Abstract
The COVID-19 global pandemic presents a challenge to orthopaedic education. Around the world, including in the United States, elective surgeries are being deferred and orthopaedic residents and fellows are being asked to make drastic changes to their daily routines. In the midst of these changes are unique opportunities for resident/fellow growth and development. Educational tools in the form of web-based learning, surgical simulators, and basic competency tests may serve an important role. Challenges are inevitable, but appropriate preparation may help programs ensure continued resident growth, development, and well-being while maintaining high-quality patient care.
COVID-19 is a growing pandemic, with projections for a surge in inpatient demand that may exceed both general ward and intensive care unit (ICU) capacity by 10-fold.1 In response, hospitals have adopted drastic changes to care structures, including upgrading general wards to having ICU capabilities, deferring and canceling elective surgeries, and redefining the roles of healthcare providers. Orthopaedic surgeons, including residents and fellows in-training, have not been immune to these changes. As many hospitals have canceled elective surgeries, orthopaedic case volume has dwindled drastically.2 There has also been a growing emphasis on maintaining the health of care providers on the front line, including the resident and fellow workforce. Owing to these factors, orthopaedic surgery departments have established a list of priorities to guide administrative and organizational actions during this time (Table 1). Although the pandemic presents a number of challenges, preparation and planning will contribute to continued learning and unique opportunities for resident/fellow growth and development.
Table 1.
Orthopaedic Surgery Residency Program Priorities During the COVID-19 Pandemic
| Maintaining resident health and well-being |
| Providing high-quality patient care for urgent orthopaedic issues |
| Aiding in overflow care of emergency department, medical wards, and/or ICUs |
| Continuing orthopaedic education for residents |
| Encouraging individual research/professional opportunities |
ICU = intensive care unit
Changes to Clinical Service Structure
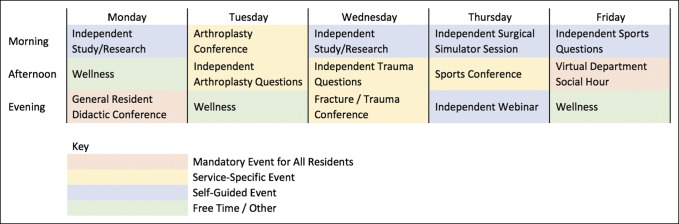
Many departments have adopted a residency surge plan.3 Under such a strategy, a portion of the residents are assigned to hospital duties (ie, direct patient care, rounding on inpatients, and covering urgent surgeries), whereas the remainder are quarantined to their home environment (Figure 1). Doing so ensures that urgent orthopaedic care can continue to be provided. Although research has widely reported that COVID-19 causes only mild symptoms in individuals in their twenties and thirties with few medical comorbidities (most resident/fellow physicians),4 a situation in which an entire residency program falls ill with the highly virulent COVID-19 would be potentially catastrophic. In addition, if a large group of residents contract the virus with little to no symptoms, they may unintentionally expose a large number of vulnerable patients or other healthcare workers to the pathogen. The surge plan and its early adoption help mitigate these possibilities.
Figure 1.
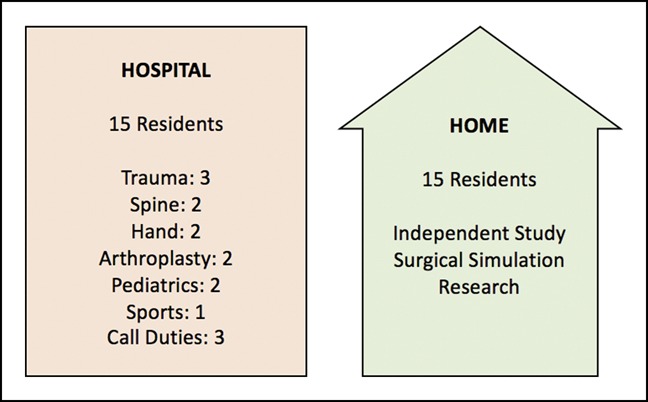
Illustration showing theresidency surge plan. Schematic diagram of a residency surge plan for an orthopaedic program with 30 residents. After a 2-week period, the Hospital team switches with the Home team, helping to ensure that at least half of the residents are healthy at any one time.
