Abstract
The purpose of this study was to (i) assess whether squat and gait biomechanical measures improve in patients with femoroacetabular impingement syndrome (FAIS) 6 months after surgery compared to pre-operative measures and (ii) compare biomechanical properties to controls without FAIS. In this prospective study, biomechanical data during a double leg squat task and gait for 15 FAIS patients and 9 controls were collected using three-dimensional motion analysis. Data were collected in the FAIS group at two-time points, pre-operatively and 6-month post-operatively following arthroscopic hip surgery, and at a single time point for the healthy controls. Independent sample’s t-test were used to compare the FAIS group to the controls, and paired samples t-test were used to determine within-group differences before and after hip arthroscopy in the FAIS group. The results indicated that there were significant within-group increases for sagittal plane moment rate during the double leg squat task (P = 0.009) between the pre-operative and post-operative time points for the FAIS group. Between-group differences showed that FAIS patients pre-operatively exhibit slower squat velocities during the descent (P = 0.005) and ascent phase (P = 0.012) of a double leg squat when compared healthy controls. Reduced hip external rotation moments during gait (P = 0.02) were also found between FAIS patients pre-operatively and controls. In conclusion, alterations in hip biomechanics are present before surgery for FAIS when compared to healthy controls, and joint mechanics change 6 months after surgery. However, the biomechanical differences during a double leg squat and gait were minimal.
INTRODUCTION
Femoroacetabular impingement syndrome (FAIS) is a common cause of hip pain in young adults, and hip arthroscopy is an effective treatment for FAIS that has failed conservative treatment and rehabilitation [1–4]. A number of studies have demonstrated that hip arthroscopy for the treatment of FAIS provides significant improvements in pain, timely return to sport, high rates of achieving meaningful clinical function, and high satisfaction at short-, mid- and long-term follow-up [5–8]. To date, hip arthroscopy for FAIS has predominately been evaluated with metrics such as patient-reported outcome scores, reported ability to return to sport, rate of revision and conversion to arthroplasty. However, several recent studies have introduced motion analysis as a new outcome measure following surgery for FAIS [9–14].
FAIS has been shown to alter hip kinematic and kinetic parameters during gait compared to matched controls [15–19]. The findings between studies have been relatively inconsistent and have demonstrated that persons with cam FAIS have decreased transverse, frontal and sagittal plane hip kinematics when compared to healthy controls [11, 13, 15, 16]. Rylander et al. (2013) reported that patients with FAIS demonstrated sagittal plane hip motion and peak hip internal rotation during stair climbing when compared to healthy controls, while Bagwell et al. (2015) demonstrated a reduced mean hip extensor moment and peak hip internal rotation in patients with FAIS compared to controls during a double leg deep squat task [13, 20]. Moreover, many of these lower extremity gait parameters have been shown to correlate with the extent of radiographic cam and pincer morphology in FAIS patients [21]. Two studies have demonstrated improvements in gait kinematics following arthroscopic surgery for FAIS [13, 14]. Interestingly, no differences in hip kinetics were found in these cohorts after arthroscopic surgical intervention for FAIS. Several studies have also reported differences between people with FAIS and healthy controls during a double leg squat task [16, 20, 22]. However, only a single study has evaluated double leg squat biomechanics before and after surgery for FAIS, although, this cohort underwent open, not arthroscopic, surgical intervention [12]. Variables such as joint impulse and rates of force development are often considered when evaluating squat performance [23, 24]. However, previous motion analysis studies that evaluate squatting in persons with FAIS have limited analysis to discrete biomechanical variable such as peak hip joint moment or angle.
In addition to limited evidence on squat and gait biomechanics before and after arthroscopic surgical intervention, there is limited information on the short-term impact (i.e. ≤6 months post-operative) of hip arthroscopic surgery for FAIS on squat and gait biomechanics. Therefore, the primary purpose of this study was to (i) assess whether squat and gait biomechanical measures improve in patients with FAIS 6 months after surgery compared to pre-operative measures and (ii) compare biomechanical properties to controls without FAIS. A 6-month time-point was chosen as many patients are able to return to their athletic endeavors at this time [25]. We hypothesized that patients with FAIS would achieve significant improvements in squat and gait parameters by 6 months post-operatively, and that baseline differences would exists between the pre-operative time point and healthy controls. We also hypothesize that no biomechanical differences would exist between the post-operative time point and healthy controls.
A secondary purpose was to explore differences in biomechanical variables that are a function of time. These variables include: ascent and descent squat velocity, moment rate and joint moment impulse. We hypothesized that prior to surgery patients with FAIS would demonstrate slower squat descent and ascent velocities, slower moment rate and lower joint moment impulses during a squat when compared to healthy controls and that there would be no difference in these variables between controls and FAIS patients 6 months following hip arthroscopic surgery.
METHODS
Patient selection
Institutional Review Board approval was obtained prior to patient enrollment and data collection. All patients underwent pre-enrollment informed consent. Consecutive symptomatic subjects with clinical and radiographic diagnosis of FAIS, failure of conservative management and who were scheduled for hip arthroscopy between 2011 and 2013 by a single fellowship-trained surgeon were asked to participate in pre-operative gait and squat analysis. Inclusion criteria for FAIS patients included clinical signs, symptoms and radiographic findings [26], failure of at least 3 months of conservative management (including activity modification, oral anti-inflammatories and physical therapy); and ability to walk a quarter of a mile and squat without significant difficulty. Exclusion criteria consisted of hip arthroscopy for an indication other than FAIS, prior history of bilateral hip surgery, prior ipsilateral hip surgery, signs of osteoarthritis (Tonnis grade >1), hip dysplasia (LCEA < 20°) or a history of congenital hip disorders (slipped capital femoral epiphysis [SCFE], developmental hip dysplasia, etc.). Healthy control subjects had no hip pain, no history of hip or lower extremity injury or surgery, no lumbar pathology and with examination and radiographs showing no evidence of FAIS. Controls also underwent informed consent prior to participation.
