Abstract
Objective.
Behavioral economic research suggests that increasing the salience of a delayed reward may improve capacity for delaying gratification and increase behavior allocated towards obtaining larger, delayed substance-free reward rather than smaller, more immediate reward such as alcohol use. This study aimed to improve the efficacy of outpatient alcohol use disorder (AUD) treatment by adding elements that target behavioral economic mechanisms of change.
Method.
Forty-one (N = 41) adults in outpatient AUD treatment were recruited and 37 participants were retained at follow-up. Following baseline assessment, participants received either the Substance Free Activity Session (SFAS), a single-session behavioral economic–informed intervention focused on increasing future orientation and engagement in values-based substance-free activities or a health education control intervention. Participants in both conditions received weekly prompts (via text or email) relevant to their respective intervention for four weeks. Participants (68.3% male; 70.7% Caucasian, M age = 38.24, SD=12.69) reported an average of 3.95 (SD=4.72) binge drinking episodes (4/5 drinks per occasion for a woman/man) and 5.05 (SD=5.32) drinks per drinking day 30-days prior to treatment entry.
Results.
The study provided initial support for the feasibility and acceptability of implementing the SFAS within a treatment setting. Participants reported high levels of satisfaction with the SFAS (M = 9.08 (SD=.94), on a scale of 1–10). At 3-month follow-up, the SFAS was associated with reductions in the proportion of activity participation and enjoyment (reinforcement) related to substance-use relative to substance-free activities and in alcohol demand compared to control.
Conclusion.
These preliminary results provide initial support for targeting behavioral economic mechanisms of change in an outpatient AUD treatment with a single-session intervention plus remote delivery of booster prompts.
1. Introduction
Alcohol use disorder (AUD) is a significant public health problem affecting an estimated 16 million people in the United States (Center for Behavioral Health Statistics and Quality, 2015). AUD is associated with burden both at the societal and individual level, including high healthcare costs, crime, lost productivity, and poor physical and mental health outcomes (Collins, Lapsley, Lecavalier, & Single, 2000; Rehm et al., 2014). Behavioral AUD therapies, such as cognitive behavioral therapy, twelve-step facilitation, or motivation enhancement therapy, are widely utilized and generally effective (Magill, Kiluk, McCrady, Tonigan, & Longabaugh, 2015; Longabough et al., 2005; Miller & Welbourne, 2002). However, AUD treatment is typically associated with relatively small effect sizes and high relapse rates (Magill & Ray, 2009; Anton et al., 2006). There is a need to enhance treatment and increase effect sizes with novel brief intervention elements that target theory-based mechanisms of behavior change.
1.1. Behavioral economic theory of substance abuse
The behavioral economic reinforcer pathology model suggests that individuals with AUD overvalue alcohol relative to other reinforcers (Bickel et al., 2018). The primary behavioral economic measure of alcohol value is the hypothetical Alcohol Purchase Task (APT), which asks participants how many drinks they would purchase and consume across a range of prices (Murphy & MacKillop, 2006). Responses on the APT are used to generate alcohol demand curve indices of reinforcing efficacy—including maximum alcohol consumption (demand intensity), maximum alcohol expenditure (Omax), and alcohol price sensitivity (demand elasticity)—that are correlated with alcohol problem severity (Murphy & MacKillop, 2006). Demand is also associated with intervention response. Although higher pretreatment demand is associated with increased levels of follow-up drinking (MacKillop & Murphy, 2007), interventions can reduce demand, and the degree of post-treatment reduction predicts lowered drinking at follow-up (Murphy et al., 2015).
Research suggests that environments deprived of substance-free reinforcement are associated with high rates of substance use, whereas environments with higher levels of alternative rewards are associated with lower use (Volkow & Baler, 2014; Carroll, Anker, & Perry, 2009; Higgins, Heil, & Lussier, 2004). Moreover, treatments that enhance the availability of substance-free alternative reinforcers are generally effective (Correia et al., 2005; McKay, 2017), and research with emerging adults suggests that lower levels of substance-free reinforcement at baseline predict poor response to brief interventions (Murphy, Correia, Colby, & Vuchinich, 2005).
Individuals who drink heavily may under-engage in constructive alternatives to drinking because the benefits of these activities are generally delayed. Delay discounting assesses the degree of decrease in subjective value associated with the temporal delay of a reward and is an important individual difference risk factor for substance use, as well as a predictor of treatment response (Bickel, Johnson, Koffarnus, MacKillop, & Murphy, 2014). Increasing the salience of delayed outcomes and the extent to which the behavior leading to those rewards or punishers is viewed as part of a coherent pattern can reduce impulsive choices (Rung, Peck, Hinnenkamp, Preston, & Madden, 2019). Experimental studies using Episodic Future Thinking (EFT), a task that requires participants to vividly imagine positive future events, have demonstrated reductions in delay discounting (see Rung & Madden, 2018 for a review). Thus, a unique implication of behavioral economic theory is that interventions should attempt to aggregate more global day-today decisions and activities (both substance-related and substance-free) into cohesive patterns that have implications for long-term substance-free rewards.
1.2. Brief behavioral economic alcohol interventions
Murphy and colleagues (2012a) developed the substance-free activity session (SFAS), a single-session supplement to a standard alcohol brief motivational intervention (BMI) for college student heavy drinkers. The SFAS uses principles of motivational interviewing (MI; Miller & Rollnick, 2012) and personalized feedback to target behavioral economic mechanisms of substance-free reinforcement and delay discounting. The overall goal of the SFAS is to enhance the salience and value of delayed academic and career goals, to help students to make a connection between their current patterns of behavior and the attainment of delayed rewards, and to increase engagement in goal-directed and enjoyable substance-free activities. Murphy et al. (2012a) found that the alcohol MI + SFAS, relative to alcohol MI + relaxation training control condition, was associated with larger reductions in alcohol-related problems, increased time spent studying in the evenings, and higher scores on a measure of future orientation. Findings from a larger multisite follow-up trial (Murphy et al., 2019) suggest the alcohol MI + SFAS and alcohol MI + relaxation training both demonstrated moderate to large effect-size reductions in alcohol use and problems that were maintained across a 16-month follow-up relative to an assessment-only condition. Furthermore, the proportion of total activity participation and enjoyment related to substance-related activities mediated the effect of the intervention on both drinking level and alcohol problems.
Murphy et al.’s (2012a, 2019) findings provide support for the utility of enhancing standard alcohol treatments with behavioral economic treatment elements. Although many AUD behavioral treatment protocols encourage engagement in substance-free activities, most do not include systematic efforts to increase patterns of substance-free activity engagement. Thus, there is a need for novel brief approaches to incorporate these behavioral economic interventions that have the potential to enhance AUD treatments. The SFAS approach can extend standard treatment by 1) implementing a more tailored and personalized approach to identifying alternative activities that are consistent with personal goals, 2) providing personalized feedback that aggregates behaviors into patterns and frames those patterns in terms of their impact on future rewards, and 3) attempting to increase the subjective salience and value of future outcomes.
