Abstract
Despite the use of digital technology in healthcare, telemedicine has not been readily adopted. During the COVID-19 pandemic, healthcare systems have begun crisis management planning. To appropriately allocate resources and prevent virus exposure while maintaining effective patient care, our orthopaedic surgery department rapidly introduced a robust telemedicine program during a 5-day period. Implementation requires attention to patient triage, technological resources, credentialing, education of providers and patients, scheduling, and regulatory considerations. This article provides practical instruction based on our experience for physicians who wish to implement telemedicine during the COVID-19 pandemic. Between telemedicine encounters and necessary in-person visits, providers may be able to achieve 50% of their typical clinic volume within 2 weeks. When handling the massive disruption to the routine patient care workflow, it is critical to understand the key factors associated with an accelerated introduction of telemedicine for the safe and effective continuation of orthopaedic care during this pandemic.
Level of Evidence:
V
Telemedicine in the Time of SARS-COV-2
The use of digital technology in the US healthcare system has increased since the implementation of electronic medical record (EMR) systems.1,2 However, telehealth services have not been readily adopted.2,3 As of 2017, only 6.6 telemedicine visits per year were recorded per 1,000 practitioners in the United States, although telehealth delivery for primary care and mental health services is predicted to grow.4
The unanticipated outbreak of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has abruptly changed those predictions. Given the rapid global spread beginning in late 2019 and the severity of coronavirus disease 2019 (COVID-19), especially among the elderly, the US healthcare system has braced for impact.5 With anecdotal reports of shortages of supplies and personnel in Italy and China, as well as parts of the United States, hospital systems have anticipated the sequestering of healthcare resources and personnel.6 To limit the exposure of patients and practitioners to SARS-CoV-2 and to reduce resource consumption, the American College of Surgeons, in conjunction with the recommendation of the US Centers for Disease Control and Prevention, has encouraged the postponement or cancellation of all elective surgical procedures and clinics to focus resources on urgent and emergency patient care only.7
Telemedicine is defined as the remote diagnosis and treatment of patients through telecommunications technology.8,9 In the COVID-19 scenario, telemedicine helps conserve healthcare resources, such as personal protective equipment, continue safe and high-quality patient care, and maintain social distancing to minimize virus spread. In the field of orthopaedic surgery, telemedicine has previously been used to provide “virtual clinics” in rural Iowa10 and Norway11 and for follow-up after total joint arthroplasty.12 Approximately half2 of US hospitals use telemedicine, primarily in the field of radiology, in which remote diagnosis can be achieved via cloud-based imaging systems; however, this communication is largely physician to physician, not physician to patient. During the current crisis, telemedicine has been used to screen for COVID-19 symptoms and to prescribe testing, and its use for other types of care has rapidly expanded.13 In light of the COVID-19 pandemic, the US Department of Health and Human Services has temporarily suspended some Health Insurance Portability and Accountability Act (HIPAA) requirements and also extended the nature of patient visits suitable for telehealth (Table 1).14 The use of telemedicine allows providers to maintain continuity of patient care while triaging patients in preparation for an anticipated case backlog after crisis abatement. In an effort to appropriately allocate resources and prevent virus exposure while maintaining safe, efficient, and effective patient care, our department has urgently introduced a robust telemedicine program.
Table 1.
