Abstract
Purpose
To report the type and severity of ocular injuries sustained by the survivors of a bomb-loaded explosion that occurred in Mogadishu, Somalia on December 28, 2019.
Patients and Methods
The recorded data included age, gender, wounded eye, initial examination of ocular injuries and associated systemic injuries, initial visual acuity, anterior and posterior segment examinations. The type of injury (open vs closed globe), the injured zone of the globe, and the presence of a relative afferent pupil defect were evaluated in all cases where possible.
Results
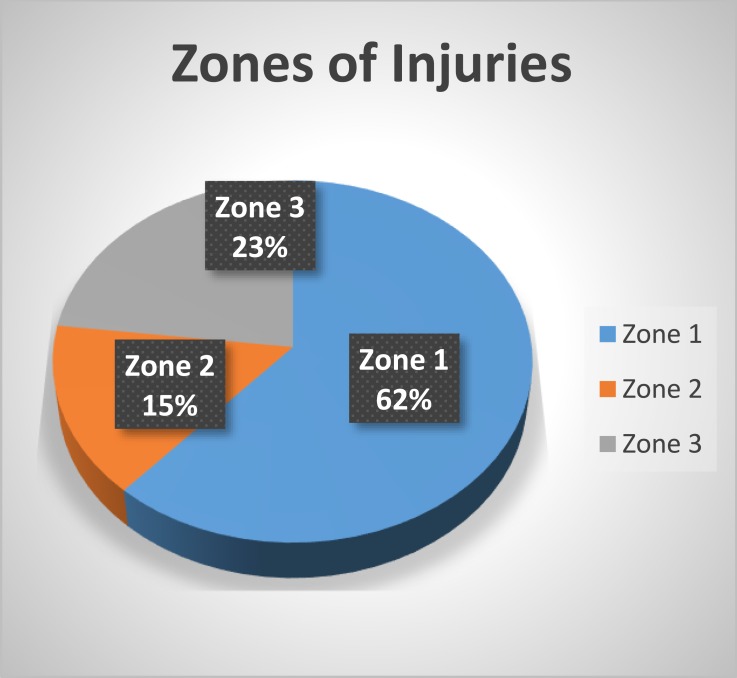
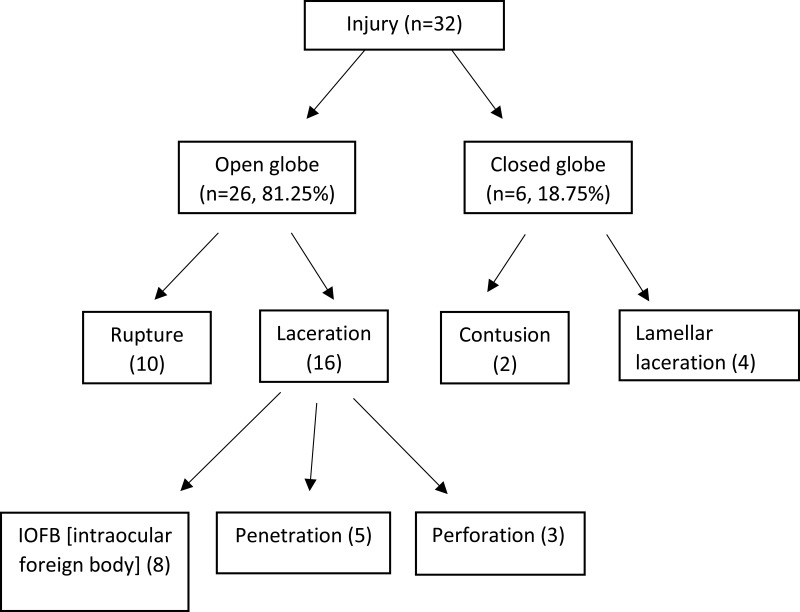
After the explosion, ocular injuries were detected in 28 of 114 patients in our hospital. Thirty-two eyes of 28 patients were included in the study. The mean age was 32.4±6.7 years. The number of open-globe injuries was more than that of closed-globe injuries (26 vs 6; 81.25% vs 18.75%, respectively). Zone 1 was the most affected zone in open-globe injuries (18/26 eyes, 61.6%), followed by Zone 3 in six (23%) patients and Zone 2 in four (15.4%) patients. Sixteen open-globe injuries were laceration type (61.5%) and 10 (38.5%) were rupture type. An intraocular foreign body was detected in eight (30.8%) eyes with open-globe injuries. A total of 28 patients had 11 (39.3%) isolated eye injuries, whereas 17 (60.7%) had concomitant systemic injuries.
