Introduction:
The purpose of this investigation is to assess the current utilization of telehealth capabilities at academic orthopaedic departments in the United States and to determine how practice patterns have been directly influenced by the coronavirus disease 19 (COVID-19) pandemic.
Methods:
Orthopaedic surgery programs participating in the Electronic Residency Application Service were identified. One hundred seventy-five (175) programs were presented with a seven-item questionnaire addressing whether each program is using telehealth services in response to the COVID-19 pandemic.
Results:
Of the 175 Electronic Residency Application Service participant orthopaedic programs, 168 responded for a total response rate of 96%. Of the 106 institutions using telehealth services, 88 (83%) cited the COVID-19 pandemic as the impetus for implementation of telehealth services. Institutions located in the Northeast and South regions were markedly more likely to offer telehealth services. Heat map analysis demonstrates an associative overlap of regional “hot spots” with direct comparison of COVID-19 cases in the United States and orthopaedic departments providing telehealth services.
Discussion:
This study demonstrates the impressive measures academic orthopaedic institutions are taking to meet the needs of our patients by identifying a notable increase in new telehealth offerings throughout the United States with a positive correlation with COVID-19 disease burden.
Rapidly evolving, modern information technologies have provided a host of options to improve communication across all fields, including medicine. Telehealth broadly refers to the use of electronic information and telecommunications technology to deliver and support health-related services including both clinical and nonclinical as well as provider education or medical training via the internet, video conferencing, wireless communications, streaming multimedia video, and store-and-forward telemedicine. Under the umbrella of telehealth is telemedicine, which specifically refers to the delivery of clinical care to a patient without an inpatient visit, often performed via secure HIPAA compliant video conferencing. It is typically used for follow-up visits of established patients, management of chronic conditions, specialist consultations, and medication management. More specifically, in a peer-reviewed article describing modern telemedicine, Sood et al1 defined it as a “branch of e-health that uses communications networks for delivery of healthcare services and medical education from one geographical location to another.” The authors also explained that telemedicine can also be used as a way “to overcome issues like uneven distribution and shortage of infrastructural and human resources.” Furthermore, telehealth can provide a safe means of delivering clinical care when the dangers of interpersonal contact outweigh the benefits of standard patient visits, as we are currently experiencing during the coronavirus disease 19 (COVID-19) pandemic.
Telehealth services have been used in several documented roles within orthopaedic practice including remote consultations, outpatient care, postoperative evaluations, and rehabilitation.2-6 Despite such publications highlighting utilization and benefits of telemedicine, to the authors' knowledge, it is not widely regarded as a standard service or patient expectation among most orthopaedic practices in the United States. Furthermore, there are a specific set of challenges associated with implementing telehealth services including the need for additional technological equipment, medical provider training, additional staff, patient education, altered reimbursement schedules, and absence of in-person physical examination, among others. Furthermore, there is a challenge to adhere to the HIPAA compliance, which often requires careful implementation of secure communication channels. However, given the unprecedented evolution of the COVID-19 pandemic, the federal government has suspended the established HIPAA compliance requirements and related telecommunications for telehealth services. In addition, the Centers for Medicare and Medicaid Services announced expansion of telehealth services on an emergency basis via the 1,135 waiver authority and Coronavirus Preparedness and Response Supplemental Appropriations Act. This waiver allows for Medicare coverage of “office, hospital and other visits furnished via telehealth across the country and including in patient's places of residence starting March 6, 2020.”7 This has greatly increased the providers' ability to maintain continuity of care for patients at a time when social distancing, self-isolation, and quarantine have become the new norm.
The purpose of this investigation is to assess the current utilization of telehealth capabilities at academic orthopaedic departments in the United States and to determine how practice patterns have been directly influenced by the COVID-19 pandemic. The authors hypothesize that orthopaedic departments have only recently begun to implement telehealth services in response to the pandemic with most those departments located in regions of high disease burden.
