Abstract
Posttraumatic stress disorder (PTSD) has empirically-established associations with positive emotion dysregulation. Extending existing research, we utilized a network approach to examine relations between PTSD symptom clusters (intrusions, avoidance, negative alterations in cognitions and mood [NACM], alterations in arousal and reactivity [AAR]) and positive emotion dysregulation dimensions (nonacceptance, impulse control, goal-directed behavior). We identified (1) differential relations of PTSD symptom clusters with positive emotion dysregulation, and (2) central symptoms accounting for the PTSD and positive emotion dysregulation inter-group interconnections. Participants were 371 trauma-exposed community individuals (Mage = 43.68; 70.9% females; 34.5% white). We estimated a regularized Gaussian Graphic Model comprising four nodes representing the PTSD symptom clusters and three nodes representing positive emotion dysregulation dimensions. Study results indicated the key role of AAR and intrusions clusters in the PTSD group and impulse control difficulties in the positive emotion dysregulation group. Regarding cross-group connectivity patterns, findings indicate the pivotal role of AAR in positive emotion dysregulation dimensions and nonacceptance of positive emotions and impairment in goal-directed behavior in the context of positive emotions in PTSD symptom clusters. Thus, the current study indicates the potentially central role of particular PTSD symptom clusters and positive emotion dysregulation dimensions, informing assessment and treatment targets.
Keywords: trauma, posttraumatic stress disorder, positive emotion dysregulation, difficulties regulating positive emotions, positive emotion regulation, network analyses
1. Introduction
Traumatic exposure is highly prevalent globally (Benjet et al., 2016) and has serious and long-lasting health consequences (Chen et al., 2010; Norman et al., 2012; Smith, Goldstein, & Grant, 2016). Posttraumatic stress disorder (PTSD) is a chronic and debilitating mental health condition that is etiologically linked to traumatic exposure (American Psychiatric Association [APA], 2013). PTSD has a lifetime prevalence rate of 8.3% (Kilpatrick et al., 2013) and is characterized by intrusions (e.g., nightmares, flashbacks), avoidance of trauma-related internal (e.g., physical sensations, feelings) and external (e.g., people, places) cues, negative alterations in cognitions and mood (e.g., exaggerated self-blame, anhedonia), and alterations in arousal and reactivity (e.g., hypervigilance, exaggerated startle response; APA, 2013). These symptoms are associated with considerable disability and functional impairment (Bovin et al., 2016; Kilpatrick et al., 2013), even amongst individuals who do not meet full criteria for PTSD (Hellmuth, Jaquier, Swan, & Sullivan, 2014). Thus, research is needed to better understand factors that relate to the development and course of PTSD among trauma-exposed individuals.
Over the past decade, a growing body of research has shed light on the role of emotion dysregulation in PTSD symptomatology (Seligowski, Lee, Bardeen, & Orcutt, 2015). Emotion dysregulation is a multi-faceted construct involving maladaptive ways of responding to emotions including: (a) a lack of awareness, understanding, and acceptance of emotions; (b) an inability to control behaviors when experiencing emotional distress; (c) a lack of access to situationally appropriate strategies for modulating the duration and/or intensity of emotional responses to meet individual goals and situational demands; and (d) an unwillingness to experience emotional distress when pursuing meaningful activities in life (Gratz & Roemer, 2004; Gratz & Tull, 2010). Providing early evidence for this association, results from cross-sectional examinations within clinical (McDermott, Tull, Gratz, Daughters, & Lejuez, 2009; Weiss, Tull, Anestis, & Gratz, 2013; Weiss, Tull, Lavender, & Gratz, 2013) and non-clinical (Tull, Barrett, McMillan, & Roemer, 2007; Weiss et al., 2012) samples indicated that greater problems in any or all of the above-mentioned areas of emotion dysregulation were related to PTSD. Extending this work, longitudinal studies found that PTSD and emotion dysregulation were prospectively related to one another (Bardeen, Kumpula, & Orcutt, 2013; Weiss, Walsh, DiLillo, Messman-Moore, & Gratz, in press). Finally, treatments targeting emotion dysregulation have shown efficacy in alleviating PTSD symptoms (Cloitre, Koenen, Cohen, & Han, 2002; Harned, Korslund, Foa, & Linehan, 2012). Overall, existing empirical and intervention research establishes emotion dysregulation as a key factor in PTSD.
Notably, research in this area has focused almost exclusively on dysregulation stemming from negative emotional experiences. Recent advances suggest that some individuals experience positive emotion dysregulation; this parallels what is observed with negative emotions, and includes nonacceptance of positive emotions, difficulties controlling impulsive behaviors when experiencing positive emotions, and difficulties engaging in goal-directed activities when experiencing positive emotions (Weiss, Darosh, Contractor, Schick, & Dixon-Gordon, in press; Weiss, Gratz, & Lavender, 2015). Emerging evidence suggests that trauma-exposed individuals, especially those with greater PTSD severity, exhibit heightened positive emotion dysregulation (Weiss, Darosh, Contractor, Forkus, et al., in press; Weiss, Darosh, Contractor, Schick, et al., in press; Weiss, Dixon-Gordon, Peasant, & Sullivan, 2018). Such findings sustain even after adjusting for negative emotion dysregulation (Weiss, Nelson, Contractor, & Sullivan, in press).
Several explanations for a link between PTSD and positive emotion dysregulation have been described in the literature. Individuals with PTSD may take an evaluative stance toward positive emotions, judging them to be undesirable, unpredictable, or frightening. For instance, Weiss, Dixon-Gordon, et al. (2018) suggested that some individuals with PTSD experience positive emotions as aversive because they elicit physiological arousal that is a cue for trauma-related symptoms. Relatedly, Frewen and colleagues proposed that some individuals with PTSD respond to positive emotional stimuli with negative emotions (negative affect interference) as a result of anhedonia, which also may explain why positive emotions may be aversive among individuals with PTSD (Frewen, Dean, & Lanius, 2012; Frewen, Dozois, Neufeld, & Lanius, 2012). Alternatively, other research suggests that elevated impulsivity or reward-seeking among individuals with PTSD results in behavioral dyscontrol in the context of positive emotions (Weiss, Tull, Sullivan, Dixon-Gordon, & Gratz, 2015). This early work offers conceptual and empirical support for an association between PTSD and positive emotion dysregulation.
Extending these findings, the current study examined the utility of a network analysis methodology to examine the relation between PTSD symptom clusters and dimensions of positive emotion dysregulation. Network analysis models have gained increasing popularity in the psychopathology literature (Fried & Cramer, 2017) and have been applied to the study of PTSD (Afzali et al., 2017; Armour, Fried, Deserno, Tsai, & Pietrzak, 2017; Birkeland, Greene, & Spiller, in press; Contractor, Greene, Dolan, Weiss, & Armour, 2020; Greene, Gelkopf, Epskamp, & Fried, 2018; Ross, Murphy, & Armour, 2018). This statistical approach to investigating covariance amongst symptoms stems from current conceptualizations of psychopathology that recognize the systematic ways in which symptoms reinforce one another (Fried & Cramer, 2017). Within this framework, nodes (i.e., symptoms) are connected through edges (i.e., associations among symptoms), and symptoms that are centrally (versus peripherally) connected in the network are assumed to exert greater influence.
PTSD symptom clusters and dimensions of positive emotion dysregulation can be viewed as a network of mutually interacting and reinforcing symptoms (Epskamp, Borsboom, & Fried, 2018; McNally et al., 2015). For instance, PTSD intrusion symptoms characterized by arousal may be associated with greater nonacceptance of positive emotions that elicit arousal (Weiss, Dixon-Gordon, et al., 2018); this in turn, may maintain or exacerbate PTSD intrusion symptoms and, hence, PTSD symptom severity. Thus, certain PTSD symptoms may contribute to some aspects of positive emotion dysregulation, while some aspects of positive emotion dysregulation may exacerbate the severity of PTSD symptoms; such PTSD symptoms and aspects of positive emotion dysregulation are called bridge symptoms of a network (Cramer, Waldorp, van der Maas, & Borsboom, 2010b). In considering variables to be non-interchangeable (Fried & Cramer, 2017; McNally et al., 2015), an added advantage of a network framework is the ability to adjust for the influence of all variables when examining unique relations between two singular symptoms within or across constructs such as PTSD symptom clusters and dimensions of positive emotion dysregulation (Borsboom & Cramer, 2013). Such an approach further permits examining the influence of two variables on a third variable beyond just a direct relation between any two variables (Pearl, 2000), and considers the interaction between all symptoms in understanding construct co-occurrence (Fried & Cramer, 2017).
