Abstract
Background
The Frequency Etiology Direction Severity (FEDS) system was developed as a simple but reliable method for classifying shoulder instability based on four factors attainable by history and physical examination: Frequency = Solitary, Occasional, or Frequent; Etiology = Traumatic or Atraumatic; Direction = Anterior, Posterior, or Inferior; Severity = Subluxation or Dislocation. This study investigated epidemiology and two-year surgical outcomes for FEDS categories in the prospective Multicenter Orthopaedic Outcomes Network (MOON) Shoulder Instability cohort.
Methods
1204 patients were assigned to FEDS categories at the time of surgery. Follow-up data was available for 636/734 patients (86.6%) who were at a minimum 2 years postop. The most common categories were further analyzed by patient reported outcomes (ASES, WOSI, SANE) and rates of recurrent subluxation, dislocation, and revision surgery.
Results
Sixteen of the 36 FEDS categories represented at least one percent of patients. Occasional traumatic anterior dislocation (OTAD) was the most common category with 16.4% of patients. Five other anterior categories (STAS, OTAS, FTAS, STAD, FTAD) and one posterior category (STPS) represented at least five percent of patients. Patient reported outcomes (PROs) improved significantly for each category. The highest rates of recurrent subluxation occurred in FTAS, OTAS, and OTAD; dislocation in OTAS and FTAS; and further surgery in OTAD. The lowest rates of failure occurred in STPS. Downward trends in PROs and higher failure rates were noted with increasing number of dislocations.
Conclusion
Different FEDS categories showed varying degrees of improvement and failure rates, indicating that the system can be used to provide prognostic insight for presurgical education. Overall, outcomes decreased with higher number of preoperative dislocations.
Level of Evidence
Level II; Prospective Cohort Design; Treatment Study
Keywords: shoulder, instability, dislocation, subluxation, FEDS classification, PROs
Shoulder instability is a common orthopedic condition, especially in a young active population.9; 19 However, instability of the glenohumeral joint is a heterogeneous entity in terms of history, presentation, and optimal treatment. Consequently, multiple classification schemes have been developed. Perhaps the most commonly used system is TUBS (traumatic, unilateral, Bankart, surgery) and AMBRI (atraumatic, multidirectional, bilateral, rehabilitation, inferior) described by Thomas and Matsen.28 This system includes two overarching categories, broadly defined by their preferred treatment of surgical versus non-surgical. Other classifications systems, such as that published by Silliman and Hawkins, utilize an algorithmic method based on factors deemed clinically important.25 Gerber and Nyffeler described yet another classification scheme defining dynamic glenohumeral instability by direction and presence of hyperlaxity.5
The Frequency, Etiology, Direction, Severity (FEDS) classification system for shoulder instability was developed in 2010 by Kuhn after reviewing eighteen proposed systems to determine which criteria were most commonly included.11 Only the four namesake FEDS variables were included by at least fifty percent of the reviewed classification systems. In the FEDS system, frequency is defined by episodes per year: solitary (1 episode), occasional (2–5 episodes), or frequent (>5 episodes). Etiology is defined as traumatic or atraumatic. Direction is defined as anterior, posterior, or inferior. Severity is defined as dislocation or subluxation and is determined by whether or not the patient required assistance from another person for reduction. The advantages of the FEDS system stem from both simplicity of classification and the agreed-upon importance of each component.
The FEDS system was validated in 2011 showing high intra- and inter-rater agreement, each ranging from 84–97% and 82–90% respectively for the four individual factors.12 Overall, the system allows for thirty-six possible combinations, represented by the first letter of each variable in order (e.g. Solitary Traumatic Anterior Dislocation = STAD); however, fewer categories are commonly seen. Previous work has described epidemiologic data from a cohort consisting of all patients seen for shoulder instability treated with or without surgery at three institutions over a six-year period.7 Sixteen categories represented greater than one percent of the cohort, and six represented greater than five percent. Lebus et al also looked at the same retrospective cohort to determine which FEDS variables were associated with operative intervention.13
The purpose of this study was to investigate the epidemiology of the FEDS classification system and two-year outcomes in a prospective, multicenter cohort of patients undergoing operative treatment for glenohumeral instability. Epidemiology, patient reported outcomes (PROs), and failure rates were investigated.
Methods
All patients enrolled in the Multicenter Orthopaedic Outcomes Network (MOON) Shoulder Instability cohort between 11/5/2012 and 11/30/2018 were included. The MOON Shoulder Instability cohort is an IRB approved prospective multicenter cohort consisting of patients undergoing surgical stabilization of the glenohumeral joint. It consists of twenty-five sports medicine or shoulder and elbow fellowship-trained surgeons at eleven institutions. Data were recorded by surgeons at initial visit, time of surgery, and at 6 months postoperatively. Patient reported outcomes were obtained at the initial visit and two years after surgery. The overall epidemiology of the cohort has been previously described.10
Demographics for the entire cohort were analyzed along with the four FEDS variables and sport participation. The patients were then assigned to FEDS categories to determine which were most clinically relevant for our operative cohort. A power analysis was performed to determine the minimum number of patients in a given FEDS category necessary to detect pre- to postoperative changes in patient-reported outcomes. Using a paired t-test design and an alpha level of 0.05, 34 patients would be needed in order to detect a moderate effect size (Cohen’s d = 0.50; G*Power version 3.1.9.3, Heinrich Heine University, Dusseldorf, Germany). Based on this calculation, we only assessed pre- to postoperative changes in patient-reported outcome scores for FEDS classifications with at least 34 patients (7 categories). Patients with 2-year follow-up were included in the analysis. PROs included the American Shoulder and Elbow Surgeons (ASES) shoulder score, the Western Ontario Shoulder Instability (WOSI) index, and the Single Assessment Numeric Evaluation (SANE). Recurrent subluxation, recurrent dislocation, and repeat surgery were also analyzed to evaluate rates of failure.
