Summary
The term cytokine storm syndromes describes conditions characterised by a life-threatening, fulminant hypercytokinaemia with high mortality. Cytokine storm syndromes can be genetic or a secondary complication of autoimmune or autoinflammatory disorders, infections, and haematological malignancies. These syndromes represent a key area of interface between rheumatology and general medicine. Rheumatologists often lead in management, in view of their experience using intensive immunosuppressive regimens and managing cytokine storm syndromes in the context of rheumatic disorders or infection (known as secondary haemophagocytic lymphohistiocytosis or macrophage activation syndrome [sHLH/MAS]). Interleukin (IL)-1 is pivotal in hyperinflammation. Anakinra, a recombinant humanised IL-1 receptor antagonist, is licenced at a dose of 100 mg once daily by subcutaneous injection for rheumatoid arthritis, systemic juvenile idiopathic arthritis, adult-onset Still's disease, and cryopyrin-associated periodic syndromes. In cytokine storm syndromes, the subcutaneous route is often problematic, as absorption can be unreliable in patients with critical illness, and multiple injections are needed to achieve the high doses required. As a result, intravenous anakinra is used in clinical practice for sHLH/MAS, despite this being an off-licence indication and route of administration. Among 46 patients admitted to our three international, tertiary centres for sHLH/MAS and treated with anakinra over 12 months, the intravenous route of delivery was used in 18 (39%) patients. In this Viewpoint, we describe current challenges in the management of cytokine storm syndromes and review the pharmacokinetic and safety profile of intravenous anakinra. There is accumulating evidence to support the rationale for, and safety of, intravenous anakinra as a first-line treatment in patients with sHLH/MAS. Intravenous anakinra has important clinical relevance when high doses of drug are required or if patients have subcutaneous oedema, severe thrombocytopenia, or neurological involvement. Cross-speciality management and collaboration, with the generation of international, multi-centre registries and biobanks, are needed to better understand the aetiopathogenesis and improve the poor prognosis of cytokine storm syndromes.
Introduction
Haemophagocytic lymphohistiocytosis (HLH) is a potentially life-threatening, under-recognised, hyperinflammatory syndrome characterised by immune dysregulation leading to an uncontrolled, self-sustaining cytokine storm and multiorgan damage. Different terms are used to describe the clinical presentations of HLH; in this Viewpoint, we use cytokine storm syndromes. Cytokine storm syndromes represent a key interface between rheumatology and general internal medicine. Rheumatologists often lead in management, in view of their experience with immunosuppressive therapies and managing cytokine storm syndromes in the context of rheumatic disorders or infection (known as secondary haemophagocytic lymphohistiocytosis or macrophage activation syndrome [sHLH/MAS]). However, these patients might present to any medical specialty.
Cytokine storm syndromes confer a high mortality rate, with an all-cause mortality of approximately 40% in adults;1 early recognition and initiation of treatment is crucial to improve patient outcomes.2 Interleukin (IL)-1 is pivotal to the aetiopathogenesis of these syndromes. Off-licence anakinra, a recombinant humanised IL-1 receptor antagonist, is recommended (if available) in treatment algorithms for HLH,2, 3, 4, 5 but guidance regarding the route of administration is absent. Subcutaneous dosing could be difficult in patients with cytokine storm syndromes due to unreliable absorption in the context of critical illness and the fact that multiple daily injections are needed to achieve high-doses. Additionally, subcutaneous dosing can be painful and might be contraindicated in patients with thrombocytopenia and coagulopathy. Therefore, intravenous anakinra is already used in clinical practice for some cases of cytokine storm syndrome, including sHLH/MAS, although it is an off-licence indication and route of administration and little evidence exists to support its efficacy in this context. In this Viewpoint, we describe current challenges in managing patients with cytokine storm syndromes and our experience using intravenous anakinra in patients with sHLH/MAS in three international tertiary centres. We review the pharmacokinetic and safety profile of intravenous anakinra, define potential indications for intravenous dosing in patients with cytokine storm syndromes, and outline strategies to improve outcomes in these rapidly fatal and complex conditions.
Classification, epidemiology, and aetiopathogenesis of cytokine storm syndromes
HLH was originally classified in a binary manner as either primary (genetic) or secondary (acquired) HLH, although this classification might not be appropriate given evidence from contemporary modelling suggesting a continuum of genetic risk.6 In clinical practice, multiple diagnostic labels assigned to manifestations of cytokine storm syndromes, falling under the remit of various specialties with differing diagnostic and management priorities and approaches, might have impeded progress. Hence, there is a critical need and growing call for unified nomenclature (such as cytokine storm syndromes)4 and cross-specialty collaboration to pool resources and expertise.
Primary or familial HLH usually presents in infancy or early childhood and is considered a genetic disease of impaired perforin-dependent cytotoxic function. sHLH can present at any age and can be triggered by infection (commonly Epstein-Barr virus), haematological malignancy, autoimmune or autoinflammatory disorders, or iatrogenic causes, including haematopoietic stem cell transplantation.3 Hyperinflammation has a prevalence of 3·7–4·3% in patients with sepsis (macrophage activation-like syndrome).7 Severe cytokine release syndrome also occurs in some patients following chimeric antigen receptor (CAR) T-cell therapy for haematological malignancies, and this manifestation might also reside on an HLH spectrum.8 sHLH/MAS associated with rheumatological disorders is most common in paediatric and adolescent patients with systemic juvenile idiopathic arthritis and in patients with adult-onset Still's disease. Subclinical MAS occurs in 30–40% of children with systemic juvenile idiopathic arthritis,9, 10 whereas fulminant MAS has a prevalence of 10% in this population and of 10–15% in patients with adult-onset Still's disease.11, 12, 13 Systemic juvenile idiopathic arthritis and adult-onset Still's disease lie on a continuum of a single disease entity,14, 15 with MAS representing the underlying autoinflammatory disease activity at the severe end of the spectrum rather than a separate condition.
Infection is a common inciting event for MAS, both in patients with systemic juvenile idiopathic arthritis (approximately one third of patients)16 and those with adult-onset Still's disease.11, 12 MAS occurs in 0·9–9% of patients with systemic lupus erythematosus,13, 17, 18, 19 and indeed might be a complication of most rheumatic conditions, including rheumatoid arthritis, and vasculitis. Simultaneous infection and immunosuppression is likely to be culpable in triggering disease.1, 12, 13
sHLH is associated with a very high acute all-cause mortality of approximately 40% in adults,1 which rises to 85% in the context of malignancy.20 In a multicentre study21 of 68 patients with sHLH, the median overall survival was 4 months (95% CI 0·0–10·2 months); prognosis was worse in patients with a malignancy than in those without (median survival of 2·8 vs 10·7 months; p=0·007). MAS in patients with systemic juvenile idiopathic arthritis has a reported mortality of 8–22%.16, 22, 23
The threshold model of cytokine storm syndrome is a useful concept and refers to the combination of genetic predisposition, underlying inflammation (eg, adult-onset Still's disease or malignancy), and triggering insults (eg, infection) that culminate in hyperinflammation3 (eg, heterozygous familial HLH gene mutations [PRF1 and LYST] in adult patients with influenza-associated HLH).24 The aetiopathogenesis of cytokine storm syndromes is not fully understood but is thought to involve a failure of the normal perforin-dependent cytolytic function of natural killer cells and cytotoxic CD8 T cells, which regulate inflammation and maintain homoeostasis in the context of infection or inflammation by inducing apoptosis of antigen presenting cells.3 In cytokine storm syndromes, defective clearance of antigenic stimuli results in continuous activation and proliferation of macrophages (histiocytes), haemophagocytosis, and an autocrine loop of pro-inflammatory cytokines (cytokine storm), including IL-1β, IL-6, IL-8, IL-18, interferon gamma (IFNγ), and tumor necrosis factor, resulting in clinical sequelae including unremitting fever (the cardinal feature of cytokine storm syndromes).25
Diagnostic and management challenges
The main challenges in cytokine storm syndromes include lack of recognition (limited awareness) of the disease, difficulties with diagnosis in view of contested clinical criteria and potential confounders, and selection of treatment, which is largely based on expert consensus and extrapolated from familial HLH. Initiation of treatment is time sensitive, but missed and delayed diagnoses are common. Recognition of cytokine storm syndromes is challenging because the hyperinflammatory spectrum ranges from an innocuous and indolent state to a fulminant and fatal hypercytokinaemia, with non-specific overlapping features of many systemic illnesses, including the potential underlying drivers themselves (eg, sepsis, malignancy, and rheumatic disease).