It is anticipated that inpatient demand for COVID-19 will overwhelm the hospital capacity through the summer and possibly the fall of 2020.1 Orthopaedic surgery residents are already being redeployed to ICUs and emergency departments, where coverage is stretched and thin. The Accreditation Council for Graduate Medical Education (ACGME) and the American Board or Orthopaedic Surgery (ABOS) currently mandate that first year orthopaedic surgery residents receive 6 months of nonorthopaedic education, including 3 months of general surgery and 3 months of structured training chosen from specialties such as anesthesia, emergency medicine, intensive care, or anesthesia/airway management.5 The goal of these rotations is to “foster proficiency in the basic surgical skills, the perioperative care of surgical patients, medical management of patients, and airway management skills.” Although many residents/fellows are several years removed from these rotations, the foundations for success are still present. Moreover, reassignment to a medical, anesthesia, or intensivist service may serve a good reminder that although we identify as orthopaedic surgeons, we are first and foremost medical doctors.
Virtual Learning
Time spent away from the hospital, or with nonorthopaedic care teams, will remove residents from the daily orthopaedic duties that are associated with near-constant learning. In response, residency and fellowship programs must consider unique and novel avenues of learning. Weekly meetings and conferences that previously took place in person can be carried out using virtual meeting spaces. In response to the European working time regulations, which were changes analogous to the ACGME duty hour restrictions, Palan et al6 reported their experience in establishing and conducting virtual learning platforms and virtual journal clubs to help optimize resident time spent away from the hospital. The team found a number of unique strengths relative to a traditional in-person learning format, including the ability to revisit the digitally recorded session for clarification or continued learning, ease of access to both clinical material (ie, radiographs and advance imaging) and key articles, and the ability to connect individuals of different geographic regions. Similar practices must be adopted, given the current circumstances.
Today, applications such as WebEx,7 Google Classroom,8 Microsoft Teams,9 and Zoom10 offer platforms for team-based collaboration that our department has used. Each application has unique features, and most are free for basic use (Table 2). During standard learning not influenced by a pandemic, our department hosts an average of 2 hours of didactic conference-based learning per day. This is spread out among the subspecialties (ie, adult reconstruction, hand, and sport) such that only residents assigned to that particular service are expected to attend. Given the decrease in clinical duties and the ease of use of the virtual meeting spaces, these conferences have since been opened up to all residents hoping to attend. Interestingly, attendance at these virtual conferences is now higher than normal, with generally positive reviews from faculty and attendees alike. A sample weekly schedule from our department with options for team-based and independent learning is shown in Figure 2.
Table 2.
Online Video Conferencing Applications
| Name | Description | Live Feed | Real time Collaboration | Compatibility | Cost | Maximum No. of Participants | Screen Sharing | Limitations of Free Version |
| Cisco Webex | Video conferencing platform for online meetings, screen sharing, and webinars | Yes | Yes | iOS, Android, Web Browser | Free; personal meetings; $13.50; small meetings; $26.95; large and business meetings | 3,000 depending on plan | Yes | Limit of 100 participants per meeting |
| Google Classroom | Learning management system to help organize and coordinate resident assignments, attendance, and progress | No | No | iOS, Android, Chromebook, Web Browser | Free | 250 for personal account; 1,000 with institu-tional account | Yes, via Chrome exten-sion | NA |
| Microsoft teams | Centralized virtual platform for online meeting and collaboration through Microsoft applications (Word, Excel, and PowerPoint) | Yes | Yes | iOS, Android, Microsoft Surface, Web Browser | Free; with institutional e-mail; $5.00 per user per month for Office 365 | 10,000 | Yes | Does not include Microsoft Office applications for download |
| Zoom | Video-communication tool with the ability to share the screen with audience, hold only meetings, and collaborate remotely | Yes | Yes | iOS, Android, Web Browser | Free; personal meetings; $14.99; small meetings; $19.99; enterprises with minimum of 50 hosts | 1,000 | Yes | Limit of 100 participants, and 40 min per meeting |
Figure 2.