All data were captured and stored via Teleform (OpenText, Waterloo, ON, Canada) or REDCap (REDCap, Nashville, TN, USA).6 Statistical analysis was performed using SPSS Statistics (Version 25.0.0.0; IBM, Armonk, NY, USA). Paired t-tests were used to compare baseline and two-year PRO scores. MOON Shoulder Instability is supported by the Orthopaedic Research and Education Foundation.
Results
Epidemiology
1204 patients were enrolled at the time of analysis and included in baseline (time zero) analysis. The study cohort consisted primarily of young males (82.0% male, mean age 24.6 ± 8.9) with traumatic (82.9%) anterior (76.3%) instability. 71.6% of the cohort was injured while participating in sports. Table I summarizes demographic characteristics.
Table I.
Demographics for All Enrolled Patients a
| Sex | |
| Male | 82.0 (987) |
| Female | 18.0 (217) |
| Age | 24.6 ± 8.9 (12–66) |
| Affected Arm | |
| Right | 51.7 (622) |
| Left | 48.3 (582) |
| Injured During Sport | |
| Yes | 71.6 (855) |
| No | 28.4 (339) |
| Frequency | |
| Solitary | 41.4 (498) |
| Occasional | 35.3 (425) |
| Frequent | 23.3 (281) |
| Etiology | |
| Traumatic | 82.9 (998) |
| Atraumatic | 17.1 (206) |
| Direction | |
| Anterior | 76.3 (919) |
| Posterior | 23.2 (279) |
| Inferior | 0.5 (6) |
| Severity | |
| Subluxation | 54.6 (655) |
| Dislocation | 45.4 (549) |
Reported as % (n) or mean ± SD (range). P values calculated using chi square goodness of fit.
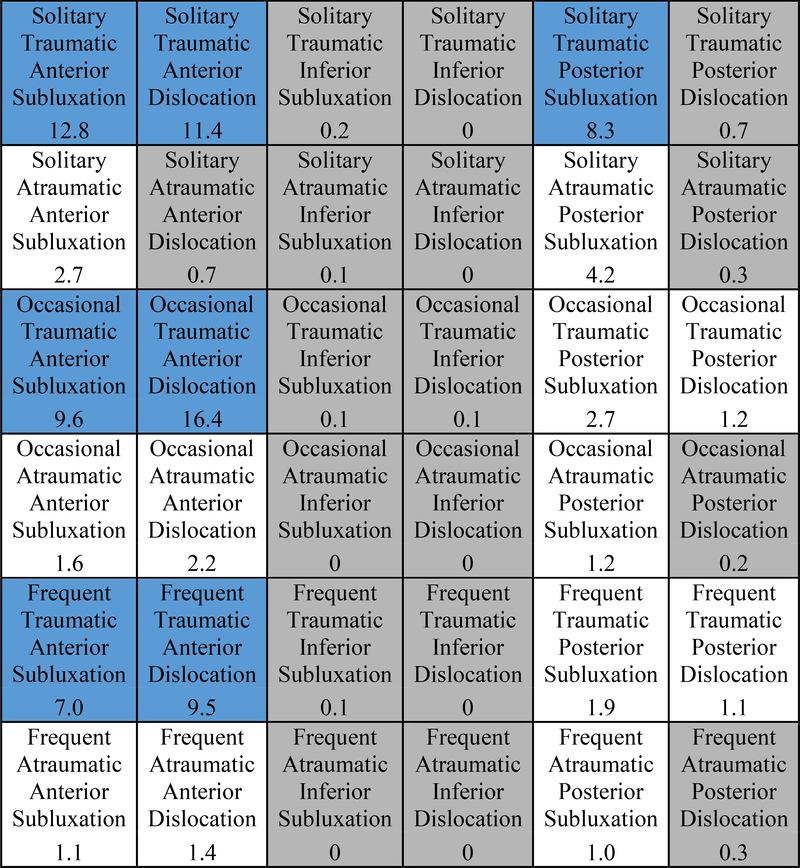
All 1204 patients were classified using the FEDS system. Nineteen FEDS categories represented at least one percent of the cohort, as seen in Figure I. Occasional traumatic anterior dislocation (OTAD) represented the most common category with 16.4% of patients, while solitary traumatic anterior subluxation (STAS) and solitary traumatic anterior dislocation (STAD) followed with 12.8% and 11.4% respectively. Four other categories consisted of more than five percent: occasional traumatic anterior subluxation (OTAS), frequent traumatic anterior subluxation (FTAS), frequent traumatic anterior dislocation (FTAD), and solitary traumatic posterior subluxation (STPS). The top seven categories encompassed 74.9% of all patients with the top nineteen comprising 97.1%.
Figure I.
