Abstract
Purpose
Older adults should be routinely screened for sarcopenia, which threatens healthy, independent aging. The most popular screening tool is the SARC-F questionnaire. As its sensitivity is unsatisfactory, two modified versions of the questionnaire have been published: SARC-CalF (including calf circumference as an additional item) and SARC-F+EBM (assessing additionally age and Body Mass Index). The diagnostic performance of the three versions of the questionnaire has not been compared. The analysis aimed to assess the diagnostic value of SARC-F, SARC-CalF, and SARC-F+EBM questionnaires, and to compare their psychometric properties against two reference standards of sarcopenia diagnosis, ie, EWGSOP1 and modified EWGSOP2 criteria.
Materials and Methods
We performed the sensitivity/specificity analysis and compared the overall diagnostic accuracy of SARC-F, SARC-CalF (31cm) (cut-off point 31 cm for both genders), SARC-CalF (33/34cm) (cut-off points: 33 cm for women and 34 cm for men), and SARC-F+EBM in 115 community-dwelling volunteers aged ≥ 65 yrs from Poland.
Results
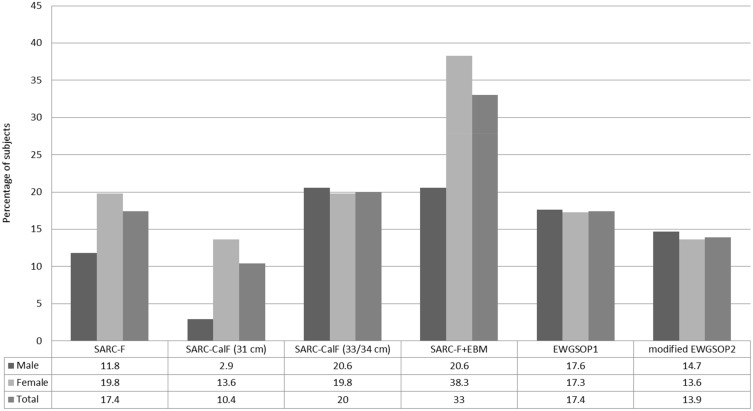
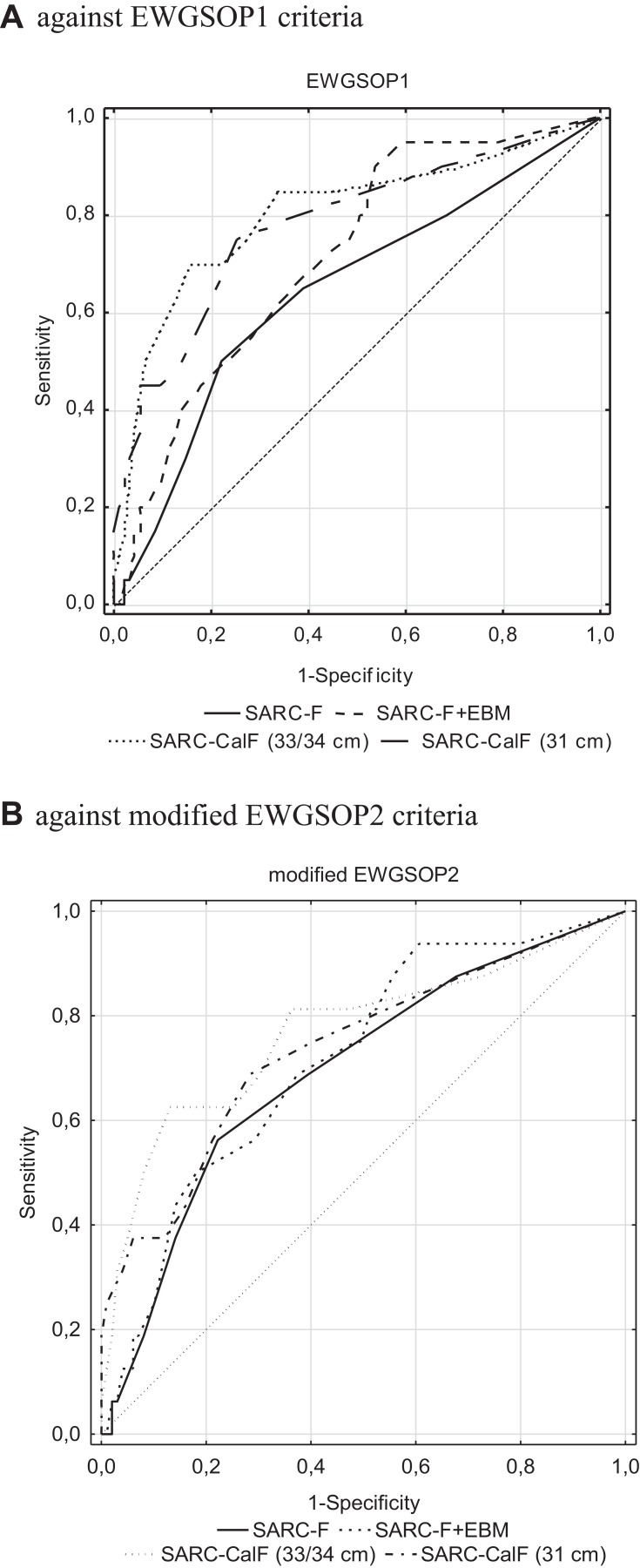
Depending on the version of the SARC-F questionnaire used, from 10.4% [SARC-CalF (31cm)] to 33.0% (SARC-F+EBM) were identified as having an increased risk of sarcopenia. Sarcopenia was identified in 17.4% by the EWGSOP1 criteria and in 13.9% by the modified EWGSOP2 criteria. With respect to the two reference standards used, the sensitivity of SARC-F, SARC-CalF (31cm), SARC-CalF (33/34cm), and SARC-F+EBM ranged 30.0–37.5%, 35.0–37.5%, 60.0–62.5%, 55.0% (the same value for both reference standards), respectively. The specificity ranged 85.3–85.9%, 93.9–94.7%, 88.4–86.9%, 70.7–71.6%, respectively. The AUC of SARC-F, SARC-CalF (31cm), SARC-CalF (33/34cm) and SARC-F+EBM ranged 0.644–0.693, 0.737–0.783, 0.767–0.804, 0.714–0.715, respectively.
Conclusion
The modified versions of SARC-F have better diagnostic performance as compared to the original questionnaire. Since an ideal screening tool should have reasonably high sensitivity and specificity, and an AUC value above 0.7, the SARC-CalF (33/34cm) seems to be the best screening tool for sarcopenia in community-dwelling older adults.