Illustration showing the sample resident weekly schedule. This sample schedule consists of a few key mandatory weekly meetings for all residents and the program director. A number of service-specific events are mandatory for residents assigned to that service but are made available to all residents wishing to attend. The remainder of time is filled with independent study, research, or webinars made available through the American Academy of Orthopaedic Surgeons or the subspecialty societies. An assigned time with a surgical simulator in the resident workspace is an option for programs that can safely provide this method of learning. All meetings take place via a virtual platform.
Independent Study
Similar to team-based learning, the value of active independent study during this tumultuous period cannot be overstated. Conveniently, diminished case volume and clinical demands may offer newfound time for this focus. We know these independent study efforts are meaningful, with previous research showing that residents with routine traditional home study habits record higher Orthopaedic In-Training Examination scores compared with those who do not.11 To this end, a number of orthopaedic professional societies have published high-quality educational materials, including didactic text or questions, aimed at resident learning (Table 3). For those resources with question banks, tests can be created that are specific to certain subspecialties (ie, adult reconstruction, hand, and sport). On competition of these tests, the scores can be sent to either the program director or subspecialty attending physicians to indicate the level of proficiency. Furthermore, the ABOS requires a specific amount of time spent on each service to graduate.12 These online testing sites allow the program leadership to document work that is being done while a resident is on service to show that the resident/fellow is working toward proficiency.
Table 3.
Online Educational Resources for Resident Learning
| Name | Publisher | Type | Cost | Ability to Track Participation and Progress | Web Address |
| Clinical Classroom | Journal of Bone and Joint Surgery (JBJS) | Text, questions | Annual subscription | Menu shows which progress for each lesson that contain interactive question formats | https://knowledgeplus.nejm.org/partner-programs/jbjs-clinical-classroom/ |
| Course OnDemand | AAOS | Text, questions | Variable | The AAOS Dashboard displays progress for each course and which courses have been completed | https://learn.aaos.org/diweb/dashboard |
| OrthoBullets | OrthoBullets | Text, questions | Free | Users create tests that are scored and recorded in a database on completion | https://www.orthobullets.com/ |
| ResStudy | AAOS | Questions | Annual subscription | Large question sets for each subspecialty; displays how many questions were completed and which questions were correct | https://learn.aaos.org/diweb/dashboard |
| Webinars in adult reconstruction | AAHKS | Text, video | Free | Page demonstrating completion at the conclusion of webinar can be saved and forwarded | http://www.aahks.org/webinars/ |
| Webinars OnDemand | AAOS | Text, video | Variable | The AAOS Dashboard displays progress for each webina, and which webinars have been completed | https://learn.aaos.org/diweb/dashboard |
AAHKS = the American Association of Hip and Knee Surgeons, AAOS = the American Academy of Orthopaedic Surgeons
A number of nontraditional education modalities, which have been changed or made available specifically in response to COVID-19, should also be explored. The 2020 Annual Meeting of American Academy of Orthopaedic Surgeons (AAOS) is now being made available through the AAOS website. This includes Instructional Course Lectures, and Ask an Expert! sessions, in addition to the traditional research studies and poster presentations. Similarly, the annual spring AAOS orthopaedic board preparation and review course will take place via a virtual platform. Opportunities specifically aimed at a fellowship level of education have also been made available. The American Association of Hip and Knee Surgeons, for example, has developed the FOCAL Initiative: Fellows Online COVID-19 AAHKS Learning, a series of online lectures by invited faculty to continue fellow education during this time.13 Similar platforms are under development with the other leading subspecialty societies.
Surgical Simulation
Before COVID-19, there had already been a push to improve orthopaedic surgical skills training outside of the operating room because of restricted hours, cost pressures, patient safety concerns, and a growing number of minimally invasive and technically challenging procedures.14 Diminished case volume, quarantine away from patient care, and active social distancing will only accelerate this movement in the coming months. Surgical simulation is a powerful tool that can help meet this training demand. As Great Britain's former Chief Medical Officer Sir Liam Donaldson once said, “If I had to have my gallbladder out, I would rather it was done by someone who had already done 100 in a simulator.”15 Various simulation modalities studied in orthopaedic surgery have included surgical skill laboratories,16 cadaveric dissection and procedural training,17 computer-based virtual reality training,18 and arthroscopic surgery simulation.19 Despite their promise of improved surgical education, high “observational” surgical volume, and time spent on direct patient care have been major barriers to widespread adoption. Hospital and residency changes surrounding COVID-19 may make more time available for these endeavors; however, the principles of cleanliness and social distancing must still be respected with use of these tools.