FEDS Distribution of MOON Shoulder Instability Cohort a
a Reported as % of entire surgical cohort; blue boxes represent > 5% of surgical cases and gray boxes represent < 1%
For the 7 largest categories, additional demographic data is reported in Table II. Average age was similar across categories, although STAD was highest at 26.8 years, likely reflecting older patients who had a dislocation from a fall or trauma. STAS and OTAS had the highest percentage of females at 20.8% and 20.7% respectively, while STPS had the lowest at 10.0%. OTAS also had the highest percentage of sports injuries at 87.1%, while STPS had the lowest at 65.0%.
Table II.
Demographics for Most Common FEDS Categories a
| Solitary Traumatic Anterior Subluxation | Occasional Traumatic Anterior Subluxation | Frequent Traumatic Anterior Subluxation | Solitary Traumatic Anterior Dislocation | Occasional Traumatic Anterior Dislocation | Frequent Traumatic Anterior Dislocation | Solitary Traumatic Posterior Subluxation | |
|---|---|---|---|---|---|---|---|
| Total | 12.8 (154) | 9.6 (116) | 7.0 (84) | 11.4 (137) | 16.4 (197) | 9.5 (114) | 8.3 (100) |
| Age | 23.6 ± 8.6 | 23.9 ± 8.2 | 23.8 ± 8.9 | 26.8 ± 9.7 | 25.4 ± 9.2 | 23.6 ± 8.5 | 23.8 ± 8.5 |
| Female | 20.8 (32) | 20.7 (24) | 14.3 (12) | 16.8 (23) | 16.8 (33) | 13.2 (15) | 10.0 (10) |
| Sport | 76.0 (117) | 87.1 (101) | 78.6 (66) | 67.2 (92) | 71.4 (140) | 72.8 (83) | 65.0 (65) |
Reported as % (n) or mean ± SD
Postoperative Patient Reported Outcomes
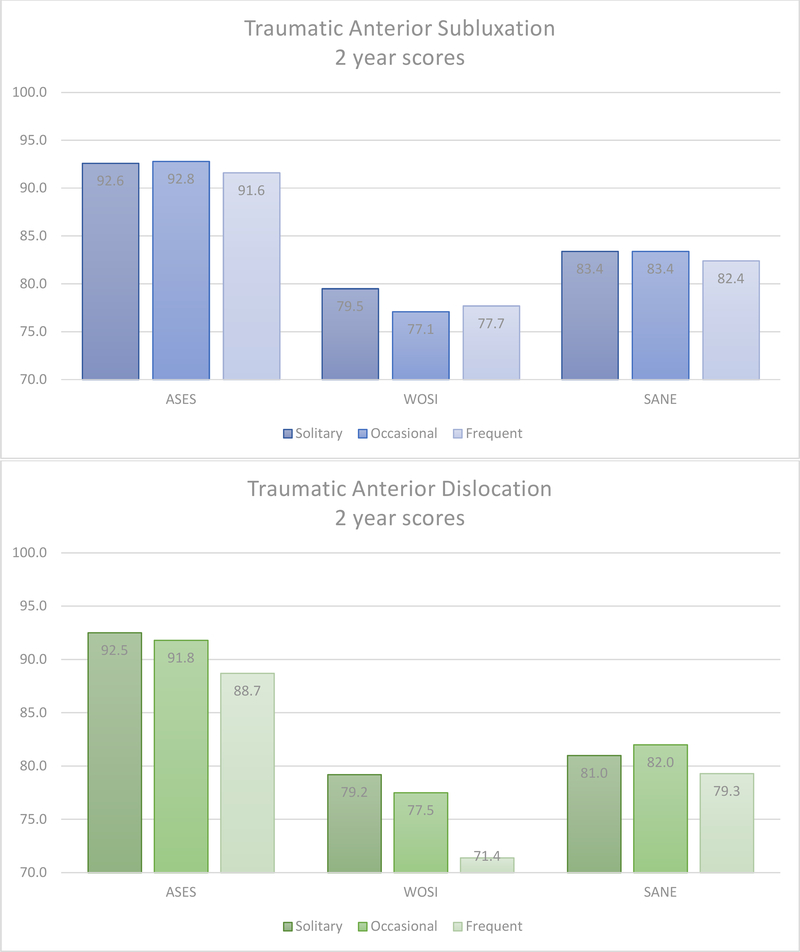
At time of analysis, 734 of 1204 patients were eligbible for two-year follow-up based on date of surgery. Two-year outcome data was available for 636/734 (86.6%). Analysis of PRO’s was limited to categories which contained at least 34 patients based on power analysis. Seven categories were eligible (STAS, OTAS, FTAS, STAD, OTAD, FTAD, and STPS). Each of the top seven FEDS categories showed significant improvement (p<.001) from baseline to two-year scores on the ASES, WOSI, and SANE, as shown in Table III. Trends for traumatic anterior subluxation and dislocation categories stratified by frequency are illustrated in Figure II.
Table III.
