Abstract
INTRODUCTION
Telemedicine can improve access to emergency stroke care in rural areas, but the benefit of telemedicine across different types and models of telemedicine networks is unknown. The objectives of this study were to (1) identify the impact of telemedicine on ED stroke care, (2) identify if telemedicine impact varied by network, and (3) describe the variation in process outcomes by telemedicine across EDs.
METHODS
A prospective cohort study identified stroke patients in four telemedicine networks between November 2015 and December 2017. Primary exposure was telemedicine consultation during ED evaluation. Outcomes included: (1) head CT interpretation within 45 minutes and (2) time-to-tPA administration. An interaction term tested for differences in telemedicine effect on stroke care by network and hospital.
RESULTS
Of the 932 stroke subjects, 36% received telemedicine consults. For subjects with a last known well time within two hours of ED arrival (27.9%), recommended CT interpretation within 45 minutes was met for 66.8%. Telemedicine was associated with higher odds of timely head CT interpretation (aOR: 3.03 [95%CI: 1.69 – 5.46]). The magnitude of the association between telemedicine and time-to-head CT interpretation differed between telemedicine networks (interaction term p=0.033). Among eligible patients, telemedicine was associated with faster time to tPA administration (aHR: 1.81. [95%CI: 1.31 – 2.50]).
DISCUSSION
Telemedicine consultation during the ED encounter decreased time-to-head CT interpretation among stroke patients, with differing magnitudes of benefit across telemedicine networks. The effect of heterogeneity of tele-stroke affects across different networks should be explored in future analyses.
INTRODUCTION
Stroke affects approximately 795,000 people each year in the United States and is the leading cause of serious long-term disability, with approximately 2% of all adults reporting disability due to stroke.1, 2 For acute ischemic stroke, timely intravenous thrombolytic therapy is an effective treatment to decrease long-term disability. Administration of tissue plasminogen activator (tPA) within 3 hours of symptom onset has been shown to improve clinical outcomes and reduce the burden of stroke symptoms.3, 4 Health care delivery strategies, such as regionalization of emergency care and development of Primary Stroke Centers, have increased rates of tPA administration and decreased time to tPA administration.5–7 This evidence has led to using time to tPA and diagnostic imaging as acute stroke care quality indicators for emergency department (ED) and inpatient performance in Primary Stroke Centers.8, 9
However, there is wide variation in timely tPA administration rates across geography.10 Rural-urban disparities in stroke care are especially concerning because (1) stroke incidence is higher in rural compared to urban areas of the United States and (2) rural hospitals have lower tPA utilization and worse time metrics.11–13 Further, 34% of Americans, who are primarily rural residents, do not have access to a Primary Stroke Center within one hour of their residence.14
Telemedicine networks that are designed to provide real-time emergency care consultation between a central hub and a remote hospital via phone or two-way audio/visual communication have improved access to high-quality stroke care.15, 16 Over the past decade, telemedicine-guided acute ischemic stroke care has been shown to be accurate, safe, and produce comparable favorable clinical outcomes compared to traditional on-site care.17–22 There is also growing evidence that telemedicine is effective in improving the rate and timeliness of tPA administration.23–26
While telemedicine models have been broadly used in ED stroke care, most prior studies have been limited in scope to a single network.15, 17–26 In order to better characterize the overall impact of telemedicine, we studied emergency stroke care in four telemedicine networks. The objectives of this study were to (1) identify the overall impact of telemedicine on ED stroke care measures of time to head computed tomography (CT) interpretation and tPA administration, (2) identify if the impact of telemedicine varied by network, and (3) describe the variation in these process outcomes by telemedicine across EDs.
METHODS
Study Design, Setting, and Participants
This is a prospective cohort study of stroke patients in EDs participating in one of four telemedicine networks. Each network received funding from the Health Resources & Services Administration (HRSA), Federal Office of Rural Health Policy (FORHP) through the Evidence-Based Tele-Emergency Network Grant Program (EB TNGP) to implement and evaluate ED-based telehealth consultation services. In addition, each network prospectively collected data in all participating EDs using the Tele-Emergency Performance Assessment Reporting Tool (T-PART), which has been reported previously.27 All networks are hub-and-spoke models that provide high-definition video, provider-to-provider telemedicine services to EDs in one to thirteen community hospitals. Two networks offer dedicated tele-stroke services with specialized neurology consults, and two telemedicine networks provide comprehensive emergency telemedicine with available specialty consultation (including neurology, trauma, critical care, mental health, and pediatrics). Telemedicine was available for all stroke patients across the four networks, and in all networks, a local emergency provider had to request telemedicine consultation for each case. Networks varied in the number of spoke hospitals(range: one to 14 spoke hospitals). In the networks providing general telemedicine, over 80% of the hospitals are Critical Access Hospitals (CAHs).28 In the networks providing specialized telemedicine, 50% of hospitals are CAHs.28 Spoke hospitals are primarily located in Western, Midwestern, and Eastern regions of the U.S.
All stroke patients (including telemedicine and non-telemedicine patients) presenting to participating EDs between November 2015 and December 2017 were eligible for the study. Stroke was identified by a presenting ED complaint of stroke symptoms and/or an ICD-10-CM diagnosis code related to stroke (i.e. I60, I61, I63). Data were abstracted from the electronic medical record using a standardized Microsoft Excel (Microsoft Corporation, Redmond, WA)-based electronic data abstraction form using a standard set of defined measures by each telemedicine network. This study is reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.29 This study was approved by Institutional Review Boards at the data coordinating and analysis center and each network hub institution.
