Summary
The aim of this study was to investigate characteristics, outcomes and risk factors for death from burn in preschool children. A retrospective study was conducted on 3688 preschool burn children admitted to the National Burn Hospital from 1/1/2016 to 31/12/2018. Collected data included patient demographics and burn characteristics. Bivariate and multivariate analysis was conducted to determine independent risk factors for death. Results showed that preschool children accounted for 78.8% of total admitted burn children. The main causal agent was scald. Boys were predominant, and 76.5% patients lived in rural areas. The highest number of burn accidents occurred in winter. In addition, average burn surface area was of 8.8% total body surface area (TBSA) and 43.5% of patients suffered deep burn injury. Overall mortality rate was 0.5% with LA50 of 81.7% and 49.1% for full thickness burn area. A significantly higher mortality rate was seen in patients with inhalation injury. Compared to survivors, patients who died had a significantly larger burn surface area and larger deep burn area. Multivariate logistic analysis for death indicated that presence of inhalation injury and increased burn extent were independent risk factors for death. Inhalation injury resulted in a 3.4 probability unit of death. In conclusion, preschool burn injuries were more common in boys living in the countryside and were mostly caused by scald, with a high proportion of deep injuries. Except for in cases of extensive burn, inhalation injury was not common but was still the main cause of death.
Keywords: burn feature, preschool age, outcome
Abstract
Le but de ce travail rétrospectif réalisé entre le 1/1/2016 et le 31/12/2018 sur 3 688 enfants hospitalisés dans l’hôpital brûlologique national était d’étudier les caractéristiques, l’évolution et les déterminants de mortalité (analyse multivariée) des brûlures touchant des enfants d’âge pré- scolaire. Ces enfants comptent pour 78,8% des admissions pédiatriques. L’ébouillantement est le mécanisme prédominant. Les garçons sont plus touchés ; 76,5 % des patients habitent en milieu rural et les brûlures sont plus fréquemment hivernales. La surface brûlée moyenne est de 8,8% et 43,5% des patients ont des atteintes profondes. La mortalité est de 0,5% avec une DL50 de 81,7% dont 49,1% de profond. En analyse multivariée, l’augmentation de surface brûlée et l’inhalation de fumées (OR 3,4) sont des facteurs indépendants de risque de mortalité. Les brûlures survenant à l’âge préscolaire sont donc des ébouillantements de garçons ruraux, fréquemment profonds. L’inhalation de fumées est donc rare mais reste un facteur de risque mortalité.
Introduction
Burns are common among children, who according to world-wide reports account for about 40-60% of total hospitalized burn patients, the percentage being especially higher in the developing world.1,2,3 Preschool children (0-6 years) are vulnerable to burn injuries because of their limited knowledge and recognition of injury, protection methods and first aid.4 In addition, the visceral organs of preschool children are immature, especially their immunologic and respiratory systems, and this could influence manifestation and outcomes compared to older children.5,6,7 To date, many authors have reported epidemiological characteristics and outcome among pediatric burn patients, but few reports mention burn patterns among preschoolers.8,9,10,11,12,13 In this study we investigated burn features, outcomes and risk factors for death among preschool children admitted to the Vietnam National Burn Hospitals over the three-year period 2016 to 2018.
Methods
A retrospective study was conducted on all burn children from 0 to 6 years of age admitted to the National Burn Hospital over a three-year period from 1/1/2016 to 31/12/2018. Collected data included patient demographics such as age, gender, burn causal agents, the season and month that burn occurred, and burn characteristics including burn extent, deep burn, full thickness burn area, inhalation injury, complication and mortality. Bivariate and then multivariate analysis was performed to determine independent risk factors for death. Lethal area fifty percent (LA50) was calculated for total burn surface area and full thickness burn area using the Probit model. Data were analyzed using Intercool Stata 10.0 software and p value < .05 was considered as a significant level. The study was approved by the National Burn Hospital’s Ethics Committee.
