ABSTRACT |
Background:
Skin diseases account for more than 35% of occupational diseases, affecting 1/1,000 workers annually.
Objective:
To characterize occupational dermatoses affecting hospital workers and identify possible triggers and susceptibility factors.
Methods:
Cross-sectional study in which we analyzed information extracted from electronic medical records of workers who performed periodic examinations in the course of one year.
Results:
About 3.56% of 1,741 included workers had a diagnosis of occupational dermatosis, being mainly women (76.85%). Thirty-four (54.84%) of the affected workers had irritant contact dermatitis, 17 (27.42%) latex allergy, 6 (9.68%) allergic dermatitis, and 5 (8.06%) two concomitant conditions. We found significant difference in prevalence as a function of occupational group (p=0.008), being highest for nursing assistants (5.11%). Prevalence was also higher for employees allocated to surgery departments (8.47%, p=0.001). Main triggers were skin disinfectants, latex, nitrile gloves, and prolonged contact with water (4.84%).
Conclusion:
The quality of the analyzed data depends on the quality of the analyzed medical records. Most subjects were nursing assistants, which fact hinders the generalization of the results. The prevalence of occupational dermatosis was just 3.56%, which might be explained by previously implemented preventive measures. The employees most frequently affected were those allocated to surgery departments and nursing assistants. Skin disinfectants were the most frequent triggers.
Keywords |: dermatitis, occupational; dermatitis, contact; latex; urticarial
RESUMO |
Introdução:
As patologias cutâneas representam mais de 35% das doenças relacionadas com o trabalho, afetando anualmente 1/1.000 trabalhadores.
Objetivos:
Caracterizar as dermatoses associadas ao trabalho em profissionais de um centro hospitalar e identificar possíveis agentes desencadeantes e fatores de suscetibilidade.
Métodos:
Estudo transversal com recolha da informação registrada no processo clínico eletrônico dos trabalhadores observados em exame de saúde periódico no período de um ano.
Resultados:
Nos 1.741 trabalhadores estudados, 3,56% tinham registro de dermatoses associadas ao trabalho, a maioria mulheres (76,85%). Dos profissionais com dermatoses, 34 (54,84%) tinham dermatite de contato irritativa, 17 (27,42%) urticária ao látex, seis (9,68%) dermatite de contato alérgica e cinco (8,06%) duas dermatoses concomitantes. Encontrou-se diferença estatisticamente significativa entre os vários grupos profissionais (p=0,008), sendo os auxiliares de enfermagem os mais afetados (5,11%). Verificou-se também maior prevalência (8,47%) em profissionais de blocos operatórios (p=0,001). Os principais agentes desencadeantes foram desinfetantes cutâneos, látex, luvas de nitrilo e contato prolongado com água (4,84%).
Conclusões:
Por tratar-se de um estudo baseado em registros clínicos, a informação está dependente da qualidade destes. Para além disso, os auxiliares de enfermagem foram a maioria representada na amostra no que se refere à população do centro hospitalar, o que limita a extrapolação dos resultados. Este estudo encontrou prevalência de dermatoses de somente 3,56%, o que talvez se deva à implementação de medidas preventivas. Os profissionais mais afetados foram os de blocos operatórios e os auxiliares de enfermagem. Os desinfetantes cutâneos foram os principais agentes apontados como desencadeantes.
INTRODUCTION
Skin disorders account for more than 35% of work-related diseases worldwide, affecting 1/1,000 workers annually1. Contact dermatitis (eczema) represents about 90% of occupational dermatoses2,3.
Healthcare workers are particularly susceptible to this type of skin disorders4-8 as a function of their frequent contact with a large number of potential irritants and sensitizing agents, as e.g. rubber gloves and disinfectants5-9.
Most cases of contact dermatitis are of the irritant type1,5. The involved substance disrupts the stratum corneum, penetrates into the deeper layers of the skin, and damages the keratinocytes1,10,11. In turn, skin lesions in allergic contact dermatitis are caused by delayed-type hypersensitivity DTH (type IV)8,11. Irritant contact dermatitis not seldom precedes allergic dermatitis12-14. Contact urticaria to latex is significant among healthcare workers. While the underlying pathophysiological mechanism seems to be different than that of irritant and allergic contact dermatitis, it exhibits high global prevalence among healthcare workers, of 10 to 17%15-20.