Diagnostic criteria have been developed for familial HLH (HLH-2004 guidelines),26 MAS associated with systemic juvenile idiopathic arthritis,10 and sHLH (HScore;27 table 1 ). Diagnostic criteria for sHLH have not been universally agreed nor adopted, and current strategies (using HLH-2004 guidelines and HScore) have substantial limitations. The HScore has been shown to be more accurate for diagnosis than the HLH-2004 criteria if used at the time of presentation (sensitivity of 90%, but specificity of only 79%),28 although it is not widely used by haemato-oncologists in clinical practice. Use of the HLH-2004 criteria in adults is questionable, as the criteria have only been validated in children and include specialist tests (eg, soluble CD25) that are expensive, often difficult to access, and associated with long turnaround times for results in some centres, resulting in delays in diagnosis and treatment. Hyperferritinaemia is a key laboratory feature in both paediatric and adult practice. Ferritin levels within the normal range (<500 ng/mL) have a high negative predictive value for HLH, and this parameter has been incorporated in diagnostic algorithms, given the wide availability and low cost of the ferritin test.4, 6 Ferritin levels of more than 10 000 mg/L are diagnostic of HLH in children, with 96% specificity and 90% sensitivity.29 Ferritin level correlates with disease activity, and serial measurements are useful to monitor the response to treatment and relapse.3, 30 Both peak ferritin levels and a fall of less than 50% after treatment are associated with higher mortality.30 Hyperferritinaemia is less specific for HLH in adults,31, 32 as it can have other causes including liver failure. Different specialties might prioritise some features for diagnostic confirmation, adding further complexity. Tissue haemophagocytosis is probably the most contentious criteria for HLH diagnosis, although technically it is not considered essential for diagnosis. Haemophagocytosis has limited sensitivity and specificity, might be absent in the early stages of disease, and might be present in critical illness without sHLH.7
Table 1.
Selected MAS and HLH classification criteria*
| fHLH26 | Adult HScore27 | MAS-sJIA10 | |
|---|---|---|---|
| Clinical | |||
| Fever | Present | <38·4 (0); 38·4–39·4 (33); >39·4 (49) | Present |
| Hepatomegaly | Not included | Included (as below) | Not included |
| Splenomegaly | Present | Neither (0); either hepatomegaly or splenomegaly (23); both (38) | Not included |
| Immunosuppression | Not included | No (0); yes (18) | Not included |
| Laboratory | |||
| Cytopenias >2 lineages | Either: haemoglobin <90 g/L, platelets <100 × 109/L, or neutrophils <1 × 109/L | One lineage (0), two lineages (24), or three lineages (34) | Not included |
| Platelets | Included in cytopenia criteria | Included in cytopenia criteria | ≤181 × 109/L |
| Ferritin, ng/mL | ≥500 | <2000 (0); 2000–6000 (35); >6000 (50) | >684 |
| Hypertriglyceridaemia, mmol | ≥3 | <1·5 (0); 1·5–4 (44); >4 (64) | >1·76 |
| Hypofibrinogenaemia, g/L | ≤1·5 | >2·5 (0); <2·5 (30) | ≤3·6 |
| Liver function tests, IU/L | Not included | AST<30 (0); >30 (19) | AST>48 |
| Low or absent natural killer cell activity | Present | Not included | Not included |
| Soluble CD25, U/mL | ≥2400 | Not included | Not included |
| Tissue | |||
| Haemophagocytosis | Present | No (0), yes (35) | Present |
| Fulfilment of criteria | |||
| Interpretation | Molecular diagnosis consistent with fHLH or ≥5 of 8 criteria | Produces a probability outcome; scores >169 are 93% sensitive and 86% specific for HLH | Febrile patient with known or suspected sJIA, ferritin >684 ng/mL and ≥2 additional items |
In adults, the diagnostic criteria are often only strictly fulfilled in the advanced stages when initiating treatment might already be futile. Withholding potentially life-saving treatment until criteria are met could result in a missed window of opportunity before a patient tips into an accelerated, unsalvageable state. A better approach to identify the spectrum of cytokine storm syndromes early is to be hypervigilant in sick patients with unexplained fever and cytopenias, especially in those at risk (eg, with underlying rheumatic disease), by monitoring trends (rather than absolute values) in laboratory parameters (eg, decreasing platelet counts or erythrocyte sedimentation rate, and increasing ferritin levels).
The benefits of potentially life-saving treatments must be balanced against potential risks of immunosuppression. There are validated protocols for treating cytokine storm syndromes secondary to familial HLH26 or CAR T-cell therapy;33 however, there is a distinct absence of validated treatment protocols or randomised controlled trials of sHLH treatment in adults. Recently published management algorithms in adults with sHLH2, 3 are based on consensus expert opinion and clinical experience, largely extrapolated from the paediatric literature. Cytokine storm syndromes require an individualised management approach with cross-specialty input, including from rheumatology, haematology, infectious diseases, and critical care, especially since the intensive immunosuppressive regimens required often appear counterintuitive in critically ill patients with putative infection and apparent sepsis. Contemporaneous access to experts in hyperinflammation outside of formal meetings is vital, as urgent action is required to successfully treat these patients. A suggested framework for management is proposed in the figure , with concurrent strategies to inhibit the cytokine storm using immunosuppression (including selective blockade of pivotal cytokines, steroids, or chemotherapy with etoposide), treat the underlying driver of inflammation (eg, chemotherapy for malignancy), and prevent or treat complications.
Figure.
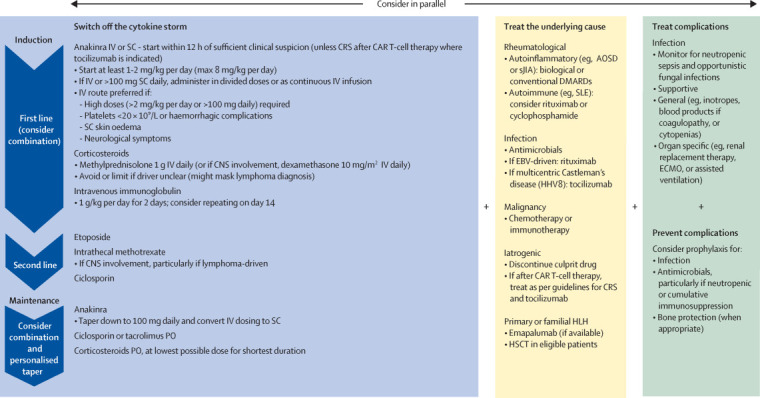
Suggested management framework for cytokine storm syndromes
A cross-specialty management approach for cytokine storm syndromes is proposed. This includes switching off the cytokine storm, treating the underlying cause, and treating and preventing complications. To target the cytokine storm, immunosuppressants (often in combination) are used in an induction-maintenance treatment paradigm. Notably, higher doses of anakinra are often required in paediatric practice. Second-line therapies are added if inflammation is not controlled. A personalised approach for tapering (withdrawal) of therapy is recommended when inflammation is controlled. The figure illustrates the positioning of anakinra in a management framework for HLH and is not intended as a definitive treatment guideline for cytokine storm syndromes, and the various underlying drivers. AOSD=adult-onset Still's disease. CAR=chimeric antigen receptor. CRS=cytokine release syndrome. DMARDs=disease modifying anti-rheumatic drugs. EBV=Epstein-Barr virus. ECMO=extracorporeal membrane oxygenation. HHV8=human herpesvirus 8. HLH=haemophagocytic lymphohistiocytosis. HSCT=haematopoietic stem cell transplant. IV=intravenous. PO=oral administration. SC=subcutaneous. sJIA=systemic juvenile idiopathic arthritis. SLE=systemic lupus erythematosus.