Keywords: sarcopenia, screening, older individuals, SARC-F, ROC analysis
Introduction
Sarcopenia is defined as progressive and generalized skeletal muscle disorder involving the accelerated loss of muscle mass and function and is associated with increased risk of falls, fractures, physical disability, and death.1 Screening may render possible to diagnose sarcopenia in an asymptomatic period and may prevent its serious health consequences. The SARC-F questionnaire was the first diagnostics tool used in 2013 in screening for sarcopenia.2 SARC-F is an acronym of 5 domains included in the questionnaire: 1) Strength, 2) Assistance with walking, 3) Rising from a chair, 4) Climbing stairs, and 5) Falls. The SARC-F questionnaire is characterized by very high specificity and relatively good overall diagnostic accuracy, but its sensitivity is low.3–6 The low sensitivity is an important limitation of the SARC-F questionnaire as a screening tool since sensitivity determines the ability of a test to correctly identify those with the disease. It has been postulated that the low sensitivity of SARC-F in diagnosing sarcopenia results from the omission of low muscle mass in the questionnaire.7–9 Consequently, modified versions of SARC-F have been published. These versions include simple anthropometric parameters, such as calf circumference (SARC-CalF questionnaire), or body mass index (BMI; SARC-F+EBM). According to their authors, these anthropometric parameters correspond well to the muscle mass.8,9
In 2016, Barbosa-Silva et al8 compared the original SARC-F questionnaire with a modified version incorporating calf circumference (SARC-CalF) in a group of 179 older Brazilians. Calf circumference assessment is a simple procedure, consisting of measurement of the widest part of the right calf with non-elastic flexible plastic tape. The World Health Organization recognized calf circumference to be the most sensitive anthropometric index of muscle mass in elderly persons.10 Comparison of SARC-CalF against SARC-F showed the former to have higher sensitivity (66.7% vs 33.3%, respectively), a higher area under the curve (AUC) value (0.736 vs 0.592, respectively), and comparable specificity (82.9% vs 84.2%, respectively).8
Three years later Kurita et al9 enhanced the SARC-F questionnaire with two routine measurements predicting sarcopenia: age ≥ 75 years (associated with increased risk of sarcopenia), and BMI ≤21 kg/m2 (indicating underweight, which is often associated with sarcopenia). The novel version was named SARC-F+EBM (E for elderly individuals, and BM for BMI). In a study performed in a group of 959 hospitalized Japanese with a musculoskeletal disease, they demonstrated that SARC-F+EBM was more sensitive as compared to SARC-F (77.8% vs 41.7%, respectively), and had higher AUC value (0.824 vs 0.557, respectively). The specificity of the two questionnaires was comparable (69.6% vs 68.5%, respectively).
To the best of our knowledge, the diagnostics performance of SARC-F+EBM in community-dwelling elderly subjects has not been assessed. Moreover, the overall diagnostic accuracy of SARC-F has not been compared to SARC-CalF and SARC-F+EBM. Therefore, we have decided to fill the research gaps in this area. The aim of our study was a comparison of the overall diagnostic accuracy of SARC-F and its two modified versions (SARC-CalF and SARC-F+EBM) in community-dwelling older adults from Poland.
Materials and Methods
The study was conducted from March to November 2019 in community-dwelling volunteers living in a city of Poznan, Poland.
The inclusion criteria were as follows: age (65 years or more), lack of cognitive impairment [defined as Abbreviated Mental Test Score (AMTS) ≥ 8 points], the ability to take a vertical position [necessary for measuring body height and analyzing body composition for the assessment of Appendicular Lean Mass (ALM)], and the ability to perform a 4-m usual walking speed test. Patients with conditions precluding the assessment of body composition with the bioimpedance analysis (BIA) method (eg, edema, implanted artificial pacemaker, or the presence of metal implants) were excluded from the study.
Reference Standard of Sarcopenia Diagnosis
The European Working Group on Sarcopenia in Older People criteria published in 2010 (EWGSOP1),11 and their modified version released in 2018 (EWGSOP2)1 were used as the reference standard of sarcopenia diagnosis. According to the EWGSOP1 criteria,11 sarcopenia was defined as low muscle mass (LMM) combined with either low muscle strength or low physical performance. We used cut-off points for LMM for the Polish population defined by the ALM index and young healthy reference population aged 18–40 years, ie, 7.4 kg/m2 for men and 5.6 kg/m2 for women.12 Each subject was considered to have low muscle mass if their ALM index was less than or equal to the sex-specific Polish cut-off points. The cut-off point for low handgrip strength (HGS) was <30 kg for men, <20 kg for women and the cut-off point for low physical performance was a gait speed (GS) of ≤0.8 m/s both sexes. According to the EWGSOP2 criteria,1 sarcopenia was defined as low muscle strength, ie, HGS < 27 kg for men and <16 kg for women, and/or chair stand test (CST) > 15 s for both sexes combined with low muscle quantity (ie low muscle mass). As EWGSOP2 cut-off points for low muscle mass are based on dual-energy X-ray absorptiometry (DXA) method, and we used the bioimpedance analysis to assess muscle mass, we decided to substitute the EWGSOP2 cut-off points for low muscle mass with the same sex-specific Polish cut-off points12 as in the EWGSOP1 algorithm (modified EWGSOP2 criteria).
Assessment of Muscle Mass
The muscle mass level was assessed using the BIA method (InBody 120, Biospace, Seoul, South Korea). In each study participant, the Appendicular Lean Mass (ALM) index [ie, the sum of lean mass of upper and lower limbs (kg) divided by the squared height (m2)] was calculated. The cut-off points applied for the ALM index are shown in the paragraph Reference standard of sarcopenia diagnosis.
Assessment of Muscle Strength
Muscle strength was assessed with handgrip dynamometer measurements (Saehan, Changwon, South Korea) and using The Chair Stand Test (CST). Participants performed the handgrip strength test in a sitting position, with arms bent to 90 degrees in the elbow and shoulder joint. Both the left and right arms were measured twice. The results were recorded in kilograms (kg). The mean value of all measurements was used as the final score for each individual. According to the EWGSOP2 algorithm,1 we also assessed lower limb strength using CST. Each subject was asked to rise five times from a chair with arms folded across the chest, and the time needed to complete the test was measured. The results were recorded in seconds (s).
Assessment of Physical Performance
Physical performance was assessed using the 4-m usual walking speed test. Participants were instructed to walk at their usual gait speed at the distance of 4 meters, and the time necessary to complete the task was measured with a stopwatch. Subjects usually using walking aids (canes, walkers) were allowed to use them during the test. The results were expressed in meters per second.
Screening for Sarcopenia
The risk of sarcopenia was evaluated in each studied subject using the following tools: SARC-F, SARC-CalF, SARC-F+EBM.
The SARC-F Questionnaire
The SARC-F2 examines five domains: 1) strength, 2) assistance with walking, 3) rising from a chair, 4) climbing stairs, and 5) falls, scored from 0 to 2. A score of ≥4 out of the maximum of 10 points indicates a risk of sarcopenia. We used the Polish version of the SARC-F questionnaire which was validated in community-dwelling older adults.13
The SARC-CalF Questionnaire
SARC-CalF8 comprises 5 items of the SARC-F, and an additional item being the calf circumference item (CC; measurement of the right calf in standing position at the point of greatest circumference). The measurement of CC requires the use of an anthropometric measuring tape. We have adopted two cut-off points used in previous research: 1) CC ≤ 31 cm for both sexes [SARC-CalF (31 cm)],14 and 2) CC ≤ 33 cm for women and CC ≤ 34 cm for men [SARC-CalF (33/34cm)].8 The CC item is scored 0 points if its value is above the cut-off point, and 10 if its value is below or equals the cut-off point. The maximal score of the SARC-CalF is 20 points. A total score of ≥11 points indicates the risk of sarcopenia.
