Abstract
Background
Spontaneous rupture of extensor pollicis longus (EPL) tendon is a rare condition often found in patients actively having regular extensive use of hands and fingers especially the thumb. In this article, we report 7 cases of spontaneous rupture of EPL tendon and investigate the associated factors and treatment outcome.
Methods
Retrospectively, the databases for the 7 cases were retrieved and studied. These cases represent all cases of spontaneous rupture of EPL in our institution. Demographic data, clinical presentation, any history of trauma or steroid injection, laboratory and clinical findings suggestive for rheumatoid arthritis, co-morbidities and imaging findings were obtained. In addition, the operative technique and findings were retrieved. Moreover, histopathological studies and follow-up assessment were included.
Results
Six males and one female were included. The mean age was 45.2 years. No prior history of trauma, rheumatological disease or steroid use was detected in any patient. All patients experienced prodromal pain in the radial side. Clinical examination was the most effective diagnostic measure. Magnetic resonance imaging (MRI) was used to confirm the diagnosis and to look for other abnormalities that may predispose to rupture. Five patients underwent extensor indicis proprius to EPL tendon transfer employing Pulvertaft weave technique and one patient underwent primary repair as there was a little gap in the tendon ends. In this study, one patient refused any treatment. All patients achieved a favorable outcome at the last follow-up.
Conclusion
Diagnosis of spontaneous ruptures of EPL tendon can be confirmed through clinical examination and MRI for patients with restricted thumb movement even with the absence of any identifiable predisposing risk factor. During surgery, detailed attention must be drawn towards the tendon ends which can have unusual gaps and bone abnormalities.
Keywords: thumb, interphalangeal joint, rheumatoid arthritis, tendon, extensor pollicis longus
Introduction
Extensor pollicis longus (EPL) is a skeletal muscle that follows a complex anatomical course in the human’s hands. EPL is responsible for the extension of the thumb’s terminal phalanx and adducts the first metacarpal.1 The origin of this muscle is from the interosseous membrane, specifically from the dorsal part of the ulna. The EPL passes through the third dorsal extensor compartment ulnar to Lister’s tubercle before turning towards to thumb.1 Anterior interosseous artery supplies the first part of the EPL tendon prior to the synovial sheath. The radial artery supplies the tendon after the synovial sheath. The tendon within the third compartment at Lister’s tubercle has poor vascularity or is avascular.2,3
The complex structural and functional aspects of the EPL may render it at a higher risk for spontaneous rupture. This is obvious by its anatomical structure in a three-dimensional plain and by its multiple source of blood and innervation supply in different regions of the tendon.1 Spontaneous rupture of EPL without any external force or strain remains unusual in the literature. Also, spontaneous rupture of the EPL tendon at the wrist is mainly described after fracture of the distal radius, in synovitis, or rheumatoid arthritis.3–5 In addition, other causes include steroid treatment and excessive abnormal motion at the wrist joint.6 Furthermore, calcific extensor carpi radialis tendon group was related to the spontaneous rupture of the EPL tendon in one report.7 However, many aspects of spontaneous rupture of the EPL tendon are still unclear. In this study, we aim to report and investigate a case series of spontaneous rupture of EPL without any predisposing factor. We also aim to analyze if there is a correlation between EPL tendon ruptures and any other clinical conditions or occupational factors.
Materials and Methods
This case series study was conducted at a tertiary care center. After obtaining the Institutional Review Board approval, we retrospectively identified those patients who were diagnosed to have ruptured EPL tendon between May 2014 and April 2018 (this period represents the first period of documentation in our institution). The following information was obtained: demographic data, clinical presentation, any history of trauma or steroid injection, laboratory and clinical findings suggestive for rheumatoid arthritis, co-morbidities and imaging findings. In addition, the operative technique and findings were retrieved. Moreover, histopathological studies and follow-up assessment were included.
