge of treatment allocation unlikely to influence outcome live birth. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Over 750 women evaluated, 50 consented to study participation; exclusions, reasons for exclusion and numbers included in the analysis at each stage were not reported. Unclear whether all evaluated participants started low‐dose aspirin before conception, prior to randomisation. Analysis by intent‐to‐treat and loss to‐follow‐up unclear. |
| Selective reporting (reporting bias) | Unclear risk | Trial not registered in clinical trial registry, but clinical trial registry at time of publication non‐existing, therefore unclear risk. No published study protocol. |
| Other bias | Low risk | No indication of any other source of bias. |
Laskin 2009.
| Study characteristics | ||
| Methods | Open‐label randomised controlled trial (N = 88). Subgroup with aPL antibodies N = 42 | |
| Participants |
Inclusion criteria 1) aged 18 to 44 years at time of randomisation 2) history of ≥ 2 unexplained consecutive pregnancy losses prior to 32 weeks' gestation 3) presence of at least 1 of the following: ANA, antiphospholipid antibodies (aCL IgG > 15 GPL or IgM > 25 MPL and/or LAC positivity, tested on 2 occasions at least 8 weeks apart), or an inherited thrombophilia 4) confirmed pregnancy by either 2 appropriately rising quantitative beta human chorionic gonadotropin (beta hCG) tests performed 48 hours apart or by ultrasound confirming fetal heart activity Exclusion criteria Systemic lupus erythematosus (fulfilling American College of Rheumatology classification criteria), known peptic ulcer disease (within the last 5 years), sensitivity to aspirin or heparin obtained by self‐report, bone mineral density z score <‐ 2.5, known platelet function abnormality, previous thromboembolic event requiring ongoing anticoagulant therapy including heparin/aspirin/warfarin verified in medical records, genetic/anatomic/hormonal aetiology for pregnancy loss was identified by (respectively) karyotype analysis of both partners, hysterosalpingogram/sonohysterogram, and a hormonal evaluation (which included either an endometrial biopsy or loss while taking progesterone or clomiphene therapy or mid luteal phase serum progesterone levels timed appropriately), geographic distance from the clinic and hospitals in Toronto/Hamilton, failure to consent. |
|
| Interventions | LMWH (dalteparin) 5000 U/day sc + aspirin 81 mg/day (N = 22) versus Aspirin 81 mg/day (N = 20) |
|
| Outcomes | Live birth | |
| Notes | 42 of 88 randomised participants had persistent presence of antiphospholipid antibodies, of whom 22 were randomised to LMWH + aspirin and 20 were randomised to aspirin alone. Aspirin and LMWH started at randomisation (after confirmed pregnancy) and continued until 35 weeks of gestation. Authors have been contacted to provide information on the secondary outcomes for the subgroup of aPL‐positive participants 32/45 in the LMWH + aspirin group had a history of early losses (≤ 14 weeks of gestation) versus 34/43 in the aspirin group. 4/45 in the LMWH + aspirin group had a still birth (20‐32 weeks of gestation) versus 7/43 in the aspirin group. Pregnancy loss in 10/45 in the LMWH + aspirin group (7/10 ≤ 14 weeks of gestation, 2/10 ectopic pregnancy, 1 stillbirth) versus 9/43 in the aspirin group (8/9 ≤ 14 weeks of gestation, 1 stillbirth). Trial registry: study registered at clinicaltrials.gov [NCT 00564174] Dates of study: recruitment period 2000‐2004, publication in 2009. Funding sources: Canadian Institute of Health Research (CIHR) Rx&D grant (PCT 37749) and by a grant from Pfizer Canada (formerly Pharmacia, Canada). LMWH was supplied by Pfizer Canada. Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Central randomisation. Stratified by presence or absence of aPL, and early (≤ 14 weeks) versus late (15‐32 weeks) losses. Women with history of both early and late losses were assigned to the late stratum. |
| Allocation concealment (selection bias) | Low risk | Adequate allocation concealment; central randomisation, communication by telephone. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusions, reasons for exclusion and numbers included in the analysis at each stage were reported; no loss to follow‐up, all participants analysed. |
| Selective reporting (reporting bias) | Low risk | Study registered at clinicaltrials.gov [NCT 00564174]. All of the study's pre‐specified outcomes and all expected outcomes of interest were reported. |
| Other bias | Low risk | Multicentre trial (2 centres). |
Pattison 2000.
| Study characteristics | ||
| Methods | Single‐centre, double‐blind, randomised, placebo‐controlled trial (N = 40) | |
| Participants |
Inclusion criteria 1) ≥ 3 miscarriages 2) persistent positive aPL antibody pre‐pregnancy or early during index pregnancy; anticardiolipin antibodies IgG ≥ 5 GPL units or IgM ≥ 5 MPL units or presence of LAC (aPTT, dRVVT or KCT). Exclusion criteria History of thrombosis, systemic lupus erythematosus, current or planned therapy with corticosteroids, NSAIDs, heparin or marine lipids. |
|
| Interventions | Aspirin 75 mg/day (N = 20) versus Placebo (N = 20) |
|
| Outcomes | Live birth, antenatal outcomes (bleeding, hypertension, preterm birth, caesarean delivery) and neonatal outcomes (birthweight, small‐for‐gestational age, neonatal admission, congenital anomalies) | |
| Notes | Randomisation after confirmation of pregnancy, if antiphospholipid antibodies were positive before pregnancy or detected during pregnancy. Aspirin and placebo commenced 50 and 44 days respectively after last menstrual period, duration of treatment was not defined. Overall percentage of previous pregnancy losses 80.7% in the aspirin group versus 74.8% in the placebo group. Median first‐trimester losses 3 (interquartile range 1.5) in the aspirin group versus 4.5 (3) in the placebo group. As study outcome total pregnancy loss reported; no specification for early and late loss reported. Trial registry: trial not registered in clinical trial registry, but clinical trial registry at time of publication non‐existing. No published study protocol. Dates of study: recruitment over a period of 39 months, no further specification. Publication in 2000. Funding sources: not stated Declarations of interest: not stated |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated list of study numbers. |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Blinding by placebo. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding by placebo. |
| Incomplete outcome data (attrition bias) All outcomes | High risk | In each arm 5/25 (20%) of participants were excluded because of inappropriate inclusion. Analyses were performed with and without these participants but results from included participants only published. No analysis by intent‐to‐treat. No loss to follow‐up. |
| Selective reporting (reporting bias) | Unclear risk | Results from included participants only published. Insufficient data to assess whether all outcomes were reported. Trial not registered in clinical trial registry, but clinical trial registry at time of publication non‐existing. No published study protocol. |
| Other bias | Low risk | No indication of any other source of bias. |
Rai 1997.
| Study characteristics | ||
| Methods | Single‐centre, randomised, non‐blinded, non‐placebo controlled trial (N = 90) | |
| Participants |
Inclusion criteria
1) history of ≥ 3 consecutive miscarriages
2) positive antiphospholipid antibodies on at least 2 occasions more than 8 weeks apart before becoming pregnant, determined by anticardiolipin antibodies IgG ≥ 5 GPL or IgM ≥ 3 MPL or a positive LAC (aPTT, dRVVT ratio ≥ 1.1 confirmed by platelet neutralisation ‐ decrease of >/= 10% of ratio). Exclusion criteria Previous thromboembolism, systemic lupus erythematosus, uterine abnormality detected on ultrasound, hypersecretion of luteinising hormone, multiple pregnancy, abnormal karyotype of either partner. |
|
| Interventions | Unfractionated heparin 5000 U twice daily sc + aspirin 75 mg/day (N = 45) versus Aspirin 75 mg/day (N = 45) |
|
| Outcomes | Live birth | |
| Notes | Aspirin commenced in all participants after positive pregnancy test. Heparin commenced in heparin only group after randomisation.
