Abstract
The novel coronavirus (COVID-19) has been declared a worldwide pandemic. It was initially thought to spare children and adolescents as significantly smaller number of cases have been reported in the pediatric population in comparison to adults. Here, we report the case of a 16-month-old female infant from Lebanon who presented with fever and severe diarrhea and tested positive for COVID-19. Her symptoms started six days prior to presentation with no cough, rhinorrhea, or other respiratory manifestations reported. Chest radiography showed lobar consolidation and bronchial infiltrates. Blood culture was positive for Streptococcus pneumoniae. Stool and urine cultures were negative. She was treated with ceftriaxone and metronidazole. Her RT-PCR test was negative after five days of treatment, suggesting that children can clear the virus faster than adults. The patient likely contracted the virus from her parents, who because of the fear of social stigma hide recent history of respiratory illness. These findings serve as a practical reference for the clinical diagnosis and medical treatment of children with COVID-19.
Keywords: covid-19, coronavirus, sars-cov-2, pediatrics, infants, pandemic, lebanon, middle east, gastrointestinal symptoms, children
Introduction
The novel coronavirus disease 2019 (COVID-19) is the result of an infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), a member of Betacoronavirus. Initial cases were detected in Wuhan, a city in China, near the end of 2019 [1]. The virus is believed to replicate in the respiratory system during the prodromal period, and exhibits human-to-human transmission patterns through respiratory droplets and contact routes [1,2]. The disease causes mild to severe illness, with symptoms appearing 2-14 days after exposure and most commonly comprising fever, cough, and shortness of breath. Most severe illness occurs in older adults but comparison with the pediatric population can be challenging as documented cases in infants and children have been scarce [3,4].
As of mid-March 2020, COVID-19 has spread rapidly and widely to become a global pandemic [5]. Outbreaks have been reported in China, South Korea, Iran, Italy, Spain, and the United States. Many other European, Asian, African, and North and South American countries have been reporting cases [6]. Nevertheless, the Middle East countries have been lagging in terms of publishing clinical outcomes [7].
Case presentation
Here, we report the first case in the Middle East of a 16-month-old Lebanese female, previously healthy, who had symptomatic COVID-19.
The patient was transferred from another hospital due to increasing hypoactivity and severe diarrhea. The referring hospital had ruled out coronavirus infection due to the absence of cough. Parents reported that the infant was healthy and had regular food intake until symptoms started six days prior to presentation. They denied exposure to or contact with infectious risk factors and affirmed that no cough/rhinorrhea symptoms were present.
Upon examination, the patient was febrile (40°C) with a respiratory rate of 24 breaths per minute and a heart rate of 166 bpm. Chest auscultation revealed rhonchi. Differential diagnoses included gastroenteritis, pneumoniae, and COVID-19, and the patient was put on isolation as a preliminary measure.
Laboratory studies revealed leukocytosis with a white cell count of 15,000 cu mm (range: 3,400-9,600) and elevated C-reactive protein level reaching 231.16 mg/L (range: 0-5) (Table 1).
Table 1. Laboratory test results of the infant upon presentation.
BUN: blood urea nitrogen; EGFR: estimated glomerular filtration rate; SGPT: serum glutamic pyruvic transaminase; CRP: C-reactive protein; RBC: red blood cell; MCV: mean corpuscular volume; MCH: mean corpuscular hemoglobin; RDW: red cell distribution width; MPV: mean platelet volume; PDW: platelet distribution width; ANC: absolute neutrophil count; ALC: absolute lymphocyte count.
*Values not within normal range.
