Abstract
Introduction
Escherichia (E.) coli can cause intestinal and extra-intestinal infections which ranged from mild to life-threatening infections. The severity of infection is a product of many factors including virulence properties and antimicrobial resistance.
Objectives
To determine the antibiotic resistance pattern, the distribution of virulence factors and their association with one another and with some selected resistance genes.
Methods
Virulence properties were analyzed phenotypically while antimicrobial susceptibility was tested by Kirby-Bauer agar disc diffusion method. In addition, 64 E. coli isolates were tested for 6 colicin genes, fimH, hlyA, traT, csgA, crl virulence genes and bla−CTX-M-15, bla−oxa-2, and bla−oxa-10 resistance genes by polymerase chain reaction (PCR).
Results
Extra-intestinal pathogenic E. coli isolated from urine and blood samples represented a battery of virulence factors and resistance genes with a great ability to produce biofilm. Also, a significant association (P<0.05) among most of the tested colicin, virulence and resistance genes was observed. The observed associations indicate the importance and contribution of the tested factors in the establishment and the progress of infection especially with Extra-intestinal E. coli (ExPEC) which is considered a great challenging health problem.
Conclusion
There is a need for studying how to control these factors to decrease the rate and the severity of infections. The relationship between virulence factors and resistance genes is complex and needs more studies that should be specific for each area.
Keywords: E. coli, virulence, resistance, colicin genes, ESBL, bla−CTX-M-15, bla−oxa-2, bla−oxa-10
Introduction
The acquisition of virulence and resistance genes is believed to increase the pathogenicity of microorganisms and the severity of infection with the great possibility of therapy failure. Escherichia coli is an opportunistic pathogen, commensal bacteria that can be found as normal flora in humans and animals. It can be classified according to the site of its existence into commensal, intestinal and extra-intestinal E. coli. Commensal E. coli may acquire many virulence genes that may, in combination, result in intestinal and extra-intestinal E. coli infections. Also, diarrheagenic E. coli strains can be classified according to their virulence into different pathotypes which are enterotoxigenic (ETEC), enteropathogenic (EPEC), enterohemorrhagic (EHEC), enteroinvasive (EIEC), and enteroaggregative (EaggEC). Each one of these pathotypes has some virulence factors that in combination are responsible for their pathogenicity of each type and have an important role in infection. For instance, toxin production, hemolysins, proteases, cell surface hydrophobicity, colicins, etc.1,2 E. coli produces bacteriocins such as colicins and microcins which are bactericidal peptides and considered as virulence factors in different E. coli strains or pathotypes.3 Colicins produced by E. coli under stress; prohibiting the colonization of other E. coli strains without affecting their producing strains. Also, colicins increase the host colonization by their producing strain. So, the resistance of other strains to colicins is considered as a cause of their pathogenicity.4
Over 25 different colicins have been specified and categorized on the base of their pathways. Colicins E1 inhibit the synthesis of all macromolecular without respiration arrest.5 Genes encoding colicins E1 were found in ExPEC4 especially uropathogenic E. coli (UPEC). Colicins E2, E7, E8 and E9 cause cleavage of DNA,6 colicins E3, E4 and E6 lead to rRNA hydrolysis,7 while colicins E5 cleave tRNA.8 Microcins V ar urovirulence,9 while colicins B are highly identified in bowel diseases caused by E. coli.10
Furthermore, virulence factors in UPEC are mainly genes encoding adhesion like fimbriae which facilitate invasion and colonization of epithelial cells11 and thin flexible aggregative protein filaments which are known as curli and their encoding genes are crl and csgA.12 Adhesion increases the expression of bacterial toxins, iron acquisition and eschewal the host defense mechanisms.13 The adhesion genes which are mostly prevalent are iha and fimH;14 while toxin gene is hlyA.15 ExPEC in bloodstream is able to overcome the serum bactericidal effect encoded by traT gene.16
In addition to the role of acquisition of virulence genes and its effect on the pathogenicity, the acquisition of resistance genes plays an important role in therapeutic failure and the increase of mortality rate. The inability to control the emergence of multi-drug (MDR), extensive drug (XDR) and pandrug resistance will increase the mortality rates to 10 million people by 2050. Misuse and overuse of antibiotics in therapeutic purposes for human and therapeutic purposes and as growth promotors in livestock lead to the emergence of resistance to many antimicrobial classes as penicillins, cephalosporines, tetracyclines, sulfonamides, macrolides and polymyxins.17
One of the most prevalent resistance factors is extended spectrum ß-lactamase (ESBL) produced by Enterobacteriaceae which first identified in the 1980s.18 The most prevalent ESBL is CTX-M type (cefotaxinase)19 and E. coli having CTX-M ESBL was multidrug-resistant to most drugs.20 OXA ß-lactamase (oxacillinase) is another type which was identified as chromosomally mediated enzyme and revealed a high resistance to penicillin and showed more carbapenems resistance activity.21 Variation of OXA ß-lactamases takes place by alteration of their amino acids and some E. coli isolates may have many variants of OXA ß-lactamases. So, the single strain may have variable types of ESBLs.22
The aim of this study was to determine the antibiotic resistance pattern, the distribution of different virulence factors of E. coli isolated from different sources of infections and their association with one another and with some selected resistance genes.
Methods
Patients, Samples and Identification of Isolates
Our study comprised 200 patients, who were admitted to Minia university hospital during the period from January to July 2019. In brief, 125 males and 75 females were included with a median age of 46 (range 23–56). Samples were collected from patients with urinary tract infections (80 urine samples), gastroenteritis (50 stool samples), septicemia (30 blood samples) and wound infections (40 wound swab samples) as part of the routine hospital laboratory procedures. Samples were obtained after 2 days of their hospitalization. The following antibiotics were used until the results of cultures were available: two doses of ciprofloxacin (urinary tract infections), one dose of cefotaxime (wound infections), two doses of metronidazole and ciprofloxacin (diarrhea) and one dose of imipenem and vancomycin (septicemia).
All samples were cultured and identified using the conventional microbiological procedures. Samples positive for E. coli showed pink colonies on MacConkey agar (Oxoid, UK). E. coli positive cultures were confirmed by different biochemical tests (catalase, sugar fermentation, indole and nitrate reduction tests) and the formation of metallic sheen on Eosin methylene blue agar (EMB) (Himedia, India).
Phenotypic Identification of Virulence Properties of E. coli Isolates
Virulence properties were determined phenotypically as follows: Hemolysis was tested by inoculating isolates into 5% sheep blood agar plates. Clear zones around colonies indicate hemolysin production. Biofilm formation was tested using the tissue culture plate method (TCP).23 Cell surface hydrophobicity was determined by the salt aggregation test (SAT). Protease test was detected by culturing the tested isolates on skim milk agar and the formation of clear zones around colonies is considered positive. Mannose resistant and mannose sensitive haemagglutination test was done by mixing one drop of blood group “O” with a drop of bacterial cultures on a slide, followed by rotating the slide for 5 min at 37̊C. Clumps formed were indicated as haemagglutination. Mannose sensitive haemagglutination was indicated by the addition of 2% w/v of d-mannose. The absence of haemagglutination indicates Mannose sensitivity while the presence of Haemagglutination indicates Mannose resistance. Curli fimbriae expression was determined by growing the tested isolates on agar plates containing 0.1% tryptone, 0.05% yeast extract, 0.002% Coomassie brilliant blue, 0.004% Congo red and 1.5% agar. Curli production can be detected by the presence of red colonies while white colonies were negative for curli. Colicin production: fresh E. coli cultures were cultured on the surface of nutrient agar for 24 hrs at 37°C. Plates were exposed for chloroform vapors for 2 hrs, and then left for 30 mins to evaporate chloroform. Isolates were inoculated perpendicular to the original cultures. The tested isolates were examined for inhibition of growth.24–29
Antimicrobial Susceptibility Testing and Phenotypic Detection of ESBL
Antimicrobial susceptibility testing of E. coli isolates was performed on Mueller Hinton agar plates using the Kirby–Bauer agar disc diffusion method.30 Antibiotic discs used in this study were obtained from Bioanalyse (Turkey). Isolates were defined as sensitive or resistant depending on the measurement of inhibition zone diameters following the criteria of Clinical Laboratory standards Institute (CLSI). The incidence of resistance to each antibiotic was calculated by the number of resistant isolates to specific antibiotics/total number of isolates Multiplied by 100. Detection of ESBL production was performed by a double-disk synergy test using E. coli ATCC 25922 as a control.31,32
DNA Extraction
The DNA template was prepared by the boiling of the suspensions of bacterial pellets for 10 min and using the supernatant directly in the PCR assay.33
PCR Primers and Testing Conditions
PCR was used to amplify the targeted virulence and resistance genes. PCR reaction mixture was done in 25 μL reaction volumes containing 12.5 μL master mix (Bioline, USA), 1 µL of each 10 μmol−1 forward and reverse primers (Laboratories Midland Certified Reagent Company Inc.), 2 µL DNA template and 8.5 µL pyrogen-free water. PCR cycling was performed using the conditions summarized in Table 1 according to Yamamoto et al,34 Johnson et al,35 Schamberger et al,36 Schamberger et al,37 Bhattacharjee et al,38 Pal and Singh,12 Lin et al,39 and Tahamtan et al40 PCR products were analyzed using 1.5% agarose gel electrophoresis containing ethidium bromide at 8 V/cm. Then, the reaction product was visualized under Gel doc/UV transilluminator.41
Table 1.
