Abstract
Recent evidence indicates the usefulness of lung ultrasound (LUS) in detecting coronavirus disease 19 (COVID-19) pneumonia. However, no data are available on the use of LUS in children with COVID-19 pneumonia. In this report, we describe LUS features of 10 consecutively admitted children with COVID-19 in two tertiary-level pediatric hospitals in Rome. LUS revealed signs of lung involvement during COVID-19 infection. In particular, vertical artifacts (70%), pleural irregularities (60%), areas of white lung (10%) and subpleural consolidations (10%) were the main findings in patients with COVID-19. No cases of pleural effusions were found. According to our experience, the routine use of LUS in the evaluation of children with suspected or confirmed COVID-19, when performed by clinicians with documented experience in LUS, was useful in diagnosing and monitoring pediatric COVID-19 pneumonia, reducing unnecessary radiation/sedation in children and exposure of health care workers to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Key Words: Lung ultrasound, Coronavirus disease 19 (COVID-19), Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), Children
Introduction
Initially described in China in December 2019, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has spread all over the world, infecting more than 1 million people and causing thousands of deaths (Zhu et al. 2020). Humans of all age groups are susceptible, including the youngest. Although currently pediatric coronavirus disease 19 (COVID-19) appears to be less severe compared with the adult form, children are by no means spared. Several case series (Dong et al. 2020; Lu et al. 2020b; Qiu et al. 2020; Tagarro et al. 2020) have documented that COVID-19 can affect children of all ages, from newborns to adolescents. Importantly, COVID-19 pneumonia has also been described in asymptomatic or pauci-symptomatic children (Dong et al. 2020; Lu et al. 2020a; Qiu et al. 2020).
Although a nasopharyngeal swab is required for a definitive etiologic diagnosis, this test has limitations, particularly because of its low sensitivity (Wang et al. 2020). For this reason, several authors have suggested the use of chest computed tomography (CT) not only for diagnosis of COVID-19 pneumonia, but also as a screening tool for the diagnosis of COVID-19 infection in epidemic settings, as CT has been reported to have better diagnostic sensitivity than nasopharyngeal swab (Ai et al. 2020). Conversely, Rubin et al. (2020) suggested an appropriate use of imaging, selecting those patients that might benefit from the adjunctive information contained in images. However, CT scan should not be routinely used in specific age groups, such as pregnant women (Moro et al. 2020) and children. Moreover, COVID-19 has become a global disease, logistic difficulties or unavailability of CT scan in low- and medium-resource settings must be considered. On the other hand, chest X-ray does not have sufficient sensitivity and specificity for detecting COVID-19 pneumonia to be considered as an alternative tool to CT scan.
In this context, recent evidence has indicated the usefulness of lung ultrasound (LUS) in detecting COVID-19 pneumonia (Buonsenso et al. 2020a; Kalafat et al. 2020; Smith et al. 2020). In particular, both Chinese (Peng et al. 2020) and Italian (Soldati et al. 2020a, 2020b) task forces on the use of LUS in COVID-19 have provided the physical bases and LUS patterns in COVID-19 patients, suggesting that LUS can be a useful tool to diagnose and monitor COVID-19 pneumonia. However, no data are available on the use of LUS in children with COVID-19 pneumonia.
For this reason, we performed this study with the aim of evaluating the role of LUS in children with COVID-19.
Methods
We conducted an observational study analyzing LUS patterns in consecutively admitted children with COVID-19 infection in two tertiary level pediatric hospitals in Rome, beginning March 15, 2019. All patients with swab-confirmed COVID-19 infection who underwent LUS within 12 h from admission were included. The use of LUS in the evaluation of children with respiratory infection has been approved by the ethics committees of our institutions. Informed consent was obtained from each parent/guardian. LUS was performed with a wireless pocket device connected to a probe, which were placed in single-use plastic covers (ATL Milano, Milan, Italy), as described by Buonsenso et al. (2020b). LUS was performed in patients in the sitting position, and all lung areas were scanned, as suggested by Soldati et al. (2020a). The two operators responsible for LUS are pediatricians with more than 5 y of experience in point-of-care ultrasound and several publications in this setting (Buonsenso et al. 2020a, 2020b, 2020c, 2020d; Musolino et al. 2019a, 2019b). The LUS patterns looked for were those described by Soldati et al. (2020a): pleural irregularities, subpleural consolidations, vertical artifacts, patchy areas of white lung, pleural effusions.
