Abstract
The nature of discomfort and level of exertion associated with wearing respiratory protection in the health care workplace are not well understood. Although a few studies have assessed these topics in a laboratory setting, little is known about the magnitude of discomfort and the level of exertion experienced by workers while they deliver health care to patients for prolonged periods. The purpose of this study was to determine the magnitude of discomfort and level of exertion experienced by health care workers while wearing respiratory protection for periods up to 8 hr when performing their typical occupational duties. This project was a multiple cross-over field trial of 27 health care workers, aged 24–65, performing their typical, hospital-based occupational duties. Each participant served as his/her own control and wore one of seven respirators or a medical mask for 8 hr (or as long as tolerable) with interposed doffing periods every 2 hr. Self-perceived discomfort and exertion were quantified before each doffing: self-perceived level of discomfort using a visual analog scale, and self-perceived level of exertion using a Borg scale. Overall, and as would be expected, discomfort increased over time with continual respirator use over an 8-hr period. Interestingly, exertion increased only marginally over the same time period. The relatively low level of exertion associated with eight respiratory protective devices, including models commonly used in the U.S. health care workplace, is not likely to substantially influence workers’ tolerability or occupational productivity. However, the magnitude of discomfort does appear to increase significantly over time with prolonged wear. These results suggest that respirator-related discomfort, but not exertion, negatively influences respirator tolerance over prolonged periods. Discomfort may also interfere with the occupational duties of workers.
Keywords: discomfort, exertion, health care, respirator, tolerance, workers
INTRODUCTION
There is widespread debate about the best and most appropriate types of respiratory protection that health care workers (HCWs) should don during influenza and other infectious disease outbreaks.(1–5) Recent reports(1, 6) of HCWs’ experiences when responding to disease outbreaks have suggested that some respirators may not be well tolerated, especially among workers who are not accustomed to wearing them for extended periods. Problems with respirator tolerability have been attributed to overall discomfort;(6–10) diminished visual,(8, 11, 12) vocal,(11, 12) or auditory(11) acuity; excessive humidity(7) or heat;(7, 10, 12, 13) headaches,(6, 14) facial pressure;(7) skin irritation or itchiness;(6, 7, 12, 13) excessive fatigue or exertion;(6, 7, 9, 10, 12, 13) malodorousness;(7, 10) anxiety or claustrophobia;(6, 13, 15, 16) and other interferences with occupational duties.(10, 17–19) However, few studies have formally field tested the tolerability of respirators commonly worn by HCWs(1) who may be called on to wear respiratory protection in extreme scenarios for the duration of their work shifts during a large-scale infectious disease outbreak.(5, 20, 21) The likelihood of U.S. health care workers tolerating respirators for 8 or more hours per day over the days and weeks of an evolving outbreak is unknown.
While infection control guidelines(2, 5, 20, 22) call for discarding disposable respirators after each patient contact, recent experiences during the 2009 H1N1 pandemic suggest that this approach may not be plausible. Limited supplies, production capabilities, and financial resources may require respirator rationing.(20–24) During an outbreak, one way to decrease costs and extend the usable period of respirators might be to cover each disposable respirator with a medical mask that would be discarded after close patient contact.(22) However, this approach has the potential to affect the seal to the face and might alter respirator discomfort or exertion necessary to breathe through the device.(25) Another way to decrease costs is to use reusable respirators. An improved understanding of the factors affecting tolerability in extreme respirator use scenarios could provide evidence-based recommendations about respirator selection and use.
METHODS
Subjects
This study was approved by the North Florida/South Georgia Veteran Affairs Medical Center (VAMC) institutional review board and research oversight committees. Twenty-seven volunteers (mean age, 48 years [SD, 11 years; range 25–65 years]; 15 women) participated in the study (Table I). To be included, participants must have previously worn a respirator in the context of their occupational duties, making them accustomed to wearing N95 filtering facepiece respirators (FFR). Participants with systemic disease or pregnancy were excluded from the study. All participants were non-smokers. The sample comprised 16 nurses, 2 nurse practitioners, 4 nurse technicians, 2 telemetry technicians, 2 respiratory therapists, and 1 clerical assistant from the intensive care unit (15), emergency department (6), and medical/surgical ward (6). Each participant was provided written informed consent. Each participant also underwent a pre-participation examination (OSHA form and brief history and physical) and was fit tested for each respirator worn in the study. All subjects were instructed to simulate the circumstances of an airborne-transmissible disease outbreak (e.g., influenza pandemic) in which their use of a respirator for the duration of their work shift would be necessary.