An induction-maintenance treatment paradigm aims to rapidly terminate the hypercytokinaemia and hyperinflammation with induction therapies, followed by maintenance therapy to control inflammation and prevent relapse. Maintenance treatment can then be gradually withdrawn (tapered) after a period of stability. In patients with an underlying malignancy, definitive treatment of the cancer should abrogate the need for long-term immunosuppression. In patients with an underlying rheumatological disease, long-term (occasionally life-long) immunosuppression might be required. Treatment should be started as soon as there is sufficient clinical suspicion of a cytokine storm syndrome, ideally within 12 h, although evidence is limited to guide optimal timeframes for initiation, escalation, or withdrawal of treatment. Formal response and withdrawal criteria have not yet been defined, and management should be personalised for each patient. Abrupt discontinuation of treatment could result in rebound inflammation.
IL-1 is central to the cytokine storm syndrome in patients with HLH. Anakinra is generally considered to be effective, safe, well tolerated, inexpensive and to have a compelling benefit:risk profile for first-line use in patients with sHLH.4, 34, 35 Use of corticosteroids in patients with sHLH could mask an underlying lymphoma; thus, if a trigger is not identified, anakinra monotherapy (or in combination with other drugs) might allow for avoidance of steroids35 until tissue biopsies (eg, lymph nodes) have been obtained. However, a steroid-free regimen is exceptionally difficult to achieve in patients with severe cytokine storm syndromes.
Anakinra has established efficacy in patients with systemic juvenile idiopathic arthritis and the associated MAS36, 37, 38, 39 and might also improve survival in patients with MAS associated with other rheumatic disorders,40 including systemic lupus erythematosus.38 A retrospective review of 44 paediatric patients (aged 10 years; range 1–19) with sHLH with various underlying causes showed that earlier initiation of anakinra (within 5 days of hospital admission) was associated with reduced mortality, especially in non-malignancy-associated HLH.41 Anakinra was associated with a better outcome in patients with underlying rheumatic disease, with 100% survival in patients with MAS associated with systemic juvenile idiopathic arthritis.41 Overall survival of paediatric patients treated with anakinra in that study was higher (73% [32 of 44] survival)41 compared with etoposide-based protocols in a report of patients with primary and sHLH (56% [63 of 113]) survival, among whom 78% [88 of 113] had sHLH).26 Anakinra has a favourable non-myelosuppressive safety profile4 compared with other available treatments for cytokine storm syndromes, for example etoposide (chemotherapy), tocilizumab (US Food and Drug Administration [FDA] approved for cytokine release syndrome after CAR T-cell therapy),42 and other therapies in development for HLH, such as Janus kinase (JAK) inhibitors (eg, ruxolitinib).43 Notably, there is emerging evidence that IL-1 blockade might also have some efficacy in cytokine release syndrome after CAR T-cell therapy,44, 45 although randomised controlled trials are pending.
When treating sHLH in the context of infections (eg, coronavirus disease 2019 [COVID-19]),46 anakinra could be preferable to tocilizumab from a safety perspective, as anakinra is likely to be less myelosuppressive and hepatotoxic, has a shorter half-life (and therefore faster wash-out if discontinued), and does not mask indicators of infection (eg, IL-6 blockade might suppress C-reactive protein and fever as a mechanistic effect). The potential efficacy of JAK inhibitors (along with their associated advantages of oral formulation and short half-life), might be offset by safety concerns around potentially deleterious effects of simultaneous (versus selective) blockade of multiple cytokines.
Notably, serum IL-1β is not a reliable biomarker of disease activity nor is it useful for predicting treatment response. IL-1β levels might be in the normal range in patients with active sHLH (although might be elevated at local sites of inflammation) and often do not correlate with outcomes following treatment with anakinra. Serum IL-1β levels might be technically difficult to measure due to assay variability and might not be comparable between laboratories.
Other first-line treatments for cytokine storm syndromes include steroids and intravenous immunoglobulin. Intravenous immunoglobulin might need to be repeated after 14 days due to its half-life of 14–21 days. With regard to steroids, rheumatologists usually elect for pulsed intravenous methylprednisolone, but dexamethasone is preferred if there is neurological involvement. Second-line therapies for refractory cytokine storm syndromes include etoposide and intrathecal methotrexate, which are usually prescribed by haematologists. Etoposide requires dose-adjustment if there is renal dysfunction, liver impairment, or previous or current neutropenia. Intravenous ciclosporin, if given at induction, is usually swapped for the oral formulation for maintenance.
Specific treatments are indicated for particular underlying causes of cytokine storm syndrome. Tocilizumab is licensed for cytokine release syndrome after CAR T-cell therapy33, 42 and is also used for multi centric Castleman's disease.47 Adjunctive B-cell depletion with rituximab (anti-CD20 monoclonal antibody [mAb]) has been shown to reduce viral load and serum ferritin levels, and to improve overall clinical outcomes in patients with Epstein-Barr virus-driven HLH.48 Chemotherapy and etoposide-based protocols are more commonly used for cytokine storm syndromes associated with lymphoproliferative disorders, where the prognosis is usually very poor. Emapalumab (anti-IFNγ mAb) was approved by the US FDA in November, 2018, for familial HLH;49 however, this drug is not licenced for use in adults. Identification of genetic mutations characteristic of familial HLH facilitate eligibility for haematopoietic stem cell transplantation, which might be curative.
Intravenous anakinra in cytokine storm syndromes
Subcutaneous anakinra, 100 mg once daily, is licenced for rheumatoid arthritis, systematic juvenile idiopathic arthritis, adult-onset Still's disease, and cryopyrin-associated periodic syndromes. Anakinra is recommended off-licence for management of sHLH/MAS, starting with at least 1–2 mg/kg per day, increasing to a maximum of 8 mg/kg per day3 (paediatric doses are often higher). Notably, refractory cases of sHLH/MAS have been reported to require 100 mg anakinra four times per day;50 as such, some clinicians choose to start at higher doses and down titrate the dose when the inflammation is controlled. Anakinra is also used intravenously in clinical practice for patients with cytokine storm syndromes, and the intravenous route was endorsed in a recent multidisciplinary consensus guideline,4 despite limited rationale and supportive evidence. It is unclear when or why the practice of intravenous administration of anakinra first started; its use might have originated from a desire to achieve a rapid onset of action in critically unwell patients with high mortality, limited treatment options, and purported poor peripheral absorption. Safety data from clinical trials of intravenous anakinra (24–48 mg/kg per day) in sepsis might have provided reassurance for its wider use in patients with cytokine storm syndromes, in whom secondary infections are almost universal, although the maximal treatment duration in these sepsis trials was only 72 hours.51 Long-term safety data for anakinra is reassuring in rheumatoid arthritis (3 years)52, 53 and cryopyrin-associated periodic syndromes (5 years);54 steroids and comorbidities could increase the risk of infections.53
The true frequency of intravenous anakinra use, compared with subcutaneous delivery, for patients with cytokine storm syndromes in current clinical practice is unknown; however, from our own experience in three international tertiary referral centres for cytokine storm syndromes, a substantial number of patients receive intravenous dosing. Among patients who received anakinra in hospital between January, 2019, and December, 2019, the intravenous route was used in 33% (10 of 30 children; aged between 15 months and 18 years) treated at the Children's of Alabama Hospital (AL, USA); in 67% (6 of 9) of adults treated at the University College London Hospital (UK); and in 29% (2 of 7) of adults treated at the Sheffield Teaching Hospital NHS Foundation Trust (UK). In total, the intravenous route was used in 39% (18 of 46) of patients who received anakinra in hospital for cytokine storm syndromes in our three centres over 12 months. Additionally, we are contacted regularly (approximately 1–4 times per month across sites) by physicians in the USA and UK, requesting remote management advice for sick patients with cytokine storm syndromes.