The included group comprises patients diagnosed with spontaneous rupture of the EPL tendon. Any case of traumatic rupture of EPL tendon was excluded. The demographic data include age, sex and occupation. The utilized imaging studies were the X-ray, magnetic resonance imaging (MRI) and computed tomography (CT) scan. Either a primary repair or a transfer of extensor indicis proprius (EIP) tendon was performed as an operative procedure. The operative findings comprised any bony abnormalities at the Lister’s tubercle, rheumatological findings and tendinous findings. Many methods were utilized for the assessment of the treatment efficacy and included disabilities of the arm, shoulder, and hand (DASH) score, extension lag in metacarpophalangeal joints (MCP) joint index and range of motion (ROM) of the distal interphalangeal joint.
During our investigation, 7 patients were identified to have spontaneous tendon ruptures. After the initial physical examinations, clinical history recording and routine laboratory investigations, all patients were subjected to X-ray imaging, MRI (except for two patients) and CT scan for one patient. The operations were performed by the same procedural guidelines.
Limited statistical analysis tests were used due to the small sample size.
Results
Clinical Characteristics and Demographics of the Patients
Seven patients were identified to have spontaneous EPL rupture. The mean age was 45.2 years (29–82 years). Except for one female patient, all patients were male.
Occupationally, two patients were teachers, one patient was a retired gardener, one patient was a police officer, one of them was a laboratory technician, one patient was a farmer and the female patient was a housewife. Therefore, the patients are from multiple fields of occupations. However, most of them were having occupations that require extensive or continuous movements of the hand and wrist.
No prior history of trauma, rheumatological disease or steroid use or osteoarthritis was detected in any patient. No wrist pathology was identified. All patients complained of persistent pain on the radial side of the wrist prior to the diagnosis and were unable to extend the thumb. Interestingly, they reported a prodromal pain in the hand 2 days to 3 weeks prior to the rupture. Ruptures occurred in 4 right and 3 left hands, 4 of these were nondominant hands and 3 were in the dominant hands. Investigations of the associated clinical conditions were carefully performed for all the 7 patients. Patient 4 and patient 7 were found to be devoid of any co-morbidity. However, all other patients have been suffering from different clinical conditions. The first patient was diagnosed with type II diabetes mellitus, the second patient was complaining of testicular germ cell tumor, the third and the fifth patient has hypertension and the sixth patient-reported valvular heart disease. All the rheumatologic investigations were turned out negative for all patients in this study.
Imaging Studies
The MRI investigations remained successful along with detailed findings. The MRI studies successfully detected the EPL tendon rupture. However, no fracture or tendinitis was detected. The X-ray studies were normal. The CT scan did not reveal any bone abnormality. Following the outcome of the examination and diagnostic tests, surgery was advised to the patients. Table 1 summarizes all points about the clinical and diagnostic aspects.
Table 1.
Patients Clinical Characteristics and Diagnosis
| Patient | Age | Sex | Hx of Trauma | Hx of Steroid | Labs for Rheumatoid | Co-Morbidities | Occupation | Side | X-ray | MRI |
|---|---|---|---|---|---|---|---|---|---|---|
| Patient 1 | 40 | Male | No | No | Negative | DM type II | Teacher | Rt thumb, nondominant | Normal | Normal except ruptured EPL |
| Patient 2 | 32 | Male | No | No | Negative | Testicular germ cell tumor | Teacher | Lt thumb, nondominant | Normal | Normal except ruptured EPL |
| Patient3 | 82 | Male | No | No | Negative | Hypertension | Retired, retail store worker | Rt thumb, dominant | Normal | Not done |
| Patient 4 | 29 | Male | No | No | Negative | Medically free | Police officer | Rt thumb, dominant | Normal | Normal except ruptured EPL |
| Patient 5 | 54 | Female | No | No | Negative | Hypertension | Housewife | Rt thumb, dominant | Normal | Normal except ruptured EPL |
| Patient 6 | 43 | Male | No | No | Negative | Valvular heart disease | Lab technician | Lt thumb, nondominant | Normal | Not done |
| Patient 7 | 37 | Male | No | No | Negative | Free | Farmer | Rt thumb, dominant | Normal | Normal except ruptured EPL |
Abbreviations: Hx, history; DM, diabetes mellitus; MRI, magnetic resonance imaging; Rt, right; Lt, left.
