Abstract
Adolescents in Sub-Saharan Africa are at disproportionately high risk for intimate partner violence (IPV) and human immune-deficiency virus (HIV). The interconnected risks for IPV and HIV present the opportunity for interventions to concurrently seek to reduce violence and sexual risk behaviors among young people. Accordingly, the present systematic review evaluates interventions that concomitantly address IPV and HIV risk among adolescents in Sub-Saharan Africa. We systematically reviewed electronic databases for studies meeting the following criteria: use of randomized control trials (RCT) or quasi-RCT in Sub-Saharan African countries; inclusion of adolescents aged 13–18 years; use of a comparison group (wait-listed, designated to a comparative treatment, or treatment as usual); and incorporation of IPV and HIV outcome assessments. Results suggested that eight studies have utilized rigorous research methodologies to evaluate integrated IPV/HIV interventions, however few have targeted adolescents. The eight studies meeting inclusion criteria indicate that current research on IPV/HIV is conducted with rigorous study designs among target populations with high IPV/HIV risk, using gender-specific risk reduction activities. The studies report promising results for IPV/HIV risk reduction. Our findings indicate there is also the need for consistent application of valid and reliable outcome measurements of IPV and HIV risk. Additional research is needed to identify best practices for reducing IPV and HIV incidence among vulnerable adolescent populations in Sub-Saharan Africa.
Keywords: Intimate partner violence, HIV, adolescents, Sub-Saharan Africa
Sub-Saharan Africa is disproportionately affected by the global burdens of intimate partner violence (IPV) and human immune-deficiency virus (HIV). According to the World Health Organization, IPV is defined as a subset of gender-based violence (GBV) in which acts or threats of physical, sexual, and emotional violence are perpetrated by a current or former intimate partner (World Health Organization, 2013). In the African region, 36.6% of women reported experience of physical or sexual intimate partner violence, compared to 23.2% in high income regions (World Health Organization, 2013). Sub-Saharan African countries also account for 64% of all new HIV infections (UNAIDS, 2017). Further, an estimated 25.5 million adults and children are living with HIV in Sub-Saharan Africa and ten countries alone are home to 80% of the global population of individuals living HIV (UNAIDS, 2014; UNAIDS, 2017). The high prevalence rates of IPV and HIV in Sub-Saharan African underscore the importance of intervening to address these dual public health concerns.
In Sub-Saharan Africa, adolescence marks a period of increased risk for both IPV and HIV (Flisher, Myer, Mèrais, Lombard, & Reddy, 2007; UNAIDS, 2017). One study among South African adolescents reported that 49.8% of the boys and 52.4% of the girls in Grades 9–12 had experienced or perpetrated physical violence in a dating relationship (Swart, Stevens, & Ricardo, 2002). Among the global population of adolescents living with HIV, nearly 85% live in Sub-Saharan Africa (UNICEF, 2017). There are several potential reasons why adolescents show elevated risk for both IPV and HIV. Sexual debut is common in adolescence, and can be associated with increased risk for negative health outcomes such as acquisition of sexually transmitted infections (STIs), unintended pregnancies, and sexual violence (Kotchick, Shaffer, Forehand, & Miller, 2001). In fact, by the age of 16, 50% or more of South African and Tanzanian youths have become sexually active (Eaton, Flisher, & Aarø, 2003; Munguti et al., 1997). High rates of transactional sex among young women 12–19 years of age in Sub-Saharan Africa may increase risk for both IPV and HIV due to power dynamics and condom negotiation within relationships (Dunkle et al., 2004a; Kaufman & Stavrou, 2002). Additionally, high rates of engagement in age-disparate sexual relationships may also increase risk for both IPV and HIV (Evan et al., 2016). A systematic review by Eaton et al. (2003) found that high rates of force, coercion, and male-dominated sexual relationships may also exacerbate HIV risk among South African adolescents (Eaton et al., 2003).
Research emerging from Sub-Saharan Africa suggests that adolescents and particularly young women who experience IPV are at higher risk for HIV and other STIs (Jewkes, Dunkle, Nduna, & Shai, 2010; Teitelman et al., 2016). Experiences of IPV can increase risk for HIV through several pathways (Dunkle et al., 2004b; Dunkle & Decker, 2013; Garcia-Moreno & Watts, 2000; Jewkes et al., 2010; Li et al., 2014; Maman et al., 2002; van der Straten et al., 1998). First, experiences of sexual victimization among women often result in tearing of sexual tissue, which can increase susceptibility to HIV infection (Kim, Martin, & Denny, 2003). Other studies suggest that power inequality in violent dating relationships is negatively associated with women’s ability to negotiate condom use and refuse unwanted sexual activity (Garcia-Moreno & Watts, 2000; Pettifor, Measham, Rees, & Padian, 2004). Research also demonstrates an association between IPV and increased engagement in sexual risk behavior among women, including engaging in sexual activity with multiple sexual partners, substance use, and transactional sex (Dunkle & Decker, 2013). HIV positive women may also face increased risk of IPV as a result of HIV status disclosure, and some women may choose not to disclose their status to sexual partners due to fear of violence (Maman, Mbwambo, Hogan, Kilonzo, & Sweat, 2001).
Currently, several reviews document the efficacy of IPV and HIV interventions for adults in Sub-Saharan Africa. For example, an evaluation of IPV prevention strategies in Sub-Saharan Africa and other low- and middle-income countries found that structural interventions are potentially effective in reducing male perpetration of IPV (Bourey, Williams, Bernstein, & Stephenson, 2015). Another review of IPV interventions in Sub-Saharan Africa reported promising results from community-based interventions that aim to change gender attitudes and the community’s tolerance of IPV (McCloskey, Boonzaier, Steinbrenner, & Hunter, 2016). Problematically, both of these recent reviews lacked attention to the specific inclusion of adolescents in these interventions; a particularly high risk group. One systemic review assessed IPV interventions targeting adolescents, but did not focus specifically on Sub-Saharan Africa (De Koker, Mathews, Zuch, Bastien, & Mason-Jones, 2014).
Reviews of HIV preventive interventions specifically targeting adolescents in Sub-Saharan Africa suggest various intervention strategies and designs currently demonstrate mixed results (Harrison, Newell, Imrie, & Hoddinott, 2010; Michielsen, Temmerman, & Van Rossem, 2013; Paul-Ebhohimhen, Poobalan, & van Teijlingen, 2008). For example, Harrison et al. (2010) reviewed eight HIV interventions for South African adolescents and found that prevention strategies which targeted social and structural factors for HIV risk, as well as causal HIV risk pathways specific to the region, had the biggest impact of sexual risk behavior reduction. Michielsen et al. (2013) reviewed HIV prevention among adolescents in Sub-Saharan Africa and attributed the limited effectiveness of current strategies to factors related to the intervention design, implementation, and evaluation. Paul-Ebhohimhen’s et al. (2008) review suggests that school-based HIV prevention have a greater statistically significant impact on outcomes related to HIV knowledge and attitudes than outcomes related to behavior change.
Taken together, whereas previous reviews of the literature document the efficacy of interventions targeting adults at risk for either IPV or HIV in Sub-Saharan Africa, research to date is lacking on the efficacy of interventions that concurrently address IPV and HIV. In fact, to our knowledge, the only review evaluating interventions addressing both HIV and IPV risk in Sub-Saharan Africa is specific to identifying interventions that could be led by nurses in health care settings (Anderson et al., 2013). No studies to date have reviewed the efficacy of interventions that concurrently target IPV and HIV risk among adolescents in Sub-Saharan Africa. Adolescence offers a crucial window of opportunity for reducing IPV and HIV incidence by preventing or curtailing problematic relationship (De Koker et al., 2014) and sexual behaviors (Pedlow & Carey, 2004) to preclude continuing patterns of violence and sexual risk into adulthood. Given the prevalence of IPV and HIV among adolescents, and the potential for interventions to address these intersecting public health concerns concurrently, the present systematic review sought to evaluate the current evidence base on interventions that concurrently target the prevention of HIV and IPV for adolescents in Sub-Saharan Africa.
Methods
Search Strategy
We used a Boolean search strategy to find studies in three electronic databases (PubMed, Embase, PsychInfo, CINAHL). The following search terms were expanded and modified, if necessary, for each electronic database: HIV, intimate partner violence, adolescent, and Sub-Saharan Africa. The search terms for each database can be found in the appended search protocol (see Appendix A).