In all the aforementioned cases, occurrence of disease is not only related to the type and intensity of exposure, but also to individual susceptibility. Atopy is the most common predisposing factor, present in up to 20% of cases21-24.
The aim of the present study was to identify and characterize cases of occupational dermatoses among workers in a university hospital center. We further sought to define possible triggers, factors related to individual susceptibility and others potentially related to occurrence of disease.
METHODS
The present cross-sectional study was based on information collected from electronic medical records of employees of a university hospital center. The study population consisted of all employees who performed periodical health examinations at the hospital occupational health department (OHD) in the course of one year (1 May 2017 to 20 April 2018) to a total of 1,741. We reviewed OHD records, which include all clinical information on employees for the past 10 years, considering: sociodemographic data (sex, age), occupational group, hospital department, length in the current job, personal history of atopy, contact dermatitis and latex allergy, dermatitis triggers, relationship between complaints and work (aggravation after exposure, improvement during time off work). We further recorded results of skin allergy tests indicated by dermatologists to workers with symptoms suggestive of contact dermatitis.
As personal history of atopy we considered allergic rhinitis, atopic eczema and allergic asthma. In regard to contact urticaria to latex, we considered all the cases in which this condition was registered in the medical records independently from the date of and presence of signs on the last periodical medical examination. Diagnosis of contact dermatitis was based on clinical findings and skin testing results. For allergic dermatitis, sensitizing agents were investigated my means of DTH skin testing. For irritant contact dermatitis, causal agents were presumably established based on aggravation following contact with definite materials or equipment. For latex allergy, diagnosis was based on its typical clinical presentation in association with specific IgE antibody or a positive DHT skin test.
The present study — which involved reviewing medical records and use of the corresponding data — was approved by the institutional ethics committee, OHD board, and the dermatology department chair.
In statistical analysis we used the Kolmogorov-Smirnov test to investigate the distribution of numerical variables. Association among categorical variables was analyzed with the χ2 and Fisher’s exact tests; mean values for nonparametric numerical variables were compared with the Mann-Whitney test. The significance level was set to 5%. Analysis was performed with software Microsoft Excel and IBM Statistical Package for the Social Sciences (SPSS).
RESULTS
Of 6,375 hospital employees, 1,741 (27.31%) were included in the present study. The average age of the sample was 41 (interquartile range=21) years old; 76.85% (n=1,338) were female. About 29.24% (n=509) of the subjects were nursing assistants, 23.89% (n=416) nurses, 20.51% (n=357) physicians, 11.66% (n=203) administrative employees, 8.21% (n=143) diagnosis and therapeutics technicians, and 6.49% (n=113) other types of technicians (Table 1).
Table 1. Sample characterization, Lisbon, Portugal, 2018 (n=1,741).
| Sex | |
|---|---|
| Female | 1,338 (76.85%) |
| Male | 403 (23.15%) |
| Age | |
| Median (interquartile range) | 41 (21) years old |
| Years in current job | |
| Median (interquartile range) | 11 (17) years |
| Job | |
| Administration | 203 (11.66%) |
| Nursing assistants | 509 (29.24%) |
| Nurses | 416 (23.89%) |
| Physicians | 357 (20.51%) |
| Diagnosis and therapeutics technicians | 143 (8.21%) |
| Other technicians | 113 (6.49%) |
| Total | n=1,741 (100%) |
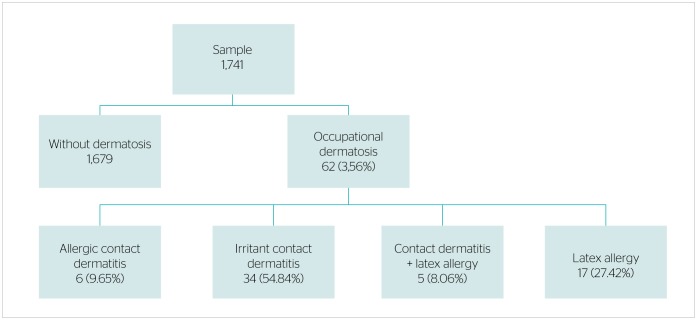
The prevalence of occupational dermatoses was 3.56% (n=62), most cases corresponded to females (82.26%). Nursing assistants (41.94%), nurses (32.26%) and physicians (19.35%) were the most frequently affected occupational groups. Forty-nine (79.03%) among these professionals were allocated to wards or outpatient clinics, 10 (14.13%) to surgery departments, and 3 (4.84%) to support services.