Surgical technique and post-operative rehabilitation
All hip arthroscopies were performed by a single fellowship-trained hip surgeon at a high-volume academic hospital using a technique that has been well-described in the literature [27–29] Every patient underwent acetabuloplasty, femoroplasty and labral repair with T capsulotomy, dynamic fluoroscopic examination and complete capsular closure via plication. Rehabilitation started on post-operative Day 1 for all patients as previously described [30, 31]. Briefly, all patients went through a four-phase rehabilitation protocol that lasted an average of 16–18 weeks. The surgical limb was initially restricted to 20-pound foot-flat-weight-bearing during the first phase, prioritizing joint protection and soft tissue mobilization techniques. Phase 2 concentrated on normal gait maintenance, full range of motion (ROM) restoration, improvement of neuromuscular control and maintenance of pelvic and core stability. Phase 3 included single leg squats and strengthening, soft tissue and joint mobilization, and cardiovascular fitness. Phase 4 emphasized return to preinjury level of sports participation. Running on an antigravity treadmill was allowed at Week 12, and patients progressed to sport-specific activities at Week 16.
Radiographic and clinical outcome measurements
Participating patients and control subjects underwent a standard set of radiographs including anteroposterior (AP) pelvis, false profile and 90° Dunn lateral views of the hip. The AP pelvis radiograph was used to measure lateral center edge angle (LCEA) and the 90° Dunn lateral was used to measure the alpha angle [32]. Pre-operative Tönnis grade was also assessed. Post-operative radiographs were obtained following hip arthroscopy for FAIS morphology as part of routine clinical care and demonstrated normalization of radiographic FAIS morphology in all cases.
Patients completed a pre- and 6-month post-operative questionnaire that included demographic information and validated hip-specific functional outcome scores [Hip Outcome Score Sport-Specific Subscale (HOS-SS) and Activities of Daily Living (HOS-ADL) subscales] [33–37].
Functional tasks—double leg squat and gait
For the double leg squat task, participants were positioned with their surgical limb or the randomly selected limb of the control group on the force plate with their feet parallel and approximately shoulder width apart facing in the anterior direction. From an initial standing position, the participants were instructed to look forward, position their arms at shoulder height out in front of them with the elbows straight and palms facing the floor. The subjects were given verbal instructions to squat down as low as possible (Fig. 1), and to then return to an upright position while maintaining a self-selected and controlled speed for the entire squat cycle [16, 38]. Keeping the upper extremity in an anterior extended position helped maintain balance and prevented the participants from using their limbs as support. The subjects were not provided a depth target or asked to squat at a certain pace in order to promote a self-selected squat strategy. A self-selected squat strategy was used to mimic how a squat would be evaluated in a clinical setting, where minimal cues are provided during movement evaluation. If subjects had difficulty squatting, which was defined as if they reported pain or apprehension during the squat, they were instructed to only squat to a comfortable depth. Subjects were reminded to maintain even weight on both legs during the squat task. Prior to recording the trials, each participant practiced the squat a minimum of two times.
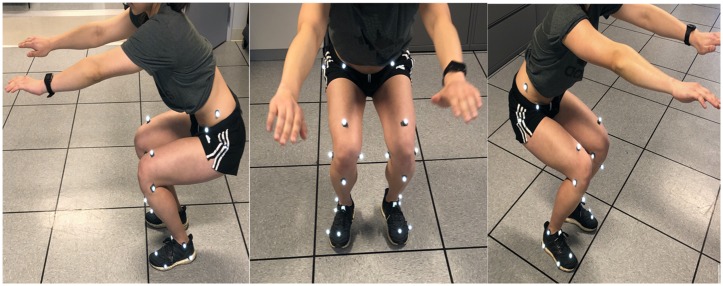
Fig. 1.
An instrumented participant demonstrates an unrestricted squat where they were instructed to squat as low as possible while keeping their upper limbs parallel to the floor and feet shoulder width apart.
For gait tests, the subjects walked at a self-selected speed along a 6-m walkway across three concealed floor embedded force plates. The subjects wore their own shoes and completed five level walking trials per limb. The data from the surgical limb and a randomly selected limb for the control subjects were averaged for the five trials. The position of the arms was at the side for walking. A self-selected walking speed was chosen for all gait trials to mimic how gait would typically be evaluated in a clinical setting where speed is rarely controlled.
Motion analysis
All FAIS patients completed both pre-operative and 6-month post-operative motion analysis testing. Pre-operative tests were conducted within 1-month of the scheduled surgical date, while post-operative evaluations were performed within 2 weeks of the 6-month post-operative date. Control subjects completed a single motion analysis testing session. The reason for a single testing session for control subjects was secondary to the rate of attrition at our institution.
Motion analysis data acquisition
Three-dimensional position data of 28 passive retroreflective markers were collected at a sampling rate of at 100 Hz with a 12-optoelectronic camera system (Qualisys, Gothenburg, Sweden) [21, 39]. Three-dimensional force data were simultaneously sampled at 1200 Hz during gait and squat tasks with three floor-embedded force plates (Bertec, Columbus, OH, USA). Retroreflective markers were placed bilaterally on the pelvic and lower extremities at the following locations: superior point of the iliac crest, anterior and posterior superior iliac spine, L5/sacrum, the greater trochanter, anterodistal thigh, lateral and medial knee joint line, tibial tuberosity, lateral and medial malleoli, lateral most point on the calcaneus, and the second and fifth metatarsal, and unilaterally on the right shoulder to denote right and left sides (Fig. 2). The same operator placed the markers in all cases to control for marker placement. The hip-joint center was estimated to be 2 cm distal to the mid-point of a line connecting the anterior superior iliac spine to the pubic symphysis [40].
Fig. 2.

Anterior and lateral views of the 28 passive retroreflective markers used for motion analysis.
Motion analysis data processing
Data were processed used The Motion Monitor software (Innovative Sports Training Inc., Chicago, IL, USA). Kinematic data were low pass filtered with a frequency cutoff of 6 Hz. The kinetic data were down sampled by a factor of 10 to match the kinematic data sample frequency of 100 Hz. An inverse dynamics approach was used to calculate external joint moments and these moments were normalized to percent body weight times height (%BWH) [41].