Conclusion
The frequency of blast-related ocular injuries is increasing. Today, the increase in the use of vehicle-borne improvised explosives in terrorist-related explosions leads to more frequent and serious ocular injuries.
Keywords: eye injury, ocular trauma, explosion, open-globe injury, improvised explosive device
Introduction
On the morning of December 28, 2019, 85 people died and more than 160 were injured in a bomb-loaded vehicle (truck) explosion that occurred in the center of Mogadishu in Somalia. The explosion was the second-largest bomb attack in the history of Somalia after the 2017 explosion, which had killed more than 500 people. A truck bomb, also known as a vehicle-borne improvised explosive device (VBIED), is placed inside a vehicle, and then detonated.1 The gasoline in the fuel tank of the truck may make the explosion more powerful and effective by dispersing and igniting the fuel. A truck-loaded bomb also produces numerous shrapnel, glass particles or flying debris, and secondary damage to the people around. In recent years, VBIEDs have been increasingly used by suicide bombers.
Although the ocular surface constitutes only 0.27% of the total body surface, 0.54% of the anterior body surface and 4.0% of the face, the rate ocular damage can be up to 50 times the body surface area.2–4 Injuries caused by explosive materials are strongly associated with severe ocular morbidity and visual impairment. Although it is a major type of injury, ocular trauma caused by VBIEDs has not yet been reported from Somalia.
After the 2019 explosion, the majority of the injured patients were referred to our hospital as the largest health center in Somalia. The aim of this study was to present and discuss ocular injuries caused by this bomb attack.
Patients and Methods
This retrospective study was conducted at Somalia Mogadishu-Turkey Education and Research Hospital and comprised cases of ocular injuries due to the explosion in the Mogadishu city center on December 28, 2019. Approval was obtained from the institutional ethical review committee (January 7, 2020 and MSTH-2944). Written informed consent was obtained from the patients and their families before any examination or treatment was performed. Patients with subconjunctival hemorrhage, relatively minor corneal abrasions, or superficial foreign bodies without anterior or posterior segment injuries were excluded from the study.
The recorded data included age, gender, wounded eye, initial examination of ocular injuries and associated systemic injuries, initial visual acuity, and anterior and posterior segment examinations. The type of injury (open vs closed globe), the injured zone of the globe, and the presence of a relative afferent pupil defect were recorded in cases where such evaluation was possible. Computed tomography was performed in all patients with ocular trauma. Additionally, closed-globe injuries were evaluated using ocular ultrasound.
The zone of ocular injury was classified as described by the Ocular Trauma Classification Group as follows: Zone 1 (wound involvement limited to the cornea, including the corneoscleral limbus), Zone 2 (wound involving the sclera and no more posterior than 5 mm from the limbus), and Zone 3 (wound involvement posterior to the anterior 5 mm of the sclera).5,6 The Birmingham Eye Trauma Terminology System was used to identify the type of ocular injury.
The Statistical Package for the Social Sciences (SPSS v. 23.0, Chicago, Illinois, USA) was used for the statistical analyses. Descriptive statistics; ie, mean ± standard deviation (SD) values were used to describe quantitative data and frequencies and percentages for qualitative data.
Results
This study evaluated the data of 114 patients, including those who were brought to the emergency department of our hospital immediately after the explosion and those referred to our clinic from other hospitals within a week. Twenty-eight (24.6%) patients had ocular injuries, and 32 eyes of 28 patients were evaluated in this study. Of these patients, 17 (60.7%) were male and 11 (39.3%) were female. The mean age was 32.4 ± 6.7 years (range 11–68 years). Four patients were under 18 years old. Right, left and bilateral ocular injuries were observed in 14 (50%), 10 (35.7%) and four (14.3%) patients, respectively (Table 1).