Treatment and Operative Findings
The first patient underwent a primary repair because there was a minimal gap at the tendinous end. Also, 5 patients underwent EIP to EPL tendon transfer and the seventh patient refused the surgery. During the surgery, each patient was investigated for abnormalities in the Lister’s tubercle in addition to any gross rheumatological abnormality. We could not find any mechanical irritants or osteophytes at the Lister’s tubercle. The Lister’s tubercle region was found normal for all cases and none of the patients showed any gross rheumatological findings. There was no evidence of synovitis except around the tendinous ends. Detailed investigations for the tendons suggested that the extensor reticulum was intact in all cases. However, the tendons were detected frayed with gaps and synovitis at the end.
Histopathological Examination
Out of 7 patients, histopathological examination was performed for 4 patients after the surgery. Special attention was provided for any association with rheumatological conditions. Patients 4, 6 and 7 were not subjected to any further histological laboratory investigation. For patient 1, pathological analysis revealed fragments of fibrous tissue with myxoid changes and granulation tissue formation. In the case of the second patient, the histopathological investigation showed fibrovascular tissue composed of thickened collagen bundles disrupted by mild perivascular lymphocytic infiltrate. In another case (patient 3), the microscopic investigation suggested the fragmentation of the tendinous tissue with pauci cellular and densely collagenized appearance along with extensive hyalinization. Further, increased vascularity and perivascular lymphocytic infiltration were also seen. Moreover, no evidence of atypical mitosis, nuclear atypia or malignancy was recorded. Detail of the fifth patient’s case is discussed in the next section.
Final Follow-Up
Range of Motion results
Except for the 7th patient who refused the surgery and terminated the treatment, all the six patients underwent surgery. The follow-up periods for the patients are summarized in Table 2. Special attention during the follow-up period was given to the analysis of the extension lag in the second MCP joint for each patient. Other than the third patient, all were found negative. Patient 3 displayed 5 degrees.
Table 2.
Treatment Findings and Follow-Up Assessment
| Patient | Surgery | Operative Findings Bony Abnormalities at Lister Tubercle | Rheumatology Findings During Surgery | Operative Findings Tendon | Histopathology | DASH Score | F/U Period | Prodrome | Interval Until Surgery | Extension Lag in MCP Joint Index | ROM of Distal Interphalangeal Joint at Final F/U |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Patient 1 | Primary repair | Normal | No | Intact reticulum, frayed tendon ends with gap | Attached | 5.7 | 50 months | Yes | 2 weeks | No | 12 Hyperextension |
| Patient 2 | EIP to EPL Transfer | Normal | No | Intact reticulum, frayed tendon ends with gap | Attached | 1.5 | 49 months | Yes | 3 days | No | 10 Hyperextension |
| Patient 3 | EIP to EPL Transfer | Normal | No | Intact reticulum, frayed tendon ends with gap | Attached | 3 | 40 months | Yes | 4 weeks | 5 degrees | 10 Hyperextension |
| Patient 4 | EIP to EPL Transfer | Normal | No | Intact reticulum, frayed tendon ends with gap | Not available | 3.3 | 35 months | No | 5 weeks | No | 5 Hyperextension |
| Patient 5 | EIP to EPL Transfer | Normal | No | Intact reticulum, frayed tendon ends with gap | Attached | 3.5 | 16 moths | Yes | 10 days | No | 5 Hyperextension |
| Patient 6 | EIP to EPL Transfer | Normal | No | Intact reticulum, frayed tendon ends with gap | Not available | 5 | 51 months | Yes | 8 weeks | No | 10 Hyperextension |
| Patient 7 | Refused treatment | Yes | 6 weeks |
Abbreviations: EIP, extensor indicis proprius; EPL, extensor pollicis longus; DASH, disabilities of the arm, shoulder, and hand; F/U, follow-up; MCP, metacarpophalangeal; ROM, range of motion.