Pharmacokinetic analysis of intravenous anakinra
Anakinra is a large polypeptide (17 kDa) with a small initial volume of distribution. The absolute bioavailability of anakinra after a 70 mg subcutaneous injection in healthy individuals is 95%55 according to the summary of product characteristics; bioavailability was recently reported as between 80% and 92%,56 independent of body weight and body-mass index (BMI). Anakinra exhibits flip-flop kinetics after subcutaneous administration; the absorption process represents the terminal phase of the concentration-time profile because subcutaneous absorption is rate limiting in the disposition. Studies have shown a similar area under the curve (reflecting exposure to the drug after administration) for a single dose of anakinra using both subcutaneous (100 mg) and intravenous (1 mg/kg) bolus injections in healthy volunteers (table 2 ).57
Table 2.
Pharmacokinetic comparison of single dose intravenous and subcutaneous anakinra in healthy volunteers*
| Intravenous (100 mg)† | Subcutaneous (100 mg)† | |
|---|---|---|
| Healthy volunteers | 7 | 8 |
| Cmax (ng/mL) | 32 193 | 1326 |
| Tmax (h) | Not applicable | 4·3 |
| t1/2(h) | 1·69 | 3·63 |
| AUC (ng*hour/mL) | 14 658 | 13 266 |
| CL (mL/min) | 122 | 134 |
Data are presented as mean values. Cmax= maximum plasma concentration. Tmax=time at which Cmax occurred. t1/2=terminal half-life. AUC=area under plasma concentration-time curve from time 0 to infinity. CL=plasma clearance.
Adapted from Yang and et al.56
These data represent volunteers with a body-mass index <35 and a body weight ≤90 kg.
The terminal half-life of ankinra is longer when delivered subcutaneously (5·24 h) than intravenously (2·64 h), with similar clearance, indicating that absorption is slower than elimination.56, 57 After subcutaneous administration, the half-life increases significantly (3·63–7·62 h; p<0·05) with both body weight and BMI,56 suggesting that the absorption rate constant decreases as these variables increase. The drug has longer half-lives in more obese individuals, suggesting that those with greater adipose tissue have slower anakinra transport and consequently less rapid systemic subcutaneous absorption.56 The maximum plasma concentration (Cmax) of anakinra is higher with intravenous dosing compared with subcutaneous dosing (24–29 times higher).56, 57 Furthermore, the time to achieve maximum plasma concentration (Tmax) after subcutaneous injection ranged from 3·7 h to 4·3 h56 in healthy volunteers (3–7 hours in patients with rheumatoid arthritis).55 Taken together these findings suggest that intravenous dosing of anakinra enables a higher and faster maximal plasma concentration (ie, higher Cmax and shorter Tmax) to be achieved, compared with subcutaneous delivery. To our knowledge, pharmacokinetic studies have not been done in patients with subcutaneous oedema, but given the influence of adiposity on the absorption rate of subcutaneous anakinra, it is plausible that intraveous dosing might be preferable in patients with peripheral oedema and anasarca. If administered intravenously, as per convention for other biologics, anakinra should be used in a dedicated line.58
Anakinra can cross the blood brain barrier when given intravenously, despite being a large protein with very low (4%) penetration into cerebrospinal fluid.58, 59 Subcutaneous delivery of anakinra is neuroprotective in rats, although very high doses are required.60 It could be inferred that intravenous administration of anakinra could be favoured in patients with cytokine storm syndromes and neurological manifestations. Clearance of anakinra is directly related to renal function.57
Dose adjustment is not recommended for subcutaneous administration in patients with mild-to-moderate renal impairment,55 but dose reduction is warranted if there is moderate–severe renal impairment or if haemofiltration is required, as anakinra is only minimally removed by dialysis.57 Therefore, there might be a risk of anakinra accumulation and toxicity in critically ill patients with cytokine storm syndromes receiving renal replacement therapy; strategies employed in clinical practice to overcome this include administering intravenous anakinra after dialysis sessions and avoiding continuous intravenous infusions.
Existing evidence for intravenous anakinra in cytokine storm syndromes
Most publications on cytokine storm syndromes describe subcutaneous use of anakinra; however, intravenous dosing has been reported in eight patients (table 3 , appendix pp 1–3) with equal gender distribution and a mean age of 22 years (range 22 months to 71 years).41, 61, 62, 63, 64, 65, 66 The reported underlying driver of cytokine storm in these patients included autoimmune or autoinflammatory diseases in three patients (one each with adult-onset Still's disease, systemic juvenile idiopathic arthritis, and systemic lupus erythematosus). Underlying infection was diagnosed in three patients (one each with cytomegalovirus, septic arthritis, and human herpesvirus 8); one patient had both underlying autoimmunity (vasculitis) and infection (cytomegalovirus); and another had underlying haematological disease (myelodysplastic syndrome). Anakinra was used intravenously at induction in all patients and was converted to subcutaneous maintenance in four of six survivors. Seven of eight patients also received corticosteroids. One patient (4-year-old female) with systemic juvenile idiopathic arthritis was treated with a combination of anakinra and abatacept (CTLA4-Ig) therapy. There were three deaths associated with multi-organ failure, of which two were associated with fungemia. No adverse events were directly attributed to anakinra. The length of follow up was documented in three patients, ranging between 2 months and 2 years.
Table 3.
Reported cases of cytokine storm syndrome (including sHLH/MAS) treated with intravenous anakinra
| Patient details | Underlying diagnosis | IV anakinra | Other acute management | Maintenance | Length of follow-up (months) | |
|---|---|---|---|---|---|---|
| Chou et al (2010)61 | 36-year-old female | MDS | Details not specified | Corticosteroids 1 mg/kg per day | Anakinra (assumed SC); prednisolone 40 mg/day | 2 |
| Nigrovic et al (2011);62 Record et al (2011)63 | 4-year-old female | sJIA, diagnosed at 8 months of age | 11·2 mg/kg per day (5·6 mg/kg twice a day); duration unspecified | Corticosteroids 1·1 mg/kg per day; MTX; 0·8 mg/kg per week | Anakinra 0·9 mg/kg per day (assumed SC); steroids 0·9 mg/kg per day; MTX 0·7 mg/kg per week; abatacept IV 0·3mg/kg per 3 weeks | 24 |
| Loh et al (2012)64 | 20-year-old male | AOSD | 200 mg once daily for 6 days | Methylprednisolone; IV hydrocortisone; CSA 100 mg twice daily | Anakinra 100 mg SC; once-daily; MTX 10 mg once-weekly | Unknown |
| Acker et al (2015)65 | 22-month-old male | Septic arthritis | Details not specified | Prednisolone oral | Anakinra (assumed SC) | 24 |
| Kemps et al (2017)66 | 71-year-old male | CMV and AAV | 400 mg every 3 days for 10 days | Not specified | Not specified | Unknown |
| Eloseily et al (2020)41 | 19-year-old female | SLE | 48 mg/kg per day for 3 days | Not specified | Not applicable | Died |
| Eloseily et al (2020)41 | 8-year-old male | HHV-6 | 8–48 mg/kg per day for 1 month | Etoposide; dexamethasone; solumedrol; CSA 4 mg/kg per day | Not applicable | Died |
| Eloseily et al (2020)41 | 16-year-old female | Gastroparesis and CMV | 4–48 mg/kg per day for 3 months | Methylprednisolone; CSA 4 mg/kg per day; abatacept; tocilizumab | Not applicable | Died |
MDS=myelodysplastic syndrome. SC=subcutaneous. sJIA=systemic juvenile idiopathic arthritis. MTX=methotrexate. AOSD=adult-onset Still's disease. IV=intravenous. CSA=ciclosporin. CMV=cytomegalovirus. AAV=ANCA-associated vasculitis. SLE=systemic lupus erythematosus. HHV-6=human herpes virus-6.
