Abstract
Introduction:
Comprehensive geriatric assessment prior to oncologic surgery can help predict surgical outcomes. We tested whether an abbreviated geriatric assessment tool, the Vulnerable Elderly Surgical Pathways and outcomes Assessment (VESPA), would predict post-operative complications among older adults undergoing oncologic surgery.
Method:
From 2008 to 2011, geriatric assessments were completed using the VESPA tool for patients age ≥ 70 seen in a pre-operative clinic. The VESPA assessed functional status, mood, cognition, and mobility, and can be completed in <10 minutes. We selected the subset of patients who underwent oncologic surgery and evaluated the VESPA’s ability to predict post-operative surgical complications, geriatric complications (e.g., delirium), length of stay, and geriatric post-discharge needs (e.g., new functional dependence).
Results:
A total of 476 patients who underwent oncologic surgery received the assessment using VESPA. Compared to patients with low VESPA scores (<9), patients with high VESPA scores (≥9) had longer length of stay (mean 6.6 vs. 2.0 days; p<0.001), more geriatric complications (39.5% vs. 5.7%; p<0.001), more surgical complications (29.5% vs. 11.8%; p<0.001), and more likely to have post discharge needs (76.0% vs. 31.7%; p<0.001). Using logistic regression, each additional point on the VESPA scale was also associated with increased probability of geriatric complications (OR = 1.3; 95% CI = 1.2–1.4), surgical complications (OR = 1.2; 95% CI = 1.1–1.2), and geriatric post-discharge needs (OR = 1.3; 95% CI = 1.2–1.3).
Conclusion:
The VESPA identifies older patients with cancer who are at risk for postoperative surgical and geriatric complications as well as functional needs at hospital discharge.
Keywords: geriatric assessment, postoperative complications, geriatric complications, functional decline
Introduction:
The geriatric population is increasing worldwide. In the United States alone, from now to the year 2050, the number of people age 65 years and older is expected to double.1 With this increase, cancer burden also increases as the majority of patients with cancer are over the age of 65.2 Treatment of solid tumors often requires surgery as part of a multimodal approach, however being able to appropriately risk stratify older patients undergoing oncologic surgery is challenging.
While older adults tend to have more comorbid medical conditions, the geriatric population is very heterogeneous. It has been well recognized that chronological age alone is not an accurate representation of a person’s physiological age nor is it an accurate predictor of surgical outcomes.3 Comprehensive geriatric assessment (CGA) is often used by geriatrician to assess an older adult’s overall wellbeing by taking into account not only comorbidities, but also functional status, cognition, mood, mobility, nutritional status, social support, and risk of polypharmacy.4 CGA has been shown to predict surgical outcomes among oncology patients in a number of studies.5,6,7 However completing a CGA can take several hours, and the time constraint is a substantial barrier to implementation in most surgery clinics. Older adults are also at risk for developing geriatric-specific complications such as delirium, falls, and functional status limitations after a surgery, which prolong hospital stay and long-term recovery.8,9 Thus, an abbreviated geriatric assessment that can predict surgical as well as geriatric complications can be used to target preventive efforts, facilitate recovery, and increase effectiveness of early discharge planning.
In that effort, a novel geriatric assessment, the Vulnerable Elderly Surgical Pathways and Outcomes Assessment (VESPA), was developed. This tool was designed for use in a general geriatric population undergoing pre-operative evaluation for elective general surgery.10 In our study we aimed to assess the VESPA’s ability to predict post-operative surgical complications, geriatric complications, length of stay, and post-discharge needs among older adults undergoing oncologic surgeries.
Methods:
Study design and population:
This is a secondary analysis of data from the VESPA study, which was a prospective, observational study of patients 70 years or older who were seen in a pre-operative clinic that is part of a large university health system for a planned elective surgery from July 2008 to January 2011. Consecutive sampling was used to apply the VESPA evaluation. We had only 1 criteria for using the tool: age 70 years or older. No part of this study involved an attempt to influence surgical treatment options. In addition to the cohort of patients who received VESPA assessment, we also identified a cohort of control patients matched by type of surgical discipline seen in the same pre-operative clinic during the same period of time who did not receive VESPA assessment. Patients who require an emergency surgery were not included in this study. We previously reported that the VESPA evaluation could be streamlined and a final set of assessment could be used to predict surgical complications.10 In this analysis, we (1) focused on the subset of patients who underwent oncologic surgery 2) re-tested the VESPA score’s ability to predict geriatric and surgical complications among oncology patients, 3) tested VESPA’s ability to predict an additional outcome of geriatric post-discharge needs in this population of patient, 4) assessed the added value of the VESPA above and beyond existing preoperative risk assessment of age and American Society of Anesthesiology (ASA) score. Oncologic surgery was defined as any procedure for the treatment of a known malignancy, any procedure for the diagnosis of a possible malignancy before the pathology is known, both curative and palliative treatment of a known malignancy, or any procedure for the treatment of a complication related to the treatment of a malignancy if the treatment of the malignancy was within 2 years of the surgery.
Data collection:
A surgical physician assistant administered the VESPA (Supplementary File 1) on the day of the routine preoperative assessment, which took place within 3 months prior to the planned elective surgery. The full VESPA can be completed in < 10 minutes. After the end of the study, medical record review was then performed to abstract basic patient characteristics, comorbidities, geriatric complications, surgical complications, and geriatric post-discharge needs. Length of stay was obtained from hospital administrative data. We obtained Current Procedural Technology (CPT) codes and International Classification of Disease (ICD)-9 codes of each patient’s primary procedure and assigned the Work-related Relative Value Unit (WRVU) for the procedure. WRVU measures the relative risk and resources necessary to perform the procedure as set by Center for Medicare and Medicaid Services.10 Instead of using the exact value of the WRVU for each procedure, we divided the WRVU into tertiles to classify the procedures into 3 broad categories of complexity (low, moderate and high). Please see Supplementary File 2 for examples of procedures in each complexity category. All data collection for this study was approved by the University of Michigan Institutional Review Board (HUM00020657).