Randomisation occurred when fetal heart activity was noted on ultrasound (6.6 weeks in aspirin group and 6.7 weeks in aspirin/heparin group). Treatment continued until 34 weeks of gestation. Median number of previous miscarriages was 4 (range 3 to 15) in the heparin + aspirin group versus 4 (range 3 to 8) in the aspirin group. 29/45 in the heparin + aspirin group had first trimester miscarriages only, 13/45 first and second trimester miscarriages. 31/34 in the aspirin group had first trimester miscarriages only, 13/45 first and second trimester miscarriages. 13/45 pregnancy losses in the UFH + aspirin group (median gestational age at miscarriage 9.4 weeks, 11/13 < 14 weeks of pregnancy) versus 26/45 in the aspirin group (median gestational age at miscarriage 8.3 weeks, 24/26 < 14 weeks of pregnancy). Trial registry: trial not registered in clinical trial registry, but clinical trial registry at time of publication non‐existing. No published study protocol. Dates of study: recruitment period not specified, publication in 1997. Funding sources: Arthritis and Rheumatism Council UK Declarations of interest: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated random number list |
| Allocation concealment (selection bias) | Low risk | Central randomisation |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusions, reasons for exclusion and numbers included in the analysis at each stage were reported; no loss to follow‐up. All participants remained in their originally allocated treatment group and outcome of all pregnancies were analysed. |
| Selective reporting (reporting bias) | Unclear risk | Trial not registered in clinical trial registry, but clinical trial registry at time of publication non‐existing. No published study protocol. |
| Other bias | Low risk | No indication of any other source of bias. |
Stephenson 2004.
| Study characteristics | ||
| Methods | Randomised pilot trial (N = 28). Subgroup of participants that conceived (N = 26) | |
| Participants |
Inclusion criteria 1) history of ≥ 3 unexplained recurrent miscarriages of earlier than 10 weeks' gestation 2) persistently positive antiphospholipid antibodies; anticardiolipin antibodies IgG or IgM or lupus anticoagulant, drawn at least 6 weeks apart Exclusion criteria Parental structural chromosome abnormality, anatomical factor (uterine septum, intrauterine adhesions, submucous fibroid), concomitant inherited thrombophilia, prior heparin use. |
|
| Interventions | Aspirin 81 mg/day preconceptionally + LMWH (dalteparin) 2500 IU once daily sc luteal phase; after conception aspirin 81mg/day + LMWH (dalteparin) 2500 IU once daily sc in first trimester, 5000 IU once daily sc in second trimester, 7500 IU once daily sc in third trimester (N = 13) versus Aspirin 81 mg/day preconceptionally + unfractionated heparin 5000 IU twice daily sc in luteal phase; after conception aspirin 81 mg/day + unfractionated heparin 5000 IU twice daily sc first trimester, 7500 IU sc twice daily second trimester, 10,000 IU twice daily sc third trimester (N = 13) |
|
| Outcomes | Live birth | |
| Notes | Aspirin was instituted preconceptionally and continued indefinitely. Heparin was started in the luteal phase for a maximum of 3 cycles and continued 6 weeks postpartum. 13 of 14 women randomised to dalteparin had at least 1 pregnancy in the trial, 13 of 14 women randomised to UFH had at least 1 pregnancy in the trial. 1 woman in the dalteparin group and 2 women in the UFH group had a second pregnancy while trial in progress. 3 women in the UFH group had a third pregnancy and 1 woman in the UFH group had a 4th pregnancy while trial in progress. Mean number of previous miscarriages in the aspirin plus LMWH group 3.8 (range 3 to 7) versus 3.9 (range 3 to 7) in the aspirin plus UFH group. As study outcome total pregnancy loss reported; no specification for early and late loss reported. Trial registry: trial not registered in clinical trial registry, but clinical trial registry at time of publication non‐existing. No published study protocol. Dates of study: recruitment period June 1998 to March 2001, publication 2004. Funding sources: British Columbia Medical Services Foundation grant support and Pharmacia Canada donation of Fragmin. Declarations of interest: none |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Random numbers table with blocks of 12. |
| Allocation concealment (selection bias) | Low risk | Central randomisation. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | No blinding, but knowledge of treatment allocation unlikely to influence outcome live birth. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Exclusions and reasons for exclusion were reported. The numbers included in the analysis at each stage (compared with the total randomised participants) were reported. Missing data were balanced across groups. |
| Selective reporting (reporting bias) | Unclear risk | Trial not registered in clinical trial registry, but clinical trial registry at time of publication non‐existing. No published study protocol. |
| Other bias | Low risk | No indication of any other source of bias. |
aCL: anticardiolipin; aPL: antiphospholipid antibodies; aPTT: activated partial thromboplastin time; BMI: body mass index; GPI: glycoprotein‐1; GPL: IgG phospholipids; IgG: immunoglobulin G; IgM: immunoglobulin M; IU: international units; IUFD: Intrauterine fetal death; IUGR: Intrauterine growth restriction; LAC: lupus anticoagulant; LMWH: low‐molecular‐weight heparin; MPL: IgM phospholipids; NSAIDS: nonsteroidal anti‐inflammatory drugs; PTT: partial thromboplastin time; SC: subcutaneous; UFH: unfractionated heparin.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agarwal 2018 | Different study population: women with inherited thrombophilia, no APS |
| Branch 2000 | Different intervention: heparin + low‐dose aspirin + intravenous immunoglobulin versus heparin + low‐dose aspirin + placebo |
| Bu 2009 | Abstract only; unclear whether randomised study or persistent presence of antiphospholipid antibodies. Insufficient data available to determine study eligibility. |
| Carta 2005 | Different intervention: low‐dose aspirin versus fish oil derivatives |
| Christiansen 1995 | No antiphospholipid antibodies detected and different intervention (intravenous immunoglobulin) |
| Clark 2009 | Different outcome: thrombotic sequelae after 20 years |
| Cowchock 1992 | Different intervention: low‐dose heparin versus prednisone 40 mg daily |
| Cowchock 1997 | No associated signs or symptoms of the antiphospholipid antibody syndrome, i.e. no recurrent pregnancy loss |
| De Veciana 2001 | Prospective longitudinal study, with different study population (women treated with prophylactic anticoagulation throughout pregnancy) and different study outcome (increase in LMWH dose, both dosing frequency and total daily dose) |
| De Vries 2012 | Women with antiphospholipid antibodies randomised into a separate study |
| Dendrinos 2007 | Abstract only, different study population: women with a history of recurrent pregnancy loss and at least 1 factor of thrombophilic disorder, APS not specified. Insufficient data available to determine study eligibility. |
| Dendrinos 2009 | Different intervention: LMWH + low‐dose aspirin versus intravenous immunoglobulin |
| Eid 2019 | Evaluation of different timing of initiation of low‐molecular weight heparin administration during pregnancy; early LMWH initiation once positive pregnancy test (week 5 of gestation) versus late LMWH initiation after sonographic confirmation of fetal cardiac pulsation (week 7 of gestation). |
| Ensom 2004 | Different study population: women with APS contemplating pregnancy, obstetric APS or recurrent miscarriage not specified Different outcome: drug exposure throughout pregnancy |
| Fu 2004 | Different intervention: aspirin + prednisone versus heparin |
| Geva 1998 | Different intervention: prednisone 10 mg + aspirin 100 mg daily versus no treatment Different endpoint: in‐vitro fertilisation embryo transfer failure |
| Gibbins 2018 | Different study design: cohort study |
| Goel 2006 | No persistent presence of antiphospholipid antibodies |
| Golding 1998 | Different study population: primiparae, no APS, no recurrent miscarriage Different outcome: occurrence of pre‐eclampsia and intrauterine growth retardation |
| Gris 1995 | Different study population: primary early recurrent unexplained miscarriages, antiphospholipid antibody positive excluded Different intervention: enoxaparin versus phenformin‐like substance Different outcome: fibrinolytic response, number of patients becoming pregnant, number of full‐term pregnancies |
| Guo 2013 | No abstract or full text retrievable; unclear whether randomised study. Insufficient data available to determine study eligibility. |
| Ismail 2016 | Evaluation of pre‐conception thromboprophylaxis: LMWH plus aspirin pre‐conception versus placebo pre‐conception. All patients received LMWH plus aspirin once pregnancy was confirmed. |
| Kaaja 1993 | Different study population: pregnant women with systemic lupus erythematosus Different intervention: production of prostacyclin and thromboxane |
| Kaandorp 2010 | Women with unexplained recurrent miscarriage, no APS |
| Kahwa 2006 | Prevalence survey with a different study population (primiparae, no APS, no recurrent miscarriage) |
| Kim 1997 | Different intervention: aspirin versus aspirin + prednisolone |
| Laskin 1997 | Different intervention: prednisone + aspirin versus placebo |
| Mahmoud 2004 | Different study population: women with recurrent pregnancy loss, no antiphospholipid antibodies Different intervention: intravenous IgG Different outcome: effects of IgG infusion on peripheral T‐cell subpopulations |
| Malathi 2011 | Abstract only; no full text retrievable. Unclear whether persistent presence of antiphospholipid antibodies. Insufficient data available to determine study eligibility. |
| Malinowski 2003 | Abstract only, no full text retrievable. Unclear whether persistent presence of antiphospholipid antibodies. Insufficient data available to determine study eligibility. |
| Mankuta 1999 | Abstract only, no full text retrievable. Different intervention (prednisone) according to abstract. |
| Mohamed 2014 | Non‐randomised study |
| Noble 2005 | Prospective, non‐randomised, controlled pilot study |
| Quenby 1992 | Abstract only, quasi‐randomised and missing information (history of recurrent fetal loss not available). Insufficient data available to determine study eligibility. |
| Radin 2017 | Different study population: healthy women attempting pregnancy, with regular menstrual cycles and had a history of 1 to 2 documented pregnancy losses, ≤ 2 live births, and no infertility Different intervention: aspirin 81mg daily for 1 to 6 menstrual cycles Different outcome: per‐cycle risk of anovulation |
| Rai 2005 | Different study intervention: low‐dose steroid + aspirin + heparin versus aspirin + heparin |
| Saad 2014 | Different study population: women with unexplained recurrent pregnancy loss, no antiphospholipid antibodies |
| Schisterman 2014 | Women with 1 or 2 pregnancy losses, APS an exclusion criterion |
| Shefras 1995 | Different study design: non‐randomised Different outcome: bone density |
| Shu 2002 | Abstract only, no full text retrievable. According to abstract different intervention: Chinese herbal medicine + human chorionic gonadotropin and progesterone versus multi‐vitamin only |
| Silver 1993 | Different intervention: prednisone + low dose aspirin versus aspirin alone |
| Tang 2012 | Different intervention: aspirin + prednisone versus aspirin + heparin |
| Triolo 2003 | Different intervention: low‐molecular‐weight heparin + aspirin versus intravenous immunoglobulin |
| Tulppala 1997 | Different study population: women with and without detectable anticardiolipin antibodies, no persistent presence of aPL Different outcome: prostacyclin and thromboxane A2 production |
| Vahid 1999 | Different study population: women with unexplained recurrent abortions, no APS Different intervention: acetylsalicylic acid and prednisolone before and during pregnancy |
| van Hoorn 2016 | Recurrent pregnancy loss not an inclusion criterion |
| Vaquero 2001 | Different intervention: prednisone + low‐dose aspirin versus intravenous immunoglobulin |
| Visser 2011 | Women with or without thrombophilia, no antiphospholipid antibodies |
| Xiao 2013 | Different intervention: prednisone + aspirin versus prednisone + aspirin + LMWH + intravenous immunoglobulin Different study design: clinical comparative study |
| Zhou 2012 | No abstract or full text retrievable; unclear whether randomised study. Insufficient data available to determine study eligibility. |
aPL: antiphospholipid antibodies; APS: antiphospholipid syndrome; IgG: immunoglobulin; LMWH: low‐molecular‐weight heparin.