The SARC-F+EBM Questionnaire
SARC-F+EBM9 examines seven domains. The first five items are identical to SARC-F. The sixth item is age (scored 10 if age ≥ 75 years, and 0 if age < 75), and the seventh item is BMI (scored 10 if BMI ≤ 21 kg/m2, and 0 if BMI > 21 kg/m2). The maximal score of the SARC-F+EBM is 30 points. A score of ≥12 points indicates a risk of sarcopenia.
Covariates
Assessment of Cognitive Function
Cognitive functions were assessed with the Abbreviated Mental Test Score (AMTS).15 AMTS comprises 10 questions. One point is given for each correct answer, and 0 for an incorrect or missing answer. The total score of 8 points or more is indicative for intact cognitive function. Only subjects who scored at least 8 points were qualified for this study.
Nutritional Assessment
Nutritional status of the study population was assessed with the Mini Nutritional Assessment (MNA).16 The full MNA contains 18 questions. First 6 items, concerning a decrease in food intake, weight loss, mobility, psychological stress or acute disease, neuropsychological problems (dementia or depression), and BMI constitute the so-called Short Form (MNA-SF). Subsequent 12 items contain questions concerning the respondent’s diet (number of meals and consumption of protein, fruit and vegetables, and liquids), eating independence, self-assessment of nutritional and health condition in comparison to subjects of the same age, the number of medications, presence of bedsores or ulcerations, and 2 anthropometric parameters (arm and calf circumference). The maximal score of the full MNA is 30 points. A score of 17 is indicative for malnutrition, 17–23.5 for risk of malnutrition, and 24 points or more for normal nutritional status.
Assessment of Independence in Activities of Daily Living
Independence in basic activities of daily living (ADL) was assessed with the Katz scale, and independence in instrumental activities of daily living with the Lawton scale.17,18 The Katz scale17 comprises six items: bathing, dressing and undressing, toileting, transferring from and to bed, and continence (bowel and bladder). Each item is scored 0 if a subject is dependent, 0.5 if partially dependent, and 1 if independent. Participants were classified into three groups based on the Katz scale: dependent (0–2 points), partially dependent (3–4 points) and independent (5–6 points).
The Lawton scale18 assesses instrumental activities of daily living (IADL). It contains 8 items concerning the following skills: the ability to use a telephone, ability to use different modes of transportation, shopping, food preparation, housekeeping (doing laundry and cleaning), control over one’s medications and ability to handle finances. Each item is scored from 1 to 3. Participants were classified as dependent (IADL score 8–18), partially dependent (19–23 points) or independent (24 points).
Statistical Analysis and Ethical Consideration
Statistical analysis was performed using the STATISTICA 12.0 package (StatSoft, Poland). Continuous data were presented as mean ± SD and compared using the Student’s t-test or the Cochran–Cox test, or Mann–Whitney test as appropriate. Categorical variables were expressed as numbers (percentage) and compared with the χ2 test with the Yates correction if applicable. The EWGSOP111 and modified EWGSOP21 criteria were used as the reference standards for sarcopenia. The sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of SARC-F, SARC-CalF (31 cm and 33/34 cm), SARC-EBM were calculated. The PPV represents the probability a subject is sarcopenic in case of a positive result of a screening test; in turn, the NPV determines the probability a subject is not sarcopenic in case of a negative result of a screening test.19 95% confidence intervals (CI) were calculated for all these parameters. The overall diagnostic accuracy of the SARC-F, SARC-CalF (31 cm and 33/34 cm) and SARC-EBM was compared using the receiver operating curves (ROC) analysis. Areas under the ROC (AUC) with 95% CI were calculated. It was assumed that the AUC values >0.9, 0.7 to 0.9, and 0.5 to 0.7 corresponded to the high, moderate and low diagnostic accuracy of the screening test, respectively.20,21 The areas under the ROC curve were compared using the Hanley–McNeil non-parametric method.22,23
Written Informed consent was obtained from each subject prior to the study. This study was conducted in accordance with the Declaration of Helsinki and the study protocol was approved by the Bioethics Committee of the Poznan University of Medical Sciences, Poland (approval No: 872/18).
Results
Characteristics of the Study Group
One hundred twenty-five persons volunteered for the study. Ten of them were excluded for the following reasons: cognitive impairment (n=5), having a pacemaker (n=2), and physical disability preventing a 4-m usual walking speed test (n=3). The remaining 115 persons were included in the analysis. The age range was 65–93 years, and 30% (n=34) were male.
Table 1 shows the baseline characteristics (including the demographic and clinical parameters) for the total study population, and subgroups with or without sarcopenia according to the EWGSOP1 and modified EWGSOP2 criteria. Subjects with sarcopenia (according to the EWGSOP1 and modified EWGSOP2 criteria) were significantly thinner and had lower BMI than non-sarcopenic persons. They had also lower calf circumference, lower ADL values, lower ALM index, and lower muscle strength in upper and lower limbs. The percentage of people with low BMI (i.e ≤21 kg/m2) and subjects with poor nutritional status (assessed with the MNA) was higher in the sarcopenic groups. However, the non-sarcopenic subjects had a similar level of physical performance as the sarcopenic ones. The mean SARC-F, SARC-CalF (31cm), SARC-CalF (33/34cm), and SARC-F+EBM scores were significantly lower in the sarcopenic groups (p< 0.001).
Table 1.