TABLE I. Characteristics of Subjects (N = 27).
| Number | Percent Total (%) | |
|---|---|---|
| Gender | ||
| Female | 15 | 55.6 |
| Male | 12 | 44.4 |
| Location | ||
| MICUA | 2 | 7.4 |
| MICU/SICU | 6 | 22.2 |
| SICUB | 7 | 25.9 |
| EDC | 6 | 22.2 |
| Medical/surgical ward | 6 | 22.2 |
| Occupation | ||
| Nurse practitioner | 2 | 7.4 |
| Nurse | 16 | 59.3 |
| Nurse technician | 4 | 14.8 |
| Telemetry technician | 2 | 7.4 |
| Clerical assistant | 1 | 3.7 |
| Respiratory therapist | 2 | 7.4 |
Medical intensive care unit.
Surgical intensive care unit.
Emergency department.
Apparatus
The respirator models most commonly used by the study centers were selected for inclusion and were acknowledged as commonly used models in many Veterans Health Administration hospitals and clinics across the United States (V. Wilkes, Department of Veterans Affairs, Washington, D.C., July 15, 2008, pers. comm.). The following ensembles were included: Medical Mask (MM); Duckbill N95 (DB); Cup N95 (N95); Cup N95 + Exhalation Valve (N95+V); Cup N95 + Medical Mask (N95+MM); Cup N95 + Exhalation Valve + Medical Mask (N95+V+MM); Half-face Elastomeric Respirator (HER); and Powered Air-Purifying Respirator (PAPR) (Table II). A medical mask (MM) was placed over two of the models to gauge the combined affect on tolerance.
TABLE II. Commonly Used Respiratory Protective Devices with or without an Overlying Medical Mask.
| Type | Model | Exhalation Style | Surgical Mask Valve Model | Overlying | Mfr. | Filter | Cartridge |
|---|---|---|---|---|---|---|---|
| Control (no respiratory protective equipment) | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Half-mask filtering facepiece | Cup-shaped | No | No | 3M | 1860 | N95 | N/A |
| Medical mask | Loose-fitting | No | N/A | Precept | 15320 | N/A | N/A |
| Half-mask filtering facepiece | Duckbill | No | No | Kimberly Clark | PFR95170 | N95 | N/A |
| Half-mask filtering facepiece | Cup-shaped | No | Yes | 3M; Precept | 1860; 15320 | N95 | N/A |
| Half-mask filtering facepiece | Cup-shaped | Yes | No | 3M | 8511 | N95 | N/A |
| Powered air-purifying | Hooded | No | No | 3M | Air-Mate | HEPF | 451–02-01 |
| Half-mask filtering facepiece | Cup-shaped | Yes | Yes | 3M; Precept | 8511; 15320 | N95 | N/A |
| Half-mask elastomeric | Half-face | Yes | No | North | 5500 | P100 | 7580P100 |
Notes: All respirators certified by NIOSH.
N95 – Filters at least 95% of airborne particles. Not resistant to oil.
P100 – Filters at least 99.97% of airborne particles. Strongly resistant to oil.
HEPF – High-efficiency particulate filter.
Surgical mask – Precept Medical Products, Arden, North Carolina.
North 5500 – North Safety Products, Cranston, Rhode Island.
Duckbill filtering facepiece respirator- Kimberly-Clark Corporation, Irving, Texas.
Cup-shaped filtering facepiece respirator- 3M Corporation, St. Paul, Minnesota.
Procedure
This was a multiple cross-over field trial of 27 health care workers, aged 24–65, while performing their typical, hospital- and clinic-based occupational duties. Each served as his/her own control and wore one of seven respirators ensembles or a medical mask for 8 hr, or as long as tolerable, with interposed doffing periods every 2 hr. This was repeated such that each participant wore each respirator ensemble, with one exception (one participant failed the duckbill N95 fit test and did not wear that ensemble during the measured trials). Each health care worker had three scheduled breaks from wearing the devices throughout the day: 15 min at the 2-hr and 6-hr mark, and 30 min at the 4-hr mark. Subjects were asked to rate their self-perceived discomfort using a 1–10 visual analog scale(26) and exertion levels using a Borg exertion scale(27) at donning, after 30 min and each subsequent 120 (± 15) min, and at doffing. The study sessions were terminated when subjects expressed a need to remove the respirator within “the next 10 minutes” because of intolerance or completed an 8-hr session. Only one participant terminated early.