Characteristics of ongoing studies [ordered by study ID]
Abdelhafez 2014.
| Study name | Use of warfarin after the first trimester in pregnant women with antiphospholipid syndrome |
| Methods | Open‐label randomised controlled trial |
| Participants |
Inclusion criteria 1) 20‐38 years of age 2) Pregnant women with APS diagnosed according to the revised classification criteria for APS in 2006 in Sydney, Australia 3) Early pregnancy body weight is 50 kg to 90 kg Exclusion criteria Systemic lupus erythematosus, active or a history of thromboembolic disorders |
| Interventions | Enoxaparin (LMWH) 40 mg/day sc versus enoxaparin 40 mg/day sc in first trimester, then warfarin (3 mg/day to 5 mg/day) until termination of pregnancy |
| Outcomes |
Primary outcome Fetal loss from 20 to 42 weeks gestational age Secondary outcomes Preterm delivery from 20 to 34 weeks gestational age, intrauterine growth restriction at birth, congenital fetal malformations at birth, haemorrhagic complications after 12 weeks gestational age up to birth, thromboembolic complications after 12 weeks gestational age up to birth |
| Starting date | November 2014 |
| Contact information | Principal Investigator: Dr. Mohamed I Eid ‐ Mansoura University, Egypt Study Director: Dr. Mohamed S Abdelhafez ‐ Mansoura University, Egypt |
| Notes | NCT02303171 |
Rodger 2017.
| Study name | Antiphospholipid syndrome low‐molecular‐weight heparin pregnancy loss evaluation: the pilot study (APPLE) |
| Methods | Randomised controlled trial (feasibility study) |
| Participants |
Inclusion criteria 1) Confirmed pregnancy 2) 18 years or older 3) 2 or more unexplained pregnancy loss before the 10th week of gestation, AND/OR 1 or more unexplained pregnancy loss at or beyond the 10th week of gestation 4) 1 or more APS laboratory criteria present, according to the revised Sapporo criteria Exclusion criteria Greater than 11 weeks + 6 days gestational age at time of randomisation, indication(s) for prophylactic or therapeutic‐dose anticoagulation, contraindication to heparin or aspirin, received 7 or more doses of LMWH, previous participation in the trial, geographic inaccessibility, refused consent. |
| Interventions | Tinzaparin (LMWH) 4500 IU sc daily until 20 weeks' gestation and then 4500 IU sc twice daily until 37 weeks' gestation + aspirin 81 mg daily versus aspirin 81 mg daily until delivery |
| Outcomes | The primary feasibility outcome of the pilot trial is the mean recruitment rate per centre per month. |
| Starting date | November 6, 2017 |
| Contact information | Principal Investigator: Marc Rodger, MD ‐ Ottawa Hospital Research Institute, Canada Principal Investigator: Leslie Skeith, MD ‐ Ottawa Hospital Research Institute, Canada |
| Notes | NCT03100123 |
APS: antiphospholipid syndrome; IU: international units; LMWH: low‐molecular‐weight heparin; sc: subcutaneous.
Differences between protocol and review
Pregnancy loss (total, early loss < 24 weeks, late loss ≥ 24 weeks) was stated as the primary outcome in the protocol. All trials reported live birth rates and most pregnancy loss as well, with only one trial reporting early or late pregnancy loss separately. Since pregnancy loss and live birth rate in fact describe the same outcome, we decided to redefine our primary outcome to live birth. Live birth and pregnancy loss are highly interrelated and in fact describe the (inverse of the) same outcome and the effects of the evaluated interventions. However, the size of the effect estimate will differ as it is an effect estimate of a relatively frequent event, i.e. live birth, as opposed to a less frequent event, i.e. pregnancy loss. Live birth is a patient‐relevant outcome and the included studies all focus on live birth rate as well. We decided to redefine our primary outcome to live birth, as this also allows for a comparison with other studies in the area of recurrent miscarriage that have “ongoing pregnancy” (for instance after 12 or 20 weeks) as a primary outcome. Pregnancy loss is reported as a secondary outcome as well in a separate analysis for each comparison, in line with a recent Cochrane Review on progestogen for prevention of recurrent miscarriage (Haas 2019).
Our protocol stated two main comparisons; 1) heparin or aspirin, or both versus no treatment or placebo and 2) heparin with or without aspirin versus aspirin. We aimed to compare aspirin, heparin (either UFH or LMWH), a combination of heparin and aspirin with another or no treatment or both, as described in our protocol in the 'Types of interventions' section. For main comparison 2, heparin with or without aspirin versus aspirin alone, we did an additional subgroup analysis per type of heparin, as we feel that the outcomes per type of heparin are more relevant for clinical practice than the overall outcome for all heparins combined. Over the course of almost 25 years, clinical practice with regard to heparin treatment has changed from using UFH subcutaneously to the current standard of care of LMWH. For this reason, we consider reporting the subgroup results for both UFH and LMWH to be a more granular description of the evidence and highly relevant for current clinical practice.
We decided to split up main comparison 2, leading to two main comparisons and five comparisons overall in the current review 1) heparin or aspirin, or both versus no treatment or placebo, 2) heparin (LMWH or UFH) plus aspirin versus aspirin, 3) heparin versus aspirin, 4) LMWH plus aspirin versus UFH plus aspirin and 5) higher dose of heparin (LMWH or UFH) plus aspirin versus lower dose of heparin (LMWH or UFH) plus aspirin. We have GRADED all pre‐specified outcomes and produced a Summary of findings table for main comparison 1 and 2.
In addition, according to our protocol, participants would be pregnant women with recurrent (two or more, which do not have to be consecutive) pregnancy losses in presence of persistent (on two separate occasions, at least 12 weeks apart) aPL. As the criteria for APS and testing for aPL changed (Miyakis 2006), studies prior to 2006 also evaluated women with persistent aPL, tested six to eight weeks apart. We decided to include all studies in which women had persistent antibodies; i.e. persistent presence of aPL, tested on two separate occasions, independent of the time‐frame.
Contributions of authors
Eva N Hamulyák: prepared the current review; performed independent data extraction and quality assessment of the included trials, and commented on all drafts of the review.
Luuk JJ Scheres: prepared the current review; performed independent data extraction and quality assessment of included trials; commented on the drafts for this review.
Mauritia C Marijnen: prepared the current review; performed independent data extraction and quality assessment of included trials.
Mariette Goddijn: commented on all drafts of the review
Saskia Middeldorp: is the guarantor of the review; third reviewer for quality assessment; commented on all drafts of the review.
Sources of support
Internal sources
-
Department of Vascular Medicine, Netherlands
Internal support
External sources
-
Netherlands Organisation for Scientific Research (NWO), Netherlands
Saskia Middeldorp is supported by a VIDI grant from The Netherlands Organisation for Health Research and Development (016.126.364)
Declarations of interest
Eva N Hamulyák: none known
Luuk JJ Scheres: is a PhD‐candidate of the CREW project (2013T083) funded by the Netherlands Heart Foundation
Mauritia C Marijnen: none known
Mariette Goddijn: has received travel expenses from European Society of Human Reproduction and Embryology regarding Executive Committee work (Amsterdam‐Brussels) until july 2019. She works at both locations of the Department of Reproductive Medicine of the Amsterdam UMC (Location AMC and location VUMC). Location VUMC has received several research and educational grants from Guerbet, Merck and Ferring, outside the scope of the submitted work.