| Laboratory Tests | At Presentation | Normal Range |
| Chemistry | ||
| Phosphorus | 3.15 mg/dL | >18 years: 2.7-4.8 |
| Na+ | 137.00 mmol/L | 136.00-145.00 |
| K+ | 3.93 mmol/L | 3.50-5.10 |
| CL- | 104.50 mmol/L | 98.00-107.00 |
| CO2 | *16.40 mmol/L | 23.00-29.00 |
| Creatinine | *0.21mg/dL | 0.51-0.95 |
| BUN | *4.00 mg/dL | 6.00-20.00 |
| Calcium | 9.33 mg/dL | 8.50-10.50 |
| Magnesium | 2.15 mg/dL | 1.70-2.60 |
| EGFR | 210.33 | >60.00 mL/min/1.72 m2 |
| SGPT | 21.00 U/L | 5.00-41.00 |
| Bilirubin total | 0.60 mg/dL | 0.20-1.00 |
| Bilirubin direct | *0.24 mg/dL | 0.00-0.20 |
| Serology | ||
| CRP | *231.16 mg/L | 0.00-5.00 |
| Hematology | ||
| RBC | *3.29 x106 cu mm | 3.92-5.13 |
| Hemoglobin (Hb) | *8.40 g/dL | 11.50-16.00 |
| Hematocrit (Ht) | *24.80% | 35.50-44.90 |
| MCV | *75.00 f L | 78.00-98.00 |
| MCH | *25.50 pg | 27.00-31.00 |
| RDW | 14.60% | 12.00-16.00 |
| Platelets | *524000 cu mm | 150000-375000 |
| MPV | 8.20 um3 | 6.00-11.00 |
| PDW | 12.80 % | 11.00-18.00 |
| WBC | *15,500 cu mm | 3400-9600 |
| Neutrophils | *74.40% | 40.00-65.00 |
| ANC | *11.50 cu mm | 1.56-6.45 |
| Lymphocytes | *15.80% | 25.00-40.00 |
| ALC | 2.45 cu mm | 0.95-3.07 |
| Monocytes | *9.30% | 2.00-8.00 |
| Monocyte count | *1.44 cu mm | 0.26-0.81 |
| Eosinophils | 0.50% | 0.00-4.00 |
| Eosinophil count | 0.08 cu mm | 0.03-0.48 |
| Basophils | 0.00% | 0.00-1.00 |
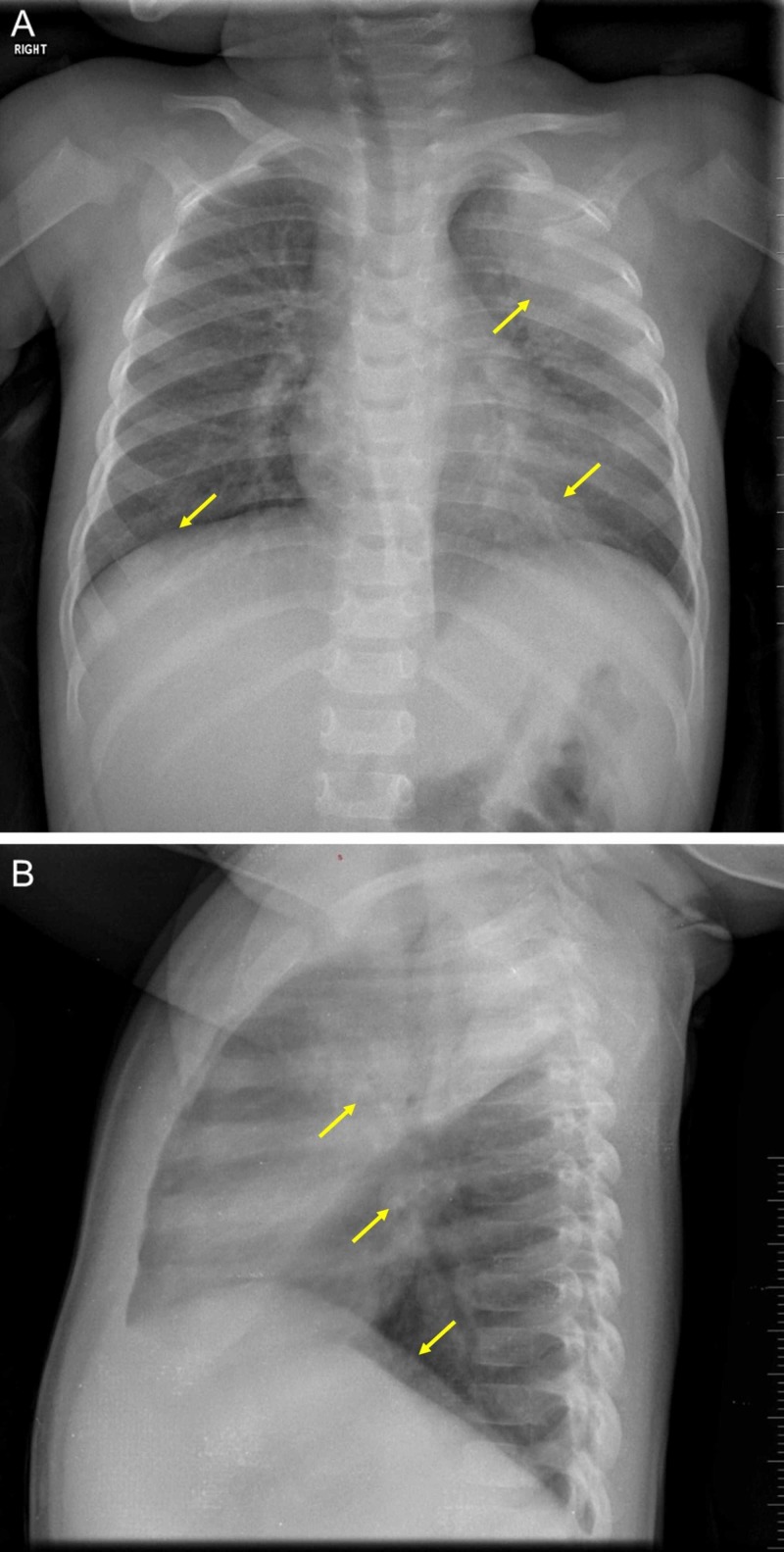
Cultures for blood, urine, and stool were taken. A chest radiograph showed left upper lobe consolidation and bilateral lower lobe infiltrates (Figure 1). This warranted nasopharyngeal swabs for an RT-PCR to test for SARS-CoV-2.
Figure 1. A chest radiograph.
Imaging of the infant’s chest shows large consolidation at the left apical lobe with bronchial infiltrates that are dominant at the left base, and asymmetrical lung bases (A). The heart size is normal, the rib cage is intact, and the diaphragmatic arches are in normal position (A). A discrete blunting at the left pleural sinus can be observed (B).
In the meantime, the patient was put on a hydration regimen and was started on ceftriaxone (75 mg/kg/day) and metronidazole (10 mg/kg, every eight hours). On day 2 of admission, the patient became afebrile and exhibited improvement in physical activity. On day 3, the result of the RT-PCR test returned positive for COVID-19. Blood culture was positive for Streptococcus pneumoniae. Stool and urine cultures were negative.