Despite the applicability of a network analytical approach to understand the inter-group relations between PTSD symptoms and positive emotion dysregulation, no study has examined this research question. Addressing this critical limitation, the current study investigated (1) differential relations of PTSD symptom clusters with aspects of positive emotion dysregulation; and (2) most central symptom clusters accounting for the PTSD and positive emotion dysregulation inter-group interconnections (bridge centrality). Consistent with existing research using a network perspective, we expected stronger associations among variables in the same group (i.e., PTSD and positive emotion dysregulation, separately). Within the PTSD group, evidence suggests that psychological reactivity, intrusive traumatic memories, detachment, and disinterest in activities are among the most central symptoms (Fried et al., 2018). While not yet studied using a network approach, cross-sectional examinations of positive emotion dysregulation indicate that difficulties controlling impulsive behavior in the context of positive emotions is most strongly associated with the other aspects of positive emotion dysregulation (Weiss, Darosh, Contractor, Schick, et al., in press; Weiss, Gratz, et al., 2015). Further, consistent with investigations using a network perspective, it was expected that the between-group (bridge) edges would be much weaker than the within-group edges. Again, while not tested using a network approach, findings from cross-sectional studies suggest that PTSD may be more strongly linked to nonacceptance of positive emotions and impairment in goal-directed behavior in the context of positive emotions (Weiss, Dixon-Gordon, et al., 2018).
Notably, despite some concerns regarding the usability of network analysis (Bringmann & Eronen, 2018), results may help to identify possible comorbidity mechanisms underlying the co-occurrence of PTSD and positive emotion dysregulation, thereby informing future studies examining etiology and course of these constructs (Cramer, Waldorp, van der Maas, & Borsboom, 2010a; Fried & Cramer, 2017). If replicated using longitudinal network analyses, identification of positive emotion dysregulation dimensions that are more strongly connected to PTSD symptoms could also inform intervention. For instance, interventions targeting symptom(s) with high bridge centrality may reduce the likelihood of a second phenomenon. Thus, application of a network approach to this area of study could inform the refinement of treatments for PTSD.
2. Method
2.1. Procedures
The study was approved by the [redacted] Institutional Review Board. It was described as a 30-minute study examining emotional experiences across racial and ethnic groups. Participants were recruited from Qualtrics Online Panels, an internet-based crowdsourcing platform that allows researchers to target specific populations. Research indicates that internet-based crowdsourcing platforms generate reliable data (Buhrmester, Kwang, & Gosling, 2011; Shapiro, Chandler, & Mueller, 2013) and represent the general population in terms of demographics (Mischra & Carleton, 2017) and prevalence of trauma and mental health problems (Shapiro et al., 2013). The inclusionary criteria included being >/= 18 years, having a working knowledge of English, residing in North America, and Asian, Black/African American, Hispanic/Latino/a, or White racial/ethnic background. Recruitment was stratified by race/ethnicity to assure equal representation of individuals from these four racial/ethnic groups. Eligible participants who provided informed consent and completed the entire online (i.e., Qualtrics) survey without failing validity checks received monetary compensation.
2.2. Exclusions, Missing Data, and Sample Characteristics
A total of 1,160 participants attempted the survey. We excluded participants for one or more of the following reasons: being < 18 years (n = 121); not having a working knowledge of English (n = 27); not residing in North America (n = 303); identifying as a race/ethnicity other than Asian, Black or African American, Hispanic or Latino/a, or White (n = 76; because the goal of the larger study was to examine racial and ethnic differences among highly represented groups in the United States); failing validity checks inserted to ensure attention and comprehension (n = 380; Meade & Craig, 2012; Oppenheimer, Meyvis, & Davidenko, 2009; Thomas & Clifford, 2017); and attempting to take the survey more than once (n = 24). We further excluded individuals endorsing no distressing event on the Life Events Checklist for DSM-5 (n = 63). The final sample of 371 participants averaged 43.68 years of age (SD = 14.80); Most participants were female (70.9%). Detailed information on demographics is provided in Table 1.
Table 1.
Demographic Data
| M (SD) | n (%) | |
|---|---|---|
| Age | 43.68 (14.80) | |
| Gender | ||
| Female | 263 (70.9%) | |
| Male | 104 (28.0%) | |
| Male to Female Transgender | 2 (0.5%) | |
| Female to Male Transgender | 1 (0.3%) | |
| Agender | 1 (0.3%) | |
| Sexual Identity | ||
| Straight | 332 (90.0%) | |
| Bisexual | 22 (6.0%) | |
| Lesbian or gay | 14 (3.8%) | |
| Asexual | 1 (0.3%) | |
| Race/Ethnicity | ||
| White | 128 (34.5%) | |
| Hispanic or Latinx | 120 (32.3%) | |
| African American/Black | 98 (26.4%) | |
| Asian | 85 (22.9%) | |
| Employment Status | ||
| Employed Full-time | 165 (45.5%) | |
| Not in labor force (student, homemaker) | 82 (22.6%) | |
| Unemployed | 67 (18.5%) | |
| Employed Part-time | 49 (13.5%) | |
| Family Annual Income | ||
| Less than $15,000 | 143 (53.2%) | |
| $15,000– $24,999 | 18 (6.8%) | |
| $25,000 – $34,999 | 26 (9.5%) | |
| $35,000 – $49,999 | 22 (8.2%) | |
| $50,000 – $64,999 | 30 (10.9%) | |
| $65,000 – $79,999 | 10 (3.7%) | |
| $80,000 or higher | 32 (12.0%) |
2.3. Measures
2.3.1. The Life Events Checklist for DSM-5 (LEC-5; Weathers, Blake, et al., 2013)
The LEC-5 is a 17-item self-report measure designed to screen for traumatic events in a respondent’s lifetime. It assesses exposure to 16 traumatic events, and the 17th item assesses stressful events not captured in the first 16 items. For each event, the respondent indicates if: a) it happened to them, b) they witnessed it, c) they learned about it, d) they experienced it as part of their job, e) they aren’t sure if they experienced it, or f) they didn’t experience it. Any of the first four response options indicated a positive Criterion A traumatic event endorsement. An additional item was included to ascertain participants’ most distressing traumatic event. The LEC has demonstrated convergent validity with measures assessing traumatic exposure and psychopathology known to relate to traumatic exposure (Gray, Litz, Hsu, & Lombardo, 2004). See Table 2 for prevalence rates for the most distressing traumatic events.
Table 2.
Percentage of Index Trauma Types
| Trauma Types |
|---|
| Transportation accident (for example, car accident, boat accident, train wreck, plane crash) |
| Sexual assault (rape, attempted rape, made to perform any type of sexual act through force or threat of harm) |
| Natural disaster (for example, flood, hurricane, tornado, earthquake) |
| Any other very stressful event or experience |
| Physical assault (for example, being attacked, hit, slapped, kicked, beaten up) |
| Life-threatening illness or injury |
| Sudden accidental death |
| Other unwanted or uncomfortable sexual experience |
| Assault with a weapon (for example, being shot, stabbed, threatened with a knife, gun, bomb) |
| Fire or explosion |
| Serious accident at work, home, or during recreational activity |
| Severe human suffering |
| Sudden violent death (for example, homicide, suicide) |
| Combat or exposure to a war-zone (in the military or as a civilian) |
| Exposure to toxic substance (for example, dangerous chemicals, radiation) |
| Captivity (for example, being kidnapped, abducted, held hostage, prisoner of war) |
| Serious injury, harm, or death you caused to someone else |
2.3.2. The PTSD Checklist for DSM-5 (PCL-5; Weathers, Litz, et al., 2013)
The PCL-5 is a 20-item self-report measure that assesses PTSD symptoms stemming from the traumatic event identified as most distressing on the LEC-5. The PCL-5 items have a five-point Likert-type scale (0 = not at all, 4 = extremely). The PCL-5 has excellent psychometric properties (Bovin et al., 2016; Wortmann et al., 2016). Internal consistency in the current sample was excellent for each of the symptom clusters (αs = .93, .90, .94, and .91 for intrusions, avoidance, NACM, and AAR, respectively).