During the final follow-up, an assessment of the ROM of the involved thumb interphalangeal joint was performed for every patient to identify any restrictions. The normal value of the hyperextension/flexion remains within 15H/80 for the thumb interphalangeal joint. The first patient showed 12° extensions during the final follow-up. The second, third and fifth patients displayed the ROM extension value of 10° each and the fourth and fifth patients showed ROM extension values of 5°.
DASH Scoring Outcome
The disabilities of the arm, shoulder, and hand DASH scale are used to assess the recovery of a patient from relevant surgical procedures and for the optimal outcome. Generally, the scoring technique contains two different components, the disability/symptom section, and the high-performance section. The first section was utilized in this study as there were no athletic people or related recovery measures required for the patients under consideration. The seventh patient discontinued the treatment, therefore, not considered for this post-surgical recovery assessment. All other patients were subjected to the DASH score assessment at the last follow-up. All patients showed a score of less than 6 which means that all of them recovered well without any disability. The lesser the obtained score, the better recovery. Table 2 summarizes all aspects of the treatment and the follow-up.
Demonstrative Case (Patient 5)
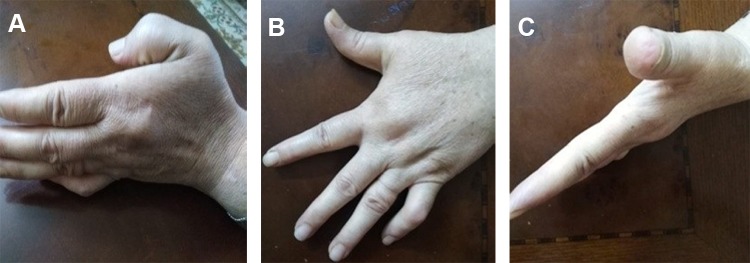
The fifth patient was a 54-year-old housewife right-handed female. One week before the presentation, she started to feel pain in the radial side of her left wrist joint. After that, she was unable to extend her left thumb (Figure 1). Similar to the other cases, she denied any history of trauma, steroid consumption, and rheumatological diseases. The examination revealed the inability to extend the left thumb interphalangeal joint.
Figure 1.

The patient cannot extend left thumb IPJ.
The X-ray and CT were normal (Figure 2). The MRI showed the presence of a complete rupture of the EPL (Figure 3). There were no tenosynovitis and fractures detected in the MRI. As there was no evidence of prior predisposing factors, the case was considered as a spontaneous rupture of EPL tendon.
Figure 2.
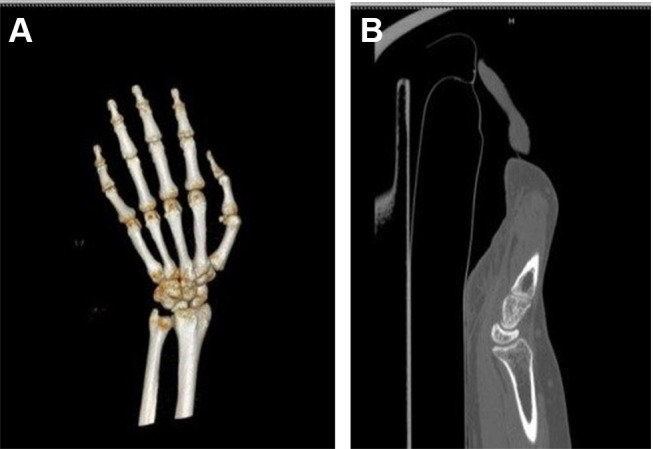
3DCT scan (A) and 2D sagittal view CT scan (B) show no recent bone injury identified.
Figure 3.