Patient Reported Outcomes by FEDS Categories a
| Solitary Traumatic Anterior Subluxation (n = 98) | Occasional Traumatic Anterior Subluxation (n = 72) | Frequent Traumatic Anterior Subluxation (n = 48) | Solitary Traumatic Anterior Dislocation (n = 67) | Occasional Traumatic Anterior Dislocation (n = 90) | Frequent Traumatic Anterior Dislocation (n = 49) | Solitary Traumatic Posterior Subluxation (n = 61) | |
|---|---|---|---|---|---|---|---|
| ASES | |||||||
| Baseline | 65.5 ± 18.0 | 69.1 ± 19.5 | 71.1 ± 21.0 | 68.5 ± 19.6 | 66.7 ± 20.5 | 65.8 ± 23.0 | 61.5 ± 20.3 |
| 2 year | 92.6 ± 10.4 | 92.8 ± 11.0 | 91.6 ± 9.8 | 92.5 ± 11.6 | 91.8 ± 12.6 | 88.7 ± 15.9 | 88.3 ± 15.0 |
| MCID | 82.7% | 81.7% | 74.5% | 80.6% | 86.9% | 79.2% | 89.8% |
| WOSI | |||||||
| Baseline | 46.3 ± 18.3 | 44.5 ± 19.3 | 46.9 ± 19.5 | 45.4 ± 20.0 | 43.3 ± 20.6 | 39.5 ± 18.1 | 46.4 ± 19.3 |
| 2 year | 79.5 ± 22.4 | 77.1 ± 22.8 | 77.7 ± 20.2 | 79.2 ± 21.2 | 77.5 ± 19.8 | 71.4 ± 21.0 | 79.8 ± 19.9 |
| MCID | 81.6% | 81.7% | 87.2% | 79.1% | 83.0% | 87.5% | 86.4% |
| SANE | |||||||
| Baseline | 46.8 ± 22.4 | 50.9 ± 24.7 | 50.9 ± 22.3 | 44.4 ± 23.8 | 46.3 ± 25.1 | 36.9 ± 26.6 | 53.0 ± 23.8 |
| 2 year | 83.4 ± 17.1 | 83.4 ± 16.2 | 82.4 ± 13.0 | 81.0 ± 20.8 | 82.0 ± 16.8 | 79.3 ± 19.2 | 83.1 ± 17.4 |
| MCID | 81.6% | 71.8% | 76.1% | 71.6% | 76.1% | 85.1% | 74.1% |
Reported as mean ± SD; ASES = American Shoulder and Elbow Surgeons score; WOSI = Western Ontario Shoulder Instability index; SANE = Single Assessment Numeric Evaluation; MCID = % of patients improving by the minimal clinically important difference (ASES = 6.4; WOSI = 220; SANE = 9.5); p<.001 for change between baseline and 2 year for each PRO
Figure II.
Traumatic Anterior Subluxation and Dislocation 2 Year PROs by Frequency a
a ASES = American Shoulder and Elbow Surgeons score; WOSI = Western Ontario Shoulder Instability index; SANE = Single Assessment Numeric Evaluation
Mean baseline ASES scores for the top seven categories ranged from 61.5 (STPS) to 71.1 (FTAS). Mean two-year scores showed a narrow distribution of 88.3 (STPS) to 92.8 (OTAS). Mean improvement ranged from 20.6 (FTAS) to 27.0 (STAS), with each category showing mean improvement greater than the published minimal clinically important difference (MCID) of 6.4 for the ASES.17 At least 80% of patients in each category improved by the MCID except FTAS in which 74.5% of patients improved by at least 6.4 points. STPS showed the highest percentage of MCID improvement with 89.8% of patients.
Mean baseline WOSI scores converted to a 100-point scale ranged from 39.5 (FTAD) to 46.9 (FTAS). Mean two-year scores ranged from 71.4 (FTAD) to 79.8 (STPS), the widest distribution of the four reported PROs. MCID improvement on the WOSI, reported as 220 on the 2100-point scale and converted to 10.5 out of 100, was reached at the highest rate by FTAD at 87.5%.8 STAD showed the lowest percentage of patients improving by the MCID with 79.1%.
Mean baseline SANE scores ranged from 36.9 (FTAD) to 53.0 (STPS). Two-year scores showed a narrow distribution of the 79.3 (FTAD) to 83.4 (OTAS). FTAD showed the greatest percentage of patients improving by the MCID of 15.0 with 85.1% but had the lowest two-year SANE.27 STAD showed the lowest MCID improvement with 71.6 %.
Failure
Failure, determined by three separate benchmarks of recurrent subluxation, recurrent dislocation, or revision surgery was calculated using data from patients who with minimum two-year follow-up. Overall 28.9% of patients experienced recurrent subluxation, 7.0% experienced recurrent dislocation, and 3.9% underwent repeat surgery. Patients who required further surgery due to failure underwent revision at a mean of 21.4 months (range 7.1 – 60.8 months).