Squat motion data analysis
Three trials of a double leg squat task were analyzed. The squat cycle was divided into the descent and ascent phase. This phase was defined by using the vertical position of the sacral marker. The initiation of the squat cycle was defined as when the mean baseline quiet stance position of the sacral marker changed by greater than two standard deviations from baseline. The termination of the squat cycle was defined as when the sacral marker position returned to the equal or less than one-half SD of the baseline sacral marker position. The squat descent phase was defined from the initiation of the squat cycle to the point where the sacral marker reached a minimum vertical position and ascent phase was defined from the point after the minimum sacral marker position to the termination of the squat cycle point.
Squat depth was quantified as the change in vertical position of the sacral marker. A custom-written MATLAB (Mathworks, Natick, MA, USA) program was used to calculate squat depth. First, the mean vertical position of the sacral marker for the first 15 frames of squat data was calculated and used to represent baseline quiet stance. The minimum vertical position of the sacral marker was identified, and squat depth was calculated as the differences between baseline quiet stance vertical position and the minimum vertical position of the sacral marker during the squat. Squat descent and ascent velocity were calculated as the first derivatives of position of the sacral marker during the ascent and descent phases of the squat cycle and were reported in meters per second (m s−1).
Squat descent and ascent velocity, sagittal plane moment rate and sagittal plane joint moment impulse for both the descent and ascent phases of the squat were determined. Sagittal plane moment rate was calculated as the slope of the joint moment curve during the descent and ascent phases of the squat. Joint moment impulse was calculated as the area under the curve of the sagittal plane moment using a trapezoidal method. Being that the entire external sagittal plane squat moment is in the direction of flexion, this will be referred to as the flexion joint moment impulse. All discrete variables were extracted and calculated from non-time normalized kinematic and kinetic waveform data. However, all squat kinematic and kinetic data were time normalized to 100 data points to represent the squat cycle for the purpose of data presentation. All calculations were performed using a custom written program in MATLAB (Mathworks, Natick, MA, USA).
Gait motion data analysis
Filtered and non-time normalized joint kinematic and kinetic waveforms were extracted for analysis from five trials of gait. Biomechanical segment parameters were determined using the position of the markers and individual anthropometric data as inputs [39]. The spatiotemporal parameter of gait speed was calculated from a virtual center of mass marker that represented a weighted average of the center of mass of each segment included in the biomechanical model [21, 39, 42]. The gait variables of interest extracted for analysis were: peak hip joint flexion, extension and sagittal plane joint ROM and peak hip joint kinetics in all planes of motion. All discrete gait variables of interest were calculated and extracted from non-time normalized kinematic and kinetic waveform data. The kinematic and kinetic waveform data were then time normalized to 100 data points to represent the entire gait cycle.
Statistical analysis
All data were inspected to determine if parametric statistical testing was appropriate. The Shapiro–Wilk test revealed all data were normally distributed. No significant outliers were present in the data when all variables were examined with box plots. Descriptive statistics were calculated for all data. Within group comparisons for the FAIS group at the pre-operative and 6-month post-operative time point were performed using paired samples t-tests. Between-group comparisons for pre-operative patients and controls and post-operative patients and controls were performed using independent samples t-tests. Data from a single subject and the post-operative data from another subject were eliminated secondary to a technical error that lead to unusable motion analysis data. As such, the within-group comparison included n = 12 FAIS subjects with data from both the pre-operative and 6-month post-operative time point, and n = 14 FAIS subjects pre-operatively, and n = 13 subjects at the 6-month post-operative time point for the between group comparisons. An a priori alpha value of 0.05 was set to determine statistical significance. All statistical analyses were performed using SPSS software (version 22; IBM, Armonk, NY, USA). Considering there was no within-or-between-group difference in squat depth or gait speed, it was decided that these variables should not be entered as co-variates into the analysis for the other biomechanical variables. The authors chose not to control for multiple comparisons because of the exploratory nature of the study.
RESULTS
Patient demographics, radiographic parameters and patient-reported outcomes
There were no differences in age or BMI between patient with FAIS and healthy controls (Table I). FAIS patients pre-operatively, had significantly greater alpha angles and lower patient-reported outcome scores when compared to controls. A statistically significant improvement in alpha angle, HOS-SS and HOS-ADL was observed when comparing pre-operative versus post-operative score averages.
Table I. .
Demographics, radiographic measurements and patient-reported outcomes for FAIS group at the pre-operative and 6-month post-operative time points and healthy controls
| Pre | Post | Con | P-value | P-value | P-value | |
|---|---|---|---|---|---|---|
| (n = 14) | (n = 13) | (n = 9) | ||||
| Pre versus Con | Pre versus Post | Post versus Con | ||||
| Gender (female) | 11 (84.6%) | 10(76.9%) | 5(55.5%) | — | — | — |
| Age (years) | 29.4 ± 9.6 | 29.5 ± 9.5 | 27.8 ± 6.5 | 0.66 | 0.64 | 0.74 |
| BMI (kg/m2) | 22.9 ± 4.8 | 23.0 ± 5.2 | 22.8 ± 3.5 | 0.92 | 0.83 | 0.89 |
| Alpha angle (°) | 62.3 ± 3.9 | 38.4 ± 4.2 | 51.4 ± 5.7 | 0.001 | 0.001 | 0.001 |
| Lateral center edge angle (°) | 32.0 ± 5.0 | 32.3 ± 4.8 | 32.9 ± 8.6 | 0.75 | 0.61 | 0.82 |
| HOS-ADL | 67.3 ± 15.1 | 90.6 ± 7.7 | 100 ± 0.0 | — | 0.001 | — |
| HOS-SS | 48.4 ± 18.0 | 80.8 ± 12.9 | 100 ± 0.0 | — | 0.001 | — |
Pre, pre-operative time point FAIS group; Post, 6-month postoperative time point FAIS group; Con., healthy control; F, female, M, male; BMI, body mass index; HOS-ADL, Hip Outcome Score Activity of Daily Living Subscale; HOS-SS, Hip Outcome Score Sport Specific Subscale.