Characteristics of the Whole Study Population and According to EWGSOP1 and Modified EWGSOP2 Criteria
| Characteristics | Total n=115 |
Sarcopenia (EWGSOP1) n=20 |
Without Sarcopenia (EWGSOP1) n=95 |
p | Sarcopenia (Modified EWGSOP2) n=16 |
Without Sarcopenia (Modified EWGSOP2) n=99 |
p |
|---|---|---|---|---|---|---|---|
| Age | 74.2 ± 6.7 | 74.4 ± 8.0 | 74.2 ± 6.5 | 0.8796 | 75.9 ± 8.0 | 73.9 ± 6.5 | 0.3999 |
| Sexa | |||||||
| Women | 81 (70.4) | 14 (70.0) | 67 (70.5) | 0.9626 | 11 (68.8) | 70 (70.7) | 0.8918 |
| Men | 34 (29.6) | 6 (30.0) | 28 (29.5) | 5 (31.2) | 29 (29.3) | ||
| Age cohorta | |||||||
| 65–74 yrs | 64 (55.7) | 11 (55.0) | 53 (55.8) | 0.9485 | 8 (50.0) | 56 (56.6) | 0.6238 |
| 75 yrs or more | 51 (44.3) | 9 (45.0) | 42 (44.2) | 8 (50.0) | 43 (43.3) | ||
| SARC-F+EBM score | 7.6 ± 6.7 | 11.5 ± 6.4 | 6.8 ± 6.5 | 0.0024 | 11.6 ± 6.5 | 6.9 ± 6.6 | 0.0059 |
| Sarcopenia according to SARC-F+EBMa | |||||||
| Yes | 38 (33.0) | 11 (55.0) | 27 (28.4) | 0.0216 | 9 (56.2) | 29 (29.3) | 0.0334 |
| No | 77 (67.0) | 9 (45.0) | 68 (71.6) | 7 (43.8) | 70 (70.7) | ||
| SARC-F score | 1.8 ± 1.8 | 2.5 ± 2.0 | 1.6 ± 1.8 | 0.0383 | 2.8 ± 2.0 | 1.6 ± 1.8 | 0.0169 |
| Sarcopenia according to SARC-Fa | |||||||
| Yes | 20 (17.4) | 6 (30.0) | 14 (14.7) | 0.1894 | 6 (37.5) | 14 (14.1) | 0.0534 |
| No | 95 (82.6) | 14 (70.0) | 81 (85.3) | 10 (62.5) | 85 (85.9) | ||
| SARC-Cal-F (33/34cm) score | 4.3 ± 5.0 | 9.5 ± 5.5 | 3.1 ± 4.2 | 0.0000 | 9.1 ± 6.1 | 3.5 ± 4.4 | |
| Sarcopenia according to SARC-CalF (33/34 cm) a | |||||||
| Yes | 23 (20.0) | 12 (60.0) | 11 (11.6) | 0.0000 | 10 (62.5) | 13 (13.1) | 0.0000 |
| No | 92 (80.0) | 8 (40.0) | 84 (88.4) | 6 (37.5) | 86 (86.9) | ||
| SARC-Cal-F (31cm) score | 2.9 ± 4.0 | 7.0 ± 5.6 | 2.1 ± 2.0 | 0.0001 | 6.6 ± 6.0 | 2.3 ± 3.2 | 0.0020 |
| Sarcopenia according to SARC-CalF (31cm) a | |||||||
| Yes | 12 (10.4) | 7 (35.0) | 5 (5.3) | 0.0004 | 6 (37.5) | 6 (6.1) | 0.0007 |
| No | 103 (89.6) | 13 (65.0) | 90 (94.7) | 10 (62.5) | 93 (93.9) | ||
| Calf circumference (cm) | 35.7 ± 3.8 | 31.6 ± 4.1 | 36.6 ± 3.1 | 0.0000 | 32.2 ±4.1 | 36.3 ± 3.4 | 0.0014 |
| MNA full score | 25.1 ± 3.6 | 21.7 ± 5.4 | 25.8 ± 2.6 | 0.0019 | 22.0 ± 5.4 | 25.6 ± 2.9 | 0.0169 |
| MNA-full, statusa | |||||||
| Malnutrition | 5 (4.3) | 5 (25.0) | 0 (0.0) | 0.0000 | 4 (25.0) | 1 (1.0) | 0.0003 |
| Risk of malnutrition | 27 (23.5) | 8 (40.0) | 19 (20.0) | 6 (37.5) | 21 (21.2) | ||
| Normal nutritional status | 83 (72.2) | 7 (35.0) | 76 (80.0) | 6 (37.5) | 77 (77.8) | ||
| Number of medications according to the full MNAa | |||||||
| 0-3 | 45 (39.1) | 5 (25.0) | 40 (42.1) | 0.1543 | 4 (25.0) | 41 (41.4) | 0.2120 |
| 4 or more | 70 (60.9) | 15 (75.0) | 55 (57.9) | 12 (75.0) | 58 (58.6) | ||
| ADL, statusa | |||||||
| Independent | 114 (99.1) | 20 (100.0) | 94 (98.9) | 0.3876 | 16 (100.0) | 98 (99.0) | 0.2950 |
| Partially dependent | 1 (0.9) | 0 (0.0) | 1 (1.1) | 0 (0.0) | 1 (1.0) | ||
| Dependent | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | ||
| IADL score | 23.1 ± 1.7 | 22.7 ± 1.7 | 23.2 ± 1.7 | 0.1039 | 22.6 ± 1.8 | 23.2 ± 1.7 | 0.0597 |
| IADL, statusa | |||||||
| Independent | 77 (67.0) | 11 (55.0) | 66 (69.5) | 0.2012 | 8 (50.0) | 69 (69.7) | 0.1510 |
| Partially dependent | 35 (30.4) | 9 (45.0) | 26 (27.4) | 8 (50.0) | 27 (27.3) | ||
| Dependent | 3 (2.6) | 0 (0.0) | 3 (3.1) | 0 (0.0) | 3 (3.0) | ||
| AMTS score | 9.2 ± 0.6 | 9.1 ± 0.8 | 9.3 ± 0.6 | 0.1881 | 9.1 ± 0.8 | 9.3 ± 0.6 | 0.2905 |
| Handgrip strength (kg) | 23.2 ± 8.6 | 17.9 ± 5.7 | 24.3 ± 8.8 | 0.0007 | 16.6 ± 5.2 | 24.3 ± 8.6 | 0.0001 |
| Gait speed (m/s) | 1.0 ± 0.3 | 0.9 ± 0.3 | 1.0 ± 0.3 | 0.0718 | 0.9 ± 0.3 | 1.0 ± 0.3 | 0.0877 |
| Chair stand testb (s) | 12.8 ± 4.4 | 15.1 ± 5.5 | 12.3 ± 4.0 | 0.0279 | 15.9 ± 5.9 | 12.3 ± 3.9 | 0.0180 |
| ALM (kg) | 18.1 ± 4.5 | 14.6 ± 4.5 | 18.9 ± 4.2 | 0.0000 | 14.5 ± 4.6 | 18.7 ± 4.2 | 0.0003 |
| ALM index (kg/m2) | 6.8 ± 1.1 | 5.7 ± 1.0 | 7.1 ± 0.9 | 0.0000 | 5.7 ± 1.0 | 7.0 ± 1.0 | 0.0000 |
| Weight (kg) | 70.1 ± 14.5 | 54.0 ± 13.5 | 73.5 ± 12.3 | 0.0000 | 54.4 ± 12.1 | 72.6 ± 13.2 | 0.0000 |
| Height (cm) | 161.8 ± 9.6 | 158.7 ± 11.2 | 162.4 ± 9.1 | 0.0642 | 157.7 ± 11.6 | 162.4 ± 9.1 | 0.0333 |
| BMI (kg/m2) | 26.7 ± 5.2 | 21.3 ± 3.5 | 27.9 ± 4.7 | 0.0000 | 21.7 ± 3.1 | 27.6 ± 5.0 | 0.0000 |
| Low BMI (kg/m2)a,c | |||||||
| Yes | 16 (13.9) | 9 (45.0) | 7 (7.4) | 0.0000 | 6 (37.5) | 10 (10.1) | 0.0108 |
| No | 99 (86.1) | 11 (55.0) | 88 (92.6) | 10 (62.5) | 89 (89.9) |
Notes: Most variables shown as mean ± SD, except a data were presented as n (%); bn=110, excluded five women who were unable to complete the chair stand test due to low back pain; clow BMI according to Global Leadership Initiative on Malnutrition criteria: BMI <20 kg/m2 in subjects ≤70 yrs and <22 kg/m2 in subjects >70 yrs.
Abbreviations: BMI, body mass index; MNA, mini nutritional assessment; SF, short form; ADL, activity of daily living; IADL, instrumental activity of daily living; AMTS, Abbreviated Mental Test Score; ALM, appendicular lean mass.
Table 2 summarises the answers given to the questions from the SARC-F questionnaire, with additional routine measurements predicting sarcopenia, ie, calf circumference, age, and BMI. Almost half of the respondents reported difficulties with lifting and carrying a weight of 5 kg, and this problem was more frequently reported by subjects with sarcopenia [but only for sarcopenic groups identified by EWGSOP1 criteria (p<0.05)]. Almost one-third of all participants indicated problems with standing up from a chair or bed. Nearly a quarter of the study group experienced at least one fall in the past year. Problems climbing a flight of 10 stairs were reported by almost one-fifth of the subjects. About 13% of participants declared moderate or major difficulties in walking across a room. Twelve percent of the study population had CC ≤ 31 cm. When higher, gender-specific cut-off points were used, more than one-fourth of subjects had low calf circumference. The percent of subjects with low CC was significantly higher in both sarcopenic groups, independently of the cut-off points employed. Almost 15% of participants had low BMI (ie, ≤21 kg/m2); the percent of subjects with low BMI was higher in both sarcopenic groups.