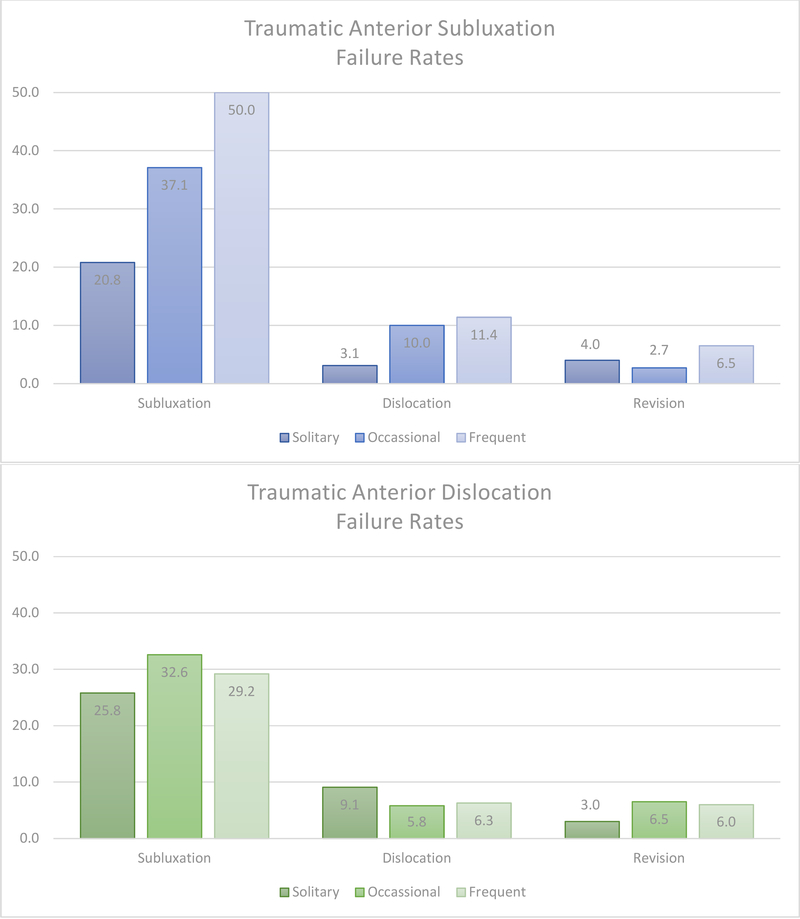
Rates of failure for FEDS categories analyzed at two years are summarized in Table IV, with trends for traumatic anterior subluxations and dislocations shown in Figure III. Rates of recurrent subluxation ranged from 19.0% (STPS) to 50.0% (FTAS) while dislocation ranged from 3.1% (STAS) to 11.4% (FTAS). The highest percentage of FTAS and OTAD patients underwent further surgery (6.5 each%) followed by FTAD (6.0%). No patients in the STPS group underwent further surgery.
Table IV.
Failure by FEDS Category a
| Solitary Traumatic Anterior Subluxation | Occasional Traumatic Anterior Subluxation | Frequent Traumatic Anterior Subluxation | Solitary Traumatic Anterior Dislocation | Occasional Traumatic Anterior Dislocation | Frequent Traumatic Anterior Dislocation | Solitary Traumatic Posterior Subluxation | |
|---|---|---|---|---|---|---|---|
| Recurrent Subluxation | 20.8 (20) | 37.1 (26) | 50.0 (22) | 25.8 (17) | 32.6 (28) | 29.2 (14) | 19.0 (11) |
| Recurrent Dislocation | 3.1 (3) | 10.0 (7) | 11.4 (5) | 9.1 (6) | 5.8 (5) | 6.3 (3) | 3.4 (2) |
| Revision Surgery | 4.0 (4) | 2.7 (2) | 6.5 (3) | 3.0 (2) | 6.5 (6) | 6.0 (3) | 0.0 (0) |
Reported as % (n)
Figure III.
Traumatic Anterior Subluxation and Dislocation 2 Failure Rates by Frequency a
a Reported as %
Discussion
Compared to the study by Hettrich et al looking at epidemiology of the FEDS system in all patients diagnosed with shoulder instability (operative and non-operative), we found our cohort to be younger (24.6 vs 30.1) and consist of more males (82.0% vs 71.5%) with more injuries during sport (71.6% vs 50.1%).7 These results are in agreement with Lebus et al, who found age and sport participation to be significantly associated with surgical management in patients with glenohumeral instability.13 Hettrich et al reported sixteen clinically relevant categories with greater than one percent of all patients. Six categories in their study comprised greater than five percent of patients, representing 72.1% of the cohort: STAD, OTAD, STAS, FTAS, FTAD, and OTAS ranging from 24.8% to 6.8%. These six categories correspond to the classic definition of TUBS by Thomas and Matsen.12; 28 These six categories were also the most common amongst surgical patients, but STPS also had more than 5% of patients. The addition of this category is also in agreement with the Lebus study, which found a significantly greater proportion of posterior instability in their surgical group compared to nonsurgical. These findings support recent evidence demonstrating a higher prevalence of posterior instability requiring surgery than previously recognized.26 As the FEDS system requires a primary direction, multidirectional instability is not directly accounted for, although FAAS, FAIS, and FAPS most closely resemble the definition. These categories accounted for a total of 2.1% of surgical cases in the cohort, similar to previous findings. McFarland et al reported the rate of multidirectional instability treated surgically to range from 1.2% to 8.3% based on different definitions used to classify patients within the same cohort, noting a significant effect of definition in determining rates, demonstrating the effect of having ambiguity in the definition.15
When developing the FEDS system, Kuhn described frequency as an indirect measure of the severity of pathology.11 This was further strengthened by the findings of Rugg et al who showed that higher frequency of dislocation was associated with a higher rate of anterior glenoid bone loss and biceps pathology in the MOON cohort. Additionally, they found that higher frequency was associated with a longer duration from onset of symptoms and a higher incidence of open surgery, suggesting that bone loss may be a direct result of untreated long-standing instability.23 Lebus reported a significant difference in the distribution of frequency between surgical and nonsurgical groups, with solitary predominating in the nonsurgical group but a nearly even split amongst solitary, occasional, and frequent in the surgical group.13 In contrast, our study showed 41.4% of patients in solitary categories, and only 23.4% classified as frequent. This predominance of solitary instability managed operatively could possibly result from the trend to earlier intervention before patients experience additional events.