Saskia Middeldorp has received a Netherlands Organisation for Scientific Research (NWO) personal Innovation VIDI grant (paid to her institution) on Thrombophilia and Reproduction from the Netherlands Organisation for Scientific Research (NWO). She has carried out paid consultancy (paid to her institution, and not in relation to this review) for Daiichi Sankyo (as a member of the Writing Committee of the Hokusai VTE study (published in 2013)); Daiichi Sankyo, Bayer, and Janssen (local investigator for various treatment and prophylaxis studies in VTE patients). She has received payment (to her institution) for lectures on VTE treatment from Bayer, BMS/Pfizer, Boehringer Ingelheim, Daiichi Sankyo, Sanofi, and for developing educational presentations for Bayer, Aspen, Daiichi Sankyo, BMS/Pfizer). Saskia also has grants/grants for investigator‐initiated studies from Aspen, Daiichi Sankyo and Bayer, all paid to her institution.
New
References
References to studies included in this review
Alalaf 2012 {published data only}
- Alalaf S. Bemiparin versus low dose aspirin for management of recurrent early pregnancy losses due to antiphospholipid antibody syndrome. Archives of Gynecology and Obstetrics 2012; 285(3):641-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bao 2017 {published data only}
- Bao SH, Zhou Q, Frempong ST, Tu WY, Sheng SL, Liao H. Use of d-dimer measurement to guide anticoagulant treatment in recurrent pregnancy loss associated with antiphospholipid syndrome. American Journal of Reproductive Immunology 2017; 78(6):e12770. [DOI] [PubMed] [Google Scholar]
Farquharson 2002 {published data only}ISRCTN55179279
- Farquharson R, ISRCTN55179279. Antiphospholipid syndrome in pregnancy: a controlled treatment trial. www.isrctn.com/ISRCTN55179279 (first received 23 January 2004).
- Farquharson RG, Quenby S, Greaves M. Antiphospholipid syndrome in pregnancy: a randomized, controlled trial of treatment. Obstetrics & Gynecology 2002; 100:408-13. [DOI] [PubMed] [Google Scholar]
- Farquharson RG. Antiphospholipid syndrome in pregnancy: a controlled treatment trial. Journal of Obstetrics and Gynaecology 2001; 21 Suppl 1:S22. [Google Scholar]
Fouda 2010 {published data only}
- Fouda UM, Sayed AM, Ramadan DI, Fouda IM. Efficacy and safety of two doses of low molecular weight heparin (enoxaparin) in pregnant women with a history of recurrent abortion secondary to antiphospholipid syndrome. Journal of Obstetrics and Gynaecology 2010; 30(8):842-6. [DOI] [PubMed] [Google Scholar]
Fouda 2011 {published data only}
- Fouda UM, Sayed AM, Abdou AM, Ramadan DI, Fouda IM, Zaki MM. Enoxaparin versus unfractionated heparin in the management of recurrent abortion secondary to antiphospholipid syndrome. International Journal of Gynecology & Obstetrics 2011; 112(3):211-5. [ClinicalTrials.gov: NCT01051778]] [DOI] [PubMed] [Google Scholar]
- NCT01051778. Low-molecular-weight heparin (LMWH) versus unfractionated heparin (UFH) in pregnant women with history of recurrent abortion secondary to antiphospholipid syndrome. clinicaltrials.gov/ct2/show/results/NCT01051778 (first received 20 January 2010).
Kutteh 1996a {published data only}
- Kutteh WH. Antiphospholipid antibody-associated recurrent pregnancy loss: treatment with heparin and low-dose aspirin is superior to low-dose aspirin alone. American Journal of Obstetrics and Gynecology 1996; 174(5):1584-9. [DOI] [PubMed] [Google Scholar]
Kutteh 1996b {published data only}
- Kutteh WH, Ermel LD. A clinical trial for the treatment of antiphospholipid antibody-associated recurrent pregnancy loss with lower dose heparin and aspirin. American Journal of Reproductive Immunology 1996; 35:402-7. [DOI] [PubMed] [Google Scholar]
Laskin 2009 {published data only}
- Laskin CA, NCT00564174. A randomized controlled trial comparing low molecular weight heparin and aspirin to aspirin alone in women with unexplained recurrent pregnancy loss. clinicaltrials.gov/ct2/show/NCT00564174 (first received 27 November 2007).
- Laskin CA, Spitzer KA, Clark CA, Crowther MR, Ginsberg JS, Hawker GA, et al. Low molecular weight heparin and aspirin for recurrent pregnancy loss: results from the randomized, controlled HepASA Trial. Journal of Rheumatology 2009; 36(2):279-87. [DOI] [PubMed] [Google Scholar]
Pattison 2000 {published data only}
- Pattison NS, Chamley LW, Birdsall M, Zanderigo AM, Liddell HS, McDougall J. Does aspirin have a role in improving pregnancy outcome for women with the antiphospholipid syndrome? A randomized controlled trial. American Journal of Obstetrics and Gynecology 2000; 183:1008-12. [DOI] [PubMed] [Google Scholar]
Rai 1997 {published data only}
- Cohen H. Randomized trial of aspirin versus aspirin and heparin in pregnant women with the antiphospholipid syndrome. Annales de Medecine Interne 1996; 147 Suppl 1:44. [PubMed] [Google Scholar]
- Rai R, Cohen H, Dave M, Regan L. Randomised controlled trial of aspirin and aspirin plus heparin in pregnant women with recurrent miscarriage associated with phospholipid antibodies (or antiphospholipid antibodies). BMJ 1997; 314:253-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rai R, Regan L. Antiphospholipid antibodies and recurrent miscarriage. Acta Obstetricia et Gynecologica Scandinavica 1997; 76(Suppl(167:4)):6. [Google Scholar]
- Rai RS, Cohen H, Regan L. Prospective randomized trial of aspirin versus aspirin + heparin in pregnant women with a history of recurrent miscarriage in association with antiphospholipid antibodies. Human Reproduction 1996; 11:25. [Google Scholar]
- Rai RS, Regan L, Dave M, Cohen H. Prospective randomised trial of aspirin versus aspirin plus heparin in pregnant women with the antiphospholipid syndrome [abstract]. British Journal of Haematology 1996; 93(Suppl 1):5. [Google Scholar]
Stephenson 2004 {published data only}
- Stephenson MD, Ballem PJ, Tsang P, Purkiss S, Ensworth S, Houlihan E, et al. Treatment of antiphospholipid antibody syndrome (aps) in pregnancy: a randomized pilot trial comparing low molecular weight heparin to unfractionated heparin. Journal of Obstetrics & Gynaecology Canada: JOGC 2004; 26(8):729-34. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Agarwal 2018 {published data only}
- Agarwal N, CTRI/2018/04/013167. Screening for inherited thrombophilia in recurrent pregnancy loss and role of therapy with aspirin and low molecular weight heparin (LMWH). ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=22008 (first received 11 April 2018).