Outcomes:
The outcomes of interest were obtained via detailed review of inpatient medical record of patients who completed VESPA using abstraction tools (Supplemental file 3) and procedures noted in the original VESPA study.10 The surgical complications included 30-day mortality, unplanned readmission within 30 days, and postoperative complications defined by the National Surgical Quality Improvement Program (NSQIP). We also measured the length of stay for each patient. Geriatric complications included delirium (which was defined as any documented evidence of acute confusion, altered mental status, agitation, or the use of restraints or as-needed antipsychotic medications for treatment of delirium symptoms), development of pressure ulcer (defined as new or worsening pressure ulcer documented in any medical or nursing note), fall (defined as any unintentional loss of position from one level to another), and malnutrition (defined as inadequate oral intake documented by a dietician (a dietician consultation automatically occured after 5 days of nothing by mouth, upon initiation of ventilator support, and any tube feeding order), or for remaining patients without dietician consult, a documented meal intake of < 25% on average for over 5 days). Geriatric post-discharge needs included: discharge to a non-home location (such as a post-acute rehabilitation facility), discharge to new living situation to receive more help (such as moving in with a family member), new skilled or unskilled nursing needs at discharge, functional dependence at discharge (defined as requiring help, excluding the use assistive device, in any of these areas: eating, toileting, bathing, walking, meal preparation, transportation, and medication administration), or unpaid caregiving plan at discharge (such as caregiving tasks completed by a family member).
VESPA tool and VESPA score:
The full version of the VESPA tool (Supplementary File 1) incorporated multiple domains that are addressed in the CGA including: functional status, mobility, cognition, and mood. The design of the VESPA tool is described in detail in the initial VESPA study.10 To briefly summarize, the VESPA includes 14 questions about difficulty with Basic and Instrumental Activities of Daily Living (BADL/IADLs). Mobility impairment screen was considered positive if any abnormality was seen on a brief gait and balance exam, Time-Up-and-Go (TUG test) was greater than 20 seconds, or if there was a history of at last one fall in the past year. Mini-cog test was used to screen cognitive impairment using a cutoff sore of ≤ 3 out of 5. Finally we screened for depression with a modified Patient Health Questionnaire 2 (PHQ-2). The original PHQ items were designed to be administered on paper, but in this study we modified for verbal administration in older adults: (1) patients were asked to recall for one month (rather than two weeks) to increase the sensitivity for capturing depressive symptoms; and (2) we used a yes/no answer (instead of the 4-part response) for each question. In our study, depression screen is considered positive if the answer is “Yes” to any of the two questions (Supplementary File 1).
The VESPA score was calculated using selective domains of the geriatric assessment and surgical complexity that were found to be predictive of surgical and geriatric complications in the general geriatric population undergoing elective surgeries. For the model building of the original VESPA score (which was derived for patients undergoing both oncologic and non-oncologic elective surgeries), we first used univariate logistic regression to determine the candidate factors on risk of geriatric or surgical complications using odds ratios (ORs) of > 1.2 and p-values of <0.05 as criteria for potential retention. These candidate factors were then entered into a multivariate logistic regressions model in predicting the combined outcome of both geriatric and surgical complications. Whole points were assigned to the risk factors in the multivariate model with an effect size of at least an OR of 1.2 and p value < 0.05.10 The derivation of the long and short versions the VESPA scoring system, 14-item BADL/IADL model vs. a shorter 5-item BADL/IADL model proposed by the American College of Surgeons (ACS), was discussed previously.10 In this study cohort, we used the short version (5-item model) (see Table 1 for point value assignment and supplemental file 4 for a user-friendly scoring sheet). The VESPA score ranges from 0 to 20, with higher scores representing a greater risk of postoperative complications. As previously reported, a cutoff score of ≥ 9 has 68% sensitivity and 76% specificity in predicting increased risk of postoperative complications in the general geriatric population with AUC of 0.76.10
Table 1:
VESPA Score
| VESPA Variables | Assigned VESPA Score | |
|---|---|---|
| BADL | Transferring, Dressing, Bathing, | 1 point for each item impaired (0–3 points) |
| IADL | Preparing Meals, Grocery Shopping | 1 point for each item impaired (0–2 points) |
| Can you manage your care for several hours alone after discharge? | 2 points if answered “no” | |
| Male | 2 points | |
| Charlson Comorbidity Index Score of ≥ 2 | 2 points | |
| Procedure Complexity (WRVU)* | Low | 0 points if low, 2 points if moderate, 9 points if high |
| Moderate | ||
| High | ||
| Total | 20 points maximum | |
BADL = Basic activity of daily living; IADL = instrumental activity of daily living; WRVU = Work-related Relative Value Unit; VESPA = Vulnerable Elders Surgical Pathways and outcomes Assessment
Please see Supplementary File 2 for the example of procedures included in each category.
Statistical analysis:
In this current study, we used t-test, χ2, or fisher’s exact test to compare the complication rates between patients receiving oncologic procedures with high and low VESPA score (≥ vs. <9). Logistic regression was used to test whether the VESPA score predicts each of the 3 post-operative complications measured in this study. Additionally, we used multivariate logistic regression to assess the added value of VESPA score to other predictors (including age and ASA score) by comparing the change in area under the ROC curve (AUC). In this subset of oncology surgical patients we also tested whether items that were excluded from the final VESPA scoring system would add information regarding the new outcome of geriatric discharge needs. To do this, we tested whether each of the previously-excluded items (mini-cog, depression, and mobility screen) independently predicts geriatric discharge needs, using p<0.05 as a criterion for consideration for future inclusion, and we also considered substantive value by evaluating the odds ratio. Finally we used t-test, χ2, or fisher’s exact test to compare the patient characteristics between the VESPA cohort and the control cohort of patient who did not receive VESPA. All statistical analyses were conducted using STATA version 13 (StataCorp LP College Station, TX).
