Abstract
Background:
Few exercise training studies in patients with heart failure (HF) report adherence to guideline-recommended 150 minutes of moderate intensity exercise per week and no studies have focused on a primary outcome of adherence.
Methods and Results:
This randomized controlled trial evaluated the effect of a multi-component intervention (Heart failure Exercise And Resistance Training Camp - HEART Camp) on adherence to exercise (6, 12 and 18 months) compared to an enhanced usual care (EUC) group. Patients (n=204) were 55.4% male; average age 60.4 years; and 47.5 % non-Caucasian. The HEART Camp group had significantly greater adherence at 12 (42%) and 18 months (35%) compared to the EUC group (28% and 19%, respectively). No significant difference (p > 0.05) was found at 6 months. The treatment effect did not differ based on patient’s age, race, gender, marital status, type of HF (preserved or reduced ejection fraction) or NYHA class. Left ventricular ejection fraction (LVEF) significantly moderated the treatment effect with greater adherence at higher LVEF.
Conclusions:
The multi-component HEART Camp intervention did show efficacy with significant effects at 12 months and 18 months. Adherence levels remain modest indicating a need for additional research to address methods and strategies to promote adherence to exercise in patients with HF.
Keywords: exercise, heart failure, adherence, exercise training
Introduction
Adherence to the Heart Failure Society of America (HFSA) 2010 guidelines that recommend 30 minutes of supervised moderate intensity exercise five days per week1 is difficult for the 6.5 million patients with heart failure (HF).2–4 Studies indicate that between 40% and 91% of patients with HF do not engage in any regular exercise. Patients report fear of exercising5,6 and lack of opportunity or skills for exercise7 as reasons for not exercising. Programs designed to teach patients with HF how to exercise and to maintain the behavior of exercise are needed. In 2014 the Centers for Medicare and Medicaid (CMS) approved reimbursement for cardiac rehabilitation (CR) in beneficiaries with heart failure with reduced ejection fraction (HFrEF); however, in spite of this favorable step to provide access, very few (2.6%) actually participate in CR.8 Among those patients that do participate, many do not continue to exercise once the formal program is completed.9,10
Studies that focus on adherence to exercise are limited, and as a result, we know very little about effective strategies that improve adherence in patients living with chronic HF. Studies that specifically focused on adherence to exercise only considered short term (6 months or less) adherence outcomes.11–13 The multi-center HF-ACTION trial (Heart Failure – A Controlled Trial Investigating Outcomes of Exercise Training) reported adherence to exercise beyond 12 months and results showed adherence levels as low as 34% at 24 months.14 Adherence to exercise recommendations are not being met and there is need for a paradigm shift to focus on long-term adherence to exercise in the chronically ill population with heart failure. Therefore, the purpose of this study was to evaluate the effect of a federally funded (R01-HL112949) multi-component intervention (Heart failure Exercise And Resistance Training Camp - HEART Camp) on adherence to exercise and to explore selected demographic variables (race, gender, age, body mass index, and ejection fraction) as potential moderators of the effect of the HEART Camp intervention on adherence. Specific aims of the study were: 1) To evaluate the effect of HEART Camp on adherence to exercise and 2) to explore the effect of the demographic and clinical variables as potential moderators of the HEART Camp intervention on adherence. We hypothesized that subjects in the HEART Camp (HC) intervention group would have significantly greater adherence to exercise than the enhanced usual care (EUC) group at each time point (6, 12, and 18 months) with a maximum difference expected at 18 months.
Methods
Design.
A prospective, randomized two-group repeated measures experimental design with four data collection points (baseline, 6, 12 and 18 months) was used. Subjects were randomized to the 2 groups and stratified by site and gender. The 2010 HFSA guidelines recommend moderate intensity exercise training in a supervised setting; therefore, both groups (EUC and HC) received 9 supervised exercise training sessions during a 3 week run-in period and were instructed to then continue to exercise in the setting of a health care exercise facility. Only subjects who completed 6 or more of the 9 supervised exercise sessions were randomized. The 9 exercise training sessions prior to randomization included moderate-intensity aerobic (40%−80% heart rate reserve; HRR)15,16 and resistance (10–15 repetitions to volitional fatigue)17,18 training. The decision to only randomize individuals who attended at least 6 of the 9 sessions was made to insure safety of individuals to exercise since participants in the EUC group would not have close supervision of the exercise coach during the 18 months of exercise. We recognize this limits generalizability, but we feel it is an important first step in investigating adherence to exercise in individuals who have an initial desire to exercise and an informed understanding of exercise expectations. A cardiopulmonary exercise test was also completed on all subjects at the beginning of the study. The study protocol specifically provided the supervision needed to assure safety of all subjects.15,16,19,20 Access to the exercise training facility was provided for both groups (EUC and HC).