Variables
The primary exposure was defined as telemedicine consultation during the ED visit. Telemedicine consultation was defined as having a synchronous audio-visual interaction with the hub site, which includes an ED physician or other consulting provider (e.g. neurologist, hospitalist, etc.). Visits that were not considered successful due to technology failures (n=2) were excluded. The primary outcome was time to head CT interpretation (in minutes). This was defined as the time from ED arrival to the time when the earliest head CT interpretation was completed or reported. This time represents the time to preliminary read, or if no preliminary read was rendered, this is the time to final read. All CT’s were interpreted by staff radiologists. Secondary outcomes included time to tPA administration, and two accepted stroke quality of care metrics: (1) head CT or MRI scan results interpretation for acute stroke within 45 minutes of ED arrival (Centers for Medicare & Medicaid Services (CMS) National Quality Forum (NQF) ID# 0661); and (2) tPA initiation within three hours of time last known well for patients presenting to ED within two hours of last known well (Joint Commission Stroke-4 (STK-4)).8, 9 Time from last known well, or estimated stroke onset, was defined as time prior to hospital arrival that the patient was last free from the signs and symptoms of the current stroke or at the subject’s baseline status of health. Time to tPA administration was only assessed for subjects meeting eligibility criteria for tPA, defined as: (1) did not have cardiac arrest, respiratory arrest, cardiopulmonary resuscitation, defibrillation, or ED intubation; (2) were not “Comfort Measures Only” and did not have subject/family refusal of tPA; (3) documentation of a National Institutes of Health Stroke Scale of greater than zero in the ED; (4) physician determined subject needed tPA; and (5) no other tPA contraindication.
Characteristics of the subjects and the ED encounter were measured including age (25–44, 45–64, 65–74, or 75 or more years), sex, race (White, Black/African American, or Other), ethnicity (Hispanic/Latinx), and primary payer (Dual Medicare/Medicaid, Medicare only, Medicaid only, Private Insurance, Self-Pay/Uninsured, and other). Emergency Severity Index (ESI: Resuscitation, Emergent, Urgent, Less Urgent, Non-urgent, and Missing) was used as a proxy for severity of illness.30 ESI is a systematic algorithm used by trained ED triage nurses to quantify patient severity on ED arrival and is based on perceived risk of death, urgency, anticipated resource need, and vital signs.30 Arrival time was dichotomized as business hours (07:30 to 17:30) or non-business hours (all other hours). ED arrival day of the week (i.e. Sunday to Saturday) was recorded. Reason for visit was abstracted from the recorded ED “Chief Complaint,” or primary reason reported for ED visit upon ED arrival.
Statistical Methods
Descriptive statistics are reported for cohort characteristics by telemedicine consultation status. Differences in characteristics by telemedicine consultation were assessed using chi-square and Fisher’s exact tests, based on expected cell frequencies. For the primary outcomes, differences in time to head CT interpretation and time to tPA administration, univariate Cox proportional hazard models were constructed with the proportional hazards assumption tested and upheld using the Schoenfeld residuals test. Covariate selection was informed by clinical practice patterns and previous literature and added to a multivariable model, with Akaike Information Criteria (AIC) used to determine the most parsimonious model. Expected survival curves after adjustment were constructed to visualize the association between telemedicine and time to tPA and head CT interpretation. Similar modelling techniques utilizing generalized estimating equations (binomial distribution with logit link) were used for the secondary outcomes of CT interpretation within 45 minutes of arrival and tPA administration within three hours of last known well.
It was hypothesized that observations may violate the assumption of independence due to similarities in practice patterns within hospitals or telemedicine networks, so standard errors were initially clustered. After using AIC to compare models clustering at the hospital and network levels, standard errors were clustered at the hospital level for all models. Hospital- and network-level random effects were tested in frailty models. However, the multi-level frailty model incorporating hospital- and network-level clustering failed to converge, so the effects of hospital-level and network-level random effects were evaluated in separate frailty models. Partial log likelihood ratio tests were used to determine if the random effects were significant compared to a model without random effects.
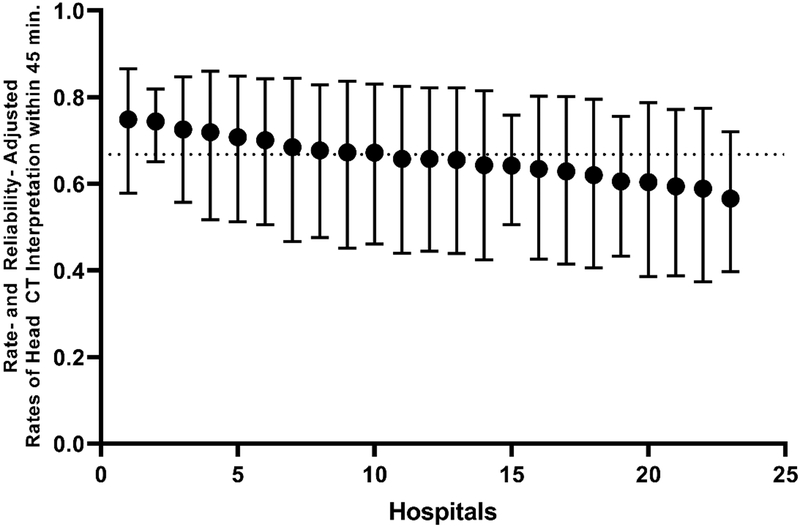
To estimate variation in the impact of telemedicine across hospitals and networks, the rate of head CT interpretation completed within 45 minutes of ED arrival was calculated for each hospital. Head CT interpretation within 45 minutes of ED arrival is an established quality target for stroke patients presenting to the ED within two hours of time last known well.1 Risk and reliability-adjusted estimates of rates of head CT interpretation by hospital rank were reported in a caterpillar plot for telemedicine and non-telemedicine consults.31 Risk adjustment was performed using age, ESI, race, and payer as fixed effects with hospital as a random effect in a multilevel logistic regression. An empirical Bayes estimate of the random effect for each hospital was used to calculate the hospital-specific reliability-adjusted rate of head CT interpretation compliance.31 All analyses were conducted with complete cases, excluding missing data (unless Missing category noted in variable definition). Statistical analyses were conducted in STATA (StataCorp LP, College Station, Texas) and R (RStudio Inc., Vienna, Austria).
