Abstract
Research suggests that electronic nicotine delivery system (ENDS) use is associated with other substance use in adolescents; however, the magnitude of this association and whether this differs between adolescents and adults is not yet well understood. This meta-analysis aimed to quantify the extent to which ENDS use is associated with alcohol and marijuana use among adolescents and to compare the odds across adolescent samples and a comparison group of adult samples. A comprehensive literature review was conducted examining the relationship between ENDS use and alcohol (adolescent k=40 from 19 independent studies; adult k=35 from 12 independent studies) and marijuana (adolescent k=24 from 14 independent studies; adult k=6 from 3 independent studies) use. Adolescents who use ENDS had greater odds of reporting co-occurring alcohol use (OR=4.50, p<.001), particularly binge drinking (OR=4.51), and marijuana use (OR=6.04, p<.001) than adolescent who did not use ENDS. Adults who use ENDS were also more likely to use alcohol (OR=1.57, p<.001) and marijuana (OR=2.04, p<.001) than those who did not use ENDS. ENDS use was associated with significantly greater odds of alcohol use (log odds ratio; LOR=0.96 (OR=2.61), p<.001) and a trend of greater marijuana use (LOR=0.93 (OR=2.53), p=0.08) in adolescents than in adults. Effects were large in adolescents and small in adults. Findings suggest that ENDS use should be assessed in adolescents in both research and clinical settings. Importantly, ENDS use is strongly associated with co-occurring alcohol or marijuana use in adolescents.
Keywords: electronic nicotine delivery system, substance use, alcohol, marijuana, adolescents
Introduction
Electronic nicotine delivery system (ENDS) use rates are increasing in adolescents, surpassing rates of cigarette use. Recent data indicate that approximately 13% of eighth through twelfth graders report past month ENDS use, while only 7% report cigarette use (Johnston et al., 2016). With increasing popularity of ENDS use, research has begun to examine how ENDS use is associated with other substance use among adolescents. Due to differences across studies, effect sizes of these relationships vary quite widely and estimating the extent to which ENDS use is associated with other substance use is difficult at best. This meta-analysis aimed to review the emerging literature on ENDS use in order to characterize the size of the relationship between ENDS use and substance use in adolescents. The present study also aimed to compare the size of these effects across adolescent samples and a comparison group of adult samples.
In the current meta-analysis, we were primarily concerned with how ENDS use is associated with co-occurring alcohol and marijuana use in adolescents, as these behaviors are illegal, but prevalent, in this age group, are associated with a slew of negative outcomes that persist well into adulthood (e.g. Meier et al., 2012; Hemphill et al., 2014; Cobb-Clark et al., 2015), and negatively influence brain development during this maturational period (see Bava & Tapert, 2010; Lishdahl et al., 2018; Squeglia et al., 2009; Squeglia & Gray, 2016). Earlier age of adolescent onset alcohol use is associated with higher frequency of problematic alcohol use (Ohannessian et al., 2015), a higher likelihood of developing a substance use disorder, lower likelihood of graduating high school, and increased likelihood of having a criminal justice record in adulthood (Green et al., 2016). Additionally, heavy adolescent marijuana use is related to lower income and higher anxiety as an adult (Green et al., 2017). Both alcohol and marijuana use as an adolescent are related to decline in verbal memory, working memory, attention, psychomotor speed, and visuospatial functioning (Hanson et al., 2011; Nguyen-Louie et al., 2015), with greater use associated with greater declines in cognitive functioning (Winward et al., 2014). Such cognitive deficits are linked to disrupted development of grey and white matter in the brain (i.e., disrupted neuron development), which likely contributes to later behavioral undercontrol (Luciana et al., 2013),.
Overall, the growing body of literature indicates that ENDS use is associated with alcohol use and marijuana use in adolescents. Effect sizes for the odds of reporting co-occurring ENDS use and alcohol use in adolescents range from modest (Leventhal et al., 2016) to large (Camenga et al., 2014); effects sizes for the relationship between ENDS use and marijuana use range from small (Kong et al., 2016) to medium (Milicic & Leatherdale, 2017) to large (Camenga et al., 2014). This variability in effect sizes across studies necessitates a comprehensive review to determine a more robust estimate of these relationships and to examine potential moderators affecting these relationships across studies. Interestingly, the state of the literature appears to suggest that these relationships may be larger in adolescents than in adults: alcohol effects range from small (Hershberger, et al, 2016a; Saddleson et al., 2015) to modest (Cohn et al., 2015; Littlefield et al, 2015) and marijuana effects are generally small in adults (Saddleson et al., 2015; Cohn et al., 2015). However, no study has quantitatively compared the size of these relationships across adolescent and adult samples, so the field does not yet know if these effect size patterns indicate increased odds in adolescents. Therefore, the main goal of the current meta-analysis was to quantify the extent to which ENDS use is associated with alcohol and marijuana use among adolescents and to compare the size of the effects across adolescent samples and a comparison group of adult samples.
In a further attempt to understand the emerging literature, we also aimed to examine multiple potential moderators of the relationship between ENDS use and both alcohol and marijuana use in adolescents, including age, gender, and type of use (current vs. lifetime use of the substance). First, some evidence suggests ENDS use prevalence increases with age in adolescence, but that the strength of the relationship between ENDS and alcohol use is smaller as age increases (Miech et al., 2015). Second, although similar rates of ENDS use have been found between girls and boys, there is some evidence to suggest that the relationship between ENDS use and alcohol and marijuana use is larger for girls (Kristjansson et al., 2015). Third, type of use (i.e., current vs. lifetime use) may also be a viable moderator of the relationship between ENDS use and alcohol and marijuana use. For example, Leventhal & colleagues (2016) found medium effects for the relationship between marijuana use and ever use of ENDS, although the size of the effect varied across current problematic use versus ever use. Fourth, indicators of problematic alcohol use, such as binge drinking (NIAAA, 2017), could have a stronger relationship with ENDS use. For example, Kristjansson et al. (2015) found a strong relationship between binge drinking and ENDS use.
Thus, the goals of the current manuscript were to 1) quantify the extent to which ENDS use is associated with alcohol and marijuana use among adolescents, 2) compare the odds across adolescent samples and a comparison group of adult samples, and 3) examine the moderating role of age, gender, type of use (current vs. lifetime use), and alcohol use pattern in explaining differences in effect size estimates across studies. We aimed to compare the odds across adolescent and adult samples in order to determine if these effects are unique to adolescents or represent a more general risk factor. The latter would suggest that the relationships equally apply across these two groups. If ENDS use is a general risk factor, ENDS use could be used as a marker of alcohol or marijuana use in both adults and adolescents. Whether or not ENDS use influences later alcohol or marijuana use, or vice versa, asking a person about their ENDS use might be a marker of individual risk for alcohol or marijuana use behaviors. However, if odds are elevated in adolescents, as suggested by effect size patterns in the existing literature, this would suggest that it is more important to consider and measure ENDS use in this high-risk group, both in research and clinical practice, even if we do not yet understand the causal direction of the relationship. Documenting this increased risk would also help to catalyze and focus future research attempts in this high-risk group.
Methods
Literature search
Studies for the present meta-analysis were identified using Medline, PsychInfo, EMBase and PsychArticles. Articles published through March 2019 were chosen based on an exhaustive combination of the following keyword groups: 1) electronic cigarette, e-cig*, ENDS, vape, vaping, e-hookah, e-pipe, electronic vapor product, EVP OR electronic nicotine delivery, AND 2) alcohol, drink*, marijuana, cannabis, substance, ethyl alcohol, ethanol, weed, pot, OR drug. Weekly e-mail alerts were setup to identify articles published after the original search, reference sections of articles were searched, and forward searches were conducted using identified articles and studies citing identified articles, until no unique studies were identified. To obtain missing data needed for the present meta-analysis (e.g., when a study reported measuring study variables, but did not include data in article), authors were contacted.
Inclusion and Exclusion Criteria
The present meta-analysis included dissertations, published data, and data received from contacted authors. Adult studies (defined here as an average age > or = 18) were included for comparison to adolescent samples. Specific inclusion criteria were 1) any measure of ENDS use (e.g., past 30-day use, ever use), 2) any measure of any alcohol or marijuana use, and 3) article available in English. Exclusion criteria were 1) sample population was individuals in treatment for a substance use disorder and 2) study assessed ENDS use only to vape cannabis.
Coding of Studies
The following variables were coded for each study included in the present meta-analysis: publication year, study design, publication type, sample type (e.g., high-school, college), sample size, gender, ethnicity, type of use (i.e., current use vs. ever use), and substance assessed (i.e., alcohol or marijuana). For studies reporting longitudinal effect sizes (k=2), cross-sectional relationships were used in calculating the summary effect in order to remain consistent in study design and to reduce confounding the summary effect. Studies were coded by the first author and 25% of studies were coded by the second author for inter-rater reliability. Coders consulted on methodology of coding (e.g., which table to gather values from to compute the effect size) prior to coding and data analysis. There were no discrepancies between coders.
Construct definitions
Current and lifetime ENDS use.