Bold type indicates statistical significance at α = 0.05.
Comparison of pre-operative versus 6-month post-operative within squat kinematics among FAIS patients
FAIS patients demonstrated a greater pre-operative external peak hip extension moment during the double leg squat when compared to the 6-month post-operative time point (Pre: 0.4 ± 0.5 versus Post: 0.1 ± 0.4 N·m/BW·H; P = 0.006) (Table II). There were no differences in any other biomechanical variable the double leg squat task between the pre-operative and 6-month post-operative time for FAIS patients.
Table II. .
Comparisons of the kinematic and kinetic variables during a double leg squat for the FAIS group between pre-operative and 6-month post-operative time points, and the healthy control group
| Pre | Post | Con | P-value | P-value | P-value | |
|---|---|---|---|---|---|---|
| Pre versus Post | Pre versus Con | Post versus Con | ||||
| Kinematics | ||||||
| Max. Flex. (°) | 98.5 ± 19.6 | 99.2 ± 16.7 | 104.8 ± 6.2 | 0.95 | 0.37 | 0.35 |
| Max. Ext. (°) | 3.9 ± 5.0 | 2.7 ± 3.5 | 3.5 ± 4.2 | 0.06 | 0.83 | 0.62 |
| Sagittal ROM (°) | 94.7 ± 22.9 | 96.6 ± 17.4 | 101.4 ± 7.5 | 0.61 | 0.41 | 0.45 |
| Descent squat velocity (m·s−1) | 0.4 ± 0.2 | 0.5 ± 0.2 | 0.6 ± 0.2 | 0.08 | 0.005 | 0.26 |
| Ascent squat velocity (m·s−1) | 0.4 ± 0.2 | 0.5 ± 0.2 | 0.6 ± 0.2 | 0.10 | 0.012 | 0.22 |
| Kinetics | ||||||
| Flex. Mom. (N·m/BW·H) | −6.4 ± 1.6 | −6.3 ± 1.7 | −5.9 ± 0.9 | 0.77 | 0.44 | 0.53 |
| Ext. Mom. (N·m/BW·H) | 0.4 ± 0.5 | 0.1 ± 0.4 | 0.2 ± 0.3 | 0.006 | 0.50 | 0.51 |
| Add. Mom. ((N·m/BW·H) | 2.4 ± 1.6 | 1.9 ± 2.0 | 1.5 ± 1.7 | 0.06 | 0.21 | 0.61 |
| Abd. Mom. (N·m/BW·H) | 1.2 ± 0.9 | 1.1 ± 1.1 | 0.6 ± 0.4 | 0.71 | 0.08 | 0.20 |
| ER Mom. (N·m/BW·H) | 0.5 ± 0.5 | 0.4 ± 0.7 | 0.6 ± 0.4 | 0.67 | 0.45 | 0.42 |
| IR Mom. (N·m/BW·H) | 0.8 ± 0.8 | 0.5 ± 0.5 | 0.5 ± 0.7 | 0.18 | 0.26 | 0.94 |
| Descent Flex. Mom. Rate (N·m/BW·H) | −2.7 ± 1.5 | −3.6 ± 1.5 | −3.5 ± 1.9 | 0.10 | 0.59 | 0.43 |
| Ascent Flex. Mom. Rate (N·m·BW·H)·s−1 | −3.5 ± 1.6 | −3.9 ± 1.9 | −3.1 ± 1.3 | 0.54 | 0.36 | 0.88 |
| Flex. Impulse (N·m/ BW·H )·s | −12.3 ± 4.5 | −9.6 ± 3.5 | −11.1 ± 4.9 | 0.10 | 0.46 | 0.27 |
Data reported as mean ± standard deviation.
Pre, FAIS group pre-operative time point; Post, FAIS group 6-month postoperative time point; Con, healthy control group; Max. Flex., maximum flexion angle; Max. Ext., maximum extension angle; Sagittal ROM, total sagittal plane joint range of motion; Flex Mom., peak flexion joint moment; Ext. Mom, peak extension joint moment; Add. Mom., peak adduction joint moment; Abd. Mom., peak abduction joint moment; ER Mom., peak external rotation joint moment; IR Mom., peak internal rotation joint moment; Descent Flex. Mom. Rate, flexion joint moment rate during descent phase; Ascent Flex. Mom. Rate, flexion joint moment rate during ascent phase; Flex. Joint Impulse, flexion joint impulse during the squat cycle.
Bold type indicates statistical significance at α = 0.05.
Comparison of pre-operative versus 6-month post-operative within gait biomechanics among FAIS patients
There were no differences in gait speed between the pre-operative and 6-month post-operative time point for FAIS patients (Pre: 1.3 ± 0.1 m·s−1 versus Post: 1.4 ± 0.1 m·s−1, P = 0.43). There were no differences in any biomechanical variables during gait between the pre-operative and 6-month post-operative time point in patients with FAIS (Table II).
Comparison of squat biomechanics between FAIS versus healthy control group
Patients with FAIS pre-operatively demonstrated slower hip flexion joint angular velocity during the descent (0.4 ± 0.2 versus 0.6 ± 0.2; P = 0.005) and ascent (0.4 ± 0.2 versus 0.6 ± 0.2; P = 0.012) phase of a double leg squat when compared to healthy control (Table II). There were no differences in any squat biomechanical variable between the FAIS patients at the 6-month post-operative time point and healthy controls (P > 0.05 for all).
Comparison of pre-operative gait biomechanics between FAIS group versus Healthy control
FAIS patients pre-operatively demonstrated lower peak hip external rotation moments during gait compared to healthy controls (FAI: 0.6 ± 0.2 versus controls: 0.8 ± 0.2 N·m/BW·H; P = 0.02) (Table III). There were no between group differences were observed during gait between FAIS patients at the pre-operative or 6-month post-operative time point and healthy controls (P > 0.05 for all).
Table III. .
