In response to the outbreak of coronavirus disease 2019 (COVID-19), a guidance on the treatment strategy of acute myocardial infarction (AMI) and personal protection for medical staff during the COVID-19 epidemic was released by the Chest Pain Center Committee, Medical Quality Control Center of Cardiovascular Diseases in Liaoning province, China,1 which received great attention from cardiologists, with >30 000 online viewings at the time of writing. The guideline is briefly outlined.
General principles2,3
All patients with chest pain should be first screened for COVID-19 and be classified into four categories: confirmed, suspected, ruled out, and cannot be ruled out at present (no epidemiological exposure history, no fever, 1–2 clinical manifestations of COVID-19, but insufficient for the suspected patients criteria).
To minimize the risk of cross-infection, several principles were addressed.
Low-risk patients, i.e. those with non-ST-segment elevation myocardial infarction (NSTEMI) with GRACE score <108, are not recommended for admission to hospital until the epidemic is under control.
All patients should be treated nearby or in situ.
Patients who cannot be ruled out for COVID-19 should be temporarily first contacted in the quarantine area of emergency departments.
Patients with suspected/confirmed COVID-19 should be admitted to the quarantine wards of the designated hospitals.
An airtight/negative-pressure ambulance should be used for transport of patients with suspected/confirmed COVID-19.
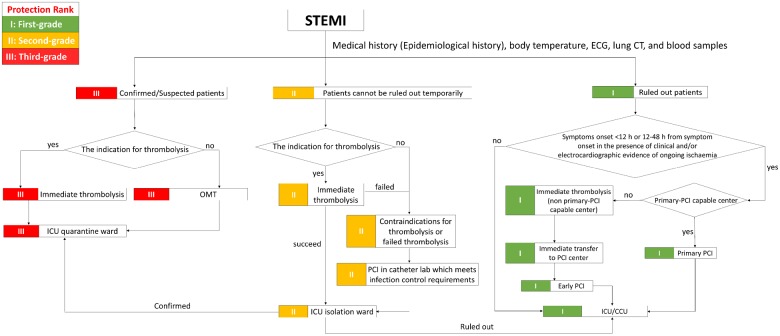
Figure 1.
Algorithm for management of STEMI. CCU, coronary care unit; ECG, electrocardiogram; ICU, intensive care unit; PCI, percutaneous coronary intervention; OMT, optimized medical treatment; STEMI, ST-segment elevation myocardial infarction
Treatment strategy of STEMI
Patients with STEMI with suspected/confirmed COVID-19 should be treated in the designated hospital as soon as possible.
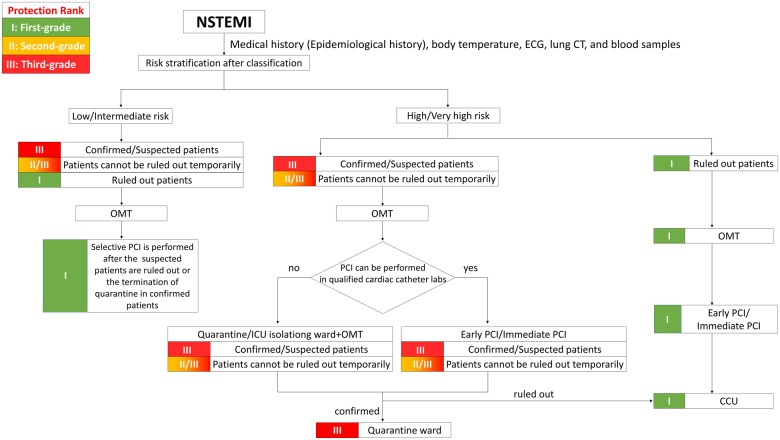
Figure 2.
Algorithm for management of NSTEMI. ECG, electrocardiogram; ICU, intensive care unit; PCI, percutaneous coronary intervention; NSTEMI, non-ST-segment elevation myocardial infarction; OMT, optimized medical treatment.
For patients with symptom onset within 12 h, thrombolysis is a first priority option if indicated. Percutaneous coronary intervention (PCI) is considered only for patients with contraindications or failed thrombolysis, and should be performed in qualified cardiac catheter labs (equipped with negative-pressure, laminar flow ventilation).
For patients with symptom onset beyond 12 h, optimized medical treatment (OMT) in intensive care unit (ICU) quarantine wards is recommended.
For patients with unstable vital signs, decision-making is the same as above and should be additional to haemodynamic stabilization measures (such as intra-aortic balloon pump or temporary cardiac pacing).
Unstable patients presenting with respiratory failure rather than heart failure should be transferred to the ICU quarantine wards for optimized medical treatment (OMT) and auxiliary respiratory therapy.
Third-grade protection for medical staff should be adopted during the whole medical process.
STEMI patients who cannot be ruled out for COVID-19 at the time should remain in a single-bed ICU isolation ward until a definitive diagnosis. Lung CT scanning and COVID-19 nucleic acid testing should be performed as soon as possible. Treatment strategies are the same as those for suspected/confirmed patients. PCI is recommended after ruling out COVID-19 or, if necessary, should be performed in qualified cardiac catheter labs or those with central air conditioning turned off if negative-pressure ventilation is not available. Medical staff should adopt at least second-level protection.
Treatment strategy of NSTEMI
Patients with suspected/confirmed COVID-19 presenting as low- or intermediate-risk NSTEMI should be treated with OMT in the quarantine wards. Selective PCI should be performed after the termination of quarantine. Patients at high or very high risk (GRACE score >140) should be treated with early (<24 h) or immediate (<2 h) PCI following OMT, respectively, in qualified cardiac catheter labs. Otherwise they should receive OMT in ICU quarantine wards. Third-level protection for medical staff should be adopted.
NSTEMI patients who cannot be ruled out for COVID-19 should be temporarily treated the same as suspected/confirmed patients and should be diagnosed as soon as possible. At least second-level protection should be adopted.
Principles of quarantine and protection of personnel 4–7
First-level protection should be maintained the same as the basic protection for medical staff in chest pain centres and outpatient departments, which can be updated in conjunction with changes in the epidemic situation.
Contact with febrile patients should be initiated in the fever clinic and second-level protection should be adopted. It is necessary to upgrade the protection level after consulting nosocomial infection control experts if patients with suspicion of COVID-19 were contacted.
All the inpatients should wear surgical masks. Febrile patients should be monitored closely and screened for COVID-19 as early as possible. Once the inpatients with epidemiological history have fever, they should be quarantined immediately. Medical staff should then upgrade the protection level and be quarantined if necessary.
It is recommended to minimize the members of the operating team, shorten the operation time, and decrease the consumption of disposable protective equipment in the catheter labs as far as possible.
Third-level or at least second-level protection for medical staff should be adopted during PCI for suspected/confirmed COVID-19 patients and for those in whom COVID-19 cannot yet be ruled out, respectively.
Medical staff participating in the treatment of suspected/confirmed COVID-19 patients should be quarantined and observed for 2 weeks in facilities designated by the government before returning to normal.
Yaling Han*
*Corresponding author. Department of Cardiology, General Hospital of Northern Theater Command, 83 Wenhua Road, 110840 Shenyang, China. Tel: +86 24 28856123, Fax: +86 24 28897310, Email: hanyaling@263.net
References
References are available as supplementary material at European Heart Journal online.
Supplementary Material
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.