List of Primers Used in This Study
| Name of Gene | Primer Sequence | Amplicon Size | PCR Condition | Reference |
|---|---|---|---|---|
| Colicin V | F:CACACACAAACGGGAGCTGTT R:CTTCCCGCAGCATAGTTCCAT |
680 bp | 35 cycles of 94 ºC for 30s, 55 ºC for 30 s, 72 ºC for 1 min | (Johnson and Stell, 2000) [35] |
| Colicin Ia/Ib | F:ACGTATTACAAATCCCGGTGC R:CTTTTTCCTTCAACAGGGCA |
1250 bp | 35 cycles of 94 ºC for 30s, 55 ºC for 30 s, 72 ºC for 1 min | (Schamberger and Diez-Gonzalez, 2004) [36] |
| Colicin B | F:AAGAAAATGACGAGAAGACG R:GAAAGACCAAAGGCTATAAGG |
493 bp | 35 cycles of 94 ºC for 30s, 55 ºC for 30 s, 72 ºC for 1 min | (Schamberger and Diez-Gonzalez, 2004) [36] |
| Colicin M | F:CATCACCATCAACTAACTTACC R:CTCTTTACCAGAAAACATCG |
737 bp | 35 cycles of 94 ºC for 30s, 55 ºC for 30 s, 72 ºC for 1 min | (Schamberger and Diez-Gonzalez, 2004) [36] |
| Colicin E1 | F:TTTGAATGGTACTCCTGACGG R:GTTCCAGCAAGCAAGCTAAA |
1398 bp | 35 cycles of 94 ºC for 30s, 55 ºC for 30 s, 72 ºC for 1 min | (Schamberger and Diez-Gonzalez, 2004) [36] |
| Colicin E2-E9 | F:CGACAGGCTAAAGCTGTTCAGGT R:TGCAGCAGCATCAAATGCAGCCT |
219 bp | 35 cycles of 94 ºC for 1 min, 60 ºC for 1 min, 72 ºC for 1 min | (Tahamtan et al, 2012) [40] |
| crl | F:TTTCGATTGTCTGGCTGTAT R:CTTCAGATTCAGCGTCGTC |
250 bp | 30 cycles of 94 ºC for 40 s, 52ºC for 40 s, 72ºC for 45 s | (Pal and Singh, 2007) [12] |
| csgA | F:ACTCTGACTTGACTATTACC R:AGATGCAGTCTGGTCAAC |
200 bp | 30 cycles of 94 ºC for 1 min, 48ºC for 1min, 72ºC for 1 min | (Pal and Singh, 2007) [12] |
| fimH | F:TGCAGAACGGATAAGCCGTGG R:GCAGTCACCTGCCCTCCGGTA |
508 bp | 25 cycles of 94ºC for 30s, 63 ºC for 30 s, 68 ºC for 3min | (Johnson and Stell, 2000) [35] |
| hlyA | F:AACAAGGATAAGCACTGTTCTGGCT R:ACCATATAAGCGGTCATTCCCGTCA |
1177 bp | 25 cycles of 94ºC for 30s, 63 ºC for 30 s, 68 ºC for 3min | (Yamamoto et al, 1995) [34] |
| traT | F:GGTGTGGTGCGATGAGCACAG R:CACGGTTCAGCCATCCCTGAG |
290 bp | 25 cycles of 94ºC for 30s, 63 ºC for 30 s, 68 ºC for 3min | (Johnson and Stell, 2000) [35] |
| bla−OXA-2 | F: AAGAA ACGCTACTCGCCTGC R: CCACTCAACCCATC CTACCC′ |
478 bp | 40 cycles of 94 ºC for 1 min, 55ºC for 1min, 72ºC for 1 min | (Bhattacharjee et al, 2007) [38] |
| bla−OXA-10 | F:TCTTTCGAGTACGGCATTAGC R:CCA ATGATGCCCTCACTTTCC |
760bp | 35 cycles of 96 ºC for 1 min, 56ºC for 1min, 72ºC for 1 min | (Lin et al, 2012) [39] |
| bla−CTX-M-5 | F:CGCTTTGCGATGTGCAG R:ACCGCGATATCGTTGGT |
550 bp | 40 cycles of 94 ºC for 1 min, 55ºC for 1min, 72ºC for 1 min | (Bhattacharjee et al, 2007) [38] |
Statistical Analysis
Statistical analysis was performed using SPSS, 17 statistical software (SPSS Inc., Chicago, IL). In order to compare the frequencies obtained for phenotypic properties, virulence genes and antibiotic resistance, chi-square (X2) and Fisher’s exact test were used. Correlations were established using Pearson’s correlation coefficient (r2) in bivariate linear correlations (P< 0.05). P-value is significant if it is ≤0.05.
Results
Out of 200 samples, 96 (48%) and 88 (44%) samples were positive for Gram-negative and Gram-positive bacteria, respectively, while 16 samples (8%) were negative for growth.
Out of 96 Gram-negative bacteria, 64 isolates (66.66%) were confirmed as E. coli (10 (15.6%) from wound samples, 22 (34.4%) from urine samples, 23 (35.9%) from stool samples and 9 (14%) from blood samples).
Phenotypic Characteristics
E. coli isolated from urine samples showed greater hemolytic activity (19/22, 86.3%), MRHA (14/22, 63.6%) (Adherence mediated by non-type I pili) and curli fimbriae production (20/22, 90.9%) compared to E. coli isolated from other sources. On the other hand, about 88.8% (8/9 isolates) and 66.6% (6/9 isolates) of E. coli isolated from blood samples showed high cell surface hydrophobicity and mannose sensitivity (adherence mediated by type I pili). A high incidence of strong biofilm production was observed among E. coli isolated from urine (5/22, 22.7%) followed by those isolated from blood samples (2/9, 22.2%) (Table 2).
Table 2.
Distribution of Virulence Properties Among E. coli Clinical Isolates Collected from Different Infections
| Virulence Properties | Samples (N= 64) | P-value | Total | |||
|---|---|---|---|---|---|---|
| Urine (n=22) N (%)* | Stool (n=23) N (%)* | Blood (n=9) N (%)* | Wound Swabs (n=10) N (%)* | N (%)** | ||
| Hemolysis | 19 (86.3) | 2 (8.6) | 4 (44.4) | 2 (20) | <0.001* | 27 (42.1) |
| Colicin production | 17 (77.2) | 20 (86.9) | 5 (50) | 6 (60) | 0.185 | 58 (90.6) |
| MRHA test | 14 (63.6) | 12 (52.2) | 5 (55.5) | 5 (50) | 0.849 | 36 (56.2) |
| Mannose sensitivity | 13 (59) | 8 (34.7) | 6 (66.6) | 6(60) | 0.241 | 33 (51.5) |
| Curli fimbriae production | 20 (90.9) | 19 (82.6) | 6 (66.6) | 6 (60) | 0.160 | 51 (79.6) |
| Cell surface hydrophobicity | 18 (81.8) | 20 (86.9) | 8 (88.8) | 6 (60) | 0.283 | 52 (81.2) |
| Protease production | 7 (31.8) | 9 (39.1) | 2 (22.2) | 3 (30) | 0.821 | 21 (32.8) |
Biofilm
|
9 (40.9) 8 (36.3) 5 (22.7) |
10 (43.4) 8 (34.7) 5 (21.7) |
3 (33.3) 4 (44.4) 2 (22.2) |
2 (20) 3 (30) 1 (10) |
0.978 | 24 (37.5) 23 (35.9) 13 (20.3) |
Notes: *Percentages were correlated to the total number of each type of samples. **Percentages were correlated to the total number of E. coli isolate. P values are significant at <0.05.
Abbreviation: MRHA, Mannose Resistant Hemagglutination test.