Between group comparisons of the kinematic and kinetic variables during gait for the FAIS group at the pre-operative and 6-month post-operative time points and healthy control group
| Pre | Post | Con | P-value | P-value | P-value | |
|---|---|---|---|---|---|---|
| Pre versus Post. | Pre versus Con | Post versus Con | ||||
| Kinematics | ||||||
| Max. Flex. (°) | 18.7 ± 4.2 | 19.3 ± 3.9 | 19.8 ± 6.0 | 0.61 | 0.61 | 0.82 |
| Max. Ext. (°) | −14.2 ± 6.0 | −12.1 ± 3.8 | −12.0 ± 4.7 | 0.16 | 0.37 | 0.93 |
| Sagittal ROM (°) | 32.6 ± 6.4 | 31.5 ± 4.8 | 31.8 ± 4.9 | 0.17 | 0.73 | 0.88 |
| Kinetics | ||||||
| Flex. Mom. (N·m/BW·H) | −4.1 ± 1.1 | −3.9 ± 1.0 | −4.3 ± 1.4 | 0.11 | 0.62 | 0.38 |
| Ext. Mom. (N·m/BW·H) | 3.6 ± 1.5 | 3.0 ± 1.1 | 3.7 ± 1.4 | 0.46 | 0.92 | 0.24 |
| Add. Mom. (N·m/BW·H) | −4.9 ± 1.2 | −5.1 ± 1.0 | −4.6 ± 0.9 | 0.15 | 0.58 | 0.23 |
| Abd. Mom. (N·m/BW·H) | 1.0 ± 0.3 | 0.9 ± 0.3 | 1.0 ± 0.3 | 0.42 | 0.73 | 0.2 |
| ER Mom. (N·m/BW·H) | 0.6 ± 0.2 | 0.8 ± 0.2 | 0.9 ± 0.3 | 0.06 | 0.02 | 0.33 |
| IR Mom. (N·m/BW·H) | −1.0 ± 0.3 | −1.0 ± 0.2 | −0.9 ± 0.2 | 0.53 | 0.5 | 0.7 |
Data reported as mean ± standard deviation.
Pre, FAIS group pre-operative time point; Post, FAIS group 6-month post-operative time point; Con, healthy control group; Max. Flex., maximum flexion angle; Max. Ext., maximum extension angle; Sagittal ROM, total sagittal plane joint range of motion; Flex Mom., peak flexion joint moment; Ext. Mom, peak extension joint moment; Add. Mom., peak adduction joint moment; Abd. Mom., peak abduction joint moment; ER Mom., peak external rotation joint moment; IR Mom., peak internal rotation joint moment.
Bold type indicates statistical significance at α = 0.05.
DISCUSSION
The primary findings of this study were that FAIS patients demonstrated a significantly decreased peak external hip extension moment during a double leg squat post-operatively compared to baseline prior to surgery. No other differences between pre-operative and post-operative measurements were found for during the double leg squat task or gait biomechanics. When comparing the FAIS to healthy control group at baseline, the FAIS group had a slower ascent and descent during the double leg squat. During gait, FAIS patients pre-operatively demonstrated smaller peak hip external rotation moments when compared to healthy controls. Furthermore, there were no differences in post-operative hip biomechanics during a double leg squat or gait between these two groups. While the current results indicate that hip joint biomechanics change 6 months after arthroscopic surgery for FAIS, it is difficult to draw definitive conclusions regarding whether changes indicate functional improvement in hip joint biomechanics. Further studies are needed to determine the impact of FAIS on hip joint function [13, 43, 44].
Previous studies have evaluated squat biomechanics in FAIS patients and compared them to healthy controls [19]. Diamond et al. compared squat biomechanics in 15 pre-operative patients to healthy controls and observed a difference in descent speed between the two groups [45]. Similar to the current study, FAIS patients demonstrated slower descent speed as compared to health individuals matched by age and sex [45]. These results are also reflected in Malloy et al. when patients with FAIS performed a single-leg squat more slowly than individuals without hip pain [19]. Collectively, patients with FAIS may slow their squatting speed descent in anticipation of discomfort felt in the squatting position.
The current study indicates that FAIS patients demonstrate a significantly reduced peak hip extension moment 6 months after undergoing hip arthroscopy. We also noted a statistical trend (P = 0.06) toward reduced peak hip extension angle was present. Although peak hip extension angles occurred during periods of upright stance prior to the beginning of the actual squat, this phenomenon may help explain the difference in the peak hip extension moments between the pre-operative and post-operative time points. External moments are offset by internal moments of the antagonistic muscle groups; therefore, a lower peak external extension moment may decrease the demand on the hip flexors to reduce pain and/or discomfort. During the stance phase, hip flexor muscle activation would likely cause a more flexed posture at the hip. However, in the current study, perhaps FAIS patients standing in 2° more of hip extension after arthroscopic surgery helped facilitate a reduction in hip flexor muscle activity. The greater amount of hip extension would be driven by the hip extensor muscles (such as the gluteus maximus and hamstrings), and could potentially reduce the amount of activation of the hip flexor muscles, thereby leading to smaller peak hip extension moments after hip arthroscopic surgery. These data suggest physical rehabilitation needs to consider hip flexion strength to improve movement patterns following hip arthroscopic surgery. In addition to post-operative rehabilitation focusing on hip flexor strengthening, it is possible that these patients may benefit from pre-operative rehabilitation as well, since previous studies have indicated that this may have an effect on post-operative hip flexor strength in FAIS patients [46].