2.3.3. The Difficulties in Emotion Regulation Scale – Positive (DERS-P; Weiss, Gratz, et al., 2015)
The DERS-P is a 13-item self-report measure that assesses positive emotion dysregulation, specifically nonacceptance of positive emotions (Accept), difficulties engaging in goal-directed behaviors when experiencing positive emotions (Goals), and difficulties controlling impulsive behaviors when experiencing positive emotions (Impulse). Participants rated items using a 5-point Likert-type scale (1 = almost never, 5 = almost always). The DERS-P has excellent psychometric properties (Weiss, Darosh, Contractor, Schick, et al., in press; Weiss, Gratz, et al., 2015). Internal consistency in the current sample was good to excellent for the dimensions (αs = .94, .86, and .95 for Accept, Goals, and Impulse, respectively).
2.4. Data Analysis
For a partial correlation network of seven nodes, we had 21 parameters (Epskamp & Fried, 2018). Following used practices at least three-five individuals per parameter, our sample size was sufficient for exploratory data-driven analyses. Notably, we used the word “group” to reference nodes of the same construct; thereby, PTSD symptom clusters and positive emotion dysregulation, each represented a conceptually distinct group of nodes within that construct.
Network Estimation, Visualization, and Accuracy
None of the variables violated normality (skewness > 3 and kurtosis > 10; Kline, 2015). Thus, the appropriate Pairwise Markov Random Field (PRMF) model was the Gaussian Graphical Model (GGM; Costantini et al., 2015), which was used to estimate an undirected network (Cox & Wermuth, 1994; McNally et al., 2015). To reduce the likelihood of spurious edges and obtain a parsimonious network, we estimated a regularized partial correlation network structure with Pearson correlations, using the graphical least absolute shrinkage and selection operator (glasso; Epskamp & Fried, 2018; Friedman, Hastie, & Tibshirani, 2008). Further, we used the Extended Bayesian Information Criterion (EBIC; Chen & Chen, 2008) to select a value for the tuning parameter.
In the current network, a node indicated a variable of interest (averaged score of each of the four PTSD symptom clusters; averaged score of each of the three positive emotion dysregulation clusters) and an edge depicted a regularized partial correlation between two nodes after statistically controlling for other nodes in the network (Borsboom & Cramer, 2013). For each edge, we examined its weight reflecting strength and sign reflecting whether the association is positive or negative (Costantini et al., 2019); weights were graphically represented by line thickness (Borsboom & Cramer, 2013; Costantini et al., 2019). The network’s graphical layout was based on the Fruchterman-Reingold algorithm (Fruchterman & Reingold, 1991) which placed connected nodes closer and unconnected nodes farther apart. We used the bootnet v. 1.2.4 (Epskamp et al., 2018) and qgraph v. 1.6.1 (Epskamp, Cramer, Waldorp, Schmittmann, & Borsboom, 2012) packages in R. Additionally, to examine network accuracy, we estimated confidence intervals (CIs) on the edge-weights (nonparametric bootstrapping with replacement; Supplementary Figure A. 1) and significant differences between the obtained edge-weights (bootstrapped difference test; Supplemental Figure A. 2; Epskamp et al., 2018).
Finally, to quantify the relative strength of each of the 7 nodes in the network, we examined the centrality index of node strength (Costantini et al., 2019; McNally et al., 2015) with the R package qgraph (Epskamp et al., 2012). Node strength references the sum of weights (i.e., regularized partial correlation magnitudes) of each edge linked to that particular node (Epskamp & Fried, 2018). Higher values reflect a node’s greater centrality to the overall network (Epskamp & Fried, 2018). We further examined node strength stability under observing subsets of cases (case-dropping subset bootstrap; Supplemental Figure A. 3; Epskamp et al., 2018) by computing the correlation stability (CS) coefficient with the R package bootnet (Epskamp et al., 2018). The CS coefficient quantifies the proportion of data that can be dropped to retain a correlation of ≥.70 with the original centrality coefficient at a 95% certainty level (Epskamp & Fried, 2018). Guidelines suggest to not interpret a centrality index if the CS-coefficient is < .25, and a value of .50 indicates sufficient stability (Costantini et al., 2019; Epskamp & Fried, 2018).
Bridge Centrality
To examine cross-group connectivity patterns, we examined bridge centrality values for each node of the network (Jones, Ma, & McNally, 2019, April 25). Using the R package networktools, we first computed bridge strength; this index is the sum of the absolute values of edges between a node of one group and all nodes of the second group (i.e., node’s total connectivity with the other group).
3. Results
Network Estimation, Visualization, and Accuracy
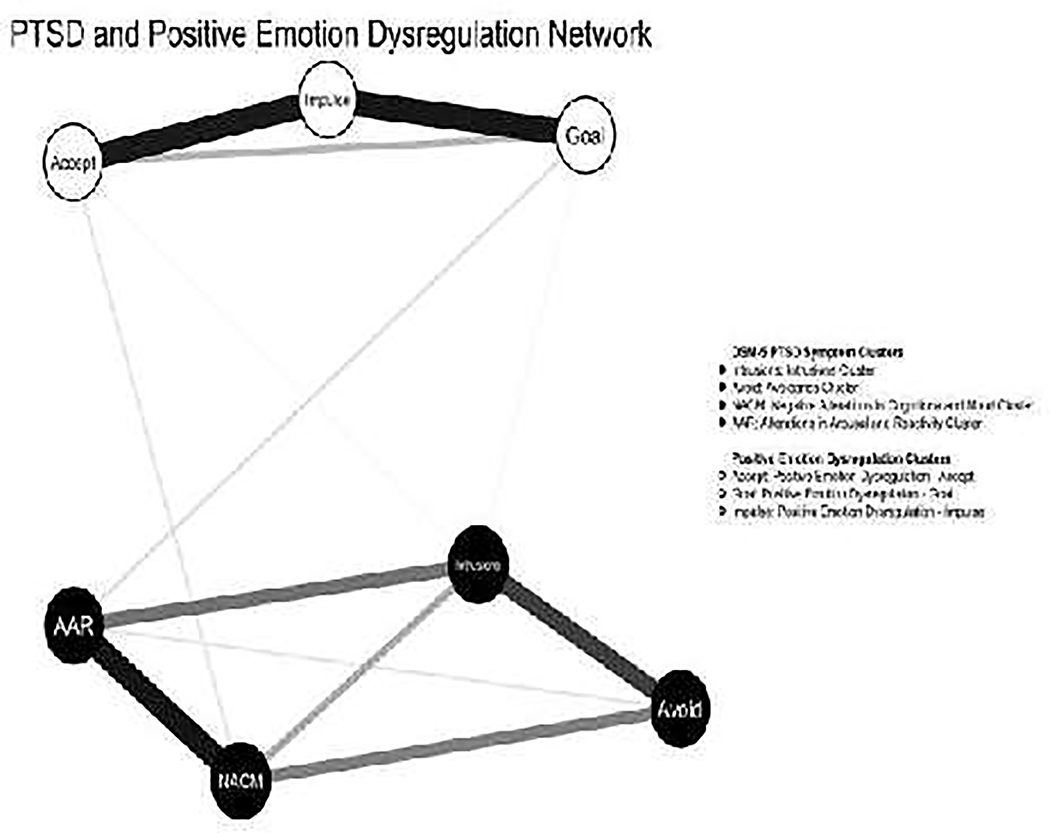
Figure 1 indicates the regularized partial correlation network corresponding to Table 2 values. Associations among all of the study variables were positive. Examining the edge weights within the PTSD symptom clusters group, the strongest edges were between AAR and NACM (.57), intrusions and avoidance (.43), and between intrusions and AAR (.30). Within the positive emotion dysregulation group, the strongest edges were between Accept and Impulse (.55) and Goals and Impulse (.56).