Methods
All orthopaedic surgery programs participating in the Electronic Residency Application Service (ERAS) were identified. One hundred seventy-five (175) participant orthopaedic programs were directly contacted via telephone on March 23, 2020, through March 26, 2020, to ascertain their current utilization of telehealth services (Tables 1 and 2). The seven-item questionnaire addressed whether each program is currently using telehealth services and if such offerings have only recently been implemented as a direct response to the COVID-19 pandemic. For those programs not offering telehealth services at present, we further inquired as to whether they were in the process of actively setting it up. We further attempted to ascertain which level of provider would perform the telehealth visits, which were categorized as physician (MD), advanced practice provider (APP), or trainee (fellow or resident physician). Each program was additionally asked if preappointment imaging would be available and if a co-payment and referral are requirements for a telehealth visit. Finally, we inquired as to which electronic medical/health record (EMR/EHR) is being used at each institution. In addition, geographic region was determined for the comparison of regional differences between the Northeast, South, Midwest, and West regions (Tables 1 and 3). These geographic data were further used to create a heat map of orthopaedic departments providing telehealth services (Figure 2) with direct comparison with a heat map produced by the Centers for Disease Control and Prevention (CDC) depicting the COVID-19 disease burden in the United States (Figure 1). In addition, select “hot spots” of disease burden from differing regions of the United States were identified by the number of COVID-19 positive patients, per CDC reporting, and evaluated regarding the number of institutions providing telehealth services before the pandemic and those providing new telehealth services in direct response to the pandemic (Table 4).
Table 1.
Descriptive Statistics of Orthopaedic Departments Participating in the Electronic Residency Application Service
| Institution Characteristics (N = 168)a | N (%) |
| Orthopaedic departments offering telehealth visits | |
| Yes | 106 (63.1) |
| No | 62 (36.9) |
| Currently setting up | 14 (22.6) |
| No comment | 48 (77.5) |
| Region | |
| South | 56 (33.3) |
| Midwest | 46 (27.4) |
| Northeast | 43 (25.6) |
| West | 23 (13.7) |
| EMR/her | |
| Epic | 99 (58.9) |
| Cerner | 33 (19.6) |
| Allscripts | 12 (7.1) |
| Athena | 4 (2.4) |
| eClinicalWorks | 3 (1.79) |
| NextGen | 2 (1.19) |
| Otherb | 15 (8.9) |
EMR/EHR = electronic medical/health record
Seven institutions were unable to be reached by phone and were thus excluded from analysis.
EMR/EHR with a frequency <2 were grouped together as “Other.”
Table 2.
Characteristics of Orthopaedic Departments Providing Telehealth Services
| Institution Characteristics (N = 106) | N (%) |
| Has your telehealth service been recently implemented as a direct result of the novel coronavirus (COVID-19) pandemic? | |
| Yes | 88 (83.0) |
| No | 18 (17.0) |
| What level of provider will perform the telehealth visit? | |
| MD only | 75 (70.8) |
| MD + APP | 30 (28.3) |
| APP only | 1 (0.9) |
| Trainee | 0 (0.0) |
| Is it possible to get pre-appointment imaging? | |
| Yes | 51 (48.1) |
| No | 17 (16.0) |
| Don't know | 38 (35.8) |
| Is a co-payment required? | |
| Yes | 57 (53.8) |
| No | 13 (12.3) |
| Don't know | 36 (34.0) |
| Is a referral required? | |
| Yes | 57 (53.8) |
| No | 16 (15.1) |
| Don't know | 33 (31.1) |
| Which EMR/EHR does your department use? | |
| Epic | 73 (68.9) |
| Cerner | 13 (12.3) |
| Athena | 4 (3.8) |
| Allscripts | 3 (2.8) |
| eClinicalWorks | 3 (2.8) |
| NextGen | 2 (1.9) |
| Othera | 8 (7.5) |
APP = advanced practice provider, COVID-19 = coronavirus disease, EMR/EHR = electronic medical/health record
EMR/EHR with an overall frequency of one were grouped together as “Other.”
Table 3.
Orthopaedic Telehealth Services in the United States
| Characteristic | Telehealth,a N (%) | OR (95% CI) | P Value | Overall P Value |
| Region | 0.029b | |||
| Midwest | 21/46 (45.7) | Reference | — | |
| Northeast | 32/43 (74.4) | 3.46 (1.41-8.5) | 0.007b | |
| South | 37/56 (66.1) | 2.32 (1.04-5.16) | 0.04b | |
| West | 16/23 (69.6) | 2.72 (0.94-7.86) | 0.64 | |
| EMR/EHR | 0.003b | |||
| Epic | 73/99 (73.7) | — | — | |
| Cerner | 13/33 (39.4) | — | — | |
| Athena | 4/4 (100) | — | — | |
| Allscripts | 3/12 (25) | — | — | |
| eClinicalWorks | 3/3 (100) | — | — | |
| NextGen | 2/2 (100) | — | — | |
| Other | 8/15 (53.3) | — | — |
CI = confidence interval, EMR/EHR = electronic medical/health record, OR = odds ratio
Reported as # institutions using telehealth/total institutions contacted (%).