Analyses
Means and standard deviations for discomfort and exertion levels were calculated. Missing discomfort and exertion outcomes were imputed by carrying the last observation forward based on our understanding of missing mechanism in this study. Linear mixed-effect models were used to examine if discomfort and exertion levels were different among different respirators and changed over time, where random effects were included for clustering by subject and location to account for the correlation within cluster. In all models, we controlled for effects of gender, age, and physical activity. Standard model diagnostics were used to assess model adequacy. To account for the Type I error inflation, we used the Bonferroni stepdown method to adjust p-values, shown to be more powerful than the classic Bonferroni adjustment while maintaining strong control of the family-wise Type I error.(28, 29)
RESULTS
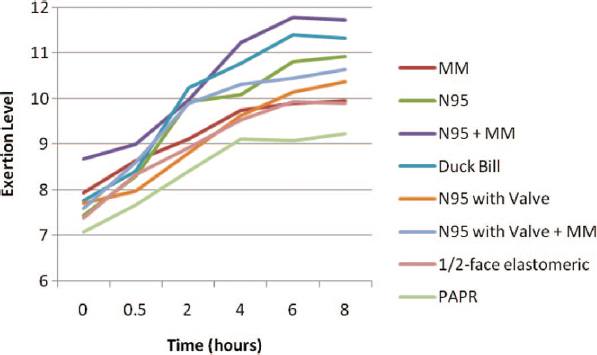
Twenty-seven of 28 subjects who consented met eligibility criteria and completed the study. Figures 1 and 2 show the mean discomfort and exertion ratings, respectively, for all ensembles during 8 hr, and p-values <0.05 compared with the PAPR to provide a standardized comparison.
FIGURE 1. Mean discomfort level over 8-hr work shift. Notes: Interrupted y-axis to improve visualization of data. Fitted linear mixed-effect model showed: average discomfort level was significantly different among respirators (p = 0.0351) and over time (p < 0.0001). N95 had significantly different discomfort level from PAPR at 6 hr (adjusted p = 0.0065) and at 8 hr (adjusted p = 0.0072). N95+MM had significantly different discomfort level from PAPR at 4 hr (adjusted p = 0.0280), 6 hr (adjusted p = 0.0042), and 8 hr (adjusted p = 0.0015). N95+V+MM had significantly different discomfort level from PAPR at 6 hr (adjusted p = 0.0441) and at 8 hr (adjusted p = 0.0088). N95+V+MM and N95+V did not have significantly different discomfort level (adjusted p > 0.1). N95 + MM and N95 did not have significantly different discomfort level (adjusted p > 0.9).
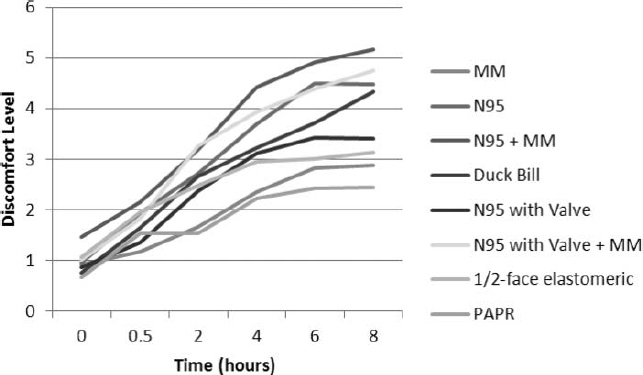
FIGURE 2. Mean exertion level over time. Notes: Interrupted y-axis to improve visualization of data. Fitted linear mixed effect model showed: average exertion level was significantly different among some respirators and over time (p < 0.0001). DB had significantly different exertion level from PAPR at 6 hr (adjusted p = 0.0256) and marginally at 8 hr (adjusted p = 0.0510). N95 had marginally different exertion level from PAPR at 6 hr and 8 hr (adjusted p = 0.0510). N95+V+MM and N95+V did not have significantly different exertion level (adjusted p > 0.5). N95 + MM and N95 did not have significantly different exertion level (adjusted p > 0.5).