Branch 2000 {published data only}
- Branch DW, Peaceman AM, Druzin M, Silver RK, El-Sayed Y, Silver RM, et al, for the Pregnancy Loss Study Group. A multicenter, placebo-controlled pilot study of intravenous immune globulin treatment of antiphospholipid syndrome during pregnancy. American Journal of Obstetrics and Gynecology 2000; 182(1 Pt 1):122-7. [DOI] [PubMed] [Google Scholar]
Bu 2009 {published data only}
- Bu MX. Clinical observation 40 autoimmune habitual abortion patients with low molecular weight heparin calcium. China Practical Medicine 2009; 4:73-4. [Google Scholar]
Carta 2005 {published data only}
- Carta G, Iovenitti P, Falciglia K. Recurrent miscarriage associated with antiphospholipid antibodies: prophylactic treatment with low-dose aspirin and fish oil derivates. Clinical & Experimental Obstetrics & Gynecology 2005; 32(1):49-51. [PubMed] [Google Scholar]
Christiansen 1995 {published data only}
- Christiansen OB, Mathiesen O, Husth M, Rasmussen KL, Ingerslev HJ, Lauritsen JG, et al. Placebo-controlled trial of treatment of unexplained secondary recurrent spontaneous abortions and recurrent late spontaneous abortions with iv immunoglobulin. Human Reproduction 1995; 10:2690-5. [DOI] [PubMed] [Google Scholar]
Clark 2009 {published data only}
- Clark CA, Spitzer KA, Laskin CA. Longterm follow-up of asa/p trial participants: no evidence of thrombotic sequelae 20 years after anti-phospholipid-associated recurrent pregnancy loss. Arthritis and Rheumatism 2009; 60(Suppl 10):1283. [Google Scholar]
Cowchock 1992 {published data only}
- Cowchock FS, Reece EA, Balaban D, Ware D, Plouffe L. Repeated fetal losses associated with antiphospholipid antibodies: a collaborative randomized trial comparing prednisone with low-dose heparin treatment. American Journal of Obstetrics and Gynecology 1992; 166:1318-23. [DOI] [PubMed] [Google Scholar]
Cowchock 1997 {published data only}
- Cowchock S, Reece EA. Do low-risk pregnant women with antiphospholipid antibodies need to be treated? Organizing Group of the Antiphospholipid Antibody Treatment Trial. American Journal of Obstetrics and Gynecology 1997; 176(5):1099-100. [DOI] [PubMed] [Google Scholar]
Dendrinos 2007 {published data only}
- Dendrinos S, Kalogirou I, Makrakis E, Theodoridis T, Mahmound EA, Christopoulou-Cokkinou V, et al. Safety and effectiveness of tinzaparin sodium in the management of recurrent pregnancy loss. Clinical and Experimental Obstetrics and Gynecology 2007; 34(3):143-5. [PubMed] [Google Scholar]
Dendrinos 2009 {published data only}
- Dendrinos S, Sakkas E, Makrakis E. Low-molecular-weight heparin versus intravenous immunoglobulin for recurrent abortion associated with antiphospholipid antibody syndrome. International Journal of Gynecology & Obstetrics 2009; 104(3):223-5. [DOI] [PubMed] [Google Scholar]
De Veciana 2001 {published data only}
- De Veciana M, Trail P, Dattel B, Slotnick RN, Abuhamad A. Dalteparin versus unfractionated heparin for prophylactic anticoagulation during pregnancy [abstract]. American Journal of Obstetrics and Gynecology 2001; 185(6 Suppl):S182. [Google Scholar]
De Vries 2012 {published data only}
- Vries JI, Pampus MG, Hague WM, Bezemer PD, Joosten JH, FRUIT Investigators. Low-molecular-weight heparin added to aspirin in the prevention of recurrent early-onset pre-eclampsia in women with inheritable thrombophilia: the FRUIT-RCT. Journal of Thrombosis and Haemostasis 2012; 10(1):64-72. [DOI] [PubMed] [Google Scholar]
- Hoorn M, Hague WM, Pampus MG, Bezemer P. Low-molecular-weight heparin added to aspirin in the prevention of recurrent early-onset preeclampsia in women with antiphospholipid antibodies. Journal of Thrombosis and Haemostasis 2013; 11(Suppl 2):435. [Google Scholar]
Eid 2019 {published data only}
- Eid MI, Abdelhafez MS, El-Refaie W, El-Zayadi AA, Samir K, Abdelrazik MM, et al. Timing of initiation of low molecular weight heparin administration in pregnant women with antiphospholipid syndrome: a randomized clinical trial of efficacy and safety. International Journal of Women's Health 2019; 11:41-7. [DOI: 10.2147/IJWH.S193293] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ensom 2004 {published data only}
- Ensom MH, Stephenson MD. Pharmacokinetics of low molecular weight heparin and unfractionated heparin in pregnancy. Journal of the Society for Gynecologic Investigation 2004; 11(6):377-83. [DOI] [PubMed] [Google Scholar]
Fu 2004 {published data only}
- Fu JH, Wang ZY, Lang FF. Study of heparin on pregnant woman with recurrent pregnant loss and positive anti-phospholipid antibody. Chinese Journal of Perinatal Medicine 2004; 7:276-8. [Google Scholar]
Geva 1998 {published data only}
- Geva E, Amit A, Lerner-Geva L, Lessing JB. Prevention of early pregnancy loss in autoantibody seropositive women [letter]. Lancet 1998; 351(9095):34-5. [DOI] [PubMed] [Google Scholar]
Gibbins 2018 {published data only}
- Gibbins KJ, Mumford SL, Sjaarda LA, Branch DW, Perkins NJ, Ye A, et al. Preconception antiphospholipid antibodies and risk of subsequent early pregnancy loss. Lupus 2018; 27(9):1437-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goel 2006 {published data only}
- Goel N, Tuli A, Choudhry R. The role of aspirin versus aspirin and heparin in cases of recurrent abortions with raised anticardiolipin antibodies. Medical Science Monitor 2006; 12(3):CR132-6. [PubMed] [Google Scholar]
Golding 1998 {published data only}
- Golding J. A randomised trial of low dose aspirin for primiparae in pregnancy. The Jamaica Low Dose Aspirin Study Group. British Journal of Obstetrics and Gynaecology 1998; 105(3):293-9. [DOI] [PubMed] [Google Scholar]
Gris 1995 {published data only}
- Gris J, Neveu S, Tailland M, Courtieu C, Mares P, Schved J. Use of a low-molecular weight heparin (enoxaparin) or of a phenformin-like substance (moroxydine chloride) in primary early recurrent aborters with an impaired fibrinolytic capacity. Thrombosis and Haemostasis 1995; 73:362-7. [PubMed] [Google Scholar]
Guo 2013 {published data only}
- Guo LJ. Study of heparin on pregnant woman with recurrent pregnant loss and positive anti-phospholipid antibody. China Practical Medicine 2013; 8:57-9. [Google Scholar]
Ismail 2016 {published data only}
- Ismail A, NCT01661439. A randomized clinical trial of using preconceptional enoxaparin and low dose aspirin 81mg in patient with antiphospholipid syndrome (aps). clinicaltrials.gov/ct2/show/record/NCT01661439 (first received 9 August 2012).
- Ismail AM, Hamed AH, Saso S, Abu-Elhasan AM, Abu-Elghar MM, Abdelmeged AN. Randomized controlled study of pre-conception thromboprophylaxis among patients with recurrent spontaneous abortion related to antiphospholipid syndrome. International Journal of Gynaecology and Obstetrics: the Official Organ of the International Federation of Gynaecology and Obstetrics 2016; 132:219-23. [DOI] [PubMed] [Google Scholar]
Kaaja 1993 {published data only}
- Kaaja R, Julkunen H, Viinikka L, Ylikorkala O. Production of prostacylin and thromboxane in lupus pregnancies: effect of small dose of aspirin. Obstetrics & Gynecology 1993; 81:327-31. [PubMed] [Google Scholar]
Kaandorp 2010 {published data only}
- Kaandorp SP, Goddijn M, Post JA, Hutten BA, Verhoeve HR, Hamulyák K, et al. Aspirin plus heparin or aspirin alone in women with recurrent miscarriage. New England Journal of Medicine 2010; 362(17):1586-96. [DOI] [PubMed] [Google Scholar]
Kahwa 2006 {published data only}
- Kahwa EK, Sargeant LA, McCaw-Binns A, McFarlane-Anderson N, Smikle M, Forrester T, et al. Anticardiolipin antibodies in Jamaican primiparae. Journal of Obstetrics and Gynaecology 2006; 26(2):122-6. [DOI] [PubMed] [Google Scholar]
Kim 1997 {published data only}
- Kim CH, Chae HD, Koo JN, Kim NY, Kang BM, Chi HS. Comparison of pregnancy outcome between low dose aspirin alone and aspirin plus prednisolone treatment in recurrent spontaneous abortion associated with antiphospholipid antibodies. Korean Journal of Obstetrics and Gynecology 1997; 40(7):1404-11. [Google Scholar]
Laskin 1997 {published data only}
- Laskin CA, Bombardier C, Hannah ME, Mandel FP, Ritchie JW, Farewell V, et al. Prednisone and aspirin in women with autoantibodies and unexplained recurrent fetal loss. New England Journal of Medicine 1997; 337(3):148-53. [DOI] [PubMed] [Google Scholar]
Mahmoud 2004 {published data only}
- Mahmoud F, Diejomaoh M, Omu A, Abul H, Haines D. Effect of IgG therapy on lymphocyte subpopulations in the peripheral blood of Kuwaiti women experiencing recurrent pregnancy loss. Gynecologic and Obstetric Investigation 2004; 58(2):77-83. [DOI] [PubMed] [Google Scholar]
Malathi 2011 {published data only}
- Malathi V. Treatment outcome in women suffering from recurrent miscarriages and antiphospholipid syndrome. In: 54th All India Congress of Obstetrics and Gynaecology; 2011 January 5-9; Hyderabad, Andhra Pradesh, India. 2011:184.
Malinowski 2003 {published data only}
- Malinowski A, Dynski MA, Maciolek-Blewniewska G, Glowacka E, Pawlowski T, Babula G. Treatment outcome in women suffering from recurrent miscarriages and antiphospholipid syndrome [Wyniki leczenia kobiet z nawracajacymi samoistnymi poronieniami i zespolem antyfosfolipidowym]. Ginekologia Polska 2003; 74(10):1213-22. [PubMed] [Google Scholar]
Mankuta 1999 {published data only}
- Mankuta D, Spitzer KA, Seaward G, Farine D, Ryan G, Clark-Soloninka CA, et al. Prednisone does not affect the biophysical score in pregnant women with autoantibodies. American Journal of Obstetrics and Gynecology 1999; 180(1 Pt 2):S163. [Google Scholar]
Mohamed 2014 {published data only}
- Mohamed KAA, Saad AS. Enoxaparin and aspirin therapy for recurrent pregnancy loss due to anti-phospholipid syndrome (APS). Middle East Fertility Society Journal 2014; 19(3):176-82. [Google Scholar]
Noble 2005 {published data only}
- Noble LS, Kutteh WH, Lashey N, Franklin RD, Herrada J. Antiphospholipid antibodies associated with recurrent pregnancy loss: prospective, multicenter, controlled pilot study comparing treatment with low-molecular-weight heparin versus unfractionated heparin. Fertility & Sterility 2005; 83(3):684-90. [DOI] [PubMed] [Google Scholar]
Quenby 1992 {published data only}
- Quenby S, Farquharson R, Ramsden G. The obstetric outcome of patients with positive anticardiolipin antibodies: aspirin vs no treatment. In: Proceedings of 26th British Congress of Obstetrics and Gynaecology; 1992 July 7-10; Manchester, UK. 1992:443.