1.3. Current study
The current study assessed the feasibility and preliminary efficacy of an adapted SFAS for an adult outpatient AUD treatment population and evaluated the SFAS in a randomized controlled pilot trial with a health education (HE) control condition. This adapted SFAS aimed to increase the potency of the SFAS (originally developed for non-treatment seeking college students; Murphy et al., 2012) by including an EFT task to increase salience of delayed outcomes and adding booster contact following the intervention. Patients received either the SFAS or HE session to augment their treatment as usual plus four weekly booster (via text or email) messages related to the intervention. We hypothesized that the SFAS condition would be associated with reductions in proportionate reinforcement from substance-related activities, alcohol demand, and delay discounting at 3-month follow-up compared to the HE active control condition.
2. Method
2.1. Participants and procedures
Participants were 41 patients in outpatient AUD treatment (intensive outpatient program [n = 36]), individual counseling (n = 3), or mutual help group (SMART Recovery, n = 2) in the mid-South region of the United States. Across treatment programs, although frequency of treatment varied, cognitive behavioral strategies were commonly used as an approach to AUD treatment. The sample was 68.3% male, 70.7% non-Hispanic white, and the mean age was 38.24 (SD = 12.69) years. See Figure 1 for CONSORT diagram and Table 1 for descriptive statistics. Study eligibility included a diagnosis of AUD, current engagement in alcohol treatment, and 18 years of age or older. Eligible participants provided informed consent, completed a battery of self-report and clinical interview assessments, and were randomized into one of two study conditions. Randomization utilized a block design that stratified by gender and treatment site.
Figure 1.
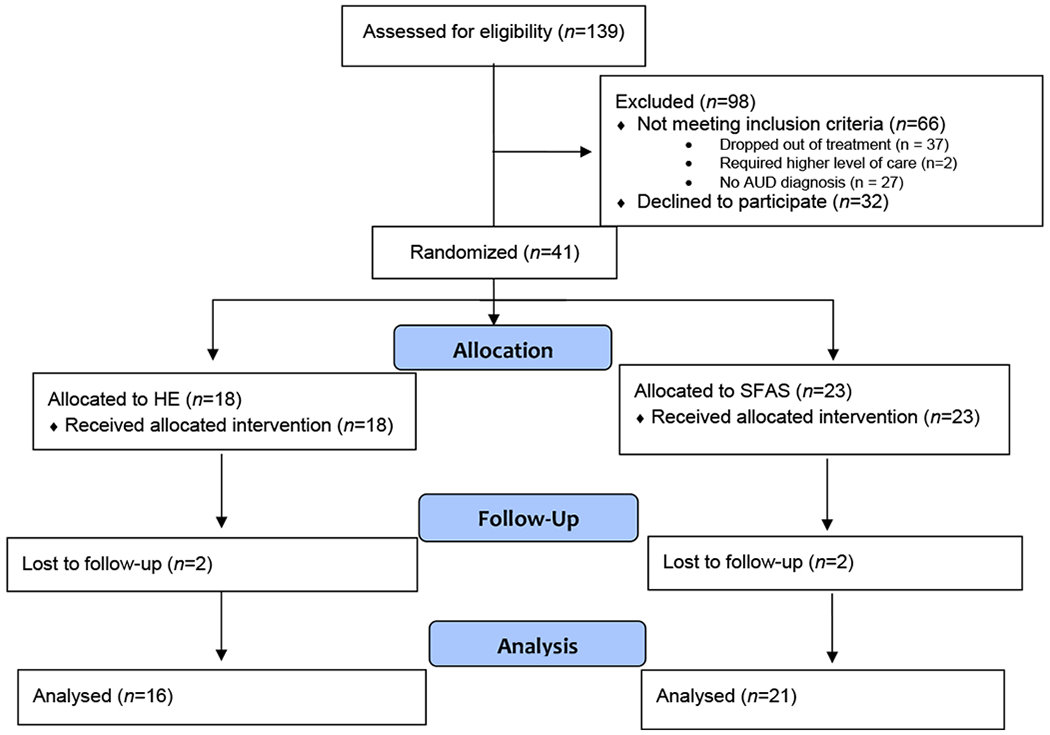
CONSORT diagram of participant recruitment, randomization, and completion of follow-up assessment of the study.
Table 1.
Descriptive statistics, N (%) or mean (standard deviation), for demographic and drinking (out of 30 days) variables.
| Total Sample (N=41) | SFAS (n=23) | HE (n=18) | Statistical Test | |
|---|---|---|---|---|
| Gender | χ2(2) = 0.88 | |||
| Male | n = 28 (68.3%) | n = 15 (65.2%) | n = 13 (72.2%) | |
| Female | n = 12 (29.3%) | n = 7 (30.4%) | n = 5 (27.8%) | |
| Transgender | n = 1 (2.4%) | n = 1 (4.3%) | n = 0 (0.0%) | |
| Race | χ2 (2) = 2.94 | |||
| White | n = 29 (70.7%) | n = 18 (78.3%) | n = 11 (61.1%) | |
| Black | n = 11 (26.8%) | n = 4 (17.4%) | n = 7 (38.9%) | |
| Multiracial | n = 1 (2.4%) | n = 1 (4.3%) | n = 0 (0.0%) | |
| Age | 38.24 (12.69) | 37.83 (12.26) | 38.78 (13.56) | t (39) = 0.24 |
| Days in treatment | 25.98 (15.19) | 26.87 (17.71) | 24.83 (11.60) | t (39) = −0.42 |
| Binge episodes | 3.95 (4.72) | 4.87 (5.34) | 2.78 (3.59) | t (39) = −1.42 |
| Drinking days | 6.19 (6.31) | 6.30 (2.26) | 6.06 (6.56) | t (39) = −0.12 |
| Drinks per drinking day | 5.05 (5.32) | 5.71 (5.46) | 4.21 (5.17) | t (39) = −0.88 |
| AUD symptoms | 7.39 (2.61) | 7.35 (2.52) | 7.44 (2.79) | t (39) = 0.12 |
Note. AUD = Alcohol Use Disorder. SFAS = Substance-Free Activity Session condition. HE = Health Education condition. Binge Episodes are defined as 4/5 or more drinks per occasion for woman/man.
After completion of baseline assessment and randomization, participants returned within one week for either the 60-minute SFAS or the HE control session. Immediately following the in-person intervention session, participants evaluated the session in a secure web-based survey. Over the 4 weeks following the intervention, participants received a brief weekly booster message that augmented their SFAS or HE session via their choice of text-message or email. A follow-up assessment was conducted three months post-baseline. Participants received $25 and $40 for completing the baseline and follow-up assessments, respectively. The university Institutional Review Board approved all study procedures. This trial and the analyses presented below were planned as part of the first author’s dissertation (F31AA024381) but were not registered on clinicaltrials.gov.