Table 1.
Demographic Features of the Study Participants
| Characteristics | Number of Patients (n = 28) |
|---|---|
| Age, years | 32.4±6.7 |
| Age Groups | |
|
4 (14.3%) |
|
24 (85.7%) |
| Gender | |
|
17 (60.7%) |
|
11 (39.3%) |
| Side | |
|
14 (50.0%) |
|
10 (35.7%) |
|
4 (14.3%) |
| Type of Injury | |
|
26 (81.25%) |
|
6 (18.75%) |
The number of open-globe injuries was more than that of closed-globe injuries [26 (81.25%) vs 6 (18.75%)]. Zone 1 was the most affected zone in open-globe injuries (18/26 eyes, 61.6%), followed by Zone 3 in six (23%) patients and Zone 2 in four (15.4%) patients (Figure 1). Sixteen open-globe injuries were laceration type (61.5%) and 10 (38.5%) were rupture type. An intraocular foreign body was detected in eight (30.8%) eyes with open-globe injuries (Figure 2).
Figure 1.
Zone categorization of open-globe injuries.
Figure 2.
Distribution of ocular injuries according to the Birmingham Eye Trauma Terminology System classification.
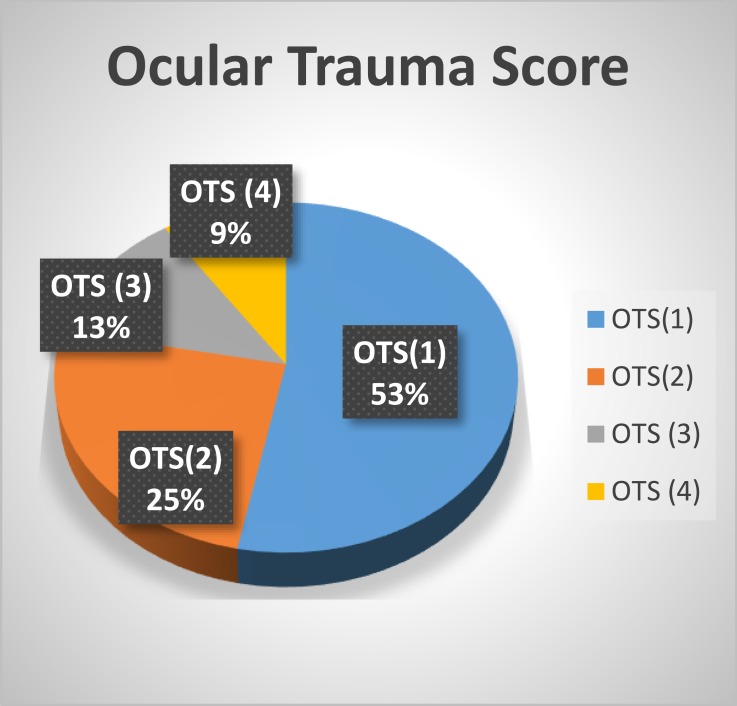
Most of the eyes had serious injuries, and the Ocular Trauma Score (OTS) was found to be 1 for 53% of the cases and 2 for 25%. Of the remaining eyes, 13% had OTS-3% and 9% had OTS-4 injuries. None of the injuries were classified as OTS-5 (Figure 3).
Figure 3.
Ocular Trauma Score (OTS) categorization of ocular injuries.
The most common type of injury was corneal/scleral perforation (81.2%), followed by vitreous hemorrhage (34.4%) and traumatic cataract (31.2%) (Table 2). The initial visual acuity was no perception of light in 17 (53.1%), hand movement in eight (25%), counting fingers in four (12.5%), and 6/60 to 6/18 in three (9.4%) eyes. A total of 28 patients had 11 (39.3%) isolated eye injuries, whereas 17 (60.7%) had concomitant systemic injuries (Table 3).