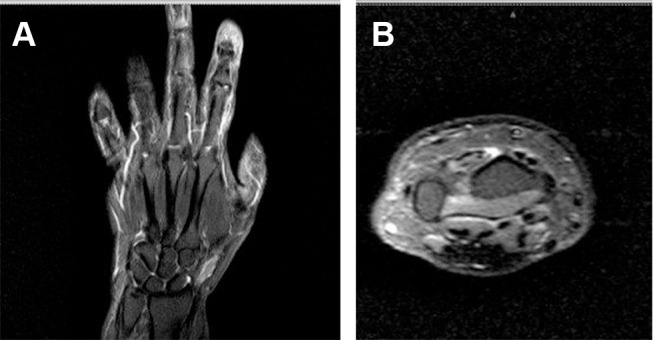
MRI imaging coronal (A) and axial (B) views show an empty 3d extensor compartment with no EPL tendon at Lister’s tubercle level.
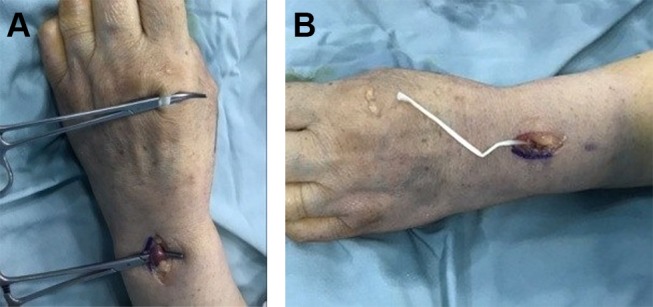
The surgery was conducted within 2 days of the preliminary diagnosis. During the surgery, the extensor retinaculum was found to be intact (Figure 4A). There was no bony cortical roughness at the Lister’s tubercle and no macroscopic tenosynovitis or synovitis was noted. As per other cases, tendon inspection resulted in frayed tendons and gaps at the end (Figure 4B). First, reconstruction of the EPL tendon was done by identifying and sectioning of the EIP tendon using a transverse incision at the second MCP joint (Figure 5). The distal end of EIP was sutured to the extensor digitorum communis tendon. After that, the proximal end was transferred through the subcutaneous tunnel and interwoven with EPL using Pulvertaft repair technique at the level of the 1st carpometacarpal joint with the thumb interphalangeal and MCP joints held in zero degree of extension, keeping the wrist in a neutral position.
Figure 4.
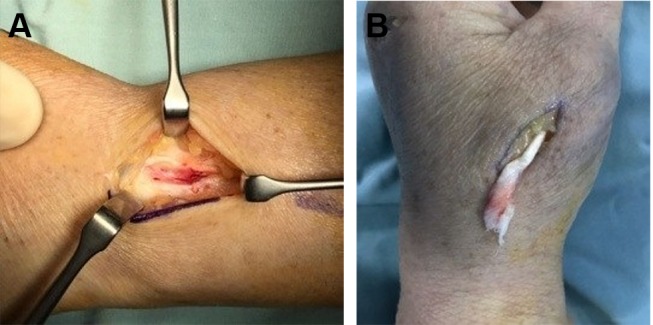
(A) Empty but normal 3d compartment (left), and (B) frayed tendon end (right).
Figure 5.
Identifying (A) and sectioning (B) of EIP tendon.
The patient was immobilized using a short-arm splint, keeping the wrist in a neutral position and the thumb in abduction and extension for 4 weeks. Later on, the splint was weaned, and a gentle range of motion exercises was allowed. The patient was able to extend the left thumb fully after 15 weeks of operation (Figure 6).
Figure 6.
Representation of post-operative range of motion after months.;(A) in flexion and (B and C) in extension.
Histopathological examination of the specimen showed fibroblast hyperplasia with myxoid degeneration. After a follow-up of 16 months, there was no extension lag in the index finger with a normal range of motion of the thumb. A DASH score of 3.5 was attained at the end of the treatment.