Sample Triage List for Determining Which Patients May be Appropriate for In-Person Visits During a Public Health Emergency
| Indication for In-Person Visit | Telemedicine May be Appropriate if… |
| Acute fracture requiring surgery or reduction | Imaging is adequate and operative treatment is anticipated |
| Acute joint instability | |
| Acute ligamentous disruption | |
| Acute tendon disruption | |
| Brace complication | |
| Cast change | |
| Concern for acute infection | |
| Concern for dislocation | |
| Drain removal | Home health aide or visiting nurse can safely perform after remote wound check |
| Inability to bear weight | |
| Need for imaging | Adequate imaging has been performed elsewhere with remote review, and patient is otherwise appropriate for remote visit |
| New-onset swelling | |
| New tumor | |
| Pathologic/impending pathologic fracture | |
| Pin removal | |
| Symptomatic tumor | |
| Neurological deficits, including myelopathy | |
| Suture/staple removal | Home health aide or visiting nurse can safely perform after remote wound check |
| Wound complication |
Rapid Implementation
Patient Triage
Before the COVID-19 public health emergency declaration, only one of 36 surgeons in our department was prepared to use synchronous (real-time) remote video technology for patient encounters. A crucial element of telemedicine effectiveness is careful patient selection. Each orthopaedic division within our department created guidelines for determining which patients may require in-person visits, which can be served via telemedicine, and which are appropriate to be rescheduled for after crisis abatement (Table 1). Common reasons that patients were deemed ineligible for telehealth visits were the need for suture or staple removal, the need for a cast change, and the need for a hands-on clinical examination to determine appropriate treatment of an acute injury. Patients who required imaging were assessed on an individual basis to determine whether imaging would best be performed at our clinic (prompting an in-person visit) or at an imaging center near the patient's home (with remote review of images via a HIPAA-compliant, cloud-based platform). Most standard wound checks, range-of-motion checks, and standard postoperative visits do not require in-person visits and are deemed appropriate for telemedicine. Patients whose scenarios are indeterminate are offered a telemedicine visit for remote triage to decide whether an in-person visit is necessary. Each patient who must be seen in the clinic is screened for symptoms of COVID-19 before entering the clinical care area.
Technological Resources
Several priorities were identified for the introduction of this initiative (Table 2). One of the first priorities is to determine the technology resources available in the practice. Each provider requires a device with a functioning camera and microphone, and computing power similar to that required for common video-chat applications, such as Skype (Microsoft, Redmond, WA) or FaceTime (Apple, Cupertino, CA). Providers who intend to perform video visits from a patient care area, such as an office examination room, may consider using a lens cover to avoid unintentionally capturing video of other patients. Our department purchased several additional cameras with lens covers for this purpose. In addition to testing the microphone's audio and camera's video quality, we found it helpful to test each device to ensure adequate bandwidth to support video transfer, particularly in remote locations such as providers' homes.
Table 2.
Task Checklist for Telemedicine Launch
| Category | Tasks |
| Information technology | Ensure adequate bandwidth for remote visits |
| Ensure EMR compatibility | |
| Confirm working cameras/microphones | |
| Obtain covers for cameras as needed | |
| Obtain background shields (to block background from patient view) as needed | |
| Ensure adequate electronic devices/remote computers | |
| Office management | Alter clinic templates |
| Educate patients on telemedicine | |
| Patient triage | Select patients appropriate for telemedicine |
| Policy/credentialing | Ensure telemedicine is within patient care guidelines of institution |
| Ensure telemedicine is within scope of practice as defined by hospital/state | |
| Provider education | Ensure familiarity with telemedicine software |
| Teach providers how to share screen and use other capabilities of the telemedicine platform | |
| Ensure familiarity with camera/microphone setup, troubleshooting | |
| Teach providers how to conduct visits with EMR | |
| Teach providers how to document visits with EMR | |
| Regulations | Obtain patient consent |
| Acknowledge whether originating site restrictions apply | |
| Adhere to billing and coding requirements | |
| Testing | Simulate check-in and visit process |
EMR = electronic medical record
To implement telemedicine, practices may use routine consumer video applications or may select more sophisticated medical applications that interface with common EMR platforms (Table 3). For example, our health system uses Epic software (Epic Systems, Verona, WI) and hosts a HIPAA-compliant remote patient portal. Through this portal, patients connect remotely through the Polycom RealPresence application (Plantronics, Santa Cruz, CA) for a secure, synchronous (real-time) audiovisual encounter. EMR-linked telehealth applications have the advantages of HIPAA compliance and integration with the patient's medical record for documentation and billing purposes. Server requirements for such a platform included 16 physical cores and at least 2.0-GHz speed, and 16 virtual cores to support approximately six simultaneous encounters. Practices running an EMR typically have adequate server capacity to support remote video visits without interfering with office operations. Anecdotally, when running a HIPAA-compliant platform through our practice's server, we have experienced an audiovisual delay of approximately 1 second during video visits. This delay may not impair the quality of the visit but occasionally interrupts the smooth flow of discussion.15,16 For practices not using an EMR system, more basic teleconferencing software may be preferable, which may not require this server capacity.
