To the Editor:
We performed a literature review on viral epidemics and pandemics, including the severe acute respiratory syndrome (SARS), the Middle East respiratory syndrome (MERS), influenza H1N1, and the novel severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) with the goal of identifying the neurological symptoms, signs, and complications of these infections within the context of the COVID-19 pandemic (Figure).
FIGURE.
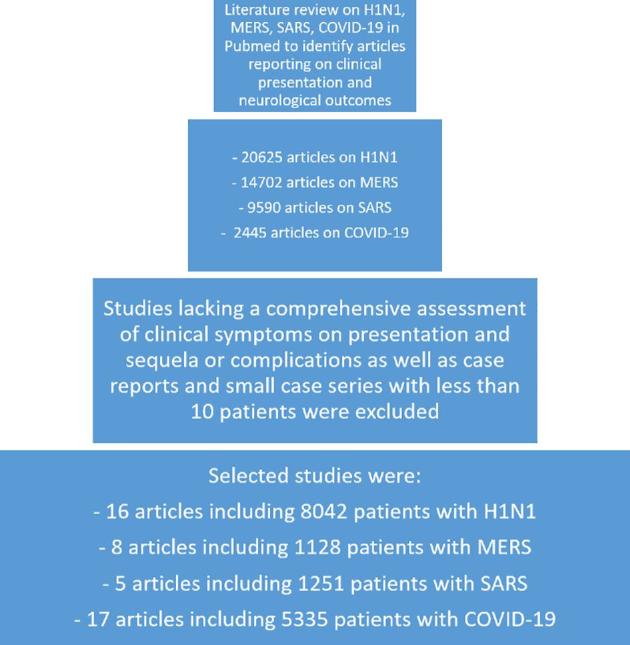
Flow diagram of study selection criteria and results.
Of 16 articles that included 8042 patients with H1N1, neurological involvement was reported in 1286 patients (15.99%). Excluding headaches, 771 patients had neurological involvement (9.6%) (Table 1). Of 8 articles consisting of 1128 patients with MERS, 323 patients (28.6%) had neurological findings and 170 patients (15.07%) without headache. Of 5 articles with 1251 patients with SARS, 187 patients (14.95%) were reported to have neurological involvement and 6.2% (n = 78) with the exclusion of headache. Of 17 articles on 5335 patients with COVID-19, 744 patients were reported to have neurological signs, symptoms, or sequelae (13.9%) to date, with a rate of 2.47% when headache was excluded (n = 132) (Table 2).
TABLE 1.
Summary of Literature Reviewa
| Study and year | Number of patients | Summary of neurological findings |
|---|---|---|
| H1N1 | ||
| Wilking et al, 201418 | 365 | Seizure: 17, encephalitis: 4, meningitis: 4, encephalopathy: 3, meningismus: 3, focal hemorrhagic brain lesions: 2, brain infarction: 1, sensorineural hearing loss: 1 |
| Frobert et al, 201119 | 181 | Seizure: 8, encephalitis: 2, encephalopathy: 1, basilar artery thrombosis: 1, myasthenic crisis: 1, decreased consciousness: 1 |
| Ekstrand et al, 201020 | 303 | Seizure: 12, status epilepticus: 7, encephalopathy: 9, headache: 3, focal neurological findings: 5, myositis: 1, aphasia: 6 |
| Glaser et al, 201221 | 2069 | Encephalopathy/encephalitis: 29, seizure: 44, meningitis: 3, Guillain-Barré syndrome: 1 |
| Jain et al, 200922 | 272 | Headache: 92 |
| Tokuhira et al, 201223 | 81 | Seizure: 19, encephalopathy: 14, neurologic long-term complications: 5 |
| Dominguez-Cherit et al,200924 | 58 | Weakness: 41, headache: 33 |
| Kumar et al, 200925 | 168 | Altered level of consciousness: 17 |
| Archer et al, 200926 | 100 | Headache: 62 |
| Kwon et al, 201227 | 1389 | Seizures: 22, meningitis: 1, encephalopathy: 2 |
| Cao et al, 200928 | 426 | Headache: 83 |