Discomfort
The fitted, linear mixed-effect model showed average discomfort level was significantly different among respirators (p = 0.0351) and over time (p<0.0001) (Figure 1). Specifically, the N95 had a significantly greater discomfort level than PAPR at 6 hr (adjusted p = 0.0065) and at 8 hr (adjusted p = 0.0072). The N95+MM had a significantly greater discomfort level than the PAPR at 4 hr (adjusted p = 0.0280), 6 hr (adjusted p = 0.0042), and 8 hr (adjusted p = 0.0015). In addition, the N95+V+MM had a significantly greater discomfort level than PAPR at 6 hr (adjusted p = 0.0441) and at 8 hr (adjusted p = 0.0088), while the N95+V+MM and N95+V did not have a significantly greater discomfort level (adjusted p > 0.1). Finally, the N95 + MM and N95 did not have a significantly greater discomfort level (adjusted p > 0.9). Of note, participants received a 45-min break at the first 4 hr and a 15-min break after the subsequent 4 hr of investigation. The longer break time of the first 4 hr may have been a factor given that the N95 and N95+V+MM had no difference compared with PAPR at 4 hr.
Exertion
On average, self-perceived exertion level rose proportionately, approximately two points on the validated Borg scale (Figure 2), which corresponds to an energy expenditure of approximately one to two metabolic equivalents (METs).(30, 31) The fitted, linear mixed-effect model showed average exertion level was significantly greater among some respirators and over time (p<0.0001). Specifically, DB had a significantly different exertion level than PAPR at 6 hr (adjusted p = 0.0256) and marginally at 8 hr (adjusted p = 0.0510). The N95 had a marginally greater exertion level than the PAPR at 6 hr and 8 hr (adjusted p = 0.0510). The N95+V+MM and N95+V did not have a significantly different exertion level (adjusted p > 0.5). Similarly, the N95 + MM and N95 did not have a significantly different exertion level (adjusted p > 0.5).
DISCUSSION
We sought to determine the level of discomfort and exertion experienced by HCWs wearing commonly used respirator models for an 8-hr work shift. Concerns about global shortages(32) of disposable filtering facepiece respirators during periods of peak demand have helped make this a pressing topic.
For participating HCWs, the level of self-perceived discomfort increased over time and across respirators. While this finding hardly seems unexpected, the fact that discomfort increases with prolonged respirator use has not been quantified in this fashion and reported in peer-reviewed literature, to our knowledge. As previously reported,(21) we found that approximately half the subjects in our study, HCWs who were accustomed to wearing respirators for brief periods, were not willing to wear most respirators or a medical mask for the 8-hr work shift even with interposed break periods. Facial heat,(7, 10, 12, 13, 21) pain,(6, 14, 21) and pressure(7, 21) are among the most common complaints associated with discomfort. Placing an MM over an N95 with and without an exhalation valve did not significantly change the discomfort associated with these models.
While discomfort increased notably over time, the influence of respirators on exertion appears to be less robust in the health care environment. Therefore, strategies to primarily reduce discomfort—specifically the heat, pressure, and pain complaints—may be best suited to increase respirator tolerability and compliance. Among commonly used and relatively inexpensive respirator models, an N95 with an exhalation valve was the most comfortable after 8 hr. The medical mask was mildly more comfortable; however, the MM is primarily meant to prevent the spread of contaminants by the wearer instead of protecting the wearer from outside contaminants.(22)
Study limitations include the small sample size, locations limited to one hospital system, and a setting that simulated only a pandemic scenario. Health care workers caring for patients with contagious life-threatening illnesses during a pandemic may be willing to tolerate respirators for longer periods than observed in our study, although subjects were asked to imagine themselves in such a setting. It is important to note that infection control procedures and appropriate processes for disinfecting, charging, and maintaining respirators would need to be considered if HCWs were to use respirators for extended wear periods, with use between patients, and with respirator re-use. Likewise, appropriate hand hygiene and contact precautions should always be observed. A participation bias may have led to higher tolerance levels among the study subjects than would be expected in the U.S. health care work force. The most common reason for HCWs declining to participate was unwillingness to wear the respirator equipment for prolonged periods.
Recent undertakings to better understand respirator selection, communication, and speech ineligibility have been completed.(33, 35) Current, topical studies have also investigated physiological respirator impact in persons with mild respiratory disease(35) and respirator impact on task performance.(36) Further studies will be necessary to better understand the limitations posed by respirators to the health care work force. Engaging HCWs in the design of new models may facilitate development of new respirators with improved comfort and tolerability.
Footnotes
The information in this article represents the personal opinions of the authors and does not reflect the position of the Department of Veterans Affairs, the National Center for Occupational Health and Infection Control or the University of California.