P < 0.05.
ORs and subgroup P values for region were calculated using a univariate logistic regression.
Overall P values were calculated from the chi-square or Fisher exact test for categorical variables.
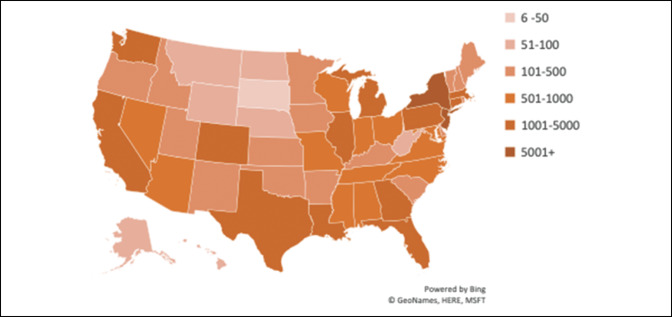
Figure 2.
Chart showing the number of orthopaedic departments providing telehealth services as of March 26, 2020.
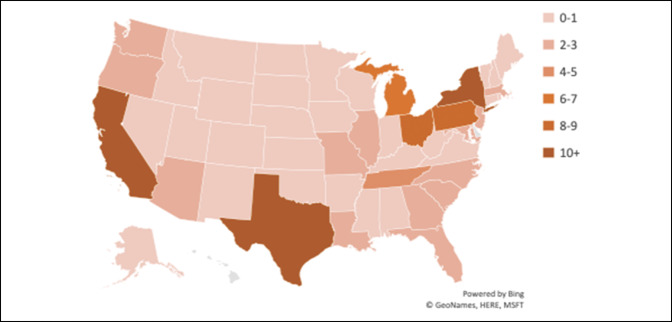
Figure 1.
Chart showing the number of coronavirus disease 19 cases in the United States as of March 26, 2020.
Table 4.
Correlation of COVID-19 Regional Disease Burden With Orthopaedic Telehealth Services
| State | COVID-19 Casesa | Before Pandemicb | New In Response to Pandemicb | % Increase |
| New York | 38,977 | 2 | 11 | 550 |
| California | 3,777 | 1 | 9 | 900 |
| Pennsylvania | 1,688 | 4 | 6 | 150 |
| Texas | 1,396 | 0 | 12 | >1,200 |
COVID-19 = coronavirus disease 19
Centers for Disease Control and Prevention Data as of March 26, 2020.
Number of orthopaedic departments providing telehealth services.
Statistical analysis was performed via utilization of the statistical software package STATA 14.2 (StataCorp LLC). Overall P values were calculated via the chi-square analysis and Fisher exact test for categorical variables. Odds ratios and subgroup regional P value analysis was calculated via univariate logistic regression. Statistical significance was set a priori at P < 0.05.
Results
Of the 175 ERAS participant orthopaedic programs, 168 responded for a total response rate of 96% (Table 1). The geographic regional distribution of orthopaedic departments consists of 43 (25.6%) in the Northeast, 46 (27.4%) in the Midwest, 56 (33.3%) in the South, and 23 (13.7%) in the West (Table 1). Of the 168 institutions included for analysis, 106 (63%) are currently offering telehealth services as an option for orthopaedic appointments. Of note, 14 (22.6%) of the 62 institutions not currently offering telehealth services are actively setting up their telehealth capabilities.
Of the 106 institutions using telehealth services, 88 (83%) cited the COVID-19 pandemic as the impetus for implementation of telehealth services (Table 2). Seventy-five (70.8%) reported performing telehealth visits with a MD as the primary provider. Thirty (28.3%) institutions use both MDs and APPs with 1 (0.9%) using only APPs as their main provider. No institutions are using trainees (fellow or resident physician) in the delivery of telehealth services. Co-payments and referrals are required at 57 institutions (53.8%). At the time of contact, 13 institutions(12.3%) were waiving co-payments and 16 (15.1%) did not require a referral. In addition, Epic (Epic Systems Corporation) (N = 73, 68.9%) was identified as the most frequently used EMR/EHR in those institutions providing telehealth services.
Regarding geographic region, 74.4% of institutions in the Northeast (32 of 43) offer telehealth services compared with 69.6% in the West (16 of 23), 66.1% in the South (37 of 56), and 45.7% in the Midwest (21 of 46) (Table 3). Institutions located in the Northeast and South regions were significantly more likely to offer telehealth services with odds ratios and P values of 3.46 and 0.007 as well as 2.32 and 0.04, respectively. In addition, the type of EMR/EHR used by each institution was significantly associated with the availability of telehealth services with a P value of 0.003.