Prevalence of Virulence Genes Among the Tested Isolates
Irrespective of the source of E. coli isolates, the most common virulence genes among all isolates were csgA and crl (50/64 (78.1%) and 49/64 (76.5%), respectively) and fimH (48/64, 75%). The distribution of virulence factors among E. coli isolates isolated from different sources is represented in Table 3 which showed that all eight virulence genes tested appeared in the tested urine and stool samples. On the other hand, col la-lb was determined among E. coli isolated from different sources with high prevalence among E. coli isolated from stool (19/23, 82.6%) while colV was more common among fecal and blood isolates (14/23, 60.8% and 5/9, 55.5%, respectively) (Table 3).
Table 3.
Distribution of Virulence Genes Among E. coli Clinical Isolates Collected from Different Infections
| Virulence Genes | Samples | P-value | Total (n = 64) N (%)** | |||
|---|---|---|---|---|---|---|
| Urine (n=22) N (%)* | Stool (n=23) N (%)* | Blood (n=9) N (%)* | Wound Swabs (n=10) N (%) * | |||
| Colicin genes: | ||||||
| Col M | 4 (18.2) | 0 (0) | 0 (0) | 2 (20) | 0.109 | 5 (7.8) |
| Col B | 4 (18.2) | 0 (0) | 0 (0) | 1 (10) | 0.084 | 6 (9.3) |
| Col V | 4 (18.2) | 14 (60.8) | 5 (55.5) | 4 (40) | 0.027* | 27 (42.1) |
| Col E1 | 8 (36.4) | 18 (78.3) | 0 (0) | 3 (30) | 0.001* | 29 (45.3) |
| Col E2-E9 | 4 (18.2) | 15 (65.2) | 0 (0) | 1 (10) | <0.001* | 20 (31.25) |
| Col la-lb | 8 (36.4) | 19 (82.6) | 2 (22.2) | 5 (50) | 0.003* | 34 (53.1) |
| Other virulence genes | ||||||
| fimH | 20 (90.9) | 18 (78.3) | 6 (66.6) | 4 (40) | 0.019* | 48 (75) |
| HlyA | 18 (81.8) | 4 (17.4) | 5 (55.5) | 2 (20) | <0.001* | 29 (45.3) |
| traT | 13 (59.1) | 7 (30.4) | 5 (55.5) | 4 (40) | 0.237 | 29 (45.3) |
| CsgA | 20 (90.9) | 18 (78.3) | 8 (88.8) | 4 (40) | 0.011* | 50 (78.1) |
| Crl | 19 (86.4) | 17 (73.9) | 8 (88.8) | 5 (50) | 0.114 | 49 (76.5) |
| No virulence genes found in each isolate | ||||||
| 0 | 2 (9) | 3 (13) | 1 (11.1) | 3 (30) | 0.451 | 9 (14) |
| 1 | 0 (0) | 2 (8.6) | 2 (22.2) | 2 (20) | 0.147 | 6 (9.3) |
| 2 | 2 (9) | 3 (13) | 1 (11.1) | 2 (20) | 0.857 | 8 (12.5) |
| 3 | 10 (45.4) | 7 (30.4) | 2 (22.2) | 0 (0) | 0.069 | 19 (29.6) |
| 4 | 1 (4.5) | 1 (4.3) | 0 (0) | 0 (0) | 0.999 | 2 (3.1) |
| 5 | 1 (4.5) | 2 (8.6) | 0 (0) | 0 (0) | 0.999 | 3 (4.6) |
| 6 | 0 (0) | 0 (0) | 1 (11.1) | 0 (0) | 0.999 | 1 (1.5) |
| 7 | 1 (4.5) | 2 (8.6) | 2 (22.2) | 1 (10) | 0.499 | 6 (9.3) |
| 8 | 1 (4.5) | 1 (4.3) | 0 (0) | 0 (0) | 0.499 | 2 (3.1) |
Notes: *Percentages were correlated to the total number of E. coli isolated from each type of samples. **Percentages were correlated to the total number of E. coli isolates. P values are significant at <0.05.
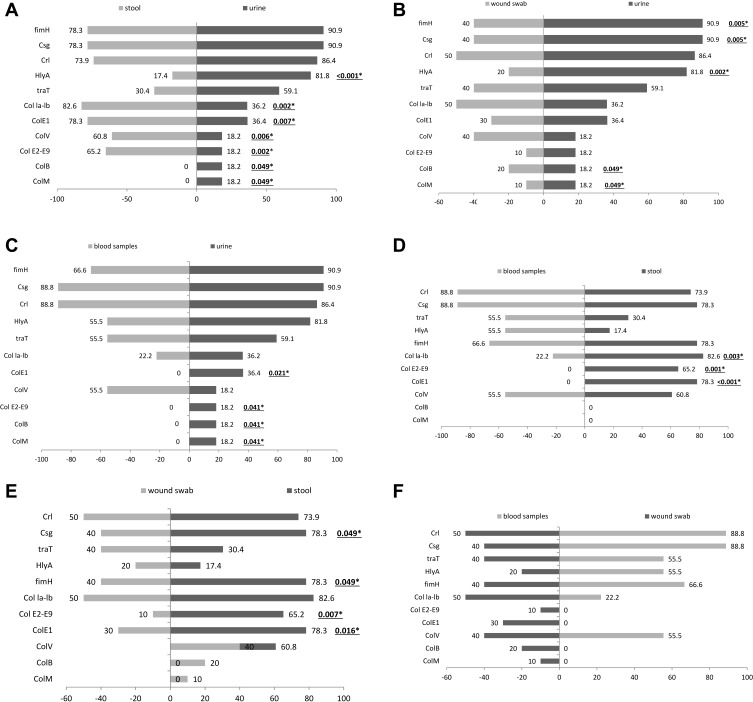
High prevalence of colE1 genes was observed among E. coli isolated from stool and urine samples (18/23, 78.3% and 8/22, 36.4%, respectively). colM and colB genes were not identified in any isolates obtained from blood and stool samples but low prevalence for both genes was observed among E. coli isolated from wound swab samples (20% for colM and 10% for colB, respectively) and uropathogenic E. coli (4/22, 18.2% each) was observed. Also, all E. coli isolates obtained from blood samples were negative for col E1, col E2-E9. On the other hand, fimH (90.9%), csgA (90.9%), HlyA (81.8%) and crl (86.4%) genes were the most common virulence genes in UPEC while crl and csgA (88.8% each) genes were the most common virulence genes in E. coli isolated from blood samples (Table 3). The difference in the distribution and frequency of virulence genes among E. coli isolates with respect to the source of samples is illustrated in Tornado Figure 1.
Figure 1.
Virulence genotypes of the tested E. coli isolates based on the type of samples. (A): Stool and urine samples. (B): Wound and urine samples. (C): Blood and urine samples. (D): Blood and stool samples. (E): Wound and stool samples. (F): Blood and wound samples.
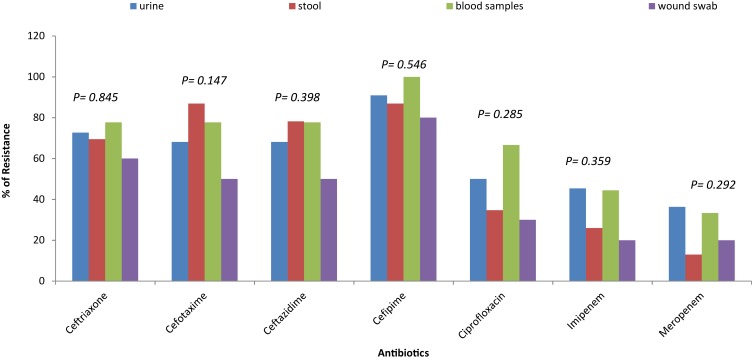
Antimicrobial Resistance of the Tested Isolates
No significant differences (P-value >0.05) among E. coli isolates of different sources in the antibiotic resistance pattern were observed. Figure 2 shows that Meropenem and imipenem were the most effective antibiotics. E. coli isolated from stool samples showed the lowest resistance to meropenem (13%) while those isolated from wound samples showed the lowest resistance to imipenem (20%).
Figure 2.
Distribution of antibiotic resistance among E. coli clinical isolates of different sources.
Prevalence of ESBL Production and the Tested Resistance Genes Among Isolates
No significant differences (P-value >0.05) among the distribution of the resistance genes and the source of samples were reported in this study. Table 4 shows that ESBL production was common among E. coli isolates isolated from blood and urine samples (5/9, 55.5 and 12/22, 54.5%, respectively). Also, bla−CTX-M-15 was more common among blood isolates followed by those isolated from urine (4/9, 44.4 and 8/22, 36.3%, respectively). The co-existence of bla−CTX-M-15 with bla−OXA-10 (1/9, 11.1%) and bla−OXA-2 (2/9, 22.2%) were more common among E. coli isolated from blood in comparison to those obtained from other sources. In addition, no association between bla−OXA-2 and bla−OXA-10 was observed among the tested isolates (Table 4).