Dislocation vs. subluxation, another indirect measure of pathology which intuitively would seem to be a significant factor in the preferred treatment, appears to be the FEDS variable least associated with surgery. Lebus found no association between severity and surgical treatment, with 60% of their cohort experiencing dislocations. Our study found dislocation to only occur in 45.4% of surgical cases with subluxation accounting for the remaining 54.6%. The three traumatic anterior dislocation categories, STAD, OTAD, and FTAD, accounted for 37.1% of dislocators. OTAD was the most common individual category in our cohort (16.3%), compared to STAD (24.8%) in the cohort described by Hettrich containing both operative and nonoperative patients.7
The seven most common FEDS categories all showed significant improvement for each of the ASES, WOSI, and SANE at two-year follow-up. The highest mean baseline and two-year scores for each category were found on the ASES, which places more emphasis on pain and activities of daily living than instability.22 High ASES scores across all categories suggest that pain and daily function improved to a high-level following stabilization. The WOSI, our primary instability outcome, showed mean two-year scores of less than 80% for each category. Of note, the WOSI scores decreased with increasing frequency of the traumatic anterior dislocation groups (Figure II). FTAD, despite showing improvement by the MCID in 87.2% of patients, had a 2-year mean WOSI of 71.1, indicating improvement but less favorable absolute outcomes for patients with frequent instability following dislocation. The same trend of decreasing WOSI was not observed in the traumatic anterior subluxation groups. Two-year SANE showed a tight distribution with mean scores between those of the ASES and WOSI. Interpretation of the SANE is not as specific as either of the shoulder tools, but has been shown to correlate well with multiple shoulder PROs including the ASES.29
Overall rates of recurrent subluxation, dislocation, and revision surgery were similar to previous studies, although, as Owens et al elucidated, patients may have good long-term outcome scores and return to sport despite some degree of recurrent instability.18; 20 In our cohort, recurrent subluxation represented a substantial concern in certain categories. Subluxation occurred in greater than one third of OTAS and OTAD patients and in half of those classified as FTAS. More than ten percent of OTAS and FTAS patients also reported a dislocation event following surgery, despite indicating that their shoulder problems began with subluxation. The highest rate of revision surgery occurred in the OTAD group followed by FTAS and FTAD. The most noteworthy trend with regard to failure was the finding of less favorable outcomes in the occasional/frequent groups.
Of particular interest regarding failure, a trend appears within the three categories of traumatic anterior subluxation: STAS, OTAS, and FTAS. Rates of recurrent subluxation, dislocation, and revision surgery increase with increasing frequency (Figure III). Additionally, FTAS showed the lowest improvement in ASES scores. Together these findings may suggest a role for earlier intervention before progression to more severe categories with poorer outcomes, which is supported by the aforementioned findings of greater prevalence of glenoid bone loss with increasing frequency.23 Future work should investigate pathological findings in these groups, and whether differences exist between outcomes in the solitary and occasional/frequent categories for each corresponding combination of etiology, direction, and severity.
As noted previously, the higher prevalence of STPS was a new finding within our cohort of exclusively surgical patients. Additionally, STPS had favorable outcomes, with the lowest rate of recurrent subluxation, second lowest rate of recurrent dislocation, and no revision surgeries. PROs also suggest a high level of success from surgery within the category. Previous studies on arthroscopic treatment of posterior instability demonstrate overall good results but varying levels of failure, although some discrepancy may be due to relative rarity plus the inclusion of multidirectional instability.4; 14; 16; 21 A recent study by Bernhardson et al found anterior instability to have superior outcomes to posterior instability.2 Our study only analyzed posterior instability in solitary traumatic subluxations, which showed good results that were comparable to those of the solitary traumatic anterior subluxation category.
Boileau at al. identified factors associated with recurrent instability following Bankart repair, noting bone loss, hyperlaxity, and number of anchors to be associated with higher rates.3 Similarly, Ahmed et al described patient age, severity of glenoid bone loss, and engaging Hill-Sachs lesions as significant factors associated with recurrence following Bankart repair or capsular shift.1 Notably, these studies focus primarily on pathology associated with development of instability. The results of our study supplement the current literature by investigating the prognosis of surgical treatment of the labrum or capsule based on a simple classification which can be determined on initial presentation. Due to the importance of joint pathology, Shea suggested a modification to the FEDS system to include the primary anatomic lesion leading to instability, specifically the capsule, labrum, glenoid, humerus, or rotator cuff.24 Such an addition could provide further valuable insight into outcomes based on the FEDS system, but at the cost of detracting from its innate simplicity by using patient history and physical exam alone to classify patients.
Our current study is limited to an epidemiologic investigation based on variables attainted from history and physical examination and does not include intraoperative findings. Additionally, the numerous categories of the FEDS system reduce the sample size for any given group; however, the overall size of the cohort minimizes these concerns. The FEDS system, only includes data from patient history and physical examination and does not include data on specific pathology, which is both a strength and weakness of the classification. Future studies are also necessary to establish a patient acceptable symptomatic state (PASS) score for PROs used for instability. Strengths of our study include the large size, prospective design, and enrollment from multiple private and academic centers, likely leading to a high degree of generalizability.