Inclusion Criteria
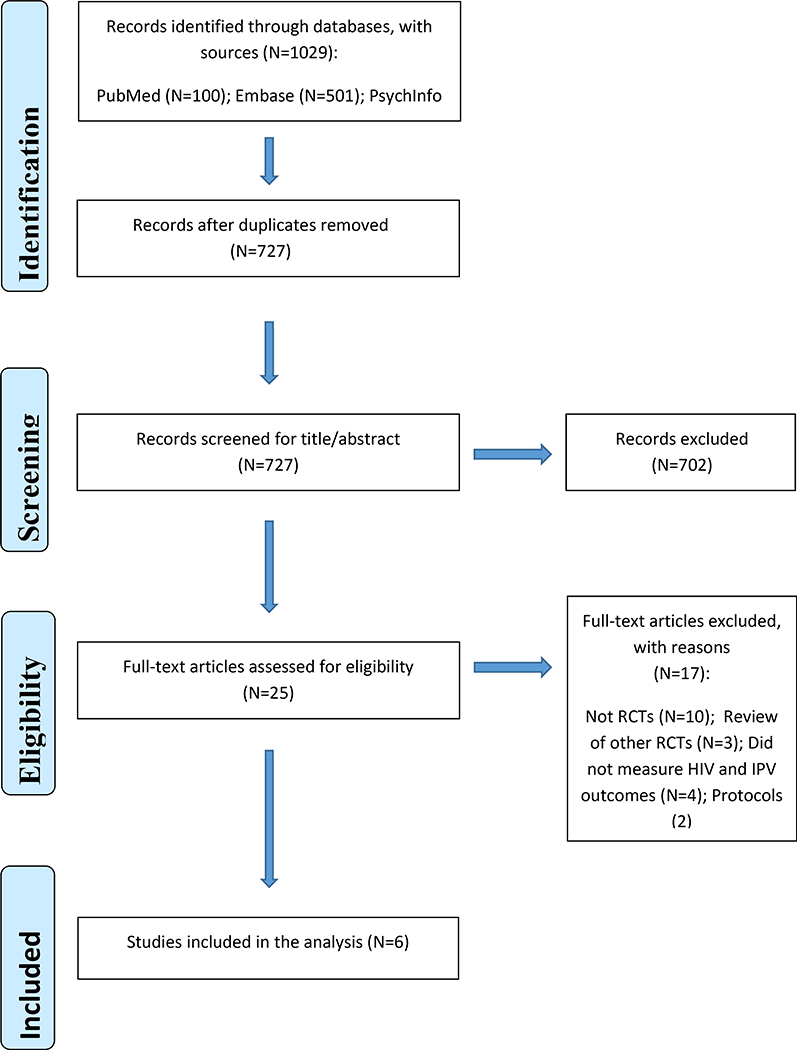
Studies were included in the systematic review if they (a) sampled people living in Sub-Saharan African countries, (b) utilized a randomized control trial (RCT) or quasi-RCT design, (c) targeted both IPV and HIV as primary outcomes for either prevention or risk reduction, (d) included a control or comparison group that received standard care (including treatment as usual/no intervention), a wait-list control group, or comparative treatment intervention, and (e) targeted, or included, adolescent participants 13 to 18 years of age (inclusive). Studies were excluded from the systematic review if the intervention (a) did not measure both IPV and HIV as outcomes or (b) lacked a comparison group. Because we were interested in reviewing all past and currently existing IPV/HIV interventions, we did not confine our search to a pre-defined publication period. The electronic databases were searched during October 2017 and yielded 727 unique reports. A preliminary review resulted in the exclusion of 702 articles as their titles or abstracts did not fulfill the inclusion criteria. After full-text review of the remaining 25 articles, 17 were excluded from analysis because they did not (a) provide an integrated IPV/HIV prevention or risk reduction intervention, (b) measure both IPV and HIV, or (c) include a control or comparison group. Figure 1 presents a PRISMA diagram depicting a graphical representation of the study selection process. Specific details were extracted from the included studies: study design, sample characteristics, format and dosage of activities, assessments, results, and follow-up times. When key study information was not provided, we contacted the authors directly for clarification. Study information was then assessed using thematic analysis with the findings presented below.
Figure 1.
Flowchart for Study Selection
Results
Overview
Eight studies that met inclusion criteria were included in the systematic review. These studies describe interventions targeting prevention or risk reduction for both IPV and HIV among adolescents in Sub-Saharan Africa. Table 1 provides details for these eight studies including a description of study samples and intervention elements. The eight studies were all published in the past 12 years including the IMAGE study (Pronyk et al., 2006), Stepping Stones (Jewkes et al., 2008), Kalichman et al.’s field trial (2009), SASA! (Abramsky et al., 2014), Safe Homes and Respect for Everyone (SHARE) (Wagman et al., 2015), PREPARE (Mathews et al., 2016), Vijana Vijiweni II (Kajula et al., 2016), and Stepping Stones and Creating Futures (Gibbs et al., 2017).
Table 1.
Integrated IPV/HIV interventions targeting or including adolescents in Sub-Saharan Africa
| Study | Location | Participant Characteristics | Intervention Description | Study Characteristics | Results |
|---|---|---|---|---|---|
| Abramsky et al. 2014 | Rubaga and Makindye Divisons, Kampala, Uganda. |
2,532 men and women at F/U Avg age men: 27 years; avg age women:28 yrs | 4 yrs, 5 mo. 1. No specific dosage of community mobilization activities: advocacy and media on local media channels, communication materials, training. 2. CG wait-listed |
Pair-matched CRCT; 4-year F/U survey. IPV outcomes: a priori; social acceptability IPV; women’s PYr exp. IPV. HIV outcome: SRBs | At 4-yr F/U, lower acceptance of IPV among women; higher acceptance of a woman refusing sex among women. Decreased past year sexual concurrency among men. |
| Jewkes et al. 2008 | Eastern Cape province of South Africa | 2,776 men and women 16–23 years old. | 6–8 wks, 1. Thirteen 1-hr sessions in single-sex groups (role play, drama, critical reflection); 3 meetings; one community meeting; 2. CG 3-hr session on HIV risk. |
CRCT; F/U at 12- mo. and 24- mo. F/U rate 75% for men and women at 12 mo., 73% of women and 69% of men at 24 mo. IPV outcome: IPV incidence questionnaire. HIV: biological outcomes; SRBs. | Intervention was not associated with lower HIV acquisition; associated with lower HISV-2. No significant effect on reported IPV perp among men. |
| Kalichman et al. 2009 | Cape Town, South Africa | 475 men. Avg age 30.2 years (standard deviation 9.5). | 1 wk 1. 5 small group sessions (skill building, goal setting, risk identification, condom use skill building, sexual communication training) 2. CG: 3-hour HIV/ alcohol risk session; no IPV component. |
Quasi-experimental intervention trial; F/U at 1-mo, 3-mo, and 6-mo. Participant retention greater than 90%. IPV outcome: 7-item domestic violence scale; past mo. IPV perp. HIV: 11-item HIV knowledge test; 4-item stigma scale; SRB intent. | Increased discussion of condoms with partner at 1-month F/U; increased reporting of HIV testing at 3-mo F/U; increased intention to reduce SRBs, decreased reporting of past-mo. physical IPV perp at 6-mo F/U. |
| Mathews et al. 2016 | Western Cape, South Africa | 3,451 Grade 8 participants. Avg age 13 years. | 21 wks 1. Weekly 1–1.5 hr after-school sessions (interactive and skill based group sessions); weekly access to PREPARE school nurse; two-day training for school safety teams. 2. CG: attended school as usual |
CRCT; F/U at 6- mo. and 12- months. 94% retention at 6 mo. and 88% retention at 12 mo. IPV outcome: IPV exp and perp past 6 months. HIV: SRBs | No significant association between intervention and SRBs at 6-mo. or 12 mo. F/U. At 12 mo. F/U, participants less likely to report IPV exp. |
| Pronyk et al. 2006 | Rural Limpopo province of South Africa | 6,576 men and women. 860 women in Cohort 1 exposed to intervention. Avg age Cohort 1: 41 years. Cohort 2: persons 14–35 yrs old sleeping in Cohort 1 household; Cohort 3: 14–35 de jure residents of Cohort 1 households. | 12–15 mo. 1. Cohort 1: Microfinance group meetings every 2 wks over 10 or 20 wk cycles; 1-hr gender and HIV training session every 2 wks; Community mobilization for 6–9 mo. following training. 2. CG wait-listed |
CRCT; F/U at 2 yrs (Cohort 1 and Cohort 2) and 3 years (Cohort 3). At 2 yr F/U, study retained 90% of intervention cohort 1 and 84% of CG cohort 1. IPV outcome: PYr IPV exp. HIV: biological outcome; SRBs | 2-yr F/U Cohort 1 less likely to report PYr IPV exp. Intervention not associated with decreased SRBs or decreased HIV acquisition in Cohorts 2 and 3. |
| Wagman et al. 2015 | Rakai, Uganda | 11,448 individuals 15–49 yrs (no avg age provided) | 4 years No specific dosage 1. Community mobilization activities (activism, campaigns, newsletters, peer groups, support counseling). 2. CG: routine HIV prevention and treatment services. |
CRCT; F/U at 16 mo. and 35 mo. after baseline. Retention 57% at 35-month F/U. IPV outcome: Conflict Tactic Scales PYr exp and perp. HIV: biological outcome; SRBs | Intervention associated with decreased exp of physical and sexual IPV at 35-mo. follow up. SHARE associated with decreased HIV acquisition. |
Average = avg; Cluster randomized control trial = CRCT; Comparison Group = CG; Experience = exp; Follow up = F/U; Hour = hr; Month = mo.; Past year = PYr; Perpetration = perp; Sexual risk behaviors = SRBs; Weeks = Wk; Year(s) =Yr(s); World Health Organization Violence Against Women = WHO VAW
Study Design
Seven of the eight studies used a cluster RCT design (Abramsky et al., 2014; Gibbs et al., 2017; Jewkes et al. 2008; Kajula et al. 2016; Mathews et al. 2016; Pronyk et al., 2006; Wagman et al., 2015) and one study utilized a quasi-experimental trial design (Kalichman et al., 2009). Seven studies implemented fully powered trials to examine the efficacy of interventions (Abramsky et al., 2014; Jewkes et al., 2008; Kajula et al., 2016; Kalichman et al., 2009; Mathews et al., 2016; Pronyk et al., 2006; Wagman et al., 2015) and one anticipated a fully powered trial pending completion of follow-up assessments.