Results:
Patient Characteristics:
During the study period, a total of 476 patients who underwent oncologic surgery received the geriatric assessment using VESPA (Table 2). The mean age was 78.2 years (range 70–97 years), and 230 (48%) of them were male. Thirteen percent of the patients reported difficulty with at least one of the functional status items, 11% screened positive for depression, 6% screened positive for cognitive impairment, 39% reported that they do not think they can manage their own care after discharge and 39% had a positive mobility impairment screen. Dermatologic procedure, such as skin cancer resection, was the most common type of oncologic procedure (28%), followed by procedures for gastrointestinal malignancies (19%), urological malignancies (19%), breast cancer (16%), and head and neck cancer (13%) (Table 2).
Table 2:
Sample Characteristics (N=476)
| Variable | Mean (SD, Range) or No. (%) | ||
|---|---|---|---|
| Age, Mean (SD, Range), y | 78.2 (5.9, 70–97) | ||
| Gender (Male) | 230 (48.3) | ||
| VESPA Items | BADL Difficulty | Transferring | 15 (3.2) |
| Dressing | 10 (2.1) | ||
| Bathing | 15 (3.2) | ||
| IADL Difficulty | Preparing Meals | 39 (8.2) | |
| Grocery Shopping | 50 (10.5) | ||
| Any Difficulty in the 5 ACS-recommended Functional Status items | 64 (13.4) | ||
| Patient Reported Inability to Manage Self-care Alone After Discharge* | 177 (38.6) | ||
| Positive Depression Screen * | 52 (11.1) | ||
| Failing Mini-Cog Test* | 25 (6.0) | ||
| Gait and Mobility Screen | Fall* | 109 (23.6) | |
| Time-Up-and-Go Test >20 sec* | 67 (14.8) | ||
| Observed Abnormal/Unsteady Gait* | 84 (19.0) | ||
| Any of the Above | 174 (39.3) | ||
| Surgery Type | Dermatologic§ | 137 (28.8) | |
| Gastrointestinal | 89 (18.7) | ||
| Urologic | 89 (18.7) | ||
| Breast | 79 (16.6) | ||
| Head and neck | 64 (13.4) | ||
| Other‡ | 11 (2.3) | ||
| Thoracic | 7 (1.5) | ||
| Work RVU, Mean (SD, Range), Unit | Low (n=168) | 3.9 (2.4, 0–9.72) | |
| Medium (n=106) | 12.0 (2.0, 9.89–15.6) | ||
| High (n=202) | 27.1 (10.4, 15.72–52.84) | ||
| Charlson Comorbidity Index Score, Mean (SD, Range), Score | 3.9 (2.1, 0–14) | ||
BADL = Basic activity of daily living; IADL = instrumental activity of daily living; WRVU = Work-related Relative Value Unit; VESPA = Vulnerable Elders Surgical Pathways and outcomes Assessment
These rows have missing observations, so the denominator has been adjusted accordingly for: cannot manage by self for several hours alone at discharge (18 missing), VESPA depression (8 missing), fail Mini-Cog test (60 missing), fall (16 missing), Time-Up-and-Go test (24 missing), observed abnormal/unsteady gait (34 missing), any gait and mobility screen positive (33 missing).
Dermatologic procedures included skin cancer removal, subsequent skin graft for wound closure, or lymph node biopsy.
Other procedures include: Ophthalmologic procedures and removal of sarcoma
Outcomes:
Of the 476 patients, 4 patients had 2 separate planned surgical admissions, (i.e. a procedure with a planned 2-stage surgery), with two separate opportunities for complications and complex discharge planning, so we considered these surgeries as independent (although they shared the same VESPA score). Thus, the analytic sample was 480 patient-admissions. Mean length of stay was 4.1 days. Twenty percent of the patients had at least one geriatric complication, and malnutrition was most common type of geriatric complication (16.9%) followed by delirium (6.9%) (Table 3). Twenty percent of the patients had at least one surgical complication, and over 50% of the patient had some form of geriatric post-discharge needs. This included patients who had worsening functional status (27.5%), unpaid care giving needs (15.2%), and skilled needs for either nursing or rehabilitation (44.6%). Out of the entire study population, 13.5% of the patients were either discharged to a post-acute rehabilitation facility or an alternative living situation to receive more help, such as moving in with a family member (Table 3). When comparing the cohort of patients who received VESPA to the matched control group, there was a statistically but not substantive difference with respect to mean age and gender (supplemental file 5).
Table 3:
Outcomes (N=480)
| Outcome | Mean (±SD) or No. (%) |
|---|---|
| Length of Stay, Mean (±SD) | 4.1 (±5.0) |
| Any of the Following 4 Geriatric Complications | 98 (20.4) |
| Delirium | 33 (6.9) |
| Pressure Ulcer | 5 (1.0) |
| Fall | 7 (1.5) |
| Malnutrition | 81 (16.9) |
| Any of the Following 3 Surgical Complications | 94 (19.6) |
| NSQIP Postoperative Occurrence | 83 (17.3) |
| Death within 30 Days of Surgery | 7 (1.5) |
| Unplanned Readmission within 30 Days of Surgery | 27 (5.6) |
| Any of the Following 5 Geriatric Post-discharge Needs | 247 (51.5) |
| Any inpatient note indicating functional dependence* before discharge | 132 (27.5) |
| Unskilled needs at discharge | 6 (1.3) |
| Unpaid caregiving plan at discharge | 73 (15.2) |
| Skilled needs at discharge (e.g., rehabilitation, nursing) | 214 (44.6) |
| Discharged to non-home location (assisted living, PAR, or LTAC, or dead) or alternative living situation (e.g., moving in with a family member) | 65 (13.5) |
PAR = Post-Acute Rehabilitation; LTAC = Long Term Acute Care; NSQIP = National Surgical Quality Improvement Program
Functional dependence is defined as: requiring help, excluding the use assistive device, in any of these areas: eating, toileting, bathing, walking, meal preparation, transportation, and medication administration
VESPA Score and outcomes:
Compared to patients with low VESPA scores (<9), patients with high VESPA scores (≥9) had longer length of stay (mean 6.6 vs. 2.0 days; p<0.001), more geriatric complications (39.5% vs. 5.7%; p<0.001), and more surgical complications (29.5% vs. 11.8%; p<0.001). The high VEPSA score group was also found to have more geriatric post-discharge needs (76.0% vs. 31.7%; p<0.001), including new functional dependence at discharge (51.0% vs. 9.2%; p<0.001), skilled rehabilitation or nursing needs (66.5% vs. 26.7%; p<0.001), and inability to return to prior living situation due to care needs (22.0% vs. 6.9%; p<0.001) (Table 4).