Results
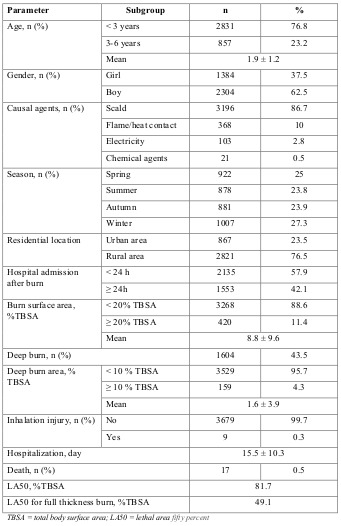
Between 2016 and 2018, out of the total 4683 pediatric burn patients admitted to our hospital, 3688 (78.8%) were under 6 years old. The main causal agent was scald (86.7%) and boys were predominant (62.5%). Regarding season and month, the highest number of burn accidents occurred in the winter (27.3%) and the highest burn incidence (10.1%) was recorded in February (data not shown). In addition, 76.5% patients lived in rural areas and 57.9% were admitted to our hospital during the first 24h post burn. Average burn surface area was 8.8% of total body surface area (TBSA). Of the 3688 patients, 2391 (64.8%) cases had a burn surface area <10% TBSA, and 11.4% patients had a burn extent of over 20% TBSA. It is noted that 43.5% patients suffered deep burn injury and most of them (95.7%) had a deep burn area < 10% TBSA. Inhalation injury was recorded in 9 cases, accounting for 0.3%. Overall mortality rate was 0.5% with LA50 of 81.7%. LA50 for full thickness burn was 49.1% (Table I).
Table I. Patient demographics and burn features.
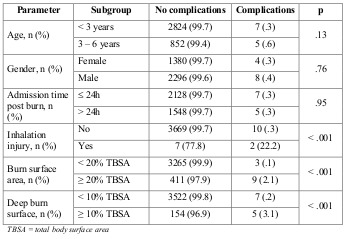
Post burn complications developed in 12 patients, accounting for 0.3% (data not shown). The most common complication was sepsis (50%). More complications were recorded in patients with inhalation injury (22.3% vs. 0.3%; p < .001) or extensive burn, while age and gender did not significantly affect complication development (Table II).
Table II. Distribution of complications by variables.
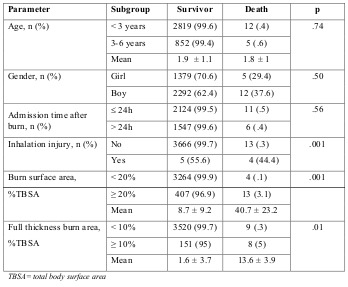
Bivariate analysis between death and other variables showed that a significantly higher mortality rate was seen in patients with inhalation injury (44.4% vs. 0.3%; p < .001), larger burn surface area (40.7 ± 23.2% vs. 8.7 ± 9.2% TBSA; p < .01) and larger full thickness burn area (13.6 ± 3.9% vs. 1.6 ± 3.7% TBSA; P < .001). It is noted that there was only 0.1% deaths in the group of patients with burn extent < 20%TBSA, and 3.1% among cases with burn extent ≥ 20% TBSA. In addition, only 0.3% of patients who suffered deep burn area < 10% TBSA died compared to 5% in the other group. Age and gender did not affect mortality rate (Table III).
Table III. Relationship between death and other variables.
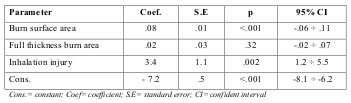
Multivariate logistic analysis for death is indicated in Table IV. As can be seen, increased burn extent and presence of inhalation injury were independent risk factors influencing mortality rate. The presence of inhalation injury resulted in a 3.4 probability unit of death with p < .01. This was .08 for burn extent with p < .001.
Table IV. Multivariate logistic analysis for death and variables.
