Abstract
Guinea pigs have been used in diverse studies to better understand acquired hearing loss induced by noise and ototoxic drugs. The guinea pig has its best hearing at slightly higher frequencies relative to humans, but its hearing is more similar to humans than the rat or mouse. Like other rodents, it is more vulnerable to noise injury than the human or nonhuman primate models. There is a wealth of information on auditory function and vulnerability of the inner ear to diverse insults in the guinea pig. With respect to the assessment of potential otoprotective agents, guinea pigs are also docile animals that are relatively easy to dose via systemic injections or gavage. Of interest, the cochlea and the round window are easily accessible, notably for direct cochlear therapy, as in the chinchilla, making the guinea pig a most relevant and suitable model for hearing. This article reviews the use of the guinea pig in basic auditory research, provides detailed discussion of its use in studies on noise injury and other injuries leading to acquired sensorineural hearing loss, and lists some therapeutics assessed in these laboratory animal models to prevent acquired sensorineural hearing loss.
I. INTRODUCTION
Stebbins et al. (1982) suggested the guinea pig to be one of the most useful species in which to assess the effects of noise on the inner ear based on overlap with the audible frequency range in the human as well as presumed overlapping vulnerabilities and the relative ease of training of guinea pigs for use in psychophysical testing. Since then, the guinea pig has been widely used in studies on hearing loss induced by noise and drug injury and prevention of this acquired sensorineural hearing loss (i.e., otoprotection). Other species are also of interest such as the cat, chinchilla, and monkey (Stebbins et al., 1982). This review paper focuses on the use of the guinea pig in studies on acquired sensorineural hearing loss and otoprotection and is broken into four main sections in which (1) basic information about the guinea pig as a laboratory animal subject is provided, (2) strategies for the assessment of auditory function are introduced, (3) necessary regulatory requirements for the maintenance of guinea pigs are provided, (4) the effects of noise and ototoxic drugs on the guinea pig inner ear are discussed, and (5) efforts to prevent noise injury and drug ototoxicity using pharmaceutical interventions are reviewed. For detailed reviews of other species widely used in hearing science, noise and drug injury, and otoprotection research, readers are referred to other papers in this special issue for reviews of the mouse (Ohlemiller, 2019), rat (Escabi et al., 2019; Holt et al., 2019), chinchilla (Trevino et al., 2019; Radziwon et al., 2019), and non-human primate (Burton et al., 2019). Briefer discussion comparing the relative strengths and weaknesses of multiple rodent species in studies on noise injury and its prevention is available in Lynch et al. (2016). The overarching goal of the current series of species-specific papers is to provide comprehensive insight into the various laboratory animal models that are commonly considered for use in drug development research focused on the prevention of NIHL, with commentary on issues that may impact study design and outcomes.
II. THE GUINEA PIG AS A LABORATORY ANIMAL
A. Basic health
Guinea pigs (Cavia porcellus) are relatively large (female: 100–900 g; male: 900–1200 g) rodents; they are very docile animals that rarely bite or scratch, making them easy to work with in laboratory settings. Guinea pigs live approximately 5–7 years (Quesenberry, 1994). The guinea pig and chinchilla (Chinchilla lanigera) are subgroups of the order Rodentia, belonging to the suborder Hystricognathi and infraorder (family) Caviomorpha. Two of the most commonly used strains are the Hartley and Dunkin-Hartley albino strains; however, pigmented strains are also available. Detailed discussions of guinea pig physiology, husbandry, and diseases are readily available (Quesenberry, 1994; Donnelly and Brown, 2004). Healthy guinea pigs should be active, with bright eyes, shiny coats, and no discharge from the eyes or noise (Yarto-Jaramillo, 2011).
B. Pigmentation
Both pigmented and albino guinea pig strains have been used in auditory research; they exhibit differences in peripheral and central auditory function (Bock and Steel, 1984). These differences may be a consequence of the absence of melanin in the cochlea of the albino guinea pig. Melanin, produced by melanocytes in stria vascularis within the cochlea of pigmented animals, has been shown to protect against damage (Xiong et al., 2011), perhaps mediated by the involvement of melanin in the active transport of Ca2+ into endolymph (Gill and Salt, 1997) or antioxidant properties of melanin. The effect of pigmentation, including a protective role of melanin, has also been described in noise- and drug-induced hearing loss (DIHL) in other rodent species (Wu et al., 2001; Murillo-Cuesta et al., 2010). Interestingly, this protective role of pigmentation is not observed in aging animals, as pigmented guinea pigs develop more age-related hearing loss (ARHL) than albino animals (Dum et al., 1980a; 1980b; Dum, 1984). When possible, a discrimination between albino and pigmented guinea pig models is made in the descriptions of hearing loss induced by age, drugs, and noise below.
C. Diet and nutrition
Across rodents, there are important differences in digestive anatomy, leading to differences in dietary recommendations (Grant, 2014). Diet and nutrition are important considerations in the overall design of otoprotection research studies [see Spankovich and Le Prell (2019)] and are directly relevant to the use of guinea pigs in studies on noise injury and its prevention for two key reasons. First, guinea pig diets must contain vitamin C as the guinea pig, like humans, cannot synthesize its own endogenous vitamin C (Chatterjee et al., 1975; Jenkins, 2010) due to the lack of the hepatic enzyme L-gulonolactone oxidase, which converts dietary glucose into vitamin C (Jenkins, 2010; Yarto-Jaramillo, 2011). This has made the guinea pig particularly popular in studies assessing dietary supplements that include vitamin C as one of the active agents (McFadden et al., 2005; Le Prell et al., 2007a; Le Prell et al., 2011a). Second, the ototoxic side effects of noise, aminoglycosides, and cisplatin are increased in animals fed diets that have nutrient deficits, including for example low protein, low iron, and reduced vitamin A diets (Biesalski et al., 1990; Lautermann et al., 1995b; Lautermann and Schacht, 1996; Yu et al., 2016).
With respect to guinea pig digestion, food typically has left the stomach within 2 h of consumption and total duration of gastrointestinal processing is approximately 20 h [for review see Grant (2014)]. For otoprotective agents that are delivered orally, it is important to understand digestion and absorption rates for active agents [for detailed discussion of drug absorption and related issues, see Cousins (2019)]. Additional brief discussion of the importance of pharmacokinetic and pharmacodynamic data in studies on noise injury and its prevention is available in Lynch et al. (2016); oral dosing via food supplements can make the collection of such data more challenging.
It has been suggested that fresh greens, such as cabbage, kale, spinach, chicory, dandelion and beet greens, and parsley, as well as broccoli, yams, and carrots, should be provided to supplement food pellets (Quesenberry, 1994; Yarto-Jaramillo, 2011; Grant, 2014). These foods are all nutrient dense, with many of the vitamins and minerals they contain hypothesized to provide protection against ototoxic injury (Haase et al., 2009; Le Prell and Spankovich, 2013). Thus, potential confounds that may be introduced by nutrient dense food supplements that support endogenous antioxidant activity should be carefully considered as part of study design and discussed with animal husbandry to assure careful control of relevant scientific variables.
As described by Grant (2014), guinea pigs are strict herbivores, typically consuming short grasses in open grasslands in the wild; in captivity, grass hay is important for adults, and a mix of grass hay and alfalfa is necessary for juvenile guinea pigs and lactating females. Clover and alfalfa hays should be avoided for adult animals as they may damage the renal system (Yarto-Jaramillo, 2011). The highly fibrous diet in the wild wears down guinea pig (and chinchilla) teeth and, thus, their teeth grow continuously across their lifespan; dental issues in captive animals are common and access to appropriate chewing materials is necessary [see Jenkins (2010), Yarto-Jaramillo (2011), and Grant (2014)]. While these issues are not likely to directly affect hearing per se, laboratory animals that lack chewing materials and suffer from dental issues may not be able to consume chow and may suffer from nutritional deficits that influence vulnerability to noise injury.
D. Health concerns
Animals that are ill may have concomitant nutritional deficits if they are not consuming daily chow requirements, and may be predisposed to other injury. A primary health concern in guinea pigs is thus the prevention of respiratory disease (Quesenberry, 1994; Yarto-Jaramillo, 2011). Respiratory disease can result from overcrowding and other housing-related issues such as poor ventilation, temperature changes, inappropriate (too warm, too cold) temperatures, dust in the environment, and changes in humidity; pneumonia is common when housing conditions are damp or drafty [for review, see Yarto-Jaramillo (2011)]. Another leading cause of respiratory disease in guinea pigs is pathogen exposure, with bacterial, viral, and fungal pathogens all inducing respiratory issues [for review, see Yarto-Jaramillo (2011)]. Infections are particularly likely to be transferred from dogs and rabbits, if multiple species are maintained in close proximity or by the same husbandry personnel. Antibiotic management is possible, but penicillin and macrolide antibiotics are to be avoided (Quesenberry, 1994) and antibiotics (aminoglycosides) leading to hearing loss must not be used for infection control in animals in which hearing function serves as a study outcome.
A second key concern is lesions on the surfaces of the feet and injury to the feet, which can be caused by wire floors or rough bedding, as well as dirty bedding and inappropriate sanitary control (Quesenberry, 1994; Jenkins, 2010). Hair loss and superficial dermatitis secondary to biting or self-trauma are possible (Quesenberry, 1994). Biting and self-trauma can also occur subsequent to injections, particularly when intra-muscular injections are delivered to the quadriceps muscle in the hind legs. If an agent of interest must be delivered using intra-muscular injection, the needle and volume should both be as small as possible; although individual animal care units may have different specific guidance, current guidance should also be sought from relevant oversight and regulatory agencies [see, for example, the information posted on the NIH Office of Intramural Research Office of Animal Care and Use (https://oacu.oir.nih.gov/sites/default/files/uploads/training-resources/rodentinjection.pdf) or the Canadian Council on Animal Care (CCAC) (Canadian Council on Animal Care, 1993)]. Parasites such as fur mites and fungal infections can also cause hair loss with scaly or crusty lesions (Quesenberry, 1994).
E. Social behavior
Guinea pigs are highly social and herd formation has been observed in domesticated and wild guinea pig populations [for discussion, see Donnelly and Brown (2004) and Brewer et al. (2014)]. Thus, there have been some efforts to explore potential social enrichment using open-field arenas that allow herd-like interactions (Brewer et al., 2014). Guinea pigs have a diverse range of social behaviors, and a detailed review is available in Harper (1976). In brief, approach behaviors commonly include nose to nose contact, but may also include contact of the snout with the ears or perineum of other animals. At rest, guinea pigs commonly show huddling behavior in which they lie side to side, in contact with each other; however, mutual grooming is not a common social behavior within adult guinea pigs (see Harper, 1976). Female pairs typically can be housed together for social enrichment, but male pairs should be avoided to reduce the risk of fighting (Raje and Stewart, 2000). Male/female pairs are typically to be avoided as guinea pigs can start breeding as early as 4–6 weeks of age.
When guinea pigs and other rodents are group housed, study designs have sometimes employed ad libitum access to supplemented food (Le Prell et al., 2011b; Le Prell et al., 2014c) or supplemented water (Davis et al., 2007), foregoing monitoring of intake and losing the ability to estimate dosing or dose equivalence across animals. When group housing is used, potentially aggressive behaviors should be monitored during daily health checks. Aggressive postures include the head raised, mouth partially open, forelegs extended, and back legs crouched; during an attack the head is thrust forwards and biting of the nose and lips can occur if neither backs down [see Harper (1976)]. If one of the guinea pigs flees, the other may chase the fleeing animal and deliver deep bites to the retreating animal. It is possible for death to occur when males vie for dominance, although it is also possible for evenly matched males to reach a standoff limited to aggressive posturing [see Harper (1976)].
F. Vocal behavior
The guinea pig has a rich vocal behavior system which has made them a species of interest for investigating the processing of vocal communication in the central auditory system (CAS), including inferior colliculus (Suta et al., 2003; Suta et al., 2013; Lyzwa et al., 2015), thalamus (Philibert et al., 2005; Suta et al., 2007; Suta et al., 2013), and auditory cortex (Syka et al., 2005; Wallace et al., 2005; Grimsley et al., 2011; Suta et al., 2013). Early observations of vocal behavior by adult and infant guinea-pigs housed within a large colony revealed 11 call types belonging to 5 functional categories (Berryman, 1976). As per the detailed review and discussion by Harper (1976), whistles, screams, and squeals are generally higher frequency vocalizations with energy up to 16–32 000 Hz whereas chutt, chutter, whine, tweet, low whistle, purr, and drr calls generally are lower frequency calls that do not include significant energy above 4000 Hz. The whistle has been suggested to serve as a distress call (Suarez and Gallup, 1982). There is an extensive literature on changes in guinea pig vocal behavior as a tool in pharmacological research and development (Groenink et al., 2015).
There is ongoing discussion of the extent to which neurons in the medial geniculate body of the thalamus and the auditory cortex of the guinea pig are selective for complex acoustic features specific to vocalizations and thus the extent to which guinea pigs provide a good model of the specialized processing that occurs in the non-human primate and human auditory systems (Suta et al., 2008; Suta et al., 2013). There is also a significant body of research establishing the changes in CAS processing of acoustic signals that occur as a consequence of noise exposure (Mulders and Robertson, 2013; Heeringa and van Dijk, 2018). These paradigms could be readily exploited for use assessing the extent to which otoprotective agents prevent changes in processing complex signals at the level of the CAS, particularly with the significantly increased interest in the effects of noise on supra-threshold function, such as the processing of speech stimuli in quiet and in noise (Bramhall et al., 2019; Le Prell, 2019).
III. SENSORY FUNCTION IN THE GUINEA PIG
A. Sensory function
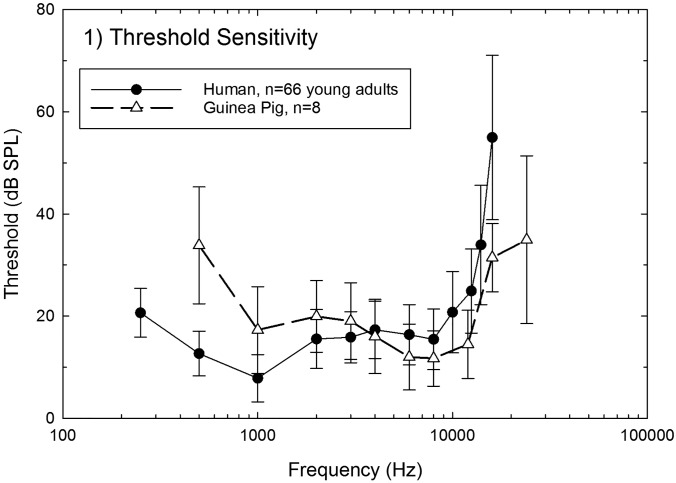
Guinea pigs have sensitive hearing and good vision. The guinea pig has better hearing at higher frequencies, relative to humans. The human hearing range is typically defined as 20–20 000 Hz, whereas the guinea pig hears sounds from 150 to 50 000 Hz. For humans, hearing is best from about 1000 to 4000 Hz, whereas for guinea pigs, hearing is best from about 8000 to 16 000 Hz. Early work using classical conditioning techniques revealed relatively good sensitivity to tones at frequencies up to about 40 to 50 000 Hz, with sharply decreasing performance through as high as 80 to 100 000 Hz (Wever et al., 1963). Subsequent work using operant conditioning techniques confirmed and extended these results (Heffner et al., 1971; Walloch and Taylor-Spikes, 1976). A comparison of the human and guinea pig audiogram is shown in Fig. 1. As noted above, the guinea pig has been previously suggested to be one of the most useful species in which to assess the effects of noise on the inner ear, based on both overlap with the human with respect to audible frequency range (which may drive overlap in vulnerability to injury), and the relative ease of training guinea pigs to perform detection and discrimination tasks [see Stebbins et al. (1982)]. Although psychophysical data provide powerful direct comparison with human results, two of the most commonly used methods of assessing auditory function in the guinea are non-behavioral tests, including otoacoustic emissions (OAEs) and the sound evoked auditory brainstem response (ABR).
FIG. 1.
Average audiometric thresholds measured from 66 normal hearing young adults who participated in the study by Spankovich et al. (2014) are illustrated in combination with average audiometric thresholds measured from eight young adult guinea pigs (unpublished data collected at the University of Florida). All data are mean ± standard deviation of the mean.
B. Otoacoustic emissions (OAEs)
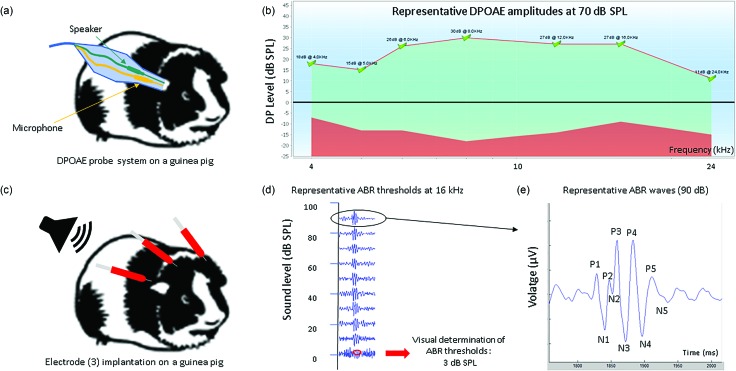
OAEs do not measure hearing per se; rather, they provide a sensitive and objective measure of how well the outer hair cell (OHC) population is functioning. One of the most commonly measured emissions is the distortion product otoacoustic emission (DPOAE); DPOAE thresholds and DPOAE response amplitude are routinely used to assess the integrity of the OHC active process both before and after noise exposure, with tests completed in control animals and animals treated with potential otoprotective agents. Prevention of noise-induced DPOAE deficits provides evidence of drug-mediated hair cell preservation. Because DPOAEs are not influenced by the status of the ascending neural pathway, they are not sensitive to damage to or protection of the neural pathways. Thus, DPOAEs are commonly measured in combination with the sound-evoked ABR. An example of the DPOAE measure is shown in Fig. 2.
FIG. 2.
(a) Schematic cartoon of the probe microphone assembly entering the ear for distortion-product otoacoustic emission (DPOAE) measurement; tones are delivered via the speaker (green) and emissions are measured using the microphone (yellow). (b) Normal DPOAE amplitude in the guinea pig is shown for test signals of 70 dB SPL. (c) Schematic cartoon illustrating three electrode locations used to record the ABR. (d) Tones are presented at decreasing levels from 0 to 90 dB SPL and ABR threshold is determine based on visual inspection of waveforms. (e) Typical ABR waveforms (16 kHz, 90 dB SPL) illustrating the peaks (P) and troughs (N), defining each wave amplitude. The five marked waves (P1–P5) reflect specific central activity. P1: auditory nerve; P2: cochlear nucleus; P3: superior olivary complex; P4: lateral lemniscus; P5: inferior colliculus. (Unpublished data collected at CILcare.)
C. Auditory brainstem response (ABR)
The ABR provides a sensitive and objective measure of the transmission of auditory information from the auditory periphery (cochlea) to the auditory nerve and across the auditory brainstem. The ABR reflects the synchronous discharge of multiple neurons induced by short tone pips. There are multiple “waves” in the ABR and each wave represents synchronous discharge of neurons at discrete locations in the peripheral and central auditory systems. For many years, ABR thresholds have been considered a gold standard measure for the recovery of auditory function after noise exposure, and the documentation of permanent noise-induced threshold changes. Although thresholds are typically about 10–15 dB higher when measured using ABR techniques instead of psychophysical detection thresholds based on behavioral detection responses, this is readily explained by reduced opportunity for temporal integration when brief tone pip signals are used instead of the longer tones used in psychophysical detection studies (Le Prell et al., 2004). More recently, ABR wave I response amplitude has emerged as a metric of interest, as decreases in the amplitude of this neural evoked response, occurring in the absence of permanent threshold shift (PTS), are highly correlated with damage to the synapses connecting the inner hair cells (IHCs) to the auditory nerve (Sergeyenko et al., 2013; Kujawa and Liberman, 2015). Prevention of noise-induced ABR threshold and amplitude deficits would provide evidence of drug-mediated protection of not only the OHCs but also the ascending neural pathway. Illustration of ABR thresholds and waves is provided in Fig. 2.
With the easy availability of equipment that facilitates the collection of OAE and ABR data in laboratory animals, the number of laboratories routinely using behavioral techniques to collect threshold data has decreased. Nonetheless, behavioral techniques provide a powerful opportunity to assess noise-induced tinnitus, and noise-induced deficits in other auditory processing domains, such as detection of intensity differences, frequency differences, and changes in vocalization signals. Thus, the sensory test paradigms that have been used to probe auditory function in guinea pigs are briefly reviewed in the following sections.
D. Positive reinforcement
Guinea pigs can be trained to push buttons or levers when they detect sound, or changes in sound, and they have therefore been widely used in psychophysical studies employing behavioral testing (Petersen et al., 1977; Stebbins et al., 1984). Many of these investigations have used positive reinforcement paradigms, with food used as a reward for correct responses in guinea pigs maintained on restricted diets. Careful investigation of the effects of food restriction and reinforcement paradigms by Hirsch and Collier (1974) reveals a need for caution with respect to the strategy used for limiting guinea pigs' access to food. Although guinea pigs compensated for limited access to food by eating either more quickly or for a longer period of time when food was available, guinea pigs with access to only a single meal per day did not achieve normal adult body weights; the significantly lower body weights were attributed to an inability to process large volumes of food in a short period of time (Hirsch and Collier, 1974). Relevant to acquired sensorineural hearing loss, operant techniques have been leveraged to assess the effects of ototoxic drugs (Prosen et al., 1978a; Prosen et al., 1978b) and excitotoxic agents (Le Prell et al., 2004) on threshold sensitivity in the guinea pig. Whereas ototoxic aminoglycoside antibiotics induced PTS, excitotoxic agents induced temporary threshold shifts (TTS) that recovered subsequent to infusion of the excitotoxin. The ability to reliably measure threshold sensitivity using positive reinforcement procedures has also resulted in extensive use of guinea pigs for evaluating the perceptual consequences of parametric manipulation of cochlear implant programming parameters (Miller et al., 1995a; Miller et al., 1995b; Miller et al., 1999; Miller et al., 2000; Su et al., 2008; Kang et al., 2010; Pfingst et al., 2011; Zhou et al., 2015).
E. Conditioned avoidance
In conditioned avoidance paradigms, animals perform a trained response in order to avoid a punishment—typically, a mild foot shock stimulus. A classic paradigm is the use of a shuttle box, in which animal subjects must move to a different compartment when an auditory stimulus is presented to avoid the delivery of the foot shock. Guinea pigs have been described as more likely to freeze than to perform the desired avoidance behavior in such paradigms (Webster and Rabedeau, 1964; Webster et al., 1965). Careful manipulation of the response window to allow avoidance behaviors to emerge subsequent to stereotypical freezing behavior has allowed some success within this paradigm (Evonic and Brimer, 1967). However, this freezing response has limited the use of the guinea pig in conventional shuttle box studies. Opportunities to use avoidance behavior as a tool within the guinea pig model are perhaps increasing given a number of recent successful efforts to use an aversive air stream in place of foot shock. The use of this less stressful stimulus has resulted in the ability to induce avoidance behavior rather than freezing behavior (Philippens et al., 1992; Agterberg et al., 2010; Agterberg and Versnel, 2014). This shuttle box-based approach has been used to investigate tinnitus in guinea pigs (Heeringa et al., 2014), and it is possible that additional work could be initiated, particularly with respect to noise-induced tinnitus.
F. Reflex inhibition
For paradigms using reflex inhibition, acoustic (“pre-pulse”) stimuli are used to modify the strength of subsequent reflexive startle responses induced by a “pulse” stimulus, such as a loud acoustic signal. Acoustic pre-pulse inhibition (PPI) protocols were largely developed using rats (Ison and Hammond, 1971; Ison et al., 1973; Ison and Krauter, 1974; Parisi and Ison, 1979; Ison, 1982) with later development in mice (Ison et al., 2002; Ison et al., 2005), but there has also been some application of this technique to the guinea pig. By manipulating the frequency and level of the preceding (pre-pulse) inhibitory signal, Young and Fechter (1983) generated guinea pig audiograms that closely paralleled audiograms generated using positive reinforcement paradigms (Prosen et al., 1978a). Although thresholds were about 10–15 dB higher when measured using pre-pulse inhibition techniques, this is readily explained by reduced opportunity for temporal integration when brief pre-pulse signals are used instead of the longer tones used in classic studies (for discussion see Young and Fechter, 1983).
In a more recent variation on this task, an airpuff is used in place of the loud acoustic signal as experimental protocols that damage the ear (i.e., noise exposure, ototoxic drug treatment) can compromise sound-induced startle reflexes (Lobarinas et al., 2013; Lobarinas et al., 2017). Another significant permutation of the task is the replacement of the acoustic pre-pulse signal with a silent gap, termed Gap-Prepulse Inhibition of the Acoustic Startle Reflex (GPIAS) (Turner et al., 2006; Turner et al., 2012; Galazyuk and Hebert, 2015; Schilling et al., 2017). Although GPIAS has been successfully applied in studies of tinnitus using guinea pigs (Mulders et al., 2014; Zhang et al., 2019), GPIAS is not fully understood within guinea pigs as GPIAS results were variable in a comparison of subjects drawn from two colonies of outbred tri-colour guinea pigs (Leggett et al., 2018). The laboratory rat remains the most prominent species used for investigating tinnitus at the behavioral level, although there are some data from guinea pigs trained to distinguish silent intervals from sound intervals (Moody, 2004). Because there is not a wide range of genetically modified rat strains, mice are also highly used in tinnitus studies (von der Behrens, 2014).
G. Schedule-induced polydipsia
In schedule-induced polydipsia paradigms, food-restricted animals are given access to both food and water during test sessions. When food pellets are delivered on a fixed time schedule, excessive drinking is observed. This phenomenon is well established in rats and mice, including development of a novel schedule-induced polydipsia avoidance conditioning paradigm for use assessing tinnitus percepts in rats (Lobarinas et al., 2004). The evidence is less consistent in guinea pigs, however, with two small studies showing the development of exaggerated drinking in either 2 of 3 guinea pigs (Porter et al., 1977) or 0 of 3 guinea pigs (Urbain et al., 1979). There has been little additional literature on schedule-induced polydipsia in guinea pigs since these early reports, and it seems unlikely that this technique will be used to further understanding of noise injury and its prevention, using the guinea pig as a model.
H. Supra-threshold processing
The above techniques, particularly operant training techniques that rely on positive reinforcement, have been used to measure supra-threshold auditory function, providing insight into intensity discrimination in guinea pigs (Prosen et al., 1981; Stebbins, 1982), interactions between acoustic and electro-acoustic stimulation (Le Prell et al., 2006), and frequency discrimination in chinchillas (Prosen et al., 1989). In a unique approach modeled after these classic psychoacoustic investigations, simple acoustic stimuli were replaced with noise-like non-harmonic broadband sounds as targets, with manipulated versions of these sounds and sound sequences used to assess recognition and discrimination (Ojima et al., 2012). Although powerful techniques for investigation of the effects of noise on auditory function are clearly available, there has been only limited collection of behavioral data after noise exposure [see, for example, Prosen et al. (1990)]. Given the significant current interest in the effects of noise on human supra-threshold function (Bramhall et al., 2019; Le Prell, 2019), it is indeed worthwhile for researchers to be familiar with the behavioral techniques that can be used to measure supra-threshold effects of noise exposure in the guinea pig model.
IV. REGULATORY ISSUES
A. National regulations
In the United States, the treatment, care and use of animals in research is regulated by the Animal Welfare Act (AWA), a federal law signed in 1966. The AWA defines the guinea pig as a protected species; hamsters (Cricetinae) and gerbils (Gerbillinae) are also protected, whereas mice (Mus) and rats (Rattus) are excluded from the protections. Compliance with AWA standards is intended to ensure the humane care and treatment of animals, including housing standards. Other nations have their own national guidance, but there are a number of commonalities across documents.
In the AWA, some specifications are defined for each species, in particular space for housing (i.e., size of the cage and the floor, see Table I) and feeding. In addition to the parameters in Table I, wire-bottom cages must be designed to provide sufficient support for the animals' feet, and the space between the wires in the floor grid must be small enough to preclude entrapment of animals' feet. The CCAC (Canadian Council on Animal Care, 1993) advocates that guinea pigs not be individually housed, but housed in groups consistent with their natural environment. Consistent with safety guidance in the AWA, they recommend that solid bottom cages be chosen to create a safe and healthy microenvironment with plastic “shoe box” or “drawer-style” cages being the preferred choice; if cages have wire mesh floors, the mesh must be smooth and hole sizes small such that injury is prevented. The cleaning of the cage requires pretreatment by acid, due to the urine of guinea pigs, produced in large volume and which contains proteins (National Research Council, 1996).