Table 4:
Comparing Characteristics and Outcomes between Two VESPA Score Groups (N=462**)
| Characteristics & Outcomes | VESPA Score§ | P-Valueⱡ | |
|---|---|---|---|
| Low (n=262) | High (n=200) | ||
| Age, Mean | 78.5 | 78.1 | .46 |
| Positive Depression Screen*, N (%) | 25 (9.7) | 26 (13.3) | .23 |
| Failing Mini-Cog Test*, N (%) | 12 (5.3) | 13 (7.4) | .37 |
| Any Gait and Mobility Impairment*, N (%) | 97 (39.8) | 74 (40.0) | .95 |
| Surgery Type | <.001 | ||
| Dermatologic£ | 96 (36.6) | 39 (19.5) | |
| Gastrointestinal | 12 (4.6) | 74 (37.0) | |
| Urologic | 34 (13.0) | 56 (28.0) | |
| Breast | 64 (24.4) | 10 (5.0) | |
| Head and neck | 46 (17.6) | 17 (8.5) | |
| Other¥ | 8 (3.1) | 1 (0.5) | |
| Thoracic | 2 (0.8) | 3 (1.5) | |
| Length of Stay, Mean | 2.0 | 6.6 | <.001 |
| Any of the Following 4 Geriatric Complications, N (%) | 15 (5.7) | 79 (39.5) | <.001 |
| Delirium, N (%) | 4 (1.5) | 27 (13.5) | <.001 |
| Pressure Ulcer, N (%) | 1 (0.4) | 4 (2.0) | .17 |
| Fall, N (%) | 1 (0.4) | 6 (3.0) | <.05 |
| Malnutrition, N (%) | 14 (5.3) | 64 (32.0) | <.001 |
| Any of the Following 3 Surgical Complications, N (%) | 31 (11.8) | 59 (29.5) | <.001 |
| NSQIP Postoperative Occurrence, N (%) | 25 (9.5) | 54 (27.0) | <.001 |
| Death within 30 Days of Surgery, N (%) | 3 (1.1) | 4 (2.0) | .47 |
| Unplanned Readmission within 30 Days of Surgery, N (%) | 11 (4.2) | 16 (8.0) | .08 |
| Any of the Following 5 Geriatric Post-discharge Needs, N (%) | 83 (31.7) | 152 (76.0) | <.001 |
| Any new functional dependence before discharge, N (%) | 24 (9.2) | 102 (51.0) | <.001 |
| Unskilled needs at discharge, N (%) | 1 (0.4) | 5 (2.5) | .09 |
| Unpaid caregiving plan at discharge, N (%) | 19 (7.3) | 51 (25.5) | <.001 |
| Skilled needs at discharge (e.g., rehabilitation, nursing), N (%) | 70 (26.7) | 133 (66.5) | <.001 |
| Discharged to non-home location (ALF, PAR, or LTAC, or dead) or alternative living situation (e.g., moving in with a family member), N (%) | 18 (6.9) | 44 (22.0) | <.001 |
ALF = assisted living facility; PAR = Post-Acute Rehabilitation; LTAC = Long Term Acute Care; VESPA = Vulnerable Elders Surgical Pathways and outcomes Assessment; NSQIP = National Surgical Quality Improvement Program
These rows have missing observations, so the denominator has been adjusted accordingly for: VESPA depression (7 missing), fail Mini-Cog test (59 missing), any gait and mobility screen positive (32 missing).
Due to 18 missing observations in “patient reported inability to manage self-care alone after discharge”, which is a scoring question for the VESPA score, 462 patients had a VESPA score (instead of 480).
Low VESPA score group are those who had score <9, and high VESPA score group are those who had score ≥9.
P value of t-test for continuous variable and χ2 test or Fisher’s exact test (for cells with small size) for dichotomous variable.
Dermatologic procedures included skin cancer removal, subsequent skin graft for wound closure, or lymph node biopsy.
