Abstract
Aims: To quantify microbial contamination on kitchen and bathroom surfaces (fomites) in rural Cambodian homes and to compare these concentrations to similar data from the United States and Japan.
Methods and Results: This study monitored the numbers of faecal coliforms (i.e. thermotolerant coliforms), total coliforms, Escherichia coli and heterotrophic plate count bacteria on household surfaces in a rural village of Cambodia. Faecal coliform levels in Cambodia were highest on moist locations such as the plastic ladle used for sink water, the toilet seat surface and the cutting board surface with 100‐fold higher levels of faecal coliform bacteria than E. coli and 100‐fold higher levels of faecal coliforms than the US and Japanese studies.
Conclusions: A single public health intervention barrier, such as an improved latrine, is only partially effective for household sanitation. For complete sanitation, multiple environmental barriers may be necessary. These barriers occur in a house constructed with easily washable surfaces, a chlorinated water distribution system, house climate control and cleaning product availability.
Significance and Impact of the Study: Results of this study can be used to emphasize the importance of increasing household environmental sanitation barriers.
Keywords: bacteria, coliforms, fomites, latrines, millennium development goal
Introduction
With the 2015 United Nations Millennium Development Goal (UN MDG) fast approaching, it has become apparent that some south‐east Asian regions will come close to reaching their sanitation and hygiene targets. The MDG 7, to ensure environmental sustainability, has the target 7C, which states ‘halve, by 2015, the proportion of people without sustainable access to safe drinking water and basic sanitation’. Indicators for this target are the proportion of the population using an improved drinking water source and the proportion of the population using an improved sanitation facility (United Nations Children’s Fund 2006). Many villages in Kompong Thom province of Cambodia are on track to meet this target; households have installed protected wells and improved latrines. The presence of the household improved latrine is a proxy indicator for basic sanitation in the household. The improved latrine represents a barrier to the environmental transmission of pathogens and is more likely to be sanitary than unimproved latrines or the absence of a latrine (United Nations Childrens Fund 2006).
Although it is important to have simple and direct goals with clear targets for the UN MDGs, these metrics do not approximate the dynamic details for the environmental transmission of pathogens within households. A household that has met the MDG metrics in a developing country by having an improved latrine may have different concentrations of microbes than a household in an industrialized country. This study quantifies microbial contamination on surfaces (fomites) in rural Cambodian homes that possess improved latrines as the UN MDG hygiene indicator and the single barrier for environmental transmission of pathogens. This paper tallies the microbes in Cambodian homes in reference to comparable surfaces in the United States and Japan (Rusin et al. 1998; Ojima et al. 2002).
Fomites in households have been found to contribute to the transmission of human pathogens (Reynolds et al. 2005). Because many microbes are capable of causing infections at low doses (Sinclair et al. 2008), pathogens can survive for hours to weeks on surfaces such as cutting boards and bathroom floors. Fomites have been proposed as a significant transmission route for outbreaks such as the SARS virus, which is known to survive up to 96 h (Duan et al. 2003) or longer on surfaces with moisture and biological substances. They are also believed to play a significant role in the transmission of other respiratory and enteric infections (Boone and Gerba 2007) and foodborne illness in the home (Scott 1996). Households in Kompong Thom province, Cambodia, were monitored for the numbers of faecal coliforms (i.e. thermotolerant coliforms), total coliforms and heterotrophic plate count (HPC) bacteria on the surfaces outlined in a similar USA‐based study (Rusin et al. 1998). The objectives of the study were to (i) assess kitchen and bathroom surface contamination to provide information regarding the areas of greatest potential exposure and public health risk in a developing country household, (ii) establish a baseline data set to be used for a later public health hand‐washing intervention and (iii) determine whether surfaces in rural Cambodian homes with ‘improved sanitation’ have similar contamination levels to homes in other countries. Such information could be used in a health education programme to aid in educational efforts focusing on hand washing, use of household disinfectants or other hygiene and sanitation practices.