Of the group with occupational dermatosis, 34 workers (54.84%) had a diagnosis of irritant contact dermatitis, 17 (27.42%) of latex allergy, 6 (9.68%) of allergic dermatitis, and 5 (8.06%) of two of these conditions simultaneously — 4 cases of latex allergy and irritant contact dermatitis, and one of latex allergy and allergic dermatitis (Figure 1). About 2.18% of the sample exhibited irritant contact dermatitis, 0.40% allergic dermatitis, and 1.26% latex allergy.
Figure 1.
Number of workers with occupational dermatoses, Lisbon, Portugal, 2018 (n=1,741).
The proportion of women was higher among the workers with dermatosis compared to those without this condition (82.26% vs. 76.65%), but this difference was not statistically significant (p=0.304). These two groups neither differed as a function of age (p=0.363) or years in the job (median 9.5 vs. 11 years, p=0.791).
The prevalence of occupational dermatoses was highest among nursing technicians (5.11%), followed by nurses (4.81%) and physicians (3.36%). Difference in prevalence per occupational group was statistically significant (p=0.008).
The proportion of cases of dermatoses was higher among the employees allocated to surgery departments compared to clinical departments and support services (8.47%, 3.70% and 0.74%, respectively); this difference was statistically significant (p=0.001).
Cases of dermatoses were more frequent among workers with personal history of atopy (4.96% vs. 3.12%), but this difference was not statistically significant (p=0.107). On separate comparisons between personal history of atopy and type of dermatosis (irritant contact dermatitis, allergic dermatitis, latex allergy) we did not find any statistically significant relationship (p=1.000, p=0.389 and p=0.778, respectively) (Table 2).
Table 2. Characteristics of employees with or without dermatosis, Lisbon, Portugal, 2018 (n=1,741).
| With dermatosis n=62 | Without dermatosisn=1,679 | p | |
|---|---|---|---|
| Sex* | |||
| Female | 51 (3.81%) | 1,287 (96.19%) | 0.304 |
| Male | 11 (2.73%) | 392 (97.27%) | |
| Age** | |||
| Median (interquartile range) | 39 (22.25) years old | 41 (21) years old | 0.363 |
| Years in current job** | |||
| Median (interquartile range) | 9.5 (15.25) years | 11 (17) years | 0.791 |
| Occupational group* | |||
| Administration | 1 (0.49%) | 202 (99.51%) | 0.008 |
| Nursing assistants | 26 (5.11%) | 483 (94.89%) | |
| Nurses | 20 (4.81%) | 396 (95.19%) | |
| Physicians | 12 (3.36%) | 345 (96.64%) | |
| Diagnosis and therapeutics technicians | 1 (0.70%) | 142 (99.30%) | |
| Other technicians | 2 (1.77%) | 111 (98.23%) | |
| Hospital department* | |||
| Surgery | 10 (8.47%) | 108 (91.53%) | 0.001 |
| Clinical | 50 (3.70%) | 1,301 (96.30%) | |
| Support services | 2 (0.74%) | 270 (99.26%) | |
| Atopy*** | |||
| Yes | 19 (5.23%) | 344 (94.77%) | 0.107 |
| No | 43 (3.12%) | 1,335 (96.88%) | |
*χ2 test; **Mann-Whitney test; ***Fisher’s exact test.
Putative triggers of irritant contact dermatitis were presumed based on clinical criteria — aggravation of complaints following exposure to definite substances. All these cases test negative for DTH. The agents most commonly involved were skin disinfectants containing alcohol and quaternary ammonium, 76.47% (n=26), nitrile gloves, 17.65% (n=6), and prolonged contact with water, 5.88% (n=2). Alcohol, surface cleaners, surgical masks and a microscope rubber piece were reported by one employee. In regard to allergic dermatitis, thiuram was involved in 4 cases, and skin disinfectants containing quaternary ammonium in 3 — one of them with concomitant latex allergy.