Other procedures include: Ophthalmologic procedures and removal of sarcoma
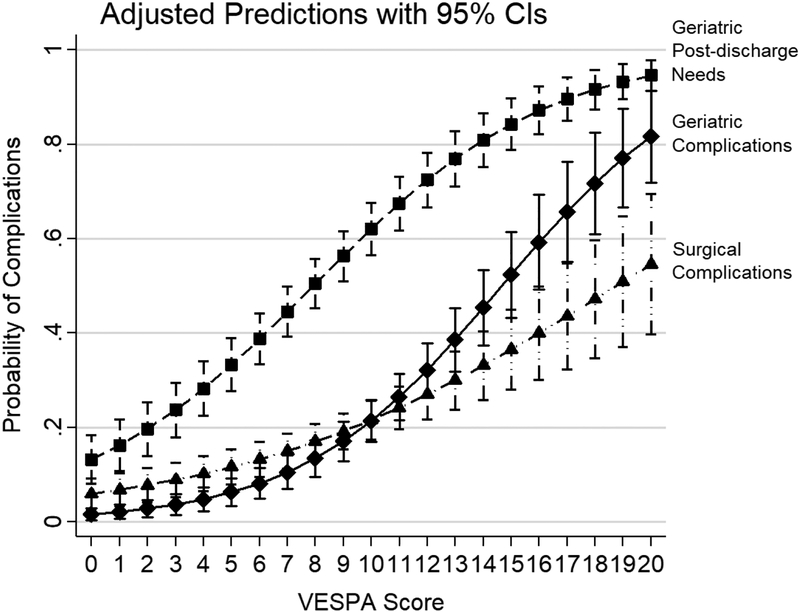
Using a logistic regression model adjusted for age, each additional point on the VESPA scale was associated with increased probability of geriatric complications (OR = 1.3 [95% CI = 1.2–1.4]; p<0.001), surgical complications (OR = 1.2 [95% CI = 1.1–1.2]; p<0.001), and geriatric post-discharge needs (OR = 1.3 [95% CI = 1.2–1.3]; p<0.001) (Table 5; Figure 1). All models showed excellent discrimination and fit (AUC 0.70–0.83 and Hosmer-Lemeshow goodness of fit test range 0.40–0.82) (Table 5). Using a multivariate logistic regression model including age and ASA score only, ASA score was predictive of geriatric complications, surgical complications, and geriatric post-discharge needs with the AUC for each complication being 0.66, 0.65 and 0.63 respectively (Table 5). However, by adding VESPA score to age and ASA score in the multivariate logistic regression model, the discrimination as measured by AUC improved to 0.83, 0.70, and 0.77 for geriatric complications, surgical complications, and geriatric post-discharge needs respectively (Table 5). And in this multivariate model, every point on the VESPA scale continued to be associated with increased probability of each complication outcome. The improvement in discrimination and VESPA’s ability to predict postoperative complications continued to hold true when we excluded patients with the low complexity procedures. (Supplemental file 6).
Table 5:
Univariate and Multivariate Logistic Regression Models for Different Complications (N=462***)
| Geriatric Complications | Surgical Complications | Geriatric Post-discharge Needs | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | Odds Ratio | P-Value | 95% CI | AUC | Odds Ratio | P-Value | 95% CI | AUC | Odds Ratio | P-Value | 95% CI | AUC |
| Univariate Logistic Regression Model 1: Age only | ||||||||||||
| Age | 1.0 | 0.228 | 1.0 – 1.1 | 0.54 | 1.0 | 0.352 | 1.0 – 1.1 | 0.54 | 1.0 | 0.033 | 1.0 – 1.1 | 0.55 |
| Multivariate Logistic Regression Model 2: Age and ASA Score | ||||||||||||
| Age | 1.0 | 0.528 | 1.0 – 1.1 | 0.66 | 1.0 | 0.528 | 1.0 – 1.1 | 0.64 | 1.0 | 0.064 | 1.0 – 1.1 | 0.63 |
| ASA Score ≥ 3 | 3.4 | <0.001 | 2.1 – 5.4 | 2.9 | <0.001 | 1.8 – 4.7 | 2.4 | <0.001 | 1.7 – 3.5 | |||
| Multivariate Logistic Regression Model 3: Age, ASA Score, and VESPA score | ||||||||||||
| Age | 1.0 | 0.17 | 1.0 – 1.1 | 0.83 | 1.0 | 0.45 | 1.0 – 1.1 | 0.73 | 1.0 | 0.035 | 1.0 – 1.1 | 0.78 |
| ASA Score ≥ 3 | 2.7 | <0.001 | 1.6 – 4.5 | 2.4 | <0.001 | 1.5 – 4.0 | 1.9 | 0.001 | 1.3 – 3.0 | |||
| VESPA Score* | 1.3 | <0.001 | 1.2 – 1.4 | 1.1 | <0.001 | 1.1 – 1.2 | 1.3 | <0.001 | 1.2 – 1.3 | |||
| Logistic Regression Model 4: VESPA score ** | ||||||||||||
| VESPA Score* | 1.3¥ | <0.001 | 1.2 – 1.4 | 0.83 | 1.2§ | <0.001 | 1.1 – 1.2 | 0.70 | 1.3⌘ | <0.001 | 1.2 – 1.3 | 0.77 |
ASA = American Society of Anesthesiologists; AUC = area under the curve
The Odds Ratio of VESPA score is for each point on the 0–20 scoring scale.
The VESPA score was controlled for age, with the mean age (78) used to estimate the probabilities.
18 patients without a VESPA score due to missing observations in “patient reported inability to manage self-care alone after discharge” were excluded from the analysis.
Hosmer-Lemeshow goodness of fit test: 0.82
Hosmer-Lemeshow goodness of fit test: 0.56
Hosmer-Lemeshow goodness of fit test: 0.40
Figure 1:
Increasing VESPA Score Predicts Geriatric, Surgical Complications and Geriatric Post-discharge Needs*
*Predicted probability based on three separate logistic regressions for Geriatric Post-Discharge Needs, Geriatric, and Surgical complications as indicated in figure. Sample was 462 older adults with oncologic surgical procedures. The VESPA score was controlled for age, with the mean age (78) used to estimate the probabilities.
As we had previously reported, the VESPA score (Table 1) was derived using items of the VESPA tool that were predictive of surgical complications or the composite geriatric complications.10 In that analysis, we did not include the outcome of geriatric post-discharge need. Thus in this study, we looked specifically at the VESPA items that were omitted from the VESPA score: depression, failing mini-cog test, and abnormal mobility screen. Of these variables tested, only failing the mini-cog test was significantly predictive of geriatric post-discharge needs independent of the VESPA score, associated with a 3-fold increase in the odds (OR = 3.0 [95% CI = 1.2–7.8]).