Discussion
To the best of our knowledge, this is most recent case series study to investigate the spontaneous rupture of ECL tendon. This study demonstrates that no prior history of trauma, rheumatological disease or steroid use were detected in any patient. All patients experienced prodromal pain in the radial side. Also, this stated states that the clinical examination is the most effective diagnostic measure. MRI may be used to confirm the diagnosis and to look for other. In addition, this study reveals that surgical treatment by EIP to EPL tendon transfer or primary repair is the most effective management step with a favorable outcome. Rupture of EPL tendon is a rare pathology. Athletics often become a victim of EPL rupture due to their vigorous hand movements and relevant possible injuries.8,9 Reports of spontaneous rupture of EPL are not so frequent but often being reported from different parts of the world. Reports of a group of cases are comparatively rare but are present in the relevant medical literature. In 1971, Nigst and Linder had reported 25 cases of rupture of EPL tendon.10 Recently, in 2015, Hu et al reported a group of 8 cases.11 They concluded that the presence of prominent and detectable predisposition fracture is not mandatory for a spontaneous rupture of EPL.11 In their study, four out of eight patients had a history of blunt trauma without fractures detected on X-rays; however, occult fracture cannot be ruled out by X-rays only, they tried to do CT scans, but the patients refused.11 Mechanical sheering may not be the most important cause of such rupture, this rare condition may be due to the patient’s specific unidentified metabolic factors or poor vasculature. Even in our study, we have observed that 3 ruptures occurred in the nondominant hand only. The literature evidence suggests that spontaneous rupture of the EPL occurs mostly for patients who have extensive use of their hands especially the wrist region due to their occupational habits.2,4 Accordingly, it is mandatory to investigate the existence of an occupational link to understand the origin of the disease’s symptoms.
In 1876, Duplay reported the first case of the spontaneous rupture of the EPL which was a rare medical event and report at that time.12 At present, many literatures are available pertaining to the pathophysiology, probable cause, plausible treatment regime to be followed and other relevant aspects.13–15 Most patients suffering from this condition are athletes, professionals who require extensive wrist or arm movement as part of their occupations and those who were having a history of taking steroids.13–15
On the other hand, reports on rare bilateral rupture are available and suggest that injury or other systemic condition such as rheumatoid arthritis could be the possible etiological cause of the condition.16 Cases are also documented where tendon transfer was avoided due to the presence of intact and functional extensor pollicis brevis which was able to hyperextend the thumb interphalangeal joint completely.17
Since years, rheumatoid arthritis has been considered as a major factor for EPL rupture.18 In parallel, steroids were also considered as a dominated cause for EPL rupture.19 Investigations for a specific etiology in a series of cases were carried out and suggested that the major important reason for EPL rupture could be a previous distal radius fracture or injury alongside rheumatoid arthritis or steroids.6 Interestingly, our finding in this report is quite different where we did not find these etiological factors associated with the reported cases.
This series of cases provided a prominent pattern that may be valuable for conducting further investigations in this relation. Irrespective of the age, gender, and other associated medical conditions, all cases had no history of trauma, rheumatoid conditions, or previous steroid uptake. During the radiological and imaging investigations and in all cases, the X-ray was found normal whereas the actual detection of the rupture was done by MRI. At the same time, MRI did not show any tenosynovitis or bony abnormality that may predispose to the rupture.
Our results support the report of Bonatz et al who reported patients devoid of a history of fracture and rheumatoid arthritis and had a spontaneous tear of EPL.20 In another similar report by Hu et al, it was observed that 4 patients had a history of falling down on outstretched hand, but no fractures were detected through X-rays.11
Diep and Adams recently reported that there might be a prodrome present prior to the rupture in the case of tendonitis.21 Therefore, the rupture might become preventable through EPL tendon decompression.21 In this article, we have reported persistent prodrome in most of the cases where a radiating pain existed in the wrist region of the patients with a period of time ranged from 2 days to 21 days. Therefore, prodrome should be analyzed carefully and that may prevent rupture as suggested by Diep and Adams.