Safety of intravenous anakinra in other indications
In a phase 3 randomised, double-blind trial67 of 893 patients with sepsis comparing anakinra (1 or 2 mg/kg per h) with placebo, anakinra failed to meet the primary endpoint of improved 28-day survival but resulted in improved survival in a subset of patients with poor prognosis (n=563; p=0·009). Based on these results, a confirmatory phase 3 trial was done in 696 patients with severe sepsis comparing intravenous anakinra (100 mg bolus followed by a 72 h continuous infusion at 2 mg/kg per h; n=350) and placebo (n=346).68 Safety data for the anakinra and placebo groups were comparable. This study68 was discontinued following an interim analysis, in which no survival benefit of anakinra could be shown. In a retrospective review 20 years after the original phase 3 trial67 was completed, 43 (5·6%) of 763 patients with available data could be classified as having hyperinflammation at enrolment, based on deranged liver function and coagulopathy as proxy markers. 26 (60%) of these patients received intravenous anakinra and 17 (40%) received placebo, with a 28-day mortality of 35% and 65%, respectively (p=0·0006).69 These post-hoc results suggest that a subgroup of patients with sepsis and inflammation (macrophage activation-like syndrome) might respond to anakinra and potentially other immunotherapy drugs. The PROVIDE trial (NCT03332225) is a double-blind randomised trial of personalised immunotherapy in sepsis, in which patients were randomly assigned to receive either 200 mg of intravenous anakinra three times daily, subcutaneous recombinant human IFNγ (rhIFNγ), or placebo for 7 days, based on a panel of biomarkers and laboratory tests to identify a hyperinflammatory profile (treated with anakinra) or hypoinflammatory profiles (treated with rhIFNγ). Although clinical trials of anakinra in sepsis have so far shown equivocal efficacy, they have not raised any safety concerns in the anakinra groups. The results of the PROVIDE trial are awaited.
Anakinra was given by a continuous intravenous infusion (400–3200 mg/day) for 7 days to 17 patients with steroid-resistant acute graft-versus-host disease.70 No safety signals were reported except for a reversible rise of liver transaminases seen in two (12%) patients. In two studies of patients with subarachnoid haemorrhage,67, 71 intravenous anakinra was given as a 500 mg bolus followed by a 10 mg/kg per h infusion for 24 h (six patients)71 or a 100 mg bolus followed by a 2 mg/kg per h infusion for 24 hours (eight patients).59 No adverse or serious adverse events attributed to anakinra were reported. In a randomised phase 2 study,72 34 patients with acute stroke were randomly assigned to anakinra (100 mg intravenous loading bolus, followed by a 2 mg/kg per h infusion over 72 h) or placebo. No adverse events were attributed to anakinra.
Indications for intravenous anakinra in cytokine storm syndromes
The subcutaneous (licenced) route of anakinra is recommended in guidelines based on consensus expert-opinion for sHLH-like cytokine storm syndromes. However, in a subgroup of patients, treated in our tertiary care centres and elsewhere, intravenous dosing is already in use for induction, with or without subcutaneous maintenance thereafter. We suggest starting anakinra within 12 h of sufficient clinical suspicion, and therefore prefilled syringes of anakinra should be stocked and locally available for emergency, out-of-hours access. As described in this Viewpoint, intravenous dosing of anakinra achieves a higher and faster maximal plasma concentration (higher Cmax and shorter Tmax), compared with subcutaneous delivery. The intravenous route is usually preferred if high doses (>2 mg/kg per day or >100 mg/day) are required (eg, to avoid pain from multiple daily injections); hence induction doses are often given by the intravenous route in critically ill patients, in whom higher starting doses are often required. Furthermore the intravenous route might be preferred if subcutaneous administration is relatively contraindicated, for example severe thrombocytopenia (platelets <20 × 109/L), haemorrhagic complications, subcutaneous skin oedema (that could impede absorption, similar to the effects of adiposity),56 or if there are neurological symptoms. If there are substantial concerns regarding infection, the intravenous route could be favoured because of the shorter half-life of the drug compared with subcutaneous dosing, potentially allowing for faster wash-out after drug discontinuation.
The optimal dosing regimen for intravenous anakinra in patients with cytokine storm syndrome is unclear. Reported regimens include intravenous loading boluses to supplement continuous intravenous infusions58, 59, 68, 71, 72 or subcutaneous injections (eg, in ulcerative colitis ISRCTN43717130).73 Use of an intravenous loading bolus or a continuous intravenous infusion could enable steady state plasma concentrations to be rapidly attained and maintained, avoiding potentially subtherapeutic troughs.58, 59, 73 Given the shorter half-life of intravenous anakinra (relative to subcutaneous delivery), we suggest administration using split dosing (eg, twice daily intravenous boluses) or a continuous infusion.
Conclusions and future directions
Cytokine storm syndromes can rapidly lead to critical illness and death if not promptly treated, and anakinra is increasingly recognised as an important treatment. Evidence is accumulating to support the safety of intravenous anakinra, which is preferable to the licenced subcutaneous route in critically unwell patients; the small number of published cases of intravenous anakinra in patients with cytokine storm syndromes is undoubtedly a marked under-representation of real world use, and it is imperative that clinical experience and outcomes are shared. Anakinra is a key drug used in the first-line management of patients with cytokine storm syndromes, and as such there are ongoing national initiatives in the UK to improve early access to this potentially life-saving treatment, similar to the existing comissioning policies for anakinra in patients with systemic juvenile idiopathic arthritis-associated MAS74 and adult-onset Still's disease.75
A systematic approach is needed to optimise recognition, diagnosis, and management of cytokine storm syndromes, acknowledging that there are likely to be different triggers of hyperinflammation in individual patients. Cross-specialty collaborative working models are increasingly being used in both adult and paediatric settings.4 In the UK, the national HLH across-speciality collaboration working group, endorsed by the Histio UK patient group, was established to improve clinical, educational, and academic outcomes and has supported the development of a national UK HLH registry and bioresource.
Although there has been progress in understanding the mechanistic basis for the initation and propogation of cytokine storm syndromes, there remains a considerable unmet need for effective therapies, better understanding of the aetiopathogenesis, and identification of biomarkers to predict treatment response and prognosis, to enable a stratified and ultimately precision medicine treatment approach.76, 77 Prospective research and comprehensive data capture, with deep phenotyping and biobanking, is crucial. The heterogenity and perceived rarity of cytokine storm syndromes, coupled with a reticence to conduct clinical trials in critically ill patients, has hampered the development of novel therapies. However, the optics are changing and momentum is building, with the recent US FDA approval of the anti-IFNγ mAb emapalumab for familial HLH,49 and an open-labelled pilot trial of ruxolitinib in patients with sHLH.43
There is a pressing need to improve prognosis for patients with cytokine storm syndromes. This requires increased awareness and recognition of cytokine storm syndromes, with cross-specialty collaboration, international multi-centre registries, and controlled trials that will facilitate the generation of evidence-based, validated guidelines to improve the prognosis of patients with cytokine storm syndromes. Rheumatologists are well placed to lead and coordinate this continued effort.