DISCUSSION
Contact dermatitis occurs frequently among healthcare workers, with reported prevalence of 17 to 70%5-8,25. Also the prevalence of latex allergy is quite high for this occupational group (up to 17%) as a function of the ubiquitous use of rubber gloves as part of the personal protection equipment, in addition to other sources of latex exposure16-19. The wide variation in the reported prevalence rates of dermatoses among healthcare workers might be due to methodological differences among studies and the particular working conditions of the analyzed populations. One study performed in 2008 in a Portuguese hospital, involving administration of a questionnaire, found a prevalence of 34.3% of occupational skin disorders among the employees26. Differently, in the present study — which data were not collected through questionnaires, but from medical records — the prevalence of dermatoses was just 3.56%.
In addition to the methodological differences, preventive measures implemented at the analyzed hospital might have contributed to reduce the number of cases of occupational dermatosis14,27. The hospital OHD participated in the purchase of equipment along the past 10 years, and advised selecting less irritating and sensitizing materials, for instance nitrile or vinyl, thiuram-free gloves. The OHD also contributed to make hand cream available in all the hospital departments, and raised awareness among workers on the relevance of regular use. Employees diagnosed with dermatitis are advised to avoid sensitizing agents and irritants25,26, are provided alternative equipment, and are instructed to wear cotton glove liners underneath disposable gloves. These measures might have significantly influenced our results, because we only analyzed clinical information recorded after implementation21.
Also the prevalence of latex allergy was lower than that reported in the literature (1.23 vs. 17%)16. The reason might be that in the investigated hospital latex gloves are exclusively used during procedures requiring asepsis, and are always powder-free and lower-protein latex gloves17,27. A study performed in the same hospital in 2010 — i.e. during the early stage of implementation of the measures described here — the prevalence of latex allergy was 6.6% for nurses28, therefore higher than the one we found.
Nevertheless, complaints in 10 cases involved nitrile gloves, including both allergic (to thiuram-containing additives, n=4) and irritant (n=6) contact dermatitis. This finding points to the need for due surveillance, even when the materials used are theoretically safer.
Besides the implemented preventive measures, the low prevalence of dermatosis in the present study might be related to the quality of the medical records. To be sure, we are aware this is one of the limitations of the present study, since the records obviously did not provide information for workers who did not reported complaints during occupational medical examinations for considering them irrelevant or having already been relocated from sites involving exposure (healthy worker effect).
The results relative to susceptibility per occupational group agree with the reports in the literature, since prevalence was higher for nursing assistants, followed by nurses and physicians23,29. The possible reason is that these workers are more exposed to irritants and sensitizing agents, such as gloves and skin disinfectants7, compared to other occupational groups. Nursing assistants are charged of cleaning and disinfecting surfaces and equipment, in addition to helping nurses in patient care tasks. Prolonged contact with water during the working hours disrupts the stratum corneum of the skin, which by itself increases the susceptibility to irritants and sensitizing agents1,30. The same factors explain differences in the prevalence of dermatoses between workers allocated to surgery departments and those in clinical departments and support services.
We found a relationship between occupational dermatosis and personal history of atopy, but it was not statistically significant, neither on separate analysis of the three investigated conditions. While some authors reported possible association between atopic eczema and irritant contact dermatitis, a similar correlation was not yet confirmed for atopy in general21,23. Therefore, the lack of association in the present study between personal history of atopy and allergic contact dermatitis or latex allergy agrees with the reports in the literature21-23.
Since in the present study we analyzed data extracted from medical records, we were not able to establish when exposures to triggers effectively started or ended. For this reason, prospective cohort studies are needed to draw conclusions on the relative risk associated with factors described in the literature as likely to increase the odds of occurrence of dermatoses12.
Finally, the fact that nursing technicians represented the majority of workers in the analyzed population — despite a similar distribution of variables sex and age across the entire population — hinders the generalization of the study results.