| Libster et al, 201029 | 251 | Headache: 6, seizures: 3 |
| Louie et al, 200930 | 1088 | Headache: 211, altered mental status: 60 |
| Kedia et al, 201131 | 307 | Seizure: 17, encephalopathy: 7 |
| Stein et al, 201032 | 478 | Headache: 51, seizure: 41, meningitis or encephalitis: 5 |
| Khandaker et al, 201233 | 506 | Seizure: 38, encephalitis/encephalopathy 5, confusion/disorientation: 5, loss of consciousness: 5, paralysis/Guillain-Barré syndrome: 2. |
| MERS | ||
| Arabi et al, 201434 | 12 | Headache: 2, altered consciousness: 1 |
| Noorwali et al, 201535 | 261 | Headache: 59, altered consciousness: 53, focal neurological deficit: 10 |
| Saad et al, 201436 | 70 | Confusion: 18, headache: 9, seizure: 6 |
| Arabi et al, 201737 | 330 | Altered consciousness: 70, headache: 34 |
| Choi et al, 201638 | 186 | Headache: 38, altered consciousness: 10 |
| Assiri et al, 201339 | 47 | Headache: 6 |
| Shalhoub et al, 201840 | 32 | Altered consciousness: 2, headache: 5 |
| Aleanizy et al, 201741 | 190 | No neurological symptoms or complications reported |
| SARS | ||
| Choi et al, 200342 | 267 | Headache: 89, dizziness: 48, confusion: 2 |
| Umapathi et al, 20045 | 206 | Large artery cerebral infarctions: 5 |
| Tsai et al, 200543 | 664 | Polyneuropathy: 3, large artery ischemic stroke: 5 |
| Leung and Chiu, 200444 | 64 | Headache: 18, dizziness: 12, altered consciousness: 3 |
| Lien et al, 200845 | 50 | Headache: 2 |
| COVID-19 | ||
| Mao et al, 202046 | 214 | Dizziness: 36, headache: 28, altered consciousness: 16, acute cerebrovascular disease: 6, ataxia: 1, seizure: 1, hypogeusia: 12, hyposmia: 11, hypopsia: 3, neuralgia: 5 |
| Xu et al, 202047 | 62 | Headache: 21 |
| Chen et al, 202048 | 274 | Headache: 3, dizziness: 21, altered consciousness: 26 |
| Wu et al, 202049 | 80 | Headache: 13 |
| Lian et al, 202050 | 788 | Headache: 75 |
| Wang et al, 202051 | 69 | Headache: 10, dizziness: 5 |
| Guan et al, 202052 | 1590 | Headache: 205, altered consciousness: 20 |
| Arentz et al, 202053 | 21 | Seizure: 1 |
| Wan et al, 202054 | 135 | Headache: 24 |
| Chu et al, 202055 | 54 | Unspecified |
| Huang et al, 202056 | 34 | Headache: 2 |
| Yang et al, 202057 | 149 | Headache: 13 |
| Yang et al, 200258 | 52 | Headache: 3 |
| Guan et al, 202059 | 1099 | Headache: 150 |
| Korea Centers for DiseaseControl and Prevention60 | 28 | Headache: 3 |
| Huang et al, 202061 | 41 | Headache: 3 |
| Zheng et al, 202062 | 645 | Headache: 67 |
All studies were retrospective, except Howlett et al, 2018, which was prospective.
TABLE 2.