Setting and Sample.
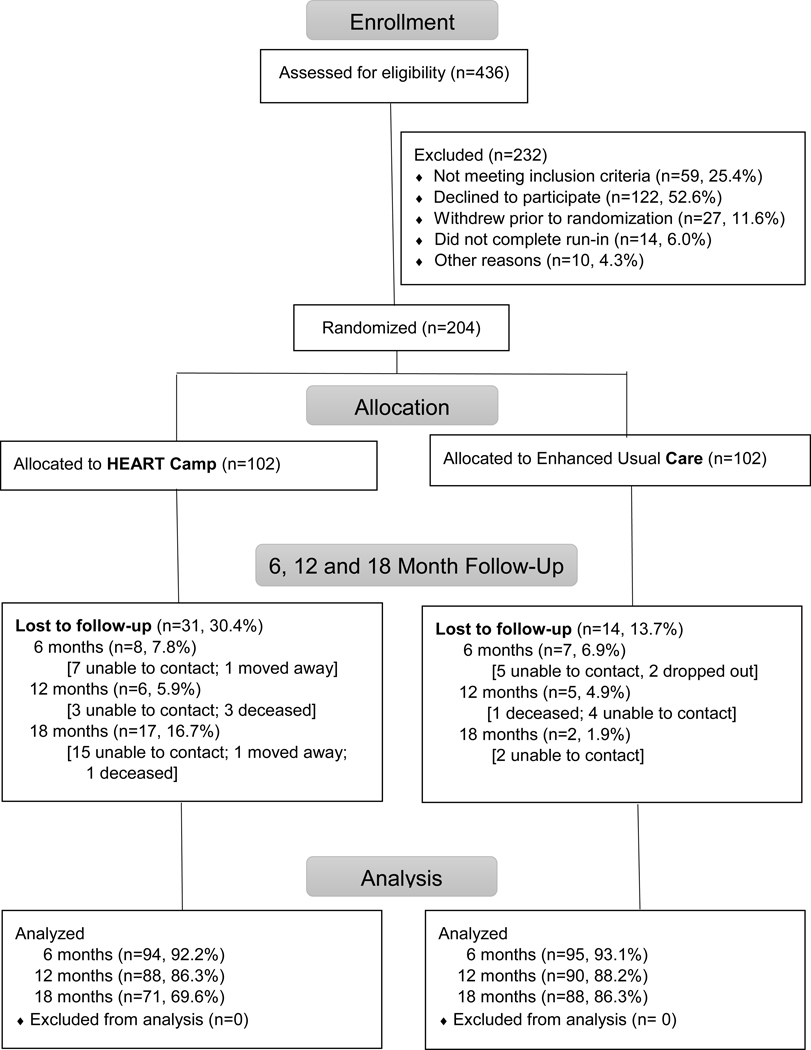
Permission to conduct the study was obtained from the institutional review boards at the University of Nebraska Medical Center, Wayne State University and Henry Ford Health System. Subjects were recruited from two urban medical centers: Bryan Heart Institute in Lincoln, NE and Henry Ford Hospital in Detroit, MI. Inclusion criteria for patients were: (a) diagnosis of HF (Stage C chronic HF confirmed by echocardiography and clinical evaluation) with preserved or reduced ejection fraction; (b) 19 years of age or greater; (c) able to speak and read English; (d) telephone access in home; and (e) stable pharmacologic therapy per guidelines for past 30 days. Exclusion criteria were: (a) clinical evidence of decompensated HF; (b) unstable angina pectoris; (c) myocardial infarction, coronary artery bypass surgery, or biventricular pacemaker less than 6 weeks prior; (d) orthopedic or neuromuscular disorders preventing participation in aerobic exercise and strength/resistance training; (e) participation in 3 times per week aerobic exercise in the past 8 weeks; (f) cardiopulmonary exercise test results that precluded safe exercise training; (g) plans to move more than 50 miles from the exercise site within the next year; (h) peak oxygen uptake (pVO2) in females > 21 ml/kg/min and in males > 24 ml/kg/min; and (i) pregnancy planned or current. All participants gave written informed consent. Numbers of subjects screened and randomized to each study arm are presented in the CONSORT diagram (Figure 1).
Figure 1.
CONSORT Diagram
HC Intervention.