Current ENDS use was defined as the study assessing use (1) or no use (0) of ENDS ranging from within the past 30 days to past year. Lifetime ENDS use was defined as the study assessing use (1) or no use (0) of ENDS ever or in their lifetime. Lifetime measures of ENDS use may have included current users, but this could not be distinguished based on the available data.
Current and lifetime alcohol or marijuana use
Current use of alcohol or marijuana was defined as the study assessing use (1) or no use (0) of alcohol or marijuana ranging from currently (specific wording in study was “currently” with no measure of duration) to past year. Lifetime alcohol or marijuana use was defined as the study assessing use (1) or no use (0) of alcohol or marijuana ever or in their lifetime. Lifetime measures of alcohol and marijuana use may have included current users, but this could not be distinguished based on the available data.
Binge drinking.
Binge drinking was defined as any report of lifetime to past two-week drunkenness or binge drinking (i.e., 5 or more drinks on one occasion for boys, 4 or more drinks on one occasion for girls).
Meta-analytic Method
Effect size calculation.
An odds ratio (OR) was used to quantify the following effect sizes: 1) Adolescent odds of reporting both ENDS use and alcohol use, 2) Adolescents odds of reporting both ENDS use and binge drinking, 3) Adolescents odds of reporting both ENDS use and marijuana use, 4) Adult odds of reporting both ENDS use and alcohol use, 5) Adult odds of reporting both ENDS use and binge drinking, and 6) Adult odds of reporting both ENDS use and marijuana use. The effect sizes represent the binary relationship between ENDS use and the alcohol or marijuana use outcome for the above 6 analyses. Effects were coded so that OR greater than one indicates ENDS use is associated with higher odds of reporting co-occurring alcohol or marijuana use.
For each study aim, a multilevel random-effects model was fitted to the data. This method enables the modeling of clustering (and thus non-independence) induced by a multilevel structure in the data (Van den Noortgate et al., 2013). Sample dependence is problematic as more weight is assigned to studies with multiple outcomes and, if the dependent outcomes are positively related, the error of the summary effect is underestimated (Borenstein et al., 2009). Multilevel random-effects modeling accounts for both within and between study variance and the correlation of effect sizes coming from the same study (i.e. dependency between effect sizes). When studies reported multiple effect sizes from the same sample, and the number of studies was too small to fit a multilevel model to the data (e.g., binge outcome analysis in adults and marijuana use in adults), effect sizes were averaged (Card, 2012) and simple random-effects models were used, in order to control for sample dependence.
Effect size estimation.
The metafor package (Viechtbauer, 2010) in the R statistical software was used to calculate a summary effect for all six analyses and follow-up z-tests were conducted to determine significance of the summary effect. Significance was determined on the p<.05 level and interpreted in accordance with Chen and colleagues (Chen et al., 2010) guidelines for small, medium, and large effects based on the baseline prevalence rates of each behavior in individuals who did not use ENDS: 1) Average marijuana use in adolescents who did not use ENDS was 6% across the studies included, resulting in effect size descriptors of small (OR=1.51), medium (OR=2.67) and large (OR=4.55) effects. 2) Average alcohol use in adolescents who did not use ENDS was 20% across the studies included, resulting in effect size descriptors of small (OR=1.41), medium (OR=2.31) and large (OR=3.75) effects. 3) Average marijuana use in adults who did not use ENDS was unavailable in the studies included; we thus used the estimates from the adolescent samples, resulting in effect size descriptors of small (OR=1.51), medium (OR=2.67) and large (OR=4.55) effects. 4) Average alcohol use in adults who did not use ENDS was 46% across the studies included, resulting in effect size descriptors of small (OR=1.38), medium (OR=2.67) and large (OR=4.55) effects. Adjusting effect size descriptors by base rates of behavior in the unexposed groups allows for better comparison across samples for which prevalence rates vary quite markedly (Chen et al., 2010).
For significant summary effects, a fail-safe N analysis was conducted to estimate the number of studies with null findings required to reduce the summary effect to non-significance. For Aim 1, a generalized/weighted least squares extension of Cochran’s Q-test for residual heterogeneity was conducted to test whether the variability in the observed effect is larger than one would expect based on sampling variability alone. The I2 index of heterogeneity (Huedo-Medina et al., 2006), which represents the percentage of the total variability due to heterogeneity, was calculated. Effect sizes with significant heterogeneity were followed-up with moderation analyses.
Moderation analyses.
Meta-regression analyses were conducted to evaluate the impact of study characteristics on effect sizes in adolescent samples only. Significance was determined on the p<.05 level. Slopes for meta-regression analyses are presented as Log Odds Ratios (LOR), although ORs are also reported. Odds were compared across adolescent and adult samples to examine the moderating role of sample (adolescent=1 versus adult=0) on the relationship between ENDS use and alcohol use, as well as between ENDS use and marijuana use, in separate models. The following moderators were examined: 1) Gender (i.e., percent female) and age (i.e., average age of sample) were examined as continuous moderator variables; 2) Type of ENDS use (i.e., 1=current use, 0=ever-use) and was examined as a dichotomous moderator variable; and 3) Type of substance use (i.e., 1=current use, 0=lifetime use) was examined as a dichotomous moderator variable. The suggested minimum sample size (k) for conducting meta-regression is k=10 (Borenstein et al., 2009), which was not achieved for adult samples in the present study; thus, meta-regression was not conducted for adult samples.
Results
A comprehensive literature review resulted in 715 initial studies after duplicates were removed. After a review of the titles, 454 studies that were not applicable to the present analysis (e.g., used animal models, stated it was a review or opinion, assessed chemical properties of ENDS) were excluded. After a review of the abstracts, an additional 155 studies were excluded (e.g. reviews, opinions, no assessment of substance use). The remaining 89 full articles were reviewed. Three authors were contacted by e-mail with a request to provide data necessary for inclusion but that was not reported in the manuscript; 1 response was received. At the end of each stage of this process, 32 independent articles met inclusion criteria for the present meta-analysis.
Odds of reporting co-occurring ENDS use and alcohol use among adolescents.
Nineteen studies met inclusion criteria for adolescent ENDS and alcohol use (see Table 1 for adolescent study characteristics, including study design). Across those studies, 40 effects were reported. The total sample size was 150,299. Average age of the sample was 15.24 (SD=1.10, range 13.60–18) and average percent girls was 51.18% (SD=3.44%, range 44% to 62.10%). Age and gender were approximately normally distributed (skewness 0.01 to 0.74; kurtosis −1.47 to 0.39). A total of k=19 effects assessed current ENDS use and k=21 assessed lifetime ENDS use. A total of k=31 effects assessed current alcohol use, k=13 assessed current binge drinking, and k=9 assessed lifetime alcohol use.
Table 1.
Adolescent meta-analytic sample descriptives
| Study | N | Grade | Age range | Age | % Female | Sample | Geographic | Marijuana Outcome (s) | Alcohol Outcome (s) | ENDS Outcome (s) |
|---|---|---|---|---|---|---|---|---|---|---|
| Camenga et al., 2014 | 1411 | 9–12 | - | - | 52.70a | High School | New York | 1. Past month | 1. Past month 2. Binge past month |
1. Past 30 days |
| Dai et al., 2018 | 10364 | - | 12–17y | - | 48.9 | Population Assessment of Tobacco and Health study | United States | - | 1. Ever use | 1. Ever use |
| de Lacy et al., 2017 | 28634 | 7–11 year | 11–17 | 13.6 | 52 | 2015 School Health Research Network | Wales | 1. Ever use 2. Past 30 days |
1. Current use | 1. Ever use |
| Demissie et al., 2017 | 13953 | 9–12 grade | - | - | - | 2015 National Youth Risk Behavior Survey | United States | 1. Past 30 days | 1. Past 30 days | 1. Past 30 days |
| Dunbar et al., 2017 | 2193 | - | 17 | 54 | 2015 Project Choice (Wave 7) | Los Angeles, California* | 1. Past year | 1. Past year 2. Past year heavy episode (>5 drinks) |
1. Past year | |
| Enlow, 2018 | 519 | 9–12th grade | 11–18y | 15.99 | 57.9 | High School | West Virginia, suburban Ohio, and Pennsylvania | 1. combined score of frequency and initiation age | 1. Ever use | 1. Ever use |
| Geidne et al., 2016 | 661 | 9 | 15–16 | 15.5 | 51.36 | 2014 School as a Setting for ANDT prevention | Sweden | - | 1. Tried 2. Used or use currently |
1. Ever use |
| Hughes et al., 2015 | 9699 | - | 14–17 | 50.8 | Trading Standards North West Alcohol and Tobacco Survey | North West England | - | 1. < 1 per week 2. < 1 per week, any binge 3. ≥ 1 per week 4. ≥ 1 per week, any binge |
1. Ever tried or purchasedb | |
| Jiang et al., 2016 | 45857 | 7–12 | 14.8 | 48.6 | School-based Survey on Smoking | Hong Kong, China | - | 1. Less than monthly 2. Greater than monthly |
1. Past 30 days | |
| Kaleta et al., 2016 | 3552 | - | 13–19 | 44 | Secondary and High School | Piotrkowski district, Poland | - | 1. Binge and moderate | 1. Ever use 2. Past 30 days |
|
| Kong et al., 2017 | 716 | - | 15–18 | - | 51.5 | High School | Ufa, Sterlitamak, and Karagaevo, Russia | 1. Ever use | 1. Ever use | 1. Ever use |
| Kristjansson et al., 2015* | 2963 | 10th grade | 15–16 | - | 50.8 | 2015 Youth in Iceland | Iceland | 1. Ever use | 1. Ever use 2. Ever drunkenness |
1. Ever use |
| Leventhal et al., 2016 | 2557 | 9th grade | - | 14.09 | 49.5 | High School | Los Angeles, California | 1. Cannabis Abuse Screening Test 2. Ever use |
1. Rutgers Alcohol Problem Index 2. Ever use |
1. Ever use |
| Miech et al., 2015* | 18100 | 8–12th grade | - | - | 50.82 | 2014 Monitoring the Future | United States | 1. Past 30 days | 1. Binge past 2 weeks | 1. Past 30 days |
| Milicic & Leatherdale, 2017 | 39837 | 9–12th grade | >18 | - | 49.98 | 2014/2015 COMPASS | Ontario and Alberta, Canada | 1. Ever use, not in past year 2. Past 12 month use |
1. Past year, less than monthly binge 2. Past year, once a month 3. Past year, weekly |
1. Past 30 days |
| Morean, et al., 2016* | 2241 | 9–12th grade | - | 15.6 | 54.4 | High School | Connecticut | - | 1. Past 30 days | 1. Past 30 days |
| Suris et al., 2015* | 621 | 10th grade | - | 16.21 | 47.94 | Recruited as 8th grade students | French Switzerland | 1. Past 30 days | 1. Past 30 days drunkenness | 1. Ever use 2. Past 30 days |
| Westling et al., 2017 | 1091** | 8th grade | - | 14.4 | 48.8 | Middle School | Oregon | 1. Ever use 2. Past 30 days |
1. Ever use 2. Past 30 days |
1. Ever use 2. Past 30 days |
| Williams & White, 2018 | 3518 | - | 12–17y | - | 49.9 | Victorian component of the Australian Secondary Students’ Alcohol and Drug (ASSAD) survey | Australia | 1. Ever use | 1. Past year use 2. Past week risky drinking (>5 drinks) |
1. past 12 month daily use 2. Ever use vs no use 3. Ever use vs cigarette use |
| Wills et al., 2017 | 2338 | 9–11th grade | 14–16 | 14.7 | 53 | High School | Hawaii | 1. 0 (never use) to 6 (daily) | - | 1. 0 (never use) to 6 (daily) |
Note.