Table 3.
Examples of Telemedicine Technology Applications and Their Functions
| Application | Manufacturer (Location) | Pros | Cons | HIPAA Compliant | Integrates with EMR |
| American Well | Amwell (Boston, MA) | Integrates with EMR for billing and documentation | Higher cost; greater server requirements | Yes | Yes |
| MDLink | MDLink, Ltd. (Kingston, Jamaica) | Yes | Yes | ||
| Polycom RealPresence | Plantronics (Santa Cruz, CA) | Yes | Yes | ||
| SnapMD | SnapMD (Glendale, CA) | Yes | Yes | ||
| CyraCom | CyraCom (Tucson, AZ) | Low cost | No EMR interface for billing or documentation | Potentiallya | No |
| Zoom | Zoom Video Communications (San Jose, CA) | Potentiallya | No | ||
| FaceTime | Apple (Cupertino, CA) | No | No | ||
| Skype | Microsoft (Redmond, WA) | No | No | ||
| Facebook (Menlo Park, CA) | No | No |
EMR = electronic medical record; HIPAA = Health Insurance Portability and Accountability Act
Standard or basic services with these telecommunication applications may not be HIPAA-compliant, although advanced packages with encryption and password protection can be made to comply with HIPAA security standards.
In addition, the US Department of Health and Human Services, together with the Office for Civil Rights, announced that it would “exercise its enforcement discretion” regarding HIPAA violations made by providers during “good faith” attempts to provide patient care during the COVID-19 pandemic, when use of a non–HIPAA-compliant IT platform is necessary.16 In light of these HIPAA considerations, surgeons may use consumer applications (eg, FaceTime) that can be implemented easily and immediately (Note: providers who use such applications may consider obscuring their cellular telephone numbers, eg, for FaceTime encounters). Cellular connections that can support FaceTime or WhatsApp (Facebook, Menlo Park, CA) are adequate for providers and patients using telemedicine. When using these commercial applications, however, documentation of the encounter within the medical record is still necessary.
Credentialing Considerations
Telemedicine capabilities were verified as being within the credentialing guidelines for providers at our institution and within the scope of practice of individual provider licenses in our state. For advanced practice providers, the addition of a virtual practice location to their state licenses was determined to be unnecessary, although this may differ by jurisdiction. Telemedicine consent forms were made available for providers and office staff to send to patients electronically, and our EMR provider was engaged to add “smart phrases” into the EMR's lexicon to document the use of a 2-way synchronous audiovisual platform of communication, the duration of the encounter (for time-based billing), and verbal consent for the telemedicine encounter (if applicable).
Education of Providers
When introducing our department's telemedicine capabilities, we found it helpful to distribute learning modules about the workflow for scheduling (for office staff) and performing (for providers) remote video encounters, including videos and webinars that simulated the telemedicine functionality. Virtual “office hours” were held by credentialed faculty members who were comfortable with the technology to facilitate peer-to-peer education. “Test patients” were added to our EMR system so that providers could practice navigating the platform independently. For practices using a teleconference platform that is independent of the EMR, “dry-run” encounters with colleagues may be beneficial to optimize the clinical workflow. We developed tip sheets to address common troubleshooting issues (Table 4), and departmental/practice frequently asked questions and lessons learned were distributed.
Table 4.