Materials and methods
Eight households in Beung village of Kompong Thom province, Cambodia, were selected for participation in the study. These households were selected with the following criteria: (i) There was a housewife or other domestic adult who is at home all day and/or does not a have a paid job outside the home, (ii) one or more children under 12 years old in the household, (iii) the occupants were not household disinfectant users and (iv) that the occupants had access to improved sanitation and an improved water source, i.e. meets the MDG definition for improved sanitation and water source (United Nations Children’s Fund 2006). The above‐mentioned criteria one through three were established for comparison purposes with the Rusin study (Rusin et al. 1998). Criteria four were established to give the study global relevence to the UN MDGs and for baseline information to be used with future Adventist Development Relief Agency (ADRA) Cambodia projects.
Selected households were monitored for the numbers of faecal coliforms, total coliforms, HPCs and Escherichia coli bacteria on the surfaces listed in Table 1. Surface samples were obtained using a sterile transport swab immersed in 1 ml of Amies solution and sponge (BD BBL, Franklin Lakes, NJ, USA). The swab was aseptically removed and completely swabbed over the sample surface of 4 cm2. The swab was then returned to the container with sponge and Amies solution, then transported to a field laboratory area on ice and processed within 10 h. The counts of bacteria obtained from a 4‐cm2 swab were interpreted to a 1‐cm2 area for comparison with the Rusin (Rusin et al. 1998) study.
Table 1.
Kitchen and bathroom surfaces sampled for contamination in Cambodia and the comparable surfaces in Tucson, AZ and USA households
| United States | Cambodia |
|---|---|
| Kitchen | |
| Sink faucet handle | Side of dipping ladle for sink water |
| Counter top | Table or counter for food preparation |
| Floor surface near kitchen sink | Same |
| Surface of cutting board | Same |
| Bathroom | |
| Toilet flush handle | Handle of ladle for anal cleansing |
| Top and underside of toilet | Top of toilet (squat style) |
| Floor surface around the base of the toilet | Same |
In the field laboratory, the swab container was mixed for 30 s using pliers to squeeze the plastic tube containing a sponge and the swab. A sterile pipette was used to remove 0·5 ml of Amies solution, which was placed in a dilution bottle with 4·5 ml of sterile phosphate buffer. Serial dilutions of 0·5 ml were transferred to additional dilution bottles.
Samples were enumerated using Petrifilm™ plates (3M™, St Paul, MN, USA) for HPC, E. coli and total coliform. Using the procedure described by the manufacturer, 1 ml of sample was removed from a dilution tube and placed in the centre of the Petrifilm, covered and allowed to rehydrate and gel. Once this was performed, E. coli and total coliform in Petrifilm media were incubated at 37°C for 24 h in a portable incubator. Positive E. coli were identified by a blue colony with the formation of gas. Red colonies with gas were identified as total coliform. Red or blue colonies without gas were not counted. The HPC Petrifilm media followed a similar protocol, but were incubated at 30°C for 3 days. For faecal coliforms, a me mbrane‐filter faecal coliform (MFC) agar (Difco) was prepared and poured onto plastic Petri dishes. A spot plate method was used (Miles and Misra 1938), where a volume of 50 μl was placed as a drop on the solid agar and allowed to dry into the agar. Up to four spots per dilution were applied to the plates. Each sample was replicated in at least triplicate using Petrifilm and up to four replicates for spot plates. The study’s standard operating procedure included the use of a sampling data entry form, a study protocol, positive controls to validate the sampling method and negative controls to detect any field sampling errors.
Data were entered in Microsoft Excel 2003 to compute measures of mean, geometric mean and standard deviation. To assess the difference from the United States to Cambodia, t‐tests were conducted using Microsoft Excel’s data analysis tool pack.
While collecting fomite samples, a sanitary observational survey was used to characterize the culture, household setting and household design with respect to hygiene and sanitation. The type of household construction, cleaning materials, use of detergents, the presence of domestic animals, personal hygiene and water source were noted for each house visited.
Households in Cambodia were monitored as a baseline measurement for a hand‐washing programme to be implemented through the ADRA, a nongovernmental organization (NGO) in rural Cambodia. Households in Tucson, Arizona, were monitored as part of a baseline for a disinfectant study previously published (Rusin et al. 1998). Data are also compared to results from a study conducted in Japan and the findings from a study in England (Scott et al. 1982; Ojima et al. 2002). The ADRA Cambodia project operates under an existing memorandum of understanding with the Cambodian Ministry of Health which allows this study and the related hand‐washing project. The IRB committees at Loma Linda University and the University of Arizona did not require any approval because there was no intervention or interaction with individuals and no individually identifiable information.