Results
We evaluated 10 consecutively admitted children with COVID-19 with positive real-time polymerase chain reaction on nasopharyngeal swabs. LUS was performed on admission when real-time polymerase chain reaction results were still pending. Clinical, laboratory and imaging parameters and outcome data are summarized in Table 1 . The median age was 11 y (interquartile range: 4 y 9 mo to 15 y). Previous medical history was unremarkable in all cases. All patients were symptomatic at the time of admission to the hospital, with fever in 80%, cough in 50% and diarrhea in 20% of cases. Anosmia (10%), arthralgia (30%), chest pain (20%) and headache (20%) were also reported. Results of laboratory investigations were within normal ranges according to patient age in all cases, with the exception of two children: one had leukopenia, and the other had a slightly altered C-reactive protein level. All children recovered, and none of them required pediatric intensive care admission.
Table 1.
Main Clinical, Laboratory and Imaging Findings in a cohort of pediatric patients with COVID-19.
| Total | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Patient 7 | Patient 8 | Patient 9 | Patient 10 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age, y | 11 (4 y 9 mo–15 y) | 13 | 1 | 15 | 1 | 15 | 6 | 16 | 10 | 12 | 7 |
| Sex | 60% Male | M | F | F | F | M | M | F | M | M | M |
| Symptoms | |||||||||||
| Fever | 80% | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes |
| Cough | 50% | Yes | Yes | Yes | Yes | No | No | Yes | No | No | No |
| Diarrhea | 20% | No | No | No | No | No | No | No | Yes | Yes | No |
| Other | No | No | Chest pain | No | Seizure (not related) | No | Chest pain Anosmia | Arthralgia Headache | Arthralgia Headache | Arthralgia | |
| WBCs/mm3 | 5520 (4550–7345) | 5400 | 14,170 | 7000 | — | 7460 | 5640 | 2790 | 4440 | 4900 | — |
| L/mm3 | 2055 (1470–2922) | 1970 | 5870 | 2140 | — | 1040 | 3150 | 1340 | 1860 | 2240 | — |
| CRP mg/L | 1,6 (0.375–5.05) | 5.5 | 33.6 | 2.4 | — | 0.8 | 0.6 | 3.7 | 0.3 | 0.3 | — |
| X-Ray Localization Consolidation Interstitial Effusion |
Not performed | Not performed |
Left No Yes No |
Not performed | Not performed | Not performed |
Bilateral No Yes No |
Not performed | Not performed | Not performed | |
| CT scan Localization Consolidation Ground glass Interstitial Effusion |
Not performed | Not performed | Not performed | Not performed | MRI* Left Yes No No No |
Not performed |
Left No Yes No No |
Not performed | Not performed | Not performed | |
| Lung ultrasound Localization Pleural irregularities Vertical artifacts White lung Consolidations Pleural effusion |
70% Bilateral 60% 70% 10% 10% 0% |
Monolateral No Yes No Yes No |
Bilateral No Yes No No No |
Bilateral Yes Yes No No No |
Bilateral No Yes No No No |
Monolateral Yes Yes No No No |
Bilateral No Yes No No No |
Monolateral Yes Yes Yes No No |
Bilateral Yes No No No No |
Bilateral Yes No No No No |
Bilateral Yes No No No No |
CRP = C-reactive protein; CT = computed tomography; L/mm3 = Lymphocite/mm3; MRI = magnetic resonance imaging; WBCs = white blood cells.
Variables are expressed as a percentage or median (interquartile range).
This patient underwent lung MRI, as brain MRI was necessary because the child had complicated afebrile seizures.