2.2. Measures
2.2.1. Activity Level Questionnaire – Substance Use Version (ALQ-SUV)
The ALQ-SUV was used to measure past-month reinforcement from substance-related and substance-free activities. Past-month ratings of activity engagement frequency (0 times in the past 30 days to 4 more than once a day) and enjoyment (0 unpleasant or neutral to 4 extremely pleasant) were made with 5-point Likert-type scales (Correia, Carey, Simons, & Borsari, 2003). The frequency and enjoyment ratings were multiplied to obtain a cross-product score (range = 0–16), which reflected activity reinforcement. A reinforcement ratio was computed by dividing the mean substance-related reinforcement by the mean of all available reinforcements (substance-free + substance-related). Internal consistency for substance-related reinforcement was good at baseline (α = .83) and 3-month follow-up (α = .84). Similarly, internal consistency for the substance-free reinforcement score was good at baseline (α = .70) and 3-month follow-up (α = .83).
2.2.2. Alcohol Purchase Task (APT)
The Alcohol Purchase Task (APT; Murphy & MacKillop, 2006) was used to measure alcohol demand at baseline and 3-month follow-up. The APT presented participants with a hypothetical drinking scenario and participants were asked how many drinks they would purchase and consume at 17 ascending prices from $0 (free) to $20 per drink. Data cleaning procedures were completed consistent with standard recommendations (Stein, Koffarnus, Snider, Quisenberry, & Bickel, 2015). No participants were omitted for inconsistent responses. The APT yields five demand indices: 1) Intensity—number of drinks consumed when the price is $0; 2) Breakpoint—the first price at which alcohol consumption is zero; 3) Omax—maximum alcohol expenditure; 4) Pmax—the price at maximum expenditure; and 5) Elasticity—sensitivity of alcohol consumption to increases in price. Elasticity is calculated using the exponentiated model (Koffarnus et al., 2015), which allows zero values and improves model fit (Yu et al., 2014). These five demand indices were used to compute two composite variables of demand, persistence and amplitude (MacKillop et al., 2009). Persistence was calculated as the standardized mean scores of Breakpoint, Omax, Pmax, and Elasticity; this index reflects price sensitivity. Elasticity values were reverse scored prior to computing persistence such that higher values reflected increased demand akin to the other demand indices in the composite. Amplitude was calculated using the standardized mean scores of Omax and Intensity; this index reflects maximum consumption and expenditure.
2.2.3. Delay discounting
Delay discounting was measured with an 8-item measure wherein participants made choices between two hypothetical amounts of money with varying temporal delays (Gray, Amlung, Acker, Sweet, & MacKillop, 2014). Sample items included: Would you rather have $100 in 6 months or $10 today? And would you rather have $50 today or $100 in 1 year? Hypothetical money choices provide a reliable and valid estimate of discounting rates (Smith & Hantula, 2008). Impulsive choice ratios (ICR) were computed by using the ratio of impulsive choices relative to all choices, such that larger ratios indicate more impulsive decision-making (MacKillop & Kahler, 2009). This brief measure has been effectively used with noncollege, adult samples (Acuff et al., 2018). The ICR in the current study demonstrated a range from .13 to 1 at baseline and 0 to 1 at follow-up. Internal consistency reliabilities were good at baseline (α = .78) and 3-month follow-up (α = .81). Additionally, ICR was normally distributed at baseline and follow-up, with no ceiling effects observed.
2.2.4. Alcohol consumption and alcohol use disorder
Alcohol consumption at baseline and follow-up was assessed using a 90-day timeline follow-back interview (TLFB; Sobell & Sobell, 1996), a calendar-assisted measure of a participant’s retrospective account of daily alcohol intake. Using the TLFB, three drinking-related dependent variables were computed: binge drinking days (5/4 or more standard drinks for men/women per occasion), number of drinking days, and number of drinks per drinking day. Although 90 days of drinking data were collected, data reported herein are for the first 30 days out of the 90 at baseline assessment and the latter 30 days of 90 at the 3-month follow up. This procedure permitted a true baseline drinking level prior to treatment engagement and a comparable data point of the most recent 30 days at follow-up. A structured clinical interview (SCID; First, 2014) was administered by trained study personnel at baseline and follow-up to assess past 90-day DSM-5 AUD symptoms. Responses to the 11-items were dichotomously coded (present/absent) to assess for AUD symptoms.
2.2.5. Evaluation of intervention delivery
To ensure intervention integrity across clinicians, a random 20% of the session recordings (SFAS, n = 4 and HE, n = 4) were selected and reviewed by two trained independent coders. Sessions from each clinician were reviewed using a brief intervention adherence protocol commonly used in intervention trials (Martens, Smith & Murphy, 2013; Murphy et al., 2012b). Each component on the protocol was rated from 0 (Didn’t do it, N/A) to 3 (Above expectations). A score of 2 or higher indicated intervention delivery was consistent with protocol. Further, a random 20-minute segment of the SFAS recording was selected and coded for MI adherence by two additional independent reviewers trained in MI and SFAS delivery. The motivational interviewing treatment integrity (MITI; Moyers, Manuel, & Ernst, 2014) was used to code the four global scores of the MITI (cultivating change talk, softening sustain talk, partnership, and empathy) rated on a 5-point Likert-type scale with 1 indicating low and 5 indicating high MI adherence. The MITI also included 8-items on MI consistent behavior counts, which include rolling with resistance, asking open ended questions, and reflections. Each of the 8 items was rated from 0 (Didn’t do it, N/A) to 3 (Above expectations).
2.2.6. Evaluation of participant satisfaction
Participants completed a brief assessment at the end of the SFAS or HE session to assess their degree of satisfaction with the intervention and the clinician (this information was not shared with clinicians). Ratings were on a 10-point Likert-type scale for intervention ratings and 4-point Likert-type scale for clinician ratings with higher numbers indicating greater satisfaction.
2.2.7. Evaluation of perceived intervention benefit
At follow-up, participants rated the intervention’s benefit on the following seven domains: helpfulness in overall treatment progress, goal pursuit, time management, balanced life, improved sleep, improved diet, and change in drinking or drug use. Participants rated the intervention’s helpfulness on a Likert scale of 1(Extremely unhelpful) - 5 (Extremely helpful).
2.3. Clinician training and supervision
Clinicians included doctoral-level clinical psychology graduate students and a licensed clinical psychologist. All clinicians completed approximately 15 hours of training in MI, including readings, DVDs, and role-playing; and approximately 5 hours of specific training in the SFAS and health education interventions. All sessions were audio-recorded and reviewed during weekly group supervision. Training and supervision was provided by a licensed clinical psychologist with expertise in MI and behavioral economics (author JGM).
2.4. Interventions
2.4.1. Substance-free activity session (SFAS)
This adapted SFAS retained similar session objectives as the original SFAS (Murphy et al., 2012a), but the content of the session and information provided to participants was modified to ensure that it was relevant to a noncollege, treatment-seeking population. Clinicians used an MI approach to develop each participants’ motivation to engage in substance-free activities and to enhance the salience of personally meaningful delayed rewards (e.g., improving health, developing a hobby, generating social support). Although each session was individually tailored, the unifying focus of the SFAS was on encouraging participants to identify short- and long-term goals related to substance-free activities, discussing the importance and potential benefits of those goals, the potential negative influence of alcohol use on goal pursuit, and committing to patterns of behavior that are consistent with those goals. Each participant was provided a graphical representation of what they reported as important life domains (e.g., family, career) and how consistent their past week actions had been within those domains (Wilson, Sandoz, Kitchens, & Roberts, 2010). This feedback was used to elicit discussion about increasing behavior that was more consistent with their personally held values. The session also included personalized feedback on participants’ reported time allocation to a variety of constructive activity categories (e.g., exercise, job-related activities, hobbies) as well as drinking/drug use. Each participant received personalized, specific information about wellness/fitness, hobby, career, social, or community activities consistent with their goals in addition to a detailed list of relevant substance-free activities available in the community.