Results
A total of eight houses were sampled for the Cambodia village survey and compared to the similar Tucson, Arizona, US study (Rusin et al. 1998). The Arizona study found the greatest concentrations of all three classes of bacteria on sites with moist environments such as the kitchen faucet handle. The highest faecal coliform contamination levels in Cambodia were on the ladle for sink water, the toilet seat surface and the cutting board surface, all moist locations (Table 2). The ladle for sink water had highest faecal coliform contamination. This is expected, as it is the comparable surface to the kitchen faucet handle in the US study. The cutting board was also highly contaminated in Cambodian homes. The cutting board is usually moist and had some food items near or on the board at the time of sampling. Similarly, the top of the squat‐style toilet was highly contaminated with faecal coliforms. These ceramic pour‐flush bowls are manufactured with two positions on either side of the toilet bowl for the user’s feet. Although made from the same smooth ceramic material as the bowl, the tread positions have grooves where water can pool allowing the area to be moister than the surrounding floor. Unlike the US study, the bathroom floor had the highest amount of HPC bacteria, but not faecal coliforms. Overall, the Cambodian study had over 100‐fold higher concentrations of faecal coliform bacteria than E. coli and over 100‐fold higher concentrations of faecal coliform bacteria than the US study.
Table 2.
Comparison of mean bacteria levels on household surfaces in Cambodia and the United States. Faecal coliform (FC), total coliform (TC), heterotrophic plate count (HPC) and Escherichia coli (EC) are shown in CFU cm−2
| US surface | FC | TC | HPC | Cambodia surface | FC | TC | HPC | EC |
|---|---|---|---|---|---|---|---|---|
| Sink faucet handle | 3 | 24 | 35 500 | Side of dipping ladle for sink water | 823 | 2 | 8370 | <1 |
| Counter top | 9 | 1 | 269 | Table or counter for food preparation | 116 | 34 | 5730 | 5 |
| Surface of cutting board | 1 | 33 | 9550 | Surface of cutting board | 740 | 1 | 15 000 | <1* |
| Toilet flush handle | 2 | 5 | 8130 | Handle of ladle for anal cleansing | 114 | 2 | 12 700 | <1* |
| Top and underside of toilet | 35 | 10 | 186 | Top of toilet (squat style) | 743 | 14 | 14 100 | 3 |
| Floor surface around the base of the toilet | 21 | 3 | 2880 | Floor surface around the base of the toilet | 395 | 4 | 16 000 | 2 |
*Escherichia coli was detected, but <1 cm−2 after converting to the Rusin et al. (1998) study’s unit of measurement.
Two sample t‐tests were used to compare the results from the US and Cambodian surfaces. While there were no significant difference between the two countries for total coliform and HPC bacteria, the faecal coliform levels in Cambodia were significantly higher (t = 2·2, df = 10, P < 0·01). This may be a function of the differences in climate, household design and overall household sanitation.
Table 3 shows the mean values for the bacteria studied but also describes the maximum and standard deviation values for the various surfaces studied in the eight Cambodian households. The maximum values are important because it is the highest concentration of enteric bacterial pathogens that pose the greatest risk (Haas 1996).
Table 3.
