The potential interplay between severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) infection and treatment with immune-checkpoint inhibitors (ICIs) of patients with cancer is presently unknown [1]. In this context, the increasing spreading of the coronavirus (COVID-19) pandemic does not help; in fact, major health resources are being redirected to counteract the pandemic [2], raising the concrete risk to hamper cancer care significantly [3]. As a result, the COVID-19 status of patients with cancer is generally not evaluated at the beginning and/or in the course of their medical treatment. In addition, the vast majority of patients with cancer receive therapy on an out-patients basis; thus, asymptomatic COVID-19 positive patients are generally free to access the Oncology Units, representing a major challenge for the possible transmission of SARS-CoV-2 to hospital personnel. On the other hand, these very same patients are challenged with the potential risk that ICI therapy may exacerbate the clinical course of their COVID-19 infection and/or that COVID-19 infection may worsen ICI-related side effects. In this composite and potentially cross-interfering scenario, sharing with the oncology community initial observations, even on a limited number of cases, may support treating physicians in their daily practice.
On March 6, an asymptomatic, 74-years-old male, Eastern Cooperative Oncology Group (ECOG) PS0, who was diagnosed with a metastatic cutaneous melanoma on November 2015 (patient 1), accessed our outpatient clinic with normal clinical and bio-humoural parameters to receive his 83rd cycle of an anti–PD-1 monoclonal antibody (mAb), being in partial objective response since June 2016. Worth mentioning, he had undergone right nephrectomy for a pT1N0M0 renal cell carcinoma on February 2016, and on October 2019 he had received a gastric wedge resection for a low-risk GIST. On March 16, the patient was admitted to the emergency room at a different hospital with a 4 days history of fever >38.0 °C, mild dyspnoea and cough and oxygen saturation of 94%. Routine nasopharyngeal and oropharyngeal swabs revealed SARS-CoV-2 infection, and the patient was therefore hospitalized (Fig. 1 ). Computed tomography (CT) scans revealed a bilateral pneumonitis, and laboratory tests were compatible with COVID-19 infection (Fig. 1) [4,5]. The local protocol for COVID-19 infection was activated, and the patient was treated with oral azothromycin, darunavir/ritonavir, hydroxychloroquine and oxygen therapy. On March 24, lymphocyte count reached the nadir (i.e., 650 × 10−9U/L), and on April 2, the patient was discharged being asymptomatic, with normal blood values, and with two subsequent swabs testing negative for SARS-CoV-2 infection (Fig. 1). Being cured from COVID-19 infection ICI therapy will be reactivated.
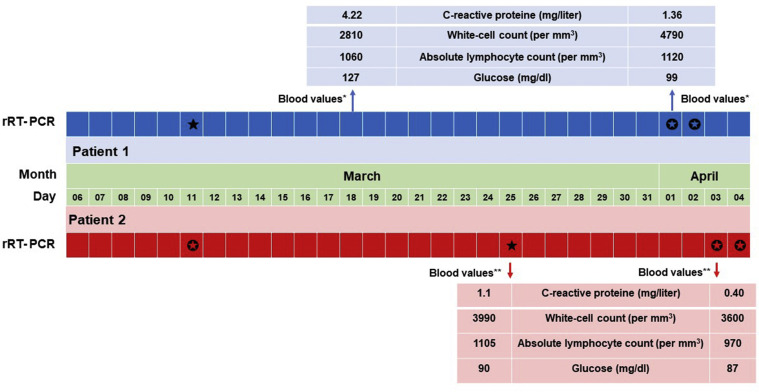
Fig. 1.
COVID-19 assessments and bio-humoural parameters of treated patients. SARS-CoV-2 infection was assessed by real-time reverse transcriptase-polymerase chain reaction (rRT-PCR) testing positive (★) or negative (✪). Reference laboratory values for patient 1∗(C-reactive protein <1.00; WBC: 4.000–10.000: ALC: 900–4500 and glucose: 70–110) and patient 2∗∗ (C-reactive protein 0.00–5.00; WBC: 4.000–11.000: ALC: 1000–3700 and glucose: 70–110).
On March 18, an asymptomatic, 51-years-old female, ECOG PS0, receiving adjuvant therapy for a locally advanced cutaneous melanoma surgically removed on July 2019 (patient 2), was admitted to our outpatient clinic with normal clinical and bio-humoural parameters to receive her 11th cycle of an anti–PD-1 mAb. Noteworthy, being the patient an MD, she had tested negative for SARS-CoV-2 infection on March 11 following a professional exposure to COVID-19. On March 19, the patient called our clinic referring asthenia, nausea, fever >38.0 °C, headache and oxygen saturation of 98%. Owing to the persistence of the clinical symptoms, on March 25 nasopharyngeal and oropharyngeal swabs were performed, confirming SARS-CoV-2 infection (Fig. 1). Owing to the mildness of referred symptoms, and in accordance with the local protocol, the patient did not receive treatment for COVID-19 infection and was quarantined at home. On March 30, she referred improvement of clinical symptoms, while bio-humoural parameters normalized on April 3 (Fig. 1). Two subsequent swabs tested negative on April 3 and 4 for SARS-CoV-2 infection (Fig. 1); thus, the patient was considered cured from COVID-19 and she will resume ICI therapy shortly.
These two cases are representative of potential clinical scenarios with whom oncologists can be faced in their daily practice due to the COVID-19 pandemic. Undoubtedly, no general conclusion can be drawn from the positive outcome of these two patients on the reciprocal interplay between ICI therapy and SARS-CoV-2 infection. Nevertheless, these findings seem to suggest that treatment with ICI is a doable approach during the COVID-19 pandemic, and that SARS-CoV-2 infection does not seem to represent an obstacle to grant patients with cancer the best treatment in accordance with their clinical setting.
Funding
This work was supported in part by funding from the FONDAZIONE AIRC under 5 per Mille 2018 – ID 21073 program (principal investigator M. Maio).
Conflict of interest statement
A.M.D.G. has served as consultant and/or advisor to Incyte, Pierre Fabre, Merck Sharp Dohme; Sanofi, Glaxo Smith Kline and Bristol-Myers Squibb. M.M. has served as consultant and/or advisor to Roche, Bristol-Myers Squibb, Merck Sharp Dohme, Incyte, Astra Zeneca, Glaxo Smith Kline and Merck Serono. E.G., S.M. and M.V. declare no conflicts of interest.
References
- 1.Calabrò L., Peters S., Soria J.C., et al. Challenges in lung cancer therapy during the COVID-19 pandemic. Lancet Resp Med. 2020 doi: 10.1016/S2213-2600(20)30170-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Emanuel E.J., Persad G., Upshur R., et al. Fair allocation of scarce medical resources in the time of covid-19. N Engl J Med. 2020 doi: 10.1056/NEJMsb2005114. [DOI] [PubMed] [Google Scholar]
- 3.Ueda M., Martins R., Hendrie P.C., et al. Managing cancer care during the COVID-19 pandemic: agility and collaboration toward a common goal. J Natl Canc Netw. 2020;20:1–4. doi: 10.6004/jnccn.2020.7560. [DOI] [PubMed] [Google Scholar]
- 4.Zhu N., Zhang D., Wang W., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen N., Zhou M., Dong X., et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]