The current outbreak of COVID-19 was first described as a pneumonia of unknown origin, which rapidly spread from the city of Wuhan to mainland China and ultimately, throughout the world.1,2 On March 11, the World Health Organization declared the COVID-19 a pandemic and urged countries to refine their planning, monitoring, and readiness to act on their confirmed and suspected cases of the virus.3 While Canada is still considered a low-risk country, with currently 39 805 patients confirmed with the disease (at press time),4 protocols are being rapidly established due to the fluidity of the situation in order to flatten the curve and contain the virus spread rate, which has already succeeded that of the SARS outbreak in 2003.5,6
In the spring of 2003, Toronto experienced the largest SARS outbreak outside Asia, with 257 cases and 43 deaths.5–8 Under the emergency management act, all non-urgent hospital admissions were restricted; unfortunately, compliance to this measure was not reinforced in an orderly fashion, based on priorities.7 During that restriction period, the rate of elective surgery had a modest decreased of 15–22% during the early and late phases of the outbreak and rates of admissions for urgent surgery remained stable.5,7 Based on the 2005 Toronto influenza pandemic prediction model, this reduction in admission numbers represented an insufficient decrease unable to manage the surge capacity when compared to the forecasted rate of admissions.7 This alerted us to the need for more efficacious public health policies on restriction of non-urgent clinical activities to increase flow capacity.8,9 At the time of writing of this editorial, most hospitals across Canada have already significantly restricted scheduled (non-urgent) elective urological surgeries. Multiple lists of both cancer and non-cancer cases that should be initially cancelled have circulated on social media. For the benefit of practices across Canada, we provide an example protocol to aid in eventual rescheduling in the face of the projected increase to our waiting lists.
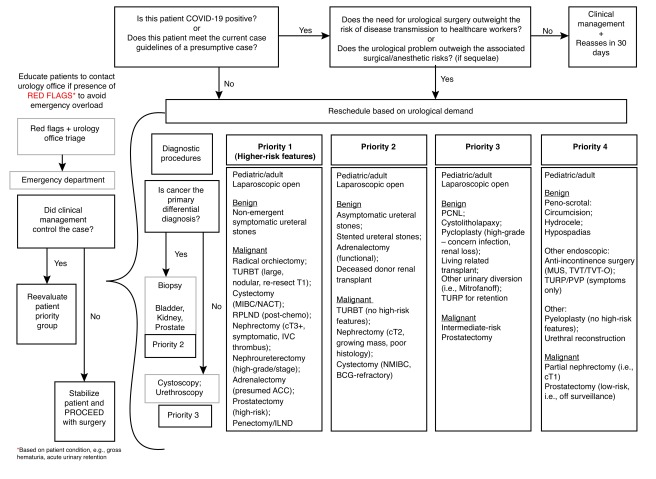
The optimal management of elective surgery waiting lists is a multifaceted problem that occurs in different countries regardless of the presence of a universal healthcare system.10 To cope with this situation, we suggest a grading system based on risk priority to reschedule elective surgeries and manage standby periods (Fig. 1). Grading occurs from 1–4, where “priority 1” is the cluster of the most severe cases based on clinical presentation, presence of red flags, and demographics. It is important to point out that classifying patients to a specific priority level is a dynamic and ongoing process where reclassification may be needed based on disease progression, as well as the surgeon’s clinical judgment. Furthermore, different practices and hospitals with specific foci of urological care may find these suggestions imperfect for their particular situation and regional role; however, we hope this protocol serves as a starting point for justifying priority of case selection in the coming weeks to months.
Fig. 1.
Decision-making algorithm for rescheduling urology elective surgeries post-COVID-19 outbreak. ACC: adenocortical carcinoma; BCG: bacillus Calmette-Guérin; ILND: inguinal lymph node dissection; IVC: inferior vena cava; MIBC: muscle-invasive bladder cancer; MUS: mid-urethral sling; NACT: neoadjuvant chemotherapy; NMIBC: non-muscle-invasive bladder cancer; PCNL: percutaneous nephrolithotomy; RPLND: retroperitoneal lymph node dissection; TURBT: transurethral resection of bladder tumour; TURP: transurethral resection of the prostate; TVT: tension-free vaginal tape; TVT-O: tension-free vaginal obturator tape.
Cancelling elective surgery is a crucial step in creating surge capacity to prioritize hospital resources during pandemics. Using priority-based grading strategies to reschedule elective surgery and procedures is a crucial strategy to help mitigate the impact of the COVID 19 outbreak on hospital performance.
Footnotes
Competing interests: The authors report no competing personal or financial interests related to this work.
References
- 1.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–1207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Coronavirus disease (COVID-2019) situation reports. [Accessed March 2020]. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200313-sitrep-53-covid-19.pdf?sfvrsn=adb3f72_2.
- 4.Government of Canada. Coronavirus disease (COVID-19): Outbreak update. [Accessed March 2020]. Available at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection.html#a5.
- 5.Schull MJ, Stukel TA, Vermeulen MJ, et al. Effect of widespread restrictions on the use of hospital services during an outbreak of severe acute respiratory syndrome. CMAJ. 2007;176:1827–32. doi: 10.1503/cmaj.061174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stukel TA, Schull MJ, Guttmann A, et al. Health impact of hospital restrictions on seriously ill hospitalized patients: Lessons from the Toronto SARS outbreak. Med Care. 2008;46:991–7. doi: 10.1097/MLR.0b013e3181792525. [DOI] [PubMed] [Google Scholar]
- 7.Schull MJ, Stukel TA, Vermeulen MJ, et al. Surge capacity associated with restrictions on non-urgent hospital utilization and expected admissions during an influenza pandemic: Lessons from the Toronto severe acute respiratory syndrome outbreak. Acad Emerg Med. 2006;13:1228–31. doi: 10.1197/j.aem.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 8.Hawryluck L, Lapinsky SE, Stewart TE. Clinical review: SARS – lessons in disaster management. Crit Care. 2005;9:384–9. doi: 10.1186/cc3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chu D, Chen RC, Ku CY, et al. The impact of SARS on hospital performance. BMC Health Serv Res. 2008;8:228. doi: 10.1186/1472-6963-8-228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kawakami J, Hopman WM, Smith-Tryon R, et al. Measurement of surgical wait times in a universal healthcare system. Can Urol Assoc J. 2008;2:597–603. doi: 10.5489/cuaj.974. [DOI] [PMC free article] [PubMed] [Google Scholar]