Figure 1. Regularized partial correlation network.
Note. Solid lines indicate positive associations; there were no negative associations
The between-group (bridge) edges were much weaker than the within-group edges. AAR was positively associated with Accept (.01), Goals (.06), and Impulse (.002). Further, intrusions was positively associated with Accept and Goals (.02 each). Lastly, NACM was positively associated with Accept (.05). Further, for the PTSD and positive emotion dysregulation groups, all nodes within each group had edges with other nodes of that same group. Across these groups, positive emotion dysregulation-accept and positive emotion dysregulation-goal, each had two edges with nodes of the PTSD group; and AAR and intrusions, each had two edges with nodes of the positive emotion dysregulation group.
Regarding network accuracy (Supplemental Figures 1 and 2), results indicated that the NACM-AAR edge weight was significantly stronger than other edge weights, excluding the Goals with Impulse edge weight and the Accept with Impulse edge weight. Further, the Goals with Impulse, the Accept with Impulse, and the intrusions with avoidance edge weights were significantly stronger than more than half of the other edge weights. Finally, the CS-coefficient for node strength (CS[cor = 0.7] = 0.52) indicates interpretability and stability under subsetting cases.
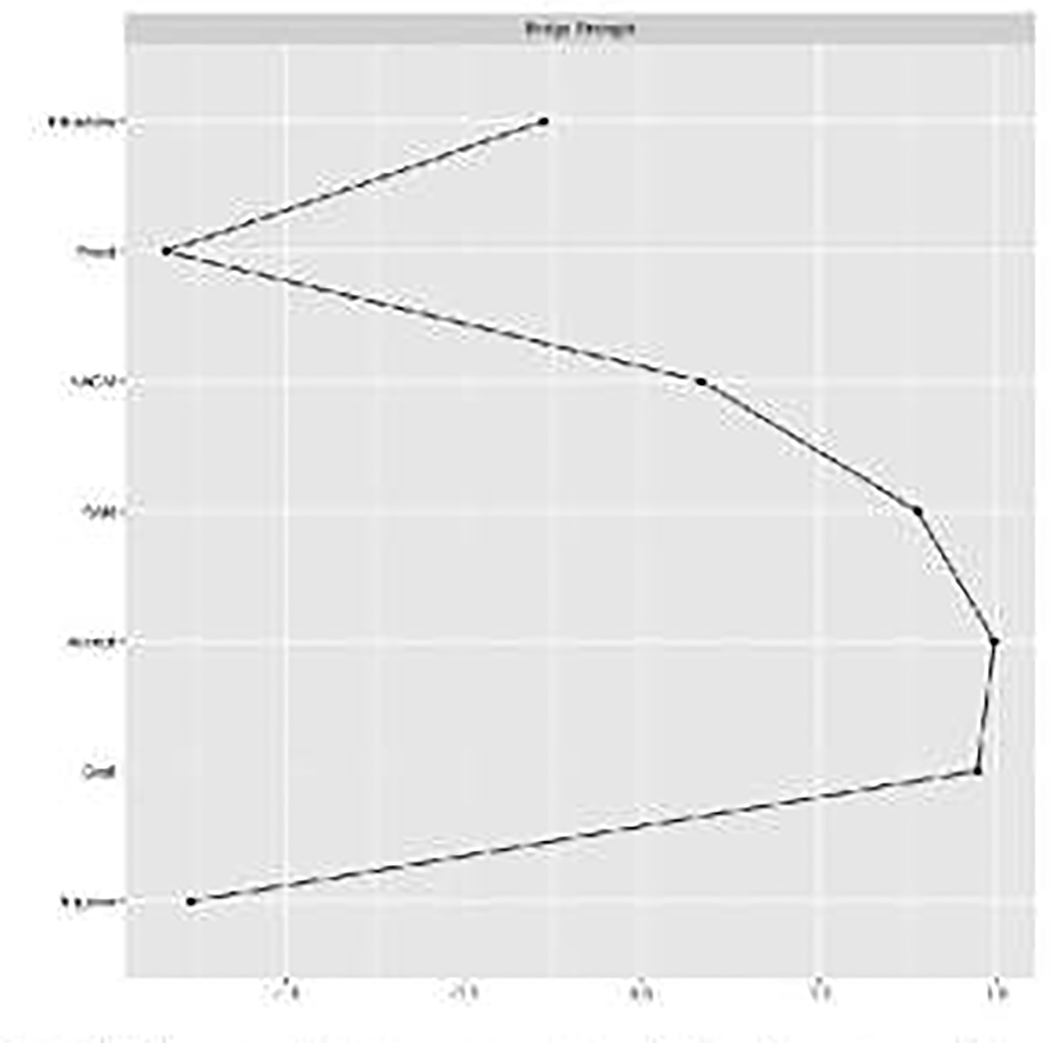
Bridge Centrality
Standardized bridge centrality indices are presented in Figure 2. From the PTSD cluster group, AAR (followed by NACM) had the highest bridge associations with positive emotion dysregulation dimensions (associations could be in either direction). From the positive emotion dysregulation group, Accept and Goals had the highest bridging associations with PTSD symptom clusters (associations could be in either direction).
Figure 2. Bridge centrality.
Note. NACM = negative alterations in cognitions and mood. AAR = alterations in arousal and reactivity. Accept = nonacceptance of positive emotions. Goals = difficulties engaging in goaldirected behaviors when experiencing positive emotions. Impulse = difficulties controlling impulsive behaviors when experiencing positive emotions
4. Discussion
PTSD symptom clusters have empirically-established associations with positive emotion dysregulation (Weiss, Darosh, Contractor, Forkus, et al., in press; Weiss, Darosh, Contractor, Schick, et al., in press; Weiss, Dixon-Gordon, et al., 2018; Weiss, Nelson, et al., in press). Extending existing literature in this area, the current study uniquely applied a network methodology to explore the relations between PTSD symptom clusters and dimensions of positive emotion dysregulation among trauma-exposed community individuals. Primarily, study results indicated the role of PTSD AAR and positive emotion dysregulation Accept and Goals driving inter-group associations. Results advance our understanding of the relation between PTSD symptoms and positive emotion dysregulation, underscoring aspects of these constructs that may be of particular relevance to future research and practice.
Referencing inter-group connections, the AAR symptom cluster had the highest bridge associations with positive emotion dysregulation dimensions. As one example, this finding aligns with the suggestion that arousal may underlie positive emotion dysregulation among individuals with PTSD (Weiss, Dixon-Gordon, et al., 2018). PTSD has been linked to heightened physiological arousal to positive emotional stimuli (Litz, Orsillo, Kaloupek, & Weathers, 2000). Among individuals with PTSD symptoms, the arousal that accompanies some positive emotions may be experienced as distressing, perhaps because of the association of arousal to PTSD symptoms (APA, 2013). Thus, over time, fear of arousal originally associated with trauma cues may generalize to other stimuli that elicit arousal such as some positive emotions (Roemer, Litz, Orsillo, & Wagner, 2001). In turn, individuals may respond to arousing positive emotions with nonacceptance, and may engage in behaviors that are impulse or not aligned with their goals to escape or avoid these emotional experiences. There is also evidence from a dynamic network analysis based on intensive longitudinal data that indicates that arousal drives negative emotions (Greene, Gelkopf, Fried, Robinaugh, & Lapid Pickman, in press). Thus, it may be that a feedback loop exists in which positive emotions lead to arousal, which in turn leads to negative emotions, thereby creating a cycle of emotional dysregulation.
Existing research also provides evidence for an association of other AAR symptoms beyond hyperarousal and startle to positive emotion dysregulation. For instance, deficits in the ability to inhibit prepotent responses and take into account the consequences of an action have been linked to both positive emotion dysregulation and risk-taking (Billieux, Gay, Rochat, & Van der Linden, 2010), which may help explain the role of positive emotion dysregulation in AAR externalizing symptoms (e.g., PTSD Criterion E1 and E2). These findings suggest that the AAR symptom cluster may play a significant role in both PTSD and its correlates.