Estimate based on sample of
“Have you ever tried or purchased ENDS?”, classified as ENDS use
Effect size calculated based on 2×2, ENDS x substance use table
At wave 7 (used for present study), some youth had moved nationally and internationally
Summary effect: Alcohol use.
The weighted mean effect size for the relationship between ENDS use and alcohol use in adolescents was large (k=40, OR=4.50, 95% CI 3.31 to 6.13) and statistically significant, z=9.60, p<.001. The effect size indicated that adolescents who report ENDS use have 4.50 times greater odds of reporting alcohol use than those who do not report ENDS use. A fail-safe N analysis indicated that 8,724 studies with null effects would be needed to reduce the summary effect to non-significance. The test of heterogeneity was significant (Q(df=41)=132.08, p< 0.001), indicating that a significant proportion of variability in effect sizes was due to between study variation. The I2 Index of effect size heterogeneity was 73.84, indicating that 73.84% of the total variability was due to between study heterogeneity.
Summary effect: Binge drinking.
The weighted mean effect size for the relationship between any ENDS use and binge drinking in adolescents was large (k=13, OR=4.51, 95% CI 3.13 to 6.51) and statistically significant, z=8.07, p<.001. The effect size indicated that adolescents who report ENDS use have 4.51 greater odds of reporting binge drinking than those who do not report ENDS use. A fail-safe N analysis indicated that 875 studies with null effects would be needed to reduce the summary effect to non-significance. The test of heterogeneity was significant (Q(df=12)=21.26, p=0.05), indicating that a significant proportion of variability in effect sizes was due to between study variation. The I2 Index of effect size heterogeneity was 49.79.
Moderator Analyses.
The relationship between ENDS use and alcohol use (k=40) did not vary significantly by age of the sample (LOR=−0.13 (OR=0.88), z=−0.67, p=.50), gender (LOR=−0.05 (OR=0.95), z=−1.08, p=.28), type of alcohol use (current vs. lifetime use; LOR=0.03 (OR=1.03), z=0.14, p=.89), or type of ENDS use (current vs. lifetime use; LOR=0.21(OR=1.23), z=1.00, p=.32).
Odds of reporting co-occurring ENDS use and marijuana use among adolescents.
Fourteen studies met inclusion criteria for adolescent ENDS and marijuana use (see Table 1 for adolescent study characteristics, including study design). Across those studies, 24 effects were reported. The total sample size was 89,962. Average age of the sample was 15.14 (SD=1.26, range 13.60–18) and average percent girls was 51.81% (SD=3.25%, range 47.94% to 58.60%). Age and gender were approximately normally distributed (skewness 0.21 to 0.85; kurtosis −1.82 to −0.45). A total of k=11 effects assessed current ENDS use and k=13 assessed lifetime ENDS use. A total of k=13 effects assessed current marijuana use and k=10 assessed lifetime marijuana use (with dependent effects).
Summary effect: Marijuana use.
The weighted mean effect size for the relationship between ENDS use and marijuana use in adolescents was large (k=24, OR=6.04, 95% CI 3.80 to 9.60) and statistically significant, z=7.60, p<.001. The effect size indicated that adolescents who report ENDS use have 6.04 times greater odds of reporting marijuana use than those who do not report ENDS use. A fail-safe N analysis indicated that 6,205 studies with null effects would be needed to reduce the summary effect to non-significance. The test of heterogeneity was significant (Q(df=23)=134.40, p<0.001), indicating that a significant proportion of variability in effect sizes was due to between study variation. The I2 Index of effect size heterogeneity was 84.77.
Moderator Analyses.
The relationship between ENDS use and marijuana use in adolescents did not vary significantly by age of the sample (LOR=−0.31 (OR=0.73), z=−1.10, p=0.27), type of marijuana use (current vs. lifetime use; LOR=−0.07(OR=0.93), z=−0.36, p=0.72), or type of ENDS use (current vs. lifetime use; LOR=0.18 (OR=1.20), z=0.66, p=.51). Gender was a significant moderator of the relationship between ENDS use and marijuana use (LOR=−0.19 (OR=0.83), z=2.61, p=.01), indicating that as the percent of females in the sample increased, the relationship between ENDS and marijuana use became weaker.
Odds of reporting co-occurring ENDS use and alcohol use among adults.
Twelve studies met inclusion criteria for adult ENDS and alcohol use (see Table 2 for adult study characteristics). Across those studies, 35 effects were reported. Included studies were conducted between 2014 and 2019 and had a total sample size of 57,622. Average age of the sample was 29.57 years (SD=10.66, range 19–47.50). Average percent female was 56.68% (SD=5.65%, range 48.8–69.5). Age and gender were approximately normally distributed (skewness 0.61 to 0.62; kurtosis −1.38 to −0.33). A total of k=33 effects assessed current alcohol use and k=2 effect assessed lifetime alcohol use. A total of k=24 effects assessed current ENDS use and k=11 effects assessed lifetime ENDS use (with dependent effects).
Table 2.
Adult meta-analytic sample descriptives
| Study | N | Age range | Age | % Female | Sample | Geographic | Marijuana Outcome (s) | Alcohol Outcome (s) | ENDS Outcome (s) |
|---|---|---|---|---|---|---|---|---|---|
| Bartoli et al., 2014 | 590 | 18–24 | 20.65 | 51.5 | College | Italy | - | 1. Binge past 2 weeks | 1. Past 30 days |
| Cohn et al., 2015 | 1772 | 18–24 | 20.90a | - | National survey | United States | 1. Ever use | 1. Ever use | 1. Ever use 2. Past 30 days |
| Hefner et al., in press | 631 | >18 | - | 62.1 | College | United States | - | 1. Current use | 1. Ever use 2. Past 30 days |
| Hershberger et al., 2016a | 410 | 21–77 | 34.17 | 48.8 | Online adult | United States | - | 1. Total drinking days past 2 weeks 2. Average drinks per drinking day past 2 weeks past 2 weeks 3. AUDIT (past year) |
1. Current use |
| Hershberger et al., 2016b | 358 | 21–83 | 32.86 | 57.10 | Online adult | United States | - | 1. Total drinking days past 2 weeks 2. Average drinks per drinking day past 2 weeks 3. AUDIT (past year) |
1. Current use |
| Jaber et al., 2018 | 5423 | >18 | 47.5 | 51.8 | National Health and Nutrition Examination Survey | United States | - | 1. > 12 times use in past year | 1. Past 5 day use |
| Llanes et al., 2019 | 3755 | 17–74 | 26.63 | 58.4 | College | United States | - | 1. Past 90-day use | 1. Past month use |
| Lee et al., 2016 | 5338 | >19 | 45.7 | 51b | National survey of adults | South Korea | - | 1. ≤ Monthly past year 2. Weekly past year 3. Daily past year |
1. Ever use 2. Past 30 days |
| Littlefield et al., 2015* | 494 | 17–25 | 19.13 | 59.76 | College | United States | - | 1. Binge past 30 days | 1. Past 30 days |
| Roberts et al., 2018 | 36287 | - | 45.63 | 56.3 | National Epidemiologic Survey on Alcohol and Related Conditions | United States | - | 1. >1 drink in past year | 1. Past 12-month daily use vs. nonuse 2. Past 12-month nondaily use vs. nonuse |
| Saddleson et al., 2015 | 1430 | 18–23 | 19 | 61.2 | College | United States | 1. Past year | 1. Past 30 days 2. Binge past 30 days |
1. Ever use 2. Past 30 days |
| Tavolacci et al., 2016 | 1134 | - | 20.8 | 69.5 | College | France | 1. Past year | 1. ≥ 2 binge 2. ≤ 1 binge 3. AUDIT (past year) |
1. Ever use 2. Past 30 days |
Note.