Discussion:
Despite mounting evidence supporting the use of geriatric assessment and recent recommendations by the American College of Surgeons (ACS), American Geriatric Society (AGS), and the International Society of Geriatric Oncology (SIOG) to incorporate geriatric assessment in evaluating older adults for surgery,3,4,11 the use of geriatric assessment in the preoperative setting is still limited. The SIOG surgical task force developed a tool called “Preoperative Assessment in Elderly Cancer Patients” (PACE).12,13 Like the VESPA tool, PACE also included assessment of cognition, functional status (ADL and IADL), depression and comorbidities. PACE had additional assessments such as American Society for Anesthesiologist scale, ECOG performance status, and brief fatigue inventory, and thus would take longer to complete then the VESPA. In a large prospective study, the SIOG surgical task force was able to show that the PACE tool is a valuable tool to identify patients at risk for surgical complications.14 Even after the publication of this study, a recent survey by the SIOG surgical task force found that in assessing older adults for oncologic surgery, only 6% of the surgeons used CGA in their daily practice, only 8% asked about ADL and IADLs, and collaboration with geriatrician was low (36.3%).15 This can be partially due to time constraint, lack of geriatric trained staff to complete a geriatric assessment or limited access to geriatricians for consultation.
Given these real-world limitations, we think that the VESPA tool addresses an unmet need. VESPA is an abbreviated geriatric assessment tool that has been tested in a busy general surgical pre-operative clinic. Given that the original full assessment (Supplementary File 1) can be completed in <10 minutes,10 we believe the use of the abbreviated VESPA score (Table 1) would take even less time which will likely increase the sustainability of this assessment tool. While we would encourage collaboration with geriatricians, formal geriatric fellowship training is not necessary to complete the VESPA, which makes this tool more applicable in clinical settings where there is a shortage of geriatricians and geriatric trained staff. In our original study, the staff who administered the VESPA were surgical physician assistants who had only 1 hour of in-service training by a geriatrician on geriatric assessment screening tools.
In addition to the abbreviated VESPA, we found that the Mini-cog in our study cohort (patients undergoing oncologic procedures) is independently predictive of complex discharge needs that are unique to older adults, above and beyond the VESPA score. Mini-cog was also found to be helpful to assessing a patient’s expectation of post discharge independence.16 An abnormal mini cog should trigger early clinical action aimed at preventing complex discharge, including early discharge planning, early social work involvement, and preoperative17 or early post-operative physical and occupational therapy to prevent these discharge complications. Thus we propose that the Mini-cog should be included in the preoperative assessment of oncology patients in addition to the abbreviated VESPA.
We considered the broad range of oncologic surgery types that’s included in our study cohort as a strength of this research. In the original study of all surgical procedures, it was the cancer patients who underwent the most complex surgeries, as well as provided the bulk of the simpler procedures such as diagnostic procedures.10 It is natural that the extensiveness of the surgery, represented by WRVUs, would predict clinical outcomes. We believe it is important to retain predictors that a-priori predict outcomes of interest, in order to determine the value of collecting additional information. In this and our prior studies, we described the additional predictive power of collecting information on physical function (BADL and IADL), cognitive function, co-morbidities, and patients reported assessment of self-care ability above and beyond the WRVU categories.16 In our study cohort, we found that even among patients who score 9 points from planning an extensive surgery based on WRVU, as shown in Fig 1, the predicted risks continue to increase throughout the range of the VESPA score (0–20). In our study, we also found that even when we excluded patients receiving low complexity surgery, each point on the VESPA scale continued to predict increased risk for all postoperative complications for patients receiving moderate and high complexity surgeries. While ASA score was able to predict postoperative complications, we found that by including VESPA to ASA score, the model’s ability to correctly predict these complications improved as demonstrated in the AUC increase. The AUC in this multivariate model is also very similar to the model that used only VESPA score as a predictor while controlling for age, as shown in Table 5. All of this underscored the importance of a geriatric assessment in the pre-operative setting.
Prior studies have evaluated other geriatric assessment tools in the preoperative setting for oncology patients, such as the PACE tool, however the main endpoints of these studies were postoperative surgical complications,14,18,19,20,21,22,23,24 and only a few small studies evaluated the risk of delirium as an endpoint.25,26,27,28 VESPA adds to this existing body of research by providing risk prediction for not only surgical complications, but also postoperative adverse outcomes that are unique to older adults including delirium, falls, malnutrition, new functional dependence and care giving needs. Discussing these possible outcomes is a crucial step when considering older patients for cancer treatment, not only in guiding treatment decisions, but also to prepare the patients and their families for new functional status impairments after surgery.