Novel intervention components specific to this adapted SFAS included the EFT task, specific feedback on reported values and actions pertaining to those values (Wilson, Sandoz, Kitchens, & Roberts, 2010), and booster text messages or emails following the intervention. The EFT asked participants to vividly imagine and write about a positive future event with the goal of making future outcomes more salient in the present. Indeed, EFT tasks have been shown to reduce delay discounting and alcohol demand in laboratory studies (Snider, LaConte, & Bickel, 2016; Daniel, Stanton, & Epstein, 2013) but have not yet been tested as part of a clinical intervention trial. Prior to completing the EFT task, participants were asked to: Write about a specific type of positive experience yon are looking forward to. It could be how you want to grow mentally, spiritually, physically, or anything that gives you a sense of meaning, mission, or purpose. Consider including what you will be doing, who you will be with, how you will feel, or the types of thoughts and emotions you expect to have.
The session concluded with the participant and the clinician formulating specific goals to help the participant reallocate his or her time and optimize progress toward goals. Finally, each participant received individually tailored booster text messages or emails (38 participants chose text messages and 3 chose email) with reminders about the activities/goals he/she had committed to in the SFAS session, and additional personalized feedback on locally available substance-free activities consistent with their stated interests. An example of a booster message is: “You were interested in [company name], an organization that helps students with reading. Their next tutor training is [date] and you can get more information here [link].” Participants were asked to confirm receiving each message.
2.4.2. Health education (HE)
The HE protocol was developed using sleep hygiene educational materials from The National Sleep Foundation (2015) and nutrition educational materials from the United States Department of Agriculture Food and Nutrition Service (2015). The session was an individual, counselor-administered, educational, interactive session but did not include personalized feedback or motivational interviewing components. For HE participants, standardized booster texts/emails (delivered weekly for 4 weeks) provided reminders of information on sleep and nutrition education. An example of the standard messages delivered to HE participant is as follows, “We are reminding you that a balanced diet of protein, fruits, vegetables, and grains can help you boost energy, control weight, help fight disease, and improve heart health and mood.” Participants were asked to respond to confirm receiving each message.
2.5. Data analytic plan
Data analyses were computed using SPSS version 21.0 and MPlus version 7.3. Values greater than 3.29 SDs above the mean on a given variable were considered outliers and Winsorized to one unit greater than the greatest nonoutlier value (Tabachnick & Fidell, 2013). Baseline descriptive characteristics of the sample are presented in Table 1. Attrition effects were evaluated by testing whether systematic differences existed between those participants who completed the 3-month follow-up (n = 37) versus those who did not (n = 4). Maximum likelihood estimation was used to estimate regression parameters. This approach assumes that data are missing at random, and it is a preferred method for estimation with missing data (Schafer & Graham, 2002).
A series of linear regression models were computed to assess associations between treatment condition and change in the following behavioral economic variables: reinforcement ratio (as measured with the ALQ-SUV), alcohol demand composite variables of amplitude and persistence, and delay discounting at follow-up (Bandyopadhyay, DeSantis, Korte, & Brady, 2011). Amplitude and persistence, instead of individual demand metrics, were utilized in this sample as alcohol demand was suppressed at follow-up with 29% of the sample reporting they would not purchase alcohol at any price. The composite variables permitted the use of mean standardized scores to include all reported data, without excluding individuals who did not purchase hypothetical drinks. Regression analyses included treatment condition and baseline levels of the outcome as covariates. Additional exploratory analyses controlled for treatment clinician, treatment site, and standard treatment duration, but results yielded similar outcomes. Thus, we present the more parsimonious models without these exploratory covariates. We conducted significance testing for behavioral economic outcomes based on a priori support from EFT studies with small sample sizes that found significant reductions in alcohol demand and delay discounting (Snider, LaConte, & Bickel, 2016; Daniel, Stanton, & Epstein, 2013) and, given the pilot nature of the work, we reported effect sizes for alcohol use outcomes.
3. Results
3.1. Baseline characteristics
At baseline, approximately 26.8% of participants (n=11) reported abstinence. Those who engaged in drinking reported an average of 6.19 (SD = 6.31) drinking days out of 30 days, 3.95 (SD = 4.72) binge drinking episodes, 5.05 (SD = 5.32) drinks per drinking day, 7.39 (SD = 2.61) AUD symptoms, and having been in treatment for 25.98 (SD = 15.19) days (see Table 1). Statistical analyses indicated no significant differences between the intervention groups on any demographic variables or baseline alcohol-related outcome variables. Follow-up rate was 90.2% (Figure 1) with no significant differences by condition. There were no significant baseline differences for participants who completed versus those who did not complete the follow-up assessment on any of the baseline drinking variables. There were no clinician or recruitment site effects on outcome variables.
3.2. Intervention feasibility, validity, & acceptability
Of the 139 participants screened for study eligibility, 41 participants consented, completed the baseline survey, were randomized, and received the in-person intervention. Of the four booster messages sent to each participant, on average, participants confirmed receiving 3.14 (SD=1.04) messages. There were no significant group differences in confirmed booster message receipts—on average SFAS participants confirmed 3.22 (SD = 0.95) and control participants confirmed 3.06 (SD = 1.16) messages.
3.2.1. Internal validity
Independent coders’ average rating of content fidelity for the SFAS was 2.07 (SD = .09; on a scale of 1– 3), with 100% of the intervention elements meeting or exceeding expectations. Similarly, the HE average rating was 2.03 (SD = .07), with 100% of the intervention elements meeting or exceeding expectations. Coding on Mi-specific skills for the SFAS indicated an average rating of 4.41 (SD = .23, on a scale of 1–5) for the 4 items on the global scale and an average rating of 2.14 (SD = .29, on a scale of 0–3) for the 8 items of MI consistent behavior counts, with 92% of the behavior counts rated as meeting or exceeding expectations.
3.2.2. Participant satisfaction
SFAS participants reported average satisfaction ratings of the clinician 3.79 (SD = .30, on a scale of 1–4) and satisfaction rating of the session 9.08 (SD = .94, on a scale of 1–10). HE participants reported average satisfaction ratings of the clinician 3.67 (SD = .31, on a scale of 1–4) and satisfaction ratings of the session 8.44 (SD = 1.76, on a scale of 1–10). There were no significant differences across interventionists for clinician or session ratings in either condition.