RESULTS
Description of Study Cohort
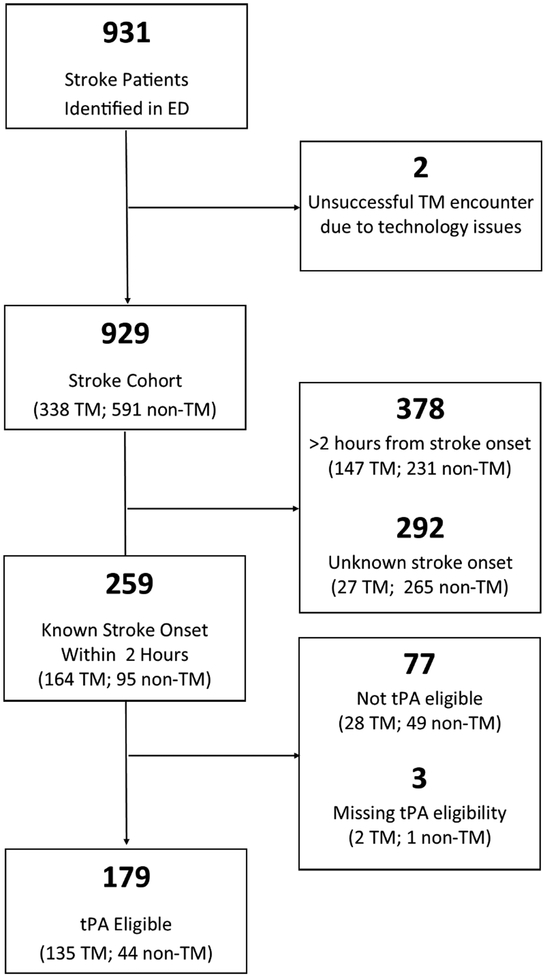
Overall, 931 stroke subjects were identified (Figure 1), 338 of which received telemedicine. Two subjects were excluded due to technology issues during the telemedicine encounter leading to unsuccessful consultations. In the study cohort the plurality of subjects were older than 75 years (47.6%), white (91.9%), Medicare beneficiaries (65.1%), and emergent severity (ESI = 2) upon ED admission (56.5%) (Table 1).
Figure 1.
Flow chart of study subjects.
Table 1.
Characteristics of Study Subjects by Telemedicine Consult Status.
| Total | No Telemedicine Use | Telemedicine Use | p-value | ||
|---|---|---|---|---|---|
| N=929 | N=591 | N=338 | |||
| Patient age | 25–44 | 30 (3.2%) | 10 (1.7%) | 20 (5.9%) | <0.001 |
| 45–64 | 260 (28.0%) | 153 (25.9%) | 107 (31.7%) | ||
| 65–74 | 197 (21.2%) | 115 (19.5%) | 82 (24.3%) | ||
| 75 or older | 442 (47.6%) | 313 (53.0%) | 129 (38.2%) | ||
| Patient sex | Female | 487 (52.4%) | 312 (52.8%) | 175 (51.8%) | 0.770 |
| Male | 442 (47.6%) | 279 (47.2%) | 163 (48.2%) | ||
| Patient race | American Indian/Alaska Native | 14 (1.5%) | 11 (1.9%) | 3 (0.9%) | <0.001 |
| Asian | 3 (0.3%) | 2 (0.3%) | 1 (0.3%) | ||
| Black/African American | 40 (4.3%) | 32 (5.4%) | 8 (2.4%) | ||
| Unknown | 18 (1.9%) | 2 (0.3%) | 16 (4.7%) | ||
| White | 854 (91.9%) | 544 (92.0%) | 310 (91.7%) | ||
| Patient ethnicity | Hispanic/Latinx | 3 (0.3%) | 1 (0.2%) | 2 (0.6%) | <0.001 |
| Not Hispanic/Latinx | 809 (87.1%) | 579 (98.0%) | 230 (68.0%) | ||
| Unknown | 117 (12.6%) | 11 (1.9%) | 106 (31.4%) | ||
| Primary payer - recoded data | Medicare only | 605 (65.1%) | 423 (71.6%) | 182 (53.8%) | <0.001 |
| Private Insurance | 179 (19.3%) | 91 (15.4%) | 88 (26.0%) | ||
| Dual Medicare/Medicaid | 44 (4.7%) | 23 (3.9%) | 21 (6.2%) | ||
| Medicaid only | 41 (4.4%) | 16 (2.7%) | 25 (7.4%) | ||
| Self-pay/uninsured | 40 (4.3%) | 25 (4.2%) | 15 (4.4%) | ||
| Other | 20 (2.2%) | 13 (2.2%) | 7 (2.1%) | ||
| ED Arrival time | Bus. hrs (0730–1730) | 616 (66.3%) | 432 (73.1%) | 184 (54.4%) | <0.001 |
| Not bus. hrs | 313 (33.7%) | 159 (26.9%) | 154 (45.6%) | ||
| ED visit arrival day of work | Monday | 136 (14.6%) | 91 (15.4%) | 45 (13.3%) | 0.061 |
| Tuesday | 134 (14.4%) | 80 (13.5%) | 54 (16.0%) | ||
| Wednesday | 135 (14.5%) | 98 (16.6%) | 37 (10.9%) | ||
| Thursday | 148 (15.9%) | 98 (16.6%) | 50 (14.8%) | ||
| Friday | 131 (14.1%) | 84 (14.2%) | 47 (13.9%) | ||
| Saturday | 104 (11.2%) | 63 (10.7%) | 41 (12.1%) | ||
| Sunday | 141 (15.2%) | 77 (13.0%) | 64 (18.9%) | ||
| Emergency severity index | 1-Resuscitation | 66 (7.1%) | 32 (5.4%) | 34 (10.1%) | <0.001 |
| 2-Emergent | 525 (56.5%) | 297 (50.3%) | 228 (67.5%) | ||
| 3-Urgent | 167 (18.0%) | 122 (20.6%) | 45 (13.3%) | ||
| 4-Less urgent | 10 (1.1%) | 7 (1.2%) | 3 (0.9%) | ||
| 5-Non-urgent | 1 (0.1%) | 0 (0.0%) | 1 (0.3%) | ||
| Unknown | 160 (17.2%) | 133 (22.5%) | 27 (8.0%) | ||
| Time from last known well to ED arrival (minutes) | 1 Missing | 292 (31.4%) | 265 (44.8%) | 27 (8.0%) | <0.001 |
| 2 <=60 min | 155 (16.7%) | 55 (9.3%) | 100 (29.6%) | ||
| 3 61–120 min | 104 (11.2%) | 40 (6.8%) | 64 (18.9%) | ||
| 4 121–360 min | 149 (16.0%) | 77 (13.0%) | 72 (21.3%) | ||
| 5 >360 min | 229 (24.7%) | 154 (26.1%) | 75 (22.2%) |
Effect of Telemedicine on Stroke Process Measures
Time to Head CT Interpretation.