Upon further investigation, the father admitted that he had ‘flu-like’ symptoms two weeks before presentation but denied travel history or contact with a defined case of COVID-19. The mother also confessed having similar symptoms but did not seek medical consultation at the time. This hinted that the patient likely contracted the virus from her parents, who, in turn, might have been infected through community transmission. The family was transferred to a designated quarantine for isolation. On day 5, the RT-PCR test of the infant was negative, and the patient’s symptoms had resolved.
Discussion
Cases of COVID-19 in children are not as rare as they might have been thought [8,9]. This is the first case reported from the Middle East that involves a 16-month-old female infant. Around 2.4% of cases with COVID-19 were reported to be among the pediatric population in China [10]. Ages ranged between 3 and 14 years, with males being predominantly affected [10-12].
Uniquely, our patient presented with fever and diarrhea; cough and other respiratory symptoms were not reported. Previous COVID-19 studies in the pediatric population noted that common symptoms include fever, cough, sore throat, and rhinorrhea. Diarrhea has not been reported yet [6,10]. This warrants a more comprehensive definition of the symptoms that govern COVID-19 in the pediatric population, as gastrointestinal symptoms have been documented in our case and among adults [13].
The RT-PCR test was negative after five days of treatment and 11 days after the onset of symptoms. This suggests that children might clear the virus more rapidly than adults. Similarly, previous research in children indicates that the RT-PCR test becomes negative within 12 days (range: 6-22) after the presentation of symptoms [6]. The first RT-PCR test took two days for the result to generate, whereas the subsequent test was much faster, and the result was obtained on the same day due to the expansion of the testing capacity by the Lebanese Ministry of Public Health.