Geometric mean (μ), maximum bacteria levels (max) and standard deviation (σ) are shown for household surfaces in Cambodia. Faecal coliform (FC), total coliform (TC), heterotrophic plate count (HPC) and Escherichia coli (EC) are shown in log units per 4 cm2. Values shown in bold represent the maximum concentration per column
| Fomite | FC | TC | ||||
|---|---|---|---|---|---|---|
| μ | Max | σ | μ | Max | σ | |
| Side of dipping ladle for sink water | 4·12 | 5·00 | 1·25 | 1·52 | 3·48 | 1·25 |
| Basin for washing | 2·90 | 4·00 | 0·97 | 3·38 | 5·04 | 1·80 |
| Counter top | 3·27 | 3·54 | 0·38 | 2·74 | – | – |
| Cutting board | 4·07 | 5·30 | 1·74 | 1·22 | 2·59 | 0·99 |
| Handle of ladle for anal cleansing | 3·26 | 6·78 | 3·09 | 1·58 | 3·00 | 1·05 |
| Top of toilet (squat style) | 4·08 | 4·15 | 0·11 | 2·34 | 4·04 | 1·61 |
| Floor surface around base of toilet | 3·80 | 4·60 | 1·13 | 1·80 | 4·01 | 1·23 |
| Bucket to retrieve water from well | 1·91 | 2·81 | 1·28 | 0·50 | 0·50 | 0·50 |
| Rim of well | 0·50 | – | – | 0·86 | 2·30 | 0·81 |
| Floor around well (well apron) | – | – | – | 3·27 | 5·02 | 1·51 |
| Fomite | HPC | EC | ||||
|---|---|---|---|---|---|---|
| μ | Max | σ | μ | Max | σ | |
| Side of dipping ladle for sink water | 5·13 | 6·00 | 0·99 | 0·50 | 0·50 | 0·50 |
| Basin for washing | 4·65 | 6·00 | 1·26 | 1·00 | 4·01 | 1·74 |
| Counter top | 4·96 | 5·62 | 0·93 | 1·92 | 2·92 | 1·67 |
| Cutting board | 5·38 | 5·84 | 0·49 | 0·27 | 1·35 | 0·60 |
| Handle of ladle for anal cleansing | 5·31 | 5·97 | 0·70 | 0·33 | 1·00 | 0·47 |
| Top of toilet (squat style) | 5·35 | 5·74 | 0·64 | 1·60 | 3·54 | 1·61 |
| Floor surface around base of toilet | 5·41 | 5·85 | 0·45 | 1·50 | 2·63 | 1·19 |
| Bucket to retrieve water from well | 5·00 | 5·77 | 0·82 | 0·50 | 0·50 | 0·50 |
| Rim of well | 5·06 | 5·72 | 0·61 | 0·50 | 0·50 | 0·50 |
| Floor around well (well apron) | 5·48 | 5·62 | 0·19 | 2·08 | 3·85 | 1·55 |
Sanitation survey
All eight houses sampled have similar stilt‐house construction with elevated living and sleeping quarters, leaving the space under the house for the mid‐day activities. Five of the eight houses had a kitchen attached to the upper level, while the remaining houses had their kitchen area in an improvised zone under the house. Houses were constructed with wooden walls and tile or corrugated metal roofs. Unlike houses in the United States, no insulation or additional wall material is added to the wall. The rudimentary kitchen consists of some large plastic basins for washing dishes, a wooden table for arranging food, a charcoal stove, some plastic containers for vegetables, a cutting board and a plastic rack with eating utensils. All kitchen areas are smoky and dark with no natural light. Breakfast and lunch meals are eaten in the outdoor area on a table under the house, while dinner is eaten in the main house on a roll‐out plastic mat. Refrigerators were not observed and Cambodian project assistants explained that food is sometimes stored in a cabinet overnight.
Houses were selected for this study on the basis that they had a latrine. Through a subsidy programme with the NGO ADRA, all houses had a pour‐flush latrine built from cement or a cement–wood combination (Fig. 1). These were white ceramic pour‐flush latrines, which are most suitable where people use water for anal cleansing and squat to defecate. These latrines were built with a cement septic tank and PVC plumbing. The septic tank was built from circular cement rings, which are also used to line wells. Three of the eight houses had a separate wash or bathing room next to the room with the pour‐flush latrine. In four of the eight houses, children were seen going in and out of the latrine, indicating regular use by the household. Five latrines had a pair of sandals near the doorstep for use while using the latrine. Latrines and bathrooms were kept relatively clean, but no soap or other cleaning material was seen with the exception of powdered laundry detergent at one house. Dishes are washed with plastic scrub brush in large plastic basins with water, which was obtained from the onsite well. The dishes are then air‐dried on a rack and sometimes wiped with a rag designated for the kitchen. There was a plastic ladle cup, which is used to transfer water to the dish washing basins. This cup was reported to be a multitasking tool, where it is used to wash dishes, wash clothes, prepare food and occasionally used as a cup for drinking water. Soap was seen in only one of the houses and was a powdered laundry detergent. This type of soap is used for washing laundry, dishes and hands. No bar soap or other form was seen. Bathing and showers occasionally take place in the built bathroom located outside of the house, but more commonly using a bucket while standing next to their household well and wearing the traditional Kramah sarong. Although no pets were reported, many pigs, chickens, stray dogs and cats were seen in the all of the house yards.