Estimate based on a weighted sample of 1788
Estimate based on sample of 3477
Effect size calculated based on 2×2, ENDS x substance use table
Summary effect: Alcohol use.
The weighted mean effect size for the relationship between ENDS use and alcohol use in adults was small (OR=1.57, 95% CI 1.25–1.99) and statistically significant, z=3.81, p<.001. The effect size indicated that adults who report ENDS use have 1.57 times greater odds of reporting alcohol use than those who report no ENDS use. A fail-safe N analysis indicated that 320 studies with null effects would be needed to reduce the summary effect to non-significance. The test of heterogeneity was nonsignificant (Q(df=32)=37.57, p=0.31), indicating that most of the variability in effect sizes was not due to sampling error. The I2 Index of effect size heterogeneity was 39.67.
Summary effect: Binge drinking.
Four independent studies examined binge drinking, with 10 effects reported. Because the number of studies was too small to fit a multilevel model to the data, dependent effect sizes were averaged. The weighted mean effect size for the relationship between ENDS use and binge drinking in adults was small (OR=1.63, 95% CI 1.14 to 2.35) and statistically significant, z=2.65, p=.008. The effect size indicated that adults who report ENDS use have 1.63 greater odds of reporting binge drinking than those who do not report ENDS use. A fail-safe N analysis indicated that 24 studies with null effects would be needed to reduce the summary effect to non-significance. The I2 Index of effect size heterogeneity was significant, (I2=65.21, p=.01), indicating that a significant proportion of variability in effect sizes was due to between study variation.
Odds of reporting co-occurring ENDS use and marijuana use among adults.
Three independent studies met inclusion criteria for adult ENDS and marijuana use (see Table 2 for adult study characteristics). Across those studies, 6 effects were reported. Because the number of studies was too small to fit a multilevel model to the data, dependent effect sizes were averaged and random effects meta-analysis was fitted. Included studies were conducted between 2015 and 2017 and had a total sample size of 8,093 (mean=2,023, SD=1,184.87, range 1,134–3757). Average age of the sample was 19.8 years (SD=1.23, range 18.5–20.9). Average percent female was 65.35% (SD=4.58%, range 61.20–69.50). Sample size was approximately normally distributed (skewness −0.22; unable to compute age and gender due to k=2). The majority of data was collected in the United States (k=2). A total of 2 effects assessed current marijuana use and 1 effect assessed lifetime marijuana use. A total of 3 effects assessed current ENDS use and 3 effects assessed lifetime ENDS use (with dependent effects).
Summary effect.
The weighted mean effect size for the relationship between ENDS use and marijuana use in adults was small (OR=2.04, 95% CI 1.53 to 2.73) and statistically significant, z=4.84, p<.001. The effect size indicated that adults who report ENDS use have 2.04 time greater odds of reporting marijuana use than those who do not report ENDS use. A fail-safe N analysis indicated that 139 studies with null effects would be needed to reduce the summary effect to non-significance.
Comparison of odds across adolescent and adult samples
The relationship between ENDS use and alcohol use was significantly stronger in adolescent samples than adult samples (LOR=0.96 (OR=2.61), z=4.21, p<.001), suggesting that the odds of reporting ENDS use and co-occurring alcohol use are stronger in adolescents than adults. The relationship between ENDS use and marijuana use trended to be stronger in adolescent samples than adult samples (LOR=0.93 (OR=2.53), z=1.76, p=0.08), suggesting that the odds of reporting ENDS use and co-occurring marijuana use are stronger in adolescents than adults1.
Discussion
The present meta-analysis provides a synthesis of existing data examining the relationship between ENDS use and both alcohol and marijuana use in adolescents. First, our findings suggest that adolescents who use ENDS have approximately 4.5 to 6 times greater odds of reporting co-occurring alcohol or marijuana use. This is important: Although the state of the literature does not allow a precise understanding of the nature of this association (i.e., does ENDS use in adolescents increase odds for alcohol and marijuana use or do alcohol and marijuana use in adolescents increase odds for ENDS use), this relationship is large and suggests that ENDS use should be assessed in adolescents in both research and clinical settings, as it might be a marker of alcohol and marijuana use. Given that ENDS use is generally more socially acceptable, adolescents may be more likely to report openly and honestly concerning their ENDS use than other use behaviors. Thus, if adolescents report ENDS use, this might suggest further assessment of other substance use. Research should aim to clarify if ENDS use is a risk indicator for marijuana and alcohol use and what the directional nature of this relationship might be in adolescents. It is our hope that this finding of increased odds will lead to more targeted research in this high-risk group.
Higher odds of alcohol and marijuana use associated with ENDS use is of high research and clinical impact. ENDS, alcohol, and marijuana use have the potential to be mutually reinforcing (e.g., Rohsenow et al., 1997; Ericson et al., 2003; Soderpalm et al., 2000), meaning that the use of one may reinforce and thereby increase the use of the others and vice versa. Although beyond the scope of the present study, we see this as a critical area for future research, with this study demonstrating feasibility of such research. Mutual reinforcement among alcohol, marijuana, and ENDS is particularly concerning for adolescents because of recent large increases in ENDS use in this high-risk group (Johnston et al., 2016). Negative consequences of alcohol and marijuana use in adolescents are well-acknowledged, such as the development of problematic use and substance use disorders in later adolescence into adulthood (Bolland et al., 2016), as well as increased risk for negative health outcomes, such as heart attack (Hall & Degenhardt, 2009; Castellanos-Ryan et al., 2013). Marijuana and alcohol use during this developmental period can lead to negative outcomes including poor grades (Cobb-Clark et al., 2015), impaired memory and reasoning (Meier et al., 2012), and higher likelihood of arrest (Hemphill et al., 2014), as well as negative effects on brain development that are related to worse outcomes later in life (Green et al., 2016; Nguyen-Louie, 2015; Winward et al., 2014). Thus, anything associated with increased risk for these behaviors in adolescents should be studied in research and tracked clinically. Of course, ENDS use itself is also associated with negative health consequences, such as impaired respiratory and cardiovascular function (Kosmider et al., 2014; Lerner et al., 2015; Schweitzer et al., 2015; Sussan et al. 2015), and increases subsequent substance use risk (Unger et al., 2016), and thus is in interest in and of itself in this this high-risk group. The odds of reporting co-occurring ENDS use and alcohol or marijuana use were generally unaffected by type of use (current vs. lifetime use), but were higher as the proportion of males in the sample increased. This suggests that ENDS and marijuana use are more highly related in adolescent boys.
Although emerging research indicates that ENDS use is associated with future increased marijuana use in adolescents (Wills et al., 2017), we believe future research should seek to determine the causal direction of these relationship. We propose three plausible, although not mutually exclusive, explanations for how ENDS use may be strongly associated with alcohol and marijuana use in adolescents, which we discuss here: 1) alcohol and marijuana use are related to ENDS use through common risk factors, 2) alcohol and marijuana use contribute to ENDS use, and 3) ENDS use contributes to alcohol and marijuana use (Wills et al., 2017).
First, there appear to be common factors associated with ENDS use and alcohol use. For example, children of alcoholic fathers are more likely to both use ENDS and to co-use ENDS and alcohol (Lessard et al., 2014), thus suggesting a genetic component putting adolescents at risk for both ENDS and alcohol use; however, marijuana use has not been examined. ENDS use is related to impulsive personality traits (Hershberger et al., 2017), which are well-established risk factors for both alcohol and marijuana use (Coskunpinar et al., 2013; VanderVeen et al., 2016), thus suggesting shared personality-based risk factors for both ENDS use and alcohol and marijuana use. Additionally, given present findings indicating a more robust relationship between ENDS use and both alcohol and marijuana use in adolescents, age could be a risk factor for the use of both substances, with multiple candidate mechanisms to explain this age risk (e.g., impulsive personality traits; Romer et al., 2009).