The heat map analysis demonstrated an associative overlap of regional “hot spots” with a direct comparison of COVID-19 cases in the United States (Figure 1) and orthopaedic departments providing telehealth services (Figure 2). Additional subgroup analysis of regional “hot spots” demonstrated a 550% increase in telehealth services provided in the state of New York in response to the COVID-19 pandemic, with a 900% increase in California, a 150% increase in Pennsylvania, and more than a 1,200% increase in Texas.
Discussion
In this study, we investigated the current utilization of telehealth services at 168 academic orthopaedic departments across the United States to determine practice patterns in response to the novel coronavirus (COVID-19) pandemic. Consistent with our hypothesis, we identified a notable increase in new telehealth offerings in orthopaedic departments throughout the United States, with a positive correlation to COVID-19 disease burden as depicted by the heat map analysis (Figures 1 and 2).
The epicenter of the novel COVID-19 outbreak emerged in December 2019 from Wuhan, People's Republic of China, and has rapidly spread across the globe, requiring the World Health Organization (WHO) to officially declare COVID-19 a pandemic on March 11, 2020. Per the WHO, “a pandemic is the worldwide spread of a new disease” with the WHO reporting 638,146 confirmed cases and 30,105 confirmed deaths in 203 countries.8,9 In the United States, the CDC reports the burden of disease as 122,653 total cases with 2,112 confirmed deaths across all 50 states, the District of Columbia, Puerto Rico, Guam, Northern Marianas, and the U.S. Virgin Islands as of March 29, 2020.10 In response to the rapid spread of COVID-19, national guidelines were issued by the White House Coronavirus Task Force on March 16, 2020, with a series of recommendations to slow the spread of disease.11 Simultaneously, the Centers for Medicare and Medicaid Services, the American College of Surgeons, the U.S. Surgeon General, and the American Academy of Orthopaedic Surgeons issued recommendations to delay elective surgeries in response to the rapidly evolving pandemic.12-14 These collective recommendations have been issued during an unprecedented time requiring rapid adjustment in how the orthopaedic community continues to deliver high-quality patient care. As such, the Office for Civil Rights at the U.S. Department of Health and Human Services announced an historic expansion of telehealth access to combat the COVID-19 pandemic.15
Given these measures, we identified that 63.1% of the ERAS participant orthopaedic institutions are providing telehealth services with an additional 22.5% currently setting up telehealth capabilities. Furthermore, 83% of the 106 institutions currently providing telehealth visits have only recently implemented such services in direct response to the COVID-19 pandemic with 68.9% using Epic. This clearly demonstrates the rapid and appropriate implementation of telehealth services by academic orthopaedic institutions throughout the country with the Northeast and South regions markedly more likely to offer telehealth services. This is distinctly portrayed via the heat map analysis demonstrating a positive correlation between telehealth services offered by academic orthopaedic departments and COVID-19 disease burden in the United States. In response to the pandemic, a significant increase in telehealth services have been realized in specific “hot spot” regions with a 550% increase in the state of New York and a 900% increase in California.
The concept of using telehealth services to improve patient care is not new in orthopaedic practice. Sathiyakumar et al16 compared patient satisfaction between telemedicine and in-person follow-up appointments for orthopaedic trauma patients. A total of 24 patients were enrolled and randomized to each group with a total of four follow-up appointments during a 6-month period. The authors reported no difference in patient satisfaction between telemedicine and in-person clinic visits; however, no one in the telemedicine group took time off from work and spent markedly less time on their visits compared with the clinic follow-up group with most patients (75%) agreeing to future follow-up visits with telemedicine. In addition, Sharareh and Schwarzkopf17 found that patients receiving telemedicine visits after total joint arthroplasty reported higher satisfaction with less calls to the clinic staff. Similarly, in a systematic review by Gilbert et al,18 patients readily accepted the idea of using real time video conferencing for their visits with orthopaedic surgery providers.
This study demonstrates the impressive measures academic orthopaedic institutions are taking to meet the needs of our patients during unprecedented times and can serve as a roadmap for other sections of the healthcare community in the implementation of telehealth services. The telehealth landscape may be permanently changed in response to the COVID-19 pandemic, with evolving telehealth deliverables as valuable complements to in-person orthopaedic clinic visits with net improvement realized in the quality and value of care delivered.