Discussion
Worldwide, childhood burns continue to be considered as one of the major problems resulting in significant morbidity and death. It is estimated that about one-third of burn injuries in the United States occur in the pediatric population, and they are mostly caused by scalding in the subgroup of children under 5 years of age.14 Generally, management of burn injuries in children and adults is similar, but there are significant physiological and psychological differences. In addition, the skin’s dermal layer is thinner in children than in adults. Increased evaporative loss and the need for isotonic fluids increases the risk of hypothermia in pediatric patients.5,6
Most studies on pediatric burns have indicated a predominance of males with most injuries due to scald. For example, in 2005 Maghsoudi and Samnia reported the male:female ratio to be 1.6:1, and scalds to be the most common type of burn among children under 5 years of age.15 In Israel, Haik and colleagues reported that children aged 1 and under accounted for 22.2% of total burn cases, with the most common etiology being hot liquids (45.8%).16 Another report from Israel by Goldman and co. showed that infants (ages 0-1) had the highest prevalence (45%), and scalds accounted for 68% of burns.17 Ying and Ho reported that in Hong Kong scalding was the most common cause of burn injury (90.4% of admissions), followed by flame burns (8.2%).13 Ramakrishnan et al. analyzed 535 children aged 0-18 years in India and showed that scalds were the most common type of burn among children under 4 years of age.18 However Kuma et al., also from India, reported that among childhood burns, females were affected more than males (74.1 vs. 25.9%) and injuries were mostly caused by scald (72.5%) followed by flame and electrical burn.10 In Turkey, Sakallioğlu and colleagues reported that the highest proportion of patients belonged to the preschool age group, and that scalding (59.7%) was the leading cause of burn.19 In China, works by Tang Ket al. indicated that children suffered more scald burns (83%).20 The results of our study agree with world-wide reports: boys were predominant (62.5%) with 86.7% cases caused by scalding.
The explanation for the higher proportion of preschool burns in developing countries could be that not all children under 6 years old are cared for in kindergarten and a significant number of them stay at home, playing together, under standard care.
It is noted that gender was not associated with burn outcomes in preschool children. A study by Maghsoudi and Samnia showed that except for burn incidence, there were no significant differences between males and females.15 In our study, more complications and a higher mortality rate were recorded for male patients but the difference did not reach significant level compared to the female group. The same result has also been reported by other authors.18
Regarding burn extent, most studies reported that children suffered small burn size. Goldman and coworker indicated that 83% of infant patients suffered less than 20% TBSA burn.17 A report by Kuma et al. in India reported that 63.1% of the children received burn injuries in the range of 0 to 20% burn surface area.10 In our study, 88.6% preschool burn children had a burn extent of < 20% burn surface area.
Despite advances in critical care, including early excision and grafting, aggressive resuscitation and hypermetabolic regulation and nutritional support, mortality rate is still high among pediatric patients with severe burns, especially in developing countries.21,22,23 Ramakrishnan et al. analyzed 535 children aged 0-18 in India and reported that large burn size and infection were the strongest predictors of mortality.18 Kuma and coworkers studied 309 children with burns injuries, also in India, and reported that overall pediatric burn mortality was 7.4%.10 According to Williams et al. the leading causes of death over 20 years among pediatric burn patients were sepsis (47%), respiratory failure (29%), anoxic brain injury (16%) and shock (8%).24 In general, literature indicates that children tolerate more extensive burns and quite higher LA50 values compared to adults.25 Keshavarzi et al. reported that in Iran the LA50 for pediatric burn patients £10 years was 61.96%.26 LA50 of the pediatric burns in our study was 81.7% TBSA and 49.1% TBSA for full thickness burns.
Besides an immature immunological system, the respiratory tract of preschool children is narrower than that of older children, and it is easier for them to suffer edema after inhalation injury, leading to a high risk of airway compromise requiring intubation.5,27
Current reports indicate that inhalation injury is uncommon but leads to a significantly high mortality rate.16,18,28 In addition, it is difficult to manage a child with inhalation injury, especially with mechanical ventilation.29,30 According to a report by Ying and Ho in Hong Kong, 1.6% of childhood burn patients had inhalation injury requiring intubation and ventilation support.13 This incidence in our study was only 0.3%, but mortality rate was 44.4% and inhalation injury was one of the independent risk factors for death. In Iran, one report showed that death by inhalation injury amongst preschool children was up to 100%. According to Morrow et al., inhalation injuries were strongly associated with large burns and death in infants compared to few deaths seen in cases of burn size less than 30% TBSA without inhalation injury.31 Barrow and colleagues reported that amongst children with 21-80% TBSA burns, there was a significant difference in mortality between those with and without inhalation injury (13.9% vs. 2.9%). In our study, the presence of inhalation injury resulted in a 3.4 probability unit of death.