Second, alcohol and marijuana use could contribute to later ENDS use in adolescents. A vast research literature has highlighted how classically conditioned behavioral cues and mutually reinforcing chemical properties link alcohol and cigarette use (Soderpalm et al., 2000; Tizabi et al., 2002; Ericson et al., 2003; Funk et al., 2006). These mechanisms may also apply to the relationship between ENDS and both alcohol and marijuana use. For example, Rohsenow and colleagues (1997) found that exposure to typical alcohol cues (e.g., odor) increases cigarette craving and likely consumption as well. Additionally, co-occurring ENDS use and alcohol and/or marijuana use may lead to synergistic drug effects (Rabin & George, 2015) by which nicotine and alcohol and/or marijuana may become mutually rewarding. Blocking nicotinic receptors of the dopamine reward system has shown to lessen alcohol consumption (Soderpalm et al., 2000) and blocking nicotine receptors during alcohol consumption eliminates alcohol-induced dopamine release (Tizabi et al., 2002; Ericson et al., 2003; Funk et al., 2006). Given the similarities in drug content of ENDS and cigarettes (Dawkins et al., 2014; Etter et al., 2014; Flouris et al., 2013), it is possible ENDS use and alcohol or marijuana use could share similar mutually rewarding chemical properties.
Third, ENDS use could contribute to marijuana and alcohol use in adolescence. Many of the mechanisms discussed above for how alcohol and marijuana use contribute to ENDS use are potential mechanisms also for how ENDS use could contribute to alcohol and marijuana use. For example, cigarette use and marijuana use share a route of administration (Rabin & George, 2015), which may cue marijuana use through increased cravings (Penetar et al., 2005). Similarly, the endocannabinoid system may mediate the rewarding properties of nicotine (Valjent et al., 2002) and exposure to nicotine, regardless of route of administration, increases the subjective reward value of marijuana (Penetar et al., 2005). Developmental research indicates that early onset (< 16 years old) cigarette use is related to increased odds of alcohol dependence and other illicit drug dependence eleven to twelve years later, while early onset of alcohol and illicit substance use does not appear to lead to increased odds of later cigarette use (Moss et al., 2014). The positive longitudinal relationship between cigarette use and substance use progression has been replicated in samples of African Americans (Strong et al., 2016), Korean Americans, and Chinese Americans (Myers et al., 2013), and thus likely generalizes across ethnic groups in the United States. Importantly, recent research on the longitudinal relationship between ENDS and marijuana use indicates that ENDS use may significantly predict future increased marijuana use (Wills et al., 2017), thus ENDS use may have a gateway effect on other substance use.
An extremely important finding of the current study is that odds associated with ENDS use are stronger in adolescents than adults. Although the state of the literature doesn’t allow full understanding concerning why these differences occur, we offer two potential reasons for stronger odds in adolescents. First, these findings could be related to a cohort effect. ENDS are a relatively new form of nicotine delivery, and, as such, became popular during the adolescence period of the current cohort. It’s been well-established that adolescence is a developmental time period for increased risk taking, particularly substance use (see Crone et al., 2012) and that many individuals “mature out” of this use, making substance use and related problems less likely into adulthood (Verges et al., 2013). This could also explain the increasing rates of ENDS use among adolescents (Johnston et al., 2016). As adults are less likely to have new onset substance use than adolescents (Verges et al., 2013), adults may be less vulnerable to beginning ENDS use or to have increased associated odds of marijuana and alcohol use.
Second, the reasons or motives for using ENDS likely differ between adolescents and adults. Adolescents tend to report using ENDS for experimentation, out of boredom, and to have a good time (Patrick et al., 2016), whereas adults typically use ENDS for smoking cessation (Malas et al., 2016). It is possible that using ENDS to reduce smoking might be associated with lower odds for other substance use, and using for fun or experimentation might be associated with higher odds of using other substances. Findings indicate that adolescents are increasingly exposed and targeted in ENDS advertisements (CDC, 2014), which may increase the likelihood of adolescents using ENDS.
Overall research is needed to better explain these differences and how best to leverage them for intervention and prevention. This heightened risk in adolescents is important, given the effect of marijuana, alcohol, and nicotine on the developing brain, including neurodegeneration and neurocognitive deficits (Zeigler et al., 2005), decreased white-matter volume in tracts associated with mood regulation (Squeglia et al., 2009), and disruption of acetylcholine receptors, which are vital for neurotransmitter regulation, cell survival, and synaptic formation and maturation (Dwyer et al., 2009).
Since the majority of research in this area to date is cross-sectional, a great amount of research is needed to better elucidate the ENDS use and alcohol and marijuana use relationship, including research utilizing both longitudinal and experimental designs. First, longitudinal research would be useful to test and determine the causal direction between ENDS use and both alcohol and marijuana use, which would inform how best to understand and leverage this relationship. For example, if longitudinal data indicate that ENDS use tends to precede alcohol and marijuana use, ENDS use may be a modifiable risk factor to prevent or reduce the risk of future alcohol or marijuana use in adolescent populations. If ENDS use follows alcohol or marijuana use, ENDS use would better be used as a screener of other substance use. We propose that given the more socially acceptability of ENDS (Hershberger et al., 2017), screening for ENDS use might result in more honest endorsement in adolescents, which would then suggest further screening of other substance use.
Second, experimental designs would help determine if ENDS use and alcohol and marijuana use co-occur in time and place for adolescents, as well as to identify mechanisms that underlie these relationships, which could then be leveraged for treatment and prevention. Further, this work would help differentiate unique mechanisms underlying ENDS (rather than mechanisms common to both ENDS and cigarette use) in adolescents. One prime candidate is expectancies: for example, adolescents often cite using ENDS for experimentation and taste (Patrick et al., 2016), while the goal of cigarette use is typically positive or negative reinforcement (McKee eet al., 2004). These different expectancies may suggest the need for the design and testing of specific prevention and intervention approaches for ENDS (although there are likely similar expectancies across cigarettes and ENDS that could be applied to prevention approaches for both behaviors).
Limitations
There are limitations of the current work. First, this study is subject to common limitations of meta-analytic design, including the file-drawer problem and the number of studies used in analyses. The sample size for both adolescent meta-analytic questions was large, increasing our confidence in the present findings, and further, fail-safe N analyses support that it is unlikely additional studies would reduce the effect sizes to non-significant values. At the same time, the sample size for adults was more limited, for example, with k=3 effects assessing adult ENDS and marijuana use, and thus may be less robust. The present findings represent the odds of co-occurring ENDS and alcohol or marijuana use, and no conclusions can be drawn on the causal nature or direction of this relationship. Additionally, given the self-report nature of included studies, findings are subject to self-report bias. Samples in college students may or may not generalize to other samples, although our current findings showed similar effects across college and non-college adults. We included studies with samples from all over the world, which may mask differences across countries2. Tthe dichotomous nature of outcome variables limits inferences to an either/or nature of each behavior (e.g., either using ENDS or not). To improve future studies, ENDS use and alcohol and marijuana use should be measured as continuous variables in order to improve inferences that can be made from the data. There are well-established continuous measures of alcohol and marijuana use, although there is little consensus on the continuous measure of ENDS use. We believe ENDS use should be assessed through frequency of ENDS use (e.g., days per week) and through measures of nicotine dependence for ENDS users (Foulds et al., 2014). Finally, studies did not indicate if ENDS used did or did not contain nicotine. It could be that there is a differential relationship between ENDS containing and not containing nicotine and alcohol and marijuana use, and this should be examined in future studies.
Conclusions
The present meta-analysis highlights that although ENDS use is associated with increased odds for alcohol and marijuana use in both adults and adolescents, the odds are significantly higher in adolescents. The relationships between ENDS use and alcohol use, marijuana use, and binge drinking are all large in adolescents, whereas the relationships are small in adults. Together, the present findings suggest that clinicians and researchers alike should assess and further study ENDS use in adolescents. Significant research is needed to better understand how and why ENDS use is so strongly associated with alcohol and marijuana use in adolescents and we hope this study stimulates future interest in this work. It is imperative that future studies employ increased methodological rigor (e.g., continuous measurements, longitudinal designs, experimental studies), including the investigation of the potential mechanisms and moderators of the relationship between ENDS use and alcohol and marijuana use in adolescents. Given the negative effects of substance use for adolescents, many of which are long-standing, this research should be done with the long-term goal of understanding how best to decrease negative outcomes in this high-risk group. Early assessment and detection of adolescent substance use, including assessing for ENDS use, is essential to mitigating long-term persistence of substance use across the lifespan.
Figure 1.