The HC intervention was based on social-cognitive theory and used group-based (i.e. educational sessions) and individual-based (coach trainer) strategies to deliver the intervention. Five components: knowledge, attitudes, self-efficacy, self-management skills and social support were emphasized throughout the three intervention phases: adoption (baseline – 6 months), transition (months 7–12) and maintenance (months 13–18). In the adoption phase, six group-based educational sessions (attitudes toward exercise, pathophysiology of HF and benefits of exercise, HF symptoms and exercise, medications and exercise, sodium/fluid intake and relationship to exercise and exercising safely) were provided. The coach trainer met with individuals on a weekly basis during the adoption and transition phases. This meeting included review of the exercise diary, discussion of exercise prescriptions, goal setting, monitoring, relapse prevention and self-management strategies for exercise. Coaches contacted participants if they did not attend this weekly meeting. During the maintenance phase (13–18 months) participants submitted weekly exercise diaries and if a diary was not submitted the exercise coach followed up with a phone call to the participant. . The intervention protocol is described in detail elsewhere.21
Measures.
Demographic data (age, race, gender and marital status) were obtained at baseline. Clinical information (Body Mass Index, left ventricular ejection fraction [LVEF], type of HF [preserved or reduced ejection fraction] and New York Heart Association classification) was obtained from the subject’s record.
Adherence is defined as the extent to which a person’s behavior corresponds to the recommendations of a healthcare provider.22 Adherence behavior has been defined as meeting 80% of the recommended behavior 23,24 and this definition has been used in exercise trials to date 20,25 Consistent with the literature this study defined adherence as achieving at least 80% of the recommended 150 minutes (i.e., more than 120 minutes) of moderate intensity aerobic activity per week. Participants were directed to complete their exercise diaries on a daily basis which included information on date, duration of exercise (minutes) and average HR (intensity). Only minutes of exercise in the moderate intensity range (HRR 40–80%) were counted in measurement of adherence. Weekly adherence data were obtained from participants self-reported exercise diaries and verified with data obtained from a heart rate monitor. The 6, 12 and 18 month adherence levels were computed as the averages across the 4 weeks prior to each measurement time-point.
A heart rate monitor (Polar RS400, Polar Electro Inc., Lake Success, NY) was used to guide intensity of exercise and to validate self-reported diary data. Subjects were instructed to wear the Polar RS 400and record each exercise session. The Polar RS400 provided adequate storage of data and could be programmed with target heart rate ranges (THRR) using the Polar Pro Trainer software. The THRR for each subject was determined by the core lab from the cardio-pulmonary exercise (CPX) tests done at baseline using 40–80% HR reserve for each participant. Participants were provided with the THRR and asked to regulate the intensity of their exercise to keep their HR within this range. Data from the watch was downloaded using the Polar Pro Trainer software to obtain a breakdown on date, time spent in exercise, average HR and amount of exercise time within the THRR. Exercise coaches collected diaries and downloaded the stored heart rate monitor data from HC intervention participants during weekly coaching sessions. Research personnel collected this data for the EUC subjects by appointment every two months. Exercise duration data from the self-reported exercise diaries were validated and considered in the calculation of exercise adherence minutes if it was within 10% of the objective data from the Polar RS400 on exercise time spent above the minimum THRR (greater than 40% HRR). Exercise time spent below the THRR (below 40%HRR) was not considered in calculation of adherence minutes.
Statistical Analysis
A power analysis was completed using levels of adherence from HF-ACTION14 and our own pilot study data. An adherence level of 0.25 was the level of crossover in HF-ACTION for the control group and reported adherence in the exercise group was 0.38 at 12 months and 0.36 at 18 months. Our pilot study data achieved adherence of 86% at 3 months in the intervention group, therefore we expected to achieve adherence of at least 0.50 at 18 months. A one-tailed z-test of the difference in proportions of 0.50 would have power of 0.90 (α = 0.05) with a total sample size of 126 subjects. We recruited 246 patients (123 subjects from each study site) to allow for the following attrition rates (10% not meeting medical criteria for safe participation in the study; 30% failing to attend at least 6 of the 9 planned sessions during the run-in period; and an additional 15% attrition over the 18 months of the study) resulting in the final desired sample size of 63 per group (total N=126).