Table 4.
Distribution of ESBL Production and Resistance Genes Among the Isolated E. coli from Different Sources
| Source of Isolates | P-value | ||||
|---|---|---|---|---|---|
| Urine (n=22) N (%)* | Stool (n=23) N (%)* | Blood (n=9) N (%)* | Wound Swabs (n=10) N (%) * | ||
| ESBL Producers | 12 (54.5) | 10 (43.4) | 5 (55.5) | 3 (30) | 0.672 |
| Resistance Genes | |||||
| bla-CTX-M-15 | 8 (36.3) | 6 (26) | 4 (44.4) | 3 (30) | 0.756 |
| bla-OXA-2 like | 3 (13.6) | 0 (0) | 2 (22.2) | 1 (10) | 0.203 |
| bla-OXA-10 like | 2 (9) | 1 (4.3) | 2 (22.2) | 0 (0) | 0.999 |
| bla-CTX-M-15 + bla-OXA-2 like | 2 (9) | 0 (0) | 2 (22.2) | 1 (10) | 0.999 |
| bla-CTX-M-15 + bla-OXA-10 like | 1 (4.5) | 0 (0) | 1 (11.1) | 1 (10) | 0.999 |
| bla-OXA-2 like+ bla-OXA-10 like | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0.999 |
Notes: *Percentages were correlated to the total number of E. coli isolated from each type of samples. P values are significant at <0.05.
Associations Among Virulence Factors
There were distinctive, complex associations and relationships among the tested virulence factors and with one another (Tables 5–8). Colicin genes were found to be common among E. coli isolated from urine and stool samples. In UPEC, a significant strong positive association between colM with col E1, colB, traT and csgA was reported. colB was positively associated with colV, colE1, col Ia-Ib and crl genes, while colV showed a positive association with colE1, col Ia-Ib, fimH, traT and crl genes. col E2-E9 showed a positive association with col Ia-Ib and csgA genes, while col Ia-Ib showed a positive association with hlyA, traT, csgA and crl genes (Table 5). A moderate positive association was reported among the tested genes in E. coli isolated from wound samples (Table 6).
Table 5.
Relationships Between Virulence Factors Genes and Resistance Genes in Uropathogenic E. coli Isolates
| Correlations | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| colM | colB | colV | colE1 | colE2-E9 | colIa-lb | fimH | hlyA | traT | CsgA | Crl | bla−CTX-M-15 | bla−oxa-2 | bla−oxa-10 | |
| ColM | NA | 0.681** | 0.550* | 0.719** | 0.586* | 0.540* | 0.568* | 0.559* | 0.678** | 0.658* | 0.477 | 0.617** | 0.861* | 0.693** |
| ColB | NA | 0.747** | 0.851** | 0.609* | 0.767** | 0.466 | 0.611* | 0.572* | 0.671** | 0.797** | 0.668 | 0.853** | 0.517** | |
| ColV | NA | 0.774** | 0.677** | 0.788** | 0.673** | 0.515 | 0.690** | 0.479 | 0.746* | 0.717** | 0.657 | 0.256** | ||
| Col E1 | NA | 0.672** | 0.821** | 0.549* | 0.591* | 0.743** | 0.595* | 0.722** | 0.670** | 0.814** | 0.494 | |||
| Col E2-E9 | NA | 0.665** | 0.422 | 0.445 | 0.518 | 0.667** | 0.584* | 0.775* | 0.615** | 0.372** | ||||
| Col Ia-Ib | NA | 0.289 | 0.691** | 0.667** | 0.767** | 0.668* | 0.788** | 0.661** | 0.418** | |||||
| fimH | NA | 0.309 | 0.715** | 0.187 | 0.350* | 0.454 | 0.437** | 0.023* | ||||||
| hlyA | NA | 0.545* | 0.749** | 0.520* | 0.538* | 0.557 | 0.250* | |||||||
| traT | NA | 0.511 | 0.254 | 0.551 | 0.508 | 0.116 | ||||||||
| CsgA | NA | 0.430 | 0.744 | 0.677 | 0.466 | |||||||||
| Crl | NA | 0.683 | 0.736 | 0.571 | ||||||||||
| bla−CTX-M-15 | NA | 0.635 | 0.501 | |||||||||||
| bla-Oxa-2 | NA | 0.750 | ||||||||||||
| bla−Oxa-10 | NA | |||||||||||||
Notes: Statistical analysis of associations between virulence factors (VFs). P values were calculated by Fisher’s exact test. *Correlation is significant at 0.05 level (2-tailed). **Correlation is significant at 0.01 level (2-tailed).
Abbreviation: NA, not applicable.
Table 8.
Relationships Between Virulence Factors Genes and Resistance Genes in E. coli Isolated from Blood Samples
| Correlations | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| colM | colB | colV | colE1 | colE2-E9 | colIa-lb | fimH | hlyA | traT | CsgA | Crl | bla−CTX-M-15 | bla−oxa-2 | bla−oxa-10 | |
| ColM | NA | – | – | – | – | – | – | – | – | – | – | – | – | – |
| ColB | NA | – | – | – | – | – | – | – | – | – | – | – | – | |
| ColV | NA | – | – | 0.695** | 0.944** | 0.892** | 0.814** | 0.866** | 0.924a | 0.758a | 0.544 | 0.430a | ||
| Col E1 | NA | – | – | – | – | – | – | – | – | – | – | |||
| Col E2-E9 | NA | – | – | – | – | – | – | – | – | – | ||||
| Col Ia-Ib | NA | 0.699** | 0.678** | 0.854** | 0.817** | 0.772a | 0.582a | 0.202** | 0.243a | |||||
| fimH | NA | 0.939** | 0.823** | 0.912** | 0.977a | 0.603a | 0.448** | 0.274a | ||||||
| hlyA | NA | 0.918** | 0.885** | – | – | – | – | |||||||
| traT | NA | 0.878 | 0.871 | 0.655 | 0.515 | 0.460 | ||||||||
| CsgA | NA | 0.968 | 0.563 | 0.376 | 0.190 | |||||||||
| Crl | NA | 0.578 | 0.408 | 0.253 | ||||||||||
| bla−CTX-M-15 | NA | 0.815 | 0.666 | |||||||||||
| bla-Oxa-2 | NA | 0.770 | ||||||||||||
| bla−Oxa-10 | NA | |||||||||||||
Notes: Statistical analysis of associations between virulence factors (VFs). P values were calculated by Fisher’s exact test. *Correlation is significant at 0.05 level (2-tailed). **Correlation is significant at 0.01 level (2-tailed). aCannot be computed because at least one variable is constant.
Abbreviation: NA, not applicable.
Table 6.
Relationships Between Virulence Factors Genes and Resistance Genes in E. coli Isolated from Wound Samples
| Correlations | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| colM | colB | colV | colE1 | colE2-E9 | colIa-lb | fimH | hlyA | traT | CsgA | Crl | bla−CTX-M-15 | bla−oxa-2 | bla−oxa-10 | |
| ColM | NA | 0.147 | 0.505 | −0.048 | 0.222 | −0.184 | 0.471 | 0.167 | 0.427 | 0.059 | −0.050 | 0.615 | 0.577 | 0.417 |
| ColB | NA | 0.387 | 0.576* | 0.079 | 0.040 | 0.531 | 0.059 | 0.151 | 0.458 | 0.354 | 0.165 | 0.000 | 0.079* | |
| ColV | NA | 0.569* | 0.014 | −0.293 | 0.499 | −0.063 | 0.121 | 0.099 | −0.025 | 0.461 | 0.438 | 0.309* | ||
| Col E1 | NA | 0.176 | −0.081 | 0.314 | 0.216 | 0.177 | 0.610* | 0.489 | 0.348* | −0.083* | 0.288 | |||
| Col E2-E9 | NA | 0.642* | 0.609* | 0.556* | 0.552* | 0.380 | 0.378 | 0.368 | 0.192 | 0.481 | ||||
| Col Ia-Ib | NA | 0.450 | 0.184 | 0.154 | 0.287 | 0.430 | −0.115 | −0.294 | −0.151 | |||||
| fimH | NA | 0.881** | 0.491 | 0.265 | 0.518 | 0.408 | 0.471 | |||||||
| hlyA | NA | 0.881** | 0.576* | 0.400 | 0.722 | 0.289 | 0.750 | |||||||
| traT | NA | 0.465 | 0.352 | 0.850 | 0.462 | 0.801 | ||||||||
| CsgA | NA | 0.636 | 0.430 | −0.136 | 0.288 | |||||||||
| Crl | NA | 0.289 | −0.231 | 0.144 | ||||||||||
| bla−CTX-M-15 | NA | 0.662 | 0.863 | |||||||||||
| bla-Oxa-2 | NA | 0.770 | ||||||||||||
| bla−Oxa-10 | NA | |||||||||||||
Notes: Statistical analysis of associations between virulence factors (VFs). P values were calculated by Fisher’s exact test. *Correlation is significant at 0.05 level (2-tailed). **Correlation is significant at 0.01 level (2-tailed).