Table 2.
Ocular Manifestations and Number of Ocular Injuries
| Type of Injury | No. of Eyes (%) |
|---|---|
| Vitreous hemorrhage | 11 (34.4%) |
| Cataract | 10 (31.2%) |
| Hyphema | 9 (28.1%) |
| Corneal edema | 9 (28.1%) |
| Retinal hemorrhage | 8 (25.0%) |
| Retinal detachment | 8 (25.0%) |
| IOFB+ | 8 (25.0%) |
| Corneal lamellar laceration | 5 (15.6%) |
| Sealed perforation | 3 (9.4%) |
Abbreviation: IOFB, intraocular foreign body.
Table 3.
Distribution of Systemic Injuries Associated with Ocular Injury
| Accompanying Systemic Injury | Number of Injuries |
|---|---|
| Maxillofacial injury | 11 |
| Upper/lower-limb injuries | 6 |
| Thoracic injury | 6 |
| Fingertip injuries | 5 |
| Abdominal injury | 5 |
| Tympanic membrane perforation | 4 |
| Brain injury | 4 |
| Pelvic injury | 3 |
| Neck vascular injury | 3 |
Note: Some patients had more than one injury.
Discussion
Improvised explosive devices (IEDs) and VBIEDs are increasingly used by terrorist groups worldwide.7 While most IEDs are used to incur damage to soldiers, VBIEDs are specifically utilized to create casualties in the civilian population.1 As the area affected by VBIEDs is wider, it has a greater direct effect on the ground,8 causing greater damage to the buildings and people in close vicinity. In addition to the direct impact of the explosion, soil, stone, glass and metal fragments which break off from the ground where the vehicle is located and the surrounding buildings result in further injuries to people.
Ocular injuries are common in mass-casualty incidents.9 In our study, the ocular injury rate was 24.6% in survivors. In previous studies, the ocular injury rate after explosion varies widely, being reported as 3% for the 1996 Manchester bombing,10 28% for the US embassy bombing in Nairobi, Kenya in 1998,11 26% for the 2001 World Trade Center bombing,12 and 2.13% for the 2012 Chinese explosion.13 Due to the placement of VBIEDs higher above the ground level compared to other IEDs and mines, they cause more head and ocular injuries. These are also responsible for severe ocular injuries and have become a major source of ocular morbidity.14 The severity of the injuries observed in the current study may be due to the relatively high impact of VBIEDs over a large area and their even greater impact on the head.
Currently, explosives cause four types of blast injuries. A primary blast injury acts by creating an overpressure shock wave in air-filled organs, such as lungs, intestines, and tympanic membranes. A secondary blast injury is caused by direct damage caused by explosive parts. Typically, open-globe injuries and penetrating injuries to the head, chest, and abdomen occur through this mechanism. A tertiary blast injury caused by the blast wind can throw a person into other objects, resulting in closed-globe injuries and orbital fractures. Quaternary blast injuries include damages caused by intense heat and fire from explosives and lead to severe burns and respiratory damage. Another quaternary effect of a blast is triggered by falling debris, resulting in crush injuries to the head or face.15,16
In our study, the presence of globe rupture in patients with hyphema and intra-vitreous hemorrhage without intraocular foreign bodies suggest that the explosion had a primary effect. Primary blast injuries are caused by barotrauma due to overpressure or low pressure relative to atmospheric pressure.17 The energy produced by the gases in the open-air explosion has three components. These are positive pressure shock wave, negative pressure suction wave and blast current. The positive pressure shock wave is a very short and fast process that takes milliseconds and reaches the maximum pressure load suddenly. The negative pressure (sub-atmospheric pressure) that occurs after the positive pressure has a relative vacuum effect that attracts air and debris. This phase takes three to 10 times longer