TABLE I.
Comparison of recommended space for Guinea pigs in US, Canada and Europe.
| Countries | Weight (g) | Minimal height (cm) | Floor area/animal (cm2) | Comments |
|---|---|---|---|---|
| U.S. | <350 | 17.8 | 387 | Larger animals may require more space to meet the performance standard |
| >350 | 17.8 | 651.5 | ||
| Canada | <350 | 18 | 300 | — |
| >350 | 22 | 650 | ||
| Europe | <200 | 23 | 200 | — |
| Over 200 to 300 | 23 | 350 | ||
| Over 300 to 450 | 23 | 500 | ||
| Over 450 to 700 | 23 | 700 | ||
| >700 | 23 | 900 |
With respect to feeding, the feeder must not be suspended; a J-shape feeder placed on the floor is the best device, as this prevents guinea pigs from nesting in the feeder. As noted above, guinea pig diets must be fortified with vitamin C, directly provided in the drinking water or via food supplements including vegetables as kale (National Research Council, 1996). As per the CCAC, automatic watering devices are to be avoided as guinea pigs often play with these devises, potentially resulting in wet bedding or flooding (Canadian Council on Animal Care, 1993). Human caretakers are encouraged to pay attention to the vocalization of guinea pigs, as vocalizations are an important part of their social behavior (as described above).
The European Union (EU) also uses legislation to protect the welfare of animals. Directive 2010/63/EU (European Parliament, 2010) follows the Replacement, Reduction, and Refinement (3 R) principles specified in other national guidelines. Like other guidance noted above, the Directive provides general guidelines for the facility, environmental controls including temperature and lighting, housing, enrichment and feeding requirements for rodents, guinea pigs and non-human primates, and specific guidelines for minimum enclosure area measurements for guinea pigs. There are many other national regulations. Researchers working in different countries must of course comply with their own national regulations and ethical committee rules and guidance; however, many journals require that research published within their journal comply with specific ethical guidance documents. For example, the Journal of the Acoustical Society of America requires that studies be in compliance with the Council for International Organizations of Medical Sciences (CIOMS) document: “International Guiding Principles for Biomedical Research Involving Animals-1985”) (Acoustical Society of America, 2004). Other auditory journals that commonly publish otoprotection research have different requirements. For example, the journal Hearing Research requires compliance with the ARRIVE guidelines originally published in PLOS Biology, in addition to requiring compliance with the U.K. Animals (Scientific Procedures) Act, 1986, EU Directive 2010/63/EU for animal experiments, or the National Institutes of Health Guide for the Care and Use of Laboratory animals (NIH Publications No. 8023, revised 1978). Those working in non-U.S. and non-U.K. locations should be aware of the U.S. and U.K. requirements and should assure compliance with these commonly cited compliance requirements. Broad compliance with common standards will improve reproducibility of scientific outcomes, by decreasing the variability in housing and animal care factors that may influence animal health, stress, and nutritional status, all of which may influence study outcomes.
B. Anesthesia
Anesthesia of guinea pigs and other laboratory animals is regulated by national standards; moreover, there are basic effects of anesthesia on auditory function that should be additionally considered as part of the scientific design of studies assessing auditory function. Isoflurane, a commonly used anesthetic, can impair the morphology of the ABR waveform in a dose-dependent manner in rodents.
Investigations, mainly conducted in rats, have shown that dose and duration of this volatile anesthetic can induce inconsistent changes in latency and amplitude of the ABR (Santarelli et al., 2003; Bielefeld, 2014). Comparison between ABR measures obtained under isoflurane and those obtained under ketamine/xylazine anesthesia has revealed increased ABR thresholds under isoflurane with concentration-dependent effects (Ruebhausen et al., 2012). Similarly, isoflurane dose-dependently reduced the amplitude and increased the latency of the ABR in guinea pigs (Stronks et al., 2010). More recently, isoflurane has been shown to significantly reduce DPOAE amplitudes compared to ketamine/xylazine, and to increase variability of DPOAE responses (Sheppard et al., 2018).
Additional attention must be paid to the use of anesthesia when anesthesia is administered during noise exposure, as anesthesia can modify noise injury (Rubinstein and Pluznik, 1976). A protective effect of chemical or volatile anesthetics administered during noise exposure has been shown in other rodent species (Kim et al., 2005; Chung et al., 2007). These protective effects could be explained by intrinsic properties of anesthetics and the involvement of stress processes in awake animals. When xylazine alone or ketamine together with xylazine were used as anesthesia during noise exposure, TTS was reduced compared to that in awake animals (Giraudet et al., 2002). At least for the ketamine plus xylazine anesthetic protocol, this may be related to ketamine's action as an N-methyl-D-aspartic acid (NMDA) receptor antagonist, which could reduce both glutamate excitotoxicity and sympathetic activity (Giraudet et al., 2002). Xylazine blocks noradrenaline release from the sympathetic system through its actions as a pre-synaptic alpha2-adrenoreceptor agonist and thus mediates the protective effects through other mechanisms (Giraudet et al., 2002). There is also a protective effect of propofol against NIHL and hair cell loss induced by noise (Wen et al., 2017). In addition, the use of gas during noise exposure of animals, for example, when using isoflurane anesthesia, reduces NIHL, at least in mice (Kim et al., 2005; Chung et al., 2007).
Administration of general anesthesia to the guinea pig can be difficult since they often maintain their pedal reflex; some oversight committees may recommend or require monitoring of heart rate or other physiological measures during periods of anesthesia.
V. USE OF THE GUINEA PIG IN AUDITORY RESEARCH
Guinea pigs were commonly used in early studies assessing the normal structure and function of the cochlea and auditory pathways. Based on the wealth of information from such early studies, they have also been highly utilized in studies of the pathological auditory system, after damage induced by noise exposure, ototoxic drug treatment, or other insults including aging. Interestingly, one of the experiments investigating early “rate” and “place” theories of hearing was actually a noise exposure study using guinea pigs as subjects and noise exposure at different intensities. The results were interpreted as suggesting that more intense exposure resulted in wider regions of damage, with damage centered at a specific place along the basilar membrane corresponding to the pitch of the exposure tone (Upton, 1929). Additional related studies using guinea pigs as a model further clarified place-based tonotopic cochlear stimulation using stimuli that varied in both frequency and level, in combination with sound evoked potential measurements collected in both the base and the apex (Tasaki et al., 1952; Suga et al., 1967). The remainder of this section provides a brief overview of historic major findings regarding normal structure and function, providing context for pathologies described and discussed below.
A. Outer hair cell (OHC) research
The guinea pig has commonly been used in efforts to understand the active electromotile expansion and contraction of OHCs in response to voltage change (Dallos, 1985; for discussion see Kakehata et al., 2000). Detailed reviews of the OHC active process are available for interested readers (Brownell, 1990; Manley, 2001; Hudspeth, 2008; Reichenbach and Hudspeth, 2014; Goutman et al., 2015; Brownell, 2017); in brief, this active process provides approximately 40-dB of threshold gain, increasing the sensitivity for detection of acoustic signals. The phenomena of OHC electromotility was first identified in OHCs dissected from the guinea pig cochlea (Brownell, 1984; Brownell et al., 1985; Rabbitt et al., 2005; Hakizimana et al., 2012). Subsequent in vitro manipulation of isolated OHCs has allowed in-depth insight into the biochemistry and biomechanics of OHC electromotility (Dallos and Evans, 1995; Gitter and Zenner, 1995; Sziklai et al., 1996; Dallos et al., 1997; Lue and Brownell, 1999; Frolenkov et al., 2000; Sziklai et al., 2001; Szonyi et al., 2001; He et al., 2003; Zhang et al., 2003; Matsumoto et al., 2010; Park and Kalinec, 2015). Additional in vivo investigation of OHC electromotility that builds on this substantive in vitro body of work has largely been completed using the guinea pig as a model (Nuttall and Ren, 1995; Nilsen and Russell, 1999; Nuttall et al., 1999; Grosh et al., 2004). The DPOAE tests discussed above provide a highly specific objective tool for quickly and easily measuring the overall integrity of the OHC active process using non-invasive in vivo procedures that do not require direct access to the cochlea.
B. Auditory nerve research
Some of the earliest efforts to understand the neural innervation of the cochlea were completed in guinea pig (Fernandez, 1951; Tsuji and Liberman, 1997), including early investigations of spontaneous and sound-evoked auditory nerve discharge (Tasaki, 1954) and adaptation (Sorensen, 1959). Noise exposure paradigms have served as a helpful tool for probing the contributions of the OHC active process to auditory nerve tuning (Cody, 1992). Although use of the guinea pig in early auditory nerve research was significant, extensive parallel activities using the cat as a model must also be noted (Gerstein and Kiang, 1960; Kiang and Peake, 1960; Kiang et al., 1962; Peake and Kiang, 1962; Rodieck et al., 1962; Kiang et al., 1967; Sachs and Kiang, 1968). A number of later studies provided insight into the coding of speech-like sounds at the level of the auditory nerve in both guinea pig (Palmer et al., 1986; Palmer, 1990; Steadman and Sumner, 2018) and cat (Kiang, 1980; Delgutte and Kiang, 1984d; 1984c; 1984b; 1984a; Le Prell et al., 1996; May et al., 1996). The effects of noise on the auditory nerve and its response properties are also described in detail in both guinea pig (Thomsen and Pakkenberg, 1962; Pakkenberg and Thomsen, 1964; Hallen et al., 1965; Brown and Abbas, 1987) and cat (Kiang et al., 1970; Kiang et al., 1976; Liberman and Kiang, 1978; 1984; Pettigrew et al., 1984; Bruce et al., 2003). This extensive literature provides guidance and insight into study design for use in otoprotection research.
Auditory nerve recordings in guinea pigs have recently been used in an effort to understand the coding of high-frequency spectral notches that importantly contribute to sound localization (Alves-Pinto et al., 2014). In other recent work, auditory nerve response measurements in the guinea pig have been used to identify the increased vulnerability of nerve fibers that have low and medium spontaneous rates of firing (Furman et al., 2013), findings that have significant implications regarding the potential for deficits in the processing of supra-threshold signals (Kujawa and Liberman, 2015; Liberman and Kujawa, 2017; Kujawa and Liberman, 2019). With the wealth of data on auditory nerve response in the guinea pig, they are an ideal model with which to probe the earliest effects of noise on the inner ear, as well protection of neural function using otoprotective agents.
C. Auditory evoked potentials
Much of our understanding of the brainstem generators of the ABR came from studies completed in guinea pigs (Gardi and Bledsoe, 1981; Wada and Starr, 1983a; 1983c; 1983b; Harrison and Palmer, 1984; Palmer and Harrison, 1984) although parallel work in cat again closely followed (Jewett, 1970; Buchwald and Huang, 1975; Fullerton et al., 1987; Fullerton and Kiang, 1990; Melcher et al., 1996a; Melcher and Kiang, 1996; Melcher et al., 1996b). Binaural interaction components within the ABR have been investigated in guinea pigs (Dum et al., 1981; Gardi and Berlin, 1981; Wilson et al., 1985; Ozdamar et al., 1986); binaural processing is critical to accurate localization of sound and can be compromised by noise injury. Differences between species are driven by factors such as the size of the brain stem nuclei and lengths of the connecting fiber tracts, but the overall physiology and response properties appear to be well correlated across species (Huang, 1980). As noted above, the ABR is the current gold standard used to measure the functional effects of noise on the inner ear, and there is no reason to assume it will not continue to be heavily utilized in guinea pigs and across laboratory animal models.
D. Neurochemistry research
Because the cochlea and round window are easy to access in the guinea pig, they have also been popular for use in studies employing round window based drug delivery and perilymph sampling for the purposes of measurement of neurotransmitters, neuromodulators, and the movement of chemical ions during transduction. A number of detailed reviews that discuss data collected across species are already available (Bledsoe et al., 1988; Eybalin, 1993; Puel, 1995; Le Prell et al., 2001). It should be noted that much of the early work establishing glutamate (Glu) as the putative excitatory transmitter was completed in guinea pigs (Bobbin and Thompson, 1978; Bobbin, 1979; Bledsoe et al., 1981; Jenison and Bobbin, 1985; Littman et al., 1989). Detailed review and discussion of the Glu receptors located in the cochlea and the pathology observed during activation of these receptors are available [see Le Prell et al. (2001), Ruel et al. (2007), and Takago and Oshima-Takago (2018)] and this early work is highly relevant to the effects of noise on the inner ear given that noise-induced excitotoxicity has been a target in some otoprotection research (Yamasoba et al., 2005). Much of the early work on adenosine triphosphate (ATP) as a neuromodulator was also completed within the guinea pig cochlea (Skellett et al., 1997; Chen et al., 1998). More recent investigations in guinea pigs have now revealed the importance of P2X receptors (Sueta et al., 2003; Thorne et al., 2004; Yu and Zhao, 2008; Zhu and Zhao, 2012), and noise-induced changes in the receptor subunit distribution have been described (Szucs et al., 2006). Chemical changes in the cochlea subsequent to noise exposure are not fully understood, and additional research is needed.
E. Olivocochlear efferent neuroanatomy and neurochemistry
Much of the work that established the ultrastructure (Satake and Liberman, 1996) and neurochemistry of the medial (MOC) and lateral (LOC) olivocochlear efferent systems was completed in guinea pigs, although the rat must also be acknowledged (White and Warr, 1983; Faye-Lund, 1986; Vetter et al., 1991; Vetter and Mugnaini, 1992; Warr et al., 1997). Transmitters investigated in the guinea pig model include acetylcholine (ACh), calcitonin-gene related peptide (CGRP), dopamine (DA), dynorphin (dyn), enkephalin (enk), and gamma-aminobutyric acid (GABA) [for detailed reviews and discussion see Eybalin (1993), Puel (1995), Le Prell et al. (2001), Ruel et al. (2007), and Wersinger and Fuchs (2011)]. Studies assessing the functional consequences of efferent stimulation have significantly relied on guinea pig as a model (Sridhar et al., 1995; Kujawa and Liberman, 2001), and several investigations suggest a stronger MOC system is associated with decreased vulnerability to noise injury (Liberman and Gao, 1995; Reiter and Liberman, 1995; Maison and Liberman, 2000). More recent data extending insight into the LOC system continue to emerge from studies employing lesions of the LOC pathway (Le Prell et al., 2003; Le Prell et al., 2005; Le Prell et al., 2014a), electrical stimulation of the LOC system (Groff and Liberman, 2003), and neurochemical manipulation of the guinea pig cochlea (Garrett et al., 2011; Lendvai et al., 2011; Le Prell et al., 2014b; Wang et al., 2014). The role of the MOC and LOC transmitter systems in mediating vulnerability to noise injury are not fully understood, but the guinea pig is an ideal model for continued research efforts given the wealth of information about these pathways in the guinea pig model.
F. Noise conditioning
Noise does not always cause trauma; there is a phenomena in which exposure to lower level noise can prevent later damage that occurs during a subsequent exposure to louder, more hazardous sound. This conditioning, or toughening, phenomena has been well investigated in the guinea pig, and is evident across species [for review see Niu and Canlon (2002)]. Data collected in the guinea pig model indicate that conditioning may mediate vulnerability by changing the OHC cellular cytoskeleton protein composition (Zuo et al., 2008) and presynaptic vesicle content (Canlon et al., 1993). However, other data in this animal model have shown upregulation of bcl-2 in the OHCs (Niu et al., 2003), decreased levels of systemic malondialdehyde (suggesting decreased metabolic stress) (Liu et al., 2000), and an upregulation in tyrosine hydroxylase positive neurons in the lateral superior olive (LSO) and dorsolateral periolivary nuclei (Niu et al., 2004), suggesting other potential mechanisms of conditioning mediated protection. Other data have implicated the MOC system, based on conditioning induced changes in MOC neuron firing rates (Brown et al., 1998) and protection of the MOC terminals (Canlon et al., 1999).
Increases in DPOAE amplitude post-conditioning appear to be fairly consistent, whereas the direction of change in MOC reflex strength post-conditioning has varied across studies (Canlon and Fransson, 1995; Kujawa and Liberman, 1999; Peng et al., 2007). Interestingly, when the MOC system is lesioned using strychnine, conditioning still confers protection, suggesting the MOC system is not necessary for conditioning (Yamasoba et al., 1999a). Given mixed evidence for MOC effects with surgical transection of the efferent bundle (Kujawa and Liberman, 1997), it may be the case that the completeness of the lesion and method of lesion influence conditioning outcomes.
In some cases, conditioning is highly specific with respect to frequency, with protection observed when the conditioning stimulus and traumatic stimulus are at the same frequency, but no protection when there is a mismatch between the stimulus frequencies (Pourbakht and Imani, 2012). The temporal pattern of the noise matters as well, with intermittent conditioning noise suggested to be more effective than continuous exposure to the conditioning noise (Skellett et al., 1998). In addition, longer post-conditioning delays reduce the effectiveness of the conditioning exposure (Canlon and Fransson, 1998). This continues to be an active research area. In an interesting recent investigation, for example, it was reported that gentamicin conditioning could be used in place of noise conditioning in order to toughen the ear and reduce vulnerability to noise injury (Strose et al., 2014).
G. Perilymph sampling
Early efforts to sample cochlear perilymph in the guinea pig revealed a significant increase in potassium (K+) and chloride (Cl−) concentrations, and a decrease in sodium (Na+) concentration, in noise exposed animals compared to control animals; this was interpreted as reflecting a change in the permeability of the barrier separating endolymph-filled and perilymph-filled compartments (Konishi et al., 1979). Since then, new protocols for perilymph sampling have been developed (Salt et al., 2006; Salt and Plontke, 2009). These new protocols have allowed the kinetics of drug movement within perilymph to be carefully investigated, with the guinea pig as the primary model, allowing new insights into the exchange of fluids across the cochlear aqueduct (Hunter et al., 2003; Mynatt et al., 2006; Plontke et al., 2008; Salt et al., 2012; Salt et al., 2015; Salt et al., 2016). In addition, the movement of systemically injected drugs into the cochlea has also become possible to quantify using this guinea pig model (Pierre et al., 2009; Hahn et al., 2013; Hellberg et al., 2013).
VI. THE DAMAGED AUDITORY SYSTEM
Early investigations providing detailed insight into specific noise-induced histopathological changes in the guinea pig cochlea after noise exposure revealed damage to hair cells, supporting cells (including phalangeal cells and Deiters' cells), Reissner's membrane, and the reticular lamina (Covell et al., 1957). As reviewed below, the guinea pig has continued to be a primary model of interest ever since, not only for studies on noise injury, but also for studies assessing DIHL, ARHL, and prevention of acquired sensorineural hearing loss subsequent to these diverse injuries.
A. Noise-induced hearing loss (NIHL)
Different noise paradigms have been used to induce NIHL in guinea pigs, with noise exposures differing in the frequency spectrum, intensity, duration, and chronicity (single or repeated exposure) (see Table II). Different types of noise have been used as traumatic insults in studies assessing otoprotective effects of pharmacological treatment [impulse noise, see Bielefeld et al. (2019); octave band noise, see Gittleman et al. (2019); blast, see Zhang (2019)]. Although some noise exposures are intended to mimic real-world exposure, such as impulse noise trauma intended to correspond to gunshot exposure affecting the military population, there are typically differences in impulse duration and frequency spectrum that decrease real-world relevance of the laboratory-generated signals.
TABLE II.
A variety of noise exposure models used in the Guinea pig; for comprehensive systematic review of exposures used in otoprotection research see Hammill (2017). M: male; F: female; ND: Not Discussed; ket: ketamine; xyl: xylazine; ace: acepromazine; med: medetomidine; pent: pentobarbitol; CAP: compound action potential; DPOAE: distortion product otoacoustic emission.
| Strain | Sex | Sedation/anesthesia | Noise | Intensity (dB SPL) | Duration | Final test time | Test metric | Anatomical metrics | Author |
|---|---|---|---|---|---|---|---|---|---|
| Pigmented | ND | ND | blank shots from FAMAS F1 rifle | 170 peak SPL | 3 shots | 14 days | CAP threshold | Hair cell counts | Sendowski et al. (2006a) |
| Hartley | F | “lightly anesthetized” | blank shots from FAMAS F1 rifle | 170 or 176 peak SPL | 3 shots | 14 days | CAP threshold | Hair cell counts | Sendowski et al. (2006b) |
| Pigmented | F | None (awake) | impulse noise (20 Hz to 6 kHz) | 114 | 2 or 5 h | 30 days | ABR threshold | ND | Franzé et al. (2003) |
| Pigmented | ND | None (awake) | repeated impulse noise | 165 | 60 impulses | 4 weeks | ABR threshold | Hair cell counts | Zhou et al. (2009) |
| Albino | ND | ND | 2 kHz pure tone | 120 or 125 | 10 min | 7 days | CAP threshold; DPOAE amplitude | ND | Tabuchi et al. (2005) |
| Hartley | F | ket: 60 mg/kg | 6 kHz pure tone | 120 | 0.5 h | 7 days | CAP threshold | Hair cell counts | Fetoni et al. (2009b) |
| xyl: 2 mg/kg | |||||||||
| ace: 0.2 mg/kg | |||||||||
| Pigmented | ND | Pent: dose not provided | 6 kHz pure tone | 120 | 0.5 h | 7 days | CAP threshold and amplitude | Hair cell counts | Wang et al. (2003b) |
| Hartley | ND | ket: 25 mg/kg | 6 kHz pure tone | 120 | 1 h | 21 days | ABR threshold | Hair cell counts | Fetoni et al. (2010) |
| xyl: 5 mg/kg | |||||||||
| ace: 1.5 mg/kg | |||||||||
| Hartley | ND | ket: 25 mg/kg | 6 kHz pure tone | 120 | 1 h | 21 days | ABR threshold | Hair cell counts | Fetoni et al. (2011) |
| xyl: 5 mg/kg | |||||||||
| ace: 1.5 mg/kg | |||||||||
| Hartley | ND | “General anesthesia” | 6 kHz pure tone | 130 | 15 min | 7 days | ABR threshold | Hair cell counts | Tona et al. (2014) |
| Hartley | ND | pent: 33 mg/kg | center frequency of 4 kHz; bandwidth ND | 130 | 3 h | 14 days | ABR threshold | Hair cell counts | Takemoto et al. (2004) |
| Hartley | M and F | None (awake) | narrow band noise centered at 2.5--3.5 kHz | 130 | 1h | 14 days | ABR threshold; DPOAE amplitude | Hair cell counts | Chen et al. (2014) |
| Pigmented | M and F | ket: 40 mg/kg | one-third octave band noise centered at 6.3 kHz | 110 | 1 h | 7 days | ABR threshold | ND | Chen et al. (2003) |
| xyl: 4 mg/kg | |||||||||
| Pigmented | M | None (awake) | Octave band centered at 4 kHz | 100 | 8 h/day for 3 days | 8 days | ABR threshold | Hair cell counts | Hou et al. (2003) |
| Hartley | F | ket: 40 mg/kg | Octave band centered at 4 kHz | 105 or 110 | 2h | 10 days | ABR threshold | ND | Harrop-Jones et al. (2016) |
| xyl: 10 mg/kg | |||||||||
| ace: 0.75 mg/kg | |||||||||
| Hartley | ND | med: 1 mg/kg | Octave band centered at 4 kHz | 110 | 3h | 14 days | ABR threshold | Hair cell counts; synaptic ribbon density | Kanagawa et al. (2014) |
| xyl: 2 mg/kg | |||||||||
| pent: 24 mg/kg | |||||||||
| Pigmented | M | None (awake) | Octave band centered at 4 kHz | 110 | 4h | 7 days | CAP threshold | Hair cell counts | Le Prell et al. (2011a) |
| Hartley | M and F | ND | Octave band centered at 4 kHz | 114 | 6 h | 21 days | ABR threshold | Hair cell counts | McFadden et al. (2005) |
| Hartley | M | None (awake) | Octave band centered at 4 kHz | 115 | 3 h | 7 days | ABR threshold | Auditory nerve dendrite swelling | Yamasoba et al. (2005) |
| Pigmented | ND | None (awake) | Octave band centered at 4 kHz | 115 | 5 h | 7 days | ABR threshold | Hair cell counts | Shoji et al. (2000a) |
| Pigmented | ND | None (awake) | Octave band centered at 4 kHz | 115 | 5 h | 7 days | ABR threshold | Hair cell counts | Shoji et al. (2000b) |
| Hartley | F | None (awake) | Octave band centered at 4 kHz | 115 | 5 h | 10 days | ABR threshold | Hair cell counts | Ohinata et al. (2000) |
| Hartley | F | None (awake) | Octave band centered at 4 kHz | 117 | 24 h | 7 days | ABR threshold | Hair cell counts | Shibata et al. (2007) |
| Pigmented | F | None (awake) | white noise (20 Hz to 8 kHz) | 120 | 2 or 5 h | 30 days | ABR threshold | ND | Franzé et al. (2003) |
| Hartley | M | ND | Octave band centered at 4 kHz | 120 | 3 h | 21 days | ABR threshold | Hair cell counts | Inaoka et al. (2009) |
| Pigmented | M | ND | Octave band centered at 4 kHz | 120 | 5 h | 10 days | ABR threshold | Hair cell counts | Minami et al. (2007) |
| Pigmented | M | None (awake) | Octave band centered at 4 kHz | 120 | 5 h | 10 days | ABR threshold | Hair cell counts | Yamashita et al. (2005) |
| Hartley | F | None (awake) | Octave band centered at 4 kHz | 125 | 5 h | 14 days | ABR threshold | Hair cell counts | Pourbakht and Yamasoba (2003) |
| Pigmented | M | None (awake) | Octave band centered at 4 kHz | 120 | 5h | 10 days | ABR threshold | Hair cell counts | Le Prell et al. (2007a) |
| Hartley | M | None (awake) | Octave band centered at 4 kHz | 120 | 6h | 15 days | ABR threshold | ND | Mohammadian et al. (2017) |
| Hartley | M | None (awake) | Octave band centered at 4 kHz | 120 | 24 h | 7 days | ABR threshold | Hair cell counts | Takemura et al. (2004) |
| Hartley | ND | med: 1 mg/kg | Octave band centered at 4 kHz | 130 | 3h | 7 days | ABR threshold | Hair cell counts; synaptic ribbon density | Kanagawa et al. (2014) |
| xyl: 2 mg/kg | |||||||||
| pent: 24 mg/kg | |||||||||
| Hartley | M | Pent: 33 mg/kg | Octave band centered at 4 kHz | 130 | 3 h | 7 days | ABR threshold | Hair cell counts | Mikuriya et al. (2005) |
| Pigmented | F | None (awake) | broadband noise | 102 | 3 h/day for 5 days | 3 weeks | ABR threshold | Hair cell counts | Yamasoba et al. (1998) |
| Hartley | M | ND | broadband (white) noise (.125-15 kHz) | 105 ± 2 | 10 min | 7 days | ABR threshold | NA; enzyme analyses completed | Cheng et al. (2008) |
| Hartley | ND | None (awake) | broadband (white) noise (.125-15 kHz) | 105 | 6h | 14 days | ABR threshold | ND | Lo et al. (2013) |
| Pigmented | M and F | ND | broadband noise (8-16 kHz) | 115 | 3h | 21 days | CAP threshold | Hair cell counts; spiral ganglion counts | Landegger et al. (2016) |
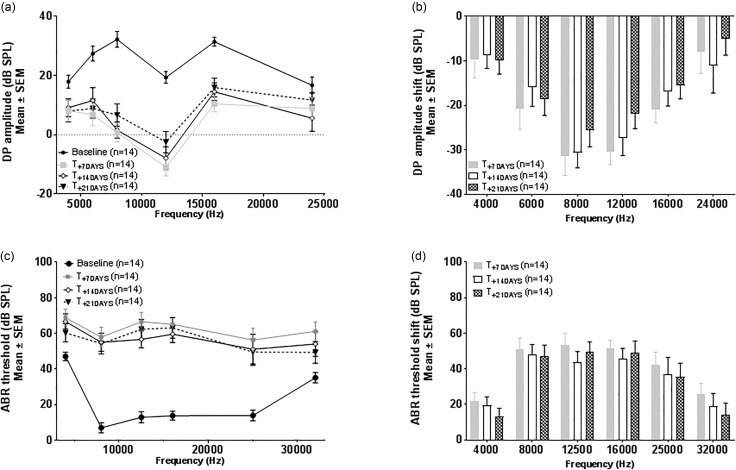
Depending on the intensity and duration of the sound exposure, either a transient TTS or a lasting PTS will result [for review see Ryan et al. (2016)]. Threshold shifts that recover to baseline in the hours, days or weeks following exposure are termed TTS, whereas PTS is hearing loss that does not recover to pre-exposure levels. After some noise exposures, a compound threshold shift (CTS) is observed, including a large TTS which only partially recovers, such that a smaller PTS remains at the end of the recovery window. In addition, repeated exposures to noise that initially induce only a TTS may induce PTS subsequent to later exposures to the same noise stimulus (Wang and Ren, 2012). In animal models, the recovery window has sometimes extended up to 3 weeks and thus it may not be possible to fully distinguish TTS and PTS in animal models until a minimum of 3 weeks post-exposure [for review see Ryan et al. (2016)]. As an example, baseline and shift data measured using DPOAEs and ABRs are provided in Fig. 3. In this NIHL paradigm, guinea pigs were exposed to 115 dB sound pressure level (SPL) noise (1/3 octave band centered at 8 kHz) for 45 min, with PTS showing little recovery across a three week post-noise recovery window.