Neurologic Complications by Viral Disease
| Neurologic finding | Number of patients | Percent |
|---|---|---|
| H1N1 | ||
| Headache | 541 | 6.73% |
| Seizure | 228 | 2.84% |
| Encephalitis/encephalopathy(often grouped together) | 76 | 0.95% |
| Weakness | 41 | 0.51% |
| Altered level of consciousness | 22 | 0.27% |
| Meningitis | 13 | 0.16% |
| Speech difficulties | 6 | 0.07% |
| Cognitive and memory issues | 5 | 0.06% |
| Cranial nerve or focal deficit | 5 | 0.06% |
| Neurological long-termcomplications, not specified | 5 | 0.06% |
| Stroke | 4 | 0.05% |
| Guillain-Barré syndrome | 3 | 0.04% |
| Hearing impairment andtinnitus | 1 | 0.01% |
| MERS | ||
| Headache | 147 | 13.03% |
| Altered level of consciousness | 136 | 12.06% |
| Cognitive or memory issues | 18 | 1.60% |
| Cranial nerve or focal deficit | 10 | 0.89% |
| Seizure | 6 | 0.53% |
| SARS | ||
| Headache | 109 | 8.71% |
| Dizziness | 60 | 4.80% |
| Stroke | 10 | 0.80% |
| Altered level of consciousness | 5 | 0.40% |
| Neuropathy | 3 | 0.24% |
| COVID-19 | ||
| Headache | 620 | 11.74% |
| Dizziness | 62 | 1.17% |
| Altered level of consciousness | 62 | 1.17% |
| Diminished taste sensation | 12 | 0.23% |
| Diminished smell | 11 | 0.21% |
| Stroke | 6 | 0.11% |
| Neuralgia | 5 | 0.09% |
| Seizure | 2 | 0.04% |
| Ataxia | 1 | 0.02% |
At this time, the neurological complications of COVID-19 are not fully understood, but reports of prominent neurological symptoms and complications are beginning to emerge.1 The current incidence of neurological findings with COVID-19 is relatively low, but as data from prior epidemics show, particularly prior coronavirus-related epidemics, the rate is likely to further increase. Neurological manifestations, including headache, dizziness, altered level of consciousness, focal neurological deficits, cranial nerve involvement,2 seizures, and to a lesser extent meningoencephalitis,3 more severe necrotizing encephalopathy,4 cerebral edema, and stroke,5 have been reported with the recent viral epidemics. Importantly, with prior epidemics (Table 3), there are also several reports of patients developing neurological sequelae months to weeks later, including cerebellitis,6,7 neuropathy,8 Guillain-Barré syndrome,9 postinfluenza myositis,10 and postviral Parkinsonism.11
TABLE 3.
Year Identified, Total Case Numbers, and Case Fatality Rates of SARS, H1N1, MERS, and COVID-19
| Virus | Year identified | Number of countries affected | Number of cases | Number of deaths | Case fatality rate |
|---|---|---|---|---|---|
| H1N1 | 2009 | >214 | 0.7 to 1.4 billion | 18 036 (confirmed) 284 000 (estimated) | 0.03% (estimated) |
| SARS (SARS-CoV) | 2002 | 26 | 8437 | 813 | 9.6% |
| MERS | 2012 | 27 | 2499 | 861 | 34.5% |
| COVID-19 | 2019 | >205 | >2 million | 33 509 | 4.8% |
Coronaviruses are thought to disseminate to the central nervous system (CNS) through either hematogenous spread, retrograde neuronal dissemination, or direct invasion of the olfactory epithelium.12
Furthermore, the ACE2 receptor, which is present in the nervous system and the skeletal system,13 was identified as the functional receptor for SARS-CoV-2.14 There is also some speculation that invasion into the CNS and damage to the medullary cardiorespiratory centers may lead to worsening respiratory symptoms.15 Also, with the prior SARS epidemic, multiple human brain specimens demonstrated direct infection of neuronal cells within the cerebral cortex and hypothalamus.16
Additionally, there are reports of a hypercoagulable state in certain cases of COVID-19, placing patients at a higher risk of stroke, especially in the setting of acute illness and in the elderly population.17
Given the higher prevalence of neurological sequelae reported with prior coronavirus-related pandemics, COVID-19 has the potential of leading to similar if not worse neurological sequelae due to its enhanced virulence. Neurological sequelae can lead to significant morbidity and mortality within survivors, and a heightened attention to neurological findings is required in the ensuing weeks to months.
In conclusion, with the continuing spread of COVID-19 throughout the world and from what the experience from prior epidemics has shown us, neurological findings are likely to increase; therefore, continued monitoring and early recognition is imperative.
Disclosures
The authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article.