Performance Metrics
One challenge with a reliance on nonconventional learning is ensuring continued maintenance or improvement in both technical and nontechnical skill levels during this period. Self-reported resident questionnaires are an easy option but are typically not considered as valid proficiency measures because of massive internal bias.20 The Objective Structured Assessment of Technical Skills (OSATS), Global Rating Scales, and ABOS Surgical Skills Assessment Program are objective measures completed by independent observers who evaluate a trainee's preparedness and performance using a list of specific knowledge-based and performance-based checkpoints for a particular procedure (Table 4). These assessments have been publicized and validated across a number of subspecialties, including hand and wrist surgery,21 shoulder surgery,22 and arthroscopic knee surgery.23 The tools provide objective scores that are simple to record and track over time. In the setting of COVID-19, potential methods of use include recording a baseline OSATS or Global Rating Scales score of particular interest at the time of initial home duty (eg, the carpal tunnel OSATS24 for a resident assigned to the hand service) and ensuring that this score can be matched on the resident's return to the workforce. Doing so will not only encourage active resident learning during the time away but may also contribute to higher quality of patient care.
Table 4.
Objective Performance Metrics for Resident/Fellow Education
| Name | Used in Resident Education Since: | Intended Use | Strengths | Limitations |
| Traditional ACGME case log | 1981 | Allow residents and program directors to ensure a breadth of procedural exposure, in addition to meeting minimum requirements | Widely-published guidelines from the ABOS and ACGME, considerable historical data, early introduction to procedural codes | No measure of technical ability, not indicative of the degree of resident involvement, limitations in reflecting resident learning during COVID-19 |
| OSATS | 1990 | Provides objective scoring system unique to specific orthopaedic procedure that judges technical skill and ability | Historically good indicator of technical ability and has been expanded for some procedures to reflect nontechnical skills, including indications and perioperative management | Depending on the procedure, assessment of technical skill may be at an introductory level |
| GRS | 1996 | Scoring system of technical skills based on universal principles of good surgical technique, including respect for tissue, instrument handling, understanding of procedure, and overall timing/efficiency | Suggested to be more refined indicator of technical skill relative to OSATS | No true measure of awareness of surgical indications, counseling, or patient management outside of surgery |
| ABOS surgical skills assessment program | 2016 | Offer standardized method for resident education and tracking resident technical ability with specific procedures | Offers instructional videos and easy-to-use performance assessments for reviewers; wide range from introductory to complex procedures | Focus on technical skill rather than knowledge base |
ABOS = the American Board or Orthopaedic Surgery, ACGME = the Accreditation Council for Graduate Medical Education, GRS = Global Rating Scales, OSATS = Objective Structured Assessment of Technical Skills
Research and Professional Opportunities
A diminished case volume and, for many, time away from the hospital environment may allow residents to delve into research and other professional opportunities. At the heart of these is the role of mentorship and guidance from faculty and role models.25 Because the emphasis on value-based care, maximizing reimbursement, and productivity metrics has rapidly grown over the past several years, the designated time for mentorship and professional development has been unintentionally compromised.26 Schedule changes and increased availability in the setting of COVID-19 may offer newfound time for residents to connect with mentors over fellowship applications, career paths, and research projects. At our programs, for instance, each resident sends their mutually-selected mentor(s) a weekly list of projects they have been working on and the progress made over the past week. They are encouraged to attend research team meetings that have also successfully transitioned to the virtual setting. Fourth-year residents also regularly communicate with their mentors regarding fellowship options and for guidance regarding their respective rank lists. These communications are overseen by the program director, who ensures that all residents are participating to a satisfactory level.