Abbreviation: NA, not applicable.
For E. coli isolated from stool samples, colM showed positive association with colE2-E9, col Ia-Ib and fimH. colV showed a moderate association with col E2-E9, col Ia-Ib (Table 7). A forceful positive correlation between colV and fimH, hlyA, traT, csgA and crl genes was observed in E. coli isolated from blood samples (Table 8).
Table 7.
Relationships Between Virulence Factors Genes and Resistance Genes in Fecal E. coli Isolates
| Correlations | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| colM | colB | colV | colE1 | colE2-E9 | colIa-lb | fimH | hlyA | traT | CsgA | Crl | bla−CTX-M-15 | bla−oxa-2 | bla−oxa-10 | |
| ColM | NA | – | 0.487 | 0.552* | 0.636* | 0.616* | 0.574* | 0.208 | 0.132 | 0.366 | 0.371 | 0.018a | . | −0.245* |
| ColB | – | NA | – | – | – | – | – | – | – | – | – | – | – | – |
| ColV | NA | 0.423 | 0.600* | 0.680** | 0.458 | 0.269 | 0.221 | 0.434 | 0.545 | −0.144a | – | 0.063 | ||
| Col E1 | NA | 0.260 | 0.384 | 0.298 | 0.057 | −0.007 | 0.206 | 0.212* | 0.090a | – | 0.134 | |||
| Col E2-E9 | NA | 0.972** | 0.226 | 0.037 | −0.016 | 0.187 | 0.129* | −0.215a | – | −0.394 | ||||
| Col Ia-Ib | NA | 0.196 | −0.013 | −0.019 | 0.182 | 0.158* | −0.251a | – | −0.380 | |||||
| fimH | NA | 0.719** | 0.740** | 0.825** | 0.857* | −0.057a | – | 0.224 | ||||||
| hlyA | NA | 0.859** | 0.843** | 0.847 | −0.288a | – | 0.168 | |||||||
| traT | NA | 0.833 | 0.905 | −0.265 | – | 0.155 | ||||||||
| CsgA | NA | 0.918 | −0.234 | – | 0.116 | |||||||||
| Crl | NA | −0.252 | – | 0.160 | ||||||||||
| bla−CTX-M-15 | NA | – | 0.714 | |||||||||||
| bla-Oxa-2 | NA | – | ||||||||||||
| bla−Oxa-10 | . | NA | ||||||||||||
Notes: Statistical analysis of associations between virulence factors (VFs). P values were calculated by Fisher’s exact test. *Correlation is significant at 0.05 level (2-tailed). **Correlation is significant at 0.01 level (2-tailed). aCannot be computed because at least one variable is constant.
Abbreviation: NA, not applicable.
fimH gene showed significant strong association only with traT gene in uropathogenic E. coli (UPEC) isolates and those isolated from wound infections but showed a significant strong positive association with hlyA, traT, csgA and crl genes in E. coli isolated from stool and blood samples. On the other hand, hlyA showed a strong positive association with csgA gene in UPEC isolates. Furthermore, hlyA showed a strong correlation with fimH, traT, csgA in blood and stool isolates. In fecal isolates, a strong association between hlyA, traT, csgA and crl genes was observed (Tables 5–8).
Association of Virulence Factors and Resistance Genes
It was found that bla−CTX-M-15 gene showed significant (P<0.01) positive association with colV, colE2-E9, col Ia-lb, hlyA and csgA in UPEC isolates but showed a negative association with the tested virulence genes in E. coli isolated from stool. Also, bla−CTX-M-15 showed no significant correlation with colV, fimH, traT genes in E. coli isolated from blood samples and colV, fimH, hlyA and traT in E. coli isolated from Wound samples. bla−OXA-2 showed strong correlations with colM, colB, colE and crl genes in UPEC but showed moderate correlations with colM in wound isolates. bla-OXA-10 was mostly associated with bla-CTX-M-15 in case of E. coli isolated from stool and blood samples, with traT, hlyA and bla-CTX-M-15 in case of E. coli isolated from wound samples and with colM, colB, crl and bla-CTX-M-15 genes in case of uropathogenic E. coli (Tables 5–8).
Discussion
Having many bacterial virulence factors was reported to affect the severity and the extent of infection of any pathogenic microorganisms. In addition, the ability of a microorganism to cause diseases depends not only on their virulence factors but also due to the patient underlying diseases and the other host determinants.42–44
Fimbriae and pili have a role in the hydrophobic characters of bacterial cells and in the adhesion. Hemolytic activity plays a role in tissue damage and the interference with the local immune response. Also, MRHA are adhesive factors which are essential in the well establishment of E. coli to various tissues. Cell surface hydrophobicity of the bacterial cell surface promotes the adherence of the bacteria to various surfaces like the mucosal epithelial cells. Our results showed that the hemolytic activity, mannose resistant haemagglutination and curli fimbriae production were more common in the urinary tract infection isolates in comparison to other extra-intestinal and fecal isolates which were in agreement with that reported by Fakruddin et al45 and Najar et al25 Furthermore, we found that hydrophobic E. coli were common among blood isolates that were different from that reported by Fakruddin et al45 who found that urinary isolates were more hydrophobic than isolates from other sources but blood isolates showed low hydrophobicity with high values of salt aggregation test (SAT) suggesting that surface hydrophobicity has the minor role in the pathogenesis of septicemia. Shruthi et al46 reported that MRHA was more in fecal isolates than in urine isolates.
Biofilm formation is a crucial step that facilitates the initial adhesion, exopolysaccharide production and subsequent dispersion and spread. Our results showed no significant difference among the tested E. coli isolates isolated from different sources but it was observed that biofilm production was most common among isolates obtained from blood and urine samples. Reisner et al47 reported that biofilm production is not dependent on the E. coli origin but it is affected by the composition of growth media, environmental conditions and the expression of some biofilm promoting factors such as curli and nonconjugative pili which can increase biofilm production. In addition, most E. coli isolates were moderate biofilm producers (urine (45.4%), stool (34.7), blood (44.4%) and wound swabs (30%)). Prevalence of moderate production of biofilm by urine isolates was also reported by Samie and Nkgau48 Protease production was common in fecal and urine isolates that may indicate the ability of these isolates to cause damage to urinary and the intestinal cells. Fujishige et al49 and Vermelho et al50 reported the importance of detecting the proteolytic activity of the microorganisms that help in the understanding of their role in the pathogenesis and tissue damage.
Colicin production is an important character that is observed in both pathogenic and commensal E. coli. Colicins have mainly three cytotoxic functions which are: nuclease activity causing degradation of DNA or RNA of the target cells (colicins E2-E9), pore-forming colicins which can form channels and depolarize cytoplasmic membranes (colB, col Ia-Ib, K) and the inhibition of peptidoglycan synthesis that only represented by colicin M.51
Irrespective to E. coli isolates from stool samples, Uropathogenic E. coli showed a high prevalence of colM and colE1 in comparison to other ExPEC that was in agreement with Azpiroz et al52 and Rijavec et al53 ColV (microcin V) was common among ExPEC isolated from blood which agreed with that reported by Davies et al,54 Fakruddin et al45 and Micenková et al55 E. coli isolated from wound samples showed a high prevalence of colM in comparison to the other ExPEC while 50% of isolates were positive for Col Ia-Ib which is in agreement with that reported by Micenková et al.55
There was a positive correlation among colicin production and the expression of other virulence factors. Many researchers showed the high frequency and the positive correlation of bacteriocin production and the expression of many virulence factors indicating the possibility of their contribution to E. coli pathogenicity.9,55-57 Ozanne et al58 and Smith59 showed that mice injected by colV showed 100% death for macrophages in the peritoneal fluids. Also, mice showed symptoms resemble that observed in endotoxin shock. These findings suggested the contribution of colV in E. coli pathogenesis.
In this study we tried to determine the most frequently occurring virulence factors among E. coli isolates isolated from different origins. fimH gene is the gene encoding type 1 fimbriae and is important in the establishment of infections. It was found that fimH, hlyA, traT, csgA, and crl genes were more common among Uropathogenic E. coli compared to isolates of other ExPEC and intestinal isolates indicating that uropathogenic isolates were more virulent than other tested isolates. Cergole-Novella et al60 showed that there was an association among fimH, crl, csg, traT and colV with bla−CTX-M-15 in E. coli isolated from gastroenteritis which was in agreement with our results.