REFERENCES
- 1. Sun T, Guan J. Novel coronavirus and central nervous system. Eur J Neurol. published online: March 26, 2020 (doi:10.1111/ene.14227). [DOI] [PubMed] [Google Scholar]
- 2. Kahle KT, Walcott BP, Nahed BV et al.. Cerebral edema and a transtentorial brain herniation syndrome associated with pandemic swine influenza A (H1N1) virus infection. J Clin Neurosci. 2011;18(9):1245-1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Akins PT, Belko J, Uyeki TM, Axelrod Y, Lee KK, Silverthorn J. H1N1 encephalitis with malignant edema and review of neurologic complications from influenza. Neurocrit Care. 2010;13(3):396-406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lyon JB, Remigio C, Milligan T, Deline C. Acute necrotizing encephalopathy in a child with H1N1 influenza infection. Pediatr Radiol. 2010;40(2):200-205. [DOI] [PubMed] [Google Scholar]
- 5. Umapathi T, Kor AC, Venketasubramanian N et al.. Large artery ischaemic stroke in severe acute respiratory syndrome (SARS). J Neurol. 2004;251(10):1227-1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ishikawa T, Fujio Y, Morita M, Takiyama Y, Nakano I. [An adult case of acute cerebellitis after influenza A infection with a cerebellar corical lesion on MRI]. Rinsho Shinkeigaku. 2006;46(7):491-495. [PubMed] [Google Scholar]
- 7. Hayase Y, Tobita K. Probable post-influenza cerebellitis. Intern Med. 1997;36(10):747-749. [DOI] [PubMed] [Google Scholar]
- 8. Algahtani H, Subahi A, Shirah B. Neurological complications of Middle East respiratory syndrome coronavirus: a report of two cases and review of the literature. Case Rep Neurol Med. 2016;2016:3502683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sivadon-Tardy V, Orlikowski D, Porcher R et al.. Guillain-Barré syndrome and influenza virus infection. Clin Infect Dis. 2009;48(1):48-56. [DOI] [PubMed] [Google Scholar]
- 10. D'Silva D, Hewagama S, Doherty R, Korman TM, Buttery J. Melting muscles: novel H1N1 influenza A associated rhabdomyolysis. Pediatr Infect Dis J. 2009;28(12):1138-1139. [DOI] [PubMed] [Google Scholar]
- 11. Jang H, Boltz DA, Webster RG, Smeyne RJ. Viral parkinsonism. Biochim Biophys Acta. 2009;1792(7):714-721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Desforges M, Le Coupanec A, Dubeau P et al.. Human coronaviruses and other respiratory viruses: underestimated opportunistic pathogens of the central nervous system? Viruses. 2019;12(1):E14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hamming I, Timens W, Bulthuis ML, Lely AT, Navis G, van Goor H. Tissue distribution of ACE2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631-637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yan R, Zhang Y, Li Y, Xia L, Guo Y, Zhou Q. Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2. Science. 2020;367(6485):1444-1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Li YC, Bai WZ, Hashikawa T. The neuroinvasive potential of SARS-CoV2 may play a role in the respiratory failure of COVID-19 patients. J Med Virol. published online: February 27 2020 (doi:10.1002/jmv.25728). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gu J, Gong E, Zhang B et al.. Multiple organ infection and the pathogenesis of SARS. J Exp Med. 2005;202(3):415-424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Terpos E, Ntanasis-Stathopoulos I, Elalamy I et al.. Hematological findings and complications of COVID-19. Am J Hematol. published online: April 13, 2020 (doi:10.1002/ajh.25829). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Wilking AN, Elliott E, Garcia MN, Murray KO, Munoz FM. Central nervous system manifestations in pediatric patients with influenza A H1N1 infection during the 2009 pandemic. Pediatr Neurol. 2014;51(3):370-376. [DOI] [PubMed] [Google Scholar]
- 19. Frobert E, Sarret C, Billaud G et al.. Pediatric neurological complications associated with the A(H1N1)pdm09 influenza infection. J Clin Virol. 2011;52(4):307-313. [DOI] [PubMed] [Google Scholar]
- 20. Ekstrand JJ, Herbener A, Rawlings J et al.. Heightened neurologic complications in children with pandemic H1N1 influenza. Ann Neurol. 2010;68(5):762-766. [DOI] [PubMed] [Google Scholar]
- 21. Glaser CA, Winter K, DuBray K et al.. A population-based study of neurologic manifestations of severe influenza A(H1N1)pdm09 in California. Clin Infect Dis. 2012;55(4):514-520. [DOI] [PubMed] [Google Scholar]
- 22. Jain S, Kamimoto L, Bramley AM et al.. Hospitalized patients with 2009 H1N1 influenza in the United States, April-June 2009. N Engl J Med. 2009;361(20):1935-1944. [DOI] [PubMed] [Google Scholar]