There are several limitations to our study. Although we found that while Mini-cog was predictive of complex discharge needs, we have previously reported that the Mini-cog score did not predict delirium alone in a subsample analysis of this cohort.29 We believe this due to a number of reasons. First the delirium incidence of 6.9% is likely a low estimate in this oncologic surgery population and our study is underpowered and not designed to capture delirium by itself. Secondly delirium was measured retrospectively by chart review, which only captures severe cases, thus insensitive to the true delirium as reported by prospective studies that utilize more effective ways to catch delirium symptoms. Because we have under-detected the outcome, our results are biased towards the null finding, that is, we expect that the true ability of the VESPA for detecting the full spectrum of delirium would be better than the results of this study. Thus a negative finding of Mini-cog on its ability to predict postoperative delirium in our study should not detract from its effectiveness. Another limitation of this study is the use of the modified PHQ2 which is not validated, thus for future studies, we would plan on using a validated tool such as the PHQ9 of Geriatric Depression Scale without modification. Another limitation of the VESPA tool is that it is not designed to replace a comprehensive geriatric assessment, and should be used to complement existing assessments already in practice for each specific cancer. How to reduce pre-surgical modifiable risk factors requires more than just calculating risk, but individualizing interventions based on the planned procedure, the patient’s abilities, and the cancer itself. Another limitation of our study is that the surgical complexity component of the VESPA score in this study relies on the WRVU of the procedure which was obtained post-operatively, instead of during the pre-operative visit, and knowing the exact number of WRVUs in advance of a planned procedure are infeasible. Thus, to overcome this limitation, we grouped broad ranges of WRVUs into 3 complexity categories and have published the ranges of the WRVUs in order to provide clinicians with a general idea of the types of procedures for each complexity category (supplemental file 2). We suggest that clinicians use their best judgment to classify patients into the three categories once they review the range of surgery types in each category. Additional study is needed to validate a prospectively-calculated VESPA score. Additionally, including a severity scale for the complications (such as the Clavien-Dindo grading score for surgical complications) would have been an elegant outcome to study, however, our study was limited to the complications collected by the National Surgical Quality Improvement Program (NSQIP) registry. Future studies to evaluate the VESPA’s ability to distinguish the degree of complication severity would be extremely interesting. Our study was a single centered study in a university setting with a large geriatric department and a high-volume, centralized pre-operative clinic serving nearly all surgery types. While the VESPA was administered by a surgical PA, a geriatrician (KH) worked closely with the surgical team in the development and implementation of the VESPA tool. Thus, it is possible that our experience with integrating VESPA into the workflow of overall patient care may differ in lower-volume or single-specialty surgery clinics. After further streamlining of the VESPA, we plan to retest at smaller pre-operative evaluation sites within our health care center. Despite these limitations, our study has demonstrated that the VESPA tool is a practical tool that can identify older patients with cancer at risk for postoperative surgical and geriatric complications as well as functional dependence and care needs at discharge. The VESPA tool offers a way to overcome common real-life barriers to complete a CGA, such as limited staff resources and time constraint. We think that the VESPA tool should be considered as part of the routine evaluation of older patients with cancer under going surgery. We are currently in the process of developing a quality improvement project at our institution to incorporate the VESPA tool into our electronic medical record system (Epic) as a user-friendly tool for older patients being evaluated for elective surgery. We plan to use the information obtained from the VESPA to not only identify patients who are at risk for postoperative complications, but also to set up interventions to prevent and prepare for these complications. In order to improve the sustainability of this tool, in our next phase of the VESPA project, we plan to target patients with at least moderately-complex surgeries (planned inpatient stay of at least 1 night, thus eliminating the simple same-day biopsies), implement annual reinforcement to continue training new physician assistants, provide feedback of VESPA evaluation rates to participating providers, implement automated reminders in the electronic medical record system to deploy the VESPA template on the targeted population during the pre-operative visit based on age and planned overnight stay, link the results to a clinical intervention to prevent surgical complications common to older adults, therefore providing surgery providers a clinical reason to perform these additional assessments. Further studies are needed to evaluate the outcomes of these interventions.
Supplementary Material
Footnotes
Conflict of interest: None
References
- 1.He W, Goodkind D, Kowal P. An Aging World : 2015 International Population Reports. Aging (Albany NY). 2016;(March):165 doi:P95/09-1. [Google Scholar]
- 2.Howlader N; Noone AM; Krapcho M; Miller D; Bishop K; Kosary CL; Yu M; Ruhl J; Tatalovich Z; Mariotto A; Lewis DR; Chen HS; Feuer EJ; Cronin KA (eds). CANCER STATISTICS REVIEW 1975–2014. SEER. 2014. [Google Scholar]