Geography
Five studies took place in South Africa (Gibbs et al. 2017; Jewkes et al. 2008, Kalichman et al. 2009; Mathews et al. 2016; Pronyk et al. 2006), two studies were implemented in Uganda (Abramsky et al. 2014; Wagman et al. 2015), and one was conducted in Tanzania (Kajula et al. 2016). No studies from western or central Africa were identified.
Target Population
The target populations varied considerably. Importantly, only two of the eight studies included in our review specifically targeted youths or young adults (Jewkes et al., 2008; Mathews et al., 2016) The age range criteria in the youth-tailored interventions were defined as 16–23 years (Jewkes et al., 2008) and Grade 8 adolescents (Mathews et al., 2016). Six of the eight studies included, but did not target, adolescents, with inclusion criteria for age ranges defined as 15 years and older (Kajula et al., 2016), 15–49 years (Wagman et al., 2015), 18–30 years (Gibbs et al., 2017), 18–49 years (Abramsky et al., 2014), and 18 years and older (S. Kalichman, personal communication, March 22, 2018). One study did not provide age specifications for direct recipients of the intervention, but gathered data on intervention impact from two cohorts of participant household members 14–35 years old (Pronyk et al., 2006).
Among the six studies that did not specifically target adolescents or students, participants were recruited based on their identification as general community members (Abramsky et al., 2014; Kalichman et al., 2009), residence in informal settlements (Gibbs et al., 2017), membership in “camps” or social networks (Kajula et al., 2016), enrollment in existing cohort studies (Wagman et al., 2015), or loan eligibility (Pronyk et al., 2006). Among the eight studies, two exclusively recruited male participants (Kajula et al., 2016; Kalichman et al., 2009) and one delivered the intervention exclusively to female participants, but gathered additional outcome data from male and female community members (Pronyk et al., 2006).
Control Condition
Half of the studies’ used control groups that were wait-listed to receive the intervention after the trial was complete (Abramsky et al. 2014, Gibbs et al. 2017; Kajula et al. 2016; Pronyk et al. 2006), two control groups received routine health services (Wagman et al. 2015, Mathews et al. 2016), and two control groups received one 3-hour session on HIV risk, without mention of IPV (Jewkes et al. 2008; Kalichman et al. 2009).
Intervention Dose and Format
The eight studies implemented the intervention activities in group settings. The interventions typically prescribed lengths for each session, ranging from 1-hour (Mathews et al., 2016; Pronyk et al., 2006) to 3-hours (Gibbs et al., 2017; Jewkes et al., 2008; Kalichman et al., 2009). Three studies did not include or prescribe specific lengths for intervention activities (Abramsky et al., 2014; Kajula et al., 2016; Wagman et al., 2015). The dosages of the interventions sessions varied considerably. Kalichman et al. (2009) implemented five 3-hour sessions over the course of five consecutive days. Other studies implemented intervention activities on a weekly or biweekly basis over the course of six to eight weeks (Jewkes et al., 2008; Gibbs et al., 2017), 21 weeks (Mathews et al., 2016), or six to nine months (Pronyk et al., 2006; Kajula et al., 2016). Abramsky et al. (2014) and Wagman et al. (2015) implemented community mobilization activities without pre-specified dosage over the course of roughly four years. The intervention settings varied between and within studies. When provided, intervention locations included schools (Mathews et al., 2016), HIV clinics (Wagman et al., 2015), local media channels (Abramsky et al., 2014), microfinance loan centers (Pronyk et al., 2006), and community settings (Abramsky et al. 2014; Kalichman et al., 2009; Wagman et al., 2015).
Intervention Approaches
Five of the eight studies aimed to reduce perpetration and experience of IPV (Abramsky et al., 2014; Gibbs et al., 2017; Jewkes et al., 2008; Mathews et al., 2016; Wagman et al., 2015). Two of the studies exclusively targeted IPV perpetration (Kajula et al., 2016; Kalichman et al., 2009) and one study focused specifically on reducing experience of IPV (Pronyk et al, 2006). HIV risk was predominantly operationalized as decreased condom use and concurrent sexual partners (Abramsky et al., 2014; Gibbs et al., 2017; Jewkes et al., 2008; Kajula et al., 2016; Kalichman et al., Mathews et al., 2016; Pronyk et al., 2006; Wagman et al., 2015).
Four studies implemented structural interventions to target the social and economic environments influencing HIV and IPV risk. Intervention activities included microfinance programs and community mobilization events to address cultural norms towards violence (Abramsky et al. 2014; Kajula et al. 2016; Pronyk et al. 2006; Wagman et al. 2015). The other studies can be described as multi-component interventions in which group-based activities target modifiable individual behaviors, structural level causes of HIV and IPV risk, and attitudes towards gender equality. The multi-component intervention activities focused on modification of individual risk behaviors, addressed beliefs relating to gender equality, and built sexual health skills (Gibbs et al. 2017; Jewkes et al. 2008; Kalichman et al. 2009; Mathews et al. 2016). The eight studies are grouped by intervention approach and described below:
Structural interventions
SASA! is a community-level mobilization intervention targeting intimate partner violence and sexual-risk behavior reduction among individuals 18–49 years of age living in Kampala, Uganda (Abramsky et al. 2014). Participants in communities receiving the intervention were exposed to various activities led by trained Community Activists (CAs), including group discussions, public events, trainings, and films. The intervention activities aimed to reduce social acceptability of IPV among community members to reduce perpetration and victimization, as well as sexual risk behavior reduction addressing the increased risk of HIV associated with concurrent sexual partners among male participants. The intervention did not have a prescribed dosage of intervention exposure, but supported the CAs progression through the program’s phases and strategies. More than 11,000 activities were implemented during the duration of the study. The control group was wait-listed for the intervention. The average age of men and women in the intervention group and control groups fell within the range of 27–29 years. The study did not report the proportion of participants 18 years of age. Comparison of baseline and follow-up data demonstrated that the intervention was associated with reduced social acceptance of IPV among women (aRR 0.54, 95% CI 0.38–0.79), and increased acceptance among women that women can refuse sex (aRR 1.28, 95% CI 1.07–1.52). The intervention was also associated with decreased sexual risk behaviors, measured by self-reports of concurrent sexual partners among non-polygamous men (aRR 0.57, 95% CI 0.36–0.91).