- 23. Tokuhira N, Shime N, Inoue M et al.. Mechanically ventilated children with 2009 pandemic influenza A/H1N1. Pediatr Crit Care Med. 2012;13(5):e294-e298. [DOI] [PubMed] [Google Scholar]
- 24. Dominguez-Cherit G, Lapinsky SE, Macias AE et al.. Critically ill patients with 2009 influenza A(H1N1) in Mexico. JAMA. 2009;302(17):1880-1887. [DOI] [PubMed] [Google Scholar]
- 25. Kumar A, Zarychanski R, Pinto R et al.. Critically ill patients with 2009 influenza A(H1N1) infection in Canada. JAMA. 2009;302(17):1872-1879. [DOI] [PubMed] [Google Scholar]
- 26. Archer BN, Timothy GA, Cohen C et al.. Introduction of 2009 pandemic influenza A virus subtype H1N1 into South Africa: clinical presentation, epidemiology, and transmissibility of the first 100 cases. J Infect Dis. 2012;206(suppl 1):S148-S153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kwon S, Kim S, Cho MH, Seo H. Neurologic complications and outcomes of pandemic (H1N1) 2009 in Korean children. J Korean Med Sci. 2012;27(4):402-407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cao B, Li XW, Mao Y et al.. Clinical features of the initial cases of 2009 pandemic influenza A (H1N1) virus infection in China. N Engl J Med. 2009;361(26):2507-2517. [DOI] [PubMed] [Google Scholar]
- 29. Libster R, Bugna J, Coviello S et al.. Pediatric hospitalizations associated with 2009 pandemic influenza A (H1N1) in Argentina. N Engl J Med. 2010;362(1):45-55. [DOI] [PubMed] [Google Scholar]
- 30. Louie JK, Acosta M, Winter K et al.. Factors associated with death or hospitalization due to pandemic 2009 influenza A(H1N1) infection in California. JAMA. 2009;302(17):1896-1902. [DOI] [PubMed] [Google Scholar]
- 31. Kedia S, Stroud B, Parsons J et al.. Pediatric neurological complications of 2009 pandemic influenza A (H1N1). Arch Neurol. 2011;68(4):455-462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Stein M, Tasher D, Glikman D et al.. Hospitalization of children with influenza A(H1N1) virus in Israel during the 2009 outbreak in Israel: a multicenter survey. Arch Pediatr Adolesc Med. 2010;164(11):1015-1022. [DOI] [PubMed] [Google Scholar]
- 33. Khandaker G, Zurynski Y, Buttery J et al.. Neurologic complications of influenza A(H1N1)pdm09: surveillance in 6 pediatric hospitals. Neurology. 2012;79(14):1474-1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Arabi YM, Arifi AA, Balkhy HH et al.. Clinical course and outcomes of critically ill patients with Middle East respiratory syndrome coronavirus infection. Ann Intern Med. 2014;160(6):389-397. [DOI] [PubMed] [Google Scholar]
- 35. Noorwali AA, Turkistani AM, Asiri SI et al.. Descriptive epidemiology and characteristics of confirmed cases of Middle East respiratory syndrome coronavirus infection in the Makkah region of Saudi Arabia, March to June 2014. Ann Saudi Med. 2015;35(3):203-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Saad M, Omrani AS, Baig K et al.. Clinical aspects and outcomes of 70 patients with Middle East respiratory syndrome coronavirus infection: a single-center experience in Saudi Arabia. Int J Infect Dis. 2014;29(6):301-306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Arabi YM, Al-Omari A, Mandourah Y et al.. Critically ill patients with the Middle East respiratory syndrome: a multicenter retrospective cohort study. Crit Care Med. 2017;45(10):1683-1695. [DOI] [PubMed] [Google Scholar]
- 38. Choi WS, Kang CI, Kim Y et al.. Clinical presentation and outcomes of Middle East respiratory syndrome in the Republic of Korea. Infect Chemother. 2016;48(2):118-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Assiri A, Al-Tawfiq JA, Al-Rabeeah AA et al.. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013;13(9):752-761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Shalhoub S, Al-Hameed F, Mandourah Y et al.. Critically ill healthcare workers with the Middle East respiratory syndrome (MERS): a multicenter study. PLoS One. 2018;13(11):e0206831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Aleanizy FS, Mohmed N, Alqahtani FY, El Hadi Mohamed RA. Outbreak of Middle East respiratory syndrome coronavirus in Saudi Arabia: a retrospective study. BMC Infect Dis. 2017;17(1):23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Choi KW, Chau TN, Tsang O et al.. Outcomes and prognostic factors in 267 patients with severe acute respiratory syndrome in Hong Kong. Ann Intern Med. 2003;139(9):715-723. [DOI] [PubMed] [Google Scholar]