Descriptive statistics were calculated on adherence and all study variables. In order to assess adherence between groups at 18 months (primary aim), a chi-square test was used to test group differences in the proportion of the sample that adhered to at least 80% of the 150 minutes per week recommendation. A significance level was set at p < 0.05. Tests were carried out at 6, 12, and 18 months, the primary data collection points in the study. The analysis included all participants according to the condition to which they were assigned and was based on all available data. In order to assess the possible effect of attrition on outcomes, sensitivity analyses were performed. Attrition or “lost to follow-up” (n=45) is depicted on the consort diagram (Figure 1) and included: unable to contact (n=36); died (n=5); moved (n=2); dropped out (n=2). Chi-square tests at 6 and 12 months were analyzed both with and without participants who were lost to follow-up at 12 months. Further, a sensitivity analysis with generalized estimating equations (GEE) analysis was performed with both complete cases and all available data to test whether attrition has an impact on the group differences in adherence over the course of the study.
In order to explore effects of selected demographic variables on adherence, potential moderators of the effect of the intervention on adherence were tested. Logistic regression models were performed with adherence at 18 months as the dependent variable. The moderators tested were gender, age, race (Caucasian vs. non-Caucasian), BMI, and ejection fraction. For continuous moderators, the raw scores were used in the analysis, and median splits were only performed in order to create interaction plots if significant interactions were found. Significant moderator by group interactions indicate that the intervention effect varies as a function of participants’ levels on the moderating variables.
Results
Descriptive statistics for the primary outcomes of the study are presented in Table 1. Of the 204 patients included in the analysis, there were 113 men (55.4%) and 91 women (44.6%), with an average age of 60.4 years (SD = 11.5). There were 165 subjects (80.9%) with heart failure reduced ejection fraction (HFrEF) and 39 subjects (with heart failure preserved ejection fraction (HFpEF). Ninety-one of the 95 (19.1%) non-Caucasian subjects were African-American. The majority of subjects were New York Heart Association Classification (NYHA) II and III (n=186, 91.2%). Pharmacologic management included 97.5% (n=199) on beta blocker medications and 85.7% (n=175) on ace-inhibitor or angiotensin receptor blockers. No significant differences were found between groups for any of the demographic and clinical variables.
Table 1.
Descriptives of Sample - Demographic and Clinical Variables
| Intervention | Enhanced Usual Care | p value | |
|---|---|---|---|
| Number | 102 | 102 | |
| Demographic variables | |||
| Age, mean (SD) | 59.8 (12.6) | 60.9 (10.3) | .482 |
| Gender, female, n (%) | 45 (44.1%) | 46 (45.1%) | .888 |
| Married, n (%) | 52 (51.0%) | 61 (59.8%) | .205 |
| Non-Caucasian, n (%) | 51 (50.0%) | 44 (43.1%) | .326 |
| Clinical variables | |||
| HFrEF, n (%) | 85 (83.3%) | 80 (78.4%) | .373 |
| HFpEF, n (%) | 17 (16.7%) | 22 (21.6%) | |
| NYHA Class, n (%) | .248 | ||
| I | 5 (4.9%) | 11 (10.8%) | |
| II | 54 (52.9%) | 59 (57.8%) | |
| III | 42 (41.2%) | 31 (30.4%) | |
| IV | 1 (1.0%) | 1 (1.0%) | |
| Beta blocker medication, n (%) | 99 (97.1) | 100 (98.0) | .651 |
| ACE/ARB medication, n (%) | 92 (90.2%) | 83 (81.4%) | .071 |
| LVEF, mean (SD) | 39.3 (12.1) | 40.5 (14.0) | .504 |
| BMI, mean (SD) | 35.0 (8.6) | 34.7 (7.8) | .828 |
Abbreviations: HFrEF, heart failure with reduced ejection fraction; HFpEF, heart failure with preserved ejection fraction; NYHA, New York Heart Association Classification; ACE, Ace-Inhibitor; ARB, Angiotensin-receptor blocker; LVEF, left ventricular ejection fraction; BMI, Body mass index.