At follow-up, participants reported on the benefit of the intervention in the domains targeted by each intervention (e.g., goal pursuit for SFAS or improved sleep for HE), as well as the overall contribution to treatment progress and change in drinking. Means, standard deviations, and Cohen’s d are presented in Table 2. SFAS participants’ scores suggest moderate between group effect sizes in the intervention helping with time management (d = .65) and living a balanced life (d = .50). SFAS participants’ report suggest a small effect size in overall treatment progress (d = .36) and goal pursuit (d = .41). The HE condition reported higher means in improved sleep with a small between group effect size (d = .44). These ratings are consistent with each intervention’s targeted elements, other than the fact that the HE session was not perceived as helpful for changing diet. The interventions were rated comparably in helping to support change in drinking/drug use.
Table 2.
Mean (SD) ratings of perceived intervention benefit and between group effect size (Cohen’s d) in each category at 3-month follow-up.
| Perceived Helpfulness of Study | Total (n = 35) | SFAS (n=20) | HE (n=15) | Between Group (d) |
|---|---|---|---|---|
| Overall Treatment Progress | 3.97 (.82) | 4.10 (.79) | 3.80 (.86) | .36 |
| Pursuing goals | 3.91 (.78) | 4.05 (.76) | 3.73 (.79) | .41 |
| Time management | 3.60 (.74) | 3.80 (.62) | 3.33 (.82) | .65 |
| Balanced life | 3.74 (.95) | 3.95 (.76) | 3.47 (1.13) | .50 |
| Improved sleep | 3.51 (.89) | 3.35 (.93) | 3.73 (.78) | − .44 |
| Improved diet | 3.43 (.88) | 3.40 (.75) | 3.47 (1.06) | − .08 |
| Changed drinking or drug use | 3.71 (1.07) | 3.75 (1.16) | 3.67 (.98) | .07 |
Note: The items ranged from 1 (extremely unhelpful) to 5 (extremely helpful).
3.3. Behavioral economic outcomes
Linear regression analyses, controlling for baseline reinforcement from the ALQ-SUV, indicated that the SFAS condition had lower reinforcement ratio values at follow-up compared to controls, B (SE) = −0.61 (0.29), p = .032 (Table 3 and Figure 2). Similarly, linear regression analyses that controlled for the respective alcohol demand composite scores from the baseline APT indicated that individuals in the SFAS condition had lower alcohol demand persistence (B (SE) = −0.77 (0.23), p = .006) and amplitude (B (SE) = −0.60 (0.30), p = .046) at follow-up compared to controls (see Table 3). Similar analyses indicated no intervention group differences in delay discounting at follow-up, B (SE) = 0.58 (0.24), p = .397.
Table 3.
Linear regression results for behavioral economic variables of relative reinforcing value of alcohol-related activities (reinforcement ratio), alcohol demand composite variables of persistence and amplitude, and impulsive choice ratio (ICR) as a measure of delay discounting.
| SFAS M (SD) | HE M (SD) | B (SE) | [95% CI] | p | Between Group (d) | |
|---|---|---|---|---|---|---|
| Reinforcement Ratio | ||||||
| Treatment (HE = 0; SFAS = 1) | 0.28 (.33) | 0.45 (.25) | −0.61 (.29) | [−1.08, −0.14] | .032* | 0.58 |
| Baseline reinforcement ratio | 1.36 (.52) | [−0.51, 2.22] | ||||
| Persistence | ||||||
| Treatment (HE = 0, SFAS = 1) | −0.31 (.78) | 0.33 (.93) | −0.77 (.28) | [−1.23, −0.31] | .006** | 0.74 |
| Baseline persistence | 0.06 (.20) | [−0.27, 0.38] | ||||
| Amplitude | ||||||
| Treatment (HE = 0, SFAS = 1) | −0.23 (.91) | 0.29 (.80) | −0.60 (.30) | [−1.10, −0.11] | .046* | 0.61 |
| Baseline amplitude | 0.03 (.20) | [−0.31, 0.36] | ||||
| Delay Discounting | ||||||
| Treatment (HE = 0; SFAS = 1) | 0.58 (.24) | 0.51 (.28) | 0.26 (.30) | [−0.24, 0.76] | .397 | 0.27 |
| Baseline ICR | 1.86 (.54) | [0.98, 2.75] |
Note. AUD = Alcohol Use Disorder. SFAS = Substance-Free Activity Session condition. HE = Health Education condition.
p <.05.
<.01
Figure 2.
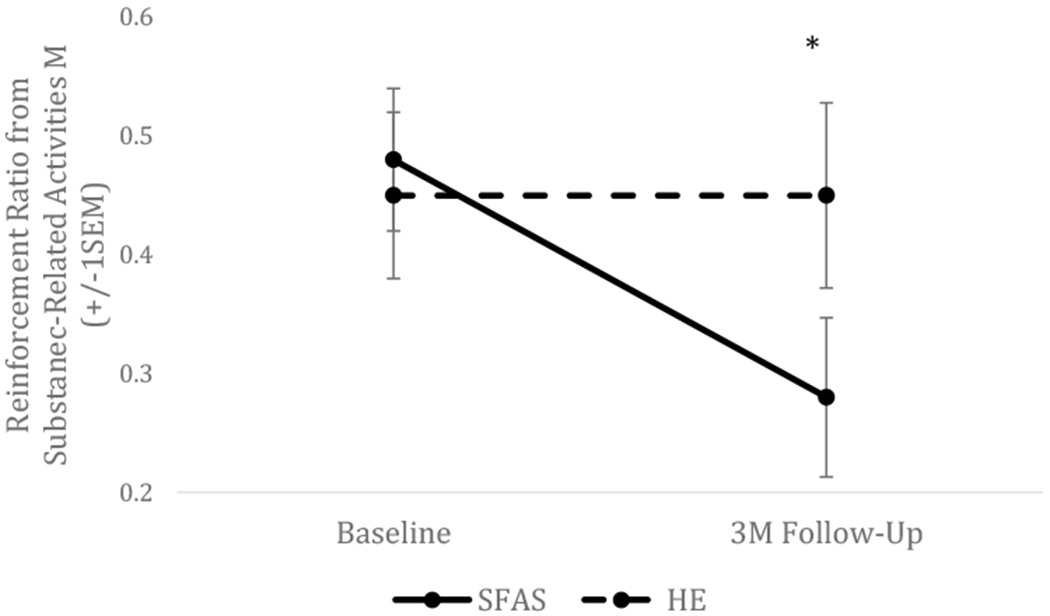
Change in level of reinforcement from substance-related activities relative to all available activities (reinforcement ratio) from baseline to 3-month follow-up by treatment condition. SFAS was associated with lower reinforcement ratio at 3-month compared to HE control condition. SEM – standard error of the mean.
3.4. Alcohol use outcomes
Descriptive alcohol use data are presented in Table 4. Between group comparison suggests a small effect size in which the SFAS condition reported fewer binge episodes (d = .26) at follow up. Similar small effect sizes are observed in which the HE condition reported fewer drinks per drinking day (d = .21) and AUD symptoms (d = .25) at follow-up.
Table 4.