- 43. Tsai LK, Hsieh ST, Chang YC. Neurological manifestations in severe acute respiratory syndrome. Acta Neurol Taiwan. 2005;14(3):113-119. [PubMed] [Google Scholar]
- 44. Leung CW, Chiu WK. Clinical picture, diagnosis, treatment and outcome of severe acute respiratory syndrome (SARS) in children. Paediatr Respir Rev. 2004;5(4):275-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Lien TC, Sung CS, Lee CH et al.. Characteristic features and outcomes of severe acute respiratory syndrome found in severe acute respiratory syndrome intensive care unit patients. J Crit Care. 2008;23(4):557-564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mao L, Mengdie W, Shengcai C et al.. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: a retrospective case series study. JAMA Neurol. published online: April 10, 2020 (doi:10.1101/2020.02.22.20026500). [Google Scholar]
- 47. Xu XW, Wu XX, Jiang XG et al.. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-CoV-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Chen T, Wu D, Chen H et al.. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wu J, Liu J, Zhao X et al.. Clinical characteristics of imported cases of COVID-19 in Jiangsu province: a multicenter descriptive study. Clin Infect Dis. published online: February 29, 2020 (doi:10.1093/cid/ciaa199). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lian J, Jin X, Hao S et al.. Analysis of epidemiological and clinical features in older patients with corona virus disease 2019 (COVID-19) out of Wuhan. Clin Infect Dis. published online: March 25, 2020 (doi:10.1093/cid/ciaa242). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wang Z, Yang B, Li Q, Wen L, Zhang R. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis. published online: March 16, 2020 (doi:10.1093/cid/ciaa272). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Guan WJ, Liang WH, Zhao Y et al.. Comorbidity and its impact on 1590 patients with Covid-19 in China: a nationwide analysis. Eur Respir J. published online: March 26, 2020 (doi:10.1183/13993003.00547-2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Arentz M, Yim E, Klaff L et al.. Characteristics and outcomes of 21 critically ill patients with COVID-19 in Washington state. JAMA. published online: March 19, 2020 (doi:10.1001/jama.2020.4326). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Wan S, Xiang Y, Fang W et al.. Clinical features and treatment of COVID-19 patients in Northeast Chongqing. J Med Virol. published online: March 21, 2020 (doi:10.1002/jmv.25783). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Chu J, Yang N, Wei Y et al.. Clinical characteristics of 54 medical staff with COVID-19: a retrospective study in a single center in Wuhan, China. J Med Virol. published online: March 29, 2020 (doi:10.1002/jmv.25793). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Huang Y, Tu M, Wang S et al.. Clinical characteristics of laboratory confirmed positive cases of SARS-CoV-2 infection in Wuhan, China: a retrospective single center analysis. Travel Med Infect Dis. published online: February 27, 2020 (doi:10.1016/j.tmaid.2020.101606). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Yang W, Cao Q, Qin L et al.. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): a multi-center study in Wenzhou city, Zhejiang, China. J Infect. 2020;80(4):388-393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Yang X, Yu Y, Xu J et al.. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. published online: February 24, 2020 (doi:10.1016/S2213-2600(20)30079-5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Guan WJ, Ni ZY, Hu Y et al.. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. published online: February 28, 2020 (doi:10.1056/NEJMoa2002032). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Covid-19 National Emergency Response Center, Epidemiology Case Management Team, Korea Centers for Disease Control Prevention Early epidemiological and clinical characteristics of 28 cases of coronavirus disease in South Korea. Osong Public Health Res Perspect. 2020;11(1):8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Huang C, Wang Y, Li X et al.. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet North Am Ed. 2020;395(10223):497-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Zheng F, Liao C, Fan QH et al.. Clinical characteristics of children with coronavirus disease 2019 in Hubei, China. Curr Med Sci. published online: March 24, 2020 (doi:10.1007/s11596-020-2172-6). [DOI] [PMC free article] [PubMed] [Google Scholar]