Search strategy and selection criteria
We searched PubMed for articles published in English from Jan 1, 2000, to Feb 1, 2020, using the search terms “HLH”, “haemophagocytic lymphohistiocytosis”, “macrophage activation syndrome”, “cytokine release syndrome”, and “intravenous anakinra”.
Contributors
PM, JJM, and RST drafted the manuscript. JJM, RST, and RQC provided clinical data. JH reviewed the pharmacokinetic section. All authors contributed to discussions and approved the manuscript.
Declaration of interests
PM is a Medical Research Council GlaxoSmithKline experimental medicine initiative to explore new therapies clinical training fellow and receives project funding, outside the submitted work. PM receives co-funding by the National Institute for Health Research University College London Hospitals Biomedical Research Centre. RQC is co-principal investigator of an investigator initiated clinical trial funded by Swedish Orphan Biovitrum (SOBI), is on the advisory board for SOBI (<US$5000), and is on the clinical trial adjudication committee for Pfizer. RST is a member of the UK systemic autoinflammatory disease network, whose meetings are funded by an unrestricted educational grant from SOBI. JH and JJM declare no competing interests.
Supplementary Material
References
- 1.Ramos-Casals M, Brito-Zerón P, López-Guillermo A, Khamashta MA, Bosch X. Adult haemophagocytic syndrome. Lancet. 2014;383:1503–1516. doi: 10.1016/S0140-6736(13)61048-X. [DOI] [PubMed] [Google Scholar]
- 2.La Rosée P, Horne A, Hines M. Recommendations for the management of hemophagocytic lymphohistiocytosis in adults. Blood. 2019;133:2465–2477. doi: 10.1182/blood.2018894618. [DOI] [PubMed] [Google Scholar]
- 3.Carter SJ, Tattersall RS, Ramanan AV. Macrophage activation syndrome in adults: recent advances in pathophysiology, diagnosis and treatment. Rheumatology (Oxford) 2019;58:5–17. doi: 10.1093/rheumatology/key006. [DOI] [PubMed] [Google Scholar]
- 4.Halyabar O, Chang MH, Schoettler ML. Calm in the midst of cytokine storm: a collaborative approach to the diagnosis and treatment of hemophagocytic lymphohistiocytosis and macrophage activation syndrome. Pediatr Rheumatol Online J. 2019;17:7. doi: 10.1186/s12969-019-0309-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kumar B, Aleem S, Saleh H, Petts J, Ballas ZK. A personalized diagnostic and treatment approach for macrophage activation syndrome and secondary hemophagocytic lymphohistiocytosis in adults. J Clin Immunol. 2017;37:638–643. doi: 10.1007/s10875-017-0439-x. [DOI] [PubMed] [Google Scholar]
- 6.Risma K, Jordan MB. Hemophagocytic lymphohistiocytosis: updates and evolving concepts. Curr Opin Pediatr. 2012;24:9–15. doi: 10.1097/MOP.0b013e32834ec9c1. [DOI] [PubMed] [Google Scholar]
- 7.Karakike E, Giamarellos-Bourboulis EJ. Macrophage activation-like syndrome: a distinct entity leading to early death in sepsis. Front Immunol. 2019;10:55. doi: 10.3389/fimmu.2019.00055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Titov A, Petukhov A, Staliarova A. The biological basis and clinical symptoms of CAR-T therapy-associated toxicites. Cell Death Dis. 2018;9:897. doi: 10.1038/s41419-018-0918-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Minoia F, Davì S, Horne A. Dissecting the heterogeneity of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. J Rheumatol. 2015;42:994–1001. doi: 10.3899/jrheum.141261. [DOI] [PubMed] [Google Scholar]
- 10.Ravelli A, Minoia F, Davì S. 2016 classification criteria for macrophage activation syndrome complicating systemic juvenile idiopathic arthritis: a European league against rheumatism/american college of rheumatology/paediatric rheumatology international trials organisation collaborative initiative. Arthritis Rheumatol. 2016;68:566–576. doi: 10.1002/art.39332. [DOI] [PubMed] [Google Scholar]
- 11.Hot A, Toh ML, Coppéré B. Reactive hemophagocytic syndrome in adult-onset Still disease: clinical features and long-term outcome: a case-control study of 8 patients. Medicine (Baltimore) 2010;89:37–46. doi: 10.1097/MD.0b013e3181caf100. [DOI] [PubMed] [Google Scholar]
- 12.Dhote R, Simon J, Papo T. Reactive hemophagocytic syndrome in adult systemic disease: report of twenty-six cases and literature review. Arthritis Rheum. 2003;49:633–639. doi: 10.1002/art.11368. [DOI] [PubMed] [Google Scholar]
- 13.Fukaya S, Yasuda S, Hashimoto T. Clinical features of haemophagocytic syndrome in patients with systemic autoimmune diseases: analysis of 30 cases. Rheumatology (Oxford) 2008;47:1686–1691. doi: 10.1093/rheumatology/ken342. [DOI] [PubMed] [Google Scholar]
- 14.Jamilloux Y, Gerfaud-Valentin M, Martinon F, Belot A, Henry T, Sève P. Pathogenesis of adult-onset Still's disease: new insights from the juvenile counterpart. Immunol Res. 2015;61:53–62. doi: 10.1007/s12026-014-8561-9. [DOI] [PubMed] [Google Scholar]
- 15.Nirmala N, Brachat A, Feist E. Gene-expression analysis of adult-onset Still's disease and systemic juvenile idiopathic arthritis is consistent with a continuum of a single disease entity. Pediatr Rheumatol Online J. 2015;13:50. doi: 10.1186/s12969-015-0047-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Minoia F, Davì S, Horne A. Clinical features, treatment, and outcome of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis: a multinational, multicenter study of 362 patients. Arthritis Rheumatol. 2014;66:3160–3169. doi: 10.1002/art.38802. [DOI] [PubMed] [Google Scholar]
- 17.Tsuji T, Ohno S, Ishigatsubo Y. Liver manifestations in systemic lupus erythematosus: high incidence of hemophagocytic syndrome. J Rheumatol. 2002;29:1576–1577. [PubMed] [Google Scholar]
- 18.Zhou WJ, Yang CD. The causes and clinical significance of fever in systemic lupus erythematosus: a retrospective study of 487 hospitalised patients. Lupus. 2009;18:807–812. doi: 10.1177/0961203309103870. [DOI] [PubMed] [Google Scholar]
- 19.Kim JM, Kwok SK, Ju JH, Kim HY, Park SH. Reactive hemophagocytic syndrome in adult Korean patients with systemic lupus erythematosus: a case-control study and literature review. J Rheumatol. 2012;39:86–93. doi: 10.3899/jrheum.110639. [DOI] [PubMed] [Google Scholar]
- 20.Lorenz F, Klimkowska M, Pawłowicz E, Brustad AB, Erlanson M, Machaczka M. Clinical characteristics, therapy response, and outcome of 51 adult patients with hematological malignancy-associated hemophagocytic lymphohistiocytosis: a single institution experience. Leuk Lymphoma. 2018;59:1840–1850. doi: 10.1080/10428194.2017.1403018. [DOI] [PubMed] [Google Scholar]
- 21.Schram AM, Comstock P, Campo M. Haemophagocytic lymphohistiocytosis in adults: a multicentre case series over 7 years. Br J Haematol. 2016;172:412–419. doi: 10.1111/bjh.13837. [DOI] [PubMed] [Google Scholar]