Radin 2017 {published data only}
- Radin RG, Sjaarda LA, Perkins NJ, Silver RM, Chen Z, Lesher LL, et al. Low-dose aspirin and sporadic anovulation in the EAGeR randomized trial. Journal of Clinical Endocrinology and Metabolism 2017; 102(1):86-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rai 2005 {published data only}
- Rai R, NCT00180778. Steroids and antiphospholipid syndrome - related pregnancy loss. clinicaltrials.gov/ct2/show/record/NCT00180778 (first received 16 September 2005).
Saad 2014 {published data only}
- Saad A, Mohamed K, NCT02144064. Pregnancy outcomes in women with recurrent miscarriage treated with low dose aspirin and unfractionated heparin. clinicaltrials.gov/ct2/show/NCT02144064 (first received 21 May 2014).
Schisterman 2014 {published data only}
- Ahrens KA, Silver RM, Mumford SL, Sjaarda LA, Perkins NJ, Wactawski-Wende J, et al. Complications and safety of preconception low-dose aspirin among women with prior pregnancy losses. Obstetrics & Gynecology 2016; 127(4):689-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell MT, Sjaarda LA, Radin RG, Kuhr D, Mumford SL, Plowden TC, et al. The effects of aspirin in gestation and reproduction (eager) trial: a story of discovery. Seminars in Reproductive Medicine 2017; 35(4):344-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibbins KJ, Branch DW, Silver RM, Sjaarda LA, Mumford SL, Perkins NJ, et al. Recurrent pregnancy loss in women with and without antiphospholipid antibodies. American Journal of Obstetrics & Gynecology 2016; 214(1 Suppl):S199. [Google Scholar]
- Lesher LL, Matyas RA, Sjaarda LA, Newman SL, Silver RM, Galai N, et al. Recruitment for longitudinal, randomised pregnancy trials initiated preconception: lessons from the Effects of Aspirin in Gestation and Reproduction trial. Paediatric and Perinatal Epidemiology 2015; 29(2):162-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mone F, McAuliffe FM. Preconception low-dose aspirin and pregnancy outcomes: results from the EAGeR randomized trial. Irish Medical Journal 2015; 108(1):5. [PubMed] [Google Scholar]
- Mumford SL, Silver RM, Sjaarda LA, Wactawski-Wende J, Townsend JM, Lynch AM, et al. Expanded findings from a randomized controlled trial of preconception low-dose aspirin and pregnancy loss. Human Reproduction 2016; 31(3):657-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pugh SJ, Schisterman EF, Browne RW, Lynch AM, Mumford SL, Perkins NJ, et al. Preconception maternal lipoprotein levels in relation to fecundability. Human Reproduction 2017; 32(5):1055-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radin RG, Mumford SL, Silver RM, Lesher LL, Galai N, Faraggi D, et al. Sex ratio following preconception low-dose aspirin in women with prior pregnancy loss. Journal of Clinical Investigation 2015; 125(9):3619-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schisterman E, Silver R, Lesher L, Faraggi D, Wactawski-Wende J, Townsend J, et al. Randomized clinical trial of preconception low dose aspirin use to improve pregnancy outcomes: EAGeR (Effects of Aspirin in Gestation and Reproduction) trial. American Journal of Obstetrics and Gynecology 2013; 208(1 Suppl 1):S352. [Google Scholar]
- Schisterman EF, Mumford SL, Schliep KC, Sjaarda LA, Stanford JB, Lesher LL, et al. Preconception low dose aspirin and time to pregnancy: findings from the EAGER (Effects of Aspirin in Gestation And Reproduction) randomized trial. Journal of Clinical Endocrinology and Metabolism 2015; 100(5):1785-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schisterman EF, NCT00467363. The effects of aspirin in gestation and reproduction: a multi-center, controlled, double-blind randomized trial. clinicaltrials.gov/ct2/show/record/NCT00467363 (first received 30 April 2007).
- Schisterman EF, Silver RM, Lesher LL, Faraggi D, Wactawski-Wende J, Townsend JM, et al. Preconception low-dose aspirin and pregnancy outcomes: results from the EAGeR randomised trial. Lancet 2014; 384(9937):29-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schisterman EF, Silver RM, Mumford SL, Galai N, Wactawski-Wende J, Stanford JB. Randomized clinical trial of preconception low dose aspirin use and time-to-pregnancy: The eager trial. Fertility and Sterility 2013; 100(3 Suppl 1):S100. [Google Scholar]
- Schisterman EF, Silver RM, Perkins NJ, Mumford SL, Whitcomb BW, Stanford JB, et al. A randomised trial to evaluate the effects of low-dose aspirin in gestation and reproduction: design and baseline characteristics.[Erratum appears in Paediatr Perinat Epidemiol. 2014 May;28(3):275]. Paediatric and Perinatal Epidemiology 2013; 27(6):598-609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver RM, Ahrens K, Wong LF, Perkins NJ, Galai N, Lesher LL, et al. Low-dose aspirin and preterm birth: a randomized controlled trial. Obstetrics and Gynecology 2015; 125(4):876-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sjaarda L, Mitchell E, Mumford SL, Radin R, Perkins NJ, Galai N, et al. Preconception low dose aspirin treatment improves clinical pregnancy and live birth in women with higher systemic inflammation. Fertility and Sterility 2015; 104(3 Suppl 1):e349. [Google Scholar]
- Sjaarda LA, Radin RG, Silver RM, Mitchell E, Mumford SL, Wilcox B, et al. Preconception low-dose aspirin restores diminished pregnancy and live birth rates in women with low grade inflammation: a secondary analysis of a randomized trial. Journal of Clinical Endocrinology and Metabolism 2017; 102(5):1495-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shefras 1995 {published data only}
- Shefras J, Farquharson RG. Heparin therapy, bone density and pregnancy. In: 27th British Congress of Obstetrics and Gynaecology; 1995 July 4-7;-Dublin, Ireland. 1995:93.
Shu 2002 {published data only}
- Shu J, Miao P, Wang RJ. Clinical observation on effect of Chinese herbal medicine plus human chorionic gonadotropin and progesterone in treating anticardiolipin antibody-positive early recurrent spontaneous abortion. Zhongguo Zhong xi yi jie he za zhi Zhongguo Zhongxiyi jiehe zazhi//Chinese Journal of Integrated Traditional and Western Medicine 2002; 22(6):414-6. [PubMed] [Google Scholar]
Silver 1993 {published data only}
- Silver RK, MacGregor SN, Sholl JS, Hobart JM, Neerhof MG, Ragin A. Comparative trial of prednisone plus aspirin vs aspirin alone in the treatment of anticardiolipin antibody-positive obstetric patients. American Journal of Obstetrics and Gynecology 1993; 169:1411-7. [DOI] [PubMed] [Google Scholar]
- Silver RK, Sholl JS, MacGregor SN, Hobart JH, Neerhof MG, Hickman AH. Prospective evaluation of single (low-dose aspirin) vs combined (aspirin plus prednisone) therapy in the treatment of the antiphospholipid syndrome. In: Proceedings of 39th Annual Meeting of the Society for Gynecologic Investigation 1992 March 18-21; San Antonio, Texas, USA. 1992:125.