Table 2.
The Characteristics of Answers Given to the Questions from the SARC-F and Additional Items (CC, Age, BMI) of the Whole Study Population and According to EWGSOP1 and Modified EWGSOP2 Criteria
| SARC-F Components | Total n=115 |
Sarcopenia (EWGSOP1) n=20 |
Without Sarcopenia (EWGSOP1) n=95 |
p | Sarcopenia (Modified) EWGSOP2) n=16 |
Without Sarcopenia (Modified EWGSOP2) n=99 |
p | |
|---|---|---|---|---|---|---|---|---|
| Q1. Strength - difficulty lifting and carrying about 5 kg | None | 59 (51.3) | 7 (35.0) | 52 (54.7) | 0.0484 | 5 (31.3) | 54 (54.5) | 0.1133 |
| Some | 34 (29.6) | 5 (25.0) | 29 (30.5) | 5 (31.3) | 29 (29.3) | |||
| A lot or unable | 22 (19.1) | 8 (40.0) | 14 (14.7) | 6 (37.5) | 16 (16.2) | |||
| Q2. Assistance in walking - difficulty walking across a room | None | 101 (87.8) | 15 (75.0) | 86 (90.5) | 0.2056 | 11 (68.8) | 90 (90.9) | 0.0820 |
| Some | 11 (9.6) | 4 (20.0) | 7 (7.4) | 4 (25.0) | 7 (7.1) | |||
| A lot, use aids, or unable | 3 (2.6) | 1 (5.0) | 2 (2.1) | 1 (6.3) | 2 (2.0) | |||
| Q3. Rise from a chair - difficulty transferring from a chair or bed | None | 82 (71.3) | 13 (65.0) | 69 (72.6) | 0.2153 | 9 (56.3) | 73 (73.7) | 0.1032 |
| Some | 29 (25.2) | 7 (35.0) | 21 (22.1) | 7 (43.8) | 21 (21.2) | |||
| A lot or unable without help | 4 (3.5) | 0 (0.0) | 5 (5.3) | 0 (0.0) | 5 (5.1) | |||
| Q4. Climb stairs - difficulty climbing a flight of 10 stairs | None | 86 (74.8) | 13 (65.0) | 73 (76.8) | 0.3823 | 10 (62.5) | 76 (76.8) | 0.2731 |
| Some | 15 (13.1) | 5 (25.0) | 19 (20.0) | 4 (25.0) | 20 (20.2) | |||
| A lot or unable | 5 (4.3) | 2 (10.0) | 3 (3.2) | 2 (12.5) | 3 (3.0) | |||
| Q5. Falls - times fallen in the past year | None | 89 (77.4) | 14 (70.0) | 75 (78.9) | 0.6952 | 10 (62.5) | 79 (79.8) | 0.3423 |
| 1–3 falls | 22 (19.1) | 5 (25.0) | 17 (17.9) | 5 (31.3) | 17 (17.2) | |||
| ≥4 falls | 4 (3.5) | 1 (5.0) | 3 (3.2) | 1 (6.3) | 3 (3.0) | |||
| Additional items | ||||||||
| Calf circumference (cm) | W > 33 cm/M >34 cm | 85 (73.9) | 6 (30.0) | 79 (83.2) | 0.0000 | 6 (37.5) | 79 (79.8) | 0.0011 |
| W ≤ 33 cm/M ≤ 34 cm | 30 (26.1) | 14 (70.0) | 16 (16.8) | 10 (62.5) | 20 (20.2) | |||
| Calf circumference (cm) | ≤ 31 cm for both gender | 14 (12.2) | 9 (45.0) | 5 (5.3) | 0.0000 | 6 (37.5) | 8 (8.1) | 0.0034 |
| > 31 cm for both gender | 101 (87.8) | 11 (55.0) | 90 (94.7) | 10 (62.5) | 91 (91.9) | |||
| Age | <75 years | 64 (55.7) | 11 (55.0) | 53 (55.8) | 0.9485 | 8 (50.0) | 56 (56.6) | 0.6238 |
| ≥75 years | 51 (44.3) | 9 (45.0) | 42 (44.2) | 8 (50.0) | 43 (43.4) | |||
| Body Mass Index | ≤21 kg/m2 | 16 (13.9) | 9 (45.0) | 7 (7.4) | 0.0001 | 6 (37.5) | 10 (10.1) | 0.0108 |
| >21 kg/m2 | 99 (86.1) | 11 (55.0) | 88 (92.6) | 10 (62.5) | 89 (89.9) | |||
Note: Data are presented as n (%).
Abbreviations: Q, question; W, women; M, men.
Prevalence of Sarcopenia
Figure 1 shows the frequency of sarcopenia in the total study population and both sexes. The prevalence of sarcopenia in the total study population was 17.4% according to the EWGSOP1 criteria, and 13.9% according to the modified EWGSOP2 criteria. Depending on the version of the SARC-F questionnaire used, from 10.4% to 33.0% of subjects were identified as having an increased risk of sarcopenia. SARC-CalF (31cm) identified the lowest number of subjects with a risk of sarcopenia (12 persons, including 11 women), whereas SARC-F+EBM – the highest (38 persons, including 31 women).
Figure 1.
Prevalence rate (%) of sarcopenia according to the SARC-F and its modified versions, and two sets of European diagnostic criteria of sarcopenia.
Diagnostic Value of the Analyzed Questionnaires for Sarcopenia Screening
Table 3 shows the results of sensitivity/specificity analyses and AUCs of the SARC-F, SARC-CalF (31 cm), SARC-CalF (33/34cm) and SARC-F+EBM when using the EWGSOP1 and modified EWGSOP2 criteria as the reference standard. Concerning the two reference standards used, the sensitivity of SARC-F, SARC-CalF (31cm), SARC-CalF (33/34 cm) and SARC-F+EBM ranged 30.0–37.5%, 35.0–37.5%, 60.0–62.5%, 55.0% (the same value for both reference standards), respectively. The specificity ranged 85.3–85.9%, 93.9–94.7%, 88.4–86.9%, 70.7–71.6%, respectively. The AUC of SARC-F, SARC-CalF (31 cm), SARC-CalF (33/34cm) and SARC-F+EBM ranged from 0.644–0.693, 0.737–0.783, 0.767–0.804, 0.714–0.715, respectively. Regarding the AUC values, the difference between SARC-F and SARC-CalF (for both cut-off values) was statistically significant (p<0.05), but only against EWGSOP1 criteria. Figure 2 shows the ROC of the 3 analyzed questionnaires.
Table 3.