Mean (SD), between and within group effect size (Cohen’s d) for alcohol use outcome (out of 30 days) variables at baseline and 3-month follow-up (adjusted for baseline value) for participants who completed the follow-up assessment. Negative between-group Cohen’s d values suggest that the SFAS group reduced more and positive values suggest more reduction in HE group.
| SFAS (n=21) | HE (n=16) | Total (n=37) | Between Group (d) | |
|---|---|---|---|---|
| Binge Episodes -Baseline | 4.52 (4.76) | 2.88 (3.71) | 3.81 (4.40) | |
| Binge Episodes −3M | 1.20 (1.82) | 1.93 (3.61) | 1.51 (2.71) | −.26 |
| Binge Episodes Within Group d | .92 | .26 | .93 | |
| Drinking Days -Baseline | 6.05 (5.85) | 5.75 (6.50) | 5.92 (6.05) | |
| Drinking Days – 3M | 3.85 (7.85) | 3.80 (5.63) | 3.83 (6.89) | .01 |
| Drinking Days Within Group d | .32 | .32 | .32 | |
| Number of Drinks -Baseline | 41.93 (44.79) | 30.56 (39.10) | 37.01 (42.24) | |
| Number of Drinks -3M | 16.25 (25.89) | 20.60 (34.23) | 18.11 (29.35) | −.14 |
| Number of Drinks Within Group d | . 70 | .27 | .52 | |
| Drinks per Drinking Day -Baseline | 5.85 (5.55) | 3.31 (3.56) | 4.75 (4.90) | |
| Drinks Per Drinking Day -3M | 4.18 (6.10) | 2.99 (4.99) | 3.67 (5.60) | .21 |
| Drinks per Drinking Day Within Group d | .29 | .21 | .21 | |
| AUD Symptoms – Baseline | 7.24 (2.61) | 7.81 (2.43) | 7.49 (2.51) | |
| AUD Symptoms – 3M | 2.65 (3.13) | 1.87 (3.02) | 2.31 (3.07) | .25 |
| AUD Symptoms Within Group d | 1.59 | 2.17 | 1.87 | |
Note. 3M = 3-month follow-up. SFAS = Substance Free Activity Session. HE = Health Education
4. Discussion
This randomized pilot study assessed the SFAS as an adjunctive intervention for outpatient AUD treatment. The study demonstrated that it was feasible to administer the SFAS within the context of AUD treatment, and that individuals in AUD treatment rated the intervention favorably and noted that it addressed its intended goals. Our results suggest excellent clinician adherence, high participant ratings of clinicians and session content, and consistent participant rating of intervention benefits with the targeted intervention content. The between group effect sizes for perceived intervention helpfulness among SFAS participants with respect to goal pursuit, time management, and living a balanced lifestyle suggest that the study successfully delivered the key elements of the SFAS intervention. Whereas the HE participants reported that their intervention helped them to improve their sleep, although not their diet. Of note, the two conditions were similar in their report of the intervention changing their alcohol use, which is likely due to the fact that all individuals made reductions to their drinking, mainly resulting from their primary AUD treatment. Overall, our results provide initial support for feasibility of implementing the SFAS within a treatment setting as well as the acceptability of the SFAS with treatment-seeking adults. This calls for establishing a future trial to investigate the effectiveness of the SFAS intervention in a treatment seeking population.
Our finding that the SFAS was associated with decreases in relative substance-related reinforcement ratio is largely consistent with previous studies. Prior findings suggest that reinforcement ratio decreased following a brief alcohol intervention with college students (Murphy et al., 2005), and that reductions in reinforcement ratio predicted lower levels of alcohol-related problems and marijuana use at follow-up (Dennhardt et al., 2015). A recent study reported that among heavy drinking young adults, reductions in reinforcement ratio mediated the effects of brief intervention on alcohol use and alcohol-related problems (Murphy et al., 2019), suggesting that shifting behavior away from drinking and toward substance-free activities may be one mechanism that accounts for intervention outcomes (McKay, 2017). Although not powered to evaluate mechanisms of change using mediation models, the current study is the first to investigate the impact of a brief intervention on reinforcement ratio with an adult alcohol-treatment sample and suggests that the SFAS is associated with reductions in reinforcement ratio compared to control. However, further investigation with a larger sample and longer follow-up period is needed to replicate these findings and to determine if change in reinforcement ratio mediates alcohol-related outcomes with adults in alcohol treatment as it does with college student heavy drinkers.
The finding that the SFAS was associated with reductions in alcohol demand, which reflects strength of desire to use alcohol, is consistent with the broader literature suggesting that alcohol demand is malleable in response to a variety of manipulations, including treatment (Acuff, et al., 2019). For example, naltrexone treated heavy drinkers reported reductions in alcohol demand indices of Intensity, Omax, and Breakpoint (Bujarski, MacKillop & Ray, 2012). Furthermore, in the context of behavioral treatment, two studies have demonstrated that brief motivational interventions are associated with reductions in demand among young adult heavy drinkers, and that these reductions predict subsequent changes in drinking (Dennhardt, Yurasek, & Murphy, 2015; Murphy et al., 2015). Results of a study of individuals with alcohol dependence suggest that engagement in an episodic future thinking (EFT) task was associated with lowered alcohol demand (Snider, LaConte, & Bickel, 2016). In this study, our SFAS intervention, which also included EFT, resulted in alcohol demand reduction for treatment-seeking adults. This is the first study to show that an intervention focusing on increasing substance-free activities that included an EFT task is associated with alcohol demand reduction three months after the intervention. This reduction of alcohol demand may be a mechanism of change such that the intervention is disrupting the overvaluation of alcohol and influencing the reward potential of substance-free future outcomes (Snider, LaConte, & Bickel, 2016). Future replication studies are needed to investigate the impact of the SFAS on alcohol demand as a possible mechanism of change in the context of treatment.
Contrary to our hypothesis, we did not find a significant treatment effect on delay discounting. The EFT task within the SFAS asked participants to vividly imagine experiencing a positive event in the future to manipulate excessive discounting of delayed outcomes. Indeed, previous studies have shown reductions in delay discounting among cigarette smokers (Stein, Tegge, Turner, & Bickel, 2018), participants with obesity (Daniel, Stanton, & Epstein, 2013), and with alcohol dependence (Snider, LaConte, & Bickel, 2016) immediately after an EFT task. The current study did not measure delay discounting immediately after the intervention but only at baseline and 3-month follow-up. It is possible that the intervention had a proximal impact on delay discounting that was not measured and that the effects were not sustained over time. Future research should measure delay discounting immediately after treatment to better capture the direct effect of the treatment. Nevertheless, it is noteworthy that the intervention was associated with enduring changes in alcohol demand and proportionate substance-related reinforcement.
Not surprisingly, due to the preliminary nature of this pilot trial, and that all participants were completing an alcohol treatment program, effect sizes for drinking outcomes were inconsistent and should be interpreted with caution. It is likely that the primary alcohol treatment was responsible for drinking changes. Despite no clear advantage for the SFAS in terms of drinking reductions, it was associated with a significantly greater reduction in alcohol demand, suggesting lower motivation to drink (specifically lower peak drinking motivation and greater drinking price sensitivity). Overall, although the study did not observe group differences in drinking outcomes in the brief 3-month follow-up, the changes in the behavioral economic variables could suggest that the SFAS is targeting mechanisms that are not routinely addressed in standard treatment. The brevity of the follow-up period may have inhibited observation of outcomes that may be sustained over time above and beyond standard treatment outcomes. When interpreting these results in the context of the extant behavioral economic studies that suggest changes in reinforcement ratio and alcohol demand lead to reductions in substance use (Dennhardt, Yurasek, & Murphy, 2015; Murphy et al., 2015, 2019), there is some cautious optimism that our results could suggest similar outcomes over time. Future trials with longer follow-up intervals and larger sample size are needed to clarify the effect of the SFAS on drinking outcomes with treatment seekers, as an intervention focused on increasing goal-oriented and enjoyable activities may improve long-term drinking outcome for treatment seeking populations (Daughters et al., 2018).