Vijana Vijiweni II is a combined microfinance and health leadership training on STI incidence and IPV perpetration among male participants (N = 1,258) belonging to 60 “camps” or social networks in Dar es Salaam, Tanzania (Kajula et al., 2016). Participants are at least 15 years of age and have belonged to a camp for at least 3 months prior to the intervention launch. The study did not report the proportion of participants 15–18 years old or the overall average age of participants. Men in the intervention group participate in a two-year microfinance program which promoted business skill training through individual loan application, weekly loan group meetings, and ensuing applications for larger loans upon successful group repayment. The peer leadership component of the intervention involved training nominated camp leaders to leader five weekly discussions among camp members on the topics of STI risk reduction, condom use, multiple sexual partners, effective communication skills, and reducing perpetration of IPV. Men in the control group are wait-listed for the intervention. Results from Vijana Vijiweni II are not yet available. The study will measure biologically verified STI incidence, attitudes and gender norms, as well as self-reported IPV perpetration to assess the efficacy of the intervention. Follow-up assessments will measure behavioral outcomes at 12-months and behavioral and biological outcomes 30-months post-intervention.
IMAGE is a combined microfinance and gender training intervention targeting women in the Limpopo province of South Africa (Pronyk et al., 2006). The intervention and control villages each contained three cohorts to study the direct and indirect impact of the intervention: eligible female loan recipients (average age 41 years), 14–35 years-old household members of the loan recipients, and randomly sampled community members. The total study population was 6,576. The study did not report the proportion of participants 14–18 years of age, but reported the youngest participants’ age in cohort 2 (16.9 years) and cohort 3 (17.1 years). The women in cohort one directly received loans through a group lending model. Loan groups held a total of ten 1-hour meetings every other week for support, discussion of credit, business assessments, and repayment. Within the 1-hour loan meetings, the intervention delivered structured trainings to explore topics of gender, IPV, HIV, and relationship skill building. Participants in the control villages were wait-listed to receive the intervention. At follow up, the study assessed past-year experience of IPV in cohort one, unprotected sex with non-spousal partners among cohort two participants, and HIV incidence in cohort three using lab-based diagnoses. IMAGE was associated with decreased experience of IPV in cohort 1 (aRR 0.45, 95% CI 0.23–0.91). The intervention was not associated with increased protection during sex among cohort two participants or HIV incidence in cohort three.
SHARE addressed IPV and HIV incidence in Rakai, Uganda (Wagman et al., 2015) using community mobilization strategies and behavioral IPV risk reduction intervention among women seeking HIV services. Study participants were 15–49 year-old individuals (N = 11,448) recruited from the existing Rakai Community Cohort Study. Among the study population, 10% (N=1,167) of participants were 15–19 years of age. Individuals in the intervention group were exposed to a range of intervention activities, including marches, distribution of learning activities, posters, newsletters, and men’s and boys’ IPV and HIV risk prevention sessions over the course of the four-year study. The study did not provide information on the dosage or length of intervention activities. The aim of the intervention activities was to change social attitudes regarding IPV and reduce perpetration and experience of IPV, while concurrently addressing various sexual risk behaviors related to multiple sexual partners, non-martial sexual partners, condom use, and alcohol use before sexual activity. Women in the intervention group seeking HIV services were also given a brief intervention to reduce the risk of IPV related to HIV disclosure. The control group received standard HIV services offered through the ongoing cohort study, which included HIV prevention and treatment, HIV testing, counseling, and care referral. Analysis of self-reported experience and perpetration of IPV found that the intervention was associated with decreased incidence of both physical IPV (adjusted prevalence risk ratio 0.79, 95% CI 0.67–0.92) and sexual IPV (aPRR 0.80, 95% CI 0.67–0.97) in the previous year. The intervention was neither significantly associated with decreased incidence of emotional IPV nor self-reported IPV perpetration among male participants. At the 35-month follow up, lab-based diagnoses demonstrated a negative association between exposure to SHARE and HIV incidence (adjusted incidence rate ratio 0.67, 95% CI 0.46–0.97).
Multi-component interventions
PREPARE is a school-based intervention designed to reduce experience and perpetration of IPV, increase condom use, and delay sexual debut among Grade 8 adolescents (N = 3,451) in the Western Cape Province, South Africa (Mathews et al., 2016). Over the course of 21 weeks, participants (average age 13) in the intervention group attended weekly 1–1.5 hour educational sessions facilitated group discussion of IPV, relationships, sexual decision making, gender and power inequity, communication skills, and sustainable community change. The school health service included free weekly access to a PREPARE nurse for “health checks,” screenings, and referrals related to participants’ sexual health. The school safety program educated school community members about IPV prevalence, laws related to sexual violence, and school safety planning. Participants in the control group attended school and did not receive any additional programming. Results from the 12-month follow-up surveys found that PREPARE was not significantly associated with delayed sexual debut, condom use, or number of sexual partners. The intervention was associated with decreased report of experience of IPV (OR 0.77, 95% CI 0.61–0.99).
The field trial conducted by Kalichman et al. (2009) recruited male participants 18 years and older (N = 475) from two townships in Cape Town, South Africa to compare the effects of a trial IPV/HIV intervention with an HIV/alcohol intervention on IPV perpetration and risk of STI. Over the course of one week, men in the intervention group (average age 30.2 years, standard deviation 9.5 years) participated in five 3-hour integrated GBV and HIV risk-reduction sessions. The study did not provide details on the proportion of participants 18 years of age. The intervention activities included exploration of GBV/ HIV risk- identification and reduction through condom use skill building, behavioral role play with group feedback and discussion with South Africa media clips for context, and advocacy skill building. The control group received one three-hour session on HIV/alcohol risk reduction that did not include GBV or IPV intervention material. The study found that the field trial was not significantly associated with increased condom use, decreased number of sexual partners, or decreased occurrence of unprotected sex. At the six-month follow-up, the field trial was associated with decreased perpetration of past-month physical IPV (OR 0.3, 95% CI 0.2–0.4). Participants who at baseline reported they had lost their temper with a woman, men in the intervention group were less likely to report losing their temper compared to men in the control group at six-month follow-up (OR 0.5, 95% CI 0.3–0.8).
Stepping Stones is a participatory intervention designed to reduce HIV, herpes simplex type 2 (HSV-2) among young men and women 15–26 years old (N = 2,776) living in the Eastern Cape province of South Africa (Jewkes et al., 2008). Over the course of six to eight weeks, participants in the intervention group attended 13 three-hour long single-sex group meetings, three mixed-sex peer meetings, and one community meeting. Intervention activities were both group and individual based, including a variety of participatory role play, drama, and critical reflection exercises to facilitate exploration of gender equity and healthy relationships. The study designed the activities to reduce experience and perpetration of IPV, as well as sexual behaviors that increase risk of STI. The study delivered a three-hour session on safe sex, condoms, and HIV to the control group. Stepping Stones, while not associated with reduced HIV incidence, was able to demonstrate 33% reduction in Type 2 herpes simplex virus (aIRR 0.67, 95% CI 0.46–0.97). The study was also associated with a lower proportion of male participants reporting IPV perpetration at two-year follow-up in the intervention group compared to the control (aOR 0.62, 95% CI 0.38–1.01).
Stepping Stones and Creating Futures combines the gender transformative approach of Stepping Stones with an economic empowerment intervention, Creating Futures, to assess its efficacy in reducing HIV and IPV (Gibbs et al., 2017). The study population was comprised of 18–30 year-old men and women living in informal settlements in the eThekwini Municipality, South Africa (N = 1,357). The average age of participants was 23 years; the study did not include the proportion of participants 18 years of age. The intervention’s adapted version of Stepping Stones included ten three-hour single-sex group sessions over the course of 6–8 weeks. Drama, role play, and critical reflection exercises were used to facilitate discussion of behavioral influences, relationships, safe sex practices, HIV, GBV, and communication skills. Activities aimed to reduce experience and perpetration of IPV, as well as HIV risk behaviors including concurrent sexual partners and transactional sex. The study notes an important departure from previous editions of Stepping Stones, including the decision to emphasize sexual health and GBV factors specific to a younger study population. Following each Stepping Stones session was a 3-hour Creating Futures session, which aimed to help participants evaluate economic strategies that utilized human, financial, natural, physical, and forms of capital that may be available to them. The control group is wait-listed for the intervention. Study results are pending 24-month follow-up data collection of self-reported experience of physical IPV, sexual IPV, severe IPV, controlling behavior, and past-month earnings.