No other biomechanical differences between the pre-operative and 6-month post-operative time point where found, which suggests that hip squat biomechanics change very little at 6 months following arthroscopic surgery for FAIS. Similarly, Rylander et al. [13] reported limited improvement 1-year post-operatively for stairclimbing, an activity similar to squatting that involves a large ROM. In addition, Catelli et al. [47] observed similar findings, with no changes in squat depths at 2-years after hip arthroscopy in FAIS patients. These findings, however, are inconsistent with those from a previous study that investigated double leg squat biomechanics in FAIS patients with cam type impingement before and 1-year after surgical correction [22]. The authors reported that after surgery FAIS patient squatted to a greater mean depth compared to pre-operative measurements and demonstrated changes in ankle and knee kinematic angles. One reason for the difference between the two studies may be related to our patients undergoing hip arthroscopic surgery for FAIS whereas the patients in the previous study underwent open surgical intervention for FAIS. This key difference in technique could lead to different recovery times, with the arthroscopic technique arguably leading to shorter post-operative recovery times. In addition, the goal of the current study was to provide information on biomechanics at an early post-operative time point (i.e. 6 months), whereas Lamontagne et al. [12] examined biomechanics between 8 and 32 months after surgery. This creates a wide range of post-operative recovery period for patients, which may explain the differences in a greater number of variables between both studies. This demonstrates the importance of evaluating biomechanical parameters at multiple timepoints within a single study using a single surgical procedure.
The only difference in gait biomechanics in the current study was reduced maximum hip external rotation moments during gait, which are consistent with previous studies [15, 17]. Both Hunt et al. and King et al. demonstrated a lower external rotation moment in patients with FAIS when compared to healthy controls [15, 17]. Remembering that external moments are offset by internal moments of the antagonistic muscle groups; these data suggest lower activation of the internal rotations of the hip during walking compared with controls. This compensatory mechanism may denote a strategy to prevent positions of hip internal rotation that are often reported to be painful in patients with FAIS [21, 48]. Data from Rylander et al. [13] support this theory as patients with FAIS demonstrated a significant reduced amount of hip internal rotation compared to health controls. However, across the literature, biomechanical alterations at the hip during gait in FAIS patients have been inconsistent with recent evidence showing no differences in gait biomechanics in people with FAIS compared to controls [11, 15, 16, 22, 49]. Perhaps the reason for inconsistency in previous studies and the minimal findings in the current study are related to the fact that gait does not involve near end ranges of hip motion, and, therefore would not be expected to reproduce symptomatic impingement at the hip joint. Additionally, although forces across the hip joint can be on average three-times body weight, this demand does not seem to bring about consistent differences in people with FAIS. Future studies should focus on the role the demand of a task plays in bringing about biomechanical differences at the hip in patients with FAIS.
Limitations
There are a number of limitations in this study that should be addressed. First, the generalizability of the study’s findings may be limited due to the small sample size and the heterogeneity of the control group. However, the FAIS patients were selected prospectively from a single surgeon at a high-volume hip preservation center, therefore, our sample likely represents FAIS patients that commonly present for care. Second, the authors acknowledge the that lack of a proportional sex matching (i.e. 1:1 male:female) between the control and FAIS group does also represent a limitation of generalizability of the current study findings. Third, although 3D motion capture remains the gold standard for biomechanical studies, wearable technologies have recently been developed that may improve the ability to collect precise movement data in the clinical or other environmental setting. The authors therefore acknowledge the clinical translation of these laboratory-based methods. Fourth, an a priori was not performed since, to our knowledge, no study has evaluated the change in gait and squat kinetics/kinematics in FAIS patients after undergoing surgical treatment, and therefore an effect size has not been established for any variable to calculate the necessary population size for observed power of over 80%. A post hoc power analysis in this study is dependent on what comparison is chosen to calculate the effect size for determining the observed power. Using the pre-operative peak external rotation joint moment average during gait and comparing it to healthy controls, the effect size (Cohen’s d) is equal to 1.176697, and the observed power for a two-tailed hypothesis is 0.873. However, this power analysis may not be applicable to all the t-tests performed in this study, and it may be possible that some of the analysis is underpowered. In addition, the multiple comparisons on the current study increase the likelihood of committing type II error. However, there is limited information on hip biomechanics during functional tasks in FAIS patients; therefore, this study was somewhat exploratory in nature. As such, Bonferroni corrections were not applied as these data will also be used to guide variable selection in future studies to limit comparisons and reduce the risk of type II statistical error. Fifth, the authors did not account for the presence of pain during gait or squat and whether it had an effect on mechanics. Future studies may want to evaluate whether there is a correlation between pain during these actions and differences in kinematics. Finally, the lack of follow-up for the control group to account for a learning effect may also influence the results. The control group in the current study had a high rate of attrition that was outside of the authors’ control which posed logistical limitations to further data collection. Future studies will involve follow-up testing of the control group and will utilize methods such as incentives to reduce the amount of attrition. Additionally, although not statistically different, there was a large range of walking speeds for gait testing, this potentially could impact moment magnitudes [50].
CONCLUSION
FAIS patients demonstrate alterations in hip biomechanics during a double leg squat task when compared to healthy controls. However, alterations during gait are minimal. Hip joint biomechanics during a double leg squat change after arthroscopic hip surgery for FAIS. Nevertheless, based on our dataset, it is difficult to determine if these alterations represent improvement. Regardless, physical therapists should remain aware that hip biomechanics 6 months after arthroscopic hip surgery may continue to demonstrate change; therefore, movement patterns should be addressed during post-operative rehabilitation.
CONFLICT OF INTEREST STATEMENT
S.J.N. has received research support from Allosource, Arthrex, Inc., Athletico, DJ Orthopaedics, Linvatec, Miomed, Smith & Nephew and Stryker; is the Editorial or governing board member of American Journal of Orthopedics; is the Board or committee member of American Orthopaedic Society for Sports Medicine and Arthroscopy Association of North America; has received education payments from Arthrex, Inc.; has received education support from Elite Orthopaedics; is a paid consultant for Ossur: IP Royalties and Stryker; has received Publishing royalties, financial or material support from Springer; and has received consulting fees and hospitality payments from Stryker. G.L.C. has received education payments from Arthrex and Smith & Nephew.
FUNDING
Department of Orthopedic Surgery at Rush University Medical Center; and the Orthopaedic Research and Education Foundation Resident Research Project Grant #14-027.