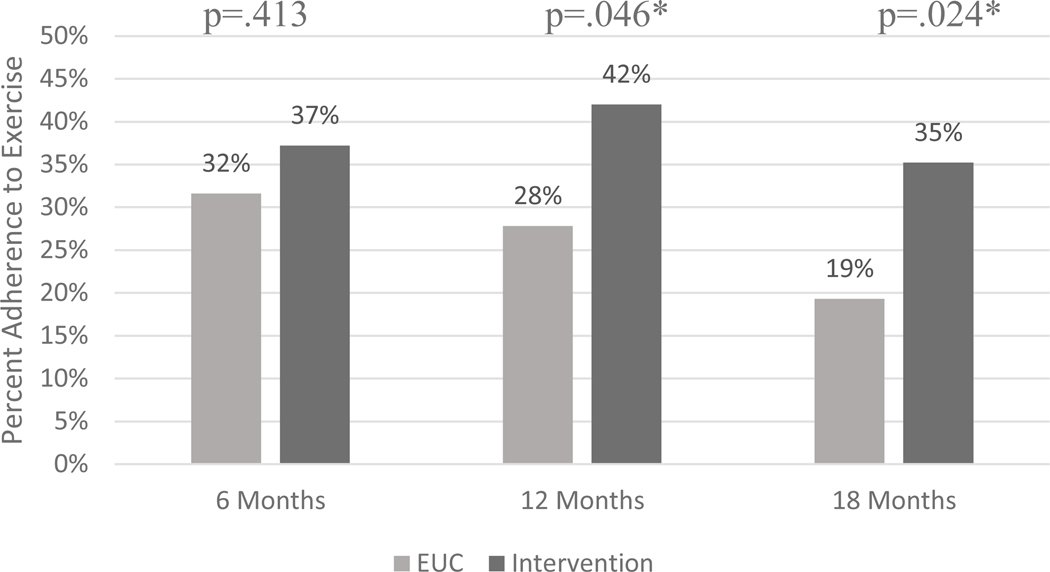
The HC group had significantly greater adherence at both 12 (42%) and 18 months (35%) compared to the EUC group (28% and 19%, respectively). No significant difference was found at 6 months (Figure 2).
Figure 2.
Adherence to exercise by group over time (all available data)
The total attrition at the end of the 18-month study was 45 participants (22.1)%, with 159 participants completing data collection at 18 months. Fifteen participants (7.4%) were lost by 6 months, an additional 11 (5.4%) were lost by the 12 month data collection point, and 19 (9.3%) more were lost by 18 months. Additional analyses were performed to examine attrition rates by group. Comparing the proportion of the sample present at 12 months (subjects had completed the 6-month data collection), no difference was found; 10.8% of the EUC group was not present at 12 months, compared to 13.7% of the intervention group (p = .539). At 18 months, however, there was a significant difference in dropout status between the groups (p = .002). More participants in the intervention group had either dropped out or did not provide adherence data (30.4%), compared to the EUC group (13.7%).
Due to the difference in dropout rate between 12 and 18 months, a sensitivity analysis was performed to determine if excluding those subjects who dropped out of the study between 12 and 18 months affected the analysis. We excluded subjects from the 6- and 12-month analyses who were not present at 18 months and found no change in the effects at 6 and 12 months (Figure 2). There was no difference in adherence rates between groups at 6 months (p = .242), and the intervention group had a significantly higher adherence rate than the enhanced standard care group (p = .017) at 12 months.
In order to assess the effect of participant dropout on group differences in adherence, generalized estimating equation (GEE) models were also performed, once with all available data, and again with completers only (i.e. sensitivity analysis; Table 2). The group effect was estimated at the last time point (18 months), since GEE uses the last time as the referent category. The group effect in both models showed significant differences in adherence at 18 months, indicating that attrition did not bias the group differences observed in adherence to exercise.
Table 2.
Sensitivity analysis using Generalized Estimating Equations (GEE)
| Sample | Term | χ2 | Df | p-value |
|---|---|---|---|---|
| Completers | Intercept | 22.83 | 1 | <.001 |
| (N = 159) | Group | 4.84 | 1 | .028 |
| Time | 8.60 | 2 | .014 | |
| Group*Time | 1.67 | 2 | .434 | |
| All Available | Intercept | 34.66 | 1 | <.001 |
| (N = 204) | Group | 3.85 | 1 | .049 |
| Time | 7.93 | 2 | .019 | |
| Group*Time | 2.00 | 2 | .367 | |
Note: Last time point is the referent category, so group effect is estimated at 18 months.