The most important factor associated with the surgery of EPL restoration is the transfer of the tendon. Meads and Bogoch suggested that the transfer of the index finger tendon is a possible and safe process in this aspect.22 In this descriptive study, we observed that EIP to EPL transfer was the best surgical option. In a similar study by Lee et al, thumb in extension after transfer and EIP elongation is recommended for restoring thumb extension at the interphalangeal joint in EIP transfer.23
The present study was a unique one in terms of patient numbers in the region. Also, the patients in this study lacked any predisposing factor. Being a retrospective study, the present work was having a limited scope to estimate the precise outcomes.
Conclusion
In the light of the present descriptive study, spontaneous rupture of EPL tendon may not be associated with the age, sex of or patients’ history of rheumatoid arthritis, trauma or steroidal medication uptake. Patients who are having radial wrist pain would be preferable to visit a physician at the earliest possible time as the pain may represent a prodrome for the EPL tendon rupture. The precise diagnosis could be done through the clinical examination. MRI can confirm the diagnosis and exclude any bone and soft tissue abnormality. During surgical procedure, detailed focus should be made on the end part of the tendon which predominantly presents gaps and evidence of tear. EIP to EPL transfer surgery is recommended. Individuals who use their hand repeatedly due to their occupational requirement may become prone to the rupture. Confirmation of these facts requires further prospective studies and a greater number of cases.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data Sharing Statement
The datasets generated and analyzed during the current study are available from the corresponding author.
Ethics Approval
Institutional approval was obtained from the Institutional Review Board at Jordan University of Science and Technology. This study was conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from the patients for publication of any case description and any accompanying images. We confirm that the privacy of the participants was saved, and the data were anonymized and maintained with confidentiality.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Platzer W. Color atlas of human anatomy, Vol. 1: locomotor system In: Austin NM, editor. Joint Structure and Function: A Comprehensive Analysis: The Wrist and Hand Complex. Philadelphia: Thieme, FA Davis Co; 2011:588. [Google Scholar]
- 2.Hirasawa Y, Katsumi Y, Akiyoshi T, et al. Clinical and microangiographic studies on rupture of the E.P.L. tendon after distal radial fractures. J Hand Surg Br. 1990;15:51–57. doi: 10.1016/0266-7681(90)90048-9 [DOI] [PubMed] [Google Scholar]
- 3.Engkvist O, Lundborg G. Rupture of the extensor pollicis longus tendon after fracture of the lower end of the radius—a clinical and microangiographic study. Hand. 1979;11:76–86. doi: 10.1016/S0072-968X(79)80015-7 [DOI] [PubMed] [Google Scholar]
- 4.Payne AJ, Harris NJ, Kehoe NJS. Bilateral delayed extensor pollicis longus rupture following bilateral undisplaced distal radial fractures. Orthopedics. 2000;23:163. [DOI] [PubMed] [Google Scholar]
- 5.Kasture S, Sakamuri R. Bilateral simultaneous traumatic thumb injuries–extensor pollicis longus rupture on one side and ulnar collateral ligament on the other. Case report. J Orthop Case Rep. 2016;6:63–65. doi: 10.13107/jocr.2250-0685.436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bjorkman A, Jorgsholm P. Rupture of the extensor pollicis longus tendon: a study of aetiological factors. Scand J Plast Reconstr Surg Hand Surg. 2004;38:32–35. doi: 10.1080/02844310310013046 [DOI] [PubMed] [Google Scholar]