Tip Sheets Developed to Assist Patients, Office Staff, and Providers With Critical Areas of Troubleshooting
| User Group | Tip Sheet |
| Patients | Welcome letter (explains process, functionality, rationale, and limitations of telemedicine) |
| Telemedicine consent form | |
| Equipment testing and software downloads (for mobile devices, computers) | |
| Electronic patient registration | |
| Office staff | Scheduling a video encounter |
| Arranging for an interpreter for a video visit | |
| How to troubleshoot for patients | |
| Electronic patient registration | |
| Providers | Equipment testing and software downloads (for mobile devices, computers) |
| Starting a scheduled video encounter | |
| Starting an “on the fly” (unscheduled) video encounter | |
| Navigating the telemedicine platform | |
| COVID-19 clinical communications | |
| Legal and billing FAQs |
Education of Patients
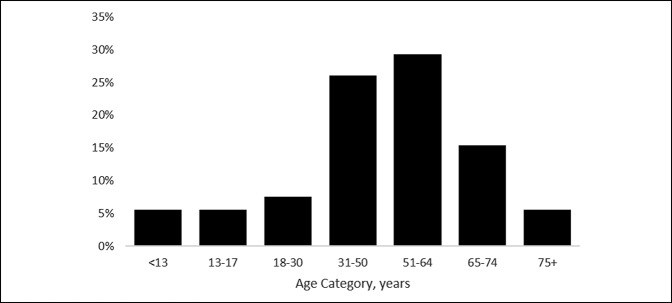
A letter explaining our department's intent to use telemedicine for future clinical encounters was sent to patients via the EMR's patient engagement portal. Other practices may use direct-to-patient marketing channels to contact patients via e-mail or text message regarding this new functionality. Our department's letter explains the decision to implement telemedicine and instructions for scheduling a telemedicine visit. For patients whose clinic visits have been postponed because of the COVID-19 pandemic, office coordinators contact them via telephone and offer to reschedule them via telemedicine. Tip sheets were developed for patients to set appropriate expectations during the encounter and to explain how they can use their devices to check-in remotely and begin a telemedicine visit. As would be expected in an orthopaedic practice, our patients who successfully completed encounters were, on average, older than 50 years (Figure 1).
Figure 1.
Figure demonstrating the age distribution of the first 250 patients who completed successful remote video encounters in one orthopaedic surgery department during the COVID-19 pandemic.
Regulatory Environment
Telemedicine visits require the use of online, synchronous (real-time), 2-way audiovisual portals for patient communication. Alternatively, “e-visits” are those in which established patients communicate asynchronously via an online patient messaging portal. As of March 6, 2020, temporary legislation (ie, a 1,135 Waiver) was enacted, allowing for telehealth parity during this crisis.17 During the COVID-19 public health emergency, the Centers for Medicare & Medicaid Services (CMS) will reimburse physicians for services rendered through telehealth at the same rate as in-person visits, for all diagnoses. Additional relaxation of restrictions on telemedicine visit requirements by CMS during the COVID-19 crisis include the following: allowing for new visits to be performed remotely, easing “originating site” (ie, the patient's location at the time of the visit) requirements to allow telemedicine for patients who were not in rural locations or within another healthcare facility, and suspension of interstate licensing laws (paving the way for states to allow providers to practice telemedicine across state lines if certain criteria are met) (Table 5).18 State licensure laws still apply during this time, although as individual states have declared healthcare emergencies, many have suspended or altered restrictions on providers with valid licenses in other states or jurisdictions providing telehealth services across state lines. This flexibility has been important for our department because approximately 19% of our patients travel from other states for their orthopaedic care. Continued daily updates on regulatory changes, as well as an online posting of frequently asked billing, coding, and regulatory questions, are provided by our department's “physician champion” to our practitioners to keep all informed during this period of frequent changes.17
Table 5.