REFERENCES
- 1. Bozic KJ, Chan V, Valone FH 3rd. et al. Trends in hip arthroscopy utilization in the United States. J Arthroplasty 2013; 28: 140–3. [DOI] [PubMed] [Google Scholar]
- 2. Colvin AC, Harrast J, Harner C.. Trends in hip arthroscopy. J Bone Joint Surg Am 2012; 94: e23. [DOI] [PubMed] [Google Scholar]
- 3. Montgomery SR, Ngo SS, Hobson T. et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy 2013; 29: 661–5. [DOI] [PubMed] [Google Scholar]
- 4. Nepple JJ, Byrd JW, Siebenrock KA. et al. Overview of treatment options, clinical results, and controversies in the management of femoroacetabular impingement. J Am Acad Orthop Surg 2013; 21 Suppl 1: S53–58. [DOI] [PubMed] [Google Scholar]
- 5. Alradwan H, Philippon MJ, Farrokhyar F. et al. Return to preinjury activity levels after surgical management of femoroacetabular impingement in athletes. Arthroscopy 2012; 28: 1567–76. [DOI] [PubMed] [Google Scholar]
- 6. Byrd JW, Jones KS.. Hip arthroscopy in athletes: 10-year follow-up. Am J Sports Med 2009; 37: 2140–3. [DOI] [PubMed] [Google Scholar]
- 7. Weber AE, Kuhns BD, Cvetanovich GL. et al. Amateur and recreational athletes return to sport at a high rate following hip arthroscopy for femoroacetabular impingement. Arthroscopy 2017; 33: 748–55. [DOI] [PubMed] [Google Scholar]
- 8. Kunze KN, Leong NL, Beck EC, Bush-Joseph CA. et al. Hip arthroscopy for femoroacetabular impingement improves sleep quality postoperatively. Arthroscopy 2019; 35: 461–9. [DOI] [PubMed] [Google Scholar]
- 9. Alradwan H, Khan M, Grassby MH. et al. Gait and lower extremity kinematic analysis as an outcome measure after femoroacetabular impingement surgery. Arthroscopy 2015; 31: 339–44. [DOI] [PubMed] [Google Scholar]
- 10. Bedi A, Dolan M, Hetsroni I. et al. Surgical treatment of femoroacetabular impingement improves hip kinematics: a computer-assisted model. Am J Sports Med 2011; 39 Suppl: 43S–9S. [DOI] [PubMed] [Google Scholar]
- 11. Brisson N, Lamontagne M, Kennedy MJ, Beaulé PE.. The effects of cam femoroacetabular impingement corrective surgery on lower-extremity gait biomechanics. Gait Posture 2013; 37: 258–63. [DOI] [PubMed] [Google Scholar]
- 12. Lamontagne M, Brisson N, Kennedy MJ, Beaule PE.. Preoperative and postoperative lower-extremity joint and pelvic kinematics during maximal squatting of patients with cam femoro-acetabular impingement. J Bone Joint Surg Am 2011; 93 Suppl 2: 40–5. [DOI] [PubMed] [Google Scholar]
- 13. Rylander J, Shu B, Favre J. et al. Functional testing provides unique insights into the pathomechanics of femoroacetabular impingement and an objective basis for evaluating treatment outcome. J Orthop Res 2013; 31: 1461–8. [DOI] [PubMed] [Google Scholar]
- 14. Rylander JH, Shu B, Andriacchi TP, Safran MR.. Preoperative and postoperative sagittal plane hip kinematics in patients with femoroacetabular impingement during level walking. Am J Sports Med 2011; 39 Suppl: 36S–42S. [DOI] [PubMed] [Google Scholar]
- 15. Hunt MA, Gunether JR, Gilbart MK.. Kinematic and kinetic differences during walking in patients with and without symptomatic femoroacetabular impingement. Clin Biomech (Bristol, Avon) 2013; 28: 519–23. [DOI] [PubMed] [Google Scholar]
- 16. Kennedy MJ, Lamontagne M, Beaule PE.. Femoroacetabular impingement alters hip and pelvic biomechanics during gait walking biomechanics of FAI. Gait Posture 2009; 30: 41–4. [DOI] [PubMed] [Google Scholar]
- 17. King MG, Lawrenson PR, Semciw AI. et al. Lower limb biomechanics in femoroacetabular impingement syndrome: a systematic review and meta-analysis. Br J Sports Med 2018; 52: 566–80. [DOI] [PubMed] [Google Scholar]
- 18. Lewis CL, Khuu A, Loverro KL.. Gait alterations in femoroacetabular impingement syndrome differ by sex. J Orthop Sports Phys Ther 2018; 48: 649–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Malloy P, Neumann DA, Kipp K.. Hip biomechanics during a single-leg squat: five key differences between people with femoroacetabular impingement syndrome and those without hip pain. J Orthop Sports Phys Ther 2019; 49: 908–16. [DOI] [PubMed] [Google Scholar]
- 20. Bagwell JJ, Snibbe J, Gerhardt M, Powers CM.. Hip kinematics and kinetics in persons with and without cam femoroacetabular impingement during a deep squat task. Clin Biomech (Bristol, Avon) 2016; 31: 87–92. [DOI] [PubMed] [Google Scholar]
- 21. Farkas GJ, Cvetanovich GL, Rajan KB. et al. Impact of femoroacetabular impingement morphology on gait assessment in symptomatic patients. Sports Health 2015; 7: 429–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kumar D, Dillon A, Nardo L. et al. Differences in the association of hip cartilage lesions and cam-type femoroacetabular impingement with movement patterns: a preliminary study. PM R 2014; 6: 681–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Farris DJ, Lichtwark GA, Brown NA, Cresswell AG.. Deconstructing the power resistance relationship for squats: a joint-level analysis. Scand J Med Sci Sports 2016; 26: 774–81. [DOI] [PubMed] [Google Scholar]
- 24. Mathiyakom W, McNitt-Gray JL, Requejo P, Costa K.. Modifying center of mass trajectory during sit-to-stand tasks redistributes the mechanical demand across the lower extremity joints. Clin Biomech (Bristol, Avon) 2005; 20: 105–11. [DOI] [PubMed] [Google Scholar]