- 22.Ravelli A, Minoia F, Davì S. Expert consensus on dynamics of laboratory tests for diagnosis of macrophage activation syndrome complicating systemic juvenile idiopathic arthritis. RMD Open. 2016;2 doi: 10.1136/rmdopen-2015-000161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zeng HS, Xiong XY, Wei YD, Wang HW, Luo XP. Macrophage activation syndrome in 13 children with systemic-onset juvenile idiopathic arthritis. World J Pediatr. 2008;4:97–101. doi: 10.1007/s12519-008-0018-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schulert GS, Zhang M, Fall N. Whole-exome sequencing reveals mutations in genes linked to hemophagocytic lymphohistiocytosis and macrophage activation syndrome in fatal cases of H1N1 influenza. J Infect Dis. 2016;213:1180–1188. doi: 10.1093/infdis/jiv550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Crayne CB, Albeituni S, Nichols KE, Cron RQ. The immunology of macrophage activation syndrome. Front Immunol. 2019;10:119. doi: 10.3389/fimmu.2019.00119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Henter J-I, Samuelsson-Horne AC, Arico M. Treatment ofhemophagocytic lymphohistiocytosis with HLH-94 immuno-chemotherapy and bone marrow transplantation. Blood. 2002;100:2367–2373. doi: 10.1182/blood-2002-01-0172. [DOI] [PubMed] [Google Scholar]
- 27.Fardet L, Galicier L, Lambotte O. Development and validation of the HScore, a score for the diagnosis of reactive hemophagocytic syndrome. Arthritis Rheumatol. 2014;66:2613–2620. doi: 10.1002/art.38690. [DOI] [PubMed] [Google Scholar]
- 28.Debaugnies F, Mahadeb B, Ferster A. Performances of the H-Score for diagnosis of hemophagocytic lymphohistiocytosis in adult and pediatric patients. Am J Clin Pathol. 2016;145:862–870. doi: 10.1093/ajcp/aqw076. [DOI] [PubMed] [Google Scholar]
- 29.Allen CE, Yu X, Kozinetz CA, McClain KL. Highly elevated ferritin levels and the diagnosis of hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2008;50:1227–1235. doi: 10.1002/pbc.21423. [DOI] [PubMed] [Google Scholar]
- 30.Lin TF, Ferlic-Stark LL, Allen CE, Kozinetz CA, McClain KL. Rate of decline of ferritin in patients with hemophagocytic lymphohistiocytosis as a prognostic variable for mortality. Pediatr Blood Cancer. 2011;56:154–155. doi: 10.1002/pbc.22774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sackett K, Cunderlik M, Sahni N, Killeen AA, Olson AP. Extreme hyperferritinemia: causes and impact on diagnostic reasoning. Am J Clin Pathol. 2016;145:646–650. doi: 10.1093/ajcp/aqw053. [DOI] [PubMed] [Google Scholar]
- 32.Schram AM, Campigotto F, Mullally A. Marked hyperferritinemia does not predict for HLH in the adult population. Blood. 2015;125:1548–1552. doi: 10.1182/blood-2014-10-602607. [DOI] [PubMed] [Google Scholar]
- 33.Chen H, Wang F, Zhang P. Management of cytokine release syndrome related to CAR-T cell therapy. Front Med. 2019;13:610–617. doi: 10.1007/s11684-019-0714-8. [DOI] [PubMed] [Google Scholar]
- 34.Rajasekaran S, Kruse K, Kovey K. Therapeutic role of anakinra, an interleukin-1 receptor antagonist, in the management of secondary hemophagocytic lymphohistiocytosis/sepsis/multiple organ dysfunction/macrophage activating syndrome in critically ill children*. Pediatr Crit Care Med. 2014;15:401–408. doi: 10.1097/PCC.0000000000000078. [DOI] [PubMed] [Google Scholar]
- 35.Bauchmuller K, Manson JJ, Tattersall R. Haemophagocytic lymphohistiocytosis in adult critical care. J Intensive Care Soc. 2020 doi: 10.1177/1751143719893865. published online Jan 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ravelli A, Grom AA, Behrens EM, Cron RQ. Macrophage activation syndrome as part of systemic juvenile idiopathic arthritis: diagnosis, genetics, pathophysiology and treatment. Genes Immun. 2012;13:289–298. doi: 10.1038/gene.2012.3. [DOI] [PubMed] [Google Scholar]
- 37.Sönmez HE, Demir S, Bilginer Y, Özen S. Anakinra treatment in macrophage activation syndrome: a single center experience and systemic review of literature. Clin Rheumatol. 2018;37:3329–3335. doi: 10.1007/s10067-018-4095-1. [DOI] [PubMed] [Google Scholar]
- 38.Aytaç S, Batu ED, Ünal Ş. Macrophage activation syndrome in children with systemic juvenile idiopathic arthritis and systemic lupus erythematosus. Rheumatol Int. 2016;36:1421–1429. doi: 10.1007/s00296-016-3545-9. [DOI] [PubMed] [Google Scholar]
- 39.Barut K, Yücel G, Sinoplu AB, Şahin S, Adroviç A, Kasapçopur Ö. Evaluation of macrophage activation syndrome associated with systemic juvenile idiopathic arthritis: single center experience over a one-year period. Turk Pediatr Ars. 2015;50:206–210. doi: 10.5152/TurkPediatriArs.2015.3299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Miettunen PM, Narendran A, Jayanthan A, Behrens EM, Cron RQ. Successful treatment of severe paediatric rheumatic disease-associated macrophage activation syndrome with interleukin-1 inhibition following conventional immunosuppressive therapy: case series with 12 patients. Rheumatology (Oxford) 2011;50:417–419. doi: 10.1093/rheumatology/keq218. [DOI] [PubMed] [Google Scholar]
- 41.Eloseily EM, Weiser P, Crayne CB. Benefit of anakinra in treating pediatric secondary hemophagocytic lymphohistiocytosis. Arthritis Rheumatol. 2020;72:326–334. doi: 10.1002/art.41103. [DOI] [PubMed] [Google Scholar]
- 42.Le RQ, Li L, Yuan W. FDA approval summary: tocilizumab for treatment of chimeric antigen receptor t cell-induced severe or life-threatening cytokine release syndrome. Oncologist. 2018;23:943–947. doi: 10.1634/theoncologist.2018-0028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ahmed A, Merrill SA, Alsawah F. Ruxolitinib in adult patients with secondary haemophagocytic lymphohistiocytosis: an open-label, single-centre, pilot trial. Lancet Haematol. 2019;6:e630–e637. doi: 10.1016/S2352-3026(19)30156-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Norelli M, Camisa B, Barbiera G. Monocyte-derived IL-1 and IL-6 are differentially required for cytokine-release syndrome and neurotoxicity due to CAR T cells. Nat Med. 2018;24:739–748. doi: 10.1038/s41591-018-0036-4. [DOI] [PubMed] [Google Scholar]
- 45.Giavridis T, van der Stegen SJC, Eyquem J, Hamieh M, Piersigilli A, Sadelain M. CAR T cell-induced cytokine release syndrome is mediated by macrophages and abated by IL-1 blockade. Nat Med. 2018;24:731–738. doi: 10.1038/s41591-018-0041-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet. 2020;395:1033–1034. doi: 10.1016/S0140-6736(20)30628-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wei A, Ma H, Li Z, Zhang L, Zhang R, Wang T. Successful treatment of a child with idiopathic multicentric Castleman disease associated with hemophagocytic lymphohistiocytosis using tocilizumab. Pediatr Blood Cancer. 2019;66 doi: 10.1002/pbc.27759. [DOI] [PubMed] [Google Scholar]
- 48.Chellapandian D, Das R, Zelley K. Treatment of Epstein Barr virus-induced haemophagocytic lymphohistiocytosis with rituximab-containing chemo-immunotherapeutic regimens. Br J Haematol. 2013;162:376–382. doi: 10.1111/bjh.12386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vallurupalli M, Berliner N. Emapalumab for the treatment of relapsed/refractory hemophagocytic lymphohistiocytosis. Blood. 2019;134:1783–1786. doi: 10.1182/blood.2019002289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kahn PJ, Cron RQ. Higher-dose Anakinra is effective in a case of medically refractory macrophage activation syndrome. J Rheumatol. 2013;40:743–744. doi: 10.3899/jrheum.121098. [DOI] [PubMed] [Google Scholar]