4.1. Strengths and limitations
This study used a randomized controlled trial to evaluate the SFAS as a novel, theoretically grounded adjunctive intervention for AUD treatment, and to evaluate the feasibility, acceptability, and internal validity of the intervention. Limitations of this study include one brief 3-month follow-up assessment, small sample size, the reliance on retrospective self-report measures of drinking and activity participation, and heterogeneity of participants’ treatment experiences (e.g., intensive outpatient program, individual counseling, and mutual help). This study did not collect information on the frequency or type of treatment participants received after study enrollment, limiting ability to assess differences in outcomes based on overall level of standard treatment received. Finally, our intervention, although brief, included a number of intervention components (discussion of goals, personalized feedback on time allocation, EFT, personalized text-messages about goals and available activities) and the design did not allow us to determine the unique efficacy of these various elements.
4.2. Implications and future directions
This is the first study to implement the behavioral economic-informed SFAS intervention, including an episodic future-thinking component, within the context of outpatient treatment and tailored for a treatment-seeking population. This pilot trial demonstrated feasibility and acceptability of the SFAS to augment outpatient treatment with high fidelity ratings and participant satisfaction ratings in both conditions. This is a brief and feasible treatment that incorporates elements not typically included in standard behavioral treatments, but that have strong theoretical and empirical associations with changes in drinking and with recovery. Given the focus on increasing positive activities and future orientation, this intervention could fit well with a variety of treatment models. Our results suggest that a brief, single-session behavioral economic intervention with remotely delivered booster contact may reduce behavioral economic indices of alcohol demand and proportionate substance-related reinforcement. The results of this pilot trial, in conjunction with an extensive body of laboratory and clinical research linking behavioral economic mechanisms of change to alcohol and drug use, provide initial support for further investigation on the utility of the SFAS as an adjunctive intervention for AUD treatment.
Highlights:
Feasibility and acceptability of behavioral economic (BE) intervention in AUD treatment.
The intervention lowered substance-related reward and alcohol demand.
There is initial support for targeting BE mechanisms of change in alcohol treatment.
Acknowledgments
This research was supported by funding from NIAAA (F31 AA024381, PI: Meshesha; T32 AA007459, PI: Monti)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acuff SF, MacKillop J, & Murphy JG (2018). Applying behavioral economic theory to problematic Internet use: An initial investigation. Psychology of Addictive Behaviors, 32(7), 846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acuff SF, Amlung M, Dennhardt AA, MacKillop J, & Murphy JG (2019). Experimental Manipulations of Behavioral Economic Demand for Addictive Commodities: A Meta-Analysis. Addiction. 10.1111/add.14865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anton RF, O’Malley SS, Ciraulo DA, Cisler RA, Couper D, Donovan DM, … & Longabaugh R. (2006). Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. Jama, 295(17), 2003–2017. [DOI] [PubMed] [Google Scholar]
- Bandyopadhyay D, DeSantis SM, Korte JE, & Brady KT (2011). Some considerations for excess zeroes in substance abuse research. The American Journal of Drug and Alcohol Abuse, 57(5), 376–382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus ΜN, MacKillop J, & Murphy JG (2014). The behavioral economics of substance use disorders: reinforcement pathologies and their repair. Annual Review of Clinical Psychology, 10, 641–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bickel WK, Mellis AM, Snider SE, Athamneh LN, Stein JS, & Pope DA (2018). 21st century neurobehavioral theories of decision making in addiction: Review and evaluation. Pharmacology Biochemistry and Behavior, 164, 4–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bujarski S, MacKillop J, Ray LA (2012) Understanding naltrexone mechanism of action and pharmacogenetics in Asian Americans via behavioral economics: a preliminary study. Experimental Clinical Psychopharmacology, 20, 181–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll ΜE, Anker JJ, & Perry JL (2009). Modeling risk factors for nicotine and other drug abuse in the preclinical laboratory. Drug and Alcohol Dependence, 104, S70–S78. [DOI] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2015). Behavioral health trends in the United States: Results from the 2014 National Survey on Drug Use and Health (HHS Publication No. SMA 15–4927, NSDUH Series H-50).
- Collins DJ, Lapsley HM, LeCavalier J, & Single E (2000). Introduction: Improving economic data to inform decisions in drug control. Bulletin on Narcotics, 52(1), 1–20. [Google Scholar]
- Correia CJ, Carey KB, Simons J, & Borsari BE (2003). Relationships between binge drinking and substance-free reinforcement in a sample of college students: A preliminary investigation. Addictive Behaviors, 28(2), 361–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Correia CJ, Benson TA, & Carey KB (2005). Decreased substance use following increases in alternative behaviors: A preliminary investigation. Addictive Behaviors, 20(1), 19–27. [DOI] [PubMed] [Google Scholar]
- Corrao G, Bagnardi V, Zambon A, & La Vecchia C (2004). A meta-analysis of alcohol consumption and the risk of 15 diseases. Preventive Medicine, 28(5), 613–619. [DOI] [PubMed] [Google Scholar]
- Daniel TO, Stanton CM, & Epstein LH (2013). The future is now: Reducing impulsivity and energy intake using episodic future thinking. Psychological Science, 24(11), 2339–2342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughters SB, Magidson JF, Anand D, Seitz-Brown CJ, Chen Y, & Baker S (2018). The effect of a behavioral activation treatment for substance use on post-treatment abstinence: A randomized controlled trial. Addiction, 112(3), 535–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennhartd AA, Yurasek AM, & Murphy JG (2015). Change in delay discounting and substance reward value following brief alcohol and drug intervention. Journal of the Experimental Analysis of Behavior, 102, 125–140 [DOI] [PubMed] [Google Scholar]
- First MB (2014). Structured Clinical Interview for the DSM (SCID). The Encyclopedia of Clinical Psychology, 1–6. [Google Scholar]
- Gray JC, Amlung MT, Acker JD, Sweet LH, & MacKillop J (2014). Item-based analysis of delayed reward discounting decision making. Behavioural Processes, 103, 256–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Heil SH, & Lussier JP (2004). Clinical implications of reinforcement as a determinant of substance use disorders. Annual Review of Psychology, 55, 431–461 [DOI] [PubMed] [Google Scholar]
- Koffamus MN, Franck CT, Stein J, Bickel WK, 2015. A modified exponential behavioral economic demand model to better describe consumption data. Experimental and Clinical Psychopharmacology, 23, 504–512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koob GF (2006). The neurobiology of addiction: A neuroadaptational view relevant for diagnosis. Addiction, 101(s1), 23–30. [DOI] [PubMed] [Google Scholar]