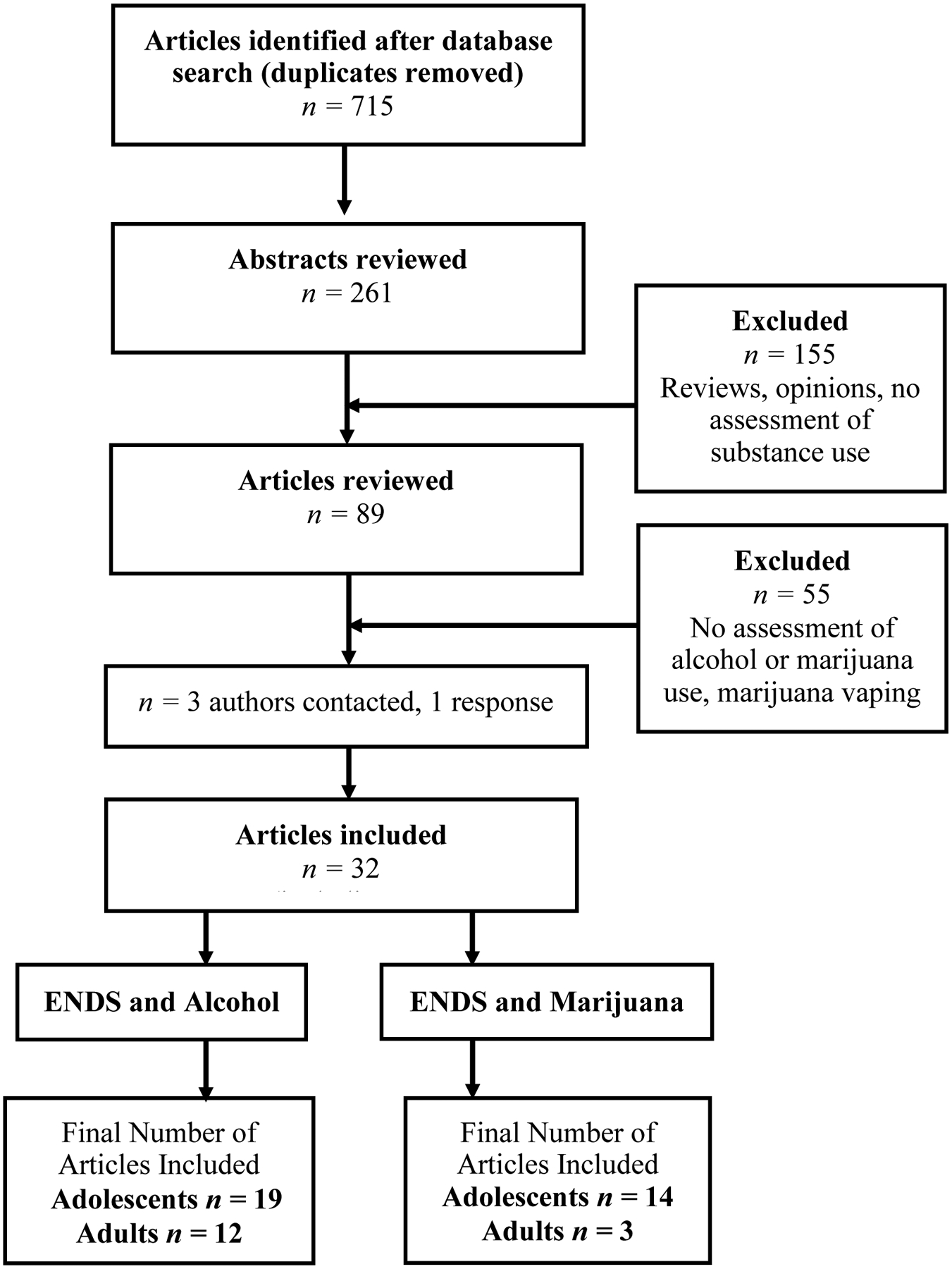
Article decision tree for meta-analysis.
Acknowledgments
This study was funded by an F31 predoctoral fellowship from NIAAA awarded to A.R.H. (F31 AA024682) under the mentorship of M.A.C.
Footnotes
A sensitivity analysis divided the samples into adolescents, college students, and non-college adults: The association between ENDS and alcohol use was not significantly different between college and non-college adult samples (p=0.860), but the relationship was larger in adolescent samples (p=0.001–0.003). The association between ENDS and marijuana use was not significantly different between college and non-college adult samples (p=0.639) and was similar across adult and adolescent samples (p=0.090–0.534), although there was a trend effect similar to what report in the manuscript. A second sensitivity analysis used age as a continuous moderator and found a similar pattern: There was a significant negative effect of age in the relationship between ENDS and alcohol use (b=−0.031, p=0.030) and between ENDS and marijuana use (b=−0.223, p=0.016).
A sensitivity analysis found that ORs in the current study did not differ across U.S. and non-U.S. samples with one exception: the OR for adolescent ENDS and alcohol use was 6.5 in U.S. samples vs. 4.5 when using all the samples in study. Thus, in general, U.S. and non-U.S. samples had similar effects, but the relationship between ENDS and alcohol in adolescents may be larger in the U.S. as compared to other countries.
References
* Adolescent meta-analytic sample
** Adult meta-analytic sample
- **.Bartoli F, Carretta D, Crocamo C, Schivalocchi A, Brambilla G, Clerici M, & Carrà G (2014). Prevalence and correlates of binge drinking among young adults using alcohol: a cross-sectional survey. BioMed Research International, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bava S, & Tapert SF (2010). Adolescent brain development and the risk for alcohol and other drug problems. Neuropsychology Review, 20(4), 398–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolland KA, Bolland JM, Tomek S, Devereaux RS, Mrug S, & Wimberly JC (2016). Trajectories of adolescent alcohol use by gender and early initiation status. Youth & Society, 48(1), 3–32. [Google Scholar]
- Borenstein M, Hedges LV, Higgins J, Rothstein HR (2009). Introduction to Meta-analysis. Chichester, U.K: John Wiley & Sons, Ltd. [Google Scholar]
- *.Camenga DR, Kong G, Cavallo DA, Liss A, Hyland A, Delmerico J, Cumming KM & Krishnan-Sarin S (2014). Alternate tobacco product and drug use among adolescents who use electronic cigarettes, cigarettes only, and never smokers. Journal of Adolescent Health, 55(4), 588–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Card N (2012). Applied meta-analysis for social science research. New York, NY: Guilford Press. [Google Scholar]
- Castellanos-Ryan N, Parent S, Vitaro F, Tremblay RE, & Séguin JR (2013). Pubertal development, personality, and substance use: a 10-year longitudinal study from childhood to adolescence. Journal of Abnormal Psychology, 122(3), 782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Disease Control and Prevention (CDC). (2017). E-cigarette ads and youth. Retrieved from: https://www.cdc.gov/vitalsigns/ecigarette-ads/index.html. Accessed October 24, 2017.
- Chen H, Cohen P, & Chen S (2010). How big is a big odds ratio? Interpreting the magnitudes of odds ratios in epidemiological studies. Communications in Statistics—Simulation and Computation®, 39(4), 860–864. [Google Scholar]
- Cobb-Clark DA, Kassenboehmer SC, Le T, McVicar D, & Zhang R (2015). ‘High’-School: The Relationship between Early Marijuana Use and Educational Outcomes. Economic Record, 91(293), 247–266. [Google Scholar]
- Cohen J (1992). A power primer. Psychological bulletin, 112(1), 155. [DOI] [PubMed] [Google Scholar]
- **.Cohn A, Cobb CO, Niaura RS, & Richardson A (2015). The other combustible products: prevalence and correlates of little cigar/cigarillo use among cigarette smokers. Nicotine & Tobacco Research, 17(12), 1473–1481. [DOI] [PubMed] [Google Scholar]
- Crone EA, & Dahl RE (2012). Understanding adolescence as a period of social–affective engagement and goal flexibility. Nature Reviews Neuroscience, 13(9), 636–650. [DOI] [PubMed] [Google Scholar]
- *.Dai H, Catley D, Richter KP, Goggin K, & Ellerbeck EF (2018). Electronic cigarettes and future marijuana use: a longitudinal study. Pediatrics, 141(5), e20173787. [DOI] [PubMed] [Google Scholar]
- Dawkins L, & Corcoran O (2014). Acute electronic cigarette use: nicotine delivery and subjective effects in regular users. Psychopharmacology, 231(2), 401–407. [DOI] [PubMed] [Google Scholar]
- *.de Lacy E, Fletcher A, Hewitt G, Murphy S, & Moore G (2017). Cross-sectional study examining the prevalence, correlates and sequencing of electronic cigarette and tobacco use among 11–16-year olds in schools in Wales. BMJ Open, 7(2), e012784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Demissie Z, Jones SE, Clayton HB, & King BA (2017). Adolescent risk behaviors and use of electronic vapor products and cigarettes. Pediatrics, e20162921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Dunbar MS, Tucker JS, Ewing BA, Pedersen ER, Miles JN, Shih RA, & D’amico EJ (2017). Frequency of e-cigarette use, health status, and risk and protective health behaviors in adolescents. Journal of Addiction Medicine, 11(1), 55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dwyer JB, McQuown SC, & Leslie FM (2009). The dynamic effects of nicotine on the developing brain. Pharmacology & Therapeutics, 122(2), 125–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Enlow PT (2017). Characterizing risk factors of adolescent electronic cigarette use. West Virginia University. [Google Scholar]
- Etter J (2014). Levels of saliva cotinine in electronic cigarette users. Addiction, 109(5), 825–829. [DOI] [PubMed] [Google Scholar]
- Ericson M, Molander A, Lof E, Engel JA, Soderpalm B (2003). Ethanol elevates accumbal dopamine levels via indirect activation of ventral tegmental nicotinic acetylcholine receptors. European Journal of Pharmacology, 467(1), 85–93. [DOI] [PubMed] [Google Scholar]
- Flouris AD, Chorti MS, Poulianiti KP, Jamurtas AZ, Kostikas K, Tzatzarakis MN, Hayes W,A, Tsatsakis AM, & Koutedakis Y (2013). Acute impact of active and passive electronic cigarette smoking on serum cotinine and lung function. Inhalation Toxicology, 25(2), 91–101. [DOI] [PubMed] [Google Scholar]
- Foulds J, Veldheer S, Yingst J, Hrabovsky S, Wilson SJ, Nichols TT, & Eissenberg T (2014). Development of a questionnaire for assessing dependence on electronic cigarettes among a large sample of ex-smoking ENDSarette users. Nicotine & Tobacco Research, 17(2), 186–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk D, Marinelli PW, & Le AD (2006). Biological processes underlying co-use of alcohol and nicotine: neuronal mechanisms, cross-tolerance, and genetic factors. Alcohol Research and Health, 29(3), 186. [PMC free article] [PubMed] [Google Scholar]
- *.Geidne S, Beckman L, Edvardsson I, & Hulldin J (2016). Prevalence and risk factors of electronic cigarette use among adolescents: Data from four Swedish municipalities. Nordic Studies on Alcohol and Drugs, 33(3), 225–240. [Google Scholar]
- Green KM, Musci RJ, Johnson RM, Matson PA, Reboussin BA, & Ialongo NS (2016). Outcomes associated with adolescent marijuana and alcohol use among urban young adults: A prospective study. Addictive Behaviors, 53, 155–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green KM, Doherty EE, & Ensminger ME (2017). Long-term consequences of adolescent cannabis use: Examining intermediary processes. The American Journal of Drug and Alcohol Abuse, 43(5), 567–575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, & Degenhardt L (2009). Adverse health effects of non-medical cannabis use. The Lancet, 374(9698), 1383–1391. [DOI] [PubMed] [Google Scholar]