The high prevalence and association of fimH (90.9%) with uropathogenic isolates were reported by many studies.61–63 On the other hand, some studies showed a lower incidence of fimH among uropathogenic isolates such as Tabasi et al64 and Paniagua-Contreras et al14 HlyA gene was more frequently common among uropathogenic E. coli and those isolated from blood (81.8% and 55.5%). Prevalence of hemolysin protein contributes to virulence of both E. coli of urine or blood origin as it is a pore-forming protein. Also, it was found associated with isolates of urinary tract infections that may give rise to bacteremia.65,66 This study showed that traT was more common among E. coli isolated from urine and blood samples (59.1% and 55.5%, respectively). E. coli with serum resistance were highly virulent, as they can escape the complement system and promote serum survival and increase the risk of developing septic shock and the increase in mortality.3,16 In our study, Multi-drug resistance (MDR) (resistance to ≥3 antimicrobials of different classes) to most of the tested antibiotics was more common among urine and blood E. coli isolates especially to cefepime (100% resistance) and the other tested cephalosporins. Ciprofloxacin resistance was observed mostly among urine and blood isolates (50% and 66.6%, respectively) which in agreement with Raeispour and Ranjbar,67 Abdi et al68 and Hashemizadeh et al69 Cergole-Novella et al60 showed that fimH, crl, csg, traT and colV were common among all tested E. coli obtained from different sources (urinary tract infection, septicemia, respiratory infection and gastroenteritis) with 100% prevalence of fimH, crl, csg genes among all isolates followed by traT (83.3%). Also, they showed that biofilm production was observed among isolates from gastroenteritis, sepsis and UTI.
ESBL production was found to be more common among E. coli isolated from blood and urine samples. Also, all tested resistance genes (bla−CTX-M-15, bla−oxa-2, and bla−oxa-10) were found to be more prevalent among E. coli isolates obtained from urine and blood.70 OXA-type β- lactamases have high hydrolytic activity against oxacillin and cloxacillin but they are poorly inhibited by clavulanic acid. OXA-2 and OXA-10 have recently reported to have extended hydrolytic spectrum to include oxyimino cephalosporins. OXA-2 was first reported in pseudomonas spp. then in E. coli from Israel in 2005. Many studies reported that the increase in the expression of different virulence factors results in the increase of the microbial pathogenicity. Also, antibiotic resistance genes expression was found to increase the microbial pathogenicity. So, antibiotic resistance genes were considered as a subtype of virulence factors. By using biofilm as an example, the presence of pili, fimbriae, flagella promotes the adhesion of microbes to biotic or abiotic surfaces.71,72 In addition, these factors promote the formation of biofilm and the expression of quorum sensing signals (regulates cellular functions depending on the cellular density) resulting in the increase of pathogenicity and resistance to antibiotics.73 Furthermore, it was found that there are large plasmids that carry many virulence genes in association with antibiotic resistance genes (hybrid plasmids) which means that selection of these plasmids by antibiotics may select for some virulence characteristics (horizontal gene transfer) as an adverse effect to the antibiotic therapy.72 In another study done by Escudeiro et al,74 the authors reported that there is a strong correlation among virulence factors and antibiotic resistance and the acquisition of new virulence genes is followed by the acquisition of new resistance genes. From the previous findings, there are a widespread of virulence genes in association with resistance genes which increase the need for enhanced surveillance and the emergence of new antimicrobials with anti-virulence ability.
Conclusion
The relationship between virulence factors and resistance genes is complex and needs more studies that should be specific for each area. There is a significant association among colicin, virulence and resistance genes indicating their contribution in the establishment and the progress of infection, especially with ExPEC. Extra-intestinal E. coli isolated from urine and blood samples represent a battery of virulence factors and resistance genes with a great ability to produce biofilm which is considered a great challenging health problem. So, there is a need for studying how to control these factors to decrease the rate and the severity of infections by the emergence of new antimicrobials with anti-virulence ability.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. The authors received no financial support for the research or publication of this article.
Informed Consent
Informed consent is not required as samples were obtained from the laboratory of hospitals as part of the routine hospital laboratory procedure.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Chapman TA, Wu X-Y, Barchia I, et al. Comparison of virulence gene profiles of escherichia coli strains isolated from healthy and diarrheic swine. Appl Environ Microbiol. 2006;72(7):4782. doi: 10.1128/AEM.02885-05 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Poey ME, Albini M, Saona G, Laviña M. Virulence profiles in uropathogenic Escherichia coli isolated from pregnant women and children with urinary tract abnormalities. Microb Pathog. 2012;52(5):292–301. doi: 10.1016/j.micpath.2012.02.006 [DOI] [PubMed] [Google Scholar]
- 3.Micenková L, Beňová A, Frankovičová L, et al. Human Escherichia coli isolates from hemocultures: septicemia linked to urogenital tract infections is caused by isolates harboring more virulence genes than bacteraemia linked to other conditions. Int J Med Microbiol. 2017;307(3):182–189. doi: 10.1016/j.ijmm.2017.02.003 [DOI] [PubMed] [Google Scholar]
- 4.Petkovšek Ž, Žgur-Bertok D, Erjavec MS. Colicin insensitivity correlates with a higher prevalence of extraintestinal virulence factors among Escherichia coli isolates from skin and soft-tissue infections. J Med Microbiol. 2012;61(6):762–765. doi: 10.1099/jmm.0.037234-0 [DOI] [PubMed] [Google Scholar]
- 5.Konisky J. Colicins and other bacteriocins with established modes of action. Annu Rev Microbiol. 1982;36(1):125–144. doi: 10.1146/annurev.mi.36.100182.001013 [DOI] [PubMed] [Google Scholar]
- 6.Zakharov SD, Zhalnina MV, Sharma O, Cramer WA. The colicin E3 outer membrane translocon: immunity protein release allows interaction of the cytotoxic domain with OmpF porin. Biochemistry. 2006;45(34):10199–10207. [DOI] [PubMed] [Google Scholar]
- 7.Stahl CH, Callaway TR, Lincoln LM, Lonergan SM, Genovese KJ. Inhibitory activities of colicins against Escherichia coli strains responsible for postweaning diarrhea and edema disease in swine. Antimicrob Agents Chemother. 2004;48(8):3119–3121. doi: 10.1128/AAC.48.8.3119-3121.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tomita K, Ogawa T, Uozumi T, Watanabe K, Masaki H. A cytotoxic ribonuclease which specifically cleaves four isoaccepting arginine tRNAs at their anticodon loops. Proc Natl Acad Sci. 2000;97(15):8278–8283. doi: 10.1073/pnas.140213797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azpiroz MF, Laviña M. Modular structure of microcin H47 and colicin V. Antimicrob Agents Chemother. 2007;51(7):2412–2419. doi: 10.1128/AAC.01606-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Micenková L, Frankovičová L, Jaborníková I, et al. Escherichia coli isolates from patients with inflammatory bowel disease: ExPEC virulence-and colicin-determinants are more frequent compared to healthy controls. Int J Med Microbiol. 2018;308(5):498–504. doi: 10.1016/j.ijmm.2018.04.008 [DOI] [PubMed] [Google Scholar]
- 11.Mulvey MA. Adhesion and entry of uropathogenic Escherichia coli. Cell Microbiol. 2002;4(5):257–271. doi: 10.1046/j.1462-5822.2002.00193.x [DOI] [PubMed] [Google Scholar]
- 12.Pal M, Singh S. PCR based detection of adhesive curli gene “crl” and ‘csgA’in avian pathogenic Escherichia coli. Indian J Anim Res. 2007;41(3):226–229. [Google Scholar]