FIG. 3.
Distortion Product Otoacoustic Emission (DPOAE) amplitude (3 A) and Auditory Brainstem Response (ABR) threshold (3 C) were measured bilaterally in seven young adult Hartley albino guinea pigs before and 7, 14, and 21 days after noise exposure; changes in DPOAE amplitude (3B) and ABR threshold (3 D) were calculated as shift from baseline at each post-noise time. Noise exposure was 115 dB SPL for a 1/3 octave noise band centered at 8 kHz; exposures were 45 min in duration and applied under anesthesia. All data are mean ± standard error of the mean (SEM). This noise exposure induces a rapid decrease of DPOAE amplitudes [(a) and (b)] and increase of ABR thresholds [(c) and (d)], which are still present 21 days post-noise, with the greatest noise injury at frequencies at and within one octave above the exposure frequency of 8 kHz. (Unpublished data collected at CILcare.)
Young (2-month-old) albino guinea pigs appear to be more vulnerable to noise injury than young pigmented control animals (Conlee et al., 1986). The decreased vulnerability of pigmented animals was attributed to the finding that stria vascularis in the pigmented guinea pig cochlea contains melanocytes that produce melanin with otoprotective effect. Protection of the pigmented guinea pigs was similarly observed following impulse noise (Xiong et al., 2011). However, this protection did not extend to ARHL as pigmented guinea pigs had greater ARHL than albino animals at the age of 14-months old. When these 14-month old animals were exposed to noise, threshold shifts displayed by the pigmented animals (with poorer baseline hearing) were smaller than those of the albino animals, presumably because the pigmented animals had already lost cells during the aging process and these could not be lost again when exposed to noise (Conlee et al., 1988).
Noise exposure induces the development of reactive oxygen species (ROS), as well as stress pathway signaling and apoptosis, commonly resulting in OHC loss [for review see Le Prell et al. (2007b), Abi-Hachem et al. (2010), and Poirrier et al. (2010)]. Noise exposure can also damage the synaptic connections between the IHCs and the primary afferent neurons, a pathology termed cochlear synaptopathy [for review see Kujawa and Liberman (2015)]. The phenomenon of noise-induced cochlear synaptopathy has now been demonstrated in several species and there is significant interest in the extent to which this pathology is present in the human inner ear [for recent review and discussion, see Bramhall et al. (2019) and Le Prell (2019)]. Although the majority of research has used mouse as a model [see Kujawa and Liberman (2015) and Liberman and Kujawa (2017)], the guinea pig has also now been used in several studies assessing the potential for cochlear synaptopathy (Lin et al., 2011; Liu et al., 2012; Furman et al., 2013; Song et al., 2016). One of the important advances in understanding of the loss of synapses after noise exposure was the documentation of a decrease in the proportion of low and medium spontaneous rate fibers in guinea pigs exposed to noise that induced a TTS (Furman et al., 2013). Given interest in therapeutics for amelioration of such injuries (Wan et al., 2014; Wan and Corfas, 2015; Suzuki et al., 2016), it seems reasonable to predict that additional work in guinea pig will continue to emerge. One of the major emerging issues in synaptic regeneration research, however, is the unexpected finding of recovery of the synaptic ribbons over a one-month period following noise exposure in the guinea pig (Liu et al., 2012; Shi et al., 2013), a finding that has not been observed in mouse models. As discussed by Liberman and Kujawa (2017), additional research will be necessary to reconcile the differences in results across studies.
B. Effects of noise on cochlear blood flow
The cochlea is highly vascularized, and noise exposure constricts blood vessel diameter and decreases the velocity of cochlear blood flow [e.g., Perlman and Kimura (1962), Axelsson and Dengerink (1987), Thorne and Nuttall (1987), Meyer et al. (1991), Quirk et al. (1991), and Quirk et al. (1992)]. These effects appear to be both frequency and level dependent (Okamoto et al., 1992; Scheibe et al., 1993). Although cochlear blood flow is now well known to be decreased as a consequence of noise exposure [for reviews, see Axelsson and Dengerink (1987), Quirk and Seidman (1995), and Nuttall (1999)], recent data from blast exposed animals contrast in that an increase in cochlear blood flow was detected after blast (Chen et al., 2013). The decreases in cochlear blood flow observed during and after short-term noise (i.e., exposures lasting minutes to hours) can be prevented by vasodilating agents such as dilazep dihydrochloride (Okamoto et al., 1990) or magnesium (Haupt and Scheibe, 2002); drugs that decrease blood viscosity, such as penoxifylline (Coleman et al., 1990; Latoni et al., 1996); or, the angiotensin receptor antagonist Sarthran (Goldwin et al., 1998). Nitric oxide has been broadly implicated in cochlear blood flow and homeostasis [for review see Fessenden and Schacht (1998)]. Inhibition of nitric oxide using the nitric oxide synthase inhibitor N-nitro-L-arginine-methyl ester (L-NAME) attenuates noise induced decreases in cochlear blood flow (Ren et al., 1997). Interestingly, L-NAME similarly prevented the blast-induced increase in cochlear blood flow (Chen et al., 2013). Another potentially effective intervention assessed in the guinea pig model includes inhibition of TNF-alpha using etanercept to preserve cochlear microcirculation in strial capillaries and prevent NIHL (Arpornchayanon et al., 2013). Inhalation of carbogen—a mixture composed of 90%–95% oxygen and 5%–10% carbon dioxide–increases blood vessel diameter and blood flow velocity, and decreased NIHL (Dengerink et al., 1984; Zhao et al., 2012). Another study using 100% oxygen as an additional experimental intervention found 100% oxygen to be even more beneficial than carbogen (Hatch et al., 1991).
C. Age-related hearing loss (ARHL)
Although the focus of this review is noise injury and its prevention, there are changes in vulnerability to noise injury over the course of the lifespan (Kujawa and Liberman, 2006), and it is thus worthwhile to understand the changes in hearing that occur with aging in the guinea pig. Studies conducted in guinea pigs reveal age-related changes in hearing as observed in other mammalian species, with higher frequencies showing threshold elevations prior to the development of deficits at lower frequencies (Ingham et al., 1998a). In addition, more hearing loss is observed in pigmented strains than albino strains (Dum et al., 1980a, 1980b; Dum, 1984). With advancing age in guinea pigs (from 2 to 25 months old), there is a gradual elevation of thresholds [measured using ABR and compound action potential (CAP)] that is accompanied by prolonged ABR latencies for waves I, II, III, and IV, a finding that is generally common across species, including humans. Interestingly, although the ABR waveform amplitudes decreased, response latency (i.e., neural conduction time) associated with the individual potentials remained unchanged between old and young animals in a subset of studies (Dum et al., 1980b; Proctor et al., 1998). Individual differences in threshold elevation and latency prolongation may suggest individual differences in degenerative aging processes of the auditory system (Nozawa et al., 1996; Nozawa et al., 1997).
Age related hair cell loss (Ingham et al., 1999) and changes in microtubules (Saha and Slepecky, 2000) in the guinea pig organ of Corti suggest age-related changes in micromechanical properties of the sensory epithelium. Age-related changes in guinea pig superior colliculus have also been described (Ingham et al., 1998b). In addition, recordings from the primary auditory cortex of pigmented guinea pigs aged from 6 months to 2 years old have demonstrated an age-related “cortical hearing loss” as shown by changes in both threshold and frequency response in the cortex (Gourevitch and Edeline, 2011). Taken together, these data are consistent with the involvement of both peripheral hearing loss and biological aging in the central auditory system in presbycusis. Because the guinea pig has a longer life span than most other rodents, increasing the duration and cost of ARHL studies, the preferred model for studying ARHL has been the mouse, which has the added benefit of many genetically modified strains being available [for review, see Ohlemiller (2006) and Bowl and Dawson (2015)].
D. Drug-induced hearing loss (DIHL)
More than 150 drugs are currently known to be ototoxic. These include aminoglycosides, glycopeptides and macrolide antibiotics, platinum-based anticancer drugs, loop diuretics, quinine, and salicylate analgesics. The effects of ototoxic drugs, such as loop diuretics, macrolide antibiotics, quinine and salicylate, tend to be temporary whereas the effects of other drugs, such as cisplatin and aminoglycoside antibiotics, are generally permanent [for review, see Lanvers-Kaminsky et al. (2017) and Campbell and Le Prell (2018)]. Ototoxic drug and chemical effects can be divided into categories of cochleotoxicity, defined as damage affecting the auditory system resulting in tinnitus and/or sensorineural hearing impairment, and vestibulotoxicity, defined as injury to the vestibular system resulting in dizziness, vertigo, and loss of balance.
Although the focus of this review is noise injury and its prevention, there is tremendous overlap in the mechanisms through which noise and ototoxic drug agents injure the ear, and there is extensive overlap in the protective effects of various drugs in preventing both noise-induced and drug-induced acquired sensorineural hearing loss. Perhaps equally important, however: patients that are prescribed ototoxic medications are often exposed to noise, and there can be synergistic interactions through which the combination of drugs plus noise increase the risk of acquired sensorineural hearing loss. Data from animal models suggest that treatment with cisplatin may result in long-lasting vulnerability to the effects of subsequent noise exposure, suggesting that patients should be counseled to avoid noise exposure during and after treatment with this chemotherapeutic (Gratton et al., 1990; DeBacker et al., 2017). As discussed above for prevention of noise injury, there is tremendous interest in the potential for prevention of DIHL [for review and discussion, see Anderson and Campbell (2015), Laurell and Pierre (2015), Rybak and Brenner (2015), and Hammill and Campbell (2018)].
Several ototoxic drugs have been studied in guinea pigs. Highlighting the importance of nutrition with respect to the vulnerability of the inner ear, the ototoxic side effects of aminoglycosides and cisplatin are increased in animals fed a low-protein diet (Lautermann et al., 1995b; Lautermann and Schacht, 1996). It should be noted that protein intake will be indirectly reduced in animals that are not maintaining sufficient food intake during aminoglycoside or cisplatin therapies; weight loss during such therapies is common, including in guinea pig models (Ekborn et al., 2003; Le Prell et al., 2014c). Nutritional supplements may be necessary, and should be reported in study descriptions when they are used to treat animals in ototoxicity and otoprotection research (Spankovich and Le Prell, 2019).
VII. OTOPROTECTION: PREVENTION OF COCHLEAR INJURY AND HEARING LOSS
The guinea pig has been a preferred model to test new therapies in part due to the ease of delivering drugs into the inner ear. It has also been used in safety studies, to define the best route of administration. The assessment of otoprotective agents has used not only different investigational agents but also different administration routes, dose, and duration of treatment, which has created challenges comparing the relative benefits of different drugs studied in diverse pre-clinical models [for discussion see Le Prell and Miller (2016) and Lynch et al. (2016)]. Both preventive (prophylactic, pre-noise) and curative (rescue, post-noise) effects have been assessed. The rest of this article briefly identifies diverse agents that have been assessed for prevention of NIHL, DIHL, and ARHL in guinea pigs. Efforts to induce regeneration using stem cell and gene therapies are not discussed; readers should see the review by Lee and Park (2018) for an introduction to these approaches.
A. Neuromodulators
Glutamatergic excitotoxicity has been well studied in the guinea pig (Pujol et al., 1993; Puel et al., 1995; Pujol and Puel, 1999) and antagonizing NMDA and/or α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors in the guinea pig cochlea significantly decreases hearing impairment after noise trauma and ototoxins (see Table III). Exposure to noise trauma and ototoxins also affects the viability of sensory hair cells via the MAP kinase (MAPK) cell death signaling pathway that incorporates c-Jun N-terminal kinase (JNK) (Zine and van de Water, 2004). Blocking the MAPK-JNK signal pathway in the guinea pig cochlea also prevents hair cell death and hearing loss induced by noise and ototoxins (see Table III). Caspases mediate kinase cleavage, driving apoptotic cell death (Kurokawa and Kornbluth, 2009). Intracochlear perfusion with caspase- inhibitors prevents hearing loss induced by noise exposure and ototoxins (see Table III). For further details on mechanisms leading to hearing loss see Furness (2015) and Waters (1999).
TABLE III.
Neuromodulators assessed in guinea pig hearing loss models.
| Drugs | Target | Effect | Reference |
|---|---|---|---|
| Glutamate antagonists | |||
| — | Glutamate | Attenuation of noise-induced TTS | Khan et al. (2000) |
| Kynurenate | AMPA | Protective effect on NIHL | Puel et al. (1998) |
| Caroverine | NMDA & AMPA | Reduction of hearing impairment in NIHL | Chen et al. (2003) |
| Chen et al. (2004) | |||
| MK801 | NMDA | Protection in amikacin-induced hearing loss | Duan et al. (2000) |
| Memantine | NMDA | Prevention of toxic damage to hair cells in amikacin-induced hearing loss | Pavlidis et al. (2014) |
| Kinase | |||
| D-JNKI-1 | Blocking of MAPK-JNK signal pathway | Prevention in a dose-dependent manner of hair cell death and permanent hearing loss induced by neomycin after cochlear application | Wang et al. (2003b) see Eshraghi et al. (2007). |
| Prevention of noise-induced permanent hearing loss by a direct cochlear application | Wang et al. (2003b) | ||
| Prevention of hair cell death and PTS induced noise by RWM application | Wang et al. (2007b) | ||
| Caspase inhibitors | |||
| z-DEVD-fmk | caspase-3 | Prevention of cisplatin-induced hearing loss by intracochlear treatment | Wang et al. (2004) |
| z-LEHD-fmk | caspase-9 | ||
| z-VAD-FMK | caspase | Hearing recovery and reduction of hair cell loss after NIHL | Abaamrane et al. (2011) |
| Enzymes | |||
| MDL28170 | gamma-secretase inhibitor | Protective effect on NIHL by direct delivery into the cochlear fluids | Tona et al. (2014) |
| Calpain inhibitors | |||
| BN82270 | calpain | Prevention of hair cell degeneration induced by noise by application in cochlear fluids or onto the RWM | Wang et al. (2007a) |
| leupeptin | calpain | No effect after a gunshot noise-induced trauma by cochlear infusion | Abaamrane et al. (2011) |
| Adrenocorticotrophic Hormone (ACTH) | |||
| ORG 2766 | ACTH analogue | Protection against hair cell loss and hearing loss induced by cisplatin | Hamers et al. (1994); Smoorenburg et al. (1999); Cardinaal et al. (2000) |
B. Anti-inflammatory agents
A common process observed in DIHL, NIHL, and ARHL is cochlear inflammation (Kalinec et al., 2017). Reducing acute inflammation and related processes can be a therapeutic strategy to prevent hearing loss. This strategy has been successful in different hearing loss models in guineas pigs for several anti-inflammatory agents and inhibitors of inflammatory molecules, as listed in Table IV. A detailed review of the contribution of inflammation to NIHL is provided by Frye et al. (2019).
TABLE IV.
Anti-inflammatory agents assessed in guinea pig hearing loss models. DHEA-S: Dehydroepiandrosterone sulfate; TNF: Tumor necrosis factor.
| Drugs | Effect | Reference |
|---|---|---|
| Glucocorticoids | ||
| Dexamethasone (DEX) | Reduction of noise-induced OHC loss and ABR threshold shifts after cochlear delivery | Takemura et al. (2004) |
| Prevention of hearing loss induced by acoustic trauma after application into RW niche | Chi et al. (2011) | |
| Protective effect in NIHL by trans-RWM delivery | Shih et al. (2019) | |
| No hearing recovery of late intratympanic injection (48 h) after a mild noise trauma | Mamelle et al. (2018) | |
| OTO-104 (DEX) | Effective protection against NIHL by transtympanic administration | Harrop-Jones et al. (2016) |
| Methyl-prednisolone | Reduction of hair cell loss in NIHL by cochlear infusion | Sendowski et al. (2006a) |
| Effective protection against NIHL by intratympanic administration | Zhou et al. (2009) | |
| Effective protection against acute noise trauma by RW administration | Muller et al. (2017) | |
| Prednisolone | ||
| DEX | Intratympanic administration in cisplatin-induced ototoxicity in guinea pigs | Daldal et al. (2007); Murphy and Daniel (2011); Shafik et al. (2013) |
| Prevention of cisplatin induced hearing loss | Sun et al. (2015) | |
| OTO-104 (DEX) | Protection against hearing loss induced by both acute and chronic administration of cisplatin | Fernandez et al. (2016) |
| DEX | No protection against cisplatin-induced ototoxicity by systemic delivery | Waissbluth et al. (2013) |
| Protective effects against cisplatin-induced hearing loss by systemic administration | Sun et al. (2016) | |
| Neurosteroids | ||
| DHEA-S | Protective effect against injury of the cochlea induced by noise | Tabuchi et al. (2005) |
| Cytokines | ||
| TNF-α inhibition (etanercept) | Prevention of NIHL by improvement of cochlear blood flow | Arpornchayanon et al. (2013) |
| Prostaglandin E receptor subtype EP4 agonist | Protection of cochleae against NIHL | Hori et al. (2009) |
| Protective effect on cochleae against NIHL | Hori et al. (2013) | |
| Histone deacetylase (HDAC) inhibitor | ||
| Sodium butyrate | Attenuation of gentamicin-induced hearing loss | Wang et al. (2015) |
| Attenuation of noise-induced PTS and OHC loss | Yang et al. (2017) | |
C. Free radical scavengers (anti-oxidants)
The generation of ROS is thought to be part of the mechanism underlying NIHL [for reviews, see Le Prell et al. (2007b) and Le Prell and Bao (2012)]. ROS not removed by antioxidant defenses could be expected to cause significant damage to the sensory cells of the cochlea. Studies over the last decade have left little doubt that ROS also participate in the cellular events leading to aminoglycoside-induced hearing loss (Rybak and Brenner, 2015) and cisplatin induced hearing loss as well (Laurell and Pierre, 2015). A list of anti-oxidant agents studied in the guinea pig are provided in Table V.
TABLE V.
Anti-oxidant agents assessed in guinea pig hearing loss models.
| Drugs | Effect | Reference |
|---|---|---|
| D-Methionine | Prevention of ABR and ATPase activities induced by cisplatin | Cheng et al. (2005) |
| Attenuation of threshold shifts induced by gentamicin | Sha and Schacht (2000) | |
| Reduction of kanamycin-induced ototoxicity | Campbell et al. (2016) | |
| Rescuing noise-induced permanent threshold shift | Lo et al. (2013); Alagic et al. (2011); Cheng et al. (2008) | |
| For further details in several species, against cisplatin-, carboplatin-, aminoglycoside- and noise-induced hearing loss and hair cell loss | see Campbell et al. (2007) | |
| N-Acetylcysteine (NAC) | No protective effect on kanamycin-induced hearing loss, on the contrary, produced a more severe hearing loss and more severe cochlear damage | Bock et al. (1983) |
| Preventive effect on cisplatin ototoxicity by NAC transtympanic administration | Choe et al. (2004) | |
| Otoprotection from cisplatin ototoxicity | Mohan et al. (2014) | |
| Protective effects on noise-induced hearing loss | Fetoni et al. (2009b) | |
| Mitoquinone (MitoQ) | Prevention of ototoxicity induced by cisplatin | Tate et al. (2017) |
| Attenuation of gentamicin-induced cochlear damage and hearing loss | Ojano-Dirain et al. (2014) | |
| Limited protection against amikacin-induced hearing loss and cochlear damage | Dirain et al. (2018) | |
| NG-nitro-L-arginine methyl ester (L-NAME) (iNOS inhibitor) | Reduction of ABR threshold shifts induced by cisplatin | Watanabe et al. (2000) |
| Reduction of noise-induced cochlear damage | Diao et al. (2007); Inai et al. (2012) | |
| Aminoguanidine (iNOS inhibitor) | Prevention of hearing loss induced by gentamicin combined with furosemide | Liu et al. (2008). |
| Glutathione (GSH) | Attenuation of the progression of hearing loss and threshold shift induced by gentamicin, depending on nutritional status | Garetz et al. (1994); Lautermann et al. (1995a) |
| Attenuation of hearing loss by GSH supplementation under low protein diet | Ohinata et al. (2000) | |
| Reduction of NIHL | Yamasoba et al. (1998) | |
| Ebselen (2-phenyl-1,2-benzisoselenazol-3(2H)-one) | Attenuation of noise-induced cochlear damage, by prevention of noise-induced excitotoxicity and threshold shift | Pourbakht and Yamasoba (2003); Yamasoba et al. (2005) |
| Sodium thiosulfate | Chemoprotectant against carboplatin-induced ototoxicity | Neuwelt et al. (1996); Muldoon et al. (2000) |
| Complete prevention of cisplatin-induced hearing loss by local delivery into cochlea or middle ear | Wang et al. (2003a); Stocks et al. (2004); Berglin et al. (2011) | |
| Alpha-tocopherol | Protective effects against gentamicin ototoxicity | Fetoni et al. (2003); Fetoni et al. (2004a) |
| Protective effects against cisplatin ototoxicity | Fetoni et al. (2004b) | |
| Attenuation of noise induced cochlear damage | Hou et al. (2003) | |
| Radical scavengers (Edaravone and Tempol) | Inconsistent effects on aminoglycoside-induced ototoxicity | Song and Schacht (1996) |
| Protection of the cochleae from acoustic trauma | Takemoto et al. (2004) Tanaka et al. (2005) Minami et al. (2007) | |
| Iron chelators | Complete functional and morphological protection from gentamicin ototoxicity | Song and Schacht (1996); Sha and Schacht (1997); Song et al. (1997); Sinswat et al. (2000) |
| Protection against ototoxicity induced by neomycin, kanamycin and streptomycin | Conlon et al. (1998); Song et al. (1998) | |
| Attenuation of NIHL | Yamasoba et al. (1999b) | |
| Salicylate | Reduction of auditory threshold shifts and protection of auditory sensory cells against gentamicin | Sha and Schacht (1999). |
| Protection of the OHC against cisplatin ototoxicity at low doses | Hyppolito et al. (2006) | |
| Allopurinol | Otoprotective effect after noise exposure | Franzé et al. (2003) |
| Idebenone, a coenzyme Q10 analogue | Reduction of threshold shifts, apoptotic activation and hair cell loss induced by noise | Sergi et al. (2006); Fetoni et al. (2008); Fetoni et al. (2009a) |
| Ferulic acid (4-hydroxy 3-methoxycinnamic acid) | Protective effect on PTS in NIHL | Fetoni et al. (2010); Fetoni et al. (2011) |
D. Trophic factors
Neurotrophic factors are secreted peptides that when interacting with specific classes of membrane receptors activate intracellular signaling cascades that prevent neuronal death during embryonic development and enable neurotrophic effects in adult. Brain-derived neurotrophic factor (BDNF) and neurotrophin-3 (NT-3), members of the neurotrophin family of neurotrophic factors that also include nerve growth factor (NGF) and neurotrophin-4/5 (NT-4), are important in development of the neuronal components of the inner ear. Several studies have aimed to assess the protectives effects of neurotrophin members in different models of hearing loss. In addition, other trophic or growth factors have also demonstrated otoprotective effects. The agents in Table VI provide a list of trophic factors assessed in guinea pig models of hearing loss.
TABLE VI.
Trophic and growth factors assessed in guinea pig hearing loss models. GDNF: Glial-derived neurotrophic factor; rhIGF-1: recombinant human insulin-like growth factor 1; HGF: hepatocyte growth factor; bFGF: Basic fibroblast growth factor; G-CSF: Granulocyte colony-stimulating factor.
| Drugs | Effect | Reference |
|---|---|---|
| Neurotrophins | ||
| NT-3 | Prevention of degeneration of spiral ganglion neurons, hearing loss induced by aminoglycosides | Ernfors et al. (1996) |
| Protective effect in a dose dependent manner, enabling OHC survival and a decrease in ABR threshold shift after preventive treatment into the cochlea | Shoji et al. (2000a) | |
| NGF | Protective effects on neomycin-induced auditory nerve degeneration | Shah et al. (1995) |
| BDNF | Prevention of hearing loss induced by cisplatin by intracochlear application | Meen et al. (2009) |
| No protection on hearing and hair cell loss induced by noise after preventive treatment into the cochlea | Shoji et al. (2000a) | |
| BDNF & NT-3 | Reduction of IHC synaptopathy and recovery of high-frequency hearing in in NIHL when delivered together to the RW | Sly et al. (2016). |
| Other trophic factors | ||
| GDNF | Otoprotective effect on hair cells against cisplatin or kanamycin and ethacrynic acid by local delivery—transtympanic injection into the middle ear or infusion into the scala tympani | Kuang et al. (1999). |
| Prevention, in a dose-dependent manner, of cochlear sensory cell damage and hearing loss after acoustic trauma | Keithley et al. (1998); Shoji et al. (2000b). | |
| rhIGF-1 | Attenuation of functional and histologic damage induced by noise in guinea pigs after local application | Lee et al. (2007) |
| HGF | Reduction of ABR threshold shifts and loss of OHC induced by noise after RWM application | Inaoka et al. (2009) |
| bFGF | Protection of the hair cells from acoustic trauma and recovery of hearing by perfusion into the cochlea | Zhai et al. (2002) |
| Protection of auditory neurons and hair cells from glutamate neurotoxicity and noise exposure by intramuscular injection | Zhai et al. (2004) | |
| G-CSF | Attenuation of NIHL by preserving hair cells after intense noise exposure | Shi et al. (2014) |
VIII. CONCLUDING COMMENTS
Stebbins et al. (1982) identified critical challenges in the investigation of the effects of noise on the inner ear as including (1) the use of diverse species across studies, (2) the use of diverse protocols for threshold measurement, (3) the use of diverse noise exposures, many of which do not necessarily model human exposures, and (4) overall lack of consideration of supra-threshold measures of sensitivity. Although they called for greater uniformity and standardization to drive more rapid progress, the systematic review by Hammill (2017) clearly documents that research assessing the effects of noise and potential benefits of different otoprotective agents continues to have tremendous diversity with respect to both species and noise exposure paradigms, with few, if any, efforts to assess supra-threshold measures of sensitivity. As reviewed in this article, there is a wealth of knowledge regarding the guinea pig auditory system, and the guinea pig has become one of the most common models used within noise injury and otoprotection research. The mouse (Ohlemiller, 2019), rat (Escabi et al., 2019; Holt et al., 2019), and chinchilla (Lobarinas et al., 2019; Radziwon et al., 2019) also continue to be commonly used, and new data using nonhuman primates as subjects in noise injury research are also emerging (Burton et al., 2019). Otoprotection research designs have most commonly relied on rodent models, with specific agents typically being assessed in only one or sometimes two rodent species. To facilitate comparisons of efficacy across agents, we encourage a series of new investigations using the guinea pig as a common model based not only on the wealth of normative data from the cochlea to the auditory cortex for this species, but also the wealth of data across diverse octave band noise exposures—the exposure model that has been the most common across otoprotection research investigations (Hammill, 2017; Gittleman et al., 2019). The importance of testing using a common model does not preclude the possibility of research using other models to extend and confirm hypotheses regarding drug effects and mechanisms of action. However, only with the collection of new data using a common species and a common noise insult will we begin to be able to make reliable inferences about the relative efficacy of different agents, and the relative likelihood of success in translation to humans. As part of this effort, it will be critical to collect dose-response data to assure that the “best” (most effective) doses and dose paradigms are able to be compared across studies with otherwise shared design features; with the large number of agents already assessed in the guinea pig, there are rational starting points for dose assessment for many agents. With cooperation to reach consensus on study design, scientific research findings will be better poised to support the translation of promising agents into human clinical testing for prevention of NIHL.