Guidelines Specific to Program Leadership
It remains to be seen how exactly the COVID-19 pandemic will affect the surgical training of our orthopaedic residents and fellows. Successful leadership during this time carries a number of challenges.27 The ACGME has provided guidance regarding how to handle this situation through a three-stage system28 (Table 5). At this time, most programs, including ours, are functioning in stage 2 capacity. A portion of residents have shifted to nonorthopaedic care duties, whereas others remain dedicated to the timely care of urgent orthopaedic issues. However, a growing number of programs are moving toward stage 3 capacity. At stage 3, four principles should guide all resident/fellow actions, whereas requirements specific to specialty (ie, orthopaedic surgery) are temporarily lifted (unique from stage 2). These principles include adequate resources and training, appropriate supervision for the level of care being provided, adherence to work hour requirements, and allowance of fellows to function as attending medical staff within their core specialty. In some jurisdictions hit hardest by COVID-19, including New York, the state government has temporarily lifted work hour restrictions.29 Developing plans now is critical to prevent resident burnout and to meet the growing demand for COVID-19 care providers.
Table 5.
Three Stages of Graduate Medical Education During the COVID-19 Pandemic (Table Adapted From ACGME.org)
| Title | Stage 1 | Stage 2 | Stage 3 |
| Business as Usual | Increased Clinical Demands Guidance | Pandemic Emergency Status Guidance | |
| Definition | No notable disruption of patient care and educational activities; planning underway for increased clinical demands | Some residents/fellows must shift to patient care duties; some educational activities are suspended | Most or all residents/fellows must shift to patient care; most educational activities are suspended |
| Tthe ACGME common program requirements | Active | Active | Active |
| The ACGME specialty-specific program requirements | Active | Active | Waived |
| Guiding principles | No change from the standard guidelines | Increased emphasis on four key principles: | All resident and fellow activity is guided by four key principles: |
| Adequate resources and training | Adequate resources and training | ||
| Adequate supervision | Adequate supervision | ||
| Work hour requirement | Work hour requirement | ||
| Fellows functioning in core specialty as attending providers | Fellows functioning in core specialty as attending providers |
ACGME = the Accreditation Council for Graduate Medical Education
In addition, as previously mentioned, program leadership should maintain an account of team-based and independent resident learning during this time away from traditional clinical rotations. This includes taking attendance of general and subspecialty conferences, having residents/fellows submit proof of completed questions on a particular subspecialty, and recording progress in research efforts. In doing so, this too may help satisfy the ABOS guidelines regarding resident time spent on subspecialty services, helping to avoid delays in resident advancement and graduation for years to come.12
Finally, forced reorganization may enable administrators to take a step back and examine their program, identify the areas of potential improvement, and propose beneficial changes once COVID-19 has resolved. One must not forget that many of the powerful changes in resident education were born out of periods of change and uncertainty. For example, the ACGME was founded in 1981 in response to a concerning degree of variability in the quality of resident education.30 Duty hour limits were redefined in 2011 because of major concerns of resident fatigue and safety issues.31 The accreditation system was overhauled in 2013 in response to claims that resident ability to innovate and express themselves had disappeared.32 During the COVID-19 pandemic and this unique time of redefined roles, breaks from traditional resident rotations and a re-emphasis on medicine, program directors, and the orthopaedic leadership share another opportunity to consider and execute changes to stimulate resident education for the coming decade.
Opportunities for Resident Growth and Development
As disruptive as these changes may first seem, they present unique opportunities for resident growth and resilience. Resident education has historically focused on the development of “cognitive” skills, such as anatomic knowledge, surgical skill, and clinical intuition. There has been a recent shift, however, in the development and stimulation of “noncognitive” skills.33 These qualities have been emphasized as predictors of future personal and professional success, and notably include resilience self-control, and conscientiousness. Attainment and optimization of these ideals have been associated with improved surgical resident well-being,34 lower resident attrition rates,35 decreased likelihood of burnout as an attending surgeon,36 and higher overall rates of career satisfaction.37 Uncertainty in the work environment because of COVID-19, including novel individual responsibilities with new care teams, variable orthopaedic case mix and volume, and changes in schedule format will undoubtedly stimulate growth and resilience, in addition to refinement of these critical attributes. Finally, many residents will be asked to take on leadership roles to coordinate and plan day-to-day activities given their valuable perspective on the front lines. A key aspect of this is facilitating efficient communication between residents and the program leadership, with the goal of avoiding e-mail overload and missed information.