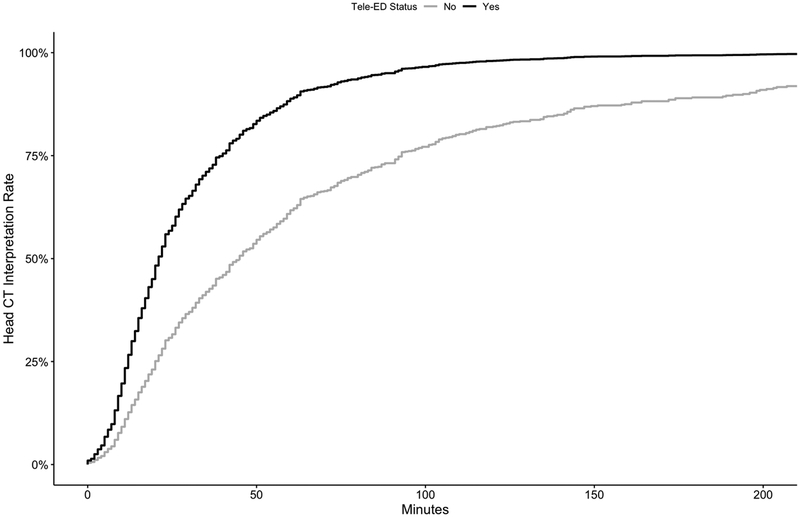
Subjects receiving telemedicine had shorter time to head CT interpretation compared to subjects that did not have telemedicine consults in the ED (median: telemedicine 33 minutes [95%CI: 31 – 37 minutes] vs. non-telemedicine 67 minutes [62 – 73 minutes], p<0.001) (Figure 2). After adjusting for primary expected payer, race, emergency severity index, and ED visit arrival day (i.e. day of week), telemedicine subjects continued to have a shorter time to head CT interpretation (aHR: 2.35 [95%CI: 1.96 – 2.83], p<0.001).
Figure 2.
Time to interpret head CT by telemedicine consult status. Curves are adjusted for model covariates (race, ethnicity, payer and ESI) and represent the average of individual survival curves. TM: telemedicine; CT: computed tomography; ESI: Emergency Severity Index.
Head CT Interpretation within 45 Minutes.
For subjects with a time last known well within two hours of ED arrival (n=259, 27.9%), the CT interpretation within 45 minutes benchmark was met for 66.8% of subjects. Subjects receiving telemedicine consult were more likely to have their head CT interpreted within 45 minutes compared to subjects that did not receive telemedicine consult (73.3% vs. 55.3%, p = 0.005). In an adjusted analysis, subjects receiving telemedicine had higher odds of head CT interpretation within 45 minutes compared to those that did not receive telemedicine consults (aOR: 3.03 [95%CI: 1.69 – 5.46], p<0.001) (Table 2).
Table 2.
Unadjusted and Adjusted Measures of Association between Telemedicine and Stroke Outcomes.
| Outcome | N | Unadj. | 95%CI | p-value | Adj.* | 95%CI | p-value | ||
|---|---|---|---|---|---|---|---|---|---|
| Time to Head CT Interpretation (HR) | 929 | 2.50 | 2.05 | 3.04 | <0.001 | 2.35 | 1.96 | 2.83 | <0.001 |
| Head CT Interpretation within 45 Minutes (OR) | 259 | 1.86 | 1.16 | 2.97 | 0.010 | 3.03 | 1.69 | 5.46 | <0.001 |
| Time to tPA Administration (HR) | 179 | 1.03 | 0.45 | 2.32 | 0.950 | 1.81 | 1.31 | 2.50 | <0.001 |
| tPA within Three Hours (OR)# | 179 | 1.45 | 0.43 | 4.87 | 0.550 | 2.13 | 0.55 | 8.24 | 0.271 |
Adjusted for race, ethnicity, Emergency Severity Index, and payer.
Adjusted for race, Emergency Severity Index, and payer.