than positive pressure, but the pressure difference in this phase is much less than the positive phase.18 And the destructive energy at the beginning of this phase is more than the positive phase.18 In our study, corneal laceration cases that are not accompanied by a foreign body may be developed with high pressure during a positive pressure shock wave. In addition, total hyphema cases that are not accompanied by a foreign body and whose corneal integrity is preserved may be developed both due to trauma in the iris veins in the positive pressure phase and due to the bleeding caused by the negative pressure suction wave in the iris vessels. Depending on these mechanisms, primary blast injury may have a greater and more severe effect than predicted in the ocular tissues.19
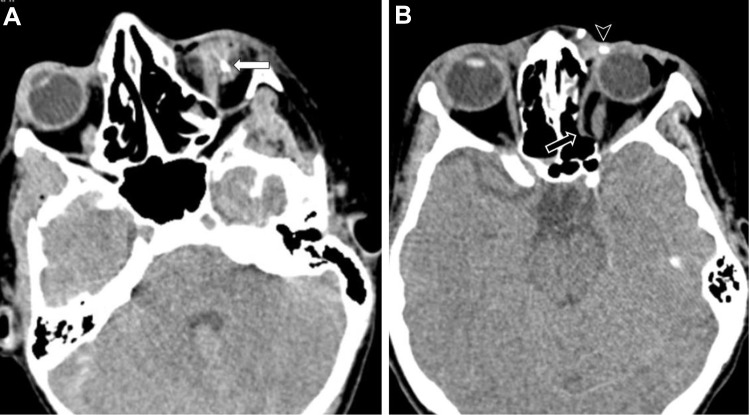
On the other hand, the high rate of open-globe injuries may also be due to the secondary effect of the explosion. Secondary blast injuries cause the majority of eye injuries among blast victims. The eye is vulnerable to small fragments of glass, cement or other debris.20 During the explosion, flying debris, stones, and fragments of glass from the surrounding affected vehicles may have caused direct injuries to the survivors’ globes as shown in Figure 4A. Mines et al reported that most of the injuries that occurred among the survivors of bombing had been caused by the secondary effects of the explosion in the form of flying and falling glass, building materials, and other debris.21 Although the development of reinforced weapon explosions increases the incidence of primary ocular blast injuries, today the most severe and harmful threat to the eyes due to the explosion is still secondary ocular blast injuries caused by fragments and debris.17 Our results are consistent with the results of previous studies. However, blast injuries may not occur due to a single mechanism. As shown in Figure 4B, ocular blast injuries can be seen with a combination of primary and secondary mechanisms.
Figure 4.
(A) 31-year-old man with left globe rupture with secondary mechanism. Non-contrast computed axial tomography image shows intra-vitreal hemorrhage (white arrow) and globe rupture caused by intraocular foreign body in the left eye. (B) In a different patient, hemorrhagic density in the sclera and eyelid and shrapnel in soft tissue (arrowhead). In addition, herniation of the medial rectus muscle into the ethmoid sinus of the orbital medial wall (lamina papyracea) fracture is observed (black arrow) (combination of primary and secondary mechanism).
In our study, the high rate of other organ injuries accompanying ocular injury (60.7%) and closed-globe injuries in six patients suggest that the tertiary mechanism may contribute to ocular damage formation. In addition, the presence of corneal edema in nine patients suggests the chemical and thermal burns caused by toxic gases released after the explosion due to the quarternary mechanism effect.
In our study, the mean age was 32.4 years, which is similar to the previous reports on ocular trauma.22–24 The average age being relatively young can be explained by the fact that the explosion occurred at a crossroads at around 8.00 am in the morning when people go to work and school.
Vitreous hemorrhage (34.4%) and cataract (31.2%) were the most frequent ocular findings of ocular injuries in our study. These findings were similar to the two other publications examining ocular combat injuries in Pakistan.25,26
The high association of ocular injuries caused by explosion with systemic injuries has been demonstrated in previous studies. In the study of Erdurman et al7 this rate was reported to be 69%, whereas Weichel et al15 found it as 66%. In our study, 60.7% of the patients examined had concomitant non-ocular injuries. Maxillofacial, orthopedic and thoracic injuries were the most frequently encountered concomitant injuries.