Sensitivity, Specificity, Positive and Negative Predictive Values and Receiver Operating Curve Model of the SARC-F, SARC-CalF (31 Cm), SARC-CalF (33/34 Cm) and SARC-F+EBM Questionnaires Against EWGSOP1 and Modified EWGSOP2 Criteria of Sarcopenia in the Whole Study Population
| Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | AUC | |
|---|---|---|---|---|---|
| EWGSOP1 | |||||
| SARC-F | 30.0 (11.9–54.3) | 85.3 (76.5–91.7) | 30.0 (15.8–49.5) | 85.3 (81.1–88.6) | 0.644 (0.505–0.783) |
| SARC-CalF (31cm) | 35.0 (15.4–59.2) | 94.7 (88.1–98.3) | 58.3 (33.1–79.9) | 87.4 (83.3–90.6) | 0.783 (0.661–0.905)* |
| SARC-CalF (33/34 cm) | 60.0 (36.1–80.9) | 88.4 (80.2–94.1) | 52.2 (36.0–67.9) | 91.3 (85.9–94.8) | 0.804 (0.683–0.926)* |
| SARC-F+EBM | 55.0 (31.5–76.9) | 71.6 (61.4–80.4) | 29.0 (19.7–40.4) | 88.3 (82.1–92.6) | 0.715 (0.599–0.831) |
| Modified EWGSOP2 | |||||
| SARC-F | 37.5 (15.2–64.6) | 85.9 (77.4–92.1) | 30.0 (16.2–48.8) | 89.5 (85.2–92.6) | 0.693 (0.552–0.834) |
| SARC-CalF (31cm) | 37.5 (15.2–64.6) | 93.9 (87.3–97.7) | 50.0 (26.9–73.1) | 90.3 (86.4–93.2) | 0.737 (0.592–0.882) |
| SARC-CalF (33/34 cm) | 62.5 (35.4–84.8) | 86.9 (78.6–92.8) | 43.5 (29.0–59.2) | 93.5 (88.3–96.4) | 0.767 (0.620–0.914) |
| SARC-F+EBM | 55.0 (31.5–76.9) | 70.7 (60.7–79.4) | 23.7 (15.5–34.5) | 90.9 (85.0–94.7) | 0.714 (0.583–0.844) |
Notes: Data are presented with the 95% CI in parenthesis; *Significantly different (p<0.05) with SARC-F.
Abbreviations: PPV, positive predictive values; NPV, negative predictive values; AUC, area under the curve; EWGSOP1, the European Working Group on Sarcopenia in Older People; EWGSOP2, extended group for the European Working Group on Sarcopenia in Older People.
Figure 2.
The ROC curves of the SARC-F, SARC-CalF (31 cm), SARC-CalF (33/34 cm) and SARC-F+EBM questionnaires against EWGSOP1 and modified EWGSOP2 criteria of sarcopenia in the whole study population.
Discussion
Sarcopenia is linked to the frailty syndrome, and is associated with unfavorable health outcomes in elderly subjects, such as disability, risk of institutionalization, and death. Older adults should be routinely screened for sarcopenia, and in case of positive results further diagnostics of frailty phenotype should be performed.24 The most popular screening tool for sarcopenia is the SARC-F questionnaire. However, its sensitivity is unsatisfactory,3–6 which was further confirmed by the results of our study. Low sensitivity of SARC-F means that a high proportion of subjects with sarcopenia are overlooked if diagnosed using this questionnaire. On the other hand, the specificity of SARC-F is high, which has also been demonstrated in our research. Specificity relates to the test’s ability to correctly reject subjects without a condition. Therefore, if a person was diagnosed non-sarcopenic based on SARC-F results, sarcopenia can be ruled out without any further diagnostics (eg dual-energy X-ray absorptiometry (DEXA), which is associated with an x-ray exposure).
To the best of our knowledge, only three analyses comparing diagnostics performance of SARC-F and SARC-CalF have been published.8,20,25 Barbosa-Silva et al demonstrated that SARC-CalF had higher sensitivity and AUC than SARC-F, while the specificity of both tests was comparable.8 Similar results were found by Yang et al in a group of 384 community-dwelling, elderly Chinese.20 Of note, in both these studies the most frequently used calf circumference cut-off value of 31 cm for both sexes14,25-27 was replaced with 33 cm in women and 34 cm in men. These higher CC cut-off points for predicting low muscle mass were determined by Barbosa-Silva et al by using ROC analysis in a population of 179 community-dwelling elderly aged 60 yrs and more from Pelotas (Brazil).28 In contrast, Bahat et al reported that the addition of CC item to SARC-F (ie SARC-CalF) improved the specificity and diagnostic accuracy of SARC-F, but it did not improve the sensitivity in 207 community-dwelling Turkish older adults.25 Bahat et al employed two different calf circumference thresholds: a standard cut-off of 31 cm (SARC-CalF-31), and a national cut-off of 33 cm (SARC-CalF-33). The same cut-off points were used in both sexes. Using EWGSOP1 criteria as the reference standard, the sensitivity of SARC-F, SARC-CalF-31, and SARC-CalF-33 was the same (25.0%). In turn, the specificity was 81.4%, 98% and 90%, respectively, and AUC was 0.522, 0.590, and 0.746, respectively. Differently from the study of Bahat et al,25 the use of cut-off values of 33 cm in women and 34 cm in men in our research resulted in increased sensitivity and AUC of SARC-CalF as compared to the original version of the questionnaire. The use of CC cut-off point of 31 cm for both sexes had no influence on sensitivity, but improved specificity and AUC. In the most recent analysis of Mo et al, which included the above-mentioned papers and 2 more studies performed in institutionalized patients, the pooled sensitivity of SARC-CalF questionnaires was 0.58, and the pooled specificity was 0.87, using EWGSOP1 criteria as a reference standard.29
It has been recently noticed that proper choice of calf circumference cut-off values is essential in diagnostics of sarcopenia. Employment of lower thresholds, without gender adjustment, may lead to an underrating of sarcopenia when using SARC-CalF.30,31 Such phenomenon was also observed in our study, particularly in men. It may be easily explained by usually higher calf circumference in men as compared to women, and it strongly supports the use of gender-specific CC cut-off values. Kim et al31 raised that calf circumference, like many other anthropometric parameters, vary not only by sex, but also by age, ethnicity, and environment, which complicates determining standard values. As national cut-off points for low CC have not been determined in Poland, we employed both thresholds used in diagnostics of sarcopenia, ie, 31 cm for both sexes, and 33 cm for women and 34 cm for men. The lack of national cut-off values for low CC is a limitation of our study.
According to Kawakami et al,32 calf circumference may be used as a surrogate marker of muscle mass in diagnostics of sarcopenia. However, anthropometric measurements are prone to errors, and obesity and edema may be important confounding factors. Obese subjects usually have high calf circumference, which implies that SARC-CalF may bear a risk of masking sarcopenia. Such a phenomenon was noticeable in our study and was previously reported by Yang et al,33 who had compared four screening questionnaires in a population of 277 elderly, institutionalized Chinese. Ishida et al34 investigated the influence of edema on calf circumference in 2101 elderly Japanese. They found that calf circumference increased by 2 cm on average in the presence of leg oedemas, and suggested that subtraction of 2 cm from the result of CC measurement enabled more accurate assessment of muscle mass in elderly subjects with leg oedemas. Subjects with leg oedemas were excluded from our research, as this condition is a contraindication for body composition analysis with the BIA method, which we used to assess muscle mass.