CONCLUSION
The prevalence of dermatoses for the analyzed sample of 1,741 hospital workers was just 3.56%. Despite limitations inherent to the study design — the quality of records, in particular — preventive measures implemented in the past decade possibly contributed to this outcome. Nevertheless, primary prevention measures should be reinforced as concerns the nursing assistants. Using less sensitizing materials and bolstering the relevance of skin care seem to be essential to reduce the occurrence of dermatosis in this occupational group.
Footnotes
Funding: none
REFERENCES
- 1.Salako KB, Chowdhury MMU. Occupational Skin Disorders. In: La Dou J, Harrison RJ, eds. Occupational & Environmental Medicine. New York: McGraw-Hill; 2014. p. 324-45. [Google Scholar]
- 2.Sasseville D. Occupational Contact Dermatitis. Allergy Asthma Clin Immunol. 2008;4(2):59-65. 10.2310/7480.2008.00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nettis E, Colanardi M, Soccio A, Ferrarini A, Tursi A. Occupational irritant and allergic contact dermatitis among healthcare workers. Contact Dermatitis. 2002;46(2):101-7. 10.1034/j.1600-0536.2002.460208.x [DOI] [PubMed] [Google Scholar]
- 4.Ibler K, Jemec G, Flyvholm M, Diepgen T, Jensen A, Agner T. Hand eczema: prevalence and risk factors of hand eczema in a population of 2274 healthcare workers. Contact Dermatitis. 2012;67(4):200-7. 10.1111/j.1600-0536.2012.02105.x [DOI] [PubMed] [Google Scholar]
- 5.Higgins C, Palmer A, Cahill J, Nixon R. Occupational skin disease among Australian healthcare workers: a retrospective analysis from an occupational dermatology clinic, 1993-2014. Contact Dermatitis. 2016;75(4):213-22. 10.1111/cod.12616 [DOI] [PubMed] [Google Scholar]
- 6.Ibler K, Jemec G, Agner T. Exposures related to hand eczema: a study of healthcare workers. Contact Dermatitis. 2012;66(5):247-53. 10.1111/j.1600-0536.2011.02027.x [DOI] [PubMed] [Google Scholar]
- 7.Hamnerius N, Svedman C, Bergendorff O, Björk J, Bruze M, Engfeldt M, et al. Hand eczema and occupational contact allergies in healthcare workers with a focus on rubber additives. Contact Dermatitis. 2018;79(3):149-56. 10.1111/cod.13042 [DOI] [PubMed] [Google Scholar]
- 8.Ibler K, Jemec G, Garvey L, Agner T. Prevalence of delayed-type and immediate-type hypersensitivity in healthcare workers with hand eczema. Contact Dermatitis. 2016;75(4):223-9. 10.1111/cod.12587 [DOI] [PubMed] [Google Scholar]
- 9.Flyvholm M, Bach B, Rose M, Jepsen K. Self-reported hand eczema in a hospital population. Contact Dermatitis. 2007;57(2):110-5. 10.1111/j.1600-0536.2007.01134.x [DOI] [PubMed] [Google Scholar]
- 10.Streit M, Braathen L. Contact dermatitis: clinics and pathology. Acta Odontol Scand. 2001;59(5):309-14. [DOI] [PubMed] [Google Scholar]
- 11.Suárez-Pérez J, Bosch R, González S, González E. Pathogenesis and diagnosis of contact dermatitis: Applications of reflectance confocal microscopy. World J Dermatol. 2014;3(3):45-9. 10.5314/wjd.v3.i3.45 [DOI] [Google Scholar]
- 12.Ale I, Maibacht I. Diagnostic approach in allergic and irritant contact dermatitis. Expert Rev Clin Immunol. 2010;6(2):291-310. [DOI] [PubMed] [Google Scholar]
- 13.Nosbaum A, Vocanson M, Rozieres A, Hennino A, Nicolas JF. Allergic and irritant contact dermatitis. Eur J Dermatol. 2009;19(4):325-32. 10.1684/ejd.2009.0686 [DOI] [PubMed] [Google Scholar]
- 14.Sartorelli P, Kezic S, Filon FL, John S. Prevention of occupational dermatitis. Int J Immunopathol Pharmacol. 2011;24(Suppl. 1):S89-93. [PubMed] [Google Scholar]