Discussion
For this systematic review, we examined the geographic distribution, study design, and target population of eight interventions designed to reduce IPV and HIV risk in Sub-Saharan African settings. Even though the field of integrated IPV/HIV prevention in Sub-Saharan Africa is in its nascent stages, it is encouraging that eight interventions have been conducted with rigorous study designs. Overall, the results of this review are encouraging with respect to the efficacy of interventions to concomitantly prevent IPV and HIV. For public health practitioners in the field of adolescent IPV and HIV prevention, our findings suggest that integrated IPV/HIV interventions may be an effective sexual risk and violence prevention strategy among adolescents in Sub-Saharan Africa. However, the low number of interventions specifically targeting adolescents highlights a significant opportunity for future research to develop age-tailored interventions for young people facing the dual risk of IPV and HIV in Sub-Saharan Africa. We have identified some of key strengths and gaps in the literature below. A summary of core implications of the current review for practice, policy, and research is provided in Table 2.
Table 2.
Implications of the Review for Practice, Policy, and Research
| Area of Impact | Implications of the Review |
|---|---|
| Practice | • The findings of this review suggest that integrated IPV/HIV interventions show promise as a sexual risk and violence prevention strategy among adolescents in Sub-Saharan Africa. |
| Policy | • Policy makers interested in preventing HIV and IPV should be aware of the dual risk pathways, and that policies in support of risk reduction in one may affect rates of the other (and vice versa). • HIV and IPV risk reduction policy should address the mechanisms by which gender and economic inequities affect rates of sexual risk behaviors and violence against women. |
| Research | • Targeting adolescents in integrated IPV/HIV interventions would provide further evidence regarding effective age-specific strategies for sexual risk behavior reduction and violence prevention. • Research on integrated IPV/HIV interventions would benefit from consistent biological outcomes and standardized IPV outcomes to improve rigorous, comparable measurement across studies. • Research examining concurrent IPV/HIV prevention should examine specific gender-targeted approaches to increase men and boys’ involvement in promoting and normalizing gender equality. |
Geographic distribution of the studies
Findings indicate that integrated IPV/HIV interventions in Sub-Saharan Africa have been rigorously evaluated in regions of Sub-Saharan Africa with the greatest burden of IPV and HIV. The eight studies were conducted in eastern and southern African countries, in which 19.4 million adults and children are living with HIV, as compared to 6.1 million in western and central African countries (UNAIDS, 2017). Southern and eastern Sub-Saharan Africa also report high IPV prevalence, with lifetime prevalence of physical or sexual abuse as high as 90% in this region (UN, 2012). In South Africa, where five of the eight interventions took place, the lifetime prevalence of physical and sexual abuse is 49% (UN, 2012).
Our findings also point to a regional gap in the literature, as no integrated IPV/HIV trials emerged from western or central African countries. This finding supports the need for increased HIV/AIDS prevention and intervention efforts in western and central African countries, where HIV prevalence rates, although lower than central and southern African countries, are not met with adequate treatment provision and transmission prevention (Djomand et al., 2014; Médecins Sans Frontières, 2016). Previous studies in West Africa have found high prevalence rates and social acceptance of IPV, including experience of dating violence among university aged women and IPV among women living with HIV/AIDS (Olorunsaiye et al., 2017; Olowookere et al., 2015; Umana, Fawole, & Adeoye, 2014; Diallo & Voia, 2016). Considering the high IPV and HIV prevalence in Sub-Saharan Africa, it is surprising that not more than eight studies fulfilling inclusion criteria emerged in our search. We recommend that future research assess the efficacy of integrated IPV/HIV interventions in all regions of Sub-Saharan Africa, as the documented burden of both IPV and HIV demonstrate the pressing need for evidence based interventions.
Study Design Elements
The results of our review demonstrate that integrated IPV/HIV interventions in Sub-Saharan Africa have been implemented with rigorous research methods. The RCTs large sample sizes are a key strength among the studies, indicating that the majority of current research is producing meaningful results through fully powered trials. The researchers reported unbiased allocation of clusters of participants to receive the intervention or comparative treatment, which can help minimize the potential for contamination between the two groups (Torgerson, 2001). The included studies’ control groups represented a range of comparison conditions, which lent varying strength to the studies’ results. Importantly, three studies compared integrated IPV/HIV interventions with HIV-focused services or risk reduction trainings, which demonstrates growing interest in the potential for combined IPV/HIV prevention to reduce a number of related sexual and interpersonal risk behaviors.
Target Population
Our results are encouraging with respect to the number of studies that included, albeit did not always specifically target adolescents. For example, although SHARE and Vijana Vijiweni II included participants as young as 15 years old, the analytic samples of these studies included older adult participants. Stepping Stones and PREPARE targeted early and late adolescence, respectively (Jewkes et al., 2008; Kajula et al., 2016; Mathews et al., 2016; Wagman et al., 2008); only PREPARE’s study sample was entirely within 13–18 years old. The studies’ inclusion criteria for participant ages varied considerably, making it difficult to compare the effect of the interventions across same age adolescents.
Our finding that participants in IPV/HIV interventions are generally older coincides with study populations in which there is evidence of current romantic relationships, cohabitation, IPV experience, IPV perpetration, concurrent sexual partners, and inconsistent condom use at baseline. Even among the youngest participants included in PREPARE’s study, at baseline 22% of the Grade 8 participants reported sexual debut, 45% had experienced IPV, and more than a quarter had perpetrated IPV (Mathews et al., 2016). The baseline findings of the eight studies indicate the majority of current research on integrated IPV/HIV examines secondary prevention intervention strategies among populations with pre-existing risk or incidence of IPV and HIV.
Addressing gender norms and identifying sexual risk behaviors during adolescence is crucial for primary prevention of both IPV and HIV (McCloskey et al., 2016; Mwale & Muula, 2017). The wide range of included ages among many of the studies limits the ability of intervention activities to include appropriate developmental tailoring, particularly among adolescent participants who may not have relationship or sexual experience. This indicates an important gap in the current research. We recommend developmentally appropriate interventions that tailor all aspects of content and activities to the target population based on specific factors, including risk behavior, gender, and, importantly, age (Pedlow & Carey, 2004). Adolescence is marked by cognitive maturation, increased risk-taking, and development of decision making skills, all of which may benefit from extended training with age-specific skill building opportunities to increase the impact of interventions (Pedlow & Carey, 2004). Additionally, within the period of adolescence remain distinct phases of sexual development which require age-tailored interventions (Pedlow & Carey, 2004). Sexual risk interventions targeting youths in pre- or early adolescence may focus on primary prevention and establish safe behaviors to promote safe relationships and delay sexual debut, as seen in PREPARE (Mathews et al., 2016). Alternatively, interventions targeting older adolescents who may already be sexually active need to focus on secondary prevention through skill building and reducing sexual risk behaviors, including inconsistent condom use and multiple sex partners (Mwale & Muula, 2017). Given the current body of literature on developmental tailoring, we had anticipated more studies targeting early adolescence in our results. The present review indicates that further research needs to examine the age-specific effects of IPV/HIV interventions to determine the most effective prevention strategies for primary prevention during early adolescence and secondary prevention among older adolescents.
Another significant finding of our review is the active engagement of male participants in seven of the eight studies. Seven of the eight interventions aimed to reduce IPV perpetration among the study population. This is highly promising and demonstrates that the current research on IPV/HIV is addressing the important role men must play in IPV prevention (Carlson et al., 2014). Two interventions were delivered exclusively to male participants (Kajula et al., 2016; Kalichman et al., 2009), while three other studies divided participants into single-sex groups to receive the intervention (Gibbs et al., 2017; Jewkes et al., 2008; Pronyk et al, 2006). We are encouraged by the specific focus on young men that has emerged in the field of integrated HIV and IPV prevention since gender targeting may be an effective means of promoting community-wide gender equality and normalizing safe sexual behaviors (Peacock & Levack, 2004). Our review found that the interventions targeting HIV and IPV risk among male participants implemented skill building activities to promote sexual communication and condom use, as well as group discussions and role play to explore the topics of HIV and IPV risk, attitudes towards women, and healthy relationships (Gibbs et al., 2017; Jewkes et al., 2008; Kajula et al., 2016; Kalichman et al., 2009). These strategies are aligned with previous literature calling for HIV and gender-targeted interventions to increase “space for boy’s voices” to direct the discourse on masculinity, identity, and renegotiation of power within relationships (Thorpe, 2002).