The latest proposal of SARC-F modification was put forward in 2019 by Kurita et al9 and involved the inclusion of two routine measurements predicting sarcopenia (older age and low BMI). The modified version of the questionnaire, named SARC-F+EBM (where E stands for Elderly individuals, and BM – for Body Mass Index), had much higher sensitivity and general diagnostics performance than the original SARC-F. The results of our study are in line with these findings. Moreover, our analysis demonstrates that the sensitivity of SARC-F+EBM is similar to that of SARC-CalF, but its specificity is lower than both SARC-CalF and SARC-F. The idea to include low BMI (≤21 kg/m2) in the questionnaire is particularly relevant, as it has been well recognized that elderly persons with low body mass index are more prone to sarcopenia than subjects with higher BMI values,35,36 which was also evident in our study. Moreover, low BMI (≤21 kg/m2) is associated with underweight and undernutrition, and the latter increases the risk of sarcopenia. Such a relationship was clearly described by Vandewounde et al in 2012, who introduced the concept of Malnutrition-Sarcopenia Syndrome.37 Additionally, low BMI (<22.9 kg/m2) was better than calf circumference and corrected arm muscle area predictor of low muscle mass in an analysis performed in 2019 by Pinheiro et al27 in a group of 173 elderly Brazilian women.
Our study has some limitations. First, a relatively small group of men (n=34) was included in this analysis – mainly due to the feminization of the older population and the reluctance of older men to volunteer for research. Moreover, a low number of men with sarcopenia involved in our study rendered impossible a comparative analysis for sarcopenia prevalence according to gender. Second, we collected neither the socio-demographic data such as marital status and level of education nor information on the number of chronic diseases and those potentially related to sarcopenia. Third, national cut-off points for low calf circumference have not been determined in Poland. Therefore, we adopted the values used in previous research. However, we cannot be sure whether these values are appropriate in our population. Fourth, we used the BIA method for the assessment of Appendicular Lean Mass instead of more precise methods, such as computed tomography (CT), magnetic resonance imaging (MRI), or DEXA. However, the BIA method is much cheaper, free of x-ray exposure, and seems to be more practical because analyzers are portable, which enables measurement in the place of living of elderly subjects. Some international groups, such as EWGSOP1,11 EWGSOP2,1 and AWGS (the Asia Working Group for Sarcopenia),38 recommended BIA as an alternative option for muscle mass measurement.
A strong point of our analysis is that, to the best of our knowledge, this is the first assessment of the diagnostic performance of the SARC-F+EBM in community-dwelling older adults, and the first study comparing all modified versions of the SARC-F questionnaire, ie, SARC-CalF and SARC-F+EBM.
Conclusion
In summary, the results of our research indicate that modified versions of the SARC-F have better diagnostic performance as compared to the original questionnaire. Since an ideal screening tool should have reasonably high sensitivity and specificity, and an AUC value above 0.7, the SARC-CalF (with calf circumference cut-off values for predicting low muscle mass ≤34 cm in men, and ≤33 cm in women) seems to be the best of evaluated in our research screening tool for sarcopenia in community-dwelling older adults.
Acknowledgments
We would like to thank prof. Jerzy Gąsowski and dr Karolina Piotrowicz from the Jagiellonian University in Cracow, Poland, for delivering the validated Polish version of the SARC-F questionnaire. This work was supported by Poznan University of Medical Sciences [Grant No.: 502-14-11141570-10595].
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Writing group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the extended group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48(1):16–31. doi: 10.1093/ageing/afy169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Malmstrom TK, Morley JE. SARC-F: a simple questionnaire to rapidly diagnose sarcopenia. J Am Med Dir Assoc. 2013;14(8):531–532. doi: 10.1016/j.jamda.2013.05.018 [DOI] [PubMed] [Google Scholar]
- 3.Woo J, Leung J, Morley JE. Validating the SARC-F: a suitable community screening tool for sarcopenia? J Am Med Dir Assoc. 2014;15(9):630–634. doi: 10.1016/j.jamda.2014.04.021 [DOI] [PubMed] [Google Scholar]
- 4.Parra-Rodríguez L, Szlejf C, García-González AI, et al. Cross-cultural adaptation and validation of the Spanish-language version of the SARC-F to assess sarcopenia in mexican community-dwelling older adults. J Am Med Dir Assoc. 2016;17(12):1142–1146. doi: 10.1016/j.jamda.2016.09.008 [DOI] [PubMed] [Google Scholar]
- 5.Kim S, Kim M, Won CW. Validation of the Korean version of the SARC-F questionnaire to assess sarcopenia: korean frailty and aging cohort study. J Am Med Dir Assoc. 2018;19(1):40–45. doi: 10.1016/j.jamda.2017.07.006 [DOI] [PubMed] [Google Scholar]
- 6.Bahat G, Yilmaz O, Kılıç C, Oren MM, Karan MA. Performance of SARC-F in regard to sarcopenia definitions, muscle mass and functional measures. J Nutr Health Aging. 2018;22(8):898–903. doi: 10.1007/s12603-018-1067-8 [DOI] [PubMed] [Google Scholar]
- 7.Rossi AP, Micciolo R, Rubele S, et al. Assessing the risk of sarcopenia in the elderly: the Mini Sarcopenia Risk Assessment (MSRA) questionnaire. J Nutr Health Aging. 2017;21(6):743–749. doi: 10.1007/s12603-017-0921-4 [DOI] [PubMed] [Google Scholar]
- 8.Barbosa-Silva TG, Menezes AM, Bielemann RM, Malmstrom TK, Gonzalez MC. For grupo de Estudos em Composição Corporal e Nutrição (COCONUT). Enhancing SARC-F: improving Sarcopenia screening in the clinical practice. J Am Med Dir Assoc. 2016;17(12):1136–1141. doi: 10.1016/j.jamda.2016.08.004 [DOI] [PubMed] [Google Scholar]
- 9.Kurita N, Wakita T, Kamitani T, Wada O, Mizuno K. SARC-F validation and SARC-F+EBM derivation in musculoskeletal disease: the SPSS-OK study. J Nutr Health Aging. 2019;23(8):732–738. doi: 10.1007/s12603-019-1222-x [DOI] [PubMed] [Google Scholar]
- 10.WHO Expert Committee on Physical Status: the Use and Interpretation of Anthropometry (1993: Geneva, Switzerland) & World Health Organization (1995). Physical status: the use of and interpretation of anthropometry, report of a WHO expert committee. World Health Organization; Available from https://apps.who.int/iris/handle/10665/37003. Accessed February10, 2020.. [PubMed] [Google Scholar]
- 11.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Report of the european working group on sarcopenia in older people. Age Ageing. 2010;39(4):412–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Krzymińska-Siemaszko R, Fryzowicz A, Czepulis N, Kaluźniak-Szymanowska A, Dworak LB, Wieczorowska-Tobis K. The impact of the age range of young healthy reference population on the cut-off points for low muscle mass necessary for the diagnosis of sarcopenia. Eur Rev Med Pharmacol Sci. 2019;23(10):4321–4332. doi: 10.26355/eurrev_201905_17938 [DOI] [PubMed] [Google Scholar]
- 13.Correction to: abstracts of the 15th International Congress of the European Geriatric Medicine Society. Eur Geriatr Med. 2020. doi: 10.1007/s41999-020-00295-1 [DOI] [PubMed] [Google Scholar]
- 14.Landi F, Onder G, Russo A, et al. Calf circumference, frailty and physical performance among older adults living in the community. Clin Nutr. 2014;33(3):539–544. doi: 10.1016/j.clnu.2013.07.013 [DOI] [PubMed] [Google Scholar]
- 15.Jitapunkul S, Pillay I, Ebrahim S. The abbreviated mental test: its use and validity. Age Ageing. 1991;20(5):332–336. doi: 10.1093/ageing/20.5.332 [DOI] [PubMed] [Google Scholar]
- 16.MNA Polish Form. Available from: http://www.mna-elderly.com/forms/MNA_polish.pdf. Accessed February10, 2020..