Conclusion
We have shown that burns in preschool children were more common in boys living in the countryside, and were mostly caused by scald, with a high proportion of deep injuries. Except for in cases of extensive burn, inhalation injury was not common but was still the main cause of death among this subgroup in Vietnam.
References
- 1.Ahmadabadi A, Tavousi SH, Sedaghat A, Khadem Rezaeyan M. Pattern of burns injury in preschool children. J Saf Promot Inj Prev. 2016;4(4):225–230. [Google Scholar]
- 2.Al-Shehri M. The pattern of pediatric burn injuries in Southwestern, Saudi Arabia. West Afr J Med. 2004;23(4):294–299. doi: 10.4314/wajm.v23i4.28144. [DOI] [PubMed] [Google Scholar]
- 3.Barcellos LG, Silva APPD,, Piva JP, Rech L, Brondani TG. Characteristics and outcome of burned children admitted to a pediatric intensive care unit. Rev Bras Ter Intensiva. 2018;30(3):333–337. doi: 10.5935/0103-507X.20180045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel DD, Rosenberg M, Rosenberg L. Poverty, population density, and the epidemiology of burns in young children from Mexico treated at a U.S. pediatric burn facility. Burns. 2018;44(5):1269–1278. doi: 10.1016/j.burns.2018.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mathias E, Srinivas Murthy M. Pediatric thermal burns and treatment: a review of progress and future prospects. Medicines (Basel) 2017;4(4):91. doi: 10.3390/medicines4040091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leung A, Balaji S, Keswani SG. Biology and function of fetal and pediatric skin. Facial Plast Surg Clin N Am. 2013;21:1–6. doi: 10.1016/j.fsc.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stamatas GN, Nikolovski J, Luedtke MA, Kollias N, Wiegand BC. Infant skin microstructure assessed in vivo differs from adult skin in organization at the cellular level. Pediatr Dermatol. 2010;27:125–131. doi: 10.1111/j.1525-1470.2009.00973.x. [DOI] [PubMed] [Google Scholar]
- 8.He S, Zuo ZL. Epidemiological investigation on 1946 hospitalized pediatric patients with burns. Zhonghua Shao Shang Za Zhi. 2018;34(10):696–700. doi: 10.3760/cma.j.issn.1009-2587.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 9.Karimi H, Montevalian A, Motabar AR, Safari R, Parvas MS, Vasigh M. Epidemiology of paediatric burns in Iran. Ann Burns Fire Disasters. 2012;25(3):115–120. [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar P, Chirayil PT, Chittoria R. Ten years epidemiological study of paediatric burns in Manipal, India. Burns. 2000;26(3):261–264. doi: 10.1016/s0305-4179(99)00109-6. [DOI] [PubMed] [Google Scholar]
- 11.Song C, Chua A. Epidemiology of burn injuries in Singapore from 1997 to 2003. Burns. 2005;31 Suppl 1:S18–S26. doi: 10.1016/j.burns.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 12.Trop M, Herzog SA, Pfurtscheller K, Hoebenreich AM. The past 25 years of pediatric burn treatment in Graz and important lessons learned. An overview. Burns. 2015;41(4):714–720. doi: 10.1016/j.burns.2014.10.001. [DOI] [PubMed] [Google Scholar]
- 13.Ying SY, Ho WS. An analysis of 550 hospitalized pediatric burn patients in Hong Kong. J Burn Care Rehabil. 2001;22(3):228–231. doi: 10.1097/00004630-200105000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Lee J, Norbury W, Herndon DN. Total Burn Care. Vol. 2012. Elsevier, Amsterdam, The Netherlands: National Library of Medicine (US); 2012. Special considerations of age: the pediatric burned patient. pp. 405–414. [Google Scholar]