Two dimensions from the positive emotion dysregulation group were found to have the highest bridging associations with PTSD symptom clusters: Accept (particularly related to AAR, intrusions, and NACM) and Goals (particularly related to AAR and intrusions). Regarding Accept, our results indicate that a tendency to take a judgmental and evaluative stance toward positive emotional states may be strongly related to PTSD symptoms following trauma. Trauma-exposed individuals who are nonaccepting of positive emotions may be more likely to engage in efforts to control, suppress, or otherwise avoid these and other emotion states (Roemer et al., 2001). This, in turn, may have paradoxical effects, increasing PTSD symptoms and related distress. Indeed, related to the intrusions symptom cluster, suppressing thoughts may increase their frequency, intensity, and duration (Wegner, Schneider, Carter, & White, 1987). Further, individuals who are non-accepting of positive emotions may begin to exhibit negative affect interference (Frewen, Dean, et al., 2012), which could lead to trouble experiencing positive emotions (a NACM symptom). Further, related to the AAR cluster, individuals who respond to positive emotions judgmentally may use risky behaviors (e.g., substances) to alleviate or distract from positive emotional states perceived as aversive, consistent with negative reinforcement (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004; Chapman, Gratz, & Brown, 2006).
Consistent with our empirical findings, theoretical links between problems focusing attention and completing tasks when experiencing positive emotions (i.e., positive emotion dysregulation-goals) and PTSD symptom clusters (AAR and intrusions in particular) are also evident. For instance, attentional deficits in the context of positive emotion may result in or stem from difficulties concentrating, one AAR symptom. Alternatively, intrusive traumatic memories may make it difficult for trauma-exposed individuals to focus attention or complete tasks when experiencing positive emotions. Research is needed to test these hypotheses.
Regarding intra-group connections, AAR and intrusions symptom clusters had relatively strong associations (i.e., edge weights) with other PTSD symptom clusters. Further, the association between AAR and NAMC was significantly stronger than other relations. Findings for AAR align with previous research in this area highlighting the central role of this cluster in influencing other PTSD symptom clusters. For instance, Schell, Marshall, and Jaycox (2004) found that AAR strongly influenced - but was not generally influenced by – other PTSD symptom clusters, and that individuals for whom AAR was most pronounced at baseline showed the least improvement in PTSD over time. Other research highlights the role of intrusions in the etiology and course of PTSD. For instance, intrusive memories (particularly those that elicit distress, lack time perspective, and lack context) have been found to distinguish between trauma-exposed individuals who go on to develop versus not develop PTSD (Ehlers, Hackmann, & Michael, 2004), and results of Sullivan, Smith, Lewis, and Jones (2018) show that intrusions have the strongest influence on other symptoms. Less understood is why the association between AAR and NACM was so strong compared to relations among the other PTSD symptom clusters. One possible reason may be drawn from factor-analytical research wherein some symptoms of AAR and NACM have been found to comprise of a common factor of dysphoria (Contractor et al., 2014; Contractor, Greene, Dolan, & Elhai, 2018); indicating a possible statistically-strong relation between some of the AAR and NACM symptoms. Future research that explores this question is warranted, including that examining symptoms.
Extending existing knowledge, positive emotion dysregulation Impulse was found to have the strongest intra-group connections. Given the recent development of a measure of positive emotion dysregulation (Weiss, Darosh, Contractor, Schick, et al., in press; Weiss, Gratz, et al., 2015), there is limited understanding of the ways in which positive emotion dysregulation dimensions interact. Our findings suggest that a tendency toward behavioral dyscontrol in the context of positive emotions may serve as a pivotal feature of positive emotion dysregulation, perhaps underlying the development, maintenance, and exacerbation of other aspects of positive emotion dysregulation such as nonacceptance of positive emotions. Future longitudinal studies are needed to better understand the ways in which positive emotion dysregulation dimensions influence one another across time.
Our study results need to be considered in light of limitations specific to a network perspective to disorders. First and foremost, the theoretical foundations of network models have been a focus of debate in the existing literature. Network and latent variable perspectives have been compared in terms of their underlying premise of whether co-occurring symptoms interact dynamically to reflect a disorder versus share a common underlying cause (Borsboom & Cramer, 2013). As of late, research has examined whether these differences are better represented (1) as being symptom- vs. syndrome-oriented, and (2) as dynamic vs. static (Bringmann & Eronen, 2018). The current investigation is not confined to any of these perspectives. Instead, a network approach was applied here because (a) it was determined to be more appropriate to explore our hypotheses related to cross-construct relations versus identifying underlying clusters or factors, and (b) allowed us to examine bridge centrality, not possible with more traditional factor analyses. Our results provide further impetus to explore the PTSD-positive emotion dysregulation relation using network and latent variable approaches (Bringmann & Eronen, 2018; Forbes et al., 2017).
Second, there are some concerns about replicability of network models (e.g., estimates of edges, most central nodes, rank-order of node centrality attributed to measurement error of nodes; Forbes, Wright, Markon, & Krueger, 2017). Given that a network methodology is data-driven, and hence specific to the characteristics of this sample (Epskamp et al., 2018), replication in other samples is needed to establish generalizability of findings. Third, while network analysis provides a more fine-grained approach to understanding the relations between aspects of PTSD and positive emotion dysregulation, the cross-sectional and correlational nature of the data precludes determination of the precise nature and direction of the examined associations. Recently, network analysis has been applied to longitudinal data (e.g., derived from ecological momentary assessment). Prospective and longitudinal investigations of the relation between PTSD and positive emotion dysregulation using network analysis are needed.
Fourth, examining the individual PTSD symptoms would have provided more nuanced results; however, our sample size was insufficient for examining resulting 23 nodes and 253 parameters (minimum recommended sample size of 760 individuals based on used practices). Thus, we chose to examine PTSD symptom clusters vs. items to preserve statistical power; this is a worthwhile area of future research. Fifth, gender and trauma types have shown to relate to PTSD severity (Contractor, Caldas, Fletcher, Shea, & Armour, 2018; Lilly, Pole, Best, Melzler, & Marmar, 2009) as well as positive emotion dysregulation (Weiss, Darosh, Contractor, Schick, et al., in press; Weiss, Gratz, et al., 2015). Thus, the scientific value of the obtained results would have increased by examining the moderating impact of gender and trauma types on the network model. However, splitting up the sample by gender (104 males and 263 females) or by interpersonal vs. non-interpersonal index trauma types (124 vs. 247, respectively) would leave us with a small and insufficient sample size and inadequate power to conduct these moderation analyses; and conducting these moderation analyses would have resulted in five network analyses transcending the scope as well as the research questions of the current study. Examining these moderating impacts with a larger sample size is a worthwhile area of future research.
Sixth, it is possible that using other types of network analyses may result in more dense networks, and future studies could investigate how well these findings replicate in larger samples, and using other network algorithms. Seventh, the current study did not examine the influence of negative emotion dysregulation in the relations between PTSD and positive emotion dysregulation. While there is some evidence to suggest that the association of positive emotion dysregulation to PTSD is weaker than that of negative emotion dysregulation to PTSD (e.g., Weiss, Forkus, Contractor, & Dixon-Gordon, in press; Weiss, Nelson, et al., in press), recent investigations indicate that the PTSD-positive emotion dysregulation relation remains significant when negative emotion dysregulation is included in the model (Weiss, Forkus, Contractor, & Dixon-Gordon, in press; Weiss, Nelson, et al., in press). Nonetheless, individuals with more severe PTSD symptoms may have wider difficulties in emotion dysregulation, including negative emotion dysregulation, suggesting the need for future studies in this area.
Beyond limitations related to our network model, it should be noted that collecting data via the internet has disadvantages that may limit generalizability of results (e.g., sample bias; Kraut et al., 2004). However, an online recruitment platform is a notable strength of our study; these platforms tend to have more diverse subject pools; represent the U.S. population in several demographic and clinical characteristics (including trauma prevalence); and generate reliable data (Buhrmester, Kwang, & Gosling, 2011; Shapiro, Chandler, & Mueller, 2013). Thus, while a strength, future research that integrates other data collection methods is necessary. Finally, we require replications of this study across more diverse samples of trauma-exposed individuals (e.g., treatment-seeking).