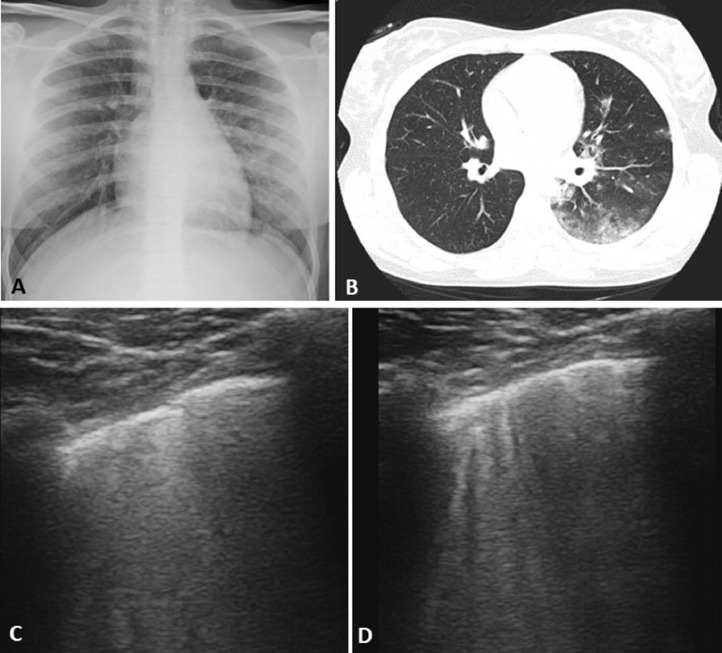
In all symptomatic cases, LUS revealed signs of lung involvement during COVID-19 infection. In particular, vertical artifacts, areas of white lung and subpleural consolidations and pleural irregularities were the main findings in pediatric COVID-19 pneumonia. There were no cases of pleural effusions. In one case, CT scan was performed, and LUS findings correlated well with chest CT (Fig. 1 ). Patient 5 was admitted for complex afebrile seizures, so to minimize the child's movements and reduce the risk of nosocomial spread, the lung imaging of choice was magnetic resonance imaging (MRI) as an extension of the brain MRI dictated by his admitting diagnosis. His pulmonary MRI revealed signs of pneumonia, confirming the LUS findings. Two patients underwent chest X-ray that revealed non-specific, diffuse interstitial thickening.
Fig. 1.
Main imaging findings in patient 7 with confirmed COVID-19. (a) Chest X-ray reveals diffuse interstitial disease, with the left lobe more involved. (b) Computed tomography scan reveals ground glass and subpleural consolidations. (c, d) Lung ultrasound reveals patchy areas of white lung (c) and long, bright, thick vertical artifacts (d).
Discussion
In this study, we found that LUS is able to detect lung pathology in children with confirmed COVID-19. In particular, LUS patterns seen in our patients were mainly vertical artifacts, pleural irregularities, subpleural consolidations and patchy areas of white lung. Since our proposal for more frequent use of LUS in COVID-19 patients (Buonsenso et al. 2020b) and the first description of a patient with vertical artifacts, pleural irregularities and subpleural consolidations (Buonsenso et al. 2020d), growing evidence in adults has revealed that LUS is able to detect COVID-19. during SARS-CoV-2 infection is much more frequent in adults than in children; however, the main patterns are similar to those we described in children. Both Italian sonographers and the Chinese Critical Care Ultrasound Study Group (Peng et al. 2020) described the same patterns in adults. Importantly, LUS has been documented as an important tool particularly in moderate to severe pneumonia (Lu et al. 2020b) and, mainly, in the monitoring of lung disease (Moro et al. 2020).