Comparison of CMS Telehealth Regulatory Requirements Before and After the COVID-19 Emergency Declaration17
| Requirement | Before Declaration | After Declaration |
| HIPAA-compliant communication technology | Required | DHHS and OCR will exercise enforcement discretion regarding HIPAA violations made by providers during “good faith” attempts to provide patient care during the COVID-19 pandemic, when use of a non–HIPAA compliant IT platform is necessary.16 |
| Eligible patients | Limited telehealth visits to patients whom the provider had seen within the previous 3 years | DHHS exercises enforcement discretion regarding an established relationship with a particular practitioner; DHHS will not conduct audits to ensure that such a prior relationship existed.20 |
| Reimbursement rate parity with in-person visits | No | Yes |
| Originating site restrictions | Patients eligible if they lived in a rural location, were in a designated healthcare facility, and were not within a metropolitan region | Originating site restrictions waived |
| Interstate practice | Providers allowed to provide telemedicine services only for patients who were currently within a state or jurisdiction where the provider holds an active license | Waiver of interstate licensure restrictions allow states to determine qualifications for providers in other states to provide care for patients across state lines |
| Flexibility for reduction or waiver of co-insurance/deductible | No | Yes; DHHS allows flexibility for providers to reduce or waive co-insurance or deductibles for federal healthcare programs |
| POS code | 02 (Telehealth) | CMS suggests a POS code of 11 during the COVID-19 public health emergency for telemedicine encounters to indicate that the patient would normally have been seen in the office; other payors may still prefer a POS code of 02 for telehealth services |
| Duration of regulations | Re-evaluated on yearly CMS final rule | Expires at the retirement of the public health emergency declaration |
CMS = Centers for Medicare & Medicaid Services; DHHS = Department of Health and Human Services; OCR = Office of Civil Rights; POS = place of service
Billing and Coding
Current CMS recommendations favor use of the standard office-based evaluation and management codes for remote telemedicine encounters performed in the outpatient setting. Although CMS suggests a “place of service” code of 11 during the COVID-19 public health emergency for telemedicine encounters, indicating the office location where the patient would normally have been seen, other payors may prefer a place of service code of 02 for telehealth services. For the duration of the public health crisis, CMS has allowed level of service requirements to be based on time-based billing or on medical decision-making alone.
Scheduling
Electronic check-in, consent processes, and billing queues were streamlined and automated to improve clinic coordinator workflow. Since the initial provider setup, the greatest continuing challenge has been managing the cameras, microphones, and software on patients' devices to allow HIPAA-compliant video communication. In recognition of the learning curve involved with telemedicine, the number of remote visits was limited at first. New clinic templates were developed to facilitate telemedicine visits. Within the first 2 weeks, most providers scheduled approximately three remote synchronous visits per day, with encounters scheduled hourly to allow time to troubleshoot and orient to the new interface. As our provider workflows have become more streamlined, each provider is paired with a medical office coordinator or medical assistant to help prepare patients for remote visits. Office coordinators and medical assistants were taught how to help patients set up their telecommunications software, test their devices, and check-in online. Patients are contacted 10 minutes before the scheduled encounter to help them prepare and to answer any questions. This format has worked well during the first 2 weeks, with visits now commonly scheduled every 30 minutes. Most providers are templated for blocks of 2 to 3 consecutive hours of remote encounters on specific days of the week.
Early Experience
One week after implementation, we surveyed providers to identify barriers to their use of telemedicine and to compile additional tips and best practices. Providers anticipated seeing, on average, approximately 25% of their normal clinic volume remotely during the following week. Respondents estimated that nearly one-third of their patients would be appropriate for telemedicine visits during the pandemic. Considering both telemedicine and in-person visits, we estimate that most providers will achieve nearly 50% of their typical clinic volume within 2 weeks of implementation. The 50% of patients visits not completed via telemedicine or in person has consisted predominantly of nonurgent follow-up and routine postoperative visits. These patients can be safely managed with asynchronous (messaging or e-mail) communication or postponement until the COVID-19 crisis has abated.17-19
Summary
As we adapt to the quickly evolving challenges during the COVID-19 pandemic, we embrace the flexibility that is imperative for crisis management. The pandemic has upended routines and patterns in our department and removed the barriers of inertia that would have prevented such major changes in our practice. The marked disruption of our ability to continue routine patient care drove the accelerated introduction of novel tools to provide evaluation and treatment involving a concerted effort across all orthopaedic divisions. We are still learning and troubleshooting our new workflows, but telemedicine has been critical to the safe and effective continuation of orthopaedic care during this challenging time. We hope that, by using such technology, we can continue serving our patients with musculoskeletal conditions while reducing infection risk and the burden on our healthcare system.
Footnotes
None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Loeb, Dr. Rao, Dr. Ficke, Dr. Morris, Dr. Riley, Dr. Levin.
References
- References printed in bold type are those published or accessed online in 2020.