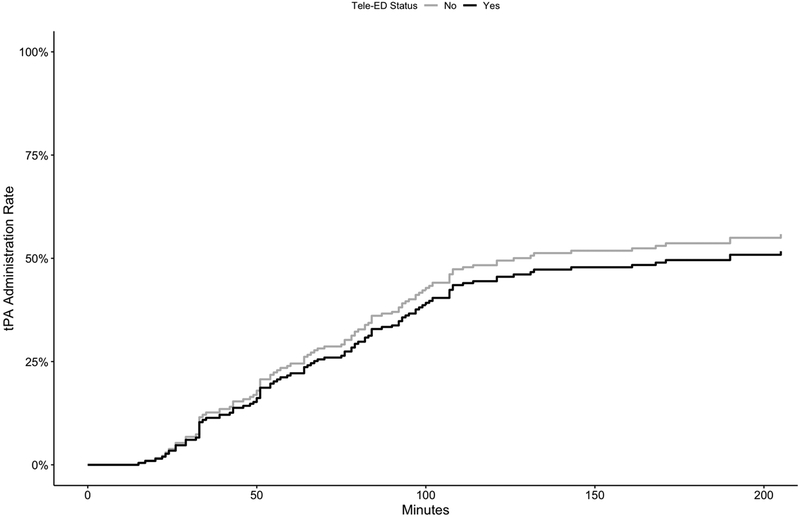
Time to tPA Administration.
Of the 929 study subjects, 346 (37.2%) were eligible for tPA. Among the tPA-eligible subjects, 103 subjects (29.8%) received tPA during the ED stay. Telemedicine consult patients were more likely to receive tPA, when eligible, compared to those without telemedicine consults. There was no difference in time to tPA administration between tPA-eligible subjects receiving telemedicine consults and those without telemedicine consults (Figure 3, p=0.400). After adjustment for the factors listed above, there was an increased hazard of tPA administration in subjects with telemedicine consults compared to no telemedicine consults (aHR: 1.81 [95%CI: 1.31 – 2.50], p< 0.001) (Table 2).
Figure 3.
Time to administer tPA by telemedicine consult status. Curves are adjusted for model covariates (race, ethnicity, payer and ESI) and represent the average of individual survival curves. tPA: tissue plasminogen activator.
tPA within Three Hours of Last Known Well.
Of the 259 subjects with a time last known well within two hours, one had an unknown tPA time and 79 were not eligible for tPA; these were excluded from analysis for this outcome. There was no difference in the proportion of subjects receiving tPA within three hours between the subjects that did and those that did not receive telemedicine consults (50.0% vs. 52.3%, p=0.900). Likewise, after adjustment for the factors listed above, telemedicine consultation in the ED was not associated with a higher odds of receiving tPA within three hours of last known well compared to those that did not receive telemedicine consults (aOR: 2.13 [95%CI: 0.55 – 8.24], p= 0.271) (Table 2).
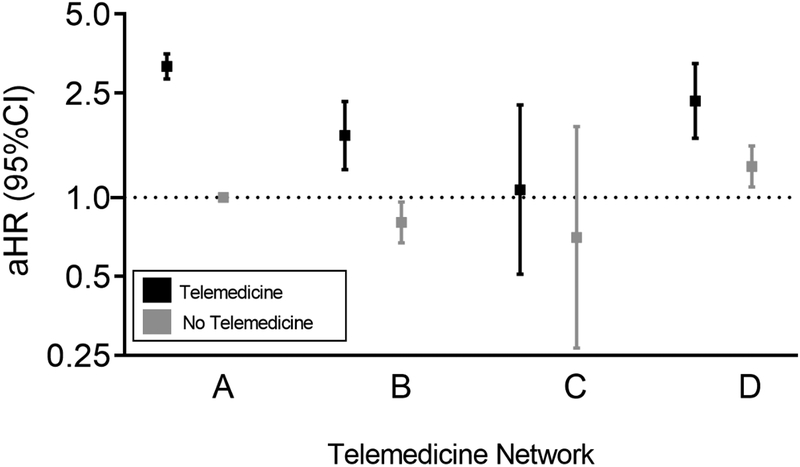
Variation of Process Outcomes among Networks and Emergency Departments
Variation in the effects of telemedicine for head CT interpretation at the network and hospital levels were measured using interaction terms and rate- and reliability-adjusted rates, respectively. The magnitude of the association between telemedicine and time to head CT interpretation was different between telemedicine networks (interaction term p=0.033). Telemedicine was associated with shorter time to head CT interpretation in three networks, but the magnitude of effect varied by network (Figure 4). The association between telemedicine and time to tPA was similar among telemedicine networks (interaction term p=0.260). On average, 66.8% of cases were adherent with recommendations for Head CT Interpretation within 45 minutes of ED arrival for subjects with time last known well within two hours of ED arrival. There was little variation among hospitals after risk adjustment for case severity and reliability adjustment due to small numbers of cases in some EDs (Figure 5). The average facility adherence rate with head CT interpretation within 45 minutes for subjects with last known well within two hours of ED arrival was 65.9% (CI 63.8% to 67.6%).
Figure 4.
Effect of telemedicine on time to interpret head CT by network. Hazard ratio >1 indicates a significantly shorter time to interpret head CT.
Figure 5.
Variation in spoke hospital time to interpret head CT by telemedicine status. Spoke hospitals are rank ordered.
DISCUSSION
This is the first evaluation of telemedicine benefit for acute stroke care across different telemedicine networks. In this multi-network study, telemedicine consultation was associated with shorter time to head CT interpretation, as well as increased adherence to existing quality measures for head CT interpretation. Telemedicine subjects were more likely to receive tPA when eligible, and telemedicine consultation was associated with decreased time to tPA administration.