- 13.Blum G, Ott M, Lischewski A, et al. Excision of large DNA regions termed pathogenicity islands from tRNA-specific loci in the chromosome of an Escherichia coli wild-type pathogen. Infect Immun. 1994;62(2):606–614. doi: 10.1128/IAI.62.2.606-614.1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Paniagua-Contreras GL, Monroy-Perez E, Rodriguez-Moctezuma JR, Dominguez-Trejo P, Vaca-Paniagua F, Vaca S. Virulence factors, antibiotic resistance phenotypes and O-serogroups of Escherichia coli strains isolated from community-acquired urinary tract infection patients in Mexico. J Microbiol Immunol Infect. 2017;50(4):478–485. doi: 10.1016/j.jmii.2015.08.005 [DOI] [PubMed] [Google Scholar]
- 15.Chiou -Y-Y, Chen M-J, Chiu N-T, Lin C-Y, Tseng -C-C. Bacterial virulence factors are associated with occurrence of acute pyelonephritis but not renal scarring. J Urol. 2010;184(5):2098–2102. doi: 10.1016/j.juro.2010.06.135 [DOI] [PubMed] [Google Scholar]
- 16.Miajlovic H, Smith SG. Bacterial self-defence: how Escherichia coli evades serum killing. FEMS Microbiol Lett. 2014;354(1):1–9. doi: 10.1111/1574-6968.12419 [DOI] [PubMed] [Google Scholar]
- 17.Kallau NHG, Wibawan IWT, Lukman DW, Sudarwanto MB. Detection of multi-drug resistant (MDR) Escherichia coli and tet gene prevalence at a pig farm in Kupang, Indonesia. J Adv Vet Anim Res. 2018;5(4):388–396. doi: 10.5455/javar.2018.e289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Matsumoto Y, Ikeda F, Kamimura T, Yokota Y, Mine Y. Novel plasmid-mediated beta-lactamase from Escherichia coli that inactivates oxyimino-cephalosporins. Antimicrob Agents Chemother. 1988;32(8):1243–1246. doi: 10.1128/AAC.32.8.1243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cantón R, Coque TM. The CTX-M β-lactamase pandemic. Curr Opin Microbiol. 2006;9(5):466–475. doi: 10.1016/j.mib.2006.08.011 [DOI] [PubMed] [Google Scholar]
- 20.Touati A, Benallaoua S, Forte D, Madoux J, Brasme L, De Champs C. First report of CTX-M-15 and CTX-M-3 β-lactamases among clinical isolates of Enterobacteriaceae in Béjaia, Algeria. Int J Antimicrob Agents. 2006;27(5):397–402. doi: 10.1016/j.ijantimicag.2005.12.007 [DOI] [PubMed] [Google Scholar]
- 21.Poirel L, Girlich D, Naas T, Nordmann P. OXA-28, an extended-spectrum variant of OXA-10 β-lactamase from Pseudomonas aeruginosa and its plasmid-and integron-located gene. Antimicrob Agents Chemother. 2001;45(2):447–453. doi: 10.1128/AAC.45.2.447-453.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ullah W, Qasim M, Rahman H, et al. CTX-M-15 and OXA-10 beta lactamases in multi drug resistant Pseudomonas aeruginosa: first report from Pakistan. Microb Pathog. 2017;105:240–244. doi: 10.1016/j.micpath.2017.02.039 [DOI] [PubMed] [Google Scholar]
- 23.Christensen GD, Simpson WA, Younger JJ, et al. Adherence of coagulase-negative staphylococci to plastic tissue culture plates: a quantitative model for the adherence of staphylococci to medical devices. J Clin Microbiol. 1985;22(6):996–1006. doi: 10.1128/JCM.22.6.996-1006.1985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim SH, Kim YH. Escherichia coli O157: h7adherence to HEp-2 cells is implicated with curli expression and outer membrane integrity. J Vet Sci. 2004;5(2):119–124. doi: 10.4142/jvs.2004.5.2.119 [DOI] [PubMed] [Google Scholar]
- 25.Najar AG, Nejad MM, Mansouri S. The comparison between virulence factors of Escherichia coli isolated from urinary tract infections and feacal flora. Res Pharm Sci. 2007;1(2):99–103. [Google Scholar]
- 26.Mansouri S, Norouzi F, Moradi M, Nakhaee N. Comparison of virulence factors among clinical isolates of Pseudomonas aeruginosa producing and non-producing extended spectrum beta-lactamases. Curr Res Bacteriol. 2011;4(3):85–93. doi: 10.3923/crb.2011.85.93 [DOI] [Google Scholar]
- 27.Mattos-Guaraldi AL, Formiga LCD, Andrade AFB. Cell surface hydrophobicity of sucrose fermenting and nonfermenting Corynebacterium diphtheriae strains evaluated by different methods. Curr Microbiol. 1999;38(1):37–42. doi: 10.1007/PL00006769 [DOI] [PubMed] [Google Scholar]
- 28.Maheswari UB, Palvai S, Anuradha PR, Kammili N. Hemagglutination and biofilm formation as virulence markers of uropathogenic Escherichia coli in acute urinary tract infections and urolithiasis. Indian J Urol. 2013;29(4):277–281. doi: 10.4103/0970-1591.120093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Reichhardt C, Jacobson AN, Maher MC, et al. Congo red interactions with curli-producing E. coli and native curli amyloid fibers. PLoS One. 2015;10(10):e0140388. doi: 10.1371/journal.pone.0140388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bauer A, Kirby W, Sherris JC, Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966;45(4_ts):493–496. doi: 10.1093/ajcp/45.4_ts.493 [DOI] [PubMed] [Google Scholar]
- 31.Tzelepi E, Giakkoupi P, Sofianou D, Loukova V, Kemeroglou A, Tsakris A. Detection of extended-spectrum beta-lactamases in clinical isolates of Enterobacter cloacae and Enterobacter aerogenes. J Clin Microbiol. 2000;38(2):542–546. doi: 10.1128/JCM.38.2.542-546.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.CLSI. Performance Standards for Antimicrobial Susceptibility Tests. 27th CLSI supplement M100 Wayne, PA, USA: Clinical Laboratory Standards Institute; 2017 [Google Scholar]
- 33.Wilson K. Preparation of genomic DNA from bacteria. Curr Protoc Mol Biol. 2001;Chapter 2:Unit2.4. [DOI] [PubMed] [Google Scholar]
- 34.Yamamoto S, Terai A, Yuri K, Kurazono H, Takeda Y, Yoshida O. Detection of urovirulence factors in Escherichia coli by multiplex polymerase chain reaction. FEMS Immunol Med Microbiol. 1995;12(2):85–90. doi: 10.1111/j.1574-695X.1995.tb00179.x [DOI] [PubMed] [Google Scholar]
- 35.Johnson JR, Stell AL. Extended virulence genotypes of Escherichia coli strains from patients with urosepsis in relation to phylogeny and host compromise. J Infect Dis. 2000;181(1):261–272. doi: 10.1086/315217 [DOI] [PubMed] [Google Scholar]
- 36.Schamberger GP, Diez-Gonzalez F. Characterization of colicinogenic Escherichia coli strains inhibitory to enterohemorrhagic Escherichia coli. J Food Prot. 2004a;67(3):486–492. doi: 10.4315/0362-028X-67.3.486 [DOI] [PubMed] [Google Scholar]
- 37.Schamberger GP, Phillips RL, Jacobs JL, Diez-Gonzalez F. Reduction of Escherichia coli O157: H7 populations in cattle by addition of colicin E7-producing E. coli to feed. Appl Environ Microbiol. 2004b;70(10):6053–6060. doi: 10.1128/AEM.70.10.6053-6060.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bhattacharjee A, Sen MR, Anupurba S, Prakash P, Nath G. Detection of OXA-2 group extended-spectrum-β-lactamase-producing clinical isolates of Escherichia coli from India. J Antimicrob Chemother. 2007;60(3):703–704. doi: 10.1093/jac/dkm267 [DOI] [PubMed] [Google Scholar]
- 39.Lin SP, Liu MF, Lin CF, Shi ZY. Phenotypic detection and polymerase chain reaction screening of extended-spectrum beta-lactamases produced by Pseudomonas aeruginosa isolates. J Microbiol Immunol Infect. 2012;45(3):200–207. doi: 10.1016/j.jmii.2011.11.015 [DOI] [PubMed] [Google Scholar]
- 40.Tahamtan Y, Shirazi Z, Pourbakhsh A, et al. Detection of colicin genes by PCR in Escherichia coli isolated from cattle in Shiraz-Iran. Arch Razi Inst. 2012;67(1):63–67. [Google Scholar]
- 41.Sambrook J, Russell D. Molecular cloning: a laboratory manual. Mol Cloning a Lab Man. 2001. [Google Scholar]
- 42.Dale AP, Woodford N. Extra-intestinal pathogenic Escherichia coli (ExPEC): disease, carriage and clones. J Infect. 2015;71(6):615–626. doi: 10.1016/j.jinf.2015.09.009 [DOI] [PubMed] [Google Scholar]
- 43.Lefort A, Panhard X, Clermont O, et al. Host factors and portal of entry outweigh bacterial determinants to predict the severity of Escherichia coli bacteremia. J Clin Microbiol. 2011;49(3):777–783. doi: 10.1128/JCM.01902-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jauréguy F, Carbonnelle E, Bonacorsi S, et al. Host and bacterial determinants of initial severity and outcome of Escherichia coli sepsis. Clin Microbiol Infect. 2007;13(9):854–862. doi: 10.1111/j.1469-0691.2007.01775.x [DOI] [PubMed] [Google Scholar]
- 45.Fakruddin M, Mazumdar RM, Chowdhury A, Mannan KSB. A preliminary study on virulence factors & antimicrobial resistance in extra-intestinal pathogenic Escherichia coli (ExPEC) in Bangladesh. Indian J Med Res. 2013;137(5):988–990. [PMC free article] [PubMed] [Google Scholar]