Figure 1.

Pour‐flush latrine in Beung village of Kompong Thom province, Cambodia. The pictured latrine features a tiled cement slab with a ceramic bowl, a cement water basin and a plastic ladle for anal cleansing.
England and Japan
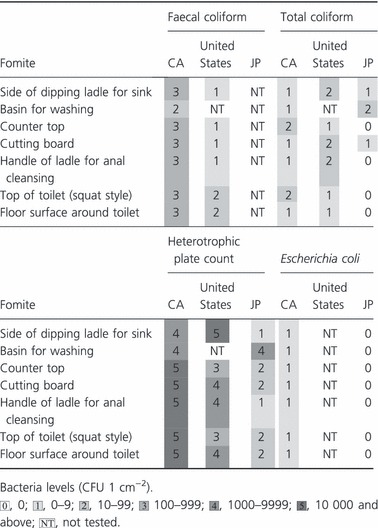
All regional studies reviewed for this paper found that moist areas in the kitchen are where the highest concentrations of indicator bacteria occur (Table 4). The Japanese study found that bacterial contamination was highest in kitchens and lowest in toilets (Ojima et al. 2002). The England household investigation found enterobacteria common at wet sites and rare at dry sites. Salmonella was also common and high numbers of E. coli were found on the kitchen sink surfaces, suggestive of active bacterial growth (Scott et al. 1982). The England study found frequent contamination of dishcloths and other wet cleaning utensils. Authors of the England study suggested that these cleaning items might be reservoirs and also disseminators of contamination in the kitchen. As discussed previously, the US study also found that the kitchen is the most contaminated site with the toilet seat being the least contaminated (Rusin et al. 1998).
Table 4.
Comparison of mean bacterial levels for Cambodian (CA) fomites with comparable surfaces reported for US (US) and Japan (JP) studies
Discussion
Heterotrophic plate count bacteria were found on all of the tested surfaces with a geometric mean range of 5000–16 000 colony forming units per square centimetre (CFU cm−2). Because all samples were positive for HPC bacteria with no consistent difference between sites, the HPC prevalence provides little information of the hygiene of various environments. Total coliforms and E. coli varied in occurrence and provided a better estimation of relative contamination levels. More research is needed to determine whether these indicators are reliable indicators of pathogen occurrence for fomites in a developing country setting.
Other authors have suggested that the areas of greatest public health risk can be found through monitoring of indicator bacteria on environmental surfaces (Reynolds et al. 2005). This study identifies areas in Cambodian households where exposure to environmental bacteria will likely occur. The methods used in this paper could be adapted as monitoring tools appropriate for a hygiene or sanitation public health intervention programme in a developing country.
A complete sanitation and hygiene improvement programme should consider multiple control points (barriers) for environmental pathogens living on food, water, hands, fomites or in the air. This multiple barrier system is detailed in a discussion of the environmental infection transmission system model (Li et al. 2009), which considers physical proximity, microbe pick‐up rate, pathogen elimination rate, deposition rate and social encounters. A complete hygiene intervention focusing on the control of these sources of contamination is rare, while a single pathway model is much more common (Eisenberg et al. 2007). The Cambodian village homes in this study were selected because they use a pour‐flush latrine as a single barrier for environmental pathogen transmission. Results from this study demonstrate that a single barrier is not effective for household sanitation. When compared to the eight homes in Cambodia, homes in industrialized countries (i.e. United States and Japan) have additional environmental barriers that may control fomite contamination. The most effective barriers are thought to be the chlorinated water distribution system, a solid waste disposal system, a more elaborate home construction with easily washable surfaces and cleaning product availability. In addition, homes in these countries have indoor climate control systems and lower relative indoor humidity than tropical Cambodia.