IX. DISCLOSURE
G.N. and M.P. are employed by CILcare, a preclinical provider of pharmacokinetics, preclinical efficacy, and GLP toxicology studies. C.L. has received contract funding from industry sources for clinical trials (Sound Pharmaceuticals, Inc., Edison Pharmaceuticals, Inc., and Hearing Health Science, Inc.) and is grateful for support from the Emilie and Phil Schepps Professorship in Hearing Science. C.L. is currently supported by USAMRAA W81XWH-19-C-0054, JPC-8/SRMRP W81XWH1820014, NIH-NIDCD 1R01DC014088, 3M Inc., and the Emilie and Phil Schepps Professorship in Hearing Science.
ACKNOWLEDGMENTS
The authors thank Dr. Yves Cazals for feedback on an earlier version of this manuscript.
References
- 1. Abaamrane, L. , Raffin, F. , Schmerber, S. , and Sendowski, I. (2011). “ Intracochlear perfusion of leupeptin and z-VAD-FMK: Influence of antiapoptotic agents on gunshot-induced hearing loss,” Eur. Arch. Otorhinolaryngol. 268, 987–993. 10.1007/s00405-011-1487-0 [DOI] [PubMed] [Google Scholar]
- 2. Abi-Hachem, R. N. , Zine, A. , and Van De Water, T. R. (2010). “ The injured cochlea as a target for inflammatory processes, initiation of cell death pathways and application of related otoprotectives strategies,” Recent Pat. CNS Drug Disc. 5, 147–163. 10.2174/157488910791213121 [DOI] [PubMed] [Google Scholar]
- 3.Acoustical Society of America (2004). https://acousticalsociety.org/ethical-principles/ (Last viewed August 28, 2019).
- 4. Agterberg, M. J. , van den Broek, M. , and Philippens, I. H. (2010). “ A less stressful animal model: A conditioned avoidance behaviour task for guineapigs,” Lab. Anim. 44, 206–210. 10.1258/la.2009.009096 [DOI] [PubMed] [Google Scholar]
- 5. Agterberg, M. J. , and Versnel, H. (2014). “ Behavioral responses of deafened guinea pigs to intracochlear electrical stimulation: A new rapid psychophysical procedure,” Hear. Res. 313, 67–74. 10.1016/j.heares.2014.04.011 [DOI] [PubMed] [Google Scholar]
- 6. Alagic, Z. , Goiny, M. , and Canlon, B. (2011). “ Protection against acoustic trauma by direct application of D-methionine to the inner ear,” Acta Otolaryngol. (Stockh). 131, 802–808. 10.3109/00016489.2011.564652 [DOI] [PubMed] [Google Scholar]
- 7. Alves-Pinto, A. , Palmer, A. R. , and Lopez-Poveda, E. A. (2014). “ Perception and coding of high-frequency spectral notches: Potential implications for sound localization,” Front Neurosci. 8, 112. 10.3389/fnins.2014.00112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Anderson, J. M. , and Campbell, K. (2015). “ Assessment of interventions to prevent drug-induced hearing loss,” in Oxidative Stress in Applied Basic Research and Clinical Practice: Free Radicals in ENT Pathology, edited by Miller J. M., Le Prell C. G., and Rybak L. P. ( Humana Press, New York: ), pp. 243–269. [Google Scholar]
- 9. Arpornchayanon, W. , Canis, M. , Ihler, F. , Settevendemie, C. , and Strieth, S. (2013). “ TNF-alpha inhibition using etanercept prevents noise-induced hearing loss by improvement of cochlear blood flow in vivo,” Int. J. Audiol. 52, 545–552. 10.3109/14992027.2013.790564 [DOI] [PubMed] [Google Scholar]
- 10. Axelsson, A. , and Dengerink, H. (1987). “ The effects of noise on histological measures of the cochlear vasculature and red blood cells: A review,” Hear. Res. 31, 183–191. 10.1016/0378-5955(87)90125-0 [DOI] [PubMed] [Google Scholar]
- 11. Berglin, C. E. , Pierre, P. V. , Bramer, T. , Edsman, K. , Ehrsson, H. , Eksborg, S. , and Laurell, G. (2011). “ Prevention of cisplatin-induced hearing loss by administration of a thiosulfate-containing gel to the middle ear in a guinea pig model,” Cancer Chemother. Pharmacol. 68, 1547–1556. 10.1007/s00280-011-1656-2 [DOI] [PubMed] [Google Scholar]
- 12. Berryman, J. C. (1976). “ Guinea-pig vocalizations: Their structure, causation and function,” Z. Tierpsychol. 41, 80–106. 10.1111/j.1439-0310.1976.tb00471.x [DOI] [PubMed] [Google Scholar]
- 13. Bielefeld, E. C. (2014). “ Influence of dose and duration of isoflurane anesthesia on the auditory brainstem response in the rat,” Int. J. Audiol. 53, 250–258. 10.3109/14992027.2013.858280 [DOI] [PubMed] [Google Scholar]
- 14. Bielefeld, E. C. , Harrison, R. T. , and DeBacker, J. R. (2019). “ Pharmaceutical otoprotection strategies to prevent impulse noise-induced hearing loss,” J. Acoust. Soc. Am. 146, 3790–3799. 10.1121/1.5132285 [DOI] [PubMed] [Google Scholar]
- 15. Biesalski, H. K. , Wellner, U. , and Weiser, H. (1990). “ Vitamin A deficiency increases noise susceptibility in guinea pigs,” J. Nutr. 120, 726–737. 10.1093/jn/120.7.726 [DOI] [PubMed] [Google Scholar]
- 16. Bledsoe, S. C., Jr. , Bobbin, R. P. , and Chihal, D. M. (1981). “ Kainic acid: An evaluation of its action on cochlear potentials,” Hear. Res. 4, 109–120. 10.1016/0378-5955(81)90040-X [DOI] [PubMed] [Google Scholar]
- 17. Bledsoe, S. C., Jr. , Bobbin, R. P. , and Puel, J. L. (1988). “ Neurotransmission in the inner ear,” in Physiology of the Ear, edited by Jahn A. F., and Santos-Sacchi J. ( Raven Press, New York: ), pp. 385–406. [Google Scholar]
- 18. Bobbin, R. P. (1979). “ Glutamate and aspartate mimic the afferent transmitter in the cochlea,” Exp. Brain Res. 34, 389–393. 10.1007/BF00235683 [DOI] [PubMed] [Google Scholar]
- 19. Bobbin, R. P. , and Thompson, M. H. (1978). “ Effects of putative transmitters on afferent cochlear transmission,” Ann. Otol. Rhinol. Laryngol. 87, 185–190. 10.1177/000348947808700207 [DOI] [PubMed] [Google Scholar]
- 20. Bock, G. R. , and Steel, K. P. (1984). “ Use of albino animals for auditory research,” Hear. Res. 13, 201–202. 10.1016/0378-5955(84)90109-6 [DOI] [PubMed] [Google Scholar]
- 21. Bock, G. R. , Yates, G. K. , Miller, J. J. , and Moorjani, P. (1983). “ Effects of N-acetylcysteine on kanamycin ototoxicity in the guinea pig,” Hear. Res. 9, 255–262. 10.1016/0378-5955(83)90030-8 [DOI] [PubMed] [Google Scholar]
- 22. Bowl, M. R. , and Dawson, S. J. (2015). “ The mouse as a model for age-related hearing loss—A mini-review,” Gerontology 61, 149–157. 10.1159/000368399 [DOI] [PubMed] [Google Scholar]
- 23. Bramhall, N. , Beach, E. F. , Epp, B. , Le Prell, C. G. , Lopez-Poveda, E. A. , Plack, C. J. , Schaette, R. , Verhulst, S. , and Canlon, B. (2019). “ The search for noise-induced cochlear synaptopathy in humans: Mission impossible?,” Hear. Res. 377, 88–103. 10.1016/j.heares.2019.02.016 [DOI] [PubMed] [Google Scholar]
- 24. Brewer, J. S. , Bellinger, S. A. , Joshi, P. , and Kleven, G. A. (2014). “ Enriched open field facilitates exercise and social interaction in 2 strains of guinea pigs (Cavia porcellus),” J. Am. Assoc. Lab. Anim. Sci.: JAALAS 53, 344–355. [PMC free article] [PubMed] [Google Scholar]
- 25. Brown, C. J. , and Abbas, P. J. (1987). “ A comparison of AP and ABR tuning curves in the guinea pig,” Hear. Res. 25, 193–204. 10.1016/0378-5955(87)90091-8 [DOI] [PubMed] [Google Scholar]
- 26. Brown, M. C. , Kujawa, S. G. , and Liberman, M. C. (1998). “ Single olivocochlear neurons in the guinea pig. II. Response plasticity due to noise conditioning,” J. Neurophysiol. 79, 3088–3097. 10.1152/jn.1998.79.6.3088 [DOI] [PubMed] [Google Scholar]
- 27. Brownell, W. E. (1984). “ Microscopic observation of cochlear hair cell motility,” Scan. Electron Microsc. 3, 1401–1406. [PubMed] [Google Scholar]
- 28. Brownell, W. E. (1990). “ Outer hair cell electromotility and otoacoustic emissions,” Ear Hear. 11, 82–92. 10.1097/00003446-199004000-00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Brownell, W. E. (2017). “ What is electromotility?—The history of its discovery and its relevance to acoustics,” Acoust. Today 13, 20–27. [PMC free article] [PubMed] [Google Scholar]
- 30. Brownell, W. E. , Bader, C. R. , Bertrand, D. , and de Ribaupierre, Y. (1985). “ Evoked mechanical responses of isolated cochlear outer hair cells,” Science 227, 194–196. 10.1126/science.3966153 [DOI] [PubMed] [Google Scholar]
- 31. Bruce, I. C. , Sachs, M. B. , and Young, E. D. (2003). “ An auditory-periphery model of the effects of acoustic trauma on auditory nerve responses,” J. Acoust. Soc. Am. 113, 369–388. 10.1121/1.1519544 [DOI] [PubMed] [Google Scholar]
- 32. Buchwald, J. S. , and Huang, C. (1975). “ Far-field acoustic response: Origins in the cat,” Science 189, 382–384. 10.1126/science.1145206 [DOI] [PubMed] [Google Scholar]
- 33. Burton, J. A. , Valero, M. D. , Hackett, T. A. , and Ramachandran, R. (2019). “ The use of nonhuman primates in studies of noise injury and treatment,” J. Acoust. Soc. Am. 146, 3770–3789. 10.1121/1.5132709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Campbell, K. C. , Martin, S. M. , Meech, R. P. , Hargrove, T. L. , Verhulst, S. J. , and Fox, D. J. (2016). “ D-methionine (D-met) significantly reduces kanamycin-induced ototoxicity in pigmented guinea pigs,” Int. J. Audiol. 55, 273–278. 10.3109/14992027.2016.1143980 [DOI] [PubMed] [Google Scholar]
- 35. Campbell, K. C. , Meech, R. P. , Klemens, J. J. , Gerberi, M. T. , Dyrstad, S. S. , Larsen, D. L. , Mitchell, D. L. , El-Azizi, M. , Verhulst, S. J. , and Hughes, L. F. (2007). “ Prevention of noise- and drug-induced hearing loss with d-methionine,” Hear Res. 226(1–2), 92–103. 10.1016/j.heares.2006.11.012 [DOI] [PubMed] [Google Scholar]
- 36. Campbell, K. C. M. , and Le Prell, C. G. (2018). “ Drug-induced ototoxicity: Diagnosis and monitoring,” Drug Saf. 41, 451–464. 10.1007/s40264-017-0629-8 [DOI] [PubMed] [Google Scholar]
- 37.Canadian Council on Animal Care (1993). “ Guide to the care and use of experimental animals,” Canadian Council on Animal Care (CCAC), Vol. 1-1993.
- 38. Canlon, B. , and Fransson, A. (1995). “ Morphological and functional preservation of the outer hair cells from noise trauma by sound conditioning,” Hear. Res. 84, 112–124. 10.1016/0378-5955(95)00020-5 [DOI] [PubMed] [Google Scholar]
- 39. Canlon, B. , and Fransson, A. (1998). “ Reducing noise damage by using a mid-frequency sound conditioning stimulus,” Neuroreport 9, 269–274. 10.1097/00001756-199801260-00017 [DOI] [PubMed] [Google Scholar]
- 40. Canlon, B. , Fransson, A. , and Viberg, A. (1999). “ Medial olivocochlear efferent terminals are protected by sound conditioning,” Brain Res. 850, 253–260. 10.1016/S0006-8993(99)02091-0 [DOI] [PubMed] [Google Scholar]
- 41. Canlon, B. , Lofstrand, P. , and Borg, E. (1993). “ Ultrastructural changes in the presynaptic region of outer hair cells after acoustic stimulation,” Neurosci. Lett. 150, 103–106. 10.1016/0304-3940(93)90118-5 [DOI] [PubMed] [Google Scholar]
- 42. Cardinaal, R. M. , de Groot, J. C. , Huizing, E. H. , Veldman, J. E. , and Smoorenburg, G. F. (2000). “ Histological effects of co-administration of an ACTH((4-9)) analogue, ORG 2766, on cisplatin ototoxicity in the albino guinea pig,” Hear. Res. 144, 157–167. 10.1016/S0378-5955(00)00061-7 [DOI] [PubMed] [Google Scholar]
- 43. Chatterjee, I. B. , Majumder, A. K. , Nandi, B. K. , and Subramanian, N. (1975). “ Synthesis and some major functions of vitamin C in animals,” Ann. N. Y. Acad. Sci. 258, 24–47. 10.1111/j.1749-6632.1975.tb29266.x [DOI] [PubMed] [Google Scholar]
- 44. Chen, C. , Skellett, R. A. , Fallon, M. , and Bobbin, R. P. (1998). “ Additional pharmacological evidence that endogenous ATP modulates cochlear mechanics,” Hear. Res. 118, 47–61. 10.1016/S0378-5955(98)00019-7 [DOI] [PubMed] [Google Scholar]
- 45. Chen, L. , Yu, N. , Lu, Y. , Wu, L. , Chen, D. , Guo, W. , Zhao, L. , Liu, M. , Yang, S. , Sun, X. , and Zhai, S. (2014). “ Hydrogen-saturated saline protects intensive narrow band noise-induced hearing loss in guinea pigs through an antioxidant effect,” PLoS One 9, e100774. 10.1371/journal.pone.0100774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Chen, W. , Wang, J. , Chen, J. , Chen, J. , and Chen, Z. (2013). “ Relationship between changes in the cochlear blood flow and disorder of hearing function induced by blast injury in guinea pigs,” Int. J. Clin. Exp. Path. 6, 375–384. [PMC free article] [PubMed] [Google Scholar]
- 47. Chen, Z. , Ulfendahl, M. , Ruan, R. , Tan, L. , and Duan, M. (2003). “ Acute treatment of noise trauma with local caroverine application in the guinea pig,” Acta Otolaryngol. 123, 905–909. 10.1080/00016480310000638 [DOI] [PubMed] [Google Scholar]
- 48. Chen, Z. , Ulfendahl, M. , Ruan, R. , Tan, L. , and Duan, M. (2004). “ Protection of auditory function against noise trauma with local caroverine administration in guinea pigs,” Hear. Res. 197, 131–136. 10.1016/j.heares.2004.03.021 [DOI] [PubMed] [Google Scholar]
- 49. Cheng, P. W. , Liu, S. H. , Hsu, C. J. , and Lin-Shiau, S. Y. (2005). “ Correlation of increased activities of Na+, K+-ATPase and Ca2+-ATPase with the reversal of cisplatin ototoxicity induced by D-methionine in guinea pigs,” Hear. Res. 205, 102–109. 10.1016/j.heares.2005.03.008 [DOI] [PubMed] [Google Scholar]
- 50. Cheng, P. W. , Liu, S. H. , Young, Y. H. , Hsu, C. J. , and Lin-Shiau, S. Y. (2008). “ Protection from noise-induced temporary threshold shift by D-methionine is associated with preservation of ATPase activities,” Ear Hear. 29, 65–75. 10.1097/AUD.0b013e31815d635b [DOI] [PubMed] [Google Scholar]
- 51. Chi, F. L. , Yang, M. Q. , Zhou, Y. D. , and Wang, B. (2011). “ Therapeutic efficacy of topical application of dexamethasone to the round window niche after acoustic trauma caused by intensive impulse noise in guinea pigs,” J. Laryngol. Otol. 125, 673–685. 10.1017/S0022215111000028 [DOI] [PubMed] [Google Scholar]
- 52. Choe, W. T. , Chinosornvatana, N. , and Chang, K. W. (2004). “ Prevention of cisplatin ototoxicity using transtympanic N-acetylcysteine and lactate,” Otol. Neurotol. 25, 910–915. 10.1097/00129492-200411000-00009 [DOI] [PubMed] [Google Scholar]
- 53. Chung, J. W. , Ahn, J. H. , Kim, J. Y. , Lee, H. J. , Kang, H. H. , Lee, Y. K. , Kim, J. U. , and Koo, S. W. (2007). “ The effect of isoflurane, halothane and pentobarbital on noise-induced hearing loss in mice,” Anesth. Analg. 104, 1404–1408. 10.1213/01.ane.0000261508.24083.6c [DOI] [PubMed] [Google Scholar]
- 54. Cody, A. R. (1992). “ Acoustic lesions in the mammalian cochlea: Implications for the spatial distribution of the ‘active process,’” Hear. Res. 62, 166–172. 10.1016/0378-5955(92)90182-M [DOI] [PubMed] [Google Scholar]
- 55. Coleman, J. K. , Quirk, W. S. , Dengerink, H. A. , and Wright, J. W. (1990). “ Pentoxifylline increases cochlear blood flow while decreasing blood pressure in guinea pigs,” Hear. Res. 47, 169–174. 10.1016/0378-5955(90)90174-N [DOI] [PubMed] [Google Scholar]
- 56. Conlee, J. W. , Abdul-Baqi, K. J. , McCandless, G. A. , and Creel, D. J. (1986). “ Differential susceptibility to noise-induced permanent threshold shift between albino and pigmented guinea pigs,” Hear. Res. 23, 81–91. 10.1016/0378-5955(86)90177-2 [DOI] [PubMed] [Google Scholar]
- 57. Conlee, J. W. , Abdul-Baqi, K. J. , McCandless, G. A. , and Creel, D. J. (1988). “ Effects of aging on normal hearing loss and noise-induced threshold shift in albino and pigmented guinea pigs,” Acta Otolaryngol. 106, 64–70. 10.3109/00016488809107372 [DOI] [PubMed] [Google Scholar]
- 58. Conlon, B. J. , Perry, B. P. , and Smith, D. W. (1998). “ Attenuation of neomycin ototoxicity by iron chelation,” Laryngoscope 108, 284–287. 10.1097/00005537-199802000-00023 [DOI] [PubMed] [Google Scholar]
- 59. Cousins, R. P. (2019). “ Medicines discovery for auditory disorders: Challenges for industry,” J. Acoust. Soc. Am. 146, 3652–3667. 10.1121/1.5132706 [DOI] [PubMed] [Google Scholar]
- 60. Covell, W. P. , Davis, H. , and Eldredge, D. H. (1957). “ Recovery from acoustic trauma in the guinea pig,” Laryngoscope 67, 66–84. 10.1288/00005537-195701000-00003 [DOI] [PubMed] [Google Scholar]
- 61. Daldal, A. , Odabasi, O. , and Serbetcioglu, B. (2007). “ The protective effect of intratympanic dexamethasone on cisplatin-induced ototoxicity in guinea pigs,” Otolaryngol. Head Neck Surg. 137, 747–752. 10.1016/j.otohns.2007.05.068 [DOI] [PubMed] [Google Scholar]
- 62. Dallos, P. (1985). “ Response characteristics of mammalian cochlear hair cells,” J. Neurosci. 5, 1591–1608. 10.1523/JNEUROSCI.05-06-01591.1985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Dallos, P. , and Evans, B. N. (1995). “ High-frequency motility of outer hair cells and the cochlear amplifier,” Science 267, 2006–2009. 10.1126/science.7701325 [DOI] [PubMed] [Google Scholar]
- 64. Dallos, P. , He, D. Z. , Lin, X. , Sziklai, I. , Mehta, S. , and Evans, B. N. (1997). “ Acetylcholine, outer hair cell electromotility, and the cochlear amplifier,” J. Neurosci. 17, 2212–2226. 10.1523/JNEUROSCI.17-06-02212.1997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Davis, R. R. , Kuo, M. W. , Stanton, S. G. , Canlon, B. , Krieg, E. , and Alagramam, K. N. (2007). “ N-Acetyl L-cysteine does not protect against premature age-related hearing loss in C57BL/6J mice: A pilot study,” Hear. Res. 226, 203–208. 10.1016/j.heares.2006.07.003 [DOI] [PubMed] [Google Scholar]
- 66. DeBacker, J. R. , Harrison, R. T. , and Bielefeld, E. C. (2017). “ Long-term synergistic interaction of cisplatin- and noise-induced hearing losses,” Ear Hear. 38, 282–291. 10.1097/AUD.0000000000000391 [DOI] [PubMed] [Google Scholar]
- 67. Delgutte, B. , and Kiang, N. Y. (1984a). “ Speech coding in the auditory nerve: I. Vowel-like sounds,” J. Acoust. Soc. Am. 75, 866–878. 10.1121/1.390596 [DOI] [PubMed] [Google Scholar]
- 68. Delgutte, B. , and Kiang, N. Y. (1984b). “ Speech coding in the auditory nerve: III. Voiceless fricative consonants,” J. Acoust. Soc. Am. 75, 887–896. 10.1121/1.390598 [DOI] [PubMed] [Google Scholar]
- 69. Delgutte, B. , and Kiang, N. Y. (1984c). “ Speech coding in the auditory nerve: IV. Sounds with consonant-like dynamic characteristics,” J. Acoust. Soc. Am. 75, 897–907. 10.1121/1.390599 [DOI] [PubMed] [Google Scholar]
- 70. Delgutte, B. , and Kiang, N. Y. (1984d). “ Speech coding in the auditory nerve: V. Vowels in background noise,” J. Acoust. Soc. Am. 75, 908–918. 10.1121/1.390537 [DOI] [PubMed] [Google Scholar]
- 71. Dengerink, H. A. , Axelsson, A. , Miller, J. M. , and Wright, J. W. (1984). “ The effect of noise and carbogen on cochlear vasculature,” Acta Otolaryngol. 98, 81–88. 10.3109/00016488409107537 [DOI] [PubMed] [Google Scholar]
- 72. Diao, M. , Gao, W. , and Sun, J. (2007). “ Nitric oxide synthase inhibitor reduces noise-induced cochlear damage in guinea pigs,” Acta Otolaryngol. 127, 1162–1167. 10.1080/00016480701242436 [DOI] [PubMed] [Google Scholar]
- 73. Dirain, C. O. , Ng, M. , Milne-Davies, B. , Joseph, J. K. , and Antonelli, P. J. (2018). “ Evaluation of mitoquinone for protecting against amikacin-induced ototoxicity in guinea pigs,” Otol. Neurotol. 39, 111–118. 10.1097/MAO.0000000000001638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Donnelly, T. M. , and Brown, C. J. (2004). “ Guinea pig and chinchilla care and husbandry,” Vet. Clin. North Am. Exot. Anim. Pract. 7, 351–373. 10.1016/j.cvex.2004.02.006 [DOI] [PubMed] [Google Scholar]
- 75. Duan, M. , Agerman, K. , Ernfors, P. , and Canlon, B. (2000). “ Complementary roles of neurotrophin 3 and a N-methyl-D-aspartate antagonist in the protection of noise and aminoglycoside-induced ototoxicity,” Proc. Natl. Acad. Sci. U.S.A. 97, 7597–7602. 10.1073/pnas.97.13.7597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Dum, N. (1984). “ Postnatal development of the auditory evoked brainstem potentials in the guinea pig,” Acta Otolaryngol. 97, 63–68. 10.3109/00016488409130965 [DOI] [PubMed] [Google Scholar]
- 77. Dum, N. , Schmidt, U. , and von Wedel, H. (1980a). “ Age-dependence of the neural auditory thresholds of albino and pigmented guinea pigs,” Arch. Otorhinolaryngol. 229, 191–199. 10.1007/BF02565521 [DOI] [PubMed] [Google Scholar]
- 78. Dum, N. , Schmidt, U. , and von Wedel, H. (1980b). “ Age-related changes in the auditory evoked brainstem potentials of albino and pigmented guinea pigs,” Arch. Otorhinolaryngol. 228, 249–258. 10.1007/BF00660737 [DOI] [PubMed] [Google Scholar]
- 79. Dum, N. , Schmidt, U. , and von Wedel, H. (1981). “ Scalp distribution of the auditory evoked brainstem potentials in the guinea pig during monaural and binaural stimulation,” Hear. Res. 5, 271–284. 10.1016/0378-5955(81)90051-4 [DOI] [PubMed] [Google Scholar]
- 80. Ekborn, A. , Lindberg, A. , Laurell, G. , Wallin, I. , Eksborg, S. , and Ehrsson, H. (2003). “ Ototoxicity, nephrotoxicity and pharmacokinetics of cisplatin and its monohydrated complex in the guinea pig,” Cancer Chemother. Pharmacol. 51, 36–42. 10.1007/s00280-002-0540-5 [DOI] [PubMed] [Google Scholar]
- 81. Ernfors, P. , Duan, M. L. , ElShamy, W. M. , and Canlon, B. (1996). “ Protection of auditory neurons from aminoglycoside toxicity by neurotrophin-3,” Nat. Med. 2, 463–467. 10.1038/nm0496-463 [DOI] [PubMed] [Google Scholar]
- 82. Escabi, C. D. , Frye, M. , and Lobarinas, E. (2019). “ The rat animal model for noise-induced hearing loss,” J. Acoust. Soc. Am. 146, 3692–3709. 10.1121/1.5132553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Eshraghi, A. A. , Wang, J. , Adil, E. , He, J. , Zine, A. , Bublik, M. , Bonny, C. , Puel, J. L. , Balkany, T. J. , and Van De Water, T. R. (2007). “ Blocking c-Jun-N-terminal kinase signaling can prevent hearing loss induced by both electrode insertion trauma and neomycin ototoxicity,” Hear. Res. 226, 168–177. 10.1016/j.heares.2006.09.008 [DOI] [PubMed] [Google Scholar]
- 84.European Parliament (2010). “ Directive 2010/63/EU of the European Parliament and of the Council of 22 September 2010 on the Protection of Animals used for Scientific Purposes.”