Intervention Strategies
Our review found that both structural and behavioral approaches have been assessed for efficacy in concomitantly reducing IPV and HIV risk in Sub-Saharan Africa. The structural interventions primarily addressed the economic and social environments that contribute to gender inequity and increased risk of HIV. The multi-component interventions employed various skill building- activities to enhance sexual communication, condom use, and personal beliefs and gender equality. Each of the eight interventions underscored gender inequity as a social factor that contributes to IPV and HIV risk. These are important strategies to address the distinct gender disparities in HIV risk; the average odds of a Sub-Saharan African woman being infected with HIV is 60% higher than her male counterpart (Magadi, 2011).
Due to the significant variety of intervention activities, dosages, and outcome measures, it is difficult to assess whether structural or behavioral approaches were more effective in reducing IPV/HIV risk. Furthermore, because of the wide age ranges in the study samples, it is also difficult to know with certainty which interventions were most effective among adolescents, and why. However, research has found that adolescent sexual and reproductive health is influenced by a combination of social and structural factors, including safe homes, parental communication, sustained livelihoods, and poverty (Bastien, Kajula, & Mahwezi, 2011; Madise, Zulu, & Ciera, 2007; Mosavel, Ahmed, & Simon, 2011). Addressing structural and ecological influences of adolescent sexual health may lead to more enduring risk reduction than behavioral interventions (DiClemente et al., 2007). While the structural interventions in this review did not specifically target adolescents, previous research shows evidence of the positive impact of structural interventions that address the economic, political, and social environments of both IPV and HIV risk (Berkman et al., 2005; Bourey et al., 2015; Handa et al., 2014; Harrison et al., 2010). The limited number of school-based integrated IPV/HIV interventions in our review highlights another priority area for future research. Schools offer the opportunity to reach large numbers of young people, increase intervention exposure by building program elements into the existing curriculum, and address social norms related to gender equity and sexual risk behaviors in the school community (Harrison et al., 2010; Mathews et al., 2016; WHO, 2010).
Efficacy
Our results show the potential for integrated IPV/HIV prevention to reduce sexual risk behavior and improve gender equality at the individual and community level. Of the six studies with available results, two interventions were associated with decreased IPV, as indicated by reduced self-reports of experience of IPV (Mathews et al., 2016; Pronyk et al., 2006). One intervention demonstrated reductions in IPV perpetration and STI incidence, but not HIV (Jewkes et al., 2008). Three interventions were associated with both statistically significant reductions in IPV and HIV risk (Abramsky et al., 2014; Kalichman et al., 2009; Wagman et al., 2015). However, the outcomes used to measure IPV and HIV reductions among these three interventions varied significantly, from social attitudes towards IPV (Abramsky et al., 2014) to self-reported incidence (Kalichman et al., 2009; Wagman et al., 2015). Similarly, the findings of Abramsky et al. (2014), Kalichman et al. (2009), and Wagman et al. (2015) represent intervention impacts on varied HIV outcomes, including both biological outcomes (Wagman et al. 2015) and self-reported sexual risk behavior reduction (Abramsky et al., 2014; Kalichman et al., 2009).
The differences in IPV and HIV effect measurement across the eight studies highlight the various ways research conceptualizes IPV and HIV, including both structural-level risks and reported incidence. All included studies relied on self-reports of IPV experience, perpetration, or measures of gender equitable attitudes which may introduce biases depending on the characteristics of the participant and the study’s definition of IPV (Schroder et al., 2003; Waltermaurer, 2005). Furthermore, studies which measure experience or perpetration of IPV exclusively cannot report reductions of all IPV incidence. In regards to HIV, half of the studies use biological outcomes to measure the interventions’ effect on HIV risk reduction, while four studies used self-reported sexual risk behaviors, which is subject to reporting bias. Increasing use of biological outcomes in HIV prevention is challenging, but our results indicate that we need more studies that include rigorous, comparable measurement. The field of integrated IPV/HIV prevention will benefit from consistent definitions and conceptualizations of IPV and HIV risk.
It is encouraging that three studies resulted in statistically significant reductions in both IPV and HIV risk. However, the mixed efficacy are surprising results and suggests that more work in intervention development and refinement is warranted. One area for increased attention is the dose of intervention and follow-up times. The included studies implemented the intervention over a significant range of time, from five consecutive days of 3-hour sessions (Kalichman et al., 2009), to more than 11,000 community mobilization activities over the course of four years (Abramsky et al., 2014). The majority of the interventions implemented weekly or bi-weekly sessions. Importantly, the three interventions with demonstrated reductions in both HIV and IPV implemented intervention activities in either concentrated doses; Kalichman et al. (2009) exposed participants to 15 hours of intervention material in five days, while the two community mobilization interventions delivered continuous activities over the course of roughly four years (Abramsky et al., 2014; Wagman et al., 2015). Further research is needed to examine the impact of different intervention dosages. The follow-up period also varied considerably, with assessments ranging from 1-month to 4-years post-intervention launch. Only one intervention (Pronyk et al., 2006) reported short duration of follow-up as a limitation to the study’s findings. Although longer durations of study and extended follow-up assessments may increase the risk of follow-up attrition or contamination between study sites, we recommend that future research employ space follow-up assessments so as to measure the long-term impact of IPV/HIV interventions.
Overall, the findings are highly encouraging for integrated IPV/HIV interventions and have important implications for public health practice as well as public health policy. The demonstrated reductions in both IPV and HIV suggest that public health policy makers should be aware of the dual risk pathways that exist between both public health problems. Policies aiming to reduce IPV may also benefit HIV reduction efforts. Further research is needed to examine the existence and effect of current policies that address both risks concurrently. However, the interventions’ strategies and promising results demonstrate that policies promoting gender and economic equity may help reduce risk factors that influence sexual risk taking and violence against women.
Limitations
The present findings should be interpreted in light of several limitations. The selected electronic databases and chosen search terms may not have provided access to all relevant studies. Due to the wide range of intervention designs, delivery methods, and outcome measurements, and limited number of existing interventions, it is difficult to compare efficacy across interventions using a meta-analytical approach. Half of the studies used self-reported sexual risk behaviors to measure HIV outcomes and all eight studies used self-reported measures of experience of IPV, which allows for social desirability and recall bias to affect study results (Schroder et al. 2003). More rigorous biological measures of HIV and IPV is needed.
Conclusion
Based on the findings of this review, interventions that integrate HIV and IPV prevention among adolescents are limited in number and are found in eastern and south African countries. Our analysis demonstrates that the majority of IPV and HIV interventions include both adult and older adolescent study populations and measure various IPV and HIV related outcomes. All included studies used group-based activities to promote gender equality and safer sexual norms. Prevention research should target specific adolescent sexual risk behaviors in a wider variety of settings throughout Sub-Saharan Africa to demonstrate which approaches are effective in reducing IPV and HIV incidence among vulnerable adolescent populations.
Supplementary Material
Acknowledgements
The authors received no financial support for the research, authorship, and/or publication of this article. The authors declared no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Contributor Information
Mary Kirtley Righi, Brown University, School of Public Health
Lindsay M. Orchowski, Alpert Medical School of Brown University, Department of Psychiatry and Human Behavior
Caroline Kuo, Brown University, School of Public Health.