- Hanson KL, Cummins K, Tapert SF, & Brown SA (2011). Changes in neuropsychological functioning over 10 years following adolescent substance abuse treatment. Psychology of Addictive Behaviors, 25(1), 127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Hefner KR, Sollazzo A, Mullaney S, Coker KL, & Sofuoglu M (2019). E-cigarettes, alcohol use, and mental health: Use and perceptions of e-cigarettes among college students, by alcohol use and mental health status. Addictive Behaviors, 91, 12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemphill SA, Heerde JA, Scholes-Balog KE, Smith R, Herrenkohl TI, Toumbourou JW, & Catalano RF (2014). Reassessing the effects of early adolescent alcohol use on later antisocial behavior: A longitudinal study of students in Victoria, Australia, and Washington state, United States. The Journal of Early Adolescence, 34(3), 360–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Hershberger AR, Karyadi KA, & Cyders MA (2016a). Prohibition of E-cigarettes in the US: Are prohibitions where alcohol is consumed related to lower alcohol consumption? Journal of Public Health Policy, 37(4), 483–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Hershberger AR, Karyadi KA, VanderVeen JD, & Cyders MA (2016b). Combined expectancies of alcohol and E-cigarette use relate to higher alcohol use. Addictive Behaviors, 52, 13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hershberger AR, Karyadi KA, VanderVeen JD, & Cyders MA (2017). Beliefs about the direct comparison of e-cigarettes and cigarettes. Substance Use & Misuse, 52(8), 982–991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hershberger A, & Cyders MA (2017). “Essentially, all models Are wrong, but some are useful”: A preliminary conceptual model of co-occurring e-cig and alcohol use. Current Addiction Reports, 4(2), 200–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, & Botella J (2006). Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychological Methods, 11(2), 193. [DOI] [PubMed] [Google Scholar]
- *.Hughes K, Bellis MA, Hardcastle KA, McHale P, Bennett A, Ireland R, & Pike K (2015). Associations between e-cigarette access and smoking and drinking behaviours in teenagers. BMC Public Health, 15(1), 244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Jaber RM, Mirbolouk M, DeFilippis AP, Maziak W, Keith R, Payne T, … & Saxena A (2018). Electronic cigarette use prevalence, associated factors, and pattern by cigarette smoking status in the United States from NHANES (National Health and Nutrition Examination Survey) 2013–2014. Journal of the American Heart Association, 7(14), e008178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, Sher KJ, Cooper ML, & Wood PK (2002). Adolescent alcohol and tobacco use: onset, persistence and trajectories of use across two samples. Addiction, 97(5), 517–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Jiang N, Wang MP, Ho SY, Leung LT, & Lam TH (2016). Electronic cigarette use among adolescents: a cross-sectional study in Hong Kong. BMC Public Health, 16(1), 202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE, & Miech RA (2016). Monitoring the Future national survey results on drug use, 1975–2015: Volume II, college students and adults ages 19–55. [Google Scholar]
- *.Kaleta D, Wojtysiak P, & Polańska K (2016). Use of electronic cigarettes among secondary and high school students from a socially disadvantaged rural area in Poland. BMC Public Health, 16(1), 703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Kong G, Idrisov B, Galimov A, Masagutov R, & Sussman S (2017). Electronic cigarette use among adolescents in the Russian Federation. Substance Use & Misuse, 52(3), 332–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosmider L, Sobczak A, Maciej F, Knysak J, Zaciera M, Kurek J, Goniewicz ML (2014). Carbonyl compounds in electronic cigarette vapors: Effects of nicotine solvent and batter output voltage, Nicotine and Tobacco Research, 16(10), 1319–1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Kristjansson AL, Mann MJ, & Sigfusdottir ID (2015). Licit and illicit substance use by adolescent e-cigarette users compared with conventional cigarette smokers, dual users, and nonusers. Journal of Adolescent Health, 57(5), 562–564. [DOI] [PubMed] [Google Scholar]
- **.Lee JA, Kim SH, & Cho HJ (2016). Electronic cigarette use among Korean adults. International Journal of Public Health, 61(2), 151–157. [DOI] [PubMed] [Google Scholar]
- Lerner CA, Sundar IK, Yao H, Gerloff J, Ossip DJ, McIntosh S, Robinson R, & Rahman I (2015). Vapors produced by electronic cigarettes and e-juices with flavorings induce toxicity, oxidative stress, and inflammatory response in lung epithelial cells and in mouse lung. Plos ONE, 10(2), 1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lessard J, Henrie J, Livingston JA, Leonard KE, Colder CR, & Eiden RD (2014). Correlates of ever having used electronic cigarettes among older adolescent children of alcoholic fathers. Nicotine & Tobacco Research, 16(12), 1656–1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Leventhal AM, Strong DR, Sussman S, Kirkpatrick MG, Unger JB, Barrington-Trimis JL, & Audrain-McGovern J (2016). Psychiatric comorbidity in adolescent electronic and conventional cigarette use. Journal of Psychiatric Research, 73, 71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisdahl KM, Shollenbarger S, Sagar KA, & Gruber SA (2018). The neurocognitive impact of alcohol and marijuana use on the developing adolescent and young adult brain. Brief Interventions for Adolescent Alcohol and Substance Abuse, 50. [Google Scholar]
- **.Littlefield AK, Gottlieb JC, Cohen LM, & Trotter DR (2015). Electronic cigarette use among college students: links to gender, race/ethnicity, smoking, and heavy drinking. Journal of American College Health, 63(8), 523–529. [DOI] [PubMed] [Google Scholar]
- **.Llanes K, Cabriales JA, Hernandez N, & Cooper TV (2019). Electronic cigarette use after the adoption of a tobacco-free campus policy. Addictive Behaviors, 90, 324–328. [DOI] [PubMed] [Google Scholar]
- Luciana M, Collins PF, Muetzel RL, & Lim KO (2013). Effects of alcohol use initiation on brain structure in typically developing adolescents. The American Journal of Drug and Alcohol Abuse, 39(6), 345–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malas M, van der Tempel J, Schwartz R, Minichiello A, Lightfoot C, Noormohamed A, Andrews J, Zawertailo L & Ferrence R (2016). Electronic cigarettes for smoking cessation: a systematic review. Nicotine & Tobacco Research, 18(10), 1926–1936. [DOI] [PubMed] [Google Scholar]
- McKee SA, Hinson R, Rounsaville D, & Petrelli P (2004). Survey of subjective effects of smoking while drinking among college students. Nicotine & Tobacco Research, 6(1), 111–117. [DOI] [PubMed] [Google Scholar]
- Meier MH, Caspi A, Ambler A, Harrington H, Houts R, Keefe RS, McDonald K, Ward A, Poulton R & Moffitt TE (2012). Persistent cannabis users show neuropsychological decline from childhood to midlife. Proceedings of the National Academy of Sciences, 109(40), E2657–E2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Miech RA, O’Malley PM, Johnston LD, & Patrick ME (2015). E-cigarettes and the drug use patterns of adolescents. Nicotine & Tobacco Research, 18(5), 654–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Milicic S, & Leatherdale ST (2017). The associations between E-cigarettes and binge drinking, marijuana use, and energy drinks mixed with alcohol. Journal of Adolescent Health, 60(3), 320–327. [DOI] [PubMed] [Google Scholar]
- *.Morean ME, Kong G, Camenga DR, Cavallo DA, Simon P, & Krishnan-Sarin S (2016). Latent class analysis of current E-cigarette and other substance use in high school students. Drug and Alcohol Dependence, 161, 292–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss HB, Chen CM, & Yi HY (2014). Early adolescent patterns of alcohol, cigarettes, and marijuana polysubstance use and young adult substance use outcomes in a nationally representative sample. Drug and Alcohol Dependence, 136, 51–62. [DOI] [PubMed] [Google Scholar]
- Myers MG, Doran NM, Edland SD, Schweizer CA, & Wall TL (2013). Cigarette smoking initiation during college predicts future alcohol involvement: a matched-samples study. Journal of Studies on Alcohol and Drugs, 74(6), 909–915. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). (2017). Drinking levels defined. Retrieved from: https://www.niaaa.nih.gov/alcohol-health/overview-alcohol-consumption/moderate-binge-drinking. Accessed October 24, 2017.