- 51.Arlet JB, Le TH, Marinho A. Reactive haemophagocytic syndrome in adult-onset Still's disease: a report of six patients and a review of the literature. Ann Rheum Dis. 2006;65:1596–1601. doi: 10.1136/ard.2005.046904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fleischmann RM, Tesser J, Schiff MH. Safety of extended treatment with anakinra in patients with rheumatoid arthritis. Ann Rheum Dis. 2006;65:1006–1012. doi: 10.1136/ard.2005.048371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ramírez J, Cañete JD. Anakinra for the treatment of rheumatoid arthritis: a safety evaluation. Expert Opin Drug Saf. 2018;17:727–732. doi: 10.1080/14740338.2018.1486819. [DOI] [PubMed] [Google Scholar]
- 54.Kullenberg T, Löfqvist M, Leinonen M, Goldbach-Mansky R, Olivecrona H. Long-term safety profile of anakinra in patients with severe cryopyrin-associated periodic syndromes. Rheumatology (Oxford) 2016;55:1499–1506. doi: 10.1093/rheumatology/kew208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.EMC Kineret 100mg solution for injection in a pre-filled syringe. https://www.medicines.org.uk/emc/product/559/smpc
- 56.Yang BB, Gozzi P, Sullivan JT. Pharmacokinetics of anakinra in subjects of heavier vs. lighter body weights. Clin Transl Sci. 2019;12:371–378. doi: 10.1111/cts.12622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yang BB, Baughman S, Sullivan JT. Pharmacokinetics of anakinra in subjects with different levels of renal function. Clin Pharmacol Ther. 2003;74:85–94. doi: 10.1016/S0009-9236(03)00094-8. [DOI] [PubMed] [Google Scholar]
- 58.Galea J, Ogungbenro K, Hulme S. Intravenous anakinra can achieve experimentally effective concentrations in the central nervous system within a therapeutic time window: results of a dose-ranging study. J Cereb Blood Flow Metab. 2011;31:439–447. doi: 10.1038/jcbfm.2010.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Gueorguieva I, Clark SR, McMahon CJ. Pharmacokinetic modelling of interleukin-1 receptor antagonist in plasma and cerebrospinal fluid of patients following subarachnoid haemorrhage. Br J Clin Pharmacol. 2008;65:317–325. doi: 10.1111/j.1365-2125.2007.03026.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rosenzweig JM, Lei J, Burd I. Interleukin-1 receptor blockade in perinatal brain injury. Front Pediatr. 2014;2:108. doi: 10.3389/fped.2014.00108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chou RC, Dinarello CA, Ferry JA, Dal Cin P. A 36-year-old woman with recurrent high-grade fevers, hypotension, and hypertriglyceridemia. Arthritis Care Res (Hoboken) 2010;62:128–136. doi: 10.1002/acr.20024. [DOI] [PubMed] [Google Scholar]
- 62.Nigrovic PA, Mannion M, Prince FH. Anakinra as first-line disease-modifying therapy in systemic juvenile idiopathic arthritis: report of forty-six patients from an international multicenter series. Arthritis Rheum. 2011;63:545–555. doi: 10.1002/art.30128. [DOI] [PubMed] [Google Scholar]
- 63.Record JL, Beukelman T, Cron RQ. Combination therapy of abatacept and anakinra in children with refractory systemic juvenile idiopathic arthritis: a retrospective case series. J Rheumatol. 2011;38:180–181. doi: 10.3899/jrheum.100726. [DOI] [PubMed] [Google Scholar]
- 64.Loh NK, Lucas M, Fernandez S, Prentice D. Successful treatment of macrophage activation syndrome complicating adult Still disease with anakinra. Intern Med J. 2012;42:1358–1362. doi: 10.1111/imj.12002. [DOI] [PubMed] [Google Scholar]
- 65.Acker WB, 2nd, Nixon SL, Lee JJ, Jacobson NA, Haftel H, Farley FA. Septic arthritis of the Hip in the setting of hemophagocytic lymphohistiocytosis: a case report. JBJS Case Connect. 2015;5:e69. doi: 10.2106/JBJS.CC.N.00230. [DOI] [PubMed] [Google Scholar]
- 66.Kemps M, Verhave JC, Claassen MAA, Ruinemans-Koerts J, van der Spek E. The case: a patient with antineutrophil cytoplasmic antibody-positive vasculitis on treatment with fever and leucopenia. Kidney Int. 2017;92:775–776. doi: 10.1016/j.kint.2017.03.039. [DOI] [PubMed] [Google Scholar]
- 67.Fisher CJ, Jr, Dhainaut JF, Opal SM. Recombinant human interleukin 1 receptor antagonist in the treatment of patients with sepsis syndrome. Results from a randomized, double-blind, placebo-controlled trial. Phase III rhIL-1ra Sepsis syndrome study group. JAMA. 1994;271:1836–1843. [PubMed] [Google Scholar]
- 68.Opal SM, Fisher CJ, Jr, Dhainaut JF. Confirmatory interleukin-1 receptor antagonist trial in severe sepsis: a phase III, randomized, double-blind, placebo-controlled, multicenter trial. The interleukin-1 receptor antagonist sepsis investigator group. Crit Care Med. 1997;25:1115–1124. doi: 10.1097/00003246-199707000-00010. [DOI] [PubMed] [Google Scholar]
- 69.Shakoory B, Carcillo JA, Chatham WW. Interleukin-1 receptor blockade is associated with reduced mortality in sepsis patients with features of macrophage activation syndrome: reanalysis of a prior phase III trial. Crit Care Med. 2016;44:275–281. doi: 10.1097/CCM.0000000000001402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Antin JH, Weinstein HJ, Guinan EC. Recombinant human interleukin-1 receptor antagonist in the treatment of steroid-resistant graft-versus-host disease. Blood. 1994;84:1342–1348. [PubMed] [Google Scholar]
- 71.Singh N, Hopkins SJ, Hulme S. The effect of intravenous interleukin-1 receptor antagonist on inflammatory mediators in cerebrospinal fluid after subarachnoid haemorrhage: a phase II randomised controlled trial. J Neuroinflammation. 2014;11:1. doi: 10.1186/1742-2094-11-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Emsley HCA, Smith CJ, Georgiou RF. A randomised phase II study of interleukin-1 receptor antagonist in acute stroke patients. J Neurol Neurosurg Psychiatry. 2005;76:1366–1372. doi: 10.1136/jnnp.2004.054882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Thomas MG, Bayliss C, Bond S. Trial summary and protocol for a phase II randomised placebo-controlled double-blinded trial of Interleukin 1 blockade in Acute Severe Colitis: the IASO trial. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2018-023765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.NHS England Clinical commissioning policy statement: biologic therapies for the treatment of juvenile idiopathic arthritis (JIA) 2015. https://www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2015/10/e03pd-bio-therapies-jia-oct15.pdf
- 75.NHS England Clinical commissioning policy: anakinra/tocilizumab for the treatment of adult-onset Still's Disease refractory to second-line therapy (adults) 2018. https://www.england.nhs.uk/wp-content/uploads/2018/07/1609-anakinra-and-tocilizumab-for-aosd.pdf
- 76.Behrens EM, Koretzky GA. Review: Cytokine storm syndrome: looking toward the precision medicine era. Arthritis Rheumatol. 2017;69:1135–1143. doi: 10.1002/art.40071. [DOI] [PubMed] [Google Scholar]
- 77.Nikiforow S, Berliner N. To “lump” or to “split” in macrophage activation syndrome and hemophagocytic lymphohistiocytosis. Arthritis Rheumatol. 2020;72:206–209. doi: 10.1002/art.41106. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