The finding that LUS is able to detect COVID-19 pneumonia in children has clinical implications. The Chinese Task Force for Pediatric COVID-19 proposed a severity classification, defining children as asymptomatic, mild, moderate, severe or critical cases (Dong et al. 2020). In particular, the “moderate” stage is based on clinical criteria (pneumonia with fever and cough, in the absence of signs of hypoxemia) and/or radiologic criteria, as “some cases may have no clinical signs and symptoms, but chest CT shows lung lesions, which are subclinical” (Dong et al. 2020). In fact, in all the large series of pediatric COVID-19 described in China (Dong et al. 2020; Lu et al. 2020; Qiu et al. 2020), the authors routinely used CT scan to determine the severity of the disease. This has caused clinicians and researchers from the rest of the world to overuse CT scan in children, even when they are asymptomatic or pauci-symptomatic. However, to date there is no evidence that diagnosis and treatment decisions based on CT scans improve outcomes in pediatric COVID-19 infection. Moreover, CT scanning should be used parsimoniously in the pediatric age group because of their increased sensitivity to radiation exposure and because it may require sedation. In fact, international guidelines state that history and examination are the main determinants of pneumonia severity and level of care, reserving imaging to compromised children requiring admission on clinical grounds (Bradley et al. 2011). Importantly, the large number of asymptomatic and mild pediatric cases of COVID-19 (Dong et al. 2020; Lu et al. 2020; Qiu et al. 2020; Tagarro et al. 2020) described so far confirms that radiologic imaging should not be routinely used. In our series, only in two cases were chest X-ray and CT scan were performed. The small number of patients undergoing traditional imaging is owing mainly to the long experience of our institutions in performing LUS, which is currently routine practice in children with respiratory symptoms that we see in our centers. In this context, thanks to the already proven accuracy of LUS in detecting pediatric pneumonia of any etiology (Pereda et al. 2015; Berce et al. 2019; Musolino et al. 2019a; Supino et al. 2019; Buonsenso et al. 2020c), and in the light of our observational findings, we suggest the routine use of bedside LUS in children with suspected or confirmed COVID-19. As previously suggested (Buonsenso et al. 2020b), LUS would also allow the same pediatrician to both perform the physical examination and collect the lung images, with the advantage of reducing the exposure of other health care workers to infected patients. Moreover, a Multinational Consensus Statement from the Fleischner Society (Rubin et al. 2020) provided five main and three additional recommendations intended to guide medical practitioners in the use of chest X-rays and CT in the management of COVID-19. They concluded, with current knowledge, that (i) imaging is not routinely indicated in patients with suspected COVID-19 and mild clinical features unless they are at risk for disease progression; (ii) imaging is indicated in a patient with COVID-19 and worsening respiratory status; and (iii) in a resource-constrained environment, imaging is indicated for medical triage of patients with suspected COVID-19 who present with moderate-severe clinical features and a high pre-test probability of disease. These guidelines support the appropriate use of imaging and, in this context, point-of-care tools such as LUS, particularly in children, who usually have milder manifestations of COVID-19.
Conclusions
The routine use of LUS in the evaluation of children with suspected or confirmed COVID-19, if performed by clinicians with documented experience in LUS, could be a useful tool in diagnosing and monitoring COVID-19 pneumonia, while reducing unnecessary radiation/sedation in children and exposure of health care workers to SARS-CoV-2.
Acknowledgments
Acknowledgments
We are grateful to all pediatricians and radiologists who actively contributed with both clinical practice and research advice, the ROMULUS COVID Team: Alessia Mesturino, Barbara Scialanga, Elena Boccuzzi, Simona Scateni, Massimo Battaglia, Eugenio Pitaro and Caterina Bock from the Department of Pediatric Emergency, Bambino Gesù Children's Hospital IRCCS, Rome, Italy; and Cristina De Rose, Rosa Morello, Rita De Sanctis, Giuseppe Zampino and Antonio Chiaretti from the Department of Woman and Child Health and Public Health, Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy.
Conflict of interest disclosure
The authors declare no competing interests.