ACKNOWLEDGMENTS
The authors are grateful to Helen Dunn and Elizabeth Franco for their efforts with data collection.
REFERENCES
- 1.Institute of Medicine (IOM) : Preparing for an Influenza Pandemic: Personal Protective Equipment for Healthcare Workers. Washington, D.C.: National Academies Press, 2008. [Google Scholar]
- 2.U.S. Department of Health and Human Services : “Interim Guidance on Planning for the Use of Surgical Masks and Respirators in Health Care Settings during an Influenza Pandemic.” [Online] Available at http://www.flu.gov/professional/hospital/maskguidancehc.html (ahttp://www.pandemicflu.gov/plan/healthcare/maskguidancehc.html. (accessed Jan. 23, 2008).
- 3.World Health Organization : “Clarification: Use of Masks by HealthCare Workers in Pandemic Settings.” [Online] Available at http://www.who.int/csr/resources/publications/influenza/MaskClarification10_11.pdf (accessed Jan. 23, 2008).
- 4.Department of Veterans Affairs : “VA Pandemic Influenza Plan.” [Online] Available at http://www.pandemicflu.va.gov/docs/VAPandemicFluPlan_2006-03-31.pdf (accessed Jan. 23, 2008).
- 5.Occupational Safety and Health Administration (OSHA) : Guidance on Preparing Workplaces for an Influenza Pandemic (OSHA 3327–02N 2007). Washington, D.C.: Department of Labor, OSHA, 2007. [Google Scholar]
- 6.Registered Nurses Association of Ontario, Canada : “SARS Unmasked: Celebrating Resilience, Exposing Vulnerability.” [Online] Available at http://www.rnao.org/Storage/24/1891_SARS_Report_June_04.pdf (accessed Feb. 26, 2008).
- 7.Li Y., Tokura H., Guo Y.P., et al. : Effects of wearing N95 and surgical facemasks on heart rate, thermal stress and subjective sensations. Int. Arch. Occup. Environ. Health 78(6): 501–509 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meyer J.P., Hery M., Herrault J., et al. : Field study of subjective assessment of negative pressure half-masks. Influence of the work conditions on comfort and efficiency. Appl. Ergon. 28(5–6): 331–338 (1997). [DOI] [PubMed] [Google Scholar]
- 9.Shimozaki S., Harber P., Barrett T., and Loisides P.: Subjective tolerance of respirator loads and its relationship to physiological effects. Am. Ind. Hyg. Assoc. J. 49: 108–116 (1988). [DOI] [PubMed] [Google Scholar]
- 10.Yassi A., and Bryce E.: Protecting the Faces of Health Care Workers: Knowledge gaps and research priorities for effective protection against occupationally acquired respiratory infectious diseases. Am. J. Infect. Control 33(2): 114–121 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khoo K.L., Leng P.H., Ibrahim I.B., and Lim T.K.: The changing face of healthcare worker perceptions on powered air-purifying respirators during the SARS outbreak. Respirology 10(1): 107–110 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Doney B.G.M., Middendorf P., and Bang K.M.: “Respirator Surveillance at Five Veterans Affairs Medical Centers.” Abstract. Presentation at American Industrial Hygiene Conference & Exhibition, May 10–15, 2003, Dallas, Texas. [Google Scholar]
- 13.Jonas-Simpson C.: Courage and commitment. Can. Nurse 99(8): 9–12 (2003). [PubMed] [Google Scholar]
- 14.Lim E.C., Seet R.C., Lee K.H., Wilder-Smith E.P., Chuah B.Y., and Ong B.K.: Headaches and the N95 face-mask amongst healthcare providers. Acta Neurol. Scand. 113(3): 199–202 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bai Y., Lin C.C., Lin C.Y., Chen J.Y., Chue C.M., and Chou P.: Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. 55(9): 1055–1057 (2004). [DOI] [PubMed] [Google Scholar]
- 16.Morgan W.P.: Psychological problems associated with the wearing of industrial respirators: A review. Am. Ind. Hyg. Assoc. J. 44(9): 671–676 (1983). [DOI] [PubMed] [Google Scholar]