Resident and Fellow Well-Being
During this time of stress and uncertainty, ensuring resident and fellow well-being is of the utmost importance. It is unclear how long this pandemic will last, how overwhelmed our hospital systems will be, and to what extent residents and fellows will be asked to participate in the care of nonorthopaedic patients. Residents and fellows share common concerns including the location and type of care being provided, whether there is enough personal protective equipment, and whether they have received appropriate training to adequately perform clinical duties for those patients. In addition, for young physicians on the front line it is unknown how their potential exposure to COVID-19 places them and their families at risk. For many residents and fellows with young families at home, the thought of bringing COVID-19 to their home and infecting their loved ones is overwhelming and some programs have even offered alternative housing.38 Involving these young physicians in the decision-making process and being receptive to feedback through weekly departmental virtual gatherings or “town hall meetings” can help to ensure that they are being heard and are taking an active role in these unique assignments.
Residents and fellows also share concerns outside the scope of immediate clinical care. These include uncertainty surrounding graduation requirements, board certification, and job prospects. Regarding resident graduation and concerns surrounding the achievement of minimum case numbers, it should be noted that according to the ACGME, the minimums are not meant to be a direct measure of resident competence. The ACGME and ABOS further explain that it is up to the program director and the program's Clinical Competency Committee to assess the proficiency of an individual resident as to whether that person is prepared to enter the unsupervised practice of medicine. Time requirements on specific services, however, do remain in place. Although the ABOS has relaxed some requirements for minimum time-dependent residency experience, this remains a subject of discussion with further guidance expected from the ABOS. It also remains to be seen how this pandemic will affect young physicians preparing for board examination and exploring job prospects. As of March 2020, the ABOS had notified senior residents that they are still planning to administer the part 1 examination in July 2020, as previously planned. To help address and navigate these changes, we have started a weekly conference series led by attending physicians that focuses on the logistics of board certification, job prospects, and financial planning during these unique and stressful times.
A number of additional resources have been made available by our institutions to ensure resident and fellow wellness. These include free boxed breakfasts and lunches for all residents in the hospital, regularly-scheduled virtual question & answer sessions between house staff and hospital leadership, and the availability of alternative housing when necessary to avoid spreading COVID-19 to the home environment. All hospital staff, including residents and fellows, also have the ability to speak to a wellness counselor or therapist as personal questions or concerns arise. This service is available at all hours of the day both anonymously and via face-to-face virtual meetings. To help inform residents while limiting e-mail overload, a single concise message is sent on a weekly basis to house staff with information regarding wellness resources and events for the coming week.
Finally, during this time of social distancing and diminished time of face-to-face interaction, our departments have hosted routine virtual social hours during which residents and faculty gather to discuss lighter topics and life outside of residency. These have been well-attended and are a positive source of resident, fellow, and faculty camaraderie. The importance of this ability to connect with peers and support systems cannot be overstated during a period of isolation. All efforts to overcome interpersonal isolation, from sharing jokes to conference calls, serve an important role in times of intense strain and stress.39 As demands on residents and fellows increase, this focus on stimulating and maintaining resident and fellow wellness must remain a central focus.
Summary
The COVID-19 pandemic presents an unprecedented challenge for orthopaedic education. Orthopaedic departments must develop a list of priorities based on their institutional needs to guide decision-making during these times of uncertainty. Between residency surge plans and cross-coverage of medical units, resident roles will undoubtedly be redefined. However, amidst the uncertainty, there are unique opportunities for resident growth and development. Potential tools include the use of virtual meeting platforms, independent home study, surgical simulation, and fostering leadership opportunities. It is of the utmost importance that in order for these plans to work, the residents must feel safe, protected, and heard. Embracing these changes will enable residency programs to rise to the challenges of COVID-19 and ensure the provision of high-quality patient care for years to come.
Acknowledgments
The authors would like to acknowledge Dr. Andrew Zhang and Dr. Patrick Massey for their contributions to Table 2 of the present manuscript.
Footnotes
None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Kogan, Dr. Klein, Dr. Hannon, and Dr. Nolte.
References
- References printed in bold type are those published within the past 5 years.