Findings of positive effects of telemedicine improving process outcomes in emergency stroke care are consistent with previous studies that have documented an association between telemedicine and increased tPA use, as well as decreased time to head CT interpretation.23–26, 32 These findings support the value of telemedicine in changing care processes and improving quality for rural stroke care. There is conflicting evidence as to whether telemedicine has an impact on the timely administration of tPA in ED stroke care due to heterogeneity of study groups.23, 24, 33, 34 While this study found telemedicine led to a decrease in time to tPA administration, there was no effect on adherence to the stroke quality measure STK-4, which is important for hospital reimbursement and certification of Primary Stroke Centers. This could indicate that telemedicine decreases overall time to tPA but does not affect ED stroke patients on the margins of receiving tPA in the first three hours of time last known well: the current guideline definition of the critical window. Alternatively, emergency clinicians could be selecting to use telemedicine for patients most likely to need rapid interventions, such as “drip and ship” tPA, immediately before inter-hospital transfer. However, this is likely not driving study findings as there was no difference in ED disposition by telemedicine use in tPA-eligible subjects in this cohort. As presentation at a rural, non-stroke center hospital in one of the geographic regions of this study (i.e. Eastern and Midwest) is a risk factor for not receiving tPA,35 addressing a combination of telemedicine availability and subsequent patient selection for telemedicine consultation will be an important consideration for future programs and research aiming to reduce rural-urban stroke treatment disparities.
This study provides novel insight about the likely impact of telemedicine on emergency stroke care as telemedicine initiatives are scaled across hospitals and regions. While previous single-center and single-network studies have indicated that telemedicine improves process outcomes in stroke care,17, 21, 23, 24, 26, 32, 34 this is the first study of multiple telemedicine networks. The multi-center design improves external generalizability and increases confidence in the reporting of the sole effect of a telemedicine program rather than a combination of telemedicine and other local quality improvement initiatives. The findings of telemedicine benefit across networks suggest that the positive effects of telemedicine on stroke quality of care indicators can be realized in settings with a variety of hospital and network characteristics. Our results indicate that telemedicine networks are a scalable intervention that may provide more equitable treatment to communities across the United States. Further, telemedicine may be an available resource to improve existing quality of care metrics for stroke care for smaller volume, non-stroke center EDs.
While telemedicine was beneficial for decreasing time to stroke care, the magnitude of telemedicine benefit varied by network for head CT interpretation timeliness. While no difference was observed in time to tPA, this may be an artifact of a small sample size of tPA-eligible subjects. The observed variation in effect across telemedicine networks is a very interesting finding. Networks function very differently in their use for non-stroke cases, staffing models, and participation in ongoing facility-level quality improvement activities. This analysis highlights how, although consistent benefit was observed, the magnitude of that benefit is not uniform. Due to the small number of networks in this study, we were not able to determine which network characteristics were associated with increased timeliness of head CT interpretation. While much prior work has sought to evaluate the “utility” of telemedicine overall, researchers and policy makers must recognize that telemedicine implementation is heterogenous and that high-functioning networks may have different outcomes than lower functioning networks.
There are several limitations to this study. First, data were collected prospectively from ED medical records. While this design allowed for a multi-network study, it also restricted the available measures of disease severity. A stroke-specific measure of disease severity on ED admission, such as the National Institutes of Health Stroke Scale,36 would be an ideal measure. As this was not available, the Emergency Severity Index was used as a proxy for severity of illness on ED arrival. This measure was highly associated with both telemedicine use and outcomes. Although information on the time of symptom onset was available, this variable was missing in some subjects and that missingness was differentially higher in the non-telemedicine group. This may indicate that recent stroke onset (and subsequent actionability of stroke management) may play a substantial role in the selection of which stroke patients receive ED telemedicine consults, as previously suggested.32 To limit the influence of selection bias on the observed effects, estimates were adjusted for severity of illness on ED presentation (ESI) and patient-level characteristics; however, residual bias in the reported estimates may remain due to selection of telemedicine subjects. Finally, this study was limited to data available during the ED encounter and does not include long-term clinical or functional outcomes. The impact of telemedicine on these patient- and policy-relevant outcomes remains an important question.
In conclusion, the use of telemedicine consultation improves process outcomes in emergency stroke care and adherence with quality of care indicators across different networks. This positive impact of telemedicine is likely generalizable across a variety of telemedicine settings, suggesting that the positive effects of telemedicine on ED stroke care are attainable in many ED settings and geographic regions. Telemedicine interventions for emergency stroke care are likely to be consistently beneficial but may have different magnitudes of effect based on the network’s implementation and management practices. Future work can focus on identifying telemedicine network characteristics associated with the greatest benefits in processes of care and evaluating effects on patient outcomes across networks.
Supplementary Material
ACKNOWLEDGEMENTS
The authors thank Amanda Bell (PI), Luke Mack, Amy Wittrock from Avera Health; Eric Pollard (PI), Martha Nikides from St. Vincent Healthcare; Stephanie Laws (PI), Hicham Rahmouni, Daniel Hardesty, Amanda O’Brien from Union Hospital; James Marcin (PI), Jamie Mouzoon from University of California-Davis; Roger Humphries (PI), Brian Dennis, Theresa Mims, Rob Sprang from University of Kentucky; and Nina Solenski (PI), Tracy Blount from University of Virginia for contributing data for these analyses.