Conclusion
This study investigated the type and severity of eye injuries in victims of explosion. Today, terror-related blasts have unique injury patterns secondary to the widespread use of highly explosive fragmentary munitions causing severe ocular blast injuries. In recent years, the use of VBIEDs has been increasing in terror-related blasts. Eye injuries caused by bomb explosions are associated with severe ocular and systemic morbidity. Explosions that occur relatively higher above the ground level have more destructive effects on vital organs, and especially the head region. Considering the severity of these injuries, comprehensive plans and strategies should be developed for the immediate and appropriate treatment of explosion victims.
Abbreviations
VBIED, Vehicle-borne improvised explosive device; OTS, Ocular Trauma Score; IEDs, Improvised explosive devices.
Ethics
Approval was obtained from the Somalia Mogadishu-Turkey Education and Research Hospital ethical review committee (January 7, 2020 and MSTH-2944).
Consent
Written informed consent was obtained from the patients and their families before any examination or treatment was performed.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no funding and no conflicts of interest for this work.
References
- 1.Winter C. War by suicide: a statistical analysis of the Islamic State’s Martyrdom industry. Terror Counter-Terrorism Stud. 2017;(December 2015). doi: 10.19165/2017.1.03 [DOI] [Google Scholar]
- 2.Gundogan FC, Akay F, Yolcu U, et al. Ocular blast injuries related to explosive military ammunition. J R Army Med Corps. 2016;162(1):39–43. doi: 10.1136/jramc-2015-000408 [DOI] [PubMed] [Google Scholar]
- 3.Thach AB, Johnson AJ, Carroll RB, et al. Severe eye injuries in the war in Iraq, 2003–2005. Ophthalmology. 2008;115(2):377–382. doi: 10.1016/j.ophtha.2007.04.032 [DOI] [PubMed] [Google Scholar]
- 4.Wong TY, Seet MB, Ang C-L. Eye injuries in twentieth century warfare: a historical perspective. Surv Ophthalmol. 1997;41(6):433–459. doi: 10.1016/S0039-6257(97)00022-2 [DOI] [PubMed] [Google Scholar]
- 5.Pieramici DJ, Sternberg P, Aaberg TM, et al. A system for classifying mechanical injuries of the eye (globe). Am J Ophthalmol. 1997;123(6):820–831. doi: 10.1016/S0002-9394(14)71132-8 [DOI] [PubMed] [Google Scholar]
- 6.Kuhn F, Morris R, Witherspoon CD, et al. Classification of ocular trauma. Ophthalmology. 1996;103(2):240–243. doi: 10.1016/S0161-6420(96)30710-0 [DOI] [PubMed] [Google Scholar]
- 7.Erdurman FC, Hurmeric V, Gokce G, Durukan AH, Sobaci G, Altinsoy HI. Ocular injuries from improvised explosive devices. Eye. 2011;25(11):1491–1498. doi: 10.1038/eye.2011.212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yokohama H, Sunde J, Ellis-Steinborner ST, Ayubi Z. Vehicle borne improvised explosive device (VBIED) characterisation and estimation of its effects in terms of human injury. Int J Prot Struct. 2015;6(4):607–627. doi: 10.1260/2041-4196.6.4.607 [DOI] [Google Scholar]
- 9.Yonekawa Y, Hacker HD, Lehman RE, et al. Ocular blast injuries in mass-casualty incidents. Ophthalmology. 2014;121(9):1670–1676.e1. doi: 10.1016/j.ophtha.2014.04.004 [DOI] [PubMed] [Google Scholar]