- 1.Ferguson NM, Laydon D, Nedjati-Gilani G, et al. : Impact of Non-pharmaceutical Interventions (NPIs) to Reduce COVID-19 Mortality and Healthcare Demand. London, Imperial College COVID-19 Response Team, 2020, pp 16. [Google Scholar]
- 2.Kelly JD, IV: CMS urges delay of non-essential medical, surgical procedures during COVID-19 pandemic. 2020. [Google Scholar]
- 3.Boden SD: How to deploy residents during COVID-19. Available at: https://ryortho.com/breaking/how-to-deploy-residents-during-covid-19/. 2020, vol 2020.
- 4.Liao J, Fan S, Chen J, et al. : Epidemiological and clinical characteristics of COVID-19 in adolescents and young adults. medRxiv 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dougherty PJ, Marcus RE: ACGME and ABOS changes for the orthopaedic surgery PGY-1 (intern) year. Clin Orthop Relat Res 2013;471:3412-3416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Palan J, Roberts V, Bloch B, Kulkarni A, Bhowal B, Dias J: The use of a virtual learning environment in promoting virtual journal clubs and case-based discussions in trauma and orthopaedic postgraduate medical education: The leicester experience. J Bone Joint Surg Br 2012;94:1170-1175. [DOI] [PubMed] [Google Scholar]
- 7.Cisco webex. Available at: https://www.webex.com/. 2020, vol 2020.
- 8.Google classroom. Available at: https://classroom.google.com/u/0/h. 2020, vol 2020.
- 9.Microsoft teams. Available at: https://products.office.com/en-us/microsoft-teams/group-chat-software?&ef_id=EAIaIQobChMI88DCmYzF6AIVBf_jBx2TSA4ZEAAYASAAEgLSKPD_BwE:G:s&OCID=AID2000955_SEM_EAIaIQobChMI88DCmYzF6AIVBf_jBx2TSA4ZEAAYASAAEgLSKPD_BwE:G:s&gclid=EAIaIQobChMI88DCmYzF6AIVBf_jBx2TSA4ZEAAYASAAEgLSKPD_BwE. 2020, vol 2020.
- 10.Zoom. Available at: https://zoom.us/. 2020, vol 2020.
- 11.Miyamoto RG, Jr, Klein GR, Walsh M, Zuckerman JD: Orthopedic surgery residents' study habits and performance on the Orthopedic In-Training Examination. Am J Orthop 2007;36:E185-E188. [PubMed] [Google Scholar]
- 12.American Board of Orthopaedic Surgery: Rules and procedures for residency education. Available at: https://www.abos.org/wp-content/uploads/2020/01/Part-I-and-II-RP-2019_10_17.pdf. 2020, vol 2020.
- 13.American Association of Hip and Knee Surgeons: COVID-19 resources. Available at: http://www.aahks.org/. vol 2020.
- 14.Pedowitz RA, Marsh LJ: Motor skills training in orthopaedic surgery: A paradigm shift toward a simulation-based educational curriculum. J Am Acad Orthop Surg 2012;20:407-409. [DOI] [PubMed] [Google Scholar]
- 15.Laurance J: Surgeons should train on simulators like pilots. The Independent. London, UK, Independent News and Media, Ltd, 2009. [Google Scholar]
- 16.Sonnadara RR, Van Vliet A, Safir O, et al. : Orthopedic boot camp: Examining the effectiveness of an intensive surgical skills course. Surgery 2011;149:745-749. [DOI] [PubMed] [Google Scholar]
- 17.Holland JP, Waugh L, Horgan A, Paleri V, Deehan DJ: Cadaveric hands-on training for surgical specialties: Is this back to the future for surgical skills development? J Surg Educ 2011;68:110-116. [DOI] [PubMed] [Google Scholar]
- 18.Blyth P, Stott NS, Anderson IA: A simulation-based training system for hip fracture fixation for use within the hospital environment. Injury 2007;38:1197-1203. [DOI] [PubMed] [Google Scholar]
- 19.Gomoll AH, O'toole RV, Czarnecki J, Warner JJ: Surgical experience correlates with performance on a virtual reality simulator for shoulder arthroscopy. Am J Sports Med 2007;35:883-888. [DOI] [PubMed] [Google Scholar]
- 20.Atesok K, Satava RM, Van Heest A, et al. : Retention of skills after simulation-based training in orthopaedic surgery. J Am Acad Orthop Surg 2016;24:505-514. [DOI] [PubMed] [Google Scholar]