- 15.Hawkey AS, Ghaffar S. Glove-related hand urticaria: an increasing occupational problem among healthcare workers. Br J Dermatol. 2016;174(5):1137-40. 10.1111/bjd.14318 [DOI] [PubMed] [Google Scholar]
- 16.Wu M, McIntosh J, Liu J. Current prevalence rate of latex allergy: Why it remains a problem? J Occup Health. 2016;58(2):138-44. 10.1539/joh.15-0275-RA [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Filon F, Cerchi R. Epidemiology of latex allergy in healthcare workers. Med Lav. 2008;99(2):108-12. [PubMed] [Google Scholar]
- 18.Valsecchi R, Leghissa P, Cortinovis R, Cologni L, Pomesano A. Contact urticaria from latex in healthcare workers. Dermatology. 2000;201(2):127-31. 10.1159/000018455 [DOI] [PubMed] [Google Scholar]
- 19.Valks R, Conde-Salazar L, Cuevas M. Allergic contact urticaria from natural rubber latex in healthcare and non-healthcare workers. Contact Dermatitis. 2004;50(4):222-4. 10.1111/j.0105-1873.2004.00327.x [DOI] [PubMed] [Google Scholar]
- 20.National Institute for Occupational Safety and Health NIOSH alert recommends the use of powder-free gloves [Internet]. NIOSH; 1998. [cited on Aug. 28, 2018] Available at: https://www.cdc.gov/niosh/ [Google Scholar]
- 21.Spiewak R. Contact dermatitis in atopic individuals. Curr Opin Allergy Clin Immunol. 2012;12(5):491-7. 10.1097/ACI.0b013e328357b05a [DOI] [PubMed] [Google Scholar]
- 22.Vijendren A, Yung M, Sanchez J. Occupational health issues amongst UK doctors: a literature review. Occup Med (Lond.). 2015;65(7):519-28. 10.1093/occmed/kqv088 [DOI] [PubMed] [Google Scholar]
- 23.Bryld L, Hindsberger C, Kyvik K, Agner T, Menné T. Risk factors influencing the development of hand eczema in a population-based twin sample. Br J Dermatol. 2003;149(6):1214-20. 10.1111/j.1365-2133.2003.05678.x [DOI] [PubMed] [Google Scholar]
- 24.Duarte I, Rotter A, Lazzarini R. Frequência da dermatite de contato ocupacional em ambulatório de alergia dermatológica. An Bras Dermatol. 2010;85(4):455-9. 10.1590/S0365-05962010000400006 [DOI] [PubMed] [Google Scholar]
- 25.Kaddourah S, Costa F, Fábrega J, Rabello L. Relação entre a ocorrência de dermatite de contato irritativa e o uso dos equipamentos de proteção individual. Rev Bras Med Trab. 2015;13(2):120-5. [Google Scholar]
- 26.Smedley J, Williams S, Peel P, Pedersen K. Management of occupational dermatitis in healthcare workers: a systematic review. Occup Environ Med. 2012;69(4):276-9. 10.1136/oemed-2011-100315 [DOI] [PubMed] [Google Scholar]
- 27.Cabeçadas M. Prevalência de dermites de contacto em enfermeiros hospitalares [MA dissertation]. Lisbon: ENSP; 2010. [Google Scholar]
- 28.Turner S, Carder M, van Tongeren M, McNamee R, Lines S, Hussey L, et al. The incidence of occupational skin disease as reported to The Health and Occupation Reporting (THOR) network between 2002 and 2005. Br J Dermatol. 2007;157(4):713-22. 10.1111/j.1365-2133.2007.08045.x [DOI] [PubMed] [Google Scholar]
- 29.Callahan A, Baron E, Fekedulegn D, Kashon M, Yucesoy B, Johnson VJ, et al. Winter season, frequent hand washing, and irritant patch test reactions to detergents are associated with hand dermatitis in health care workers. Dermatitis. 2013;24(4):170-5. 10.1097/DER.0b013e318290c57f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Visser M, Verberk M, van Dijk F, Bakker J, Bos J, Kezic S. Wet work and hand eczema in apprentice nurses: part I. Contact Dermatitis. 2014;70(1):44-55. 10.1111/cod.12131 [DOI] [PubMed] [Google Scholar]