References
- Ai T., Yang Z., Hou H., Zhan C., Chen C., Lv W., Tao Q., Sun Z., Xia L. Correlation of chest CT and RT-PCR testing in coronavirus disease 2019 (COVID-19) in China: A report of 1014 cases. Radiology. 2020;26 doi: 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berce V., Tomazin M., Gorenjak M., Berce T., Lovrenčič B. The usefulness of lung ultrasound for the aetiological diagnosis of community-acquired pneumonia in children. Sci Rep. 2019;9(1):17957. doi: 10.1038/s41598-019-54499-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley J.S., Byington C.L., Shah S.S., Alverson B., Carter E.R., Harrison C., Kaplan S.L., Mace S.E., McCracken G.H., Jr, Moore M.R., St Peter S.D., Stockwell J.A., Swanson J.T., Pediatric Infectious Diseases Society and the Infectious Diseases Society of America The management of community-acquired pneumonia in infants and children older than 3 months of age: Clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53:e25–e76. doi: 10.1093/cid/cir531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buonsenso D., Piano A., Raffaelli F., Bonadia N., de Gaetano Donati K., Franceschi F. Point-of-Care Lung Ultrasound findings in novel coronavirus disease-19 pnemoniae: A case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24:2776–2780. doi: 10.26355/eurrev_202003_20549. [DOI] [PubMed] [Google Scholar]
- Buonsenso D., Pata D., Chiaretti A. COVID-19 outbreak: Less stethoscope, more ultrasound. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30120-X. [e-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buonsenso D., Brancato F., Valentini P., Curatola A., Supino M., Musolino A.M. The use of lung ultrasound to monitor the antibiotic response of community-acquired pneumonia in children: A preliminary hypothesis. J Ultrasound Med. 2020;39:817–826. doi: 10.1002/jum.15147. [DOI] [PubMed] [Google Scholar]
- Buonsenso D., Piano A., Raffaelli F., Bonadia N., de Gaetano Donati K., Franceschi F. Point-of-care lung ultrasound findings in novel coronavirus disease-19 pnemoniaea: A case report and potential applications during COVID-19 outbreak. Eur Rev Med Pharmacol Sci. 2020;24:2776–2780. doi: 10.26355/eurrev_202003_20549. [DOI] [PubMed] [Google Scholar]
- Dong Y., Mo X., Hu Y., Qi X., Jiang F., Jiang Z., Tong S. Epidemiology of COVID-19 among children in China. Pediatrics. 2020 doi: 10.1542/peds.2020-0702. [e-pub ahead of print], Accessed April 2nd. [DOI] [PubMed] [Google Scholar]
- Kalafat E., Yaprak E., Cinar G., Varli B., Ozisik S., Uzun C., Azap A., Koc A. Lung ultrasound and computed tomographic findings in pregnant woman with COVID-19. Ultrasound Obstet Gynecol. 2020 doi: 10.1002/uog.22034. [e-pub ahead of print], Accessed April 10th. [DOI] [PubMed] [Google Scholar]
- Lu X., Zhang L., Du H., Zhang J., Li Y.Y., Qu J., Zhang W., Wang Y., Bao S., Li Y., Wu C., Liu H., Liu D., Shao J., Peng X., Yang Y., Liu Z., Xiang Y., Zhang F., Silva R.M., Pinkerton K.E., Shen K., Xiao H., Xu S., Wong G.W.K., Chinese Pediatric Novel Coronavirus Study Team SARS-CoV-2 infection in children. N Engl J Med. 2020;382:1663–1665. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu W., Zhang S., Chen B., Chen J., Xian J., Lin Y., Shan H., Su Z.Z. A clinical study of noninvasive assessment of lung lesions in patients with coronavirus disease-19 (COVID-19) by bedside ultrasound. Ultraschall Med. 2020 doi: 10.1055/a-1154-8795. Accessed April 6th. [DOI] [PubMed] [Google Scholar]
- Moro F., Buonsenso D., Moruzzi M.C., Inchingolo R., Smargiassi A., Demi L., Larici A.R., Scambia G., Lanzone A., Testa A.C. How to perform lung ultrasound in pregnant women with suspected COVID-19 infection. Ultrasound Obstet Gynecol. 2020 doi: 10.1002/uog.22028. [e-pub ahead of print], Accessed April 6th. [DOI] [PubMed] [Google Scholar]
- Musolino A.M., Tomà P., Supino M.C., Scialanga B., Mesturino A., Scateni S., Battaglia M., Pirozzi N., Bock C., Buonsenso D. Lung ultrasound features of children with complicated and noncomplicated community acquired pneumonia: A prospective study. Pediatr Pulmonol. 2019;54:1479–1486. doi: 10.1002/ppul.24426. [DOI] [PubMed] [Google Scholar]