Conclusion
The FEDS system is a simple and reproducible method for classifying instability. While overall outcomes were good for the entire cohort, certain categories yielded higher PRO scores and differing rates of improvement, recurrent subluxation, dislocation, and revision surgery. Increasing initial frequency of instability events led to lower WOSI scores and higher failure rates in the traumatic anterior dislocation groups (OTAD/FTAD), and higher failure rates in the traumatic anterior subluxation groups (OTAS/FTAS). These findings provide insight into the outcomes of patients based on factors determined during the initial patient presentation, and may indicate a benefit of earlier recognition and operative treatment. This data can be used for patient education and shared decision making when patients are considering surgery.
Acknowledgments
This study was approved by the Institutional Review Board (IRB) at the University of Iowa (DHHS Registration # IRB00000099).
This study was, in part, supported by research grants from the Orthopaedic Research & Education Fund. The grant number is: 14-003.
This study was, in part, supported by the National Center for Advancing Translational Sciences, UL1TR001998, and the Dean of the College of Medicine, University of Kentucky. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the University of Kentucky.
Footnotes
MOON Shoulder Group Collaborators:
Keith M. Baumgarten MD9, Julie Y. Bishop MD5, Matthew J. Bollier MD6, Jonathan T. Bravman MD1, Robert H. Brophy MD7, Charles L. Cox MD, MPH4, Brian T. Feeley MD2, John A. Grant MD, PhD3, Grant L. Jones MD5, C. Benjamin Ma MD2, Robert G. Marx MD, MSc8, Eric C. McCarty MD1, Bruce S. Miller MD, MS3, Matthew V. Smith MD7, Rick W. Wright MD4, Alan L. Zhang MD2
1 Department of Orthopedics, University of Colorado School of Medicine, Aurora, CO, 2 Department of Orthopaedic Surgery, University of California, San Francisco, San Francisco, CA, 3 MedSport, Department of Orthopaedic Surgery, University of Michigan, Ann Arbor, Michigan, 4 Department of Orthopaedic Surgery and Rehabilitation, Vanderbilt University Medical Center, Nashville, Tennessee, 5The Ohio State University Sports Medicine Center, Columbus, OH, 6University of Iowa Hospitals and Clinics, Iowa City, IA, 7Department of Orthopedics, Washington University Saint Louis, St. Louis, MO, 8Department of Sports Medicine, Hospital for Special Surgery, New York, NY, 9Orthopedic Institute, Sioux Falls, South Dakota, USA
Disclaimer: None
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ahmed I, Ashton F, Robinson CM. Arthroscopic Bankart repair and capsular shift for recurrent anterior shoulder instability: functional outcomes and identification of risk factors for recurrence. J Bone Joint Surg Am 2012;94:1308–1315. 10.2106/JBJS.J.01983 [DOI] [PubMed] [Google Scholar]
- 2.Bernhardson AS, Murphy CP, Aman ZS, LaPrade RF, Provencher MT. A Prospective Analysis of Patients With Anterior Versus Posterior Shoulder Instability: A Matched Cohort Examination and Surgical Outcome Analysis of 200 Patients. Am J Sports Med 2019;47:682–687. 10.1177/0363546518819199 [DOI] [PubMed] [Google Scholar]
- 3.Boileau P, Villalba M, Hery JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am 2006;88:1755–1763. 10.2106/JBJS.E.00817 [DOI] [PubMed] [Google Scholar]
- 4.Bottoni CR, Franks BR, Moore JH, DeBerardino TM, Taylor DC, Arciero RA. Operative stabilization of posterior shoulder instability. Am J Sports Med 2005;33:996–1002. 10.1177/0363546504271509 [DOI] [PubMed] [Google Scholar]
- 5.Gerber C, Nyffeler RW. Classification of glenohumeral joint instability. Clin Orthop Relat Res 2002:65–76. No doi [DOI] [PubMed] [Google Scholar]
- 6.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hettrich CM, Cronin KJ, Raynor MB, Wagstrom E, Jani SS, Carey JL et al. Epidemiology of the Frequency, Etiology, Direction, and Severity (FEDS) system for classifying glenohumeral instability. J Shoulder Elbow Surg 2019;28:95–101. 10.1016/j.jse.2018.08.014 [DOI] [PubMed] [Google Scholar]
- 8.Kirkley A, Griffin S, Dainty K. Scoring systems for the functional assessment of the shoulder. Arthroscopy 2003;19:1109–1120. 10.1016/j.arthro.2003.10.030 [DOI] [PubMed] [Google Scholar]
- 9.Kraeutler MJ, Currie DW, Kerr ZY, Roos KG, McCarty EC, Comstock RD. Epidemiology of Shoulder Dislocations in High School and Collegiate Athletics in the United States: 2004/2005 Through 2013/2014. Sports Health 2018;10:85–91. 10.1177/1941738117709764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kraeutler MJ, McCarty EC, Belk JW, Wolf BR, Hettrich CM, Ortiz SF et al. Descriptive Epidemiology of the MOON Shoulder Instability Cohort. Am J Sports Med 2018:363546518755752 10.1177/0363546518755752 [DOI] [PubMed] [Google Scholar]