In conclusion, the findings of the current study extend research on the relation between PTSD and positive emotion dysregulation by highlighting the role of the AAR symptom cluster and positive emotion dysregulation Accept and Goals in accounting for inter-group associations. Our study results have important clinical implications pending further empirical investigations and replications. Specifically, our results indicate that certain aspects of positive emotion dysregulation such as nonacceptance of positive emotions and difficulties engaging in goal-directed behavior in the context of positive emotions may be particularly impaired in relation to severity of PTSD symptom clusters. Following from this, trauma-exposed individuals may benefit from examination and monitoring of deficits in positive emotion dysregulation. Further, PTSD interventions that target positive emotion dysregulation may lead to more efficacious outcomes, particularly given evidence that positive emotion dysregulation is related to problems that frequently co-occur with PTSD such as depression (Schick, Weiss, Contractor, Dixon-Gordon, & Spillane, in press), substance use (Weiss, Forkus, Contractor, & Schick, 2018; Weiss, Risi, Bold, Sullivan, & Dixon-Gordon, in press), and risky sexual behavior (Weiss, Forkus, et al., in press). Future investigations that address the clinical utility of targeting positive emotion dysregulation in the assessment and treatment of PTSD are warranted.
Supplementary Material
Table 3.
Regularized partial correlation matrix
| M | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|---|---|
| 1. PTSD Intrusions | 6.37 | 6.05 | 0 | .43 | .17 | .30 | .02 | .02 | 0 |
| 2. PTSD Avoidance | 2.87 | 2.70 | 0 | .27 | .05 | 0 | 0 | 0 | |
| 3. PTSD NACM | 8.29 | 8.49 | 0 | .57 | .05 | 0 | 0 | ||
| 4. PTSD AAR | 6.98 | 6.87 | 0 | .01 | .06 | .002 | |||
| 5. Positive Emotion Dysregulation – Accept | 5.25 | 3.10 | 0 | .14 | .55 | ||||
| 6. Positive Emotion Dysregulation – Goals | 5.79 | 2.93 | 0 | .56 | |||||
| 7. Positive Emotion Dysregulation – Impulse | 6.53 | 3.61 | 0 |
Note. PTSD = posttraumatic stress disorder. NACM = negative alterations in cognitions and mood. AAR = alterations in arousal and reactivity. Accept = nonacceptance of positive emotions. Goals = difficulties engaging in goal-directed behaviors when experiencing positive emotions. Impulse = difficulties controlling impulsive behaviors when experiencing positive emotions.
Highlights.
Network approach was used to examine PTSD and positive emotion dysregulation
AAR and intrusions clusters had a key role in the PTSD symptom cluster community
Impulse control had a key role in the positive emotion dysregulation community
AAR cluster had a key role in positive emotion dysregulation dimensions
Nonacceptance and goal-directed behavior had a key role in PTSD symptom clusters
Acknowledgements
The authors would like to thank Nazaret Suazo for her assistance with this project.
Work on this paper by the first author (NHW) was supported by National Institute on Drug Abuse grant K23DA039327.
Appendix A. R syntax for network analyses of PTSD symptom clusters and positive emotion dysregulation facets
### Loading Packages ### install.packages(“qgraph”) library(qgraph) install.packages(“bootnet”) library(bootnet) install.packages (“haven”) library(haven) install.packages(“Rcpp”) library(Rcpp) install.packages(“foreign”) library (foreign) install.packages(“corpcor”) library(corpcor) ### Reading Data ### data <- read.csv(“Network analyses data.csv”, header = TRUE) attach(data) ### Graph Components ### ### Creating a vector with the short names of the data ### short.names <- c(“Intrusions”, “Avoid”, “NACM”, “AAR”, “Accept”, “Goal”, “Impulse”) ### Creating a vector with the long names of the data ### long.names <- c(“Intrusions Cluster”, “Avoidance Cluster”, “Negative Alterations in Cognitions and Mood Cluster”, “Alterations in Arousal and Reactivity Cluster”, “Positive Emotion Dysregulation - Accept”, “Positive Emotion Dysregulation - Goal”, “Positive Emotion Dysregulation - Impulse”) ### Creating groups and color coding the groups ### groups <- list(“DSM-5 PTSD Symptom Clusters” = c(1:4), “Positive Emotion Dysregulation Clusters” = c(5:7)) colour<-list(“DSM-5 PTSD Symptom Clusters” = c(1:4), “Positive Emotion Dysregulation Clusters” = c(5:7)) ### Setting column names for the data ### colnames(Network_analyses_data_PTSD_and_PE) <- short.names View(data) ### Estimating Networks ### ### Regularized partial correlation network ### ggm <- estimateNetwork(Network_analyses_data_PTSD_and_PE, default = “EBICglasso”, verbose = FALSE) ### Adjacency matrix for the GGM model ### getWmat(ggm) write.csv(ggm, “adjacencymatrix.csv”) ### Storing the matrix into an R variable ### adj.ggm <- getWmat(ggm) ### Printing the variable holding the edge weights matrix ### round(adj.ggm, 3) ### Exporting the generated data ### write.csv(adj.ggm, “edgeweights.csv”) #Estimating the network ### network<- qgraph(adj.ggm, layout = “spring”, labels = short.names, nodeNames = long.names, groups=colour, cut = 0, vsize = 6, border.width = 1.5, theme = “colorblind”, legend.cex = .20, title = “PTSD and Positive Emotion Dysregulation Network”) ### Plotting the network and saving as PDF ### pdf(“Network.pdf”, width=6.5, height=4) qgraph(network, layout = “spring”, labels = short.names, nodeNames = long.names, groups = colour, cut = 0, vsize = 6, border.width = 1.5, theme = “colorblind”, negDashed=TRUE, legend.cex = .2, title = “PTSD and Positive Emotion Dysregulation Network”) dev.off() ### Plotting the network and saving it as TIFF ### tiff(“Network.tiff”, width=6.5, height=4, units=“in”, res=800, compression=“lzw”) qgraph(network, layout = “spring”, labels = short.names, nodeNames = long.names, groups = colour, cut = 0, vsize = 6, border.width = 1.5, theme = “colorblind”, negDashed=TRUE, legend.cex = .2) dev.off() ### Grayscale PDF ### pdf(“Network grayscale.pdf”, width=6.5, height=4) qgraph(getWmat(ggm), layout = “spring”, labels = short.names, nodeNames = long.names, groups = colour, cut = 0, vsize = 6, border.width = 1.5, theme = “gray”, negDashed=TRUE, legend.cex = .2, title = ““) dev.off() ### Grayscale TIFF ### tiff(“Network grayscale.tiff”, width=6.5, height=4, units=“in”, res=800, compression=“lzw”) qgraph(network, layout = “spring”, labels = short.names, nodeNames = long.names, groups = colour, cut = 0, vsize = 6, border.width = 1.5, theme = “gray”, negDashed=TRUE, legend.cex = .2) dev.off() ### Edge weights accuracy ### ### Running the non-parametric bootstrap ### boot.edges <- bootnet(ggm, nboots = 2000, nCores = 8) ### Plotting the 95% bootstrapped confidence intervals ### plot(boot.edges, labels = TRUE, order = “sample”) ### Printing edge weight bootstrap as a PDF ### pdf(“Bootnet - edge weights accuracy.pdf”) plot(boot.edges, labels = TRUE, order = “sample”) dev.off() ### Printing edge weight bootstrap as TIFF ### tiff(“Edge Weight Accuracy.tiff”, width=8, height=8, units=“in”, res=800, compression=“lzw”) plot(boot.edges, labels = TRUE, order = “sample”) dev.off() ### Edge weights difference plot ### plot(boot.edges, “edge”, plot = “difference”, onlyNonZero = TRUE, order = “sample”) ### PDF for edge weights difference plot ### pdf(“Bootnet - edge weights difference.pdf”) plot(boot.edges, “edge”, plot = “difference”, onlyNonZero = TRUE, order = “sample”) dev.off() ### TIFF for edge weights difference plot ### tiff(“Edge Weight Difference.tiff”, width=8, height=8, units=“in”, res=800, compression=“lzw”) plot(boot.edges, “edge”, plot = “difference”, onlyNonZero = TRUE, order = “sample”) dev.off() ### Centrality stability ### ### Case-dropping subset bootstrap ### boot.centrality <- bootnet(ggm, nboots = 3000, nCores = 8, type = “case”) ### Plot of the centrality stability results ### plot(boot.centrality) ### Plot as PDF ### pdf(“Bootnet - centrality stability.pdf”) plot(boot.centrality) dev.off() ### Numerical value of the correlation stability coefficient ### cs<-corStability(boot.centrality) write.csv(corStability(boot.centrality), “Stability.csv”) cs ### Centrality difference