- 25. Malviya A, Paliobeis CP, Villar RN.. Do professional athletes perform better than recreational athletes after arthroscopy for femoroacetabular impingement? Clin Orthop Relat Res 2013; 471: 2477–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Griffin DR, Dickenson EJ, O'Donnell J. et al. The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med 2016; 50: 1169–76. [DOI] [PubMed] [Google Scholar]
- 27. Frank RM, Lee S, Bush-Joseph CA. et al. Improved outcomes after hip arthroscopic surgery in patients undergoing T-capsulotomy with complete repair versus partial repair for femoroacetabular impingement: a comparative matched-pair analysis. Am J Sports Med 2014; 42: 2634–42. [DOI] [PubMed] [Google Scholar]
- 28. Slikker W 3rd, Van Thiel GS, Chahal J, Nho SJ.. The use of double-loaded suture anchors for labral repair and capsular repair during hip arthroscopy. Arthrosc Tech 2012; 1: e213–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Harris JD, Slikker W 3rd, Gupta AK. et al. Routine complete capsular closure during hip arthroscopy. Arthrosc Tech 2013; 2: e89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Malloy P, Gray K, Wolff AB.. Rehabilitation after hip arthroscopy: a movement control-based perspective. Clin Sports Med 2016; 35: 503–21. [DOI] [PubMed] [Google Scholar]
- 31. Leong NL, Clapp IM, Neal WH. et al. The influence of pain in other major joints and the spine on 2-year outcomes after hip arthroscopy. Arthroscopy 2018; 34: 3196–201. [DOI] [PubMed] [Google Scholar]
- 32. Clohisy JC, Carlisle JC, Beaule PE.. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am 2008; 90 Suppl 4: 47–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Aprato A, Jayasekera N, Villar RN.. Does the modified Harris hip score reflect patient satisfaction after hip arthroscopy? Am J Sports Med 2012; 40: 2557–60. [DOI] [PubMed] [Google Scholar]
- 34. Martin RL, Kelly BT, Philippon MJ.. Evidence of validity for the hip outcome score. Arthroscopy 2006; 22: 1304–11. [DOI] [PubMed] [Google Scholar]
- 35. Martin RL, Philippon MJ.. Evidence of reliability and responsiveness for the hip outcome score. Arthroscopy 2008; 24: 676–82. [DOI] [PubMed] [Google Scholar]
- 36. Martin RL, Philippon MJ.. Evidence of validity for the hip outcome score in hip arthroscopy. Arthroscopy 2007; 23: 822–6. [DOI] [PubMed] [Google Scholar]
- 37. Skendzel JG, Philippon MJ, Briggs KK, Goljan P.. The effect of joint space on midterm outcomes after arthroscopic hip surgery for femoroacetabular impingement. Am J Sports Med 2014; 42: 1127–33. [DOI] [PubMed] [Google Scholar]
- 38. Pai YC, Rogers MW.. Speed variation and resultant joint torques during sit-to-stand. Arch Phys Med Rehabil 1991; 72: 881–5. [DOI] [PubMed] [Google Scholar]
- 39. Andriacchi TP. Dynamics of pathological motion: applied to the anterior cruciate deficient knee. J Biomech 1990; 23 Suppl 1: 99–105. [DOI] [PubMed] [Google Scholar]
- 40. Andriacchi TP, Andersson GB, Fermier RW. et al. A study of lower-limb mechanics during stair-climbing. J Bone Joint Surg Am 1980; 62: 749–57. [PubMed] [Google Scholar]
- 41. Moisio KC, Sumner DR, Shott S, Hurwitz DE.. Normalization of joint moments during gait: a comparison of two techniques. J Biomech 2003; 36: 599–603. [DOI] [PubMed] [Google Scholar]
- 42. Prodromos CC, Andriacchi TP, Galante JO.. A relationship between gait and clinical changes following high tibial osteotomy. J Bone Joint Surg Am 1985; 67: 1188–94. [PubMed] [Google Scholar]
- 43. Foucher KC, Schlink BR, Shakoor N, Wimmer MA.. Sagittal plane hip motion reversals during walking are associated with disease severity and poorer function in subjects with hip osteoarthritis. J Biomech 2012; 45: 1360–5. [DOI] [PubMed] [Google Scholar]
- 44. Matheney T, Sandell L, Foucher K. et al. Motion analysis, cartilage mechanics, and biology in femoroacetabular impingement: current understanding and areas of future research. J Am Acad Orthop Surg 2013; 21 Suppl 1: S27–32. [DOI] [PubMed] [Google Scholar]
- 45. Diamond LE, Bennell KL, Wrigley TV. et al. Squatting biomechanics in individuals with symptomatic femoroacetabular impingement. Med Sci Sports Exerc 2017; 49: 1520–9. [DOI] [PubMed] [Google Scholar]
- 46. Grant LF, Cooper DJ, Conroy JL.. The HAPI ‘Hip Arthroscopy Pre-habilitation Intervention’ study: does pre-habilitation affect outcomes in patients undergoing hip arthroscopy for femoro-acetabular impingement? J Hip Preserv Surg 2017; 4: 85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Catelli DS, Kowalski E, Beaule PE, Lamontagne M.. Increased pelvic mobility and altered hip muscles contraction patterns: two-year follow-up cam-FAIS corrective surgery. J Hip Preserv Surg 2019; 6: 140–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Byrd JW. Femoroacetabular impingement in athletes: current concepts. Am J Sports Med 2014; 42: 737–51. [DOI] [PubMed] [Google Scholar]
- 49. Diamond LE, Wrigley TV, Bennell KL. et al. Hip joint biomechanics during gait in people with and without symptomatic femoroacetabular impingement. Gait Posture 2016; 43: 198–203. [DOI] [PubMed] [Google Scholar]
- 50. Bejek Z, Paroczai R, Illyes A, Kiss RM.. The influence of walking speed on gait parameters in healthy people and in patients with osteoarthritis. Knee Surg Sports Traumatol Arthrosc 2006; 14: 612–22. [DOI] [PubMed] [Google Scholar]