- 17.Shelkey M, Wallace M. Katz index of independence in activities of daily living (ADL). Dermatol Nurs. 2002;14(3):192–193. [PubMed] [Google Scholar]
- 18.Graf C. The Lawton instrumental activities of daily living (IADL) scale. Am J Nurs. 2008;108(4):52–62. doi: 10.1097/01.NAJ.0000314810.46029.74 [DOI] [PubMed] [Google Scholar]
- 19.Locquet M, Beaudart C, Reginster JY, Petermans J, Bruyère O. Comparison of the performance of five screening methods for sarcopenia. Clin Epidemiol. 2017;10:71–82. doi: 10.2147/CLEP.S148638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang M, Hu X, Xie L, et al. Screening sarcopenia in community-dwelling older adults: SARC-F vs SARC-F combined with calf circumference (SARC-CalF). J Am Med Dir Assoc. 2018;19(3):277.e1-277.e8. doi: 10.1016/j.jamda.2017.12.016 [DOI] [PubMed] [Google Scholar]
- 21.Linden A. Measuring diagnostic and predictive accuracy in disease management: an introduction to receiver operating characteristic (ROC) analysis. J Eval Clin Pract. 2006;12(2):132–139. doi: 10.1111/j.1365-2753.2005.00598.x [DOI] [PubMed] [Google Scholar]
- 22.Hanley JA, McNeil BJ. The meaning and use of the area under a Receiver Operating Characteristic (ROC) curve. Radiology. 1982;143(1):29–36. doi: 10.1148/radiology.143.1.7063747 [DOI] [PubMed] [Google Scholar]
- 23.Hanley JA, Hajian-Tilaki KO. Sampling variability of nonparametric estimates of the areas under receiver operating characteristic curves: an update. Acad Radiol. 1997;4(1):49–58. doi: 10.1016/S1076-6332(97)80161-4 [DOI] [PubMed] [Google Scholar]
- 24.Liguori I, Russo G, Aran L, et al. Sarcopenia: assessment of disease burden and strategies to improve outcomes. Clin Interv Aging. 2018;14;13:913–927. doi: 10.2147/CIA.S149232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bahat G, Oren MM, Yilmaz O, Kılıç C, Aydin K, Karan MA. Comparing SARC-F with SARC-CalF to screen sarcopenia in community living older adults. J Nutr Health Aging. 2018;22(9):1034–1038. doi: 10.1007/s12603-018-1072-y [DOI] [PubMed] [Google Scholar]
- 26.Velazquez-Alva MC, Camacho MEI, Lazarevich I, Velazquez JD, Dominguez PA, Zepeda MAZ. Comparison of the prevalence of sarcopenia using skeletal muscle mass index and calf circumference applying the European consensus definition in elderly Mexican women. Geriatr Gerontol Int. 2017;17(1):161–170. doi: 10.1111/ggi.12652 [DOI] [PubMed] [Google Scholar]
- 27.Pinheiro PA, Coqueiro RDS, Carneiro JAO, Correia TML, Pereira R, Fernandes MH. Anthropometric indicators as screening tools for sarcopenia in older adult women. Enferm Clin. 2019;S1130-8621(19):30041–30045. [DOI] [PubMed] [Google Scholar]
- 28.Barbosa-Silva TG, Bielemann RM, Gonzalez MC, Menezes AM. Prevalence of sarcopenia among community-dwelling elderly of a medium-sized South American city: results of the COMO VAI? study. J Cachexia Sarcopenia Muscle. 2016;7(2):136–143. doi: 10.1002/jcsm.12049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mo Y, Dong X, Wang XH. Screening accuracy of SARC-F combined with calf circumference for sarcopenia in older adults: a diagnostic meta-analysis. J Am Med Dir Assoc. 2020;21(2):288–289. doi: 10.1016/j.jamda.2019.09.002 [DOI] [PubMed] [Google Scholar]
- 30.Lim WS, Chew J, Lim JP, Tay L, Hafizah N, Ding YY. Letter to the editor: case for validated instead of standard cut-offs for SARC-CalF. J Nutr Health Aging. 2019;23(4):393–395. doi: 10.1007/s12603-019-1177-y [DOI] [PubMed] [Google Scholar]
- 31.Kim S, Kim M, Lee Y, Kim B, Yoon TY, Won CW. Calf circumference as a simple screening marker for diagnosing sarcopenia in older korean adults: the Korean Frailty and Aging Cohort Study (KFACS). J Korean Med Sci. 2018;33(20):e151. doi: 10.3346/jkms.2018.33.e151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kawakami R, Murakami H, Sanada K, et al. Calf circumference as a surrogate marker of muscle mass for diagnosing sarcopenia in Japanese men and women. Geriatr Gerontol Int. 2015;15(8):969–976. doi: 10.1111/ggi.12377 [DOI] [PubMed] [Google Scholar]
- 33.Yang M, Lu J, Jiang J, Zeng Y, Tang H. Comparison of four sarcopenia screening tools in nursing home residents. Aging Clin Exp Res. 2019;31(10):1481–1489. doi: 10.1007/s40520-018-1083-x [DOI] [PubMed] [Google Scholar]
- 34.Ishida Y, Maeda K, Nonogaki T, et al. Impact of edema on length of calf circumference in older adults. Geriatr Gerontol Int. 2019;19(10):993–998. doi: 10.1111/ggi.13756 [DOI] [PubMed] [Google Scholar]
- 35.Lau EM, Lynn HS, Woo JW, et al. Prevalence of and risk factors for sarcopenia in elderly Chinese men and women. J Gerontol a Biol Sci Med Sci. 2005;60(2):213–216. doi: 10.1093/gerona/60.2.213 [DOI] [PubMed] [Google Scholar]
- 36.Wu CH, Chen KT, Hou MT, et al. Prevalence and associated factors of sarcopenia and severe sarcopenia in older Taiwanese living in rural community: the Tianliao Old People study. Geriatr Gerontol Int. 2014;14(Suppl 1):69–75. doi: 10.1111/ggi.12233 [DOI] [PubMed] [Google Scholar]
- 37.Vandewoude MF, Alish CJ, Sauer AC, Hegazi RA. Malnutrition-sarcopenia syndrome: is this the future of nutrition screening and assessment for older adults? J Aging Res. 2012;2012:651570. doi: 10.1155/2012/651570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chen L-K, Liu L-K, Woo J, et al. Sarcopenia in Asia: consensus report of the Asian working group for sarcopenia. J Am Med Dir Assoc. 2014;15(2):95–101. doi: 10.1016/j.jamda.2013.11.025 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- MNA Polish Form. Available from: http://www.mna-elderly.com/forms/MNA_polish.pdf. Accessed February10, 2020..