References
- Abramsky T, Devries K, Kiss L, Nakuti J, Kyegombe N, Starmann E, … Watts C (2014). Findings from the SASA! Study: a cluster randomized controlled trial to assess the impact of a community mobilization intervention to prevent violence against women and reduce HIV risk in Kampala, Uganda. BMC Medicine, 12. doi: 10.1186/s12916-014-0122-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson JC, Campbell JC, & Farley JE (2013). Interventions to address HIV and intimate partner violence in Sub-Saharan Africa: a review of the literature. The Journal of the Association of Nurses in AIDS Care: JANAC, 24, 383–90. doi: 10.1016/j.jana.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastien S, Kajula LJ, & Muhwezi WW (2011). A review of studies of parent-child communication about sexuality and HIV/AIDS in sub-Saharan Africa. Reproductive Health, 8 Retrieved from http://search.ebscohost.com/login.aspx?direct=true&db=edswsc&AN=000208608000025&site=eds-live&scope=site. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman A, Garcia J, Muñoz-Laboy M, Paiva V, & Parker R (2005). A Critical Analysis of the Brazilian Response to HIV/AIDS: Lessons Learned for Controlling and Mitigating the Epidemic in Developing Countries. American Journal of Public Health, 95, 1162–1172. doi:2105/AJPH.2004.054593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourey C, Williams W, Bernstein EE, & Stephenson R (2015). Systematic review of structural interventions for intimate partner violence in low- and middle-income countries: organizing evidence for prevention. BMC Public Health, 15, 1165. doi: 10.1186/s12889-015-2460-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson J, Casey E, Edleson JL, Tolman RM, Neugut TB, & Kimball E (2015). Strategies to Engage Men and Boys in Violence Prevention: A Global Organizational Perspective. Violence Against Women, 21, 1406–1425. doi.org/ 10.1177/1077801215594888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Koker P, Mathews C, Zuch M, Bastien S, & Mason-Jones AJ (2014). A Systematic Review of Interventions for Preventing Adolescent Intimate Partner Violence. Journal of Adolescent Health, 54, 3–13. doi:doi.org/ 10.1016/j.jadohealth.2013.08.008. [DOI] [PubMed] [Google Scholar]
- DiClemente RJ, Salazar LF, & Crosby RA (2007). A review of STD/HIV preventive interventions for adolescents: sustaining effects using an ecological approach. Journal of Pediatric Psychology, 32, 888–906. 10.1093/jpepsy/jsm056. [DOI] [PubMed] [Google Scholar]
- Djomand G, Quaye S, & Sullivan PS (2014). HIV epidemic among key populations in west Africa. Current Opinion in HIV and AIDS, 9, 506–513. doi: 10.1097/COH.0000000000000090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkle K, & Decker M (2013). Gender-based violence and HIV: reviewing the evidence for links and causal pathways in the general population and high-risk groups. American Journal of Reproductive Immunology, 69, 20–26. doi: 10.1111/aji.12039. [DOI] [PubMed] [Google Scholar]
- Dunkle K, Jewkes R, Brown H, Gray GE, McIntryre JA, & Harlow SD (2004a). Transactional sex among women in Soweto, South Africa: Prevalence, risk factors and association with HIV infection. Social Science and Medicine, 59, 1581–1592. doi: 10.1016/j.socscimed.2004.02.003. [DOI] [PubMed] [Google Scholar]
- Dunkle K, Jewkes R, Brown H, Gray G, McIntyre J, & Harlow S (2004b). Gender-based violence, relationship power, and risk of HIV infection in women attending antenatal clinics in South Africa. Lancet, 363, 1415–1421. doi: 10.1016/S0140-6736(04)16098-4. [DOI] [PubMed] [Google Scholar]
- Eaton L, Flisher A, & Aarø L (2003). Unsafe sexual behavior in South African youth. Social Science & Medicine, 56, 149–165. doi: 10.1016/S0277-9536(02)00017-5. [DOI] [PubMed] [Google Scholar]
- Evan M, Risher K, Zungu N, Shisana O, Moyo S, Celentano DD, … Rehle TM (2016). Age-disparate sex and HIV risk for young women from 2002 to 2012 in South Africa. Journal of the International AIDS Society, 19, 21310. doi: 10.7448/IAS.19.1.21310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flisher A, Myer L, Mèrais A, Lombard C, & Reddy P (2007). Prevalence and correlates of partner violence among South African adolescents. Journal of Child Psychology and Psychiatry and Allied Disciplines, 48, 619–627. doi.org/ 10.1111/j.1469-7610.2007.01711.x. [DOI] [PubMed] [Google Scholar]
- García-Moreno C, & Watts C (2000). Violence against women: Its importance for HIV/AIDS. AIDS, 14, S253–S265. 10.1097/00002030-200005050-00024. [DOI] [PubMed] [Google Scholar]
- Gibbs A, Washington L, Willan S, Ntini N, Khumalo T, Mbatha N, … Jewkes R (2017). The Stepping Stones and Creating Futures intervention to prevent intimate partner violence and HIV-risk behaviours in Durban, South Africa: study protocol for a cluster randomized control trial, and baseline characteristics. BMC Public Health, 17, 336. doi: 10.1186/s12889-017-4223-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handa S, Halpern CT, Pettifor A, & Thirumurthy H (2014). The Government of Kenya’s Cash Transfer Program Reduces the Risk of Sexual Debut among Young People Age 15–25. PLOS ONE, 9. doi: 10.1371/journal.pone.0085473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison A, Newell M-L, Imrie J, & Hoddinott G (2010). HIV prevention for South African youth: which interventions work? A systematic review of current evidence. BMC Public Health, 10. doi: 10.1186/1471-2458-10-102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes R, Dunkle K, Nduna M, & Shai N (2010). Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet, 376, 41–48. doi: 10.1016/S0140-6736(10)60548-X. [DOI] [PubMed] [Google Scholar]
- Jewkes R, Nduna M, Levin J, Jama N, Dunkle K, Puren A, … Duvvury N (2008). Impact of Stepping Stones on Incidence of HIV and HSV-2 and Sexual Behaviour in Rural South Africa : Cluster Randomised Controlled Trial. BMJ: British Medical Journal, 337, 391–395. doi: 10.1136/bmj.a506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS). (2017). UNAIDS Data 2017. Retrieved from http://www.unaids.org/sites/default/files/media_asset/20170720_Data_book_2017_en.pdf. [PubMed]
- Joint United Nations Programme on HIV/AIDS (UNAIDS). (2014). The Gap Report. Retrieved from http://www.unaids.org/sites/default/files/media_asset/UNAIDS_Gap_report_en.pdf. [PubMed]
- Kajula L, Balvanz P, Kilonzo MN, Mwikoko G, Yamanis T, Mulawa M, … Maman S (2016). Vijana Vijiweni II: a cluster-randomized trial to evaluate the efficacy of a microfinance and peer health leadership intervention for HIV and intimate partner violence prevention among social networks of young men in Dar es Salaam. BMC Public Health, 16. doi: 10.1186/s12889-016-2774-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Cloete A, Clayford M, Arnolds W, Mxoli M, … Kalichman MO (2009). Integrated gender-based violence and HIV risk reduction intervention for South African men: Results of a quasi-experimental field trial. Prevention Science, 10, 260–269. doi: 10.1007/s11121-009-0129-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Martin L, & Denny L (2003). Rape and HIV: post-exposure prophylaxis: addressing the dual epidemics in South Africa. Reproductive Health Matters, 11, 101–12. doi: 10.1016/S0968-8080(03)02285-7. [DOI] [PubMed] [Google Scholar]
- Kotchick B, Shaffer A, Forehand R, & Miller K (2001). Adolescent sexual risk behavior: a multi-system perspective. Clinical Psychology Review, 21, 493–519. doi: 10.1016/S0272-7358(99)00070-7. [DOI] [PubMed] [Google Scholar]
- Li Y, Marshall C, Rees H, Nunez A, Ezeanolue E, & Ehiri J (2014). Intimate partner violence and HIV infection among women: a systematic review and meta-analysis. Journal of the International AIDS Society, 17, 18845. doi: 10.7448/IAS.17.1.18845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madise N, Zulu E, & Ciera J (2007). Is poverty a driver for risky sexual behaviour? Evidence from national surveys of adolescents in four African countries. African Journal of Reproductive Health / La Revue Africaine de La Santé Reproductive, 11, 83–98. doi: 10.2307/25549733. [DOI] [PubMed] [Google Scholar]
- Magadi MA (2011). Understanding the gender disparity in HIV infection across countries in sub-Saharan Africa: Evidence from the Demographic and Health Surveys. Sociology of Health and Illness, 33, 522–539. doi: 10.1111/j.1467-9566.2010.01304.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maman S, Mbwambo J, Hogan N, Kilonzo G, & Sweat M (2001). Women’s barriers to HIV-1 testing and disclosure: challenges for HIV-1 voluntary counselling and testing. AIDS Care, 13, 595–603. doi: 10.1080/09540120120063223. [DOI] [PubMed] [Google Scholar]
- Maman S, Mbwambo J, Hogan N, Kilonzo G, Campbell J, Weiss E, & Sweat M (2002). HIV-positive women report more lifetime partner violence: findings from a voluntary counselling and testing clinic in Dar es Salaam, Tanzania. American Journal of Public Health, 92, 1331–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews C, Eggers SM, Townsend L, Aarø LE, de Vries PJ, Mason-Jones AJ, … De Vries H (2016). Effects of PREPARE, a multi-component, school-based HIV and intimate partner violence (IPV) prevention programme on adolescent sexual risk behaviour and IPV: Cluster randomised controlled trial. AIDS and Behavior, 20, 1821–1840. doi: 10.1007/s10461-016-1410-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCloskey LA, Boonzaier F, Steinbrenner SY, & Hunter T (2016). Determinants of intimate partner violence in sub-Saharan Africa: A review of prevention and intervention programs. Partner Abuse, 7, 277–315. doi: 10.1891/1946-6560.7.3.277. [DOI] [Google Scholar]
- Médecins Sans Frontières. (2016). Out of Focus: How millions of people in West and Central Africa are being left out of the global HIV Response. Retrieved from https://www.msfaccess.org/sites/default/files/MSF_assets/HIV_AIDS/Docs/HIV_report_WCA_ENG_2016.pdf.