Footnotes
Dr. Li or an immediate family member serves as a paid consultant to FH Ortho. Dr. Levine or an immediate family member serves as an unpaid consultant to Zimmer Biomet and serves as a board member, owner, officer, or committee member of the American Shoulder and Elbow Surgeons. None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Parisien, Shin, Constant, Dr. Saltzman, and Dr. Trofa.
References
- References printed in bold type are those published within the past 5 years.
- 1.Sood S, Mbarika V, Jugoo S, et al. : What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed J E Health 2007;13:573-590. [DOI] [PubMed] [Google Scholar]
- 2.Buvik A, Bergmo TS, Bugge E, Smaabrekke A, Wilsgaard T, Olsen JA: Cost-effectiveness of telemedicine in remote orthopedic consultations: Randomized controlled trial. J Med Internet Res 2019;21:e11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buvik A, Bugge E, Knutsen G, Småbrekke A, Wilsgaard T: Quality of care for remote orthopaedic consultations using telemedicine: A randomised controlled trial. BMC Health Serv Res 2016;16:483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kane LT, Thakar O, Jamgochian G, et al. : The role of telehealth as a platform for postoperative visits following rotator cuff repair: A prospective, randomized controlled trial. J Shoulder Elbow Surg 2020;29:775-783. [DOI] [PubMed] [Google Scholar]
- 5.Pastora-Bernal JM, Martín-Valero R, Barón-López FJ, Estebanez-Pérez MJ: Evidence of benefit of telerehabitation after orthopedic surgery: A systematic review. J Med Internet Res 2017;19:e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Russell TG, Buttrum P, Wootton R, Jull GA: Internet-based outpatient telerehabilitation for patients following total knee arthroplasty: A randomized controlled trial. J Bone Joint Surg Am 2011;93:113-120. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Medicare and Medicaid Services (CMS): Medicare telemedicine health care provider fact sheet. 2020. Available at: https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet. Accessed April 2, 2020.
- 8.World Health Organization (WHO): What is a pandemic? 2010. Available at: https://www.who.int/csr/disease/swineflu/frequently_asked_questions/pandemic/en/. Accessed March 29, 2020.
- 9.World Health Organization (WHO): Coronavirus disease (COVID-19) pandemic. 2020. Available at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed March 29, 2020.
- 10.U.S. Centers for Disease Control and Prevention (CDC): Coronavirus disease 2019 (COVID-19): U.S. at a glance. 2020. Available at: https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Accessed March 29, 2020.
- 11.White House Coronavirus Task Force: The president's coronavirus guidelines for America. 2020. Available at: https://www.whitehouse.gov/wp-content/uploads/2020/03/03.16.20_coronavirus-guidance_8.5x11_315PM.pdf. Accessed March 29, 2020.
- 12.Centers for Medicare and Medicaid Services (CMS): CMS adult elective surgery and procedures recommendation: Limit all non-essential planned surgeries and procedures, including dental, until further notice. 2020. Available at: https://www.cms.gov/files/document/31820-cms-adult-elective-surgery-and-procedures-recommendations.pdf. Accessed March 29, 2020.
- 13.American College of Surgeons (ACS): COVID-19: Elective case triage guidelines for surgical care. 2020. Available at: https://www.facs.org/covid-19/clinical-guidance/elective-case. Accessed March 29, 2020.
- 14.American Academy of Orthopaedic Surgeons (AAOS): COVID-19: Recommendations for elective surgery. 2020. Available at: https://www.aaos.org/about/covid-19-information-for-our-members/. Accessed March 29, 2020.
- 15.U.S. Department of Health and Human Services (HHS): Secretary azar announces historic expansion of telehealth access to combat COVID-19. 2020. Available at: https://www.hhs.gov/about/news/2020/03/17/secretary-azar-announces-historic-expansion-of-telehealth-access-to-combat-covid-19.html. Accessed March 29, 2020.
- 16.Sathiyakumar V, Apfeld JC, Obremskey WT, Thakore RV, Sethi MK: Prospective randomized controlled trial using telemedicine for follow-ups in an orthopaedic trauma population: A pilot study. J Orthop Trauma 2015;29:e139-e145. [DOI] [PubMed] [Google Scholar]
- 17.Sharareh B, Schwarzkopf R: Effectiveness of telemedicine applications in postoperative follow-up after total joint arthroplasty. J Arthroplasty 2014;29:e918-e922. [DOI] [PubMed] [Google Scholar]
- 18.Gilbert AW, Jaggi A, May CR: What is the patient acceptability of real time 1:1 videoconferencing in an orthopaedics setting? A systematic review. Physiotherapy 2018;104:178-186. [DOI] [PubMed] [Google Scholar]