- 10.Carley SD, Mackway-Jones K. The casualty profile from the Manchester bombing 1996: a proposal for the construction and dissemination of casualty profiles from major incidents. Emerg Med J. 1997;14(2):76–80. doi: 10.1136/emj.14.2.76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Odhiambo WA, Guthua SW, Macigo FG, Akama MK. Maxillofacial injuries caused by terrorist bomb attack in Nairobi, Kenya. Int J Oral Maxillofac Surg. 2002;31(4):374–377. doi: 10.1054/ijom.2001.0199 [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC). Rapid assessment of injuries among survivors of the terrorist attack on the World Trade Center–New York City, September 2001. MMWR Morb Mortal Wkly Rep. 2002;51(1):1–5 [PubMed] [Google Scholar]
- 13.Jiang H, Xue C, Gao Y, Wang Y. Analysis of ocular injury characteristics in survivors of the 8.12 Tianjin Port Explosion, China. J Ophthalmol. 2019;2019:1–7. doi: 10.1155/2019/1360805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mader TH, Carroll RD, Slade CS, George RK, Ritchey JP, Neville SP. Ocular war injuries of the Iraqi insurgency, January–September 2004. Ophthalmology. 2006;113(1):97–104. doi: 10.1016/j.ophtha.2005.07.018 [DOI] [PubMed] [Google Scholar]
- 15.Weichel ED, Colyer MH. Combat ocular trauma and systemic injury. Curr Opin Ophthalmol. 2008;19(6):519–525. doi: 10.1097/ICU.0b013e3283140e98 [DOI] [PubMed] [Google Scholar]
- 16.Sayer NA, Chiros CE, Sigford B, et al. Characteristics and rehabilitation outcomes among patients with blast and other injuries sustained during the Global War on Terror. Arch Phys Med Rehabil. 2008;89(1):163–170. doi: 10.1016/j.apmr.2007.05.025 [DOI] [PubMed] [Google Scholar]
- 17.Abbotts R, Harrison S, Cooper G. Primary blast injuries to the eye: a review of the evidence. J R Army Med Corps. 2007;153(2):119–123. doi: 10.1136/jramc-153-02-10 [DOI] [PubMed] [Google Scholar]
- 18.Gianno C, Baldan M, Molde A. War Surgery: Working with Limited Resources in Armed Conflict and Other Situations of Violence. Vol. 2 International Committee of the Red Cross; 2017. [Google Scholar]
- 19.Harrisson S, Kirkman E, Mahoney P. Lessons learnt from explosive attacks. J R Army Med Corps. 2007;153(4):278–282. doi: 10.1136/jramc-153-04-12 [DOI] [PubMed] [Google Scholar]
- 20.Morley MG, Nguyen JK, Heier JS, Shingleton BJ, Pasternak JF, Bower KS. Blast eye injuries: a review for first responders. Disaster Med Public Health Prep. 2010;4(2):154–160. doi: 10.1001/dmp.v4n2.hra10003 [DOI] [PubMed] [Google Scholar]
- 21.Mines M, Thach A, Mallonee S, Hildebrand L, Shariat S. Ocular injuries sustained by survivors of the Oklahoma City bombing 32 The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of the Army or the D. Ophthalmology. 2000;107(5):837–843. doi: 10.1016/S0161-6420(00)00030-0 [DOI] [PubMed] [Google Scholar]
- 22.Voon LW, See J, Wong TY. The epidemiology of ocular trauma in Singapore: perspective from the emergency service of a large tertiary hospital. Eye. 2001;15(1):75–81. doi: 10.1038/eye.2001.18 [DOI] [PubMed] [Google Scholar]
- 23.Thompson GJ, Mollan SP. Occupational eye injuries: a continuing problem. Occup Med (Chic Ill). 2009;59(2):123–125. doi: 10.1093/occmed/kqn168 [DOI] [PubMed] [Google Scholar]
- 24.Kıvanç SA, Akova Budak B, Skrijelj E, Tok Çevik M. Demographic characteristics and clinical outcome of work-related open globe injuries in the most industrialised Region of Turkey. Türk Oftalmol Derg. 2017;47(1):18–23. doi: 10.4274/tjo.81598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ul Islam Q, Ishaq M, Yaqub A, Saeed MK. Functional and anatomical outcome in closed globe combat ocular injuries. J Pak Med Assoc. 2016;66(12):1582–1586. [PubMed] [Google Scholar]
- 26.Alam M, Iqbal M, Khan A, Khan SA. Ocular injuries in blast victims. J Pak Med Assoc. 2012;62(2):138–142. [PubMed] [Google Scholar]