- Musolino A.M., Tomà P., Supino M.C., Scialanga B., Mesturino A., Scateni S., Battaglia M., Pirozzi N., Bock C., Buonsenso D. Lung ultrasound features of children with complicated and noncomplicated community acquired pneumonia: A prospective study. Pediatr Pulmonol. 2019;54:1479–1486. doi: 10.1002/ppul.24426. [DOI] [PubMed] [Google Scholar]
- Peng Q.Y., Wang X.T., Zhang L.N. Chinese Critical Care Ultrasound Study Group (CCUSG). Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med. 2020 doi: 10.1007/s00134-020-05996-6. [e-pub ahead of print], Accessed April 5th. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereda M.A., Chavez M.A., Hooper-Miele C.C., Gilman R.H., Steinhoff M.C., Ellington L.E., Gross M., Price C., Tielsch J.M., Checkley W. Lung ultrasound for the diagnosis of pneumonia in children: A meta-analysis. Pediatrics. 2015;135:714–722. doi: 10.1542/peds.2014-2833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu H., Wu J., Hong L., Luo Y., Song Q. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: An observational cohort study. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30198-5. [e-pub ahead of print], Accessed April 2nd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin G.D., Ryerson C.J., Haramati L.B., Sverzellati N., Kanne J.P., Raoof S., Schluger N.W., Volpi A., Yim J.J., Martin I.B.K., Anderson D.J., Kong C., Altes T., Bush A., Desai S.R., Goldin J., Goo J.M., Humbert M., Inoue Y., Kauczor H.U., Luo F., Mazzone P.J., Prokop M., Remy-Jardin M., Richeldi L., Schaefer-Prokop C.M., Tomiyama N., Wells A.U., Leung A.N. The role of chest imaging in patient management during the COVID-19 pandemic: A multinational consensus statement from the Fleischner Society. Radiology. 2020 doi: 10.1148/radiol.2020201365. [e-pub ahead of print], Accessed April 3rd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith M.J., Hayward S.A., Innes S.M., Miller A. Point-of-care lung ultrasound in patients with COVID-19—A narrative review [e-pub ahead of print] Anaesthesia. 2020 doi: 10.1111/anae.15082. Accessed March 31st. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soldati G., Smargiassi A., Inchingolo R., Buonsenso D., Perrone T., Briganti D.F., Perlini S., Torri E., Mariani A., Mossolani E.E., Tursi F., Mento F., Demi L. Proposal for international standardization of the use of lung ultrasound for COVID-19 patients: A simple, quantitative, reproducible method. J Ultrasound Med. 2020 doi: 10.1002/jum.15285. [e-pub ahead of print], Accessed March 31st. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soldati G., Smargiassi A., Inchingolo R., Buonsenso D., Perrone T., Briganti D.F., Perlini S., Torri E., Mariani A., Mossolani E.E., Tursi F., Mento F., Demi L. Is there a role for lung ultrasound during the COVID-19 pandemic? J Ultrasound Med. 2020 doi: 10.1002/jum.15284. [e-pub ahead of print], Accessed March 31st. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Supino M.C., Buonsenso D., Scateni S., Scialanga B., Mesturino M.A., Bock C., Chiaretti A., Giglioni E., Reale A., Musolino A.M. Point-of-care lung ultrasound in infants with bronchiolitis in the pediatric emergency department: A prospective study. Eur J Pediatr. 2019;178:623–632. doi: 10.1007/s00431-019-03335-6. [DOI] [PubMed] [Google Scholar]
- Tagarro A., Epalza C., Santos M., Sanz-Santaeufemia F.J., Otheo E., Moraleda C., Calvo C. Screening and severity of coronavirus disease 2019 (COVID-19) in children in Madrid, Spain [e-pub ahead of print] JAMA Pediatr. 2020 doi: 10.1001/jamapediatrics.2020.1346. Accessed April 5th. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W., Xu Y., Gao R., Lu R., Han K., Wu G., Tan W. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA. 2020 doi: 10.1001/jama.2020.3786. Accessed April 5th. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W., China Novel Coronavirus Investigating and Research Team A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]