- 85. Evonic, I. N. , and Brimer, C. J. (1967). “ Effect of variable temporal parameters in avoidance conditioning of the guinea pig,” J. Comp. Physiol. Psychol. 63, 536–538. 10.1037/h0024629 [DOI] [PubMed] [Google Scholar]
- 86. Eybalin, M. (1993). “ Neurotransmitters and neuromodulators of the mammalian cochlea,” Physiol. Rev. 73, 309–373. 10.1152/physrev.1993.73.2.309 [DOI] [PubMed] [Google Scholar]
- 87. Faye-Lund, H. (1986). “ Projection from the inferior colliculus to the superior olivary complex in the albino rat,” Anat. Embryol. (Berl). 175, 35–52. 10.1007/BF00315454 [DOI] [PubMed] [Google Scholar]
- 88. Fernandez, C. (1951). “ The innervation of the cochlea (guinea pig),” Laryngoscope 61, 1152–1172. 10.1288/00005537-195112000-00002 [DOI] [PubMed] [Google Scholar]
- 89. Fernandez, R. , Harrop-Jones, A. , Wang, X. , Dellamary, L. , LeBel, C. , and Piu, F. (2016). “ The sustained-exposure dexamethasone formulation OTO-104 offers effective protection against cisplatin-induced hearing loss,” Audiol. Neurootol. 21, 22–29. 10.1159/000441833 [DOI] [PubMed] [Google Scholar]
- 90. Fessenden, J. D. , and Schacht, J. (1998). “ The nitric oxide/cyclic GMP pathway: A potential major regulator of cochlear physiology,” Hear. Res. 118, 168–176. 10.1016/S0378-5955(98)00027-6 [DOI] [PubMed] [Google Scholar]
- 91. Fetoni, A. R. , Eramo, S. , Troiani, D. , and Paludetti, G. (2011). “ Therapeutic window for ferulic acid protection against noise-induced hearing loss in the guinea pig,” Acta Otolaryngol 131, 419–427. 10.3109/00016489.2010.539263 [DOI] [PubMed] [Google Scholar]
- 92. Fetoni, A. R. , Ferraresi, A. , Greca, C. L. , Rizzo, D. , Sergi, B. , Tringali, G. , Piacentini, R. , and Troiani, D. (2008). “ Antioxidant protection against acoustic trauma by coadministration of idebenone and vitamin E,” Neuroreport 19, 277–281. 10.1097/WNR.0b013e3282f50c66 [DOI] [PubMed] [Google Scholar]
- 93. Fetoni, A. R. , Mancuso, C. , Eramo, S. L. , Ralli, M. , Piacentini, R. , Barone, E. , Paludetti, G. , and Troiani, D. (2010). “ In vivo protective effect of ferulic acid against noise-induced hearing loss in the guinea-pig,” Neurosci. 169, 1575–1588. 10.1016/j.neuroscience.2010.06.022 [DOI] [PubMed] [Google Scholar]
- 94. Fetoni, A. R. , Piacentini, R. , Fiorita, A. , Paludetti, G. , and Troiani, D. (2009a). “ Water-soluble Coenzyme Q10 formulation (Q-ter) promotes outer hair cell survival in a guinea pig model of noise induced hearing loss (NIHL),” Brain Res. 1257, 108–116. 10.1016/j.brainres.2008.12.027 [DOI] [PubMed] [Google Scholar]
- 95. Fetoni, A. R. , Ralli, M. , Sergi, B. , Parrilla, C. , Troiani, D. , and Paludetti, G. (2009b). “ Protective effects of N-acetylcysteine on noise-induced hearing loss in guinea pigs,” Acta Otorhinolaryngol. Ital. 29, 70–75. [PMC free article] [PubMed] [Google Scholar]
- 96. Fetoni, A. R. , Sergi, B. , Ferraresi, A. , Paludetti, G. , and Troiani, D. (2004a). “ alpha-Tocopherol protective effects on gentamicin ototoxicity: An experimental study,” Int. J. Audiol. 43, 166–171. 10.1080/14992020400050023 [DOI] [PubMed] [Google Scholar]
- 97. Fetoni, A. R. , Sergi, B. , Ferraresi, A. , Paludetti, G. , and Troiani, D. (2004b). “ Protective effects of alpha-tocopherol and tiopronin against cisplatin-induced ototoxicity,” Acta Otolaryngol. 124, 421–426. 10.1080/00016480410016559 [DOI] [PubMed] [Google Scholar]
- 98. Fetoni, A. R. , Sergi, B. , Scarano, E. , Paludetti, G. , Ferraresi, A. , and Troiani, D. (2003). “ Protective effects of alpha-tocopherol against gentamicin-induced Oto-vestibulo toxicity: An experimental study,” Acta Otolaryngol. 123, 192–197. 10.1080/00016480310001484 [DOI] [PubMed] [Google Scholar]
- 99. Franzé, A. , Sequino, L. , Saulino, C. , Attanasio, G. , and Marciano, E. (2003). “ Effect over time of allopurinol on noise-induced hearing loss in guinea pigs,” Int. J. Audiolol. 42, 227–234. 10.3109/14992020309101318 [DOI] [PubMed] [Google Scholar]
- 100. Frolenkov, G. I. , Mammano, F. , Belyantseva, I. A. , Coling, D. , and Kachar, B. (2000). “ Two distinct Ca(2+)-dependent signaling pathways regulate the motor output of cochlear outer hair cells,” J. Neurosci. 20, 5940–5948. 10.1523/JNEUROSCI.20-16-05940.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Frye, M. D. , Ryan, A. F. , and Kurabi, A. (2019). “ Inflammation associated with noise-induced hearing loss,” J. Acoust. Soc. Am. 146, 4020–4032. 10.1121/1.5132545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Fullerton, B. C. , and Kiang, N. Y. (1990). “ The effect of brainstem lesions on brainstem auditory evoked potentials in the cat,” Hear. Res. 49, 363–390. 10.1016/0378-5955(90)90114-5 [DOI] [PubMed] [Google Scholar]
- 103. Fullerton, B. C. , Levine, R. A. , Hosford-Dunn, H. L. , and Kiang, N. Y. (1987). “ Comparison of cat and human brain-stem auditory evoked potentials,” Electroencephalogr. Clin. Neurophysiol. 66, 547–570. 10.1016/0013-4694(87)90102-7 [DOI] [PubMed] [Google Scholar]
- 104. Furman, A. C. , Kujawa, S. G. , and Liberman, M. C. (2013). “ Noise-induced cochlear neuropathy is selective for fibers with low spontaneous rates,” J. Neurophysiol. 110, 577–586. 10.1152/jn.00164.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Furness, D. N. (2015). “ Molecular basis of hair cell loss,” Cell Tissue Res. 361, 387–399. 10.1007/s00441-015-2113-z [DOI] [PubMed] [Google Scholar]
- 106. Galazyuk, A. , and Hebert, S. (2015). “ Gap-prepulse inhibition of the acoustic startle reflex (GPIAS) for tinnitus assessment: Current status and future directions,” Front. Neurol. 6, 88. 10.3389/fneur.2015.00088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Gardi, J. N. , and Berlin, C. I. (1981). “ Binaural interaction components. Their possible origins in guinea pig auditory brainstem response,” Arch. Otolaryngol. 107, 164–168. 10.1001/archotol.1981.00790390030009 [DOI] [PubMed] [Google Scholar]
- 108. Gardi, J. N. , and Bledsoe, S. C., Jr. (1981). “ The use of kainic acid for studying the origins of scalp-recorded auditory brainstem responses in the guinea pig,” Neurosci. Lett. 26, 143–149. 10.1016/0304-3940(81)90340-2 [DOI] [PubMed] [Google Scholar]
- 109. Garetz, S. L. , Altschuler, R. A. , and Schacht, J. (1994). “ Attenuation of gentamicin ototoxicity by glutathione in the guinea pig in vivo,” Hear. Res. 77, 81–87. 10.1016/0378-5955(94)90255-0 [DOI] [PubMed] [Google Scholar]
- 110. Garrett, A. R. , Robertson, D. , Sellick, P. M. , and Mulders, W. H. (2011). “ The actions of dopamine receptors in the guinea pig cochlea,” Audiol. Neurootol. 16, 145–157. 10.1159/000316674 [DOI] [PubMed] [Google Scholar]
- 111. Gerstein, G. L. , and Kiang, N. Y. (1960). “ An approach to the quantitative analysis of electrophysiological data from single neurons,” Biophys. J. 1, 15–28. 10.1016/S0006-3495(60)86872-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Gill, S. S. , and Salt, A. N. (1997). “ Quantitative differences in endolymphatic calcium and endocochlear potential between pigmented and albino guinea pigs,” Hear. Res. 113, 191–197. 10.1016/S0378-5955(97)00141-X [DOI] [PubMed] [Google Scholar]
- 113. Giraudet, F. , Horner, K. C. , and Cazals, Y. (2002). “ Similar half-octave TTS protection of the cochlea by xylazine/ketamine or sympathectomy,” Hear. Res. 174, 239–248. 10.1016/S0378-5955(02)00698-6 [DOI] [PubMed] [Google Scholar]
- 114. Gitter, A. H. , and Zenner, H. P. (1995). “ Electromotile responses and frequency tuning of isolated outer hair cells of the guinea pig cochlea,” Eur. Arch. Otorhinolaryngol. 252, 15–19. 10.1007/BF00171434 [DOI] [PubMed] [Google Scholar]
- 115. Gittleman, S. , Le Prell, C. G. , and Hammill, T. (2019). “ Octave band noise exposure: Laboratory models and otoprotection efforts,” J. Acoust. Soc. Am. 146, 3800–3810. 10.1121/1.5133393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Goldwin, B. , Khan, M. J. , Shivapuja, B. , Seidman, M. D. , and Quirk, W. S. (1998). “ Sarthran preserves cochlear microcirculation and reduces temporary threshold shifts after noise exposure,” Otolaryngol. Head Neck Surg. 118, 576–583. 10.1177/019459989811800503 [DOI] [PubMed] [Google Scholar]
- 117. Gourevitch, B. , and Edeline, J. M. (2011). “ Age-related changes in the guinea pig auditory cortex: Relationship with brainstem changes and comparison with tone-induced hearing loss,” Eur. J. Neurosci. 34, 1953–1965. 10.1111/j.1460-9568.2011.07905.x [DOI] [PubMed] [Google Scholar]
- 118. Goutman, J. D. , Elgoyhen, A. B. , and Gomez-Casati, M. E. (2015). “ Cochlear hair cells: The sound-sensing machines,” FEBS Lett. 589, 3354–3361. 10.1016/j.febslet.2015.08.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Grant, K. (2014). “ Rodent nutrition: Digestive comparisons of 4 common rodent species,” Vet. Clin. North Am. Exot. Anim. Pract. 17, 471–483. 10.1016/j.cvex.2014.05.007 [DOI] [PubMed] [Google Scholar]
- 120. Gratton, M. A. , Salvi, R. J. , Kamen, B. A. , and Saunders, S. S. (1990). “ Interaction of cisplatin and noise on the peripheral auditory system,” Hear. Res. 50, 211–223. 10.1016/0378-5955(90)90046-R [DOI] [PubMed] [Google Scholar]
- 121. Grimsley, J. M. , Palmer, A. R. , and Wallace, M. N. (2011). “ Different representations of tooth chatter and purr call in guinea pig auditory cortex,” Neuroreport 22, 613–616. 10.1097/WNR.0b013e3283495ae9 [DOI] [PubMed] [Google Scholar]
- 122. Groenink, L. , Verdouw, P. M. , Bakker, B. , and Wever, K. E. (2015). “ Pharmacological and methodological aspects of the separation-induced vocalization test in guinea pig pups; a systematic review and meta-analysis,” Eur. J. Pharmacol. 753, 191–208. 10.1016/j.ejphar.2014.10.062 [DOI] [PubMed] [Google Scholar]
- 123. Groff, J. A. , and Liberman, M. C. (2003). “ Modulation of cochlear afferent response by the lateral olivocochlear system: Activation via electrical stimulation of the inferior colliculus,” J. Neurophysiol. 90, 3178–3200. 10.1152/jn.00537.2003 [DOI] [PubMed] [Google Scholar]
- 124. Grosh, K. , Zheng, J. , Zou, Y. , de Boer, E. , and Nuttall, A. L. (2004). “ High-frequency electromotile responses in the cochlea,” J. Acoust. Soc. Am. 115, 2178–2184. 10.1121/1.1695431 [DOI] [PubMed] [Google Scholar]
- 125. Haase, G. M. , Prasad, K. N. , Cole, W. C. , Baggett-Strehlau, J. M. , and Wyatt, S. E. (2009). “ Antioxidant micronutrient impact on hearing disorders: Concept, rationale, and evidence,” Am. J. Otolaryngol. 32, 55–61. 10.1016/j.amjoto.2009.09.002 [DOI] [PubMed] [Google Scholar]
- 126. Hahn, H. , Salt, A. N. , Schumacher, U. , and Plontke, S. K. (2013). “ Gentamicin concentration gradients in scala tympani perilymph following systemic applications,” Audiol. Neurootol. 18, 383–391. 10.1159/000355283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Hakizimana, P. , Brownell, W. E. , Jacob, S. , and Fridberger, A. (2012). “ Sound-induced length changes in outer hair cell stereocilia,” Nat. Commun. 3, 1094. 10.1038/ncomms2100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Hallen, O. , Edstroem, J. E. , and Hamberger, A. (1965). “ Cytochemical response to acoustic stimuli in the spiral ganglion cells of guinea pigs,” Acta Otolaryngol. 60, 121–128. 10.3109/00016486509126995 [DOI] [PubMed] [Google Scholar]
- 129. Hamers, F. P. , Klis, S. F. , Gispen, W. H. , and Smoorenburg, G. F. (1994). “ Application of a neuroprotective ACTH(4-9) analog to affect cisplatin ototoxicity: An electrocochleographic study in guinea pigs,” Eur. Arch. Otorhinolaryngol. 251, 23–29. 10.1007/BF00175953 [DOI] [PubMed] [Google Scholar]
- 130. Hammill, T. L. (2017). “ An evidence-base and implementation framework for promoting best practices in pharmaceutical interventions for hearing loss (PIHL),” Doctoral thesis, The University of Texas at Austin, Austin, TX. [Google Scholar]
- 131. Hammill, T. L. , and Campbell, K. C. (2018). “ Protection for medication-induced hearing loss: The state of the science,” Int. J. Audiol. 57, S67–S75. 10.1080/14992027.2018.1455114 [DOI] [PubMed] [Google Scholar]
- 132. Harper, L. V. (1976). “ Behavior,” in The Biology of the Guinea Pig, edited by Wagner J. E. and Manning P. J. ( Academic Press, New York: ), pp. 31–51. [Google Scholar]
- 133. Harrison, R. V. , and Palmer, A. R. (1984). “ Neurone response latency in the inferior colliculus in relation to the auditory brainstem responses (ABR) in the guinea pig,” Scand. Audiol. 13, 275–281. 10.3109/01050398409042136 [DOI] [PubMed] [Google Scholar]
- 134. Harrop-Jones, A. , Wang, X. , Fernandez, R. , Dellamary, L. , Ryan, A. F. , LeBel, C. , and Piu, F. (2016). “ The sustained-exposure dexamethasone formulation OTO-104 offers effective protection against noise-induced hearing loss,” Audiol. Neurootol. 21, 12–21. 10.1159/000441814 [DOI] [PubMed] [Google Scholar]
- 135. Hatch, M. , Tsai, M. , LaRouere, M. J. , Nuttall, A. L. , and Miller, J. M. (1991). “ The effects of Carbogen, carbon dioxide, and oxygen on noise-induced hearing loss,” Hear. Res. 56, 265–272. 10.1016/0378-5955(91)90176-A [DOI] [PubMed] [Google Scholar]
- 136. Haupt, H. , and Scheibe, F. (2002). “ Preventive magnesium supplement protects the inner ear against noise-induced impairment of blood flow and oxygenation in the guinea pig,” Magnes. Res. 15, 17–25. [PubMed] [Google Scholar]
- 137. He, D. Z. , Jia, S. , and Dallos, P. (2003). “ Prestin and the dynamic stiffness of cochlear outer hair cells,” J. Neurosci. 23, 9089–9096. 10.1523/JNEUROSCI.23-27-09089.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Heeringa, A. N. , Agterberg, M. J. , and van Dijk, P. (2014). “ Spontaneous behavior in noise and silence: A possible new measure to assess tinnitus in Guinea pigs,” Front. Neurol. 5, 207. 10.3389/fneur.2014.00207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Heeringa, A. N. , and van Dijk, P. (2018). “ Neural coding of the sound envelope is changed in the inferior colliculus immediately following acoustic trauma,” Eur. J. Neurosci. 49(10), 1220–1232. 10.1111/ejn.14299 [DOI] [PubMed] [Google Scholar]
- 140. Heffner, R. , Heffner, H. , and Masterton, B. (1971). “ Behavioral measurements of absolute and frequency-difference thresholds in guinea pig,” J. Acoust. Soc. Am. 49, 1888–1895. 10.1121/1.1912596 [DOI] [PubMed] [Google Scholar]
- 141. Hellberg, V. , Wallin, I. , Ehrsson, H. , and Laurell, G. (2013). “ Cochlear pharmacokinetics of cisplatin: An in vivo study in the guinea pig,” Laryngoscope 123, 3172–3177. 10.1002/lary.24235 [DOI] [PubMed] [Google Scholar]
- 142. Hirsch, E. , and Collier, G. (1974). “ Ecological determinants of reinforcement in the guinea pig,” Physiol. Behav. 12, 239–249. 10.1016/0031-9384(74)90178-4 [DOI] [PubMed] [Google Scholar]
- 143. Holt, A. G. , Kallakuri, S. , Braun, R. , and Altschuler, R. A. (2019). “ The rat as a model for studying noise injury and otoprotection,” J. Acoust. Soc. Am. 146, 3681–3691. 10.1121/1.5131344 [DOI] [PubMed] [Google Scholar]
- 144. Hori, R. , Nakagawa, T. , Sugimoto, Y. , Sakamoto, T. , Yamamoto, N. , Hamaguchi, K. , and Ito, J. (2009). “ Prostaglandin E receptor subtype EP4 agonist protects cochleae against noise-induced trauma,” Neurosci. 160, 813–819. 10.1016/j.neuroscience.2009.03.014 [DOI] [PubMed] [Google Scholar]
- 145. Hori, R. , Nakagawa, T. , Yamamoto, N. , Hamaguchi, K. , and Ito, J. (2013). “ Prostaglandin E receptor subtype EP4 agonist serves better to protect cochlea than prostaglandin E1,” Auris. Nasus. Larynx 40, 539–542. 10.1016/j.anl.2013.05.003 [DOI] [PubMed] [Google Scholar]
- 146. Hou, F. , Wang, S. , Zhai, S. , Hu, Y. , Yang, W. , and He, L. (2003). “ Effects of alpha-tocopherol on noise-induced hearing loss in guinea pigs,” Hear. Res. 179, 1–8. 10.1016/S0378-5955(03)00065-0 [DOI] [PubMed] [Google Scholar]
- 147. Huang, C. M. (1980). “ A comparative study of the brain stem auditory response in mammals,” Brain Res. 184, 215–219. 10.1016/0006-8993(80)90601-0 [DOI] [PubMed] [Google Scholar]
- 148. Hudspeth, A. J. (2008). “ Making an effort to listen: Mechanical amplification in the ear,” Neuron 59, 530–545. 10.1016/j.neuron.2008.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149. Hunter, B. A. , Lee, S. , Odland, R. M. , and Juhn, S. K. (2003). “ Estimation of perilymph concentration of agents applied to the round window membrane by microdialysis,” Acta Otolaryngol. 123, 453–458. 10.1080/00016480310000467 [DOI] [PubMed] [Google Scholar]
- 150. Hyppolito, M. A. , de Oliveira, J. A. , and Rossato, M. (2006). “ Cisplatin ototoxicity and otoprotection with sodium salicylate,” Eur. Arch. Otorhinolaryngol. 263, 798–803. 10.1007/s00405-006-0070-6 [DOI] [PubMed] [Google Scholar]
- 151. Inai, S. , Watanabe, K. , and Okubo, K. (2012). “ Inducible nitric oxide synthase participates in cochlear damage after acoustic stimulation in Guinea pigs,” Nippon Ika Daigaku Zasshi 79, 121–128. 10.1272/jnms.79.121 [DOI] [PubMed] [Google Scholar]
- 152. Inaoka, T. , Nakagawa, T. , Kikkawa, Y. S. , Tabata, Y. , Ono, K. , Yoshida, M. , Tsubouchi, H. , Ido, A. , and Ito, J. (2009). “ Local application of hepatocyte growth factor using gelatin hydrogels attenuates noise-induced hearing loss in guinea pigs,” Acta Otolaryngol. 129, 453–457. 10.1080/00016480902725197 [DOI] [PubMed] [Google Scholar]
- 153. Ingham, N. J. , Comis, S. D. , and Withington, D. J. (1999). “ Hair cell loss in the aged guinea pig cochlea,” Acta Otolaryngol 119, 42–47. 10.1080/00016489950181918 [DOI] [PubMed] [Google Scholar]
- 154. Ingham, N. J. , Thornton, S. K. , Comis, S. D. , and Withington, D. J. (1998a). “ The auditory brainstem response of aged guinea pigs,” Acta Otolaryngol. (Stockh). 118, 673–680. 10.1080/00016489850183160 [DOI] [PubMed] [Google Scholar]
- 155. Ingham, N. J. , Thornton, S. K. , and Withington, D. J. (1998b). “ Age-related changes in auditory spatial properties of the guinea pig superior colliculus,” Brain Res. 788, 60–68. 10.1016/S0006-8993(97)01513-8 [DOI] [PubMed] [Google Scholar]
- 156. Ison, J. R. (1982). “ Temporal acuity in auditory function in the rat: Reflex inhibition by brief gaps in noise,” J. Comp. Physiol. Psychol. 96, 945–954. 10.1037/0735-7036.96.6.945 [DOI] [PubMed] [Google Scholar]
- 157. Ison, J. R. , Allen, P. D. , Rivoli, P. J. , and Moore, J. T. (2005). “ The behavioral response of mice to gaps in noise depends on its spectral components and its bandwidth,” J. Acoust. Soc. Am. 117, 3944–3951. 10.1121/1.1904387 [DOI] [PubMed] [Google Scholar]
- 158. Ison, J. R. , Castro, J. , Allen, P. , Virag, T. M. , and Walton, J. P. (2002). “ The relative detectability for mice of gaps having different ramp durations at their onset and offset boundaries,” J. Acoust. Soc. Am. 112, 740–747. 10.1121/1.1490352 [DOI] [PubMed] [Google Scholar]
- 159. Ison, J. R. , and Hammond, G. R. (1971). “ Modification of the startle reflex in the rat by changes in the auditory and visual environments,” J. Comp. Physiol. Psychol. 75, 435–452. 10.1037/h0030934 [DOI] [PubMed] [Google Scholar]
- 160. Ison, J. R. , and Krauter, E. E. (1974). “ Reflex-inhibiting stimuli and the refractory period of the acoustic startle reflex in the rat,” J. Comp. Physiol. Psychol. 86, 420–425. 10.1037/h0036134 [DOI] [PubMed] [Google Scholar]
- 161. Ison, J. R. , McAdam, D. W. , and Hammond, G. R. (1973). “ Latency and amplitude changes in the acoustic startle reflex of the rat produced by variation in auditory prestimulation,” Physiol. Behav. 10, 1035–1039. 10.1016/0031-9384(73)90185-6 [DOI] [PubMed] [Google Scholar]
- 162. Jenison, G. L. , and Bobbin, R. P. (1985). “ Quisqualate excites spiral ganglion neurons of the guinea pig,” Hear. Res. 20, 261–265. 10.1016/0378-5955(85)90030-9 [DOI] [PubMed] [Google Scholar]
- 163. Jenkins, J. R. (2010). “ Diseases of geriatric Guinea pigs and chinchillas,” Vet. Clin. North Am. Exot. Anim. Pract. 13, 85–93. 10.1016/j.cvex.2009.12.004 [DOI] [PubMed] [Google Scholar]
- 164. Jewett, D. L. (1970). “ Volume-conducted potentials in response to auditory stimuli as detected by averaging in the cat,” Electroencephalogr. Clin. Neurophysiol. 28, 609–618. 10.1016/0013-4694(70)90203-8 [DOI] [PubMed] [Google Scholar]
- 165. Kakehata, S. , Dallos, P. , Brownell, W. E. , Iwasa, K. H. , Kachar, B. , Kalinec, F. , Ikeda, K. , and Takasaka, T. (2000). “ Current concept of outer hair cell motility,” Auris. Nasus. Larynx 27, 349–355. 10.1016/S0385-8146(00)00081-X [DOI] [PubMed] [Google Scholar]
- 166. Kalinec, G. M. , Lomberk, G. , Urrutia, R. A. , and Kalinec, F. (2017). “ Resolution of cochlear inflammation: Novel target for preventing or ameliorating drug-, noise- and age-related hearing loss,” Front. Cell. Neurosci. 11, 192. 10.3389/fncel.2017.00192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Kanagawa, E. , Sugahara, K. , Hirose, Y. , Mikuriya, T. , Shimogori, H. , and Yamashita, H. (2014). “ Effects of substance P during the recovery of hearing function after noise-induced hearing loss,” Brain Res. 1582, 187–196. 10.1016/j.brainres.2014.07.024 [DOI] [PubMed] [Google Scholar]
- 168. Kang, S. Y. , Colesa, D. J. , Swiderski, D. L. , Su, G. L. , Raphael, Y. , and Pfingst, B. E. (2010). “ Effects of hearing preservation on psychophysical responses to cochlear implant stimulation,” J. Assoc. Res. Otolaryngol. 11, 245–265. 10.1007/s10162-009-0194-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Keithley, E. M. , Ma, C. L. , Ryan, A. F. , Louis, J. C. , and Magal, E. (1998). “ GDNF protects the cochlea against noise damage,” Neuroreport 9, 2183–2187. 10.1097/00001756-199807130-00007 [DOI] [PubMed] [Google Scholar]
- 170. Khan, M. J. , Seidman, M. D. , Quirk, W. S. , and Shivapuja, B. G. (2000). “ Effects of kynurenic acid as a glutamate receptor antagonist in the guinea pig,” Eur. Arch. Otorhinolaryngol. 257, 177–181. 10.1007/s004050050218 [DOI] [PubMed] [Google Scholar]
- 171. Kiang, N. Y. (1980). “ Processing of speech by the auditory nervous system,” J. Acoust. Soc. Am. 68, 830–835. 10.1121/1.384822 [DOI] [PubMed] [Google Scholar]
- 172. Kiang, N. Y. , Liberman, M. C. , and Levine, R. A. (1976). “ Auditory-nerve activity in cats exposed to ototoxic drugs and high-intensity sounds,” Ann. Otol. Rhinol. Laryngol. 85, 752–768. 10.1177/000348947608500605 [DOI] [PubMed] [Google Scholar]
- 173. Kiang, N. Y. , Moxon, E. C. , and Levine, R. A. (1970). “ Auditory-nerve activity in cats with normal and abnormal cochleas,” in Sensorineural Hearing Loss, edited by Wolstenholme G. E. W. and Knight J. ( Wiley, Hoboken, NJ: ), pp. 241–273. 10.1002/9780470719756.ch15 [DOI] [PubMed] [Google Scholar]
- 174. Kiang, N. Y. , and Peake, W. (1960). “ Components of electrical responses recorded from the cochlea,” Ann. Otol. Rhinol. Laryngol. 69, 448–458. 10.1177/000348946006900213 [DOI] [PubMed] [Google Scholar]
- 175. Kiang, N. Y. , Sachs, M. B. , and Peake, W. T. (1967). “ Shapes of tuning curves for single auditory-nerve fibers,” J. Acoust. Soc. Am. 42, 1341–1342. 10.1121/1.1910723 [DOI] [PubMed] [Google Scholar]
- 176. Kiang, N. Y. , Watanabe, T. , Thomas, E. C. , and Clark, L. F. (1962). “ Stimulus coding in the cat's auditory nerve. Preliminary report,” Trans. Am. Otol. Soc. 50, 264–283. [PubMed] [Google Scholar]
- 177. Kim, J. U. , Lee, H. J. , Kang, H. H. , Shin, J. W. , Ku, S. W. , Ahn, J. H. , Kim, Y. J. , and Chung, J. W. (2005). “ Protective effect of isoflurane anesthesia on noise-induced hearing loss in mice,” Laryngoscope 115, 1996–1999. 10.1097/01.mlg.0000180173.81034.4d [DOI] [PubMed] [Google Scholar]
- 178. Konishi, T. , Salt, A. N. , and Hamrick, P. E. (1979). “ Effects of exposure to noise on ion movement in guinea pig cochlea,” Hear. Res. 1, 325–342. 10.1016/0378-5955(79)90004-2 [DOI] [PubMed] [Google Scholar]
- 179. Kuang, R. , Hever, G. , Zajic, G. , Yan, Q. , Collins, F. , Louis, J. C. , Keithley, E. , and Magal, E. (1999). “ Glial cell line-derived neurotrophic factor. Potential for otoprotection,” Ann. N. Y. Acad. Sci. 884, 270–291. 10.1111/j.1749-6632.1999.tb08648.x [DOI] [PubMed] [Google Scholar]
- 180. Kujawa, S. G. , and Liberman, M. C. (1997). “ Conditioning-related protection from acoustic injury: Effects of chronic deefferentation and sham surgery,” J. Neurophysiol. 78, 3095–3106. 10.1152/jn.1997.78.6.3095 [DOI] [PubMed] [Google Scholar]
- 181. Kujawa, S. G. , and Liberman, M. C. (1999). “ Long-term sound conditioning enhances cochlear sensitivity,” J. Neurophysiol. 82, 863–873. 10.1152/jn.1999.82.2.863 [DOI] [PubMed] [Google Scholar]