FINANCIAL SUPPORT
This study was supported by the Federal Office of Rural Health Policy (FORHP), Health Resources and Services Administration (HRSA), U.S. Department of Health and Human Services (HHS) to the Rural Telehealth Research Center under cooperative agreement #UICRH29074. The Evidence-Based Tele-Emergency Network Grant Program provided funding for delivering teleED services to grantees - Avera Health (PI - Amanda Bell, Grant No. GO1RH27868), Saint Vincent Healthcare (PI - Eric Pollard, Grant No. G01RH27870), Union Hospital (PI - Stephanie Laws, Grant No. G01RH27871), University of California - Davis (PI - James Marcin, Grant No. G01RH27872), University of Kentucky (PI - Roger Humphries, Grant No. G01RH27873), and University of Virginia (PI - Nina Solenski, Grant No. G01RH27869). The information, conclusions, and opinions expressed are those of the authors and no endorsement by FORHP, HRSA, or HHS is intended or should be inferred. Dr. Mohr is additionally supported by grant K08 HS025753 from the Agency for Healthcare Research and Quality (AHRQ). The findings and conclusions are those of the author(s), who are responsible for its content, and do not necessarily represent the views of AHRQ.
Footnotes
DECLARATION OF CONFLICTS OF INTEREST
The Authors declare that there are no conflicts of interest.
Contributor Information
Morgan B. Swanson, Department of Emergency Medicine, Department of Epidemiology, Colleges of Medicine and Public Health, University of Iowa, Iowa City, IA.
Aspen C. Miller, Department of Emergency Medicine, University of Iowa, Iowa City, IA.
Marcia M. Ward, Department of Health Management and Policy, College of Public Health, University of Iowa, Iowa City, IA.
Fred Ullrich, Department of Health Management and Policy, College of Public Health, University of Iowa, Iowa City, IA.
Kimberly A. S. Merchant, Department of Health Management and Policy, College of Public Health, University of Iowa, Iowa City, IA.
Nicholas M. Mohr, Department of Emergency Medicine, Department of Anesthesia Division of Critical Care, Department of Epidemiology, Colleges of Medicine and Public Health, University of Iowa, Iowa City, IA.
REFERENCES
- 1.Benjamin EJ, Muntner P, Alonso A, et al. Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 2019; 139: e56–e528. 2019/02/01. DOI: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 2.Theis KA, Steinweg A, Helmick CG, et al. Which one? What kind? How many? Types, causes, and prevalence of disability among U.S. adults. Disabil Health J 2019. 2019/04/20. DOI: 10.1016/j.dhjo.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 3.National Institute of Neurological Disorders Stroke: Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995; 333: 1581–1587. 1995/12/14. DOI: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 4.Saver JL, Fonarow GC, Smith EE, et al. Time to treatment with intravenous tissue plasminogen activator and outcome from acute ischemic stroke. JAMA 2013; 309: 2480–2488. 2013/06/20. DOI: 10.1001/jama.2013.6959. [DOI] [PubMed] [Google Scholar]
- 5.Lackland DT, Roccella EJ, Deutsch AF, et al. Factors influencing the decline in stroke mortality: a statement from the American Heart Association/American Stroke Association. Stroke 2014; 45: 315–353. 2013/12/07. DOI: 10.1161/01.str.0000437068.30550.cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johnson AM, Goldstein LB, Bennett P, et al. Compliance with acute stroke care quality measures in hospitals with and without primary stroke center certification: the North Carolina Stroke Care Collaborative. J Am Heart Assoc 2014; 3: e000423. 2014/04/12. DOI: 10.1161/JAHA.113.000423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prabhakaran S, O’Neill K, Stein-Spencer L, et al. Prehospital triage to primary stroke centers and rate of stroke thrombolysis. JAMA Neurol 2013; 70: 1126–1132. 2013/07/03. DOI: 10.1001/jamaneurol.2013.293. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Medicare & Medicaid Services Joint Commission. Specifications manual for national hospital inpatient quality measures., https://www.jointcommission.org/specifications_manual_for_national_hospital_inpatient_quality_measures.aspx (2016).
- 9.National Quality Forum. ID 0661: Head CT or MRI Scan Results for Acute Ischemic Stroke or Hemorrhagic Stroke Patients who Received Head CT or MRI Scan Interpretation within 45 minutes of ED Arrival. In: Centers for Medicare & Medicaid Services, (ed.). 2018. [Google Scholar]
- 10.Gonzales S, Mullen MT, Skolarus L, et al. Progressive rural-urban disparity in acute stroke care. Neurology 2017; 88: 441–448. 2017/01/06. DOI: 10.1212/WNL.0000000000003562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Howard G, Kleindorfer DO, Cushman M, et al. Contributors to the Excess Stroke Mortality in Rural Areas in the United States. Stroke 2017; 48: 1773–1778. 2017/06/20. DOI: 10.1161/STROKEAHA.117.017089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seabury S, Bognar K, Xu Y, et al. Regional disparities in the quality of stroke care. Am J Emerg Med 2017; 35: 1234–1239. 2017/04/23. DOI: 10.1016/j.ajem.2017.03.046. [DOI] [PubMed] [Google Scholar]
- 13.Moscovice I and Rosenblatt R. Quality-of-care challenges for rural health. J Rural Health 2000; 16: 168–176. 2000/09/12. [DOI] [PubMed] [Google Scholar]