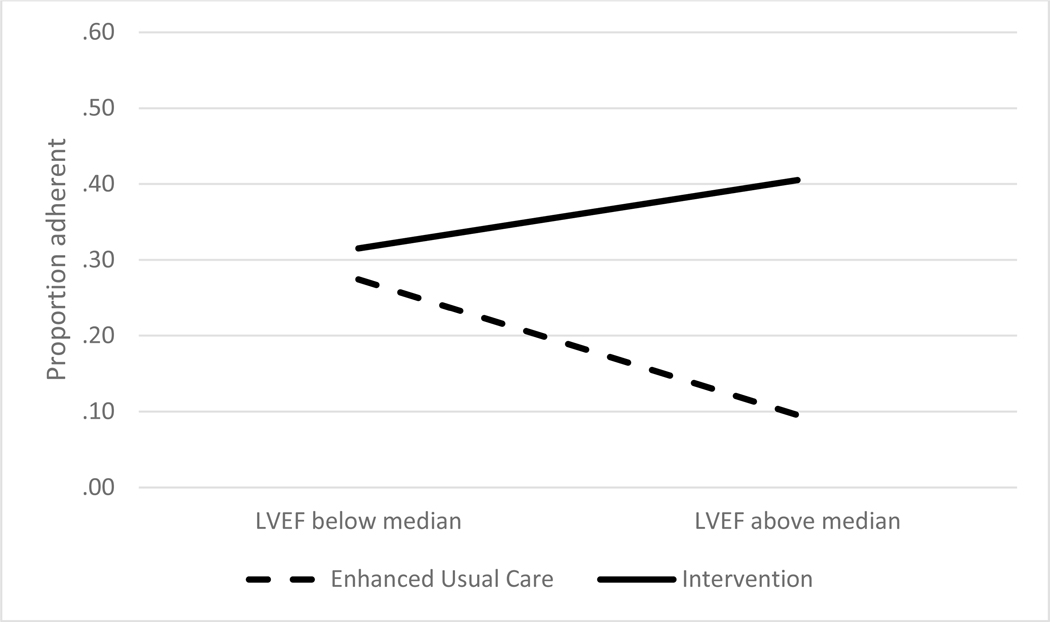
Demographic and clinical variables were tested for moderation effects of the intervention on adherence. Moderator variables are variables that affect the relationship between the independent (group) and dependent (adherence) variables. Results of the group by moderator interactions from logistic regression models testing moderators of group effects on adherence are presented in Table 3 (group by moderator interactions; one model was performed for each moderator). The treatment effect did not differ, or was equally effective, based on a patient’s age, site, race, gender, marital status or NYHA class. Left ventricular ejection fraction significantly moderated the treatment effect. The effect on adherence is greater at higher levels of LVEF. There is less of an effect for those with low LVEF (Figure 3).
Table 3.
Moderators of the intervention effect on adherence.
| B | S.E. | p | OR | 95% C.I. | |
|---|---|---|---|---|---|
| Treatment by Age | 0.007 | 0.033 | .835 | 1.007 | (0.943, 1.075) |
| Treatment by Non-White | −1.122 | 0.745 | .132 | 0.326 | (0.076, 1.403 |
| Treatment by Female | −1.383 | 0.856 | .106 | 0.251 | (0.047, 1.343) |
| Treatment by Married | 0.780 | 0.767 | .309 | 2.182 | (0.485, 9.811) |
| Treatment by BMI | 0.100 | 0.054 | .066t | 1.105 | (0.994, 1.230) |
| Treatment by LVEF | 0.079 | 0.032 | .013* | 1.082 | (1.017, 1.152) |
| Treatment by NYHA class | 0.609 | 0.955 | .524 | 1.838 | (0.283, 11.960) |
Significant at p < .05
marginal effect
Figure 3.
Moderator Analysis of LVEF
Note: A median split was performed in order to create an interaction plot for the significant interaction LVEF (Left ventricular ejection fraction)
Discussion
The multi-component HEART Camp intervention is the first RCT to examine adherence in a diverse sample of patients with HF and did show efficacy with significant effects at 12 months (42% adherent compared to 28% in EUC) and at 18 months (35% adherent compared to 19%). There was no difference in adherence between the HC group at 6 months (37% adherent) compared to the EUC group (32% adherent). This finding at 6 months suggests that giving patients access to a facility and providing 9 sessions of supervised exercise training can be equally effective in promoting short term adherence to exercise.