- 3.Audisio RA, Bozzetti F, Gennari R, et al. The surgical management of elderly cancer patients: Recommendations of the SIOG surgical task force. Eur J Cancer. 2004;40(7):926–938. doi: 10.1016/j.ejca.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 4.Extermann M, Aapro M, Bernabei R, et al. Use of comprehensive geriatric assessment in older cancer patients: Recommendations from the task force on CGA of the International Society of Geriatric Oncology (SIOG). Crit Rev Oncol Hematol. 2005;55(3):241–252. doi: 10.1016/j.critrevonc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 5.Feng MA, McMillan DT, Crowell K, Muss H, Nielsen ME, Smith AB. Geriatric assessment in surgical oncology: A systematic review. J Surg Res. 2015;193(1):265–272. doi: 10.1016/j.jss.2014.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huisman MG, Kok M, De Bock GH, Van Leeuwen BL. Delivering tailored surgery to older cancer patients: Preoperative geriatric assessment domains and screening tools - A systematic review of systematic reviews. Eur J Surg Oncol. 2017;43(1):1–14. doi: 10.1016/j.ejso.2016.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Pilotto A, Cella A, Pilotto A, et al. Three Decades of Comprehensive Geriatric Assessment: Evidence Coming From Different Healthcare Settings and Specific Clinical Conditions. J Am Med Dir Assoc. 2016;18(2):192.e1–192.e11. doi: 10.1016/j.jamda.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 8.Min L, Mazzurco L, Gure T, et al. Longitudinal Functional Recovery after Geriatric Cardiac Surgery. J Surg Res. 2015;194(1):25–33. doi: 10.1021/acschemneuro.5b00094.Serotonin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neupane I, Arora R, Rudolph J. Cardiac surgery as a stressor and the response of the vulnerable older adult. Exp gerontol. 2017;87:168–174. doi: 10.1021/acschemneuro.5b00094.Serotonin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Min L, Hall K, Finlayson E, al et. Estimating risk of postsurgical general and geriatric complications using the vespa preoperative tool. JAMA Surg. 2017;152(12):1126–1133. 10.1001/jamasurg.2017.2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chow WB, Rosenthal RA, Merkow RP, Ko CY, Esnaola NF. Optimal preoperative assessment of the geriatric surgical patient: A best practices guideline from the American college of surgeons national surgical quality improvement program and the American geriatrics society. J Am Coll Surg. 2012;215(4):453–466. doi: 10.1016/j.jamcollsurg.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 12.Audisio RA, Gennari R, Sunouchi K, et al. Preoperative Assessment of Cancer in Elderly Patients: A Pilot Study. Support Cancer Ther. 2003;1(1):55–60. doi: 10.3816/SCT.2003.n.005. [DOI] [PubMed] [Google Scholar]
- 13.Pope D, Ramesh H, Gennari R, et al. Pre-operative assessment of cancer in the elderly (PACE): A comprehensive assessment of underlying characteristics of elderly cancer patients prior to elective surgery. Surg Oncol. 2006;15(4):189–197. doi: 10.1016/j.suronc.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 14.Audisio R, Pope D, Ramesh H, et al. Shall we operate? Preoperative assessment in elderly cancer patients (PACE) can help. A SIOG surgical task force prospective study. Crit Rev Oncol Hematol. 2008;65(2):156–163. doi: 10.1016/j.critrevonc.2007.11.001. [DOI] [PubMed] [Google Scholar]
- 15.Ghignone F, Van Leeuwen BL, Montroni I, et al. The assessment and management of older cancer patients: A SIOG surgical task force survey on surgeons’ attitudes. Eur J Surg Oncol. 2016;42(2):297–302. doi: 10.1016/j.ejso.2015.12.004. [DOI] [PubMed] [Google Scholar]
- 16.Chan C-L, Diehl KM, Hall KE, Palazzolo WC, Pollock Y, Min LC. Unrealistic Postsurgical Expectation of Independence Predicts Complex Hospital Discharge. J Surg Res. 2019;235:501–512. doi: 10.1016/j.jss.2018.10.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Silver JK, Baima J. Cancer prehabilitation: An opportunity to decrease treatment-related morbidity, increase cancer treatment options, and improve physical and psychological health outcomes. Am J Phys Med Rehabil. 2013;92(8):715–727. doi: 10.1097/PHM.0b013e31829b4afe. [DOI] [PubMed] [Google Scholar]
- 18.Dale W, Hemmerich J, Kamm A, et al. Geriatric Assessment Improves Prediction of Surgical Outcomes in Older Adults Undergoing Pancreaticoduodenectomy A Prospective Cohort Study. Ann Surg. 2014;259(5):960–965. doi: 10.1097/SLA.0000000000000226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee YH, Oh H-K, Kim D-W, et al. Use of a Comprehensive Geriatric Assessment to Predict Short-Term Postoperative Outcome in Elderly Patients With Colorectal Cancer. Ann Coloproctol. 2016;32(5):161–169. doi: 10.3393/ac.2016.32.5.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pujara D, Mansfield P, Ajani J, et al. Comprehensive geriatric assessment in patients with gastric and gastroesophageal adenocarcinoma undergoing gastrectomy. J Surg Oncol. 2015;112(8):883–887. doi: 10.1002/jso.24077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaibori M, Ishizaki M, Matsui K, et al. Geriatric assessment as a predictor of postoperative complications in elderly patients with hepatocellular carcinoma. Langenbeck’s Arch Surg. 2016;401(2):205–214. doi: 10.1007/s00423-016-1388-1. [DOI] [PubMed] [Google Scholar]
- 22.Kothari A, Phillips S, Bretl T, Block K, Weigel T. Components of geriatric assessments predict thoracic surgery outcomes. J Surg Res. 2011;166(1):5–13. doi: 10.1016/j.jss.2010.05.050. [DOI] [PubMed] [Google Scholar]
- 23.Kenig J, Olszewska U, Zychiewicz B, Barczynski M. Cumulative deficit model of geriatric assessment to predict the postoperative outcomes of older patients with solid abdominal cancer. J Geriatr Oncol. 2015;6(5):370–379. doi: 10.1016/j.jgo.2015.03.004. [DOI] [PubMed] [Google Scholar]
- 24.Bouhassira J, Bosc R, Greta L, Hersant B. Factors associated with postoperative complications in elderly patients with skin cancer : A retrospective study of 241 patients. J Geriatr Oncol. 2016;7(1):10–14. doi: 10.1016/j.jgo.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 25.Choi JY, Yoon SJ, Kim SW, et al. Prediction of Postoperative Complications Using Multidimensional Frailty Score in Older Female Cancer Patients with American Society of Anesthesiologists Physical Status Class 1 or 2. J Am Coll Surg. 2015;221(3):652–660. doi: 10.1016/j.jamcollsurg.2015.06.011. [DOI] [PubMed] [Google Scholar]
- 26.Suh DH, Kim J-W, Kim HS, Chung HH, Park NH, Song YS. Pre- and intra-operative variables associated with surgical complications in elderly patients with gynecologic cancer: The clinical value of comprehensive geriatric assessment. J Geriatr Oncol. 2014;5(3):315–322. doi: 10.1016/j.jgo.2014.03.004. [DOI] [PubMed] [Google Scholar]
- 27.Fukuse T, Satoda N, Hijiya K, Fujinaga T. Importance of a comprehensive geriatric assessment in prediction of complications following thoracic surgery in elderly patients. Chest. 2005;127(3):886–891. doi: 10.1378/chest.127.3.886. [DOI] [PubMed] [Google Scholar]
- 28.Indrakusuma R, Dunker MS, Peetoom JJ, Schreurs WH. Evaluation of preoperative geriatric assessment of elderly patients with colorectal carcinoma. A retrospective study. Eur J Surg Oncol. 2015;41(1):21–27. doi: 10.1016/j.ejso.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 29.Miller AL, Englesbe MJ, Diehl KM, et al. Preoperative Psoas Muscle Size Predicts Postoperative Delirium in Older Adults Undergoing Surgery: A Pilot Cohort Study. J Am Geriatr Soc. 2017;65(1):e23–e24. doi:doi: 10.1111/jgs.14571. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.