- 17.Farquharson C., and Baguley K.: Responding to the severe acute respiratory syndrome (SARS) outbreak: Lessons learned in a Toronto emergency department. J. Emerg. Nurs. 29(3): 222–228 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Johnston A.R., Myers W.R., Colton C.E., Birkner J.S., and Campbell C.E.: Review of respirator performance testing in the workplace: Issues and concerns. Am. Ind. Hyg. Assoc. J. 53(11): 705–712 (1992). [DOI] [PubMed] [Google Scholar]
- 19.Nickeil L.A., Crighton E.J., Tracy C.S., et al. : Psychosocial effects of SARS on hospital staff: Survey of a large tertiary care institution. CMAJ 170(5): 793–798 (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Siegel J.D., Rhinehart E., Jackson M., Chiarello L., and the Healthcare Infection Control Practices Advisory Committee (HICPAC) : 2007. Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. Atlanta, Ga.: Centers for Disease Control and Prevention, 2007. [Google Scholar]
- 21.Radonovich L.J. Jr., Cheng J., Shenal B.V., Hodgson M., and Bender B.S.: Respirator tolerance in health care workers. JAMA 301(1): 36–38 (2009). [DOI] [PubMed] [Google Scholar]
- 22.National Acadamies of Sciences, Institute of Medicine : Reusability of Facemasks during an Influenza Pandemic: Facing the Flu. Washington, D.C.: National Academies Press, 2006. [Google Scholar]
- 23.Toner E., and Waldhorn R.: What hospitals should do to prepare for an influenza pandemic. Biosecur. Bioterror. 4(4):397–402 (2006). [DOI] [PubMed] [Google Scholar]
- 24.Viscusi D.J., King W.P., and Shaffer R.E.: Effect of decontamination on the filtration efficiency of two filtering facepiece respirator models. J. Int. Soc. Respir. Prot. 24: 93–107 (2007). [Google Scholar]
- 25.Roberge R.J.: Effect of surgical masks worn concurrently over N95 filtering facepiece respirators: Extended service life versus increased user burden. J. Public Health Manag. Pract. 14(2): E19—E26 (2008). [DOI] [PubMed] [Google Scholar]
- 26.Price D.D., Bush F.M., Long S., and Harkins S.W.: A comparison of pain measurement characteristics of mechanical visual analogue and simple numerical rating scales. Pain 56(2): 217–226 (1994). [DOI] [PubMed] [Google Scholar]
- 27.Borg G.A.: Perceived exertion. Exerc. Sport Sci. Rev. 2: 131–153 (1974). [PubMed] [Google Scholar]
- 28.Hochberg Y., and Tamhane A.C.: Multiple comparison procedures. New York, Wiley, 1987. [Google Scholar]
- 29.Holm S.: A simple sequentially rejective multiple test procedure. Scand. J. Stat. 6: 65–70 (1979). [Google Scholar]
- 30.McArdle W.D., Katch F.I., and Katch V.L.: Exercise Physiology: Energy, Nutrition, and Human Performance, 4th ed. Baltimore, Md.: Williams & Wilkins, 1996. [Google Scholar]
- 31.American College of Sports Medicine : ACSM's Guidelines Exercise Testing and Prescription, 5th ed. Philadelphia, Pa.: Lippincott Williams & Wilkins, 2006. [Google Scholar]
- 32.Murray M., Grant J., Bryce E., Chilton p., and Forrester L.: Facial protective equipment, personnel, and pandemics: Impact of the pandemic (H1N1) 2009 virus on personnel and use of facial protective equipment. Infect. Control Hosp. Epidemiol. 31(10): 1011–1016 (2010). [DOI] [PubMed] [Google Scholar]
- 33.Radonovich L.J., Yanke R., Cheng J., and Bender B.: Diminished speech intelligibility associated with certain types of respirators worn by healthcare workers. J. Occup. Environ. Hyg. 7: 63–70 (2009). [DOI] [PubMed] [Google Scholar]
- 34.Thomas F., Allen C., Butts W., Rhoades C., Brandon C., and Handrahan D.: Does wearing a surgical facemask or N95-respirator impair radio communication? Air Med. J. 30(2): 97–102 (2011). [DOI] [PubMed] [Google Scholar]
- 35.Harber P., Santiago S., Bansal S., Liu Y., Yun D., and Wu S.: Respirator physiologic impact in persons with mild respiratory disease. J. Occup. Environ. Med. 52(2): 155–162 (2010). [DOI] [PubMed] [Google Scholar]
- 36.Harber P., Yun D., Santiago S., Bansal S., and Liu Y.: Respirator impact on work task performance. J. Occup. Environ. Med. 53(1): 22–26 (2011). [DOI] [PubMed] [Google Scholar]