plot for strength centrality ### ### Plot as PDF ### pdf(“Bootnet - centrality difference.pdf”) plot(boot.edges, “strength”, plot = “difference”, order=“mean” ) dev.off() ### Bridge centrality ### ### Packages ### library(networktools) ### Bridge centrality estimation ### A<-qgraph(ggm$graph, labels=long.names, layout=“spring”, vsize=6, cut=0, border.width=1.5, border.color=“black”, groups=groups, color=c(‘#FFFACD’, ‘#D7BDE2’, ‘#AED6F1’, ‘#DAF7A6’, ‘#F5B7B1’), nodeNames = short.names,legend.cex=.4) B<-bridge(A, communities = groups, directed=FALSE) ### Bridge centrality values ### B ### Bridge centrality plots as PDF ### pdf(“Bridge centrality.pdf”, width=8, height=8) plot(B, include=c(“Bridge Strength”), zscore = TRUE) dev.off() ## Bridge centrality plots as TIFF ### tiff(“Bridge centrality.tiff”, width=8, height=8, units=“in”, res=800, compression=“lzw”) plot(B, include=c(“Bridge Strength”), zscore = TRUE) dev.off()
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Afzali MH, Sunderland M, Batterham PJ, Carragher N, Calear A, & Slade T (2017). Network approach to the symptom-level association between alcohol use disorder and posttraumatic stress disorder. Social Psychiatry and Psychiatric Epidemiology, 52, 329–339. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Armour C, Fried EI, Deserno MK, Tsai J, & Pietrzak RH (2017). A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in US military veterans. Journal of Anxiety Disorders, 45, 49–59. [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review, 111, 33–51. [DOI] [PubMed] [Google Scholar]
- Bardeen JR, Kumpula MJ, & Orcutt HK (2013). Emotion regulation difficulties as a prospective predictor of posttraumatic stress symptoms following a mass shooting. Journal of Anxiety Disorders, 27, 188–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benjet C, Bromet E, Karam EG, Kessler RC, McLaughlin KA, Ruscio AM, … Hill E (2016). The epidemiology of traumatic event exposure worldwide: results from the World Mental Health Survey Consortium. Psychological Medicine, 46, 327–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billieux J, Gay P, Rochat L, & Van der Linden M (2010). The role of urgency and its underlying psychological mechanisms in problematic behaviours. Behaviour Research and Therapy, 48, 1085–1096. [DOI] [PubMed] [Google Scholar]
- Birkeland MS, Greene T, Spiller TR (in press). The network approach to posttraumatic stress disorder (PTSD): A systematic review (in press). European Journal of Psychotraumatology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsboom D, & Cramer AO (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9, 91–121. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28, 1379–1391. [DOI] [PubMed] [Google Scholar]
- Bringmann LF, & Eronen MI (2018). Don’t blame the model: Reconsidering the network approach to psychopathology. Psychological Review, 125, 606–615. [DOI] [PubMed] [Google Scholar]
- Chapman AL, Gratz KL, & Brown MZ (2006). Solving the puzzle of deliberate self-harm: the experiential avoidance model. Behavior Research & Therapy, 44, 371–394. [DOI] [PubMed] [Google Scholar]
- Chen LP, Murad MH, Paras ML, Colbenson KM, Sattler AL, Goranson EN, … Prokop LJ (2010). Sexual abuse and lifetime diagnosis of psychiatric disorders: Systematic review and meta-analysis. Mayo Clinic Proceedings, 85, 618–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor AA, Caldas S, Fletcher S, Shea MT, & Armour C (2018). Empirically-derived lifespan polytraumatization typologies: A systematic review. Journal of Clinical Psychology, 74, 1137–1159. [DOI] [PubMed] [Google Scholar]
- Contractor AA, Durham TA, Brennan JA, Armour C, Wutrick HR, Frueh BC, & Elhai JD (2014). DSM-5 PTSD’s symptom dimensions and relations with major depression’s symptom dimensions in a primary care sample. Psychiatry Research, 215, 146–153. [DOI] [PubMed] [Google Scholar]
- Contractor AA, Greene T, Dolan M, & Elhai JD (2018). Relations between PTSD and depression symptom clusters in samples differentiated by PTSD diagnostic status. Journal of Anxiety Disorders, 59, 17–26. [DOI] [PubMed] [Google Scholar]
- Contractor AA, Greene T, Dolan M, Weiss NH, & Armour C (2020). Relation between PTSD clusters and positive memory characteristics: A network perspective. Journal of Anxiety Disorders, 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramer AOJ, Waldorp LJ, van der Maas HLJ, & Borsboom D (2010a). Comorbidity: A network perspective. The Behavioral and Brain Sciences, 33, 137–150. [DOI] [PubMed] [Google Scholar]
- Cramer AOJ, Waldorp LJ, van der Maas HLJ, & Borsboom D (2010b). Complex realities require complex theories: Refining and extending the network approach to mental disorders. Behavioral and Brain Sciences, 33, 178–193. [Google Scholar]
- Ehlers A, Hackmann A, & Michael T (2004). Intrusive re- experiencing in post- traumatic stress disorder: Phenomenology, theory, and therapy. Memory, 12, 403–415. [DOI] [PubMed] [Google Scholar]
- Epskamp S (2016). Brief report on estimating regularized gaussian networks from continuous and ordinal data. arXiv preprint arXiv:1606.05771. [Google Scholar]
- Epskamp S, Borsboom D, & Fried EI (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50, 195–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forbes MK, Wright AG, Markon KE, & Krueger RF (2017). Evidence that psychopathology symptom networks have limited replicability. Journal of Abnormal Psychology, 126, 969–988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frewen PA, Dean JA, & Lanius RA (2012). Assessment of anhedonia in psychological trauma: Development of the Hedonic Deficit and Interference Scale. European Journal of Psychotraumatology, 3, 8585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frewen PA, Dozois DJA, Neufeld RWJ, & Lanius RA (2012). Disturbances of emotional awareness and expression in posttraumatic stress disorder: Meta-mood, emotion regulation, mindfulness, and interference of emotional expressiveness. Psychological Trauma: Theory, Research, Practice, and Policy, 4, 152–161. [Google Scholar]
- Fried EI, & Cramer AO (2017). Moving forward: Challenges and directions for psychopathological network theory and methodology. Perspectives on Psychological Science, 12, 999–1020. [DOI] [PubMed] [Google Scholar]
- Fried EI, Eidhof MB, Palic S, Costantini G, Huisman-van Dijk HM, Bockting CL, … & Karstoft KI. (2018). Replicability and generalizability of posttraumatic stress disorder (PTSD) networks: a cross-cultural multisite study of PTSD symptoms in four trauma patient samples. Clinical Psychological Science, 6, 335–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26, 41–54. [Google Scholar]
- Gratz KL, & Tull MT (2010). Emotion regulation as a mechanism of change in acceptance- and mindfulness-based treatments In Baer RA (Ed.), Assessing Mindfulness and Acceptance: Illuminating the Theory and Practice of Change (pp. 105–133). Oakland, CA: New Harbinger Publications. [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, & Lombardo TW (2004). Psychometric properties of the Life Events Checklist. Assessment, 11, 330–341. [DOI] [PubMed] [Google Scholar]
- Greene T, Gelkopf M, Epskamp S, & Fried E (2018). Dynamic networks of PTSD symptoms during conflict. Psychological Medicine, 48, 2409–2417. [DOI] [PubMed] [Google Scholar]
- Greene T, Gelkopf M, Fried EI, Robinaugh DJ, & Lapid Pickman L (in press). Dynamic network analysis of negative emotions and DSM- 5 posttraumatic stress disorder symptom clusters during conflict. Journal of Traumatic Stress. [DOI] [PubMed] [Google Scholar]
- Hellmuth JC, Jaquier V, Swan SC, & Sullivan TP (2014). Elucidating posttraumatic stress symptom profiles and their correlates among women experiencing bidirectional intimate partner violence. Journal of Clinical Psychology, 70, 1008–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM- IV and DSM- 5 criteria. Journal of Traumatic Stress, 26, 537–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB (2015). Principles and practice of structural equation modeling. New York, NY: Guilford Press. [Google Scholar]