- 182. Kujawa, S. G. , and Liberman, M. C. (2001). “ Effects of olivocochlear feedback on distortion product otoacoustic emissions in guinea pig,” J. Assoc. Res. Otolaryngol. 2, 268–278. 10.1007/s101620010047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Kujawa, S. G. , and Liberman, M. C. (2006). “ Acceleration of age-related hearing loss by early noise exposure: Evidence of a misspent youth,” J. Neurosci. 26, 2115–2123. 10.1523/JNEUROSCI.4985-05.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Kujawa, S. G. , and Liberman, M. C. (2015). “ Synaptopathy in the noise-exposed and aging cochlea: Primary neural degeneration in acquired sensorineural hearing loss,” Hear. Res. 330, 191–199. 10.1016/j.heares.2015.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Kujawa, S. G. , and Liberman, M. C. (2019). “ Translating animal models to human therapeutics in noise-induced and age-related hearing loss,” Hear. Res. 377, 44–52. 10.1016/j.heares.2019.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Kurokawa, M. , and Kornbluth, S. (2009). “ Caspases and kinases in a death grip,” Cell 138, 838–854. 10.1016/j.cell.2009.08.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Landegger, L. D. , Honeder, C. , Zhu, C. , Schopper, H. , Engleder, E. , Gabor, F. , Gstoettner, W. , and Arnoldner, C. (2016). “ Noise trauma and systemic application of the selective glucocorticoid receptor modulator compound A,” J. Negat. Results Biomed. 15, 10. 10.1186/s12952-016-0053-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Lanvers-Kaminsky, C. , Zehnhoff-Dinnesen, A. A. , Parfitt, R. , and Ciarimboli, G. (2017). “ Drug-induced ototoxicity: Mechanisms, pharmacogenetics, and protective strategies,” Clin. Pharmacol. Ther. 101, 491–500. 10.1002/cpt.603 [DOI] [PubMed] [Google Scholar]
- 189. Latoni, J. , Shivapuja, B. , Seidman, M. D. , and Quirk, W. S. (1996). “ Pentoxifylline maintains cochlear microcirculation and attenuates temporary threshold shifts following acoustic overstimulation,” Acta Otolaryngol. 116, 388–394. 10.3109/00016489609137862 [DOI] [PubMed] [Google Scholar]
- 190. Laurell, G. , and Pierre, P. V. (2015). “ Hearing loss after cisplatin: Oxidative stress pathways and potential for protection,” in Oxidative Stress in Applied Basic Research and Clinical Practice: Free Radicals in ENT Pathology, edited by Miller J. M., Le Prell C. G., and Rybak L. P. ( Humana Press, New York: ), pp. 217–241. [Google Scholar]
- 191. Lautermann, J. , McLaren, J. , and Schacht, J. (1995a). “ Glutathione protection against gentamicin ototoxicity depends on nutritional status,” Hear. Res. 86, 15–24. 10.1016/0378-5955(95)00049-A [DOI] [PubMed] [Google Scholar]
- 192. Lautermann, J. , and Schacht, J. (1996). “ A sensitive animal model to assess acute and chronic ototoxic effects,” Arch. Otolaryngol. Head Neck Surg. 122, 837–840. 10.1001/archotol.1996.01890200027005 [DOI] [PubMed] [Google Scholar]
- 193. Lautermann, J. , Song, B. , McLaren, J. , and Schacht, J. (1995b). “ Diet is a risk factor in cisplatin ototoxicity,” Hear. Res. 88, 47–53. 10.1016/0378-5955(95)00097-N [DOI] [PubMed] [Google Scholar]
- 194. Lee, K. Y. , Nakagawa, T. , Okano, T. , Hori, R. , Ono, K. , Tabata, Y. , Lee, S. H. , and Ito, J. (2007). “ Novel therapy for hearing loss: Delivery of insulin-like growth factor 1 to the cochlea using gelatin hydrogel,” Otol. Neurotol. 28, 976–981. 10.1097/MAO.0b013e31811f40db [DOI] [PubMed] [Google Scholar]
- 195. Lee, M. Y. , and Park, Y. H. (2018). “ Potential of gene and cell therapy for inner ear hair cells,” BioMed Res. Int. 2018, 8137614. 10.1155/2018/8137614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Leggett, K. , Mendis, V. , and Mulders, W. (2018). “ Divergent responses in the gap prepulse inhibition of the acoustic startle reflex in two different guinea pig colonies,” Int. Tinnitus J. 22, 1–9. 10.5935/0946-5448.20180001 [DOI] [PubMed] [Google Scholar]
- 197. Lendvai, B. , Halmos, G. B. , Polony, G. , Kapocsi, J. , Horvath, T. , Aller, M. , Sylvester Vizi, E. , and Zelles, T. (2011). “ Chemical neuroprotection in the cochlea: The modulation of dopamine release from lateral olivocochlear efferents,” Neurochem. Int. 59, 150–158. 10.1016/j.neuint.2011.05.015 [DOI] [PubMed] [Google Scholar]
- 198. Le Prell, C. G. (2019). “ Effects of noise exposure on auditory brainstem response and speech-in-noise tasks: A review of the literature,” Int. J. Audiol. 58, S3–S32. 10.1080/14992027.2018.1534010 [DOI] [PubMed] [Google Scholar]
- 199. Le Prell, C. G. , and Bao, J. (2012). “ Prevention of noise-induced hearing loss: Potential therapeutic agents,” in Noise-Induced Hearing Loss: Scientific Advances, Springer Handbook of Auditory Research, edited by Le Prell C. G., Henderson D., Fay R. R., and Popper A. N. ( Springer Science+Business Media, LLC, New York: ), pp. 285–338. [Google Scholar]
- 200. Le Prell, C. G. , Bledsoe, S. C., Jr. , Bobbin, R. P. , and Puel, J. L. (2001). “ Neurotransmission in the inner ear: Functional and molecular analyses,” in Physiology of the Ear, edited by Jahn A. F. and Santos-Sacchi J. ( Singular Publishing, New York: ), pp. 575–611. [Google Scholar]
- 201. Le Prell, C. G. , Dolan, D. F. , Bennett, D. C. , and Boxer, P. A. (2011a). “ Nutrient treatment and achieved plasma levels: Reduction of noise-induced hearing loss at multiple post-noise test times,” Transl. Res. 158, 54–70. 10.1016/j.trsl.2011.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Le Prell, C. G. , Dolan, D. F. , Hughes, L. F. , Altschuler, R. A. , Shore, S. E. , and Bledsoe, S. C., Jr. (2014a). “ Disruption of lateral olivocochlear neurons with a dopaminergic neurotoxin depresses spontaneous auditory nerve activity,” Neurosci. Lett. 582, 54–58. 10.1016/j.neulet.2014.08.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Le Prell, C. G. , Gagnon, P. M. , Bennett, D. C. , and Ohlemiller, K. K. (2011b). “ Nutrient-enhanced diet reduces noise-induced damage to the inner ear and hearing loss,” Transl. Res. 158, 38–53. 10.1016/j.trsl.2011.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Le Prell, C. G. , Halsey, K. , Hughes, L. F. , Dolan, D. F. , and Bledsoe, S. C., Jr. (2005). “ Disruption of lateral olivocochlear neurons via a dopaminergic neurotoxin depresses sound-evoked auditory nerve activity,” J. Assoc. Res. Otolaryngol. 6, 48–62. 10.1007/s10162-004-5009-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Le Prell, C. G. , Hughes, L. F. , and Bledsoe, S. C., Jr. (2014b). “ Dynorphin release by the lateral olivocochlear efferents may inhibit auditory nerve activity: A cochlear drug delivery study,” Neurosci. Lett. 571, 17–22. 10.1016/j.neulet.2014.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Le Prell, C. G. , Hughes, L. F. , and Miller, J. M. (2007a). “ Free radical scavengers vitamins A, C, and E plus magnesium reduce noise trauma,” Free Radic. Biol. Med. 42, 1454–1463. 10.1016/j.freeradbiomed.2007.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Le Prell, C. G. , Kawamoto, K. , Raphael, Y. , and Dolan, D. F. (2006). “ Electromotile hearing: Acoustic tones mask psychophysical response to high-frequency electrical stimulation of intact guinea pig cochleae,” J. Acoust. Soc. Am. 120, 3889–3900. 10.1121/1.2359238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Le Prell, C. G. , and Miller, J. M. (2016). “ The role of oxidative stress in hearing loss,” in Oxidative Stress and Antioxidant Protection: The Science of Free Radical Biology & Disease, edited by Armstrong D., and Stratton R. D. ( Wiley, Somerset, NJ: ), pp. 115–131. [Google Scholar]
- 209. Le Prell, C. G. , Ojano-Dirain, C. P. , Rudnick, E. W. , Nelson, M. A. , deRemer, S. , Prieskorn, D. M. , and Miller, J. M. (2014c). “ Assessment of nutrient supplement to reduce gentamicin-induced ototoxicity,” J. Assoc. Res. Otolaryngol. 15, 375–393. 10.1007/s10162-014-0448-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210. Le Prell, C. G. , Shore, S. E. , Hughes, L. F. , and Bledsoe, S. C., Jr. (2003). “ Disruption of lateral efferent pathways: Functional changes in auditory evoked responses,” J. Assoc. Res. Otolaryngol. 4, 276–290. 10.1007/s10162-002-3018-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. Le Prell, C. G. , and Spankovich, C. (2013). “ Noise-induced hearing loss: Detection, prevention and management,” in Otology and Neurotology, edited by Kirtane M. V., de Souza C. E., Sanna M., and Devaiah A. K. ( Thieme, Stuttgart, Germany: ), pp. 268–284. [Google Scholar]
- 212. Le Prell, C. G. , Yagi, M. , Kawamoto, K. , Beyer, L. A. , Atkin, G. , Raphael, Y. , Dolan, D. F. , Bledsoe, S. C. J. , and Moody, D. B. (2004). “ Chronic excitotoxicity in the guinea pig cochlea induces temporary functional deficits without disrupting otoacoustic emissions,” J. Acoust. Soc. Am. 116, 1044–1056. 10.1121/1.1772395 [DOI] [PubMed] [Google Scholar]
- 213. Le Prell, C. G. , Yamashita, D. , Minami, S. B. , Yamasoba, T. , and Miller, J. M. (2007b). “ Mechanisms of noise-induced hearing loss indicate multiple methods of prevention,” Hear. Res. 226, 22–43. 10.1016/j.heares.2006.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214. Le Prell, G. , Sachs, M. , and May, B. (1996). “ Representation of vowel-like spectra by discharge rate responses of individual auditory-nerve fibers,” Aud. Neurosci. 2, 275–288. [PMC free article] [PubMed] [Google Scholar]
- 215. Liberman, M. C. , and Gao, W. Y. (1995). “ Chronic cochlear de-efferentation and susceptibility to permanent acoustic injury,” Hear. Res. 90, 158–168. 10.1016/0378-5955(95)00160-2 [DOI] [PubMed] [Google Scholar]
- 216. Liberman, M. C. , and Kiang, N. Y. (1978). “ Acoustic trauma in cats. Cochlear pathology and auditory-nerve activity,” Acta Otolaryngol. Suppl. 358, 1–63. [PubMed] [Google Scholar]
- 217. Liberman, M. C. , and Kiang, N. Y. (1984). “ Single-neuron labeling and chronic cochlear pathology. IV. Stereocilia damage and alterations in rate- and phase-level functions,” Hear. Res. 16, 75–90. 10.1016/0378-5955(84)90026-1 [DOI] [PubMed] [Google Scholar]
- 218. Liberman, M. C. , and Kujawa, S. G. (2017). “ Cochlear synaptopathy in acquired sensorineural hearing loss: Manifestations and mechanisms,” Hear. Res. 349, 138–147. 10.1016/j.heares.2017.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Lin, H. W. , Furman, A. C. , Kujawa, S. G. , and Liberman, M. C. (2011). “ Primary neural degeneration in the Guinea pig cochlea after reversible noise-induced threshold shift,” J. Assoc. Res. Otolaryngol. 12, 605–616. 10.1007/s10162-011-0277-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220. Littman, T. , Bobbin, R. P. , Fallon, M. , and Puel, J. L. (1989). “ The quinoxalinediones DNQX, CNQX and two related congeners suppress hair cell-to-auditory nerve transmission,” Hear. Res. 40, 45–53. 10.1016/0378-5955(89)90098-1 [DOI] [PubMed] [Google Scholar]
- 221. Liu, H. Y. , Chi, F. L. , and Gao, W. Y. (2008). “ Taurine attenuates aminoglycoside ototoxicity by inhibiting inducible nitric oxide synthase expression in the cochlea,” Neuroreport 19, 117–120. 10.1097/WNR.0b013e3282f3b0ec [DOI] [PubMed] [Google Scholar]
- 222. Liu, L. , Wang, H. , Shi, L. , Almuklass, A. , He, T. , Aiken, S. , Bance, M. , Yin, S. , and Wang, J. (2012). “ Silent damage of noise on cochlear afferent innervation in guinea pigs and the impact on temporal processing,” PLoS One 7, e49550. 10.1371/journal.pone.0049550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223. Liu, Y. G. , He, Y. J. , Li, D. D. , Zheng, S. X. , and Niu, C. M. (2000). “ Effects of sound preconditioning on hearing loss from low or middle-frequency noise exposure,” Space Med. Med. Eng. 13, 313–317. [PubMed] [Google Scholar]
- 224. Lo, W. C. , Liao, L. J. , Wang, C. T. , Young, Y. H. , Chang, Y. L. , and Cheng, P. W. (2013). “ Dose-dependent effects of d-methionine for rescuing noise-induced permanent threshold shift in guinea-pigs,” Neuroscience 254, 222–229. 10.1016/j.neuroscience.2013.09.027 [DOI] [PubMed] [Google Scholar]
- 225. Lobarinas, E. , Hayes, S. H. , and Allman, B. L. (2013). “ The gap-startle paradigm for tinnitus screening in animal models: Limitations and optimization,” Hear. Res. 295, 150–160. 10.1016/j.heares.2012.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Lobarinas, E. , Spankovich, C. , and Le Prell, C. G. (2017). “ Evidence of ‘hidden hearing loss’ following noise exposures that produce robust TTS and ABR wave-I amplitude reductions,” Hear. Res. 349, 155–163. 10.1016/j.heares.2016.12.009 [DOI] [PubMed] [Google Scholar]
- 227. Lobarinas, E. , Sun, W. , Cushing, R. , and Salvi, R. (2004). “ A novel behavioral paradigm for assessing tinnitus using schedule-induced polydipsia avoidance conditioning (SIP-AC),” Hear. Res. 190, 109–114. 10.1016/S0378-5955(04)00019-X [DOI] [PubMed] [Google Scholar]
- 228. Lue, A. J. , and Brownell, W. E. (1999). “ Salicylate induced changes in outer hair cell lateral wall stiffness,” Hear. Res. 135, 163–168. 10.1016/S0378-5955(99)00102-1 [DOI] [PubMed] [Google Scholar]
- 229. Lynch, E. D. , Kil, J. , and Le Prell, C. G. (2016). “ Human clinical studies in noise-induced hearing loss,” in Translational Research in Audiology and the Hearing Sciences, Springer Handbook of Auditory Research, edited by Le Prell C. G., Lobarinas E., Fay R. R., and Popper A. N. ( Springer, New York: ), pp. 105–139. [Google Scholar]
- 230. Lyzwa, D. , Herrmann, J. M. , and Worgotter, F. (2015). “ Natural vocalizations in the mammalian inferior colliculus are broadly encoded by a small number of independent multi-units,” Front. Neural Circ. 9, 91. 10.3389/fncir.2015.00091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231. Maison, S. F. , and Liberman, M. C. (2000). “ Predicting vulnerability to acoustic injury with a noninvasive assay of olivocochlear reflex strength,” J. Neurosci. 20, 4701–4707. 10.1523/JNEUROSCI.20-12-04701.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232. Mamelle, E. , El Kechai, N. , Adenis, V. , Nguyen, Y. , Sterkers, O. , Agnely, F. , Bochot, A. , Edeline, J. M. , and Ferrary, E. (2018). “ Assessment of the efficacy of a local steroid rescue treatment administered 2 days after a moderate noise-induced trauma in guinea pig,” Acta Otolaryngol. 138, 610–616. 10.1080/00016489.2018.1438659 [DOI] [PubMed] [Google Scholar]
- 233. Manley, G. A. (2001). “ Evidence for an active process and a cochlear amplifier in nonmammals,” J. Neurophysiol. 86, 541–549. 10.1152/jn.2001.86.2.541 [DOI] [PubMed] [Google Scholar]
- 234. Matsumoto, N. , Kitani, R. , Maricle, A. , Mueller, M. , and Kalinec, F. (2010). “ Pivotal role of actin depolymerization in the regulation of cochlear outer hair cell motility,” Biophys. J. 99, 2067–2076. 10.1016/j.bpj.2010.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235. May, B. J. , Huang, A. , LePrell, G. , and Hienz, R. D. (1996). “ Vowel formant frequency discrimination in cats: Comparison of auditory nerve representations and psychophysical thresholds,” Aud. Neurosci. 3, 135–162. [PMC free article] [PubMed] [Google Scholar]
- 236. McFadden, S. L. , Woo, J. M. , Michalak, N. , and Ding, D. (2005). “ Dietary vitamin C supplementation reduces noise-induced hearing loss in guinea pigs,” Hear. Res. 202, 200–208. 10.1016/j.heares.2004.10.011 [DOI] [PubMed] [Google Scholar]
- 237. Meen, E. , Blakley, B. , and Quddusi, T. (2009). “ Brain-derived nerve growth factor in the treatment of sensorineural hearing loss,” Laryngoscope 119, 1590–1593. 10.1002/lary.20515 [DOI] [PubMed] [Google Scholar]
- 238. Melcher, J. R. , Guinan, J. J., Jr. , Knudson, I. M. , and Kiang, N. Y. (1996a). “ Generators of the brainstem auditory evoked potential in cat. II. Correlating lesion sites with waveform changes,” Hear. Res. 93, 28–51. 10.1016/0378-5955(95)00179-4 [DOI] [PubMed] [Google Scholar]
- 239. Melcher, J. R. , and Kiang, N. Y. (1996). “ Generators of the brainstem auditory evoked potential in cat. III: Identified cell populations,” Hear. Res. 93, 52–71. 10.1016/0378-5955(95)00200-6 [DOI] [PubMed] [Google Scholar]
- 240. Melcher, J. R. , Knudson, I. M. , Fullerton, B. C. , Guinan, J. J., Jr. , Norris, B. E. , and Kiang, N. Y. (1996b). “ Generators of the brainstem auditory evoked potential in cat. I. An experimental approach to their identification,” Hear. Res. 93, 1–27. 10.1016/0378-5955(95)00178-6 [DOI] [PubMed] [Google Scholar]
- 241. Meyer, P. , Kuhl, K. D. , Schmidt, R. , and Grutzmacher, W. (1991). “ Guinea pig cochlear blood flow under definite sound exposure-hydrogen clearance measurement,” ORL. J. Otorhinolaryngol. Relat. Spec. 53, 327–330. 10.1159/000276240 [DOI] [PubMed] [Google Scholar]
- 242. Mikuriya, T. , Sugahara, K. , Takemoto, T. , Tanaka, K. , Takeno, K. , Shimogori, H. , Nakai, A. , and Yamashita, H. (2005). “ Geranylgeranylacetone, a heat shock protein inducer, prevents acoustic injury in the guinea pig,” Brain Res. 1065, 107–114. 10.1016/j.brainres.2005.10.045 [DOI] [PubMed] [Google Scholar]
- 243. Miller, A. L. , Morris, D. J. , and Pfingst, B. E. (2000). “ Effects of time after deafening and implantation on guinea pig electrical detection thresholds,” Hear. Res. 144, 175–186. 10.1016/S0378-5955(00)00066-6 [DOI] [PubMed] [Google Scholar]
- 244. Miller, A. L. , Smith, D. W. , and Pfingst, B. E. (1999). “ Across-species comparisons of psychophysical detection thresholds for electrical stimulation of the cochlea: II. Strength-duration functions for single, biphasic pulses,” Hear. Res. 135, 47–55. 10.1016/S0378-5955(99)00089-1 [DOI] [PubMed] [Google Scholar]
- 245. Miller, C. A. , Faulkner, M. J. , and Pfingst, B. E. (1995a). “ Functional responses from guinea pigs with cochlear implants. II. Changes in electrophysiological and psychophysical measures over time,” Hear. Res. 92, 100–111. 10.1016/0378-5955(95)00205-7 [DOI] [PubMed] [Google Scholar]
- 246. Miller, C. A. , Woodruff, K. E. , and Pfingst, B. E. (1995b). “ Functional responses from guinea pigs with cochlear implants. I. Electrophysiological and psychophysical measures,” Hear. Res. 92, 85–99. 10.1016/0378-5955(95)00204-9 [DOI] [PubMed] [Google Scholar]
- 247. Minami, S. B. , Yamashita, D. , Ogawa, K. , Schacht, J. , and Miller, J. M. (2007). “ Creatine and tempol attenuate noise-induced hearing loss,” Brain Res. 1148, 83–89. 10.1016/j.brainres.2007.02.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Mohammadian, F. , Eatemadi, A. , and Daraee, H. (2017). “ Application of stem cell for the regeneration of spiral ganglion neurons,” Cell. Mol. Biol. 63, 6–12. 10.14715/cmb/2017.63.1.2 [DOI] [PubMed] [Google Scholar]
- 249. Mohan, S. , Smyth, B. J. , Namin, A. , Phillips, G. , and Gratton, M. A. (2014). “ Targeted amelioration of cisplatin-induced ototoxicity in guinea pigs,” Otolaryngol. Head Neck Surg. 151, 836–839. 10.1177/0194599814544877 [DOI] [PubMed] [Google Scholar]
- 250. Moody, D. B. (2004). “ Animal models in tinnitus,” in Tinnitus: Theory and Management, edited by Snow J. B. ( BC Decker, Hamilton: ), pp. 80–95. [Google Scholar]
- 251. Mulders, W. H. , Barry, K. M. , and Robertson, D. (2014). “ Effects of furosemide on cochlear neural activity, central hyperactivity and behavioural tinnitus after cochlear trauma in guinea pig,” PloS One 9, e97948. 10.1371/journal.pone.0097948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252. Mulders, W. H. , and Robertson, D. (2013). “ Development of hyperactivity after acoustic trauma in the guinea pig inferior colliculus,” Hear. Res. 298, 104–108. 10.1016/j.heares.2012.12.008 [DOI] [PubMed] [Google Scholar]
- 253. Muldoon, L. L. , Pagel, M. A. , Kroll, R. A. , Brummett, R. E. , Doolittle, N. D. , Zuhowski, E. G. , Egorin, M. J. , and Neuwelt, E. A. (2000). “ Delayed administration of sodium thiosulfate in animal models reduces platinum ototoxicity without reduction of antitumor activity,” Clin. Cancer Res. 6, 309–315. [PubMed] [Google Scholar]
- 254. Muller, M. , Tisch, M. , Maier, H. , and Lowenheim, H. (2017). “ Reduction of permanent hearing loss by local glucocorticoid application: Guinea pigs with acute acoustic trauma,” HNO 65, 59–67. 10.1007/s00106-016-0266-z [DOI] [PubMed] [Google Scholar]
- 255. Murillo-Cuesta, S. , Contreras, J. , Zurita, E. , Cediel, R. , Cantero, M. , Varela-Nieto, I. , and Montoliu, L. (2010). “ Melanin precursors prevent premature age-related and noise-induced hearing loss in albino mice,” Pigm. Cell Melanoma R. 23, 72–83. 10.1111/j.1755-148X.2009.00646.x [DOI] [PubMed] [Google Scholar]
- 256. Murphy, D. , and Daniel, S. J. (2011). “ Intratympanic dexamethasone to prevent cisplatin ototoxicity: A guinea pig model,” Otolaryngol. Head Neck Surg. 145, 452–457. 10.1177/0194599811406673 [DOI] [PubMed] [Google Scholar]
- 257. Mynatt, R. , Hale, S. A. , Gill, R. M. , Plontke, S. K. , and Salt, A. N. (2006). “ Demonstration of a longitudinal concentration gradient along scala tympani by sequential sampling of perilymph from the cochlear apex,” J. Assoc. Res. Otolaryngol. 7, 182–193. 10.1007/s10162-006-0034-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258.National Research Council (1996). Laboratory Animal Management: Rodents ( The National Academies Press, Washington, DC: ). [Google Scholar]
- 259. Neuwelt, E. A. , Brummett, R. E. , Remsen, L. G. , Kroll, R. A. , Pagel, M. A. , McCormick, C. I. , Guitjens, S. , and Muldoon, L. L. (1996). “ In vitro and animal studies of sodium thiosulfate as a potential chemoprotectant against carboplatin-induced ototoxicity,” Cancer Res. 56, 706–709. [PubMed] [Google Scholar]
- 260. Nilsen, K. E. , and Russell, I. J. (1999). “ Timing of cochlear feedback: Spatial and temporal representation of a tone across the basilar membrane,” Nat. Neurosci. 2, 642–648. 10.1038/10197 [DOI] [PubMed] [Google Scholar]
- 261. Niu, X. , Bogdanovic, N. , and Canlon, B. (2004). “ The distribution and the modulation of tyrosine hydroxylase immunoreactivity in the lateral olivocochlear system of the guinea-pig,” Neuroscience 125, 725–733. 10.1016/j.neuroscience.2004.02.023 [DOI] [PubMed] [Google Scholar]
- 262. Niu, X. , and Canlon, B. (2002). “ Protective mechanisms of sound conditioning,” Adv. Otorhinolaryngol. 59, 96–105. [DOI] [PubMed] [Google Scholar]
- 263. Niu, X. , Shao, R. , and Canlon, B. (2003). “ Suppression of apoptosis occurs in the cochlea by sound conditioning,” Neuroreport 14, 1025–1029. 10.1097/01.wnr.0000070830.57864.32 [DOI] [PubMed] [Google Scholar]
- 264. Nozawa, I. , Imamura, S. , Fujimori, I. , Hashimoto, K. , Shimomura, S. , Hisamatsu, K. , and Murakami, Y. (1996). “ Age-related alterations in the auditory brainstem responses and the compound action potentials in guinea pigs,” Laryngoscope 106, 1034–1039. 10.1097/00005537-199608000-00024 [DOI] [PubMed] [Google Scholar]
- 265. Nozawa, I. , Imamura, S. , Hashimoto, K. , Shimomura, S. , and Murakami, Y. (1997). “ Age-related changes in the compound action potentials of the eighth nerve in guinea pigs,” Eur. Arch. Otorhinolaryngol. 254, 145–149. 10.1007/BF02471279 [DOI] [PubMed] [Google Scholar]
- 266. Nuttall, A. L. (1999). “ Sound-induced cochlear ischemia/hypoxia as a mechanism of hearing loss,” Noise Health 2, 17–32. [PubMed] [Google Scholar]
- 267. Nuttall, A. L. , Guo, M. , and Ren, T. (1999). “ The radial pattern of basilar membrane motion evoked by electric stimulation of the cochlea,” Hear. Res. 131, 39–46. 10.1016/S0378-5955(99)00009-X [DOI] [PubMed] [Google Scholar]
- 268. Nuttall, A. L. , and Ren, T. (1995). “ Electromotile hearing: Evidence from basilar Membrane motion and otoacoustic emissions,” Hear. Res. 92, 170–177. 10.1016/0378-5955(95)00216-2 [DOI] [PubMed] [Google Scholar]
- 269. Ohinata, Y. , Yamasoba, T. , Schacht, J. , and Miller, J. M. (2000). “ Glutathione limits noise-induced hearing loss,” Hear. Res. 146, 28–34. 10.1016/S0378-5955(00)00096-4 [DOI] [PubMed] [Google Scholar]
- 270. Ohlemiller, K. K. (2006). “ Contributions of mouse models to understanding of age- and noise-related hearing loss,” Brain Res. 1091, 89–102. 10.1016/j.brainres.2006.03.017 [DOI] [PubMed] [Google Scholar]
- 271. Ohlemiller, K. K. (2019). “ Mouse methods and models for studies in hearing,” J. Acoust. Soc. Am. 146, 3668–3680. 10.1121/1.5132550 [DOI] [PubMed] [Google Scholar]