- 7.Ertem K, Maraş Özdemir Z, Görmeli G, Köroğlu M. Attritional rupture of the extensor pollicis longus tendon due to calcified extensor carpi radialis tendon group: a case report. Eklem Hastalik Cerrahisi. 2017;28(1):59–61. doi: 10.5606/ehc.2017.45063 [DOI] [PubMed] [Google Scholar]
- 8.Dawson WJ. Sports-induced spontaneous rupture of the extensor pollicis longus tendon. J Hand Surg Am. 1992;17:457–458. doi: 10.1016/0363-5023(92)90348-S [DOI] [PubMed] [Google Scholar]
- 9.Lloyd TW, Tyler MP, Roberts AH. Spontaneous rupture of extensor pollicis longus tendon in a kick boxer. Br J Sports Med. 1998;32:178–179. doi: 10.1136/bjsm.32.2.178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nigst H, Linder P. Spontaneous rupture of extensor pollicis longus. Report of 25 cases. Reconstr Surg Traumatol. 1971;12:242–249. [PubMed] [Google Scholar]
- 11.Hu CH, Fufa D, Hsu CC, et al. Revisiting spontaneous rupture of the extensor pollicis longus tendon: eight cases without identifiable predisposing factor. Hand (NY). 2015;10:726–731. doi: 10.1007/s11552-015-9746-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duplay S. Rupture souscutanee du tendon du long extensor du ponce. Bull Mem Soc Chir Paris. 1876;2:788. [Google Scholar]
- 13.Straub LR, Wilson EH Jr. Spontaneous rupture of extensor tendons in the hand associated with rheumatoid arthritis. J Bone Joint Surg Am. 1956;38-A:1208–1217. doi: 10.2106/00004623-195638060-00003 [DOI] [PubMed] [Google Scholar]
- 14.Choi JC, Kim WS, Na HY, et al. Spontaneous rupture of the extensor pollicis longus tendon in a tailor. Clin Orthop Surg. 2011;3:167–169. doi: 10.4055/cios.2011.3.2.167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fujita N, Doita M, Yoshikawa M, et al. Spontaneous rupture of the extensor pollicis longus tendon in a professional skier. Knee Surg Sports Traumatol Arthrosc. 2005;13:489–491. doi: 10.1007/s00167-004-0539-z [DOI] [PubMed] [Google Scholar]
- 16.Gallucci GL, Pacher N, Boretto JG, De Carli P. Bilateral rupture of the extensor pollicis longus tendon. A case report. Chir Main. 2013;32:186–188. doi: 10.1016/j.main.2013.04.001 [DOI] [PubMed] [Google Scholar]
- 17.Strauch RJ, Strauch CB. Extensor pollicis brevis tendon can hyperextend thumb interphalangeal joint in absence of extensor pollicis longus: case report and review of the literature. World J Orthop. 2016;7:448–451. doi: 10.5312/wjo.v7.i7.448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris R. Spontaneous rupture of the tendon of extensor pollicis longus as a complication of rheumatoid arthritis. Ann Rheum Dis. 1951;10:298–306. doi: 10.1136/ard.10.3.298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boussakri H, Bouali A. Subcutaneous rupture of the extensor pollicis longus tendon after corticosteroid injections for DeQuervain’s stenosing tenovaginitis. Case Rep Orthop. 2014;2014:934384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bonatz E, Kramer TD, Masear VR. Rupture of the extensor pollicis longus tendon. Am J Orthop (Belle Mead NJ). 1996;25:118–222. [PubMed] [Google Scholar]
- 21.Diep GK, Adams JE. The prodrome of extensor pollicis longus tendonitis and rupture: rupture may be preventable. Orthopedics. 2016;39:318–322. doi: 10.3928/01477447-20160623-12 [DOI] [PubMed] [Google Scholar]
- 22.Meads BM, Bogoch ER. Transfer of either index finger extensor tendon to the extensor pollicis longus tendon. Can J Plast Surg. 2004;12:31–34. doi: 10.1177/229255030401200108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee JH, Cho YJ, Chung DW. A new method to control tendon tension in the transfer of extensor indicis proprius to extensor pollicis longus rupture. Ann Plast Surg. 2015;75(6):607–609. doi: 10.1097/SAP.0000000000000593 [DOI] [PubMed] [Google Scholar]