The highest percentage of subsequent adherence was 42% at 12 months which is modest but must be considered as successful behavior change in these patients with chronic HF. This level of adherence compares favorably to the HF-ACTION trial in which approximately 30% or more of the patients in the exercise training group trained at or above the target of 120 minutes of exercise per week at each of the time points.14
Comparison of adherence across studies is complicated by lack of consistent measurement.26 Studies that have reported long-term exercise adherence often only report adherence to number of sessions per week and not minutes of moderate intensity or above exercise. In the Exercise Rehabilitation Trial (EXERT) with HF patients, 43% of patients attended > 80% of scheduled program sessions at 3 months, with a noted decline over the 12 months of the study.27 Belardinelli et al. reported 88% adherence to 2 exercise sessions per week over a 10 year period.28 Poor adherence continues to be the “Achilles heel” of exercise programs.23
Testing for moderation effects demonstrated that the treatment effect did not differ based on a patient’s age, race, gender, marital status or NYHA class. This provides assurance that the HEART Camp intervention was equally effective for these different sub-groups. The significant moderating effect of LVEF attenuated the effect of the intervention for those with low LVEF compared to those with higher LVEF. While there was nothing in the methods or strategies of the intervention that would explain the moderating effect of LVEF it is not surprising that subjects with higher LVEF might respond better in terms of adherence. Exercising may not be as difficult for subjects with higher LVEF which could explain the interventions effect on adherence for these subjects. Findings from this study should not be generalized beyond this sample since this trial involved only two sites in the U.S. Although participants were only from two sites, the sample was sufficiently diverse relative to race and gender. The lack of moderation effects for race and gender demonstrated this intervention worked equally well regardless of race or gender. This finding was of particular importance given our baseline findings of less minutes of moderate and vigorous physical activity (MVPA) per day for women and non-Caucasian participants.29
While this trial demonstrated the efficacy of a multi-component intervention on adherence there remains a need for additional research addressing methods and strategies to promote adherence to recommendations for exercise in patients with HF. Cost-effective and innovative programs are needed to assist patients with HF to gain the knowledge, skills and motivation needed for long-term adherence to exercise.
Highlights:
The HEART Camp intervention significantly improved adherence to exercise at 12 and 18 months.
The intervention treatment effect did not differ based on patient’s age, race, gender, marital status, type of HF (preserved or reduced ejection fraction) or NYHA class.
Left ventricular ejection fraction (LVEF) significantly moderated the treatment effect with greater adherence at higher LVEF.
Adherence levels remain modest indicating a need for additional research to address methods and strategies to promote adherence to exercise in patients with HF.
ACKNOWLEDGEMENTS
Research reported in this publication was supported by the National Heart Lung and Blood Institute of the National Institutes of Health under award number R01HL112979. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Heart Failure Society of America, Lindenfeld J, Albert NM, et al. HFSA 2010 comprehensive heart failure practice guideline. J Card Fail. 2010;16(6):e1–194. [DOI] [PubMed] [Google Scholar]
- 2.van der Wal MH, van Veldhuisen DJ, Veeger NJ, Rutten FH Jaarsma T. Compliance with non-pharmacological recommendations and outcome in heart failure patients. Eur Heart J. 2010;31(12):1486–1493. [DOI] [PubMed] [Google Scholar]
- 3.Evangelista L, Doering LV, Dracup K, Westlake C, Hamilton M, Fonarow GC. Compliance behaviors of elderly patients with advanced heart failure. J Cardiovasc Nurs. 2003;18(3):197–206; quiz 207–8. [DOI] [PubMed] [Google Scholar]
- 4.Gary R Exercise self-efficacy in older women with diastolic heart failure: Results of a walking program and education intervention. J Gerontol Nurs. 2006;32(7):31–9; quiz 40–1. [DOI] [PubMed] [Google Scholar]
- 5.Rodriguez KL, Appelt CJ, Switzer GE, Sonel AF, Arnold RM. “They diagnosed bad heart”: A qualitative exploration of patients’ knowledge about and experiences with heart failure. Heart Lung. 2008;37(4):257–265. [DOI] [PubMed] [Google Scholar]
- 6.Pihl E, Fridlund B, Martensson J. Patients’ experiences of physical limitations in daily life activities when suffering from chronic heart failure; a phenomenographic analysis. Scand J Caring Sci. 2010. [DOI] [PubMed] [Google Scholar]
- 7.Jaarsma T, Abu-Saad HH, Dracup K, Halfens R. “Self-care behaviour of patients with heart failure”. Scand J Caring Sci. 2000;14(2):112–119. [PubMed] [Google Scholar]