In any hygiene and sanitation improvement programme, an effort should be made to include as many pathogen control points as possible. What is often left out of public health interventions is an assessment of fomite contamination as an indicator of improved household sanitation. The swab and indicator bacteria methods described in this paper can be used as monitoring tools to identify the greatest potential exposure and public health risk. Further studies in Cambodia could combine the protein and biochemical marker investigations as described by Reynolds (Reynolds et al. 2005) with a full‐scale investigation into household hygiene including subtopics on solid waste, surface disinfection and fomite contamination. Additional studies should investigate these topics among households in varying socio‐economic classes, varying house construction types and the different types of well and latrine designs as defined by UNICEF (United Nations Children’s Fund 2006).
The study successfully identified surface contamination in household environments unique to rural Cambodia. The households surveyed were all homes that meet the hardware requirement of the sanitation and water supply component of the UN MDG by possessing a pour‐flush latrine and protected water well. The high contamination found in households was easily quantified by local NGO staff and can be used as a baseline for the planned hand‐washing intervention. The study determined that contamination levels in rural villages are much higher than contamination in US households. An additional benefit of the study was the interest of the villagers in their own home’s contamination level. If followed up, this stakeholder interest can lead to a successful public health education campaign on hand washing, cleaning products or other component.
In summary, the NGO’s efforts in promoting wells, latrines and other hardware need to be combined with hygiene promotion in the household and an enabling environment for effective community disease reduction.
References
- Boone, S.A. and Gerba, C.P. (2007) Significance of fomites in the spread of respiratory and enteric viral disease. Appl Environ Microbiol 73, 1687–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan, S.M. , Zhao, X.S. , Wen, R.F. , Huang, J.J. , Pi, G.H. , Zhang, S.X. , Han, J. , Bi, S.L. et al. (2003) Stability of SARS coronavirus in human specimens and environment and its sensitivity to heating and UV irradiation. Biomed Environ Sci 16, 246–255. [PubMed] [Google Scholar]
- Eisenberg, J.N. , Scott, J.C. and Porco, T. (2007) Integrating disease control strategies: balancing water sanitation and hygiene interventions to reduce diarrheal disease burden. Am J Public Health 97, 846–852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haas, C. (1996) How to average microbial densities to characterize risk. Water Res 30, 1036–1038. [Google Scholar]
- Li, S. , Eisenberg, J.N. , Spicknall, I.H. and Koopman, J.S. (2009) Dynamics and control of infections transmitted from person to person through the environment. Am J Epidemiol 170, 257–265. [DOI] [PubMed] [Google Scholar]
- Miles, A.A. and Misra, S.S. (1938) The estimation of the baterialcidal power of the blood. J Hyg 38, 732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ojima, M. , Toshima, Y. , Koya, E. , Ara, K. , Kawai, S. and Ueda, N. (2002) Bacterial contamination of Japanese households and related concern about sanitation. Int J Environ Health Res 12, 41–52. [DOI] [PubMed] [Google Scholar]
- Reynolds, K.A. , Watt, P.M. , Boone, S.A. and Gerba, C.P. (2005) Occurrence of bacteria and biochemical markers on public surfaces. Int J Environ Heal Res 15, 225–234. [DOI] [PubMed] [Google Scholar]
- Rusin, P. , Orosz‐Coughlin, P. and Gerba, C. (1998) Reduction of faecal coliform, coliform and heterotrophic plate count bacteria in the household kitchen and bathroom by disinfection with hypochlorite cleaners. J Appl Microbiol 85, 819–828. [DOI] [PubMed] [Google Scholar]
- Scott, E. (1996) Foodborne disease and other hygiene issues in the home. J Appl Bacteriol 80, 5–9. [DOI] [PubMed] [Google Scholar]
- Scott, E. , Bloomfield, S.F. and Barlow, C.G. (1982) An investigation of microbial contamination in the home. J Hyg (Lond) 89, 279–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair, R.G. , Choi, C.Y. , Riley, M.R. and Gerba, C.P. (2008) Pathogen surveillance through monitoring of sewer systems. Adv Appl Microbiol 65, 249–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Childrens Fund (2006) Water, sanitation and hygiene:definition of indicators. (online) Available at: http://www.unicef.org/progressforchildren/2006n5/index_35533.htm (accessed 18 October 2010).