Tang 2012 {published data only}
- Tang H, Huang MY, TanY. Effect of low molecular weight heparin combined with low-dose aspirin for ACA positive recurrent spontaneous abortion. Hainan Medical Journal 2012; 23:1314. [Google Scholar]
Triolo 2003 {published data only}
- Triolo G, Ferrante A, Ciccia F, Accardo-Palumbo A, Perino A, Castelli A, et al. Randomized study of subcutaneous low molecular weight heparin plus aspirin versus intravenous immunoglobulin in the treatment of recurrent fetal loss associated with antiphospholipid antibodies. Arthritis & Rheumatism 2003; 48(3):728-31. [DOI] [PubMed] [Google Scholar]
Tulppala 1997 {published data only}
- Tulppala M, Marttunen M, Soderstrom-Anttila V, Ailus K, Palosuo T, Ylikorkala O. Low dose aspirin in the prevention of miscarriage in women with unexplained or autoimmune related recurrent miscarriage: effect on prostacyclin and thromboxane A2 production. Human Reproduction 1997; 12(1):191. [DOI] [PubMed] [Google Scholar]
- Tulppala M, Marttunen M, Soderstrom-Anttila V, Foudila T, Ailus K, Palosuo T, et al. Low-dose aspirin in prevention of miscarriage in women with unexplained or autoimmune related recurrent miscarriage: effect on prostacyclin and thromboxane A2 production. Human Reproduction 1997; 12:1567-72. [DOI] [PubMed] [Google Scholar]
Vahid 1999 {published data only}
- Vahid Dastjerdi M, Moini A, Aleyasin A, Kashaf H, Marsoosi V, Aghahosscini A. The effect of acetyl salicylic acid and prednisolone before and during pregnancy in reducing unexplained recurrent abortions. Fertility & Sterility 1999; 72:S203. [Google Scholar]
van Hoorn 2016 {published data only}
- Hoorn ME, Hague WM, Pampus MG, Bezemer D, Vries JI. Low-molecular-weight heparin and aspirin in the prevention of recurrent early-onset pre-eclampsia in women with antiphospholipid antibodies: the FRUIT-RCT. European Journal of Obstetrics, Gynecology, and Reproductive Biology 2016; 197:168-73. [DOI] [PubMed] [Google Scholar]
Vaquero 2001 {published data only}
- Vaquero E, Lazzarin N, Valensise H, Menghini S, Di Pierro G, Cesa F, et al. Pregnancy outcome in recurrent spontaneous abortion associated with antiphospholipid antibodies: a comparative study of intravenous immunoglobulin versus prednisone plus low-dose aspirin. American Journal of Reproductive Immunology 2001; 45(3):174-9. [DOI] [PubMed] [Google Scholar]
Visser 2011 {published data only}
- Visser J, Ulander VM, Helmerhorst FM, Lampinen K, Morin-Papunen L, Bloemenkamp KWM, et al. Thromboprophylaxis for recurrent miscarriage in women with or without thrombophilia - HABENOX*: a randomised multicentre trial. Thrombosis and Haemostasis 2011; 105(2):295-301. [DOI] [PubMed] [Google Scholar]
Xiao 2013 {published data only}
- Xiao J, Xiong J, Zhu F, He L. Effect of prednisone, aspirin, low molecular weight heparin and intravenous immunoglobulin on outcome of pregnancy in women with antiphospholipid syndrome. Experimental and Therapeutic Medicine 2013; 5(1):287-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhou 2012 {published data only}
- Zhou X. The effect of aspirin combined with low molecular weight heparin in treatment of 30 patients with habitual abortion and antiphospholipid syndrome. China Modern Doctor 2012; 50:60-2. [Google Scholar]
References to ongoing studies
Abdelhafez 2014 {published data only}
- Abdelhafez M, NCT02303171. Use of warfarin after the first trimester in pregnant women with antiphospholipid syndrome. clinicaltrials.gov/ct2/show/record/NCT02303171 (first received 27 November 2014).
Rodger 2017 {published data only}
- Rodger M, NCT03100123. A pilot study assessing the feasibility of a randomized controlled trial evaluating aspirin versus low-molecular-weight heparin (lmwh) and aspirin in women with antiphospholipid syndrome and pregnancy loss. clinicaltrials.gov/ct2/show/NCT03100123 (first received 4 April 2017).
Additional references
ACOG 2012
- Committee on Practice Bulletins - American College of Obstetricians and Gynecologists. Practice Bulletin No. 132: Antiphospholipid syndrome. Obstetrics and Gynecology 2012; 120(6):1514-21. [DOI] [PubMed] [Google Scholar]
Askie 2007
- Askie LM, Duley L, Henderson-Smart DJ, Stewart LA, PARIS Collaborative Group. Antiplatelet agents for prevention of pre-eclampsia: a meta-analysis of individual patient data. Lancet 2007; 369(9575):1791-8. [DOI] [PubMed] [Google Scholar]
Bates 2012
- Bates SM, Greer IA, Middeldorp S, Veenstra DL, Prabulos AM, Vandvik PO. VTE, Thrombophilia, AntithromboticTherapy, and Pregnancy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012; 141:e691S–e736S. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bates 2018
- Bates SM, Rajasekhar A, Middeldorp S, McLintock C, Rodger MA, James AH, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: venous thromboembolism in the context of pregnancy. Blood Advances 2018; 2:3317-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Burton 2009
- Burton, GJ, Woods, AW, Jauniaux, E, Kingdom, JC. Rheological and physiological consequences of conversion of the maternal spiral arteries for uteroplacental blood flow during human pregnancy. Placenta 2009; 30(6):473-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Buyon 2015
- Buyon JP, Kim MY, Guerra MM, Laskin CA, Petri M, LockshinMD, et al. Predictors of pregnancy outcomes in patients with lupus: a cohort study. Annals of Internal Medicine 2015; 163:153-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Carp 2007
- Carp HJ, Christiansen OB. Epidemiology of recurrent pregnancy loss. In: Carp HJ, editors(s). Recurrent Pregnancy Loss, Causes, Controversies and Treatment. London: Informa Healthcare Ltd, 2007:1-13. [Google Scholar]
Chaung 2001
- Chuang YJ, Swanson R, Raja SM, Olson ST. Heparin enhances the specificity of antithrombin for thrombin and factor Xa independent of the reactive center loop sequence. Evidence for an exosite determinant of factor Xa specificity in heparin-activated antithrombin. Journal of Biological Chemistry 2001; 276(18):14961-71. [DOI] [PubMed] [Google Scholar]
Cines 2017
- Cines DB, Levine LD. Thrombocytopenia in pregnancy. Blood 2017; 130:2271-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohn 2010
- Cohn DM, Goddijn M, Middeldorp S, Korevaar JC, Dawood F, Farquharson RG. Recurrent miscarriage and antiphospholipid antibodies: prognosis of subsequent pregnancy. Journal of Thrombosis and Haemostasis 2010; 8(10):2208-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
De Jong 2014
- Jong PG, Kaandorp S, Di Nisio M, Goddijn M, Middeldorp S. Aspirin and/or heparin for women with unexplained recurrent miscarriage with or without inherited thrombophilia. Cochrane Database of Systematic Reviews 2014, Issue 7. [DOI: 10.1002/14651858.CD004734.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2011
- Deeks JJ, Higgins JP, Altman DG (editors) Chapter 9: Analysing data and undertaking meta‐analyses In: Higgins JP, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Derksen 2008
- Derksen RH, Groot PG. The obstetric antiphospholipid syndrome. Journal of Reproductive Immunology 2008; 77:41-50. [DOI] [PubMed] [Google Scholar]
Di Simone 2000
- Di Simone N, Meroni PL, Papa N, Raschi E, Caliandro D, De Carolis CS, et al. Antiphospholipid antibodies affect trophoblast gonadotropin secretion and invasiveness by binding directly and through adheredbeta2‑glycoprotein I. Arthritis Rheumatology 2000; 43(1):140-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Durcan 2016
- Durcan L, Petri, M. Epidemiology of the antiphospholipid syndrome. In: Cervera R, Espinosa G, Khamashta MA, editors(s). Antiphospholipid Syndrome in Systemic Autoimmune Diseases. 2nd edition. Amsterdam: Elsevier, 2016:17-30. [Google Scholar]
Erkan 2002
- Erkan D, Yazici Y, Peterson MG, Sammaritano L, Lockshin MD. A cross-sectional study of clinical thrombotic risk factors and preventive treatments in antiphospholipid syndrome. Rheumatology 2002; 41(8):924-9. [DOI] [PubMed] [Google Scholar]
Girardi 2004
- Girardi G, Redecha P, Salmon JE. Heparin prevents antiphospholipid antibody-induced fetal loss by inhibiting complement activation. Nature Medicine 2004; 10:1222-6. [DOI] [PubMed] [Google Scholar]
Green 1994
- Green D, Hirsh J, Heit J, Prins M, Davidson B, Lensing AW. Low molecular weight heparin: a critical analysis of clinical trials. Pharmacological Reviews 1994; 46(1):89-109. [PubMed] [Google Scholar]
Gómez‐Puerta 2014
- Gómez-Puerta JA, Cervera R. Diagnosis and classification of the antiphospholipid syndrome. Journal of Autoimmunity 2014; 48-49:20-5. [DOI] [PubMed] [Google Scholar]
Haas 2019
- Haas, DM, Hathaway, TJ, Ramsey, PS. Progestogen for preventing miscarriage in women with recurrent miscarriage of unclear etiology. Cochrane Database of Systematic Reviews 2019, Issue 11. [DOI: 10.1002/14651858.CD003511.pub5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Harris 1983
- Harris EN, Gharavi AE, Boey ML, Patel BM, Mackworth-Young CG, Loizou S, et al. Anticardiolipin antibodies: detection by radioimmunoassay and association with thrombosis in systemic lupuserythematosus. Lancet 1983; 322(8361):1211-4. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003; 327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2017
- Higgins JP, Altman DG, Sterne JA (editors) Chapter 8: Assessing risk of bias in included studies In: Higgins JP, Churchill R, Chandler J, Cumpston MS (editors). Cochrane Handbook for Systematic Reviews of Interventions version 5.2.0 (updated June 2017), Cochrane, 2017. Available from www.training.cochrane.org/handbook.