Fear of social stigma drove the patient’s parents to hide information of their respiratory tract illnesses. It is important to address this issue at public health levels and to stress and highlight the social responsibility associated with reporting any relevant medical data related to the COVID-19 pandemic. Moreover, health communication and promotion strategies must be improved to increase awareness and literacy on the current pandemic, and brush off rumors and misinformation that can cause fear and panic [14].
Conclusions
This is the first case reported from the Middle East on an infant presenting with fever and diarrhea that tested positive for COVID-19. Cases of COVID-19 in children are not as rare as they might have been thought. COVID-19 related pediatric symptoms can exhibit an array of presentations, including diarrhea. Most cases recover well with symptomatic care. This case serves as a practical reference for the clinical diagnosis and medical treatment of infants with COVID-19.
The content published in Cureus is the result of clinical experience and/or research by independent individuals or organizations. Cureus is not responsible for the scientific accuracy or reliability of data or conclusions published herein. All content published within Cureus is intended only for educational, research and reference purposes. Additionally, articles published within Cureus should not be deemed a suitable substitute for the advice of a qualified health care professional. Do not disregard or avoid professional medical advice due to content published within Cureus.
The authors have declared that no competing interests exist.
Human Ethics
Consent was obtained by all participants in this study
References
- 1.Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lu R, Zhao X, Li J, et al. Lancet. 2020;395:565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.A familial cluster of infection associated with the 2019 novel coronavirus indicating potential person-to-person transmission during the incubation period [Epub ahead of print] Yu P, Zhu J, Zhang Z, Han Y. J Infect Dis. 2020 doi: 10.1093/infdis/jiaa077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.SARS-CoV-2 infection in children [Epub ahead of print] Lu X, Zhang L, Du H, et al. N Engl J Med. 2020 doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Detection of covid-19 in children in early January 2020 in Wuhan, China. Liu W, Zhang Q, Chen J, et al. N Engl J Med. 2020;382:1370–1371. doi: 10.1056/NEJMc2003717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.An epidemiological study on COVID-19: a rapidly spreading disease. Khachfe HH, Chahrour M, Sammouri J, Salhab HA, Makki BE, Fares MY. Cureus. 2020;12:0. doi: 10.7759/cureus.7313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coronavirus disease (COVID-19) and pediatric patients: a review of epidemiology, symptomatology, laboratory and imaging results to guide the development of a management algorithm. Hasan A, Mehmood N, Fergie J. Cureus. 2020;12:0. doi: 10.7759/cureus.7485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.A bibliometric analysis of COVID-19 research activity: a call for increased output. Chahrour M, Assi S, Bejjani M, et al. Cureus. 2020;12:0. doi: 10.7759/cureus.7357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.A 55-day-old female infant infected with COVID 19: presenting with pneumonia, liver injury, and heart damage [Epub ahead of print] Cui Y, Tian M, Huang D, et al. J Infect Dis. 2020 doi: 10.1093/infdis/jiaa113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Novel coronavirus infection in hospitalized infants under 1 year of age in China [Epub ahead of print] Wei M, Yuan J, Liu Y, Fu T, Yu X, Zhang ZJ. JAMA. 2020 doi: 10.1001/jama.2020.2131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features [Epub ahead of print] Cai J, Xu J, Lin D, et al. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Clinical and CT features in pediatric patients with COVID‐19 infection: different points from adults [Epub ahead of print] Xia W, Shao J, Xia W, Shao J, Xia W, Shao J. Pediatr Pulmonol. 2020 doi: 10.1002/ppul.24718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China [Epub ahead of print] Dong Y, Mo X, Hu Y, et al. Pediatrics. 2020 [Google Scholar]
- 13.Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study [Epub ahead of print] Lei P, Mi M, Hong GR, et al. https://journals.lww.com/ajg/Documents/COVID_Digestive_Symptoms_AJG_Preproof.pdf. Am J Gastroenterol. 2020 doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Health communication research in the Arab world: a bibliometric analysis. Mheidly N, Fares J. Integ Health J. 2020;2:0. doi: 10.1136/ihj-2019-000011. [DOI] [PMC free article] [PubMed] [Google Scholar]