- 8.Park LG, Schopfer DW, Zhang N, Shen H, Whooley MA. Participation in cardiac rehabilitation among patients with heart failure. J Card Fail. 2017;23(5):427–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Guiraud T, Granger R, Gremeaux V, et al. al. Telephone support oriented by accelerometric measurements enhances adherence to physical activity recommendations in noncompliant patients after a cardiac rehabilitation program. Arch Phys Med Rehabil. 2012;93(12):2141–2147. [DOI] [PubMed] [Google Scholar]
- 10.Dolansky MA, Stepanczuk B, Charvat JM, Moore SM. Women’s and men’s exercise adherence after a cardiac event. does age make a difference? Res Gerontol Nurs. 2010;3(1):30–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duncan KA, Pozehl B. Staying on course: The effects of an adherence facilitation intervention on home exercise participation. Prog Cardiovasc Nurs. 2002;17(2):59–65, 71. [DOI] [PubMed] [Google Scholar]
- 12.Duncan K, Pozehl B. Effects of an exercise adherence intervention on outcomes in patients with heart failure. Rehabil Nurs. 2003;28(4):117–122. [DOI] [PubMed] [Google Scholar]
- 13.Duncan K, Pozehl B, Norman JF, Hertzog M. A self-directed adherence management program for patients with heart failure completing combined aerobic and resistance exercise training. Appl Nurs Res. 2011;24(4):207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O’Connor CM, Whellan DJ, Lee KL, et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA. 2009;301(14):1439–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pozehl B, Duncan K, Hertzog M, Norman JF. Heart failure exercise and training camp: Effects of a multicomponent exercise training intervention in patients with heart failure . Heart Lung. 2010;39(6 Suppl):S1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Whellan DJ, O’Connor CM, Lee KL, et al. Heart failure and a controlled trial investigating outcomes of exercise training (HF-ACTION): Design and rationale. Am Heart J. 2007;153(2):201–211. [DOI] [PubMed] [Google Scholar]
- 17.Williams MA, Haskell WL, Ades PA, et al. Resistance exercise in individuals with and without cardiovascular disease: 2007 update: A scientific statement from the american heart association council on clinical cardiology and council on nutrition, physical activity, and metabolism. Circulation. 2007;116(5):572–584. [DOI] [PubMed] [Google Scholar]
- 18.Beckers PJ, Denollet J, Possemiers NM, Wuyts FL, Vrints CJ, Conraads VM. Combined endurance-resistance training vs. endurance training in patients with chronic heart failure: A prospective randomized study. Eur Heart J. 2008;29(15):1858–1866. [DOI] [PubMed] [Google Scholar]
- 19.American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. 8th ed. ed. Philadelphia, PA: Lippincott, Williams and Wilkins; 2010. [Google Scholar]
- 20.Mandic S, Tymchak W, Kim D, et al. Effects of aerobic or aerobic and resistance training on cardiorespiratory and skeletal muscle function in heart failure: A randomized controlled pilot trial. Clin Rehabil. 2009;23(3):207–216. [DOI] [PubMed] [Google Scholar]
- 21.Pozehl BJ, Duncan K, Hertzog M, et al. Study of adherence to exercise in heart failure: The HEART camp trial protocol. BMC Cardiovasc Disord. 2014;14:172–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization (WHO). Adherence to long-term therapies: Evidence for action. http://www.who.int/chp/knowledge/publications/adherence_report/en/. Accessed July/3, 2017.
- 23.Conraads VM, Deaton C, Piotrowicz E, et al. Adherence of heart failure patients to exercise: Barriers and possible solutions: A position statement of the study group on exercise training in heart failure of the heart failure association of the european society of cardiology. Eur J Heart Fail. 2012;14(5):451–458. [DOI] [PubMed] [Google Scholar]
- 24.Marti CN, Georgiopoulou VV, Giamouzis G, et al. Patient-reported selective adherence to heart failure self-care recommendations: A prospective cohort study: The atlanta cardiomyopathy consortium. Congest Heart Fail. 2013;19(1):16–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cooper LB, Mentz RJ, Sun JL, et al. Psychosocial factors, exercise adherence, and outcomes in heart failure patients: Insights from heart failure: A controlled trial investigating outcomes of exercise training (HF-ACTION). Circ Heart Fail. 2015;8(6):1044–1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Deka P, Pozehl B, Williams MA, Yates B. Adherence to recommended exercise guidelines in patients with heart failure. Heart Fail Rev. 2017;22(1):41–53. [DOI] [PubMed] [Google Scholar]
- 27.McKelvie RS, Teo KK, Roberts R, et al. Effects of exercise training in patients with heart failure: The exercise rehabilitation trial (EXERT). Am Heart J. 2002;144(1):23–30. [DOI] [PubMed] [Google Scholar]
- 28.Belardinelli R, Georgiou D, Cianci G, Purcaro A. 10-year exercise training in chronic heart failure: A randomized controlled trial. J Am Coll Cardiol. 2012;60(16):1521–1528. [DOI] [PubMed] [Google Scholar]
- 29.Pozehl BJ, Mcguire R, Duncan K, et al. Accelerometer-measured daily activity levels and related factors in patients with heart failure. Journal of Cardiovascular Nursing. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]