- Longabaugh R, Donovan DM, Karno MP, McCrady BS, Morgenstern J, & Tonigan JS (2005). Active ingredients: How and why evidence-based alcohol behavioral treatment interventions work. Alcoholism: Clinical and Experimental Research, 29(2), 235–247. [DOI] [PubMed] [Google Scholar]
- MacKillop J, & Kahler CW (2009). Delayed reward discounting predicts treatment response for heavy drinkers receiving smoking cessation treatment. Drug and Alcohol Dependence, 104(3), 197–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, & Murphy JG (2007). A behavioral economic measure of demand for alcohol predicts brief intervention outcomes. Drug and Alcohol Dependence, 89, 227–233. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Murphy JG, Tidey JW, Kahler CW, Ray LA, & Bickel WK (2009). Latent structure of facets of alcohol reinforcement from a behavioral economic demand curve. Psychopharmacology, 203(1), 33–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M, Kiluk BD, McCrady BS, Tonigan JS, & Longabaugh R (2015). Active ingredients of treatment and client mechanisms of change in behavioral treatments for alcohol use disorders: Progress 10 years later. Alcoholism: Clinical and Experimental Research, 59(10), 1852–1862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M, & Ray LA (2009). Cognitive-behavioral treatment with adult alcohol and illicit drug users: a meta-analysis of randomized controlled trials. Journal of Studies on Alcohol and Drugs, 70(4), 516–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Smith AE, & Murphy JG (2013). The efficacy of single-component brief motivational interventions among at-risk college drinkers. Journal of Consulting and Clinical Psychology, 57(4), 691–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR (2017). Making the hard work of recovery more attractive for those with substance use disorders. Addiction, 112(5), 751–757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, & Rollnick S (2012). Motivational interviewing: Helping people change. New York, NY: Guilford Press. [Google Scholar]
- Miller WR, & Wilboume PL (2002). Mesa Grande: a methodological analysis of clinical trials of treatments for alcohol use disorders. Addiction, 97(3), 265–277. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Manuel JK, & Ernst D (2014) Motivational Interviewing Treatment Integrity Coding Manual 4.2.1. Unpublished manual. [Google Scholar]
- Murphy JG, Correia CJ, Colby SM, & Vuchinich RE (2005). Using behavioral theories of choice to predict drinking outcomes following a brief intervention. Experimental and Clinical Psychopharmacology, 13(2), 93–101. [DOI] [PubMed] [Google Scholar]
- Murphy JG, & MacKillop J (2006). Relative reinforcing efficacy of alcohol among college student drinkers. Experimental and Clinical Psychopharmacology, 14(2), 219–227. [DOI] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Borsari B, Barnett NP, Colby SM, & Martens MP (2012a). A randomized controlled trial of a behavioral economic supplement to brief motivational interventions for college drinking. Journal of Consulting and Clinical Psychology, 80(5), 876–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Martens MP, Borsari B, Witkietwitz K, & Meshesha LZ (2019). A randomized clinical trial evaluating the efficacy of a brief alcohol intervention supplemented with a substance-free activity session or relaxation training. Journal of Consulting and Clinical Psychology. DOI: 10.1037/ccp0000412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AD, Yurasek AM, Skidmore JR, Martens MP, MacKillop J, & McDevitt-Murphy ME (2015). Behavioral economic predictors of brief alcohol intervention outcomes. Journal of Consulting and Clinical Psychology, 83 (6), 1033–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Skidmore JR, Dennhardt AA, Martens MP, Borsari B, Barnett NP, & Colby SM (2012b). A behavioral economic supplement to brief motivational interventions for college drinking. Addiction Research & Theory, 20(6), 456–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Sleep Foundation (2015). Sleep Hygiene. Retrieved from https://sleepfoundation.org/ask-the-expert/sleep-hygiene
- Rehm J, Dawson D, Frick U, Gmel G, Roerecke M, Shield KD, & Grant B (2014).Burden of disease associated with alcohol use disorders in the United States. Alcoholism: Clinical and Experimental Research, 55(4), 1068–1077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rung JM, & Madden GJ (2018). Experimental reductions of delay discounting and impulsive choice: A systematic review and meta-analysis. Journal of Experimental Psychology: General, 147(9), 1349–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rung JM, Peck S, Hinnenkamp JE, Preston E, & Madden GJ (2019). Changing delay discounting and impulsive choice: Implications for addictions, prevention, and human health. Perspectives on Behavior Science, 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL & Graham JW (2002) Missing data: Our view of the state of the art. Psychological Methods, 7, 147–177. [PubMed] [Google Scholar]
- Smith CL, & Hantula DA (2008). Methodological considerations in the study of delay discounting in intertemporal choice: A comparison of tasks and modes. Behavior Research Methods, 40(4), 940–953. [DOI] [PubMed] [Google Scholar]
- Snider S, LaConte SM, & Bickel WK (2016). Episodic future thinking: Expansion of the Temporal window in individuals with alcohol dependence. Alcoholism Clinical and Experimental Research, 40 (7), 1558–1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, & Sobell MB (1996). Timeline followback user’s guide: A calendar methodfor assessing alcohol and drug use. Toronto: Addiction Research Foundation. [Google Scholar]
- Solinas M, Chauvet C, Thiriet N, El Rawas R, & Jaber M (2008). Reversal of cocaine addiction by environmental enrichment. Proceedings of the National Academy of Sciences, 105(44), 17145–17150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soltis KE, Acuff SF, Dennhardt AA, Borsari B, Martens MP, & Murphy JG (2018). Self-regulation as a mediator of the effects of a brief behavioral economic intervention on alcohol-related outcomes: A preliminary analysis. Experimental and Clinical Psychopharmacology, 26(4), 347–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein JS, Koffarnus MN, Snider SE, Quisenberry AJ, & Bickel WK (2015). Identification and management of nonsystematic purchase task data: Toward best practice. Experimental and Clinical Psychopharmacology, 23(5), 377–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein JS, Tegge AN, Turner JK, & Bickel WK (2018). Episodic future thinking reduces delay discounting and cigarette demand: An investigation of the good-subject effect. Journal of Behavioral Medicine, 41(2), 269–276. [DOI] [PubMed] [Google Scholar]
- Tabachnick B & Fidell L (2013) Using Multivariate Statistics. 6th ed. Boston, MA: Pearson. [Google Scholar]
- United States Department of Agriculture Food and Nutrition Service (2015). Choose My Plate. Retrieved from http://www.choosemyplate.gov/.
- Volkow ND, & Baler RD (2014). Addiction science: Uncovering neurobiological complexity. Neuropharmacology, 76, 235–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson KG, Sandoz EK, Kitchens J, & Roberts M (2010). The Valued Living Questionnaire: Defining and measuring valued action within a behavioral framework. The Psychological Record, 60(2), 249–272. [Google Scholar]
- Yu J, Liu L, Collins RL, Vincent PC, Epstein LH, 2014. Analytical problems and suggestions in the analysis of behavioral economic demand curves. Multivariate Behavioral Research, 49, 178–192. [DOI] [PubMed] [Google Scholar]