- 272. Ojano-Dirain, C. P. , Antonelli, P. J. , and Le Prell, C. G. (2014). “ Mitochondria-targeted antioxidant MitoQ reduces gentamicin-induced ototoxicity,” Otol. Neurotol. 35, 533–539. 10.1097/MAO.0000000000000192 [DOI] [PubMed] [Google Scholar]
- 273. Ojima, H. , Taira, M. , Kubota, M. , and Horikawa, J. (2012). “ Recognition of non-harmonic natural sounds by small mammals using competitive training,” PloS One 7, e51318. 10.1371/journal.pone.0051318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274. Okamoto, A. , Hasegawa, M. , Tamura, T. , Homma, T. , and Komatsuzaki, A. (1992). “ Effects of frequency and intensity of sound on cochlear blood flow,” Acta Otolaryngol. 112, 59–64. 10.3109/00016489209100783 [DOI] [PubMed] [Google Scholar]
- 275. Okamoto, A. , Tamura, T. , Hasegawa, M. , and Togawa, T. (1990). “ Effect of vasodilating agents on cochlear blood flow under loud sound exposure,” Acta Otolaryngol. 110, 394–398. 10.3109/00016489009122565 [DOI] [PubMed] [Google Scholar]
- 276. Ozdamar, O. , Kraus, N. , and Grossmann, J. (1986). “ Binaural interaction in the auditory middle latency response of the guinea pig,” Electroencephalogr. Clin. Neurophysiol. 63, 476–483. 10.1016/0013-4694(86)90129-X [DOI] [PubMed] [Google Scholar]
- 277. Pakkenberg, H. , and Thomsen, E. (1964). “ Cytoplasmic basophilia in spiral ganglion cells of the guinea-pig following strong acoustic stimulation,” Acta Otolaryngol. 58, 299–311. 10.3109/00016486409121391 [DOI] [PubMed] [Google Scholar]
- 278. Palmer, A. R. (1990). “ The representation of the spectra and fundamental frequencies of steady-state single- and double-vowel sounds in the temporal discharge patterns of guinea pig cochlear-nerve fibers,” J. Acoust. Soc. Am. 88, 1412–1426. 10.1121/1.400329 [DOI] [PubMed] [Google Scholar]
- 279. Palmer, A. R. , and Harrison, R. V. (1984). “ On the contribution of inferior collicular neurones to brainstem evoked responses in the guinea pig,” Rev. Laryngol. Otol. Rhinol. (Bord). 105, 157–162. [PubMed] [Google Scholar]
- 280. Palmer, A. R. , Winter, I. M. , and Darwin, C. J. (1986). “ The representation of steady-state vowel sounds in the temporal discharge patterns of the guinea pig cochlear nerve and primarylike cochlear nucleus neurons,” J. Acoust. Soc. Am. 79, 100–113. 10.1121/1.393633 [DOI] [PubMed] [Google Scholar]
- 281. Parisi, T. , and Ison, J. R. (1979). “ Development of the acoustic startle response in the rat: Ontogenetic changes in the magnitude of inhibition by prepulse stimulation,” Dev. Psychobiol. 12, 219–230. 10.1002/dev.420120305 [DOI] [PubMed] [Google Scholar]
- 282. Park, C. , and Kalinec, F. (2015). “ PKCalpha-mediated signals regulate the motile responses of cochlear outer hair cells,” Biophys. J. 108, 2171–2180. 10.1016/j.bpj.2015.03.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283. Pavlidis, P. , Maurer, J. , Apostolidou, E. , Kekes, G. , and Kouvelas, D. (2014). “ Memantine's action against aminoglycoside-induced ototoxicity,” Eur. Arch. Otorhinolaryngol. 271, 1491–1496. 10.1007/s00405-013-2647-1 [DOI] [PubMed] [Google Scholar]
- 284. Peake, W. T. , and Kiang, N. Y. (1962). “ Cochlear responses to condensation and rarefaction clicks,” Biophys. J. 2, 23–34. 10.1016/S0006-3495(62)86838-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285. Peng, J. H. , Tao, Z. Z. , and Huang, Z. W. (2007). “ Long-term sound conditioning increases distortion product otoacoustic emission amplitudes and decreases olivocochlear efferent reflex strength,” Neuroreport 18, 1167–1170. 10.1097/WNR.0b013e32820049a8 [DOI] [PubMed] [Google Scholar]
- 286. Perlman, H. B. , and Kimura, R. (1962). “ Cochlear blood flow in acoustic trauma,” Acta Otolaryngol. 54, 99–110. 10.3109/00016486209126927 [DOI] [PubMed] [Google Scholar]
- 287. Petersen, M. R. , Prosen, C. A. , Moody, D. B. , and Stebbins, W. C. (1977). “ Operant conditioning in the guinea pig,” J. Exp. Anal. Behav. 27, 529–532. 10.1901/jeab.1977.27-529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288. Pettigrew, A. M. , Liberman, M. C. , and Kiang, N. Y. (1984). “ Click-evoked gross potentials and single-unit thresholds in acoustically traumatized cats,” Ann. Otol. Rhinol. Laryngol. Suppl. 93, 83–96. 10.1177/00034894840930S416 [DOI] [PubMed] [Google Scholar]
- 289. Pfingst, B. E. , Colesa, D. J. , Hembrador, S. , Kang, S. Y. , Middlebrooks, J. C. , Raphael, Y. , and Su, G. L. (2011). “ Detection of pulse trains in the electrically stimulated cochlea: Effects of cochlear health,” J. Acoust. Soc. Am. 130, 3954–3968. 10.1121/1.3651820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290. Philibert, B. , Laudanski, J. , and Edeline, J. M. (2005). “ Auditory thalamus responses to guinea-pig vocalizations: A comparison between rat and guinea-pig,” Hear. Res. 209, 97–103. 10.1016/j.heares.2005.07.004 [DOI] [PubMed] [Google Scholar]
- 291. Philippens, I. H. , Melchers, B. P. , and Wolthuis, O. L. (1992). “ Active avoidance behavior in guinea pigs: Effects of physostigmine and scopolamine,” Pharmacol. Biochem. Behav. 42, 285–289. 10.1016/0091-3057(92)90528-N [DOI] [PubMed] [Google Scholar]
- 292. Pierre, P. V. , Engmer, C. , Wallin, I. , Laurell, G. , and Ehrsson, H. (2009). “ High concentrations of thiosulfate in scala tympani perilymph after systemic administration in the guinea pig,” Acta Otolaryngol. 129, 132–137. 10.1080/00016480802116232 [DOI] [PubMed] [Google Scholar]
- 293. Plontke, S. K. , Biegner, T. , Kammerer, B. , Delabar, U. , and Salt, A. N. (2008). “ Dexamethasone concentration gradients along scala tympani after application to the round window membrane,” Otol. Neurotol. 29, 401–406. 10.1097/MAO.0b013e318161aaae [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294. Poirrier, A. L. , Pincemail, J. , Van Den Ackerveken, P. , Lefebvre, P. P. , and Malgrange, B. (2010). “ Oxidative stress in the cochlea: An update,” Curr. Med. Chem. 17, 3591–3604. 10.2174/092986710792927895 [DOI] [PubMed] [Google Scholar]
- 295. Porter, J. H. , Sozer, N. N. , and Moeschl, T. P. (1977). “ Schedule-induced polydipsia in the guinea pig,” Physiol. Behav. 19, 573–575. 10.1016/0031-9384(77)90237-2 [DOI] [PubMed] [Google Scholar]
- 296. Pourbakht, A. , and Imani, A. (2012). “ The protective effect of conditioning on noise-induced hearing loss is frequency-dependent,” Acta Med. Iran. 50, 664–669. [PubMed] [Google Scholar]
- 297. Pourbakht, A. , and Yamasoba, T. (2003). “ Ebselen attenuates cochlear damage caused by acoustic trauma,” Hear. Res. 181, 100–108. 10.1016/S0378-5955(03)00178-3 [DOI] [PubMed] [Google Scholar]
- 298. Proctor, T. B. , Velde, T. M. , Dayal, V. S. , Bhattacharyya, T. K. , Artwohl, J. , and Towle, V. L. (1998). “ Auditory brain stem response in young and old guinea pigs,” Am. J. Otol. 19, 226–229. [PubMed] [Google Scholar]
- 299. Prosen, C. A. , Halpern, D. L. , and Dallos, P. (1989). “ Frequency difference limens in normal and sensorineural hearing impaired chinchillas,” J. Acoust. Soc. Am. 85, 1302–1313. 10.1121/1.397461 [DOI] [PubMed] [Google Scholar]
- 300. Prosen, C. A. , Moody, D. B. , Stebbins, W. C. , and Hawkins, J. E., Jr. (1981). “ Auditory intensity discrimination after selective loss of cochlear outer hair cells,” Science 212, 1286–1288. 10.1126/science.7233219 [DOI] [PubMed] [Google Scholar]
- 301. Prosen, C. A. , Moody, D. B. , Stebbins, W. C. , Smith, D. W. , Sommers, M. S. , Brown, J. N. , Altschuler, R. A. , and Hawkins, J. E., Jr. (1990). “ Apical hair cells and hearing,” Hear. Res. 44, 179–193. 10.1016/0378-5955(90)90079-5 [DOI] [PubMed] [Google Scholar]
- 302. Prosen, C. A. , Petersen, M. R. , Moody, D. B. , and Stebbins, W. C. (1978a). “ Auditory thresholds and kanamycin-induced hearing loss in the guinea pig assessed by a positive reinforcement procedure,” J. Acoust. Soc. Am. 63, 559–566. 10.1121/1.381754 [DOI] [PubMed] [Google Scholar]
- 303. Prosen, C. A. , Petersen, M. R. , Moody, D. B. , Stebbins, W. C. , and Hawkins, J. E., Jr. (1978b). “ Permanent threshold shift and cochlear hair cell loss in the kanamycin-treated guinea pig,” Otolaryngology 86, ORL-886-887. [DOI] [PubMed] [Google Scholar]
- 304. Puel, J. L. (1995). “ Chemical synaptic transmission in the cochlea,” Prog. Neurobiol. 47, 449–476. 10.1016/0301-0082(95)00028-3 [DOI] [PubMed] [Google Scholar]
- 305. Puel, J. L. , Ruel, J. , Gervais d'Aldin, C. , and Pujol, R. (1998). “ Excitotoxicity and repair of cochlear synapses after noise-trauma induced hearing loss,” Neuroreport 9, 2109–2114. 10.1097/00001756-199806220-00037 [DOI] [PubMed] [Google Scholar]
- 306. Puel, J. L. , Saffiedine, S. , Gervais d'Aldin, C. , Eybalin, M. , and Pujol, R. (1995). “ Synaptic regeneration and functional recovery after excitotoxic injury in the guinea pig cochlea,” C. R. Acad. Sci. III. 318, 67–75. [PubMed] [Google Scholar]
- 307. Pujol, R. , and Puel, J. L. (1999). “ Excitotoxicity, synaptic repair, and functional recovery in the mammalian cochlea: A review of recent findings,” Ann. N. Y. Acad. Sci. 884, 249–254. 10.1111/j.1749-6632.1999.tb08646.x [DOI] [PubMed] [Google Scholar]
- 308. Pujol, R. , Puel, J. L. , Gervais d'Aldin, C. , and Eybalin, M. (1993). “ Pathophysiology of the glutamatergic synapses in the cochlea,” Acta Otolaryngol. (Stockh). 113, 330–334. 10.3109/00016489309135819 [DOI] [PubMed] [Google Scholar]
- 309. Quesenberry, K. E. (1994). “ Guinea pigs,” Vet. Clin. North Am. Small Anim. Pract. 24, 67–87. 10.1016/S0195-5616(94)50003-2 [DOI] [PubMed] [Google Scholar]
- 310. Quirk, W. S. , Avinash, G. , Nuttall, A. L. , and Miller, J. M. (1992). “ The influence of loud sound on red blood cell velocity and blood vessel diameter in the cochlea,” Hear. Res. 63, 102–107. 10.1016/0378-5955(92)90079-3 [DOI] [PubMed] [Google Scholar]
- 311. Quirk, W. S. , and Seidman, M. D. (1995). “ Cochlear vascular changes in response to loud noise,” Am. J. Otol. 16, 322–325. [PubMed] [Google Scholar]
- 312. Quirk, W. S. , Shapiro, B. D. , Miller, J. M. , and Nuttall, A. L. (1991). “ Noise-induced changes in red blood cell velocity in lateral wall vessels of the rat cochlea,” Hear. Res. 52, 217–223. 10.1016/0378-5955(91)90201-J [DOI] [PubMed] [Google Scholar]
- 313. Rabbitt, R. D. , Ayliffe, H. E. , Christensen, D. , Pamarthy, K. , Durney, C. , Clifford, S. , and Brownell, W. E. (2005). “ Evidence of piezoelectric resonance in isolated outer hair cells,” Biophys. J. 88, 2257–2265. 10.1529/biophysj.104.050872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314. Radziwon, K. , Sheppard, A. , and Salvi, R. J. (2019). “ Psychophysical changes in temporal processing in chinchillas with noise-induced hearing loss,” J. Acoust. Soc. Am. 146, 3733–3742. 10.1121/1.5132292 [DOI] [PubMed] [Google Scholar]
- 315. Raje, S. S. , and Stewart, K. L. (2000). “ Group housing female guinea pigs,” Lab animal 29, 31–32. [DOI] [PubMed] [Google Scholar]
- 316. Reichenbach, T. , and Hudspeth, A. J. (2014). “ The physics of hearing: Fluid mechanics and the active process of the inner ear,” Rep. Prog. Phys. 77, 076601. 10.1088/0034-4885/77/7/076601 [DOI] [PubMed] [Google Scholar]
- 317. Reiter, E. R. , and Liberman, M. C. (1995). “ Efferent-mediated protection from acoustic overexposure: Relation to slow effects of olivocochlear stimulation,” J. Neurophysiol. 73, 506–514. 10.1152/jn.1995.73.2.506 [DOI] [PubMed] [Google Scholar]
- 318. Ren, T. , Nuttall, A. L. , and Miller, J. M. (1997). “ ATP-induced cochlear blood flow changes involve the nitric oxide pathway,” Hear. Res. 112, 87–94. 10.1016/S0378-5955(97)00109-3 [DOI] [PubMed] [Google Scholar]
- 319. Rodieck, R. W. , Kiang, N. Y. , and Gerstein, G. L. (1962). “ Some quantitative methods for the study of spontaneous activity of single neurons,” Biophys. J. 2, 351–368. 10.1016/S0006-3495(62)86860-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 320. Rubinstein, M. , and Pluznik, N. (1976). “ Effect of anesthesia on susceptibility to acoustic trauma,” Ann. Otol. Rhinol. Laryngol. 85, 276–280. 10.1177/000348947608500213 [DOI] [PubMed] [Google Scholar]
- 321. Ruebhausen, M. R. , Brozoski, T. J. , and Bauer, C. A. (2012). “ A comparison of the effects of isoflurane and ketamine anesthesia on auditory brainstem response (ABR) thresholds in rats,” Hear. Res. 287, 25–29. 10.1016/j.heares.2012.04.005 [DOI] [PubMed] [Google Scholar]
- 322. Ruel, J. , Wang, J. , Rebillard, G. , Eybalin, M. , Lloyd, R. , Pujol, R. , and Puel, J. L. (2007). “ Physiology, pharmacology and plasticity at the inner hair cell synaptic complex,” Hear. Res. 227, 19–27. 10.1016/j.heares.2006.08.017 [DOI] [PubMed] [Google Scholar]
- 323. Ryan, A. F. , Kujawa, S. G. , Hammill, T. , Le Prell, C. , and Kil, J. (2016). “ Temporary and permanent noise-induced threshold shifts: A review of basic and clinical observations,” Otol. Neurotol. 37, e271–e275. 10.1097/MAO.0000000000001071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324. Rybak, L. P. , and Brenner, M. J. (2015). “ Aminoglycoside-induced oxidative stress: Pathways and protection,” in Oxidative Stress in Applied Basic Research and Clinical Practice: Free Radicals in ENT Pathology, edited by Miller J. M., Le Prell C. G., and Rybak L. P. ( Humana Press, New York: ), pp. 195–216. [Google Scholar]
- 325. Sachs, M. B. , and Kiang, N. Y. (1968). “ Two-tone inhibition in auditory-nerve fibers,” J. Acoust. Soc. Am. 43, 1120–1128. 10.1121/1.1910947 [DOI] [PubMed] [Google Scholar]
- 326. Saha, S. , and Slepecky, N. B. (2000). “ Age-related changes in microtubules in the guinea pig organ of Corti. Tubulin isoform shifts with increasing age suggest changes in micromechanical properties of the sensory epithelium,” Cell Tissue Res. 300, 29–46. 10.1007/s004410050045 [DOI] [PubMed] [Google Scholar]
- 327. Salt, A. N. , Gill, R. M. , and Hartsock, J. J. (2015). “ Perilymph kinetics of FITC-dextran reveals homeostasis dominated by the cochlear aqueduct and cerebrospinal fluid,” J. Assoc. Res. Otolaryngol. 16, 357–371. 10.1007/s10162-015-0512-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328. Salt, A. N. , Hale, S. A. , and Plonkte, S. K. (2006). “ Perilymph sampling from the cochlear apex: A reliable method to obtain higher purity perilymph samples from scala tympani,” J. Neurosci. Methods 153, 121–129. 10.1016/j.jneumeth.2005.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329. Salt, A. N. , Hartsock, J. J. , Gill, R. M. , King, E. , Kraus, F. B. , and Plontke, S. K. (2016). “ Perilymph pharmacokinetics of locally-applied gentamicin in the guinea pig,” Hear. Res. 342, 101–111. 10.1016/j.heares.2016.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330. Salt, A. N. , Hartsock, J. J. , Gill, R. M. , Piu, F. , and Plontke, S. K. (2012). “ Perilymph pharmacokinetics of markers and dexamethasone applied and sampled at the lateral semi-circular canal,” J. Assoc. Res. Otolaryngol. 13, 771–783. 10.1007/s10162-012-0347-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331. Salt, A. N. , and Plontke, S. K. (2009). “ Principles of local drug delivery to the inner ear,” Audiol. Neurootol. 14, 350–360. 10.1159/000241892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332. Santarelli, R. , Arslan, E. , Carraro, L. , Conti, G. , Capello, M. , and Plourde, G. (2003). “ Effects of isoflurane on the auditory brainstem responses and middle latency responses of rats,” Acta Otolaryngol. 123, 176–181. 10.1080/0036554021000028108 [DOI] [PubMed] [Google Scholar]
- 333. Satake, M. , and Liberman, M. C. (1996). “ Morphological subclasses of lateral olivocochlear terminals? Ultrastructural analysis of inner spiral bundle in cat and guinea pig,” J. Comp. Neurol. 371, 621–632. [DOI] [PubMed] [Google Scholar]
- 334. Scheibe, F. , Haupt, H. , and Ludwig, C. (1993). “ Intensity-related changes in cochlear blood flow in the guinea pig during and following acoustic exposure,” Eur. Arch. Otorhinolaryngol. 250, 281–285. 10.1007/BF00186226 [DOI] [PubMed] [Google Scholar]
- 335. Schilling, A. , Krauss, P. , Gerum, R. , Metzner, C. , Tziridis, K. , and Schulze, H. (2017). “ A new statistical approach for the evaluation of gap-prepulse inhibition of the acoustic startle reflex (GPIAS) for tinnitus assessment,” Front. Behav. Neurosci. 11, 198. 10.3389/fnbeh.2017.00198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336. Sendowski, I. , Abaamrane, L. , Raffin, F. , Cros, A. , and Clarencon, D. (2006a). “ Therapeutic efficacy of intra-cochlear administration of methylprednisolone after acoustic trauma caused by gunshot noise in guinea pigs,” Hear. Res. 221, 119–127. 10.1016/j.heares.2006.08.010 [DOI] [PubMed] [Google Scholar]
- 337. Sendowski, I. , Raffin, F. , and Braillon-Cros, A. (2006b). “ Therapeutic efficacy of magnesium after acoustic trauma caused by gunshot noise in guinea pigs,” Acta Otolaryngol. 126, 122–129. 10.1080/00016480500312547 [DOI] [PubMed] [Google Scholar]
- 338. Sergeyenko, Y. , Lall, K. , Liberman, M. C. , and Kujawa, S. (2013). “ Age-related cochlear synaptopathy: An early-onset contributor to auditory functional decline,” J. Neurosci. 33, 13686–13694. 10.1523/JNEUROSCI.1783-13.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339. Sergi, B. , Fetoni, A. R. , Paludetti, G. , Ferraresi, A. , Navarra, P. , Mordente, A. , and Troiani, D. (2006). “ Protective properties of idebenone in noise-induced hearing loss in the guinea pig,” Neuroreport 17, 857–861. 10.1097/01.wnr.0000221834.18470.8c [DOI] [PubMed] [Google Scholar]
- 340. Sha, S. H. , and Schacht, J. (1997). “ Prevention of aminoglycoside-induced hearing loss,” Keio J. Med. 46, 115–119. 10.2302/kjm.46.115 [DOI] [PubMed] [Google Scholar]
- 341. Sha, S. H. , and Schacht, J. (1999). “ Salicylate attenuates gentamicin-induced ototoxicity,” Lab. Invest. 79, 807–813. [PubMed] [Google Scholar]
- 342. Sha, S. H. , and Schacht, J. (2000). “ Antioxidants attenuate gentamicin-induced free radical formation in vitro and ototoxicity in vivo: D-methionine is a potential protectant,” Hear. Res. 142, 34–40. 10.1016/S0378-5955(00)00003-4 [DOI] [PubMed] [Google Scholar]
- 343. Shafik, A. G. , Elkabarity, R. H. , Thabet, M. T. , Soliman, N. B. , and Kalleny, N. K. (2013). “ Effect of intratympanic dexamethasone administration on cisplatin-induced ototoxicity in adult guinea pigs,” Auris. Nasus. Larynx 40, 51–60. 10.1016/j.anl.2012.05.010 [DOI] [PubMed] [Google Scholar]
- 344. Shah, S. B. , Gladstone, H. B. , Williams, H. , Hradek, G. T. , and Schindler, R. A. (1995). “ An extended study: Protective effects of nerve growth factor in neomycin-induced auditory neural degeneration,” Am. J. Otol. 16, 310–314. [PubMed] [Google Scholar]
- 345. Sheppard, A. M. , Zhao, D. L. , and Salvi, R. (2018). “ Isoflurane anesthesia suppresses distortion product otoacoustic emissions in rats,” J. Otol. 13, 59–64. 10.1016/j.joto.2018.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346. Shi, L. , Liu, L. , He, T. , Guo, X. , Yu, Z. , Yin, S. , and Wang, J. (2013). “ Ribbon synapse plasticity in the cochleae of Guinea pigs after noise-induced silent damage,” PLoS One 8, e81566. 10.1371/journal.pone.0081566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347. Shi, Z. T. , Lin, Y. , Wang, J. , Wu, J. , Wang, R. F. , Chen, F. Q. , Mi, W. J. , and Qiu, J. H. (2014). “ G-CSF attenuates noise-induced hearing loss,” Neurosci. Lett. 562, 102–106. 10.1016/j.neulet.2013.07.033 [DOI] [PubMed] [Google Scholar]
- 348. Shibata, S. B. , Osumi, Y. , Yagi, M. , Kanda, S. , Kawamoto, K. , Kuriyama, H. , Nishiyama, T. , and Yamashita, T. (2007). “ Administration of amitriptyline attenuates noise-induced hearing loss via glial cell line-derived neurotrophic factor (GDNF) induction,” Brain Res. 1144, 74–81. 10.1016/j.brainres.2007.01.090 [DOI] [PubMed] [Google Scholar]
- 349. Shih, C. P. , Chen, H. C. , Lin, Y. C. , Chen, H. K. , Wang, H. , Kuo, C. Y. , Lin, Y. Y. , and Wang, C. H. (2019). “ Middle-ear dexamethasone delivery via ultrasound microbubbles attenuates noise-induced hearing loss,” Laryngoscope 129(8), 1907–1914. 10.1002/lary.27713 [DOI] [PubMed] [Google Scholar]
- 350. Shoji, F. , Miller, A. L. , Mitchell, A. , Yamasoba, T. , Altschuler, R. A. , and Miller, J. M. (2000a). “ Differential protective effects of neurotrophins in the attenuation of noise-induced hair cell loss,” Hear. Res. 146, 134–142. 10.1016/S0378-5955(00)00106-4 [DOI] [PubMed] [Google Scholar]
- 351. Shoji, F. , Yamasoba, T. , Magal, E. , Dolan, D. F. , Altschuler, R. A. , and Miller, J. M. (2000b). “ Glial cell line-derived neurotrophic factor has a dose dependent influence on noise-induced hearing loss in the guinea pig cochlea,” Hear. Res. 142, 41–55. 10.1016/S0378-5955(00)00007-1 [DOI] [PubMed] [Google Scholar]
- 352. Sinswat, P. , Wu, W. J. , Sha, S. H. , and Schacht, J. (2000). “ Protection from ototoxicity of intraperitoneal gentamicin in guinea pig,” Kidney Int. 58, 2525–2532. 10.1046/j.1523-1755.2000.00437.x [DOI] [PubMed] [Google Scholar]
- 353. Skellett, R. A. , Chen, C. , Fallon, M. , Nenov, A. P. , and Bobbin, R. P. (1997). “ Pharmacological evidence that endogenous ATP modulates cochlear mechanics,” Hear. Res. 111, 42–54. 10.1016/S0378-5955(97)00093-2 [DOI] [PubMed] [Google Scholar]
- 354. Skellett, R. A. , Cullen, J. K., Jr. , Fallon, M. , and Bobbin, R. P. (1998). “ Conditioning the auditory system with continuous vs. interrupted noise of equal acoustic energy: Is either exposure more protective?,” Hear. Res. 116, 21–32. 10.1016/S0378-5955(97)00199-8 [DOI] [PubMed] [Google Scholar]
- 355. Sly, D. J. , Campbell, L. , Uschakov, A. , Saief, S. T. , Lam, M. , and O'Leary, S. J. (2016). “ Applying neurotrophins to the round window rescues auditory function and reduces inner hair cell synaptopathy after noise-induced hearing loss,” Otol. Neurotol. 37, 1223–1230. 10.1097/MAO.0000000000001191 [DOI] [PubMed] [Google Scholar]
- 356. Smoorenburg, G. F. , De Groot, J. C. , Hamers, F. P. , and Klis, S. F. (1999). “ Protection and spontaneous recovery from cisplatin-induced hearing loss,” Ann. N. Y. Acad. Sci. 884, 192–210. 10.1111/j.1749-6632.1999.tb08642.x [DOI] [PubMed] [Google Scholar]
- 357. Song, B. B. , Anderson, D. J. , and Schacht, J. (1997). “ Protection from gentamicin ototoxicity by iron chelators in guinea pig in vivo,” J. Pharmacol. Exp. Ther. 282, 369–377. [PubMed] [Google Scholar]
- 358. Song, B. B. , and Schacht, J. (1996). “ Variable efficacy of radical scavengers and iron chelators to attenuate gentamicin ototoxicity in guinea pig in vivo,” Hear. Res. 94, 87–93. 10.1016/0378-5955(96)00003-2 [DOI] [PubMed] [Google Scholar]
- 359. Song, B. B. , Sha, S. H. , and Schacht, J. (1998). “ Iron chelators protect from aminoglycoside-induced cochleo- and vestibulo-toxicity,” Free Radic. Biol. Med. 25, 189–195. 10.1016/S0891-5849(98)00037-9 [DOI] [PubMed] [Google Scholar]
- 360. Song, Q. , Shen, P. , Li, X. , Shi, L. , Liu, L. , Wang, J. , Yu, Z. , Stephen, K. , Aiken, S. , Yin, S. , and Wang, J. (2016). “ Coding deficits in hidden hearing loss induced by noise: The nature and impacts,” Sci. Rep. 6, 25200. 10.1038/srep25200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361. Sorensen, H. (1959). “ Auditory adaptation in nerve action potentials recorded from the cochlea in guinea pigs,” Acta Otolaryngol. 50, 438–450. 10.3109/00016485909129217 [DOI] [PubMed] [Google Scholar]
- 362. Spankovich, C. , Griffiths, S. K. , Lobarinas, E. , Morgenstein, K. E. , de la Calle, S. , Ledon, V. , Guercio, D. , and Le Prell, C. G. (2014). “ Temporary threshold shift after impulse-noise during video game play: Laboratory data,” Int. J. Audiol. 53(2), S53–S65. 10.3109/14992027.2013.865844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363. Spankovich, C. , and Le Prell, C. G. (2019). “ The role of diet in vulnerability to noise-induced cochlear injury and hearing loss,” J. Acoust. Soc. Am. 146, 4033–4043. 10.1121/1.5132707 [DOI] [PubMed] [Google Scholar]