- Michielsen K, Temmerman M, & Van Rossem R (2013). Limited effectiveness of HIV prevention for young people in sub-Saharan Africa: studying the role of intervention and evaluation. Facts, Views & Vision in ObGyn, 5, 196–208. [PMC free article] [PubMed] [Google Scholar]
- Kaufman CE, & Stavrou SE (2002). “Bus fare, please”: the economics of sex and gifts among adolescents in urban South Africa. Population Council Policy Research Division Working Papers. Retrieved from http://pdf.usaid.gov/pdf_docs/Pnada195.pdf. [Google Scholar]
- Mosavel M, Ahmed R, & Simon C (2012). Perceptions of gender-based violence among South African youth: Implications for health promotion interventions. Health Promotion International, 27, 323–330. doi.org/ 10.1093/heapro/dar04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munguti K, Grosskurth H, Newell J, Senkoro K, Mosha F, Todd J, … Hayes R (1997). Patterns of sexual behavior in a rural population in north-western Tanzania. Social Science & Medicine, 44, 1553–61. doi: 10.1016/S0277-9536(97)00014-2. [DOI] [PubMed] [Google Scholar]
- Mwale M, & Muula AS (2017). Systematic review: A review of adolescent behavior change interventions [BCI] and their effectiveness in HIV and AIDS prevention in sub-Saharan Africa. BMC Public Health, 17, 1–10. doi: 10.1186/s12889-017-4729-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olorunsaiye CZ, Brunner L, Laditka SB, Kulkarni S, & Boyd AS (2017). Associations between women’s perceptions of domestic violence and contraceptive use in seven countries in West and Central Africa. Sexual & Reproductive Healthcare, 13, 1–8. doi: 10.1016/j.srhc.2017.01.003. [DOI] [PubMed] [Google Scholar]
- Olowookere SA, Fawole OI, Adekanle DA, Adeleke NA, & Abioye-Kuteyi EA (2015). Patterns and Correlates of Intimate Partner Violence to Women Living With HIV/AIDS in Osogbo, Southwest Nigeria. Violence against Women, 21, 1330–1340. doi: 10.1177/1077801215594889. [DOI] [PubMed] [Google Scholar]
- Paul-Ebhohimhen VA, Poobalan A, & van Teijlingen ER (2008). A systematic review of school-based sexual health interventions to prevent STI/HIV in sub-Saharan Africa. BMC Public Health, 8, 4. doi: 10.1186/1471-2458-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peacock D, & Levack A (2004). The men as partners program in South Africa: Reaching men to end gender-based violence and promote sexual and reproductive health. International Journal of Men’s Health, 3, 173–188. doi: 10.3149/jmh.0303.173. [DOI] [Google Scholar]
- Pedlow CT, & Carey MP (2004). Developmentally-appropriate sexual risk reduction interventions for adolescents: Rationale, review of interventions, and recommendations for research and practice. Annals of Behavioral Medicine: A Publication of the Society of Behavioral Medicine, 27, 172–184. doi: 10.1207/s15324796abm2703_5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pettifor A, Measham D, Rees H, & Padian N (2004). Sexual power and HIV risk, South Africa. Emerging Infectious Diseases, 11, 1996–2004. 10.3201/eid1011.040252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronyk PM, Hargreaves JR, Kim JC, Morison LA, Phetla G, Watts C, … Porter JDH (2006). Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. The Lancet, 368, 1973–1983. doi: 10.1016/S0140-6736(06)69744-4. [DOI] [PubMed] [Google Scholar]
- Schroder KEE, Carey MP, & Vanable PA (2003). Methodological challenges in research on sexual risk behavior: II. Accuracy of self-reports. Annals of Behavioral Medicine, 26, 104–123. doi: 10.1207/S15324796ABM2602_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swart LA, Stevens MSG, & Ricardo I (2002). Violence in adolescents’ romantic relationships: Findings from a survey amongst school-going youth in a South African community. Journal of Adolescence, 25, 385–395. doi: 10.1006/jado.2002.0483. [DOI] [PubMed] [Google Scholar]
- Teitelman AM, Jemmott JB, Bellamy SL, Icard LD, O’Leary A, Heeren GA, … Ratcliffe SJ (2016). Partner violence, power and gender differences in South African adolescents’ HIV/STI behaviors. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association, 35, 751–760. doi: 10.1037/hea0000351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorpe M (2012). Masculinity in an HIV Intervention. Agenda: Empowering Women for Gender Equity, 53, 61–68. doi: 10.2307/4548057. [DOI] [Google Scholar]
- Torgerson DJ (2001). Contamination in trials: is cluster randomisation the answer? BMJ: British Medical Journal, 322, 355–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umana JE, Fawole OI, Adeoye IA, Koenig M, Stephenson R, Ahmed S, … Lalonde C (2014). Prevalence and correlates of intimate partner violence towards female students of the University of Ibadan, Nigeria. BMC Women’s Health, 14. doi: 10.1186/1472-6874-14-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations. (2012). Violence against women prevalence data: surveys by country. Retrieved from mailto:https://www.endvawnow.org/uploads/browser/files/vawprevalence_%0Amatrix_june2013.pdf%0A.
- United Nations Children’s Fund (UNICEF). (2017). Turning the tide against AIDS will require more concentrated focus on adolescents and young people. Retrieved from https://data.unicef.org/topic/hivaids/adolescents-young-people/#.
- van der Straten A, King R, Grinstead O, Vittinghoff E, Serufilira A, & Allen S (1998). Sexual Coercion, Physical Violence, and HIV Infection Among Women in Steady Relationships in Kigali, Rwanda. AIDS and Behavior, 2, 61–73. doi: 10.1023/A:1022311424652. [DOI] [Google Scholar]
- Diallo SA, Voia M (2016). The Threat of Domestic Violence and Women Empowerment: The Case of West Africa. African Development Review, 28, 92–103. doi: 10.1111/1467-8268.12169. [DOI] [Google Scholar]
- Wagman JA, Gray RH, Campbell JC, Thoma M, Ndyanabo A, Ssekasanvu J, … Kagaayi J (2015). Effectiveness of an integrated intimate partner violence and HIV prevention intervention in Rakai, Uganda : analysis of an intervention in an existing cluster randomised cohort. The Lancet Global Health, 3, e23–e33. doi: 10.1016/S2214-109X(14)70344-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waltermaurer E (2005). Measuring Intimate Partner Violence (IPV) you may only get what you ask for. Journal of Interpersonal Violence, 20, 501–506. doi: 10.1177/0886260504267760. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2013). Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. Retrieved from http://apps.who.int/iris/bitstream/10665/85239/1/9789241564625_eng.pdf?ua=1.
- World Health Organization. (2010). Sexual Determinants of sexual and reproductive health: informing future research and programme implementation. Retrieved from http://apps.who.int/iris/bitstream/10665/44344/1/9789241599528_eng.pdf.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.