- 15.Maghsoudi H, Samnia N. Etiology and outcome of pediatric burns in Tabriz, Iran. Burns. 2005;31(6):721–725. doi: 10.1016/j.burns.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 16.Haik J, Liran A, Tessone A. Burns in Israel: demographic, etiologic and clinical trends, 1997-2003. Isr Med Assoc J. 2007;9(9):659–662. [PubMed] [Google Scholar]
- 17.Goldman S, Aharonson-Daniel L, Peleg K. Childhood burns in Israel: a 7-year epidemiological review. Burns. 2006;32(4):467–472. doi: 10.1016/j.burns.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 18.Ramakrishnan KM, Sankar J, Venkatraman J. Profile of pediatric burns Indian experience in a tertiary care burn unit. Burns. 2005;31(3):351–353. doi: 10.1016/j.burns.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 19.Sakallioğlu AF, Başaran O, Tarim A, Türk E. Burns in Turkish children and adolescents: nine years of experience. Burns. 2007;33(1):46–51. doi: 10.1016/j.burns.2006.05.003. [DOI] [PubMed] [Google Scholar]
- 20.Tang K, Jian L, Qin Z, Zhenjiang L. Characteristics of burn patients at a major burn center in Shanghai. Burns. 2006;32(8):1037–1043. doi: 10.1016/j.burns.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 21.Arbuthnot MK, Garcia AV. Early resuscitation and management of severe pediatric burns. Semin Pediatr Surg. 2019;28(1):73–78. doi: 10.1053/j.sempedsurg.2019.01.013. [DOI] [PubMed] [Google Scholar]
- 22.Atiyeh B, Masellis A, Conte C. Optimizing burn treatment in developing low-and middle-income countries with limited health care resources (Part 2). Ann Burns Fire Disasters. 2009;22:189–195. [PMC free article] [PubMed] [Google Scholar]
- 23.Palmieri TL. Pediatric burn resuscitation. Crit Care Clin. 2016;32(4):X–X. doi: 10.1016/j.ccc.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 24.Williams FN, Herndon DN, Hawkins HK, Lee OJ. The leading causes of death after burn injury in a single pediatric burn center. Crit Care. 2009;13(6):R183. doi: 10.1186/cc8170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seyed-Forootan K, Karimi H, Motevalian SA, Momeni M. LA50 in burn injuries. Ann Burns Fire Disasters. 2016;29(1):14–17. [PMC free article] [PubMed] [Google Scholar]
- 26.Keshavarzi A, Kardeh S, Pourdavood A, Mohamadpour M, Dehghankhalili M. Determinants of the Lethal Area 50 index (LA50) in burn patients admitted to a tertiary referral burn center in Southern Iran. Bull Emerg Trauma. 2018;6(1):59–63. doi: 10.29252/beat-060109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fidkowski CW, Fuzaylov G, Sheridan RL, Coté CJ. Inhalation burn injury in children. Paediatr Anaesth. 2009;Suppl 1:147–154. doi: 10.1111/j.1460-9592.2008.02884.x. [DOI] [PubMed] [Google Scholar]
- 28.Barrow RE, Spies M, Barrow LN, Herndon DN. Influence of demographics and inhalation injury on burn mortality in children. Burns. 2004;30(1):72–77. doi: 10.1016/j.burns.2003.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Romanowski KS, Palmieri TL. Pediatric burn resuscitation: past, present, and future. Burns & Trauma. 2017;5:26. doi: 10.1186/s41038-017-0091-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Strobel AM, Fey R. Emergency care of pediatric burns. Emerg Med Clin North Am. 2018;36(2):441–458. doi: 10.1016/j.emc.2017.12.011. [DOI] [PubMed] [Google Scholar]
- 31.Morrow SE, Smith DL, Cairns BA, Howell PD. Etiology and outcome of pediatric burns. J Pediatr Surg. 1996;31(3):329–333. doi: 10.1016/s0022-3468(96)90732-0. [DOI] [PubMed] [Google Scholar]