- Nguyen-Louie TT, Castro N, Matt GE, Squeglia LM, Brumback T, & Tapert SF (2015). Effects of emerging alcohol and marijuana use behaviors on adolescents’ neuropsychological functioning over four years. Journal of Studies on Alcohol and Drugs, 76(5), 738–748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohannessian CM, Finan LJ, Schulz J, & Hesselbrock V (2015). A long-term longitudinal examination of the effect of early onset of alcohol and drug use on later alcohol abuse. Substance Abuse, 36(4), 440–444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick ME, Miech RA, Carlier C, O’Malley PM, Johnston LD, & Schulenberg JE (2016). Self-reported reasons for vaping among 8th, 10th, and 12th graders in the US: nationally-representative results. Drug and Alcohol Dependence, 165, 275–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Penetar DM, Kouri EM, Gross MM, McCarthy EM, Rhee CK, Peters EN, & Lukas SE (2005). Transdermal nicotine alters some of marihuana’s effects in male and female volunteers. Drug and Alcohol Dependence, 79(2), 211–223. [DOI] [PubMed] [Google Scholar]
- Rabin RA, & George TP (2015). A review of co-morbid tobacco and cannabis use disorders: Possible mechanisms to explain high rates of co-use. The American Journal on Addictions, 24(2), 105–116. [DOI] [PubMed] [Google Scholar]
- Ramo DE, Liu H, & Prochaska JJ (2012). Tobacco and marijuana use among adolescents and young adults: a systematic review of their co-use. Clinical Psychology Review, 32(2), 105–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter KP, Kaur H, Resnicow K, Nazir N, Mosier MC, & Ahluwalia JS (2005). Cigarette smoking among marijuana users in the United States. Substance Abuse, 25(2), 35–43. [DOI] [PubMed] [Google Scholar]
- Roberts W, Moore KE, Peltier MR, Verplaetse TL, Oberleitner L, Hacker R, & McKee SA (2018). Electronic Cigarette Use and Risk of Harmful Alcohol Consumption in the US Population. Alcoholism: Clinical and Experimental Research, 42(12), 2385–2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohsenow DJ, Monti PM, Colby SM, Gulliver SB, Sirota AD, Niaura RS, & Abrams DB (1997). Effects of alcohol cues on smoking urges and topography among alcoholic men. Alcoholism: Clinical and Experimental Research, 21(1), 101–107. [PubMed] [Google Scholar]
- Romer D, Betancourt L, Giannetta JM, Brodsky NL, Farah M, & Hurt H (2009). Executive cognitive functions and impulsivity as correlates of risk taking and problem behavior in preadolescents. Neuropsychologia, 47(13), 2916–2926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Saddleson ML, Kozlowski LT, Giovino GA, Hawk LW, Murphy JM, MacLean MG, Goniewicz ML, Homish GG, Wrotniak BH, & Mahoney MC (2015). Risky behaviors, ENDSarette use and susceptibility of use among college students. Drug and Alcohol Dependence, 149, 25–30. [DOI] [PubMed] [Google Scholar]
- Schweitzer KS, Chen SX, Law S, Van Demark MJ, Poirier C, Justice MJ, Hubbard WC, Kim ES, Lai Z, Wang M, Kranz WD, Carroll CJ, Ray BD, Bottman R, Goodpaster J, & Petrache I (2015). Endothelial disruptive pro-inflammatory effects of nicotine and ENDSarette vapor exposures. American Journal of Physiology-Lung, Cellular, and Molecular Physiology, 309(2), L175–L187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Söderpalm B, Ericson M, Olausson P, Blomqvist O, & Engel JA (2000). Nicotinic mechanisms involved in the dopamine activating and reinforcing properties of ethanol. Behavioural Brain Research, 113(1), 85–96. [DOI] [PubMed] [Google Scholar]
- Soneji S, Sargent J, & Tanski S (2016). Multiple tobacco product use among US adolescents and young adults. Tobacco Control, 25(2), 174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squeglia LM, Jacobus J, & Tapert SF (2009). The influence of substance use on adolescent brain development. Clinical EEG and Neuroscience, 40(1), 31–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squeglia LM, & Gray KM (2016). Alcohol and drug use and the developing brain. Current Psychiatry Reports, 18(5), 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong C, Juon HS, & Ensminger ME (2016). Effect of adolescent cigarette smoking on adulthood substance use and abuse: the mediating role of educational attainment. Substance Use & Misuse, 51(2), 141–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Surís JC, Berchtold A, & Akre C (2015). Reasons to use E-cigarettes and associations with other substances among adolescents in Switzerland. Drug and Alcohol Dependence, 153, 140–144. [DOI] [PubMed] [Google Scholar]
- Sussan TE, Gajghate S, Thimmulappa RK, Ma J, Kim J, Sudini K, & Biswal S (2015). Exposure to Electronic Cigarettes Impairs Pulmonary Anti-Bacterial and Anti-Viral Defenses in a Mouse Model. Plos ONE, 10(2), 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **.Tavolacci MP, Vasiliu A, Romo L, Kotbagi G, Kern L, & Ladner J (2016). Patterns of electronic cigarette use in current and ever users among college students in France: a cross–sectional study. BMJ Open, 6(5), e011344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tizabi Y, Copeland RL, Louis VA, & Taylor RE (2002). Effects of combined systemic alcohol and central nicotine administration into ventral tegmental area on dopamine release in the nucleus accumbens. Alcoholism: Clinical and Experimental Research, 26(3), 394–399. [PubMed] [Google Scholar]
- Unger JB, Soto DW, & Leventhal A (2016). E-cigarette use and subsequent cigarette and marijuana use among Hispanic young adults. Drug and Alcohol Dependence, 163, 261–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valjent E, Mitchell JM, Besson MJ, Caboche J, & Maldonado R (2002). Behavioural and biochemical evidence for interactions between Δ9-tetrahydrocannabinol and nicotine. British Journal of Pharmacology, 135(2), 564–578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Noortgate W, López-López JA, Marín-Martínez F, & Sánchez-Meca J (2013). Three-level meta-analysis of dependent effect sizes. Behavior Research Methods, 45(2), 576–594. [DOI] [PubMed] [Google Scholar]
- VanderVeen JD, Hershberger AR, & Cyders MA (2016). UPPS-P model impulsivity and marijuana use behaviors in adolescents: A meta-analysis. Drug and Alcohol Dependence, 168, 181–190. [DOI] [PubMed] [Google Scholar]
- Vergés A, Haeny AM, Jackson KM, Bucholz KK, Grant JD, Trull TJ, Wood PK, & Sher KJ (2013). Refining the notion of maturing out: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. American Journal of Public Health, 103(12), e67–e73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viechtbauer W (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(3), 1–48. [Google Scholar]
- Weitzman ER, & Chen YY (2005). The co-occurrence of smoking and drinking among young adults in college: national survey results from the United States. Drug and Alcohol Dependence, 80(3), 377–386. [DOI] [PubMed] [Google Scholar]
- *.Westling E, Rusby JC, Crowley R, & Light JM (2017). Electronic cigarette use by youth: Prevalence, correlates, and use trajectories from middle to high school. Journal of Adolescent Health, 60(6), 660–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Williams T, & White V (2018). What factors are associated with electronic cigarette, shisha-tobacco and conventional cigarette use? Findings from a cross-sectional survey of Australian adolescents. Substance Use & Misuse, 53(9), 1433–1443. [DOI] [PubMed] [Google Scholar]
- *.Wills TA, Gibbons FX, Sargent JD, & Schweitzer RJ (2017). How is the effect of adolescent e-cigarette use on smoking onset mediated: A longitudinal analysis. Psychology of Addictive Behaviors, 30(8), 876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills TA, Knight R, Sargent JD, Gibbons FX, Pagano I, & Williams RJ (2016). Longitudinal study of e-cigarette use and onset of cigarette smoking among high school students in Hawaii. Tobacco Control, tobaccocontrol-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winward JL, Hanson KL, Tapert SF, & Brown SA (2014). Heavy alcohol use, marijuana use, and concomitant use by adolescents are associated with unique and shared cognitive decrements. Journal of the International Neuropsychological Society, 20(8), 784–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeigler DW, Wang CC, Yoast RA, Dickinson BD, McCaffree MA, Robinowitz CB, & Sterling ML (2005). The neurocognitive effects of alcohol on adolescents and college students. Preventive Medicine, 40(1), 23–32. [DOI] [PubMed] [Google Scholar]