Ioannou 2010
- Ioannou Y, Rahman A. Domain I of beta2-glycoprotein I: its role as an epitope and the potential to be developed as a specific target for the treatment of the antiphospholipid syndrome. Lupus 2010; 19:400-5. [DOI] [PubMed] [Google Scholar]
Kozlowski 2011
- Kozlowski EO, Pavao MS, Borsig L. Ascidian dermatan sulfates attenuate metastasis, inflammation and thrombosis by inhibition of P-selectin. Journal of Thrombosis and Haemostasis 2011; 9(9):1807-15. [DOI] [PubMed] [Google Scholar]
Lockshin 2012
- Lockshin MD, Kim M, Laskin CA, Guerra M, Branch DW, Merrill J, et al. Prediction of adverse pregnancy outcome by the presence of lupus anticoagulant, but not anticardiolipin antibody, in patients with antiphospholipid antibodies. Arthritis and Rheumatism 2012; 64(7):2311-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lockshin 2013
- Lockshin MD. Anticoagulation in management of antiphospholipid antibody syndrome in pregnancy. Clinics in Laboratory Medicine 2013; 33(2):367-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Love 1990
- Love PE, Santoro SA. Antiphospholipid antibodies: anticardiolipin and the lupus anticoagulant in systemic lupus erythematosus (SLE) and in non-SLE disorders. Prevalence and clinical significance. Annals of Internal Medicine 1990; 112(9):682-98. [DOI] [PubMed] [Google Scholar]
Meroni 2012
- Meroni PL, Raschi E, Grossi C, Pregnolato F, Trespidi L, Ascaia B, et al. Obstetric and vascular APS: same autoantibodies but different diseases? Lupus 2012; 21(7):708-10. [DOI] [PubMed] [Google Scholar]
Meroni 2018
- Meroni PL, Borghi MO, Grossi C, Chighizola CB, Durigutto P, Tedesco F. Obstetric and vascular antiphospholipid syndrome: same antibodies but different diseases? Nature Reviews Rheumatology 2018; 14(7):433-40. [DOI] [PubMed] [Google Scholar]
Miyakis 2006
- Miyakis S, Lockshin MD, Atsumi T, Branch DW, Brey RL, Cervera R, et al. International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome (APS). Journal of Thrombosis and Haemostasis 2006; 4(2):295-306. [DOI] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, and the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. PLOS Medicine 2009; 6(7):e1000097. [DOI: 10.1371/journal.pmed1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nurmohamed 1992
- Nurmohamed MT, Rosendaal FR, Buller HR, Dekker E, Hommes DW, Vandenbroucke JP, et al. Low-molecular-weight heparin versus standard heparin in general and orthopaedic surgery: a meta-analysis. Lancet 1992; 340(8812):152-6. [DOI] [PubMed] [Google Scholar]
Oberkersch 2010
- Oberkersch R, Attorresi AI, Calabrese GC. Low-molecular-weight heparin inhibition in classical complement activation pathway during pregnancy. Thrombosis Research 2010; 125:e240-5. [DOI] [PubMed] [Google Scholar]
Opatrny 2006
- Opatrny L, David M, Kahn SR, Shrier I, Rey E. Association between antiphospholipid antibodies and recurrent fetal loss in women without autoimmune disease: a metaanalysis. Journal of Rheumatology Nov 2006;33(11):2214-21. [PubMed] [Google Scholar]
Pariente 2016
- Pariente G, Leibson T, Carls A, Adams-Webber T, Ito S, Koren G. Pregnancy-associated changes in pharmacokinetics: a systematic review. PLOS Medicine 2016; 13(11):e1002160. [DOI] [PMC free article] [PubMed] [Google Scholar]
Quao 2018
- Quao Z, Tong M, Bryce E, Guller S, Chamley L, Abrahams V. Low molecular weight heparin and aspirin exacerbate human endometrial endothelial cell responses to antiphospholipid antibodies. American Journal of Reproductive Immunology 2018; 79(1):e12785. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rai 1995
- Rai RS, Regan L, Clifford K, Pickering W, Dave M, Mackie I, et al. Antiphospholipid antibodies and beta 2-glycoprotein-I in 500 women with recurrent miscarriage: results of a comprehensive screening approach. Human Reproduction 1995; 8(10):2001-5. [DOI] [PubMed] [Google Scholar]
Redecha 2008
- Redecha P, Franzke C, Ruf W, Mackman N, Girardi G. Neutrophil activation by the tissue factor/Factor VIIa/PAR2 axis mediates fetal death in a mouse model of antiphospholipid syndrome. Journal of Clinical Investigation 2008; 118(10):3453-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- Nordic Cochrane Centre, The Cochrane Collaboration Review Manager 5 (RevMan 5). Version 5.3. Copenhagen: Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Rodger 2014
- Rodger MA, Carrier M, Le Gal G, Martinelli I, Perna A, Rey E, et al. Meta-analysis of low-molecular-weight heparin to prevent recurrent placenta-mediated pregnancy complications. Blood 2014; 123:822-8. [DOI] [PubMed] [Google Scholar]
Rolnik 2017
- Rolnik DL, Wright D, Poon LC, O'Gorman N, Syngelaki A, Paco Matallana C, et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. New England Journal of Medicine 2017; 377(7):613-22. [DOI] [PubMed] [Google Scholar]
Ruiz‐Irastorza 2010
- Ruiz-Irastorza G, Crowther M, Branch W, Khamashta MA. Antiphospholipid syndrome. Lancet 2010; 376(9751):1498-509. [DOI] [PubMed] [Google Scholar]
Samarkos 2012
- Samarkos M, Mylona E, Kapsimali V. The role of complement in the antiphospholipid syndrome: a novel mechanism for pregnancy morbidity. Seminars in Arthritis and Rheumatism 2012; 42(1):66-9. [DOI] [PubMed] [Google Scholar]
Scheres 2019
- Scheres LJJ, Bistervels IM, Middeldorp S. Everything the clinician needs to know about evidence-based anticoagulation in pregnancy. Blood Reviews 2019; 33:82-97. [DOI] [PubMed] [Google Scholar]
Schreiber 2018
- Schreiber K, Sciascia S, Groot PG, Devreese K, Jacobsen S, Ruiz-Irastorza G, et al. Antiphospholipid syndrome. Nature Reviews Disease Primers 2018; 4:18005. [DOI] [PubMed] [Google Scholar]
Shomer 2016
- Shomer E, Katzenell S, Zipori Y, Rebibo-Sabbah A, Brenner B, Aharon A. Microvesicles of pregnant women receiving low molecular weight heparin improve trophoblast function. Thrombosis Research 2016; 137:141-7. [DOI] [PubMed] [Google Scholar]
Skeith 2016
- Skeith L, Carrier M, Kaaja R, Martinelli I, Petroff D, Schleussner E, et al. A meta-analysis of low-molecular-weight heparin to prevent pregnancy loss in women with inherited thrombophilia. Blood 2016; 127(13):1650-5. [DOI] [PubMed] [Google Scholar]
Skeith 2018
- Skeith L. Anticoagulating patients with high-risk acquired thrombophilias. Blood 2018; 132(21):2219-29. [DOI] [PubMed] [Google Scholar]
Vane 1971
- Vane JR. Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nature: New Biology 1971; 231(25):232-5. [DOI] [PubMed] [Google Scholar]
Vane 2003
- Vane JR, Botting RM. The mechanism of action of aspirin. Thrombosis Research 2003; 110(5-6):255-8. [DOI] [PubMed] [Google Scholar]
Vermeulen 2018
- The ESHRE Guideline Group on RPL , Bender Atik R, Christiansen OB, Elson J, Kolte AM, Lewis S, Middeldorp S, et al. ESHRE guideline: recurrent pregnancy loss. Human Reproduction Open 2018; 2018(2):hoy004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Vignoli 2006
- Vignoli A, Marchetti M, Balducci D, Barbui T, Falanga A. Differential effect of the low-molecular-weight heparin, dalteparin, and unfractionated heparin on microvascular endothelial cell hemostatic properties. Haematologica 2006; 91(2):207-14. [PubMed] [Google Scholar]
Wat 2018
- Wat JM, Audette MC, Kingdom JC. Molecular actions of heparin and their implications in preventing pre‐eclampsia. Journal of Thrombosis and Haemostasis 2018; 16:1510-22. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Empson 2005
- Empson MB, Lassere M, Craig JC, Scott JR. Prevention of recurrent miscarriage for women with antiphospholipid antibody or lupus anticoagulant. Cochrane Database of Systematic Reviews 2005, Issue 2. [DOI: 10.1002/14651858.CD002859.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Scheres 2017
- Scheres LJJ, Marijnen MC, Middeldorp S. Aspirin or heparin or both for improving pregnancy outcomes in women with persistent antiphospholipid antibodies and recurrent pregnancy loss. Cochrane Database of Systematic Reviews 2017, Issue 11. [DOI: 10.1002/14651858.CD012852] [DOI] [PMC free article] [PubMed] [Google Scholar]