- 364. Sridhar, T. S. , Liberman, M. C. , Brown, M. C. , and Sewell, W. F. (1995). “ A novel cholinergic ‘slow effect’ of efferent stimulation on cochlear potentials in the guinea pig,” J. Neurosci. 15, 3667–3678. 10.1523/JNEUROSCI.15-05-03667.1995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365. Steadman, M. A. , and Sumner, C. J. (2018). “ Changes in neuronal representations of consonants in the ascending auditory system and their role in speech recognition,” Front Neurosci. 12, 671. 10.3389/fnins.2018.00671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366. Stebbins, W. C. (1982). “ Concerning the need for more sophisticated animal models in sensory behavioral toxicology,” Environ. Health Perspect. 44, 77–85. 10.1289/ehp.824477 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367. Stebbins, W. C. , Brown, C. H. , and Petersen, M. R. (1984). “ Sensory function in animals,” in Handbook of Physiology, Volume 3, Section 1: The Nervous System, edited by Darian-Smith I. ( American Physiological Society, Washington, DC: ), pp. 123–148. [Google Scholar]
- 368. Stebbins, W. C. , Moody, D. B. , and Serafin, J. V. (1982). “ Some principal issues in the analysis of noise effects on hearing in experimental animals,” Am. J. Otolaryngol. 3, 295–304. 10.1016/S0196-0709(82)80069-0 [DOI] [PubMed] [Google Scholar]
- 369. Stocks, R. M. , Gould, H. J. , Bush, A. J. , Dudney, B. W., Jr. , Pousson, M. , and Thompson, J. W. (2004). “ Ototoxic protection of sodium thiosulfate: Daily vs constant infusion,” Otolaryngol. Head Neck Surg. 131, 115–119. 10.1016/j.otohns.2004.02.022 [DOI] [PubMed] [Google Scholar]
- 370. Stronks, H. C. , Aarts, M. C. , and Klis, S. F. (2010). “ Effects of isoflurane on auditory evoked potentials in the cochlea and brainstem of guinea pigs,” Hear. Res. 260, 20–29. 10.1016/j.heares.2009.10.015 [DOI] [PubMed] [Google Scholar]
- 371. Strose, A. , Colombari, G. C. , Rossato, M. , Hyppolito, M. A. , and de Oliveira, J. A. (2014). “ Gentamicin conditioning confers auditory protection against noise trauma,” Eur. Arch. Otorhinolaryngol. 271, 2641–2648. 10.1007/s00405-013-2707-6 [DOI] [PubMed] [Google Scholar]
- 372. Su, G. L. , Colesa, D. J. , and Pfingst, B. E. (2008). “ Effects of deafening and cochlear implantation procedures on postimplantation psychophysical electrical detection thresholds,” Hear. Res. 241, 64–72. 10.1016/j.heares.2008.04.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373. Suarez, S. D. , and Gallup, G. G., Jr. (1982). “ Open-field behavior in guinea pigs: Developmental and adaptive considerations,” Behav. Proc. 7, 267–274. 10.1016/0376-6357(82)90042-0 [DOI] [PubMed] [Google Scholar]
- 374. Sueta, T. , Paki, B. , Everett, A. W. , and Robertson, D. (2003). “ Purinergic receptors in auditory neurotransmission,” Hear. Res. 183, 97–108. 10.1016/S0378-5955(03)00221-1 [DOI] [PubMed] [Google Scholar]
- 375. Suga, F. , Snow, J. B., Jr. , Preston, W. J. , and Glomset, J. L., Jr. (1967). “ Tonal patterns of cochlear impairment following intense stimulation with pure tones,” Laryngoscope 77, 784–805. 10.1288/00005537-196705000-00008 [DOI] [PubMed] [Google Scholar]
- 376. Sun, C. , Wang, X. , Chen, D. , Lin, X. , Yu, D. , and Wu, H. (2016). “ Dexamethasone loaded nanoparticles exert protective effects against Cisplatin-induced hearing loss by systemic administration,” Neurosci. Lett. 619, 142–148. 10.1016/j.neulet.2016.03.012 [DOI] [PubMed] [Google Scholar]
- 377. Sun, C. , Wang, X. , Zheng, Z. , Chen, D. , Wang, X. , Shi, F. , Yu, D. , and Wu, H. (2015). “ A single dose of dexamethasone encapsulated in polyethylene glycol-coated polylactic acid nanoparticles attenuates cisplatin-induced hearing loss following round window membrane administration,” Int. J. Nanomed. 10, 3567–3579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 378. Suta, D. , Kvasnak, E. , Popelar, J. , and Syka, J. (2003). “ Representation of species-specific vocalizations in the inferior colliculus of the guinea pig,” J. Neurophysiol. 90, 3794–3808. 10.1152/jn.01175.2002 [DOI] [PubMed] [Google Scholar]
- 379. Suta, D. , Popelar, J. , Burianova, J. , and Syka, J. (2013). “ Cortical representation of species-specific vocalizations in Guinea pig,” PloS One 8, e65432. 10.1371/journal.pone.0065432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380. Suta, D. , Popelar, J. , Kvasnak, E. , and Syka, J. (2007). “ Representation of species-specific vocalizations in the medial geniculate body of the guinea pig,” Exp. Brain Res. 183, 377–388. 10.1007/s00221-007-1056-3 [DOI] [PubMed] [Google Scholar]
- 381. Suta, D. , Popelar, J. , and Syka, J. (2008). “ Coding of communication calls in the subcortical and cortical structures of the auditory system,” Physiol. Res. 57(3), S149–S159. [DOI] [PubMed] [Google Scholar]
- 382. Suzuki, J. , Corfas, G. , and Liberman, M. C. (2016). “ Round-window delivery of neurotrophin 3 regenerates cochlear synapses after acoustic overexposure,” Sci. Rep. 6, 24907. 10.1038/srep24907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383. Syka, J. , Suta, D. , and Popelar, J. (2005). “ Responses to species-specific vocalizations in the auditory cortex of awake and anesthetized guinea pigs,” Hear. Res. 206, 177–184. 10.1016/j.heares.2005.01.013 [DOI] [PubMed] [Google Scholar]
- 384. Sziklai, I. , He, D. Z. , and Dallos, P. (1996). “ Effect of acetylcholine and GABA on the transfer function of electromotility in isolated outer hair cells,” Hear. Res. 95, 87–99. 10.1016/0378-5955(96)00026-3 [DOI] [PubMed] [Google Scholar]
- 385. Sziklai, I. , Szonyi, M. , and Dallos, P. (2001). “ Phosphorylation mediates the influence of acetylcholine upon outer hair cell electromotility,” Acta Otolaryngol. 121, 153–156. 10.1080/000164801300043280 [DOI] [PubMed] [Google Scholar]
- 386. Szonyi, M. , He, D. Z. , Ribari, O. , Sziklai, I. , and Dallos, P. (2001). “ Intracellular calcium and outer hair cell electromotility,” Brain Res. 922, 65–70. 10.1016/S0006-8993(01)03150-X [DOI] [PubMed] [Google Scholar]
- 387. Szucs, A. , Szappanos, H. , Batta, T. J. , Toth, A. , Szigeti, G. P. , Panyi, G. , Csernoch, L. , and Sziklai, I. (2006). “ Changes in purinoceptor distribution and intracellular calcium levels following noise exposure in the outer hair cells of the guinea pig,” J. Membr. Biol. 213, 135–141. 10.1007/s00232-006-0045-y [DOI] [PubMed] [Google Scholar]
- 388. Tabuchi, K. , Murashita, H. , Tobita, T. , Oikawa, K. , Tsuji, S. , Uemaetomari, I. , and Hara, A. (2005). “ Dehydroepiandrosterone sulfate reduces acoustic injury of the guinea-pig cochlea,” J. Pharmacol. Sci. 99, 191–194. 10.1254/jphs.SCZ050443 [DOI] [PubMed] [Google Scholar]
- 389. Takago, H. , and Oshima-Takago, T. (2018). “ Pre- and postsynaptic ionotropic glutamate receptors in the auditory system of mammals,” Hear. Res. 362, 1–13. 10.1016/j.heares.2018.02.007 [DOI] [PubMed] [Google Scholar]
- 390. Takemoto, T. , Sugahara, K. , Okuda, T. , Shimogori, H. , and Yamashita, H. (2004). “ The clinical free radical scavenger, edaravone, protects cochlear hair cells from acoustic trauma,” Eur. J. Pharmacol. 487, 113–116. 10.1016/j.ejphar.2004.01.019 [DOI] [PubMed] [Google Scholar]
- 391. Takemura, K. , Komeda, M. , Yagi, M. , Himeno, C. , Izumikawa, M. , Doi, T. , Kuriyama, H. , Miller, J. M. , and Yamashita, T. (2004). “ Direct inner ear infusion of dexamethasone attenuates noise-induced trauma in guinea pig,” Hear. Res. 196, 58–68. 10.1016/j.heares.2004.06.003 [DOI] [PubMed] [Google Scholar]
- 392. Tanaka, K. , Takemoto, T. , Sugahara, K. , Okuda, T. , Mikuriya, T. , Takeno, K. , Hashimoto, M. , Shimogori, H. , and Yamashita, H. (2005). “ Post-exposure administration of edaravone attenuates noise-induced hearing loss,” Eur. J. Pharmacol. 522, 116–121. 10.1016/j.ejphar.2005.08.026 [DOI] [PubMed] [Google Scholar]
- 393. Tasaki, I. (1954). “ Nerve impulses in individual auditory nerve fibers of guinea pig,” J. Neurophysiol. 17, 97–122. 10.1152/jn.1954.17.2.97 [DOI] [PubMed] [Google Scholar]
- 394. Tasaki, I. , Davis, H. , and Legouix, J.-P. (1952). “ The space-time pattern of the cochlear microphonics (guinea pig), as recorded by differential electrodes,” J. Acoust. Soc. Am. 24, 502–519. 10.1121/1.1906928 [DOI] [Google Scholar]
- 395. Tate, A. D. , Antonelli, P. J. , Hannabass, K. R. , and Dirain, C. O. (2017). “ Mitochondria-targeted antioxidant mitoquinone reduces cisplatin-induced ototoxicity in guinea pigs,” Otolaryngol. Head Neck Surg. 156, 543–548. 10.1177/0194599816678381 [DOI] [PubMed] [Google Scholar]
- 396. Thomsen, E. , and Pakkenberg, H. (1962). “ Cytoplasmic basophilia in the spiral ganglion of the guinea-pig immediately following acoustic stress,” Acta Otolaryngol. 55, 260–268. 10.3109/00016486209127361 [DOI] [PubMed] [Google Scholar]
- 397. Thorne, P. R. , Munoz, D. J. , and Housley, G. D. (2004). “ Purinergic modulation of cochlear partition resistance and its effect on the endocochlear potential in the Guinea pig,” J. Assoc. Res. Otolaryngol. 5, 58–65. 10.1007/s10162-003-4003-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 398. Thorne, P. R. , and Nuttall, A. L. (1987). “ Laser Doppler measurements of cochlear blood flow during loud sound exposure in the guinea pig,” Hear. Res. 27, 1–10. 10.1016/0378-5955(87)90021-9 [DOI] [PubMed] [Google Scholar]
- 399. Tona, Y. , Hamaguchi, K. , Ishikawa, M. , Miyoshi, T. , Yamamoto, N. , Yamahara, K. , Ito, J. , and Nakagawa, T. (2014). “ Therapeutic potential of a gamma-secretase inhibitor for hearing restoration in a guinea pig model with noise-induced hearing loss,” BMC Neurosci. 15, 66. 10.1186/1471-2202-15-66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400. Trevino, M. , Lobarinas, E. , Maulden, A. C. , and Heinz, M. G. (2019). “ The chinchilla animal model for hearing science and noise-induced hearing loss,” J. Acoust. Soc. Am. 146, 3710–3732. 10.1121/1.5132950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401. Tsuji, J. , and Liberman, M. C. (1997). “ Intracellular labeling of auditory nerve fibers in guinea pig: Central and peripheral projections,” J. Comp. Neurol. 381, 188–202. [DOI] [PubMed] [Google Scholar]
- 402. Turner, J. , Larsen, D. , Hughes, L. , Moechars, D. , and Shore, S. (2012). “ Time course of tinnitus development following noise exposure in mice,” J. Neurosci. Res. 90, 1480–1488. 10.1002/jnr.22827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403. Turner, J. G. , Brozoski, T. J. , Bauer, C. A. , Parrish, J. L. , Myers, K. , Hughes, L. F. , and Caspary, D. M. (2006). “ Gap detection deficits in rats with tinnitus: A potential novel screening tool,” Behav. Neurosci. 120, 188–195. 10.1037/0735-7044.120.1.188 [DOI] [PubMed] [Google Scholar]
- 404. Upton, M. (1929). “ Functional disturbances of hearing in guinea pigs after long exposure to an intense tone,” Proc. Natl. Acad. Sci. U.S.A. 15, 284–287. 10.1073/pnas.15.3.284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 405. Urbain, C. , Poling, A. , and Thompson, T. (1979). “ Differing effects of intermittent food delivery on interim behavior in guinea pigs and rats,” Physiol. Behav. 22, 621–625. 10.1016/0031-9384(79)90219-1 [DOI] [PubMed] [Google Scholar]
- 406. Vetter, D. E. , Adams, J. C. , and Mugnaini, E. (1991). “ Chemically distinct rat olivocochlear neurons,” Synapse 7, 21–43. 10.1002/syn.890070104 [DOI] [PubMed] [Google Scholar]
- 407. Vetter, D. E. , and Mugnaini, E. (1992). “ Distribution and dendritic features of three groups of rat olivocochlear neurons. A study with two retrograde cholera toxin tracers,” Anat. Embryol. (Berl). 185, 1–16. 10.1007/BF00213596 [DOI] [PubMed] [Google Scholar]
- 408. von der Behrens, W. (2014). “ Animal models of subjective tinnitus,” Neural Plast. 2014, 741452. 10.1155/2014/741452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409. Wada, S. I. , and Starr, A. (1983a). “ Generation of auditory brain stem responses (ABRs). I. Effects of injection of a local anesthetic (procaine HCI) into the trapezoid body of guinea pigs and cat,” Electroencephalogr. Clin. Neurophysiol. 56, 326–339. 10.1016/0013-4694(83)90259-6 [DOI] [PubMed] [Google Scholar]
- 410. Wada, S. I. , and Starr, A. (1983b). “ Generation of auditory brain stem responses (ABRs). II. Effects of surgical section of the trapezoid body on the ABR in guinea pigs and cat,” Electroencephalogr. Clin. Neurophysiol. 56, 340–351. 10.1016/0013-4694(83)90260-2 [DOI] [PubMed] [Google Scholar]
- 411. Wada, S. I. , and Starr, A. (1983c). “ Generation of auditory brain stem responses (ABRs). III. Effects of lesions of the superior olive, lateral lemniscus and inferior colliculus on the ABR in guinea pig,” Electroencephalogr. Clin. Neurophysiol. 56, 352–366. 10.1016/0013-4694(83)90261-4 [DOI] [PubMed] [Google Scholar]
- 412. Waissbluth, S. , Salehi, P. , He, X. , and Daniel, S. J. (2013). “ Systemic dexamethasone for the prevention of cisplatin-induced ototoxicity,” Eur. Arch. Otorhinolaryngol. 270, 1597–1605. 10.1007/s00405-012-2150-0 [DOI] [PubMed] [Google Scholar]
- 413. Wallace, M. N. , Shackleton, T. M. , Anderson, L. A. , and Palmer, A. R. (2005). “ Representation of the purr call in the guinea pig primary auditory cortex,” Hear. Res. 204, 115–126. 10.1016/j.heares.2005.01.007 [DOI] [PubMed] [Google Scholar]
- 414. Walloch, R. A. , and Taylor-Spikes, M. (1976). “ Auditory thresholds in the guinea pig: A preliminary report of a behavioral technique employing a food reward,” Laryngoscope 86, 1699–1705. 10.1288/00005537-197611000-00012 [DOI] [PubMed] [Google Scholar]
- 415. Wan, G. , and Corfas, G. (2015). “ No longer falling on deaf ears: Mechanisms of degeneration and regeneration of cochlear ribbon synapses,” Hear. Res. 329, 1–10. 10.1016/j.heares.2015.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416. Wan, G. , Gomez-Casati, M. E. , Gigliello, A. R. , Liberman, M. C. , and Corfas, G. (2014). “ Neurotrophin-3 regulates ribbon synapse density in the cochlea and induces synapse regeneration after acoustic trauma,” eLife 3, e03564. 10.7554/eLife.03564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 417. Wang, J. , Ladrech, S. , Pujol, R. , Brabet, P. , Van De Water, T. R. , and Puel, J. L. (2004). “ Caspase inhibitors, but not c-Jun NH2-terminal kinase inhibitor treatment, prevent cisplatin-induced hearing loss,” Cancer Res. 64, 9217–9224. 10.1158/0008-5472.CAN-04-1581 [DOI] [PubMed] [Google Scholar]
- 418. Wang, J. , Lloyd Faulconbridge, R. V. , Fetoni, A. , Guitton, M. J. , Pujol, R. , and Puel, J. L. (2003a). “ Local application of sodium thiosulfate prevents cisplatin-induced hearing loss in the guinea pig,” Neuropharmacology 45, 380–393. 10.1016/S0028-3908(03)00194-1 [DOI] [PubMed] [Google Scholar]
- 419. Wang, J. , Pignol, B. , Chabrier, P. E. , Saido, T. , Lloyd, R. , Tang, Y. , Lenoir, M. , and Puel, J. L. (2007a). “ A novel dual inhibitor of calpains and lipid peroxidation (BN82270) rescues the cochlea from sound trauma,” Neuropharmacology 52, 1426–1437. 10.1016/j.neuropharm.2007.02.007 [DOI] [PubMed] [Google Scholar]
- 420. Wang, J. , Ruel, J. , Ladrech, S. , Bonny, C. , van de Water, T. R. , and Puel, J. L. (2007b). “ Inhibition of the c-Jun N-terminal kinase-mediated mitochondrial cell death pathway restores auditory function in sound-exposed animals,” Mol. Pharmacol. 71, 654–666. 10.1124/mol.106.028936 [DOI] [PubMed] [Google Scholar]
- 421. Wang, J. , Van De Water, T. R. , Bonny, C. , de Ribaupierre, F. , Puel, J. L. , and Zine, A. (2003b). “ A peptide inhibitor of c-Jun N-terminal kinase protects against both aminoglycoside and acoustic trauma-induced auditory hair cell death and hearing loss,” J. Neurosci. 23, 8596–8607. 10.1523/JNEUROSCI.23-24-08596.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422. Wang, J. , Wang, Y. , Chen, X. , Zhang, P. Z. , Shi, Z. T. , Wen, L. T. , Qiu, J. H. , and Chen, F. Q. (2015). “ Histone deacetylase inhibitor sodium butyrate attenuates gentamicin-induced hearing loss in vivo,” Am. J. Otolaryngol. 36, 242–248. 10.1016/j.amjoto.2014.11.003 [DOI] [PubMed] [Google Scholar]
- 423. Wang, L. , Li, J. , Yu, L. , and Li, X. (2014). “ Regulation of dopamine D2 receptors in the guinea pig cochlea,” Acta Otolaryngol 134, 738–743. 10.3109/00016489.2014.899712 [DOI] [PubMed] [Google Scholar]
- 424. Wang, Y. , and Ren, C. (2012). “ Effects of repeated ‘benign’ noise exposures in young CBA mice: Shedding light on age-related hearing loss,” J. Assoc. Res. Otolaryngol. 13, 505–515. 10.1007/s10162-012-0329-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 425. Warr, W. B. , Boche, J. B. , and Neely, S. T. (1997). “ Efferent innervation of the inner hair cell region: Origins and terminations of two lateral olivocochlear systems,” Hear. Res. 108, 89–111. 10.1016/S0378-5955(97)00044-0 [DOI] [PubMed] [Google Scholar]
- 426. Watanabe, K. I. , Hess, A. , Bloch, W. , and Michel, O. (2000). “ Nitric oxide synthase inhibitor suppresses the ototoxic side effect of cisplatin in guinea pigs,” Anticancer. Drugs 11, 401–406. 10.1097/00001813-200006000-00011 [DOI] [PubMed] [Google Scholar]
- 427. Waters, C. (1999). “ Molecular mechanisms of cell death in the ear,” Ann. N. Y. Acad. Sci. 884, 41–51. 10.1111/j.1749-6632.1999.tb08634.x [DOI] [PubMed] [Google Scholar]
- 428. Webster, C. D. , Brimer, C. J. , and Evonic, I. N. (1965). “ Factors affecting intersession faciliation of avoidance learning in guinea pigs,” Psych. Sci. 3, 291–292. 10.3758/BF03343142 [DOI] [Google Scholar]
- 429. Webster, C. D. , and Rabedeau, R. G. (1964). “ The effect of intersession interval in shuttle-box conditioning of the guinea pig,” Psych. Sci. 1, 73–74. 10.3758/BF03342796 [DOI] [Google Scholar]
- 430. Wen, J. , Duan, N. , Wang, Q. , Jing, G. X. , and Xiao, Y. (2017). “ Protective effect of propofol on noise-induced hearing loss,” Brain Res. 1657, 95–100. 10.1016/j.brainres.2016.12.005 [DOI] [PubMed] [Google Scholar]
- 431. Wersinger, E. , and Fuchs, P. A. (2011). “ Modulation of hair cell efferents,” Hear. Res. 279, 1–12. 10.1016/j.heares.2010.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432. Wever, E. G. , Vernon, J. A. , and Peterson, E. A. (1963). “ The high-frequency sensitivity of the guinea pig ear,” Proc. Natl. Acad. Sci. U.S.A. 49, 319–322. 10.1073/pnas.49.3.319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 433. White, J. S. , and Warr, W. B. (1983). “ The dual origins of the olivocochlear bundle in the albino rat,” J. Comp. Neurol. 219, 203–214. 10.1002/cne.902190206 [DOI] [PubMed] [Google Scholar]
- 434. Wilson, M. J. , Kelly-Ballweber, D. , and Dobie, R. A. (1985). “ Binaural interaction in auditory brain stem responses: Parametric studies,” Ear Hear. 6, 80–88. 10.1097/00003446-198503000-00004 [DOI] [PubMed] [Google Scholar]
- 435. Wu, W. J. , Sha, S. H. , McLaren, J. D. , Kawamoto, K. , Raphael, Y. , and Schacht, J. (2001). “ Aminoglycoside ototoxicity in adult CBA, C57BL and BALB mice and the Sprague-Dawley rat,” Hear. Res. 158, 165–178. 10.1016/S0378-5955(01)00303-3 [DOI] [PubMed] [Google Scholar]
- 436. Xiong, M. , He, Q. , Lai, H. , and Wang, J. (2011). “ Oxidative stress in spiral ganglion cells of pigmented and albino guinea pigs exposed to impulse noise,” Acta Otolaryngol. 131, 914–920. 10.3109/00016489.2011.577448 [DOI] [PubMed] [Google Scholar]
- 437. Yamashita, D. , Jiang, H. Y. , Le Prell, C. G. , Schacht, J. , and Miller, J. M. (2005). “ Post-exposure treatment attenuates noise-induced hearing loss,” Neuroscience 134, 633–642. 10.1016/j.neuroscience.2005.04.015 [DOI] [PubMed] [Google Scholar]
- 438. Yamasoba, T. , Dolan, D. F. , and Miller, J. M. (1999a). “ Acquired resistance to acoustic trauma by sound conditioning is primarily mediated by changes restricted to the cochlea, not by systemic responses,” Hear. Res. 127, 31–40. 10.1016/S0378-5955(98)00178-6 [DOI] [PubMed] [Google Scholar]
- 439. Yamasoba, T. , Nuttall, A. L. , Harris, C. , Raphael, Y. , and Miller, J. M. (1998). “ Role of glutathione in protection against noise-induced hearing loss,” Brain Res. 784, 82–90. 10.1016/S0006-8993(97)01156-6 [DOI] [PubMed] [Google Scholar]
- 440. Yamasoba, T. , Pourbakht, A. , Sakamoto, T. , and Suzuki, M. (2005). “ Ebselen prevents noise-induced excitotoxicity and temporary threshold shift,” Neurosci. Lett. 380, 234–238. 10.1016/j.neulet.2005.01.047 [DOI] [PubMed] [Google Scholar]
- 441. Yamasoba, T. , Schacht, J. , Shoji, F. , and Miller, J. M. (1999b). “ Attenuation of cochlear damage from noise trauma by an iron chelator, a free radical scavenger and glial cell line-derived neurotrophic factor in vivo,” Brain Res. 815, 317–325. 10.1016/S0006-8993(98)01100-7 [DOI] [PubMed] [Google Scholar]
- 442. Yang, D. H. , Xie, J. , Liu, K. , Peng, Z. , Guo, J. Y. , Yu, S. K. , Wang, G. P. , and Gong, S. S. (2017). “ The histone deacetylase inhibitor sodium butyrate protects against noise-induced hearing loss in Guinea pigs,” Neurosci. Lett. 660, 140–146. 10.1016/j.neulet.2017.09.036 [DOI] [PubMed] [Google Scholar]
- 443. Yarto-Jaramillo, E. (2011). “ Respiratory system anatomy, physiology, and disease: Guinea pigs and chinchillas,” Veterin. Clin. North Am. 14, 339–355. [DOI] [PubMed] [Google Scholar]
- 444. Young, J. S. , and Fechter, L. D. (1983). “ Reflex inhibition procedures for animal audiometry: A technique for assessing ototoxicity,” J. Acoust. Soc. Am. 73, 1686–1693. 10.1121/1.389391 [DOI] [PubMed] [Google Scholar]
- 445. Yu, F. , Hao, S. , Yang, B. , Zhao, Y. , and Yang, J. (2016). “ Low iron diet increases susceptibility to noise-induced hearing loss in young rats,” Nutrients 8(8), 456. 10.3390/nu8080456 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 446. Yu, N. , and Zhao, H. B. (2008). “ ATP activates P2x receptors and requires extracellular Ca(++) participation to modify outer hair cell nonlinear capacitance,” Pflugers Arch. 457, 453–461. 10.1007/s00424-008-0522-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 447. Zhai, S. Q. , Cheng, J. C. , Wang, J. L. , Yang, W. Y. , Gu, R. , and Jiang, S. C. (2002). “ Protective effect of basic fibroblast growth factor on auditory hair cells after noise exposure,” Acta Otolaryngol. 122, 370–373. 10.1080/00016480260000030 [DOI] [PubMed] [Google Scholar]
- 448. Zhai, S. Q. , Wang, D. J. , Wang, J. L. , Han, D. Y. , and Yang, W. Y. (2004). “ Basic fibroblast growth factor protects auditory neurons and hair cells from glutamate neurotoxicity and noise exposure,” Acta Otolaryngol. 124, 124–129. 10.1080/00016480310015939 [DOI] [PubMed] [Google Scholar]
- 449. Zhang, J. (2019). “ Blast-induced tinnitus: Animal models,” J. Acoust. Soc. Am. 146, 3811–3831. 10.1121/1.5132551 [DOI] [PubMed] [Google Scholar]
- 450. Zhang, L. , Wu, C. , Martel, D. T. , West, M. , Sutton, M. A. , and Shore, S. E. (2019). “ Remodeling of cholinergic input to the hippocampus after noise exposure and tinnitus induction in Guinea pigs,” Hippocampus. 29(8), 669–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 451. Zhang, M. , Kalinec, G. M. , Urrutia, R. , Billadeau, D. D. , and Kalinec, F. (2003). “ ROCK-dependent and ROCK-independent control of cochlear outer hair cell electromotility,” J. Biol. Chem. 278, 35644–35650. 10.1074/jbc.M301668200 [DOI] [PubMed] [Google Scholar]
- 452. Zhao, J. , Sun, J. , and Liu, Y. (2012). “ Effects of carbogen on cochlear blood flow and hearing function following acute acoustic trauma in guinea pigs,” Arch. Med. Res. 43, 530–535. 10.1016/j.arcmed.2012.10.003 [DOI] [PubMed] [Google Scholar]
- 453. Zhou, N. , Kraft, C. T. , Colesa, D. J. , and Pfingst, B. E. (2015). “ Integration of pulse trains in humans and guinea pigs with cochlear implants,” J. Assoc. Res. Otolaryngol. 16, 523–534. 10.1007/s10162-015-0521-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 454. Zhou, Y. , Zheng, H. , Shen, X. , Zhang, Q. , and Yang, M. (2009). “ Intratympanic administration of methylprednisolone reduces impact of experimental intensive impulse noise trauma on hearing,” Acta Otolaryngol. 129, 602–607. 10.1080/00016480802342424 [DOI] [PubMed] [Google Scholar]
- 455. Zhu, Y. , and Zhao, H. B. (2012). “ ATP activates P2X receptors to mediate gap junctional coupling in the cochlea,” Biochem. Biophys. Res. Commun. 426, 528–532. 10.1016/j.bbrc.2012.08.119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456. Zine, A. , and van de Water, T. R. (2004). “ The MAPK/JNK signalling pathway offers potential therapeutic targets for the prevention of acquired deafness,” Curr. Drug Targ. CNS Neurol. Disord. 3, 325–332. 10.2174/1568007043337166 [DOI] [PubMed] [Google Scholar]
- 457. Zuo, H. , Cui, B. , She, X. , and Wu, M. (2008). “ Changes in Guinea pig cochlear hair cells after sound conditioning and noise exposure,” J. Occup. Health 50, 373–379. 10.1539/joh.L8032 [DOI] [PubMed] [Google Scholar]