- 21.VanHeest A, Kuzel B, Agel J, Putnam M, Kalliainen L, Fletcher J: Objective Structured Assessment of Technical Skill in upper extremity surgery. J Hand Surg 2012;37:332-337.e4. [DOI] [PubMed] [Google Scholar]
- 22.Bernard JA, Dattilo JR, Srikumaran U, Zikria BA, Jain A, LaPorte DM: Reliability and validity of 3 methods of assessing orthopedic resident skill in shoulder surgery. J Surg Educ 2016;73:1020-1025. [DOI] [PubMed] [Google Scholar]
- 23.Alvand A, Logishetty K, Middleton R, et al. : Validating a Global Rating Scale to monitor individual resident learning curves during arthroscopic knee meniscal repair. Arthroscopy 2013;29:906-912. [DOI] [PubMed] [Google Scholar]
- 24.Shanedling J, Van Heest A, Rodriguez M, Putnam M, Agel J: Validation of an online assessment of orthopedic surgery residents' cognitive skills and preparedness for carpal tunnel release surgery. J Grad Med Educ 2010;2:435-441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mulcahey MK, Waterman BR, Hart R, Daniels AH: The role of mentoring in the development of successful orthopaedic surgeons. J Am Acad Orthop Surg 2018;26:463-471. [DOI] [PubMed] [Google Scholar]
- 26.Sambunjak D, Straus SE, Marusic A: A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. J Gen Intern Med 2010;25:72-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.LaPorte DM, Tornetta P, Marsh JL: Challenges to orthopaedic resident education. J Am Acad Orthop Surg 2019;27:419-425. [DOI] [PubMed] [Google Scholar]
- 28.Accreditation Council for Graduate Medical Education: Three stages of GME during the COVID-19 pandemic. Available at: https://www.acgme.org/COVID-19/Three-Stages-of-GME-During-the-COVID-19-Pandemic. 2020, vol 2020.
- 29.Cuomo AM: No. 202.10: Continuing temporary suspension and modification of laws relating to the disaster emergency. 2020. [Google Scholar]
- 30.Benson JA: Enhancing standards of excellence in internal-medicine training. Ann Intern Med 1987;107:775-778. [DOI] [PubMed] [Google Scholar]
- 31.Philibert I, Friedmann P, Williams WT: New requirements for resident duty hours. JAMA 2002;288:1112-1114. [DOI] [PubMed] [Google Scholar]
- 32.Nasca TJ, Philibert I, Brigham T, Flynn TC: The next GME accreditation system—Rationale and benefits. N Engl J Med 2012;366:1051-1056. [DOI] [PubMed] [Google Scholar]
- 33.Camp CL, Wang D, Turner NS, Grawe BM, Kogan M, Kelly AM: Objective predictors of grit, self-control, and conscientiousness in orthopaedic surgery residency applicants. J Am Acad Orthop Surg 2019;27:e227-e234. [DOI] [PubMed] [Google Scholar]
- 34.Salles A, Cohen GL, Mueller CM: The relationship between grit and resident well-being. Am J Surg 2014;207:251-254. [DOI] [PubMed] [Google Scholar]
- 35.Salles A, Lin D, Liebert C, et al. : Grit as a predictor of risk of attrition in surgical residency. Am J Surg 2017;213:288-291. [DOI] [PubMed] [Google Scholar]
- 36.Walker A, Hines J, Brecknell J: Survival of the grittiest? Consultant surgeons are significantly grittier than their junior trainees. J Surg Educ 2016;73:730-734. [DOI] [PubMed] [Google Scholar]
- 37.Tangney JP, Boone AL, Baumeister RF: High self-control predicts good adjustment, less pathology, better grades, and interpersonal success, in Self-Regulation and Self-Control. Routledge, 2018, pp 181-220. [DOI] [PubMed] [Google Scholar]
- 38.Rose C: Am I part of the cure or am I part of the disease? Keeping coronavirus out when a doctor comes home. N Engl J Med 2020. [DOI] [PubMed] [Google Scholar]
- 39.Maunder R, Hunter J, Vincent L, et al. : The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ 2003;168:1245-1251. [PMC free article] [PubMed] [Google Scholar]