- 14.Mullen MT, Wiebe DJ, Bowman A, et al. Disparities in accessibility of certified primary stroke centers. Stroke 2014; 45: 3381–3388. 2014/10/11. DOI: 10.1161/STROKEAHA.114.006021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ward MM, Jaana M and Natafgi N. Systematic review of telemedicine applications in emergency rooms. Int J Med Inform 2015; 84: 601–616. 2015/06/15. DOI: 10.1016/j.ijmedinf.2015.05.009. [DOI] [PubMed] [Google Scholar]
- 16.Creating a Framework to Support Measure Development for Telehealth. 2017. National Quality Forum. [Google Scholar]
- 17.Baratloo A, Rahimpour L, Abushouk AI, et al. Effects of Telestroke on Thrombolysis Times and Outcomes: A Meta-analysis. Prehosp Emerg Care 2018; 22: 472–484. 2018/01/19. DOI: 10.1080/10903127.2017.1408728. [DOI] [PubMed] [Google Scholar]
- 18.Porter J, Hall RE, Kapral MK, et al. Outcomes following telestroke-assisted thrombolysis for stroke in Ontario, Canada. J Telemed Telecare 2018; 24: 492–499. 2017/07/12. DOI: 10.1177/1357633X17717601. [DOI] [PubMed] [Google Scholar]
- 19.Madhavan M and Karceski S. Telestroke: Is it safe and effective? Neurology 2016; 87: e145–148. 2016/09/28. DOI: 10.1212/WNL.0000000000003244. [DOI] [PubMed] [Google Scholar]
- 20.Kepplinger J, Barlinn K, Deckert S, et al. Safety and efficacy of thrombolysis in telestroke: A systematic review and meta-analysis. Neurology 2016; 87: 1344–1351. 2016/08/28. DOI: 10.1212/WNL.0000000000003148. [DOI] [PubMed] [Google Scholar]
- 21.Demaerschalk BM, Boyd EL, Barrett KM, et al. Comparison of Stroke Outcomes of Hub and Spoke Hospital Treated Patients in Mayo Clinic Telestroke Program. J Stroke Cerebrovasc Dis 2018; 27: 2940–2942. 2018/08/28. DOI: 10.1016/j.jstrokecerebrovasdis.2018.06.024. [DOI] [PubMed] [Google Scholar]
- 22.Agrawal K, Raman R, Ernstrom K, et al. Accuracy of Stroke Diagnosis in Telestroke-Guided Tissue Plasminogen Activator Patients. J Stroke Cerebrovasc Dis 2016; 25: 2942–2946. 2016/09/08. DOI: 10.1016/j.jstrokecerebrovasdis.2016.08.009. [DOI] [PubMed] [Google Scholar]
- 23.Ranta A, Lanford J, Busch S, et al. Impact and implementation of a sustainable regional telestroke network. Intern Med J 2017; 47: 1270–1275. 2017/07/26. DOI: 10.1111/imj.13557. [DOI] [PubMed] [Google Scholar]
- 24.Muller-Barna P, Hubert GJ, Boy S, et al. TeleStroke units serving as a model of care in rural areas: 10-year experience of the TeleMedical project for integrative stroke care. Stroke 2014; 45: 2739–2744. 2014/08/26. DOI: 10.1161/STROKEAHA.114.006141. [DOI] [PubMed] [Google Scholar]
- 25.Zhang D, Wang G, Zhu W, et al. Expansion Of Telestroke Services Improves Quality Of Care Provided In Super Rural Areas. Health Aff (Millwood) 2018; 37: 2005–2013. 2019/01/12. DOI: 10.1377/hlthaff.2018.05089. [DOI] [PubMed] [Google Scholar]
- 26.Nguyen-Huynh MN, Klingman JG, Avins AL, et al. Novel Telestroke Program Improves Thrombolysis for Acute Stroke Across 21 Hospitals of an Integrated Healthcare System. Stroke 2018; 49: 133–139. 2017/12/17. DOI: 10.1161/STROKEAHA.117.018413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Heppner S, Mohr NM, Carter K, et al. HRSA’s Evidence-Based Tele-Emergency Network Grant Program: Multi-site prospective cohort analysis across six rural tele-emergency networks [submitted]. PLoS Medicine 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heppner SMN, Carter K, Ullrich F, Merchant KAS, Ward MM. HRSA’s Evidence-Based Tele-Emergency Network Grant Program: Multi-site prospective cohort analysis across six rural tele-emergency networks [submitted]. PLoS Medicine 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008; 61: 344–349. DOI: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 30.Gilboy NTT, Travers D, Rosenau AM. Emergency Severity Index (ESI): A triage tool for emergency department care, Version 4. Implementation handbook 2012 edition. Rockville, MD: Agency for Healthcare Research and Quality, November 2011. [Google Scholar]
- 31.Dimick JB, Staiger DO and Birkmeyer JD. Ranking hospitals on surgical mortality: the importance of reliability adjustment. Health Serv Res 2010; 45: 1614–1629. 2010/08/21. DOI: 10.1111/j.1475-6773.2010.01158.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mohr NM, Young T, Harland KK, et al. Telemedicine Is Associated with Faster Diagnostic Imaging in Stroke Patients: A Cohort Study. Telemed J E Health 2019; 25: 93–100. 2018/06/30. DOI: 10.1089/tmj.2018.0013. [DOI] [PubMed] [Google Scholar]
- 33.Almallouhi E, Holmstedt CA, Harvey J, et al. Long-Term Functional Outcome of Telestroke Patients Treated Under Drip-and-Stay Paradigm Compared with Patients Treated in a Comprehensive Stroke Center: A Single Center Experience. Telemed J E Health 2018. 2018/09/27. DOI: 10.1089/tmj.2018.0137. [DOI] [PubMed] [Google Scholar]
- 34.Dutta D, Kendall J, Holmes C, et al. Evaluation of a telephone advice system for remote intravenous thrombolysis in ischemic stroke: data from a United kingdom network. Stroke 2015; 46: 867–869. 2015/01/22. DOI: 10.1161/STROKEAHA.114.008190. [DOI] [PubMed] [Google Scholar]
- 35.Messe SR, Khatri P, Reeves MJ, et al. Why are acute ischemic stroke patients not receiving IV tPA? Results from a national registry. Neurology 2016; 87: 1565–1574. 2016/10/22. DOI: 10.1212/WNL.0000000000003198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brott T, Adams HP Jr., Olinger CP, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke 1989; 20: 864–870. 1989/07/01. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.