- 46.Shruthi N, Kumar R. Phenotypic study of virulence factors in Escherichia coli isolated from antenatal cases, catheterized patients, and faecal flora. J Clin Diagn Res. 2012;6(10):1699–1703. doi: 10.7860/JCDR/2012/4669.2634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Reisner A, Krogfelt KA, Klein BM, Zechner EL, Molin S. In vitro biofilm formation of commensal and pathogenic escherichia coli strains: impact of environmental and genetic factors. J Bacteriol. 2006;188(10):3572–3581. doi: 10.1128/JB.188.10.3572-3581.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Samie A, Nkgau T. Biofilm production and antibiotic susceptibility profile of Escherichia coli isolates from HIV and AIDS patients in the Limpopo Province. Afr J Biotechnol. 2012;11(34):8560–8570. doi: 10.5897/AJB11.2865 [DOI] [Google Scholar]
- 49.Fujishige A, Smith KR, Silen JL, Agard DA. Correct folding of alpha-lytic protease is required for its extracellular secretion from Escherichia coli. J Cell Biol. 1992;118(1):33–42. doi: 10.1083/jcb.118.1.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Vermelho AB, Meirelles MNL, Lopes A, Petinate SDG, Chaia AA, Branquinha MH. Detection of extracellular proteases from microorganisms on agar plates. Mem Inst Oswaldo Cruz. 1996;91(6):755–760. doi: 10.1590/S0074-02761996000600020 [DOI] [PubMed] [Google Scholar]
- 51.Hahn-Löbmann S, Stephan A, Schulz S, et al. Colicins and Salmocins – new classes of plant-made non-antibiotic food antibacterials. Front Plant Sci. 2019;10:437. doi: 10.3389/fpls.2019.00437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Azpiroz MF, Poey ME, Laviña M. Microcins and urovirulence in Escherichia coli. Microb Pathog. 2009;47(5):274–280. doi: 10.1016/j.micpath.2009.09.003 [DOI] [PubMed] [Google Scholar]
- 53.Rijavec M, Budič M, Mrak P, Müller-Premru M, Podlesek Z, Žgur-Bertok D. Prevalence of ColE1-like plasmids and colicin K production among uropathogenic Escherichia coli strains and quantification of inhibitory activity of colicin K. Appl Environ Microbiol. 2007;73(3):1029–1032. doi: 10.1128/AEM.01780-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Davies D, Falkiner F, Hardy K. Colicin V production by clinical isolates of Escherichia coli. Infect Immun. 1981;31(2):574–579. doi: 10.1128/IAI.31.2.574-579.1981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Micenková L, Bosák J, Vrba M, Ševčíková A, Šmajs D. Human extraintestinal pathogenic Escherichia coli strains differ in prevalence of virulence factors, phylogroups, and bacteriocin determinants. BMC Microbiol. 2016;16(1):218. doi: 10.1186/s12866-016-0835-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Budič M, Rijavec M, Petkovšek Ž, Žgur-Bertok D. Escherichia coli bacteriocins: antimicrobial efficacy and prevalence among isolates from patients with bacteraemia. PLoS One. 2011;6(12):e28769. doi: 10.1371/journal.pone.0028769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Šmajs D, Micenková L, Šmarda J, et al. Bacteriocin synthesis in uropathogenic and commensal Escherichia coli: colicin E1 is a potential virulence factor. BMC Microbiol. 2010;10(1):288. doi: 10.1186/1471-2180-10-288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ozanne G, Mathieu L, Baril J. Production of colicin V in vitro and in vivo and observations on its effects in experimental animals. Infect Immun. 1977;17(3):497–503. doi: 10.1128/IAI.17.3.497-503.1977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Smith HW. A search for transmissible pathogenic characters in invasive strains of Escherichia coli: the discovery of a plasmid-controlled toxin and a plasmid-controlled lethal character closely associated, or identical, with colicine V. Microbiology. 1974;83(1):95–111. [DOI] [PubMed] [Google Scholar]
- 60.Cergole-Novella MC, Pignatari AC, Guth BE. Adhesion, biofilm and genotypic characteristics of antimicrobial resistant Escherichia coli isolates. Braz J Microbiol. 2015;46(1):167–171. doi: 10.1590/S1517-838246120140077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Malekzadegan Y, Khashei R, Sedigh Ebrahim-Saraie H, Jahanabadi Z. Distribution of virulence genes and their association with antimicrobial resistance among uropathogenic Escherichia coli isolates from Iranian patients. BMC Infect Dis. 2018;18(1):572. doi: 10.1186/s12879-018-3467-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Lee J, Subhadra B, Son YJ, et al. Phylogenetic group distributions, virulence factors and antimicrobial resistance properties of uropathogenic Escherichia coli strains isolated from patients with urinary tract infections in South Korea. Lett Appl Microbiol. 2016;62(1):84–90. doi: 10.1111/lam.12517 [DOI] [PubMed] [Google Scholar]
- 63.Gao Q, Zhang D, Ye Z, et al. Virulence traits and pathogenicity of uropathogenic Escherichia coli isolates with common and uncommon O serotypes. Microb Pathog. 2017;104:217–224. doi: 10.1016/j.micpath.2017.01.027 [DOI] [PubMed] [Google Scholar]
- 64.Tabasi M, Karam MRA, Habibi M, Yekaninejad MS, Bouzari S. Phenotypic assays to determine virulence factors of uropathogenic Escherichia coli (UPEC) isolates and their correlation with antibiotic resistance pattern. Osong Public Health Res Perspect. 2015;6(4):261–268. doi: 10.1016/j.phrp.2015.08.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Daga AP, Koga VL, Soncini JGM, et al. Escherichia coli Bloodstream Infections in Patients at a University Hospital: virulence Factors and Clinical Characteristics. Front Cell Infect Microbiol. 2019;9:191. doi: 10.3389/fcimb.2019.00191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sonnen AF-P, Henneke P. Role of pore-forming toxins in neonatal sepsis. Clin Dev Immunol. 2013;2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Raeispour M, Ranjbar R. Antibiotic resistance, virulence factors and genotyping of Uropathogenic Escherichia coli strains. Antimicrob Resist Infect Control. 2018;7(1):118. doi: 10.1186/s13756-018-0411-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Abdi S, Ranjbar R, Vala MH, Jonaidi N, Bejestany OB, Bejestany FB. Frequency of bla TEM, bla SHV, bla CTX-M, and qnrA among Escherichia coli isolated from urinary tract infection. Arch Clin Infect Dis. 2014;9(1):e18690. doi: 10.5812/archcid.18690 [DOI] [Google Scholar]
- 69.Hashemizadeh Z, Kalantar-Neyestanaki D, Mansouri S. Correlation between hlyA and cnf1 virulent genes with antibiotic resistance and non-ESBLs escherichia coli isolates collected from patient with urinary tract infections in Kerman, Iran. Arch Pediatr Infect Dis. 2017;5(4):e61653. doi: 10.5812/pedinfect.61653 [DOI] [Google Scholar]
- 70.Alqasim A, Abu Jaffal A, Alyousef AA. Prevalence and molecular characteristics of sequence type 131 clone among clinical uropathogenic Escherichia coli isolates in Riyadh, Saudi Arabia. Saudi J Biol Sci. 2020;27(1):296–302. doi: 10.1016/j.sjbs.2019.09.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ramirez MS, Traglia GM, Lin DL, Tran T, Tolmasky ME. Plasmid-mediated antibiotic resistance and virulence in gram-negatives: the klebsiella pneumoniae paradigm. Microbiol Spectr. 2014;2(5):1–15. doi: 10.1128/microbiolspec.PLAS-0016-2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Turton J, Davies F, Turton J, Perry C, Payne Z, Pike R. Hybrid resistance and virulence plasmids in “high-risk” clones of klebsiella pneumoniae, including those carrying blaNDM-5. Microorganisms. 2019;7(9):326. doi: 10.3390/microorganisms7090326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rubini D, Varthan PV, Jayasankari S, Vedahari BN, Nithyanand P. Suppressing the phenotypic virulence factors of Uropathogenic Escherichia coli using marine polysaccharide. Microb Pathog. 2020;141:103973. doi: 10.1016/j.micpath.2020.103973 [DOI] [PubMed] [Google Scholar]
- 74.Escudeiro P, Pothier J, Dionisio F, Nogueira T. Antibiotic resistance gene diversity and virulence gene diversity are correlated in human gut and environmental microbiomes. mSphere. 2019;4(3):e00135–e00119. doi: 10.1128/mSphere.00135-19 [DOI] [PMC free article] [PubMed] [Google Scholar]