- Lilly MM, Pole N, Best SR, Metzler T, & Marmar CR (2009). Gender and PTSD: What can we learn from female police officers?. Journal of Anxiety Disorders, 23, 767–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litz BT, Orsillo SM, Kaloupek D, & Weathers F (2000). Emotional processing in posttraumatic stress disorder. Journal of Abnormal Psychology, 109, 26–39. [DOI] [PubMed] [Google Scholar]
- McDermott MJ, Tull MT, Gratz KL, Daughters SB, & Lejuez CW (2009). The role of anxiety sensitivity and difficulties in emotion regulation in posttraumatic stress disorder among crack/cocaine dependent patients in residential substance abuse treatment. Journal of Anxiety Disorders, 23, 591–599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNally RJ, Robinaugh DJ, Wu GW, Wang L, Deserno MK, & Borsboom D (2015). Mental disorders as causal systems: A network approach to posttraumatic stress disorder. Clinical Psychological Science, 836–849. [Google Scholar]
- Meade AW, & Craig SB (2012). Identifying careless responses in survey data. Psychological Methods, 17, 437–455. [DOI] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, & Vos T (2012). The long-term health consequences of child physical abuse, emotional abuse, and neglect: A systematic review and meta-analysis. PLoS medicine, 9, e1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oppenheimer DM, Meyvis T, & Davidenko N (2009). Instructional manipulation checks: Detecting satisficing to increase statistical power. Journal of Experimental Social Psychology, 45, 867–872. [Google Scholar]
- Pearl J (2000). Causality: Models, reasoning, and inference. Cambridge, UK: Cambridge University Press. [Google Scholar]
- Roemer L, Litz BT, Orsillo SM, & Wagner AW (2001). A preliminary investigation of the role of strategic withholding of emotions in PTSD. Journal of Traumatic Stress, 14, 149–156. [Google Scholar]
- Ross J, Murphy D, & Armour C (2018). A network analysis of DSM-5 posttraumatic stress disorder and functional impairment in UK treatment-seeking veterans. Journal of Anxiety Disorders, 57, 7–15. [DOI] [PubMed] [Google Scholar]
- Schell TL, Marshall GN, & Jaycox LH (2004). All symptoms are not created equal: The prominent role of hyperarousal in the natural course of posttraumatic psychological distress. Journal of Abnormal Psychology, 113, 189–197. [DOI] [PubMed] [Google Scholar]
- Schick MR, Weiss NH, Contractor A, Dixon-Gordon KL, & Spillane N (in press). Depression and risky alcohol use: An examination of the role of difficulties regulating positive emotions in trauma-exposed individuals. The American Journal of Drug and Alcohol Abuse. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligowski AV, Lee DJ, Bardeen JR, & Orcutt HK (2015). Emotion regulation and posttraumatic stress symptoms: A meta-analysis. Cognitive Behaviour Therapy, 44, 87–102. [DOI] [PubMed] [Google Scholar]
- Smith SM, Goldstein RB, & Grant BF (2016). The association between post-traumatic stress disorder and lifetime DSM-5 psychiatric disorders among veterans: data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). Journal of Psychiatry Research, 82, 16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan CP, Smith AJ, Lewis M, & Jones RT (2018). Network analysis of PTSD symptoms following mass violence. Psychological Trauma: Theory, Research, Practice, and Policy, 10, 58–66. [DOI] [PubMed] [Google Scholar]
- Thomas KA, & Clifford S (2017). Validity and mechanical turk: An assessment of exclusion methods and interactive experiments. Computers in Human Behavior, 77, 184–197. [Google Scholar]
- Tull MT, Barrett HM, McMillan ES, & Roemer L (2007). A preliminary investigation of the relationship between emotion regulation difficulties and posttraumatic stress symptoms. Behavior Therapy, 38, 303–313. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013). The Life Events Checklist for DSM-5 (LEC-5).
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5).
- Wegner DM, Schneider DJ, Carter SR, & White TL (1987). Paradoxical effects of thought suppression. Journal of Personality and Social Psychology, 53, 5–13. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Darosh A, Contractor A, Forkus SR, Dixon-Gordon KL, & Sullivan TP (in press). Heterogeneity in emotion regulation difficulties among women victims of domestic violence: A latent profile analysis. Journal of Affective Disorders. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Darosh A, Contractor A, Schick MR, & Dixon-Gordon KL (in press). Confirmatory validation of the factor structure and psychometric properties of the Difficulties in Emotion Regulation Scale - Positive. Journal of Clinical Psychology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Dixon-Gordon KL, Peasant C, & Sullivan TP (2018). An examination of the role of difficulties regulating positive emotions in posttraumatic stress disorder. Journal of Traumatic Stress, 31, 775–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Forkus SR, Contractor A, Darosh A, Goncharenko S, & Dixon-Gordon KL (in press). Do difficulties regulating positive emotions contribute to risky sexual behavior among trauma-exposed individuals?: A path analysis. Archives of Sexual Behavior. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Forkus SR, Contractor AA, & Dixon-Gordon KL (in press). The interplay of negative and positive emotion dysregulation on mental health outcomes among trauma-exposed community individuals. Psychological Trauma: Theory, Research, Practice, and Policy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Forkus SR, Contractor AA, & Schick MR (2018). Difficulties regulating positive emotions and alcohol and drug misuse: A path analysis. Addictive Behaviors, 84, 45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Gratz KL, & Lavender J (2015). Factor structure and initial validation of a multidimensional measure of difficulties in the regulation of positive emotions: The DERS-Positive. Behavior Modification, 39, 431–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Nelson R, Contractor AA, & Sullivan TP (in press). Emotion dysregulation and posttraumatic stress disorder: A test of the incremental role of difficulties regulating positive emotions Anxiety, Stress, & Coping. [DOI] [PMC free article] [PubMed]
- Weiss NH, Risi MM, Bold KW, Sullivan TP, & Dixon-Gordon KL (in press). Daily relationship between positive affect and drinking to cope: The moderating role of difficulties regulating positive emotions. The American Journal of Drug and Alcohol Abuse. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Anestis MD, & Gratz KL (2013). The relative and unique contributions of emotion dysregulation and impulsivity to posttraumatic stress disorder among substance dependent inpatients. Drug and Alcohol Dependence, 128, 45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Davis LT, Dehon EE, Fulton JJ, & Gratz KL (2012). Examining the association between emotion regulation difficulties and probable posttraumatic stress disorder within a sample of African Americans. Cognitive Behaviour Therapy, 41, 5–14. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Lavender J, & Gratz KL (2013). Role of emotion dysregulation in the relationship between childhood abuse and probable PTSD in a sample of substance abusers. Child Abuse Negl, 37, 944–954. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Sullivan TP, Dixon-Gordon KL, & Gratz KL (2015). Posttraumatic stress disorder symptoms and risky behaviors among trauma-exposed inpatients with substance dependence: The influence of negative and positive urgency. Drug and Alcohol Dependence, 155, 147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Walsh KL, DiLillo D, Messman-Moore T, & Gratz KL (in press). A longitudinal examination of posttraumatic stress disorder symptoms and risky sexual behavior: Evaluating emotion dysregulation dimensions as mediators. Archives of Sexual Behavior. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, … Hembree EA (2016). Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment, 28, 1392–1403. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.