- 11.Kuhn JE. A new classification system for shoulder instability. Br J Sports Med 2010;44:341–346. 10.1136/bjsm.2009.071183 [DOI] [PubMed] [Google Scholar]
- 12.Kuhn JE, Helmer TT, Dunn WR, Throckmorton VT. Development and reliability testing of the frequency, etiology, direction, and severity (FEDS) system for classifying glenohumeral instability. J Shoulder Elbow Surg 2011;20:548–556. 10.1016/j.jse.2010.10.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lebus GFt, Raynor MB, Nwosu SK, Wagstrom E, Jani SS, Carey JL et al. Predictors for Surgery in Shoulder Instability: A Retrospective Cohort Study Using the FEDS System. Orthop J Sports Med 2015;3:2325967115607434 10.1177/2325967115607434 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lenart BA, Sherman SL, Mall NA, Gochanour E, Twigg SL, Nicholson GP. Arthroscopic repair for posterior shoulder instability. Arthroscopy 2012;28:1337–1343. 10.1016/j.arthro.2012.03.011 [DOI] [PubMed] [Google Scholar]
- 15.McFarland EG, Kim TK, Park HB, Neira CA, Gutierrez MI. The effect of variation in definition on the diagnosis of multidirectional instability of the shoulder. J Bone Joint Surg Am 2003;85-A:2138–2144. 10.2106/00004623-200311000-00011 [DOI] [PubMed] [Google Scholar]
- 16.McIntyre LF, Caspari RB, Savoie FH 3rd. The arthroscopic treatment of posterior shoulder instability: two-year results of a multiple suture technique. Arthroscopy 1997;13:426–432. [DOI] [PubMed] [Google Scholar]
- 17.Michener LA, McClure PW, Sennett BJ. American Shoulder and Elbow Surgeons Standardized Shoulder Assessment Form, patient self-report section: reliability, validity, and responsiveness. J Shoulder Elbow Surg 2002;11:587–594. 10.1067/mse.2002.127096 [DOI] [PubMed] [Google Scholar]
- 18.Mishra DK, Fanton GS. Two-year outcome of arthroscopic Bankart repair and electrothermal-assisted capsulorrhaphy for recurrent traumatic anterior shoulder instability. Arthroscopy: The Journal of Arthroscopic & Related Surgery 2001;17:844–849. [DOI] [PubMed] [Google Scholar]
- 19.Owens BD, Agel J, Mountcastle SB, Cameron KL, Nelson BJ. Incidence of glenohumeral instability in collegiate athletics. Am J Sports Med 2009;37:1750–1754. 10.1177/0363546509334591 [DOI] [PubMed] [Google Scholar]
- 20.Owens BD, DeBerardino TM, Nelson BJ, Thurman J, Cameron KL, Taylor DC et al. Long-term Follow-up of Acute Arthroscopic Bankart Repair for Initial Anterior Shoulder Dislocations in Young Athletes. The American Journal of Sports Medicine 2009;37:669–673. 10.1177/0363546508328416 [DOI] [PubMed] [Google Scholar]
- 21.Provencher MT, Bell SJ, Menzel KA, Mologne TS. Arthroscopic treatment of posterior shoulder instability: results in 33 patients. Am J Sports Med 2005;33:1463–1471. 10.1177/0363546505278301 [DOI] [PubMed] [Google Scholar]
- 22.Richards RR, An KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg 1994;3:347–352. [DOI] [PubMed] [Google Scholar]
- 23.Rugg CM, Hettrich CM, Ortiz S, Wolf BR, Group MSI, Zhang AL. Surgical stabilization for first-time shoulder dislocators: a multicenter analysis. J Shoulder Elbow Surg 2018;27:674–685. 10.1016/j.jse.2017.10.041 [DOI] [PubMed] [Google Scholar]
- 24.Shea KP. Classification of Glenohumeral Instability: A Proposed Modification of the FEDS System In. Shoulder Instability Across the Life Span: Springer; 2017. p. 7–13. ISBN 978–3-662–54077-0 [Google Scholar]
- 25.Silliman JF, Hawkins RJ. Classification and physical diagnosis of instability of the shoulder. Clin Orthop Relat Res 1993:7–19. [PubMed] [Google Scholar]
- 26.Song DJ, Cook JB, Krul KP, Bottoni CR, Rowles DJ, Shaha SH et al. High frequency of posterior and combined shoulder instability in young active patients. J Shoulder Elbow Surg 2015;24:186–190. 10.1016/j.jse.2014.06.053 [DOI] [PubMed] [Google Scholar]
- 27.Thigpen CA, Shanley E, Momaya AM, Kissenberth MJ, Tolan SJ, Tokish JM et al. Validity and Responsiveness of the Single Alpha-numeric Evaluation for Shoulder Patients. Am J Sports Med 2018;46:3480–3485. 10.1177/0363546518807924 [DOI] [PubMed] [Google Scholar]
- 28.Thomas SC, Matsen FA 3rd. An approach to the repair of avulsion of the glenohumeral ligaments in the management of traumatic anterior glenohumeral instability. J Bone Joint Surg Am 1989;71:506–513. [PubMed] [Google Scholar]
- 29.Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Outcomes measures after shoulder surgery. Am J Sports Med 1999;27:214–221. [DOI] [PubMed] [Google Scholar]