- 1.Baker J, Stanley A: Telemedicine technology: A review of services, equipment, and other aspects. Curr Allergy Asthma Rep 2018;18:60. [DOI] [PubMed] [Google Scholar]
- 2.Mechanic OJ, Kimball AB: Telehealth Systems. Treasure Island, FL, StatPearls [Internet] StatPearls Publishing. Available at: https://www.ncbi.nlm.nih.gov/books/NBK459384/. Accessed March 30, 2020. [Google Scholar]
- 3.Scott Kruse C, Karem P, Shifflett K, et al. : Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare 2018;24:4-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barnett ML, Ray KN, Souza J, Mehrotra A: Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA 2018;320:2147-2149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Del Rio C, Malani PN: COVID-19-New insights on a rapidly changing epidemic. JAMA 2020; 323:1339-1340. [DOI] [PubMed] [Google Scholar]
- 6.Ranney ML, Griffeth V, Jha AK: Critical supply shortages—the need for ventilators and personal protective equipment during the covid-19 pandemic. N Engl J Med 2020; Mar 25 [Epub ahead of print]. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 7.American College of Surgeons: COVID-19 and surgery: Clinical issues and guidance. Available at: https://www.facs.org/covid-19/clinical-guidance. Accessed March 30, 2020.
- 8.Bashshur RL, Shannon GW, Krupinski EA, et al. : National telemedicine initiatives: Essential to healthcare reform. Telemed J E Health 2009;15:600-610. [DOI] [PubMed] [Google Scholar]
- 9.NEJM Catalyst: What is telehealth? Available at: https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0268. Accessed March 30, 2020. [Google Scholar]
- 10.Gruca TS, Pyo TH, Nelson GC: Improving rural access to orthopaedic care through visiting consultant clinics. J Bone Joint Surg Am 2016;98:768-774. [DOI] [PubMed] [Google Scholar]
- 11.Buvik A, Bugge E, Knutsen G, Smabrekke A, Wilsgaard T: Patient reported outcomes with remote orthopaedic consultations by telemedicine: A randomised controlled trial. J Telemed Telecare 2019;25:451-459. [DOI] [PubMed] [Google Scholar]
- 12.Marsh J, Hoch JS, Bryant D, et al. : Economic evaluation of web-based compared with in-person follow-up after total joint arthroplasty. J Bone Joint Surg Am 2014;96:1910-1916. [DOI] [PubMed] [Google Scholar]
- 13.Hollander JE, Carr BG: Virtually perfect? Telemedicine for covid-19. N Engl J Med 2020; Mar 11 [Epub ahead of print]. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 14.Anonymous: Coronavirus Prepardness and Response Supplemental Appropriations Act, HR 6074, 116th Congress (2020). Available at: https://www.govtrack.us/congress/bills/116/hr6074. Accessed March 30, 2020. [Google Scholar]
- 15.Polycom: Polycom RealPresence Platform, Virtual Editions. Available at: https://www.polycom.com/content/dam/polycom/common/documents/data-sheets/realpresence-platform-virtual-editions-ds-enus.pdf. Accessed April 3, 2020. [Google Scholar]
- 16.U.S. Department of Health and Human Services: Notification of Enforcement Discretion for Telehealth Remote Communications During the COVID-19 Nationwide Public Health Emergency. Available at: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html. Accessed March 30, 2020. [Google Scholar]
- 17.Centers for Medicare & Medicaid Services: Medicare Telemedicine Health Care Provider Fact Sheet. Available at: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed March 30, 2020. [Google Scholar]
- 18.Centers for Medicare & Medicaid Services: 2019-Novel Coronavirus (COVID-19) Medicare Provider Enrollment Relief Frequently Asked Questions (FAQs). Available at: https://www.cms.gov/files/document/provider-enrollment-relief-faqs-covid-19.pdf. Accessed March 30, 2020. [Google Scholar]
- 19.Wongworawat MD, Capistrant G, Stephenson JM: The opportunity awaits to lead orthopaedic telehealth innovation: AOA critical issues. J Bone Joint Surg Am 2017;99:e93. [DOI] [PubMed] [Google Scholar]
- 20.Centers for Medicare & Medicaid Services: Medicare telehealth frequently asked questions (FAQs) March 17, 2020. Available at: https://edit.cms.gov/files/document/medicare-telehealth-frequently-asked-questions-faqs-31720.pdf. Accessed April 7, 2020. [Google Scholar]