Abstract
The support offered to mothers after hospital discharge can be decisive in maintaining exclusive breastfeeding during the first 6 months post‐partum. The objective of this study was to assess the impact on the duration of exclusive breastfeeding of a participatory intervention using an online social network. A randomized clinical trial was performed involving 251 mother–child pairings in a university hospital in the Northeast of Brazil, 123 of which assigned to the intervention group and 128 to the control group. After hospital discharge, the intervention group was followed through a closed group of an online social network, where weekly posters were published on topics related to breastfeeding and an active communication was established with the mothers. The groups were interviewed monthly over the phone until the child reached 6 months of age. The duration of exclusive breastfeeding was calculated through survival analysis, and the effect of the intervention was estimated through the Cox regression model. The exclusive breastfeeding frequencies were higher in the intervention group in all follow‐up months, reaching 33.3% in the sixth month versus 8.3% in the control group. The median exclusive breastfeeding duration was 149 days (95% CI [129.6, 168.4]) in the intervention group and 86 days (95% CI [64.9, 107.1]) in the control group (P < 0.0001). The proportional risk of early interruption of exclusive breastfeeding was 0.38 (95% CI [0.28, 0.51], P < 0.0001). This intervention had a positive impact on the duration and frequency of exclusive breastfeeding.
Keywords: breastfeeding, clinical trial, health education, puerperium, social media, social support
Key messages.
Participatory strategies in virtual communities have shown great potential in the promotion and support of exclusive breastfeeding (EBF).
The support provided by health professionals through an online social network to breastfeeding women after hospital discharge significantly increased the duration of EBF.
The intervention performed in this clinical trial, with the inclusion of mothers in a group of an online social network promoted by health professionals, reduced the early interruption rates of EBF during the first 6 months of life by 62% when compared with mothers who did not participate in this group.
1. INTRODUCTION
Brazil has had many successful experiences promoting, protecting, and supporting the practice of breastfeeding, which have served as examples for many other countries (Müller, Rea, & Monteiro, 2014; Pittas & Dri, 2017; Sousa, Claro, Sousa, Lima, & Santana, 2015). Cross‐sector actions undertaken in a coordinated fashion—described as a model of gears—have succeeded in increasing both the duration of total breastfeeding and the exclusive breastfeeding (EBF) of children under 6 months of age (Pérez‐Escamilla, Curry, Minhas, Taylor, & Bradley, 2012).
National data reveal that in the 1970s, the median duration of breastfeeding was little over 2 months whereas it rose to almost 6 months at the end of the 1980s (Venancio & Monteiro, 1998). The last two Brazilian studies on the prevalence of breastfeeding carried out in 1999 and 2008 recorded an increase of 30.7 days in the median duration of EBF and of 45.7 days in median total breastfeeding (BF), with the median times of 54.1 days for EBF and 341.6 days for BF being observed in 2008 (Venancio, Escuder, Saldiva, & Giugliani, 2010).
Despite the significant improvement in the practice of breastfeeding, however, a meta‐analysis showed that the EBF median in Brazil had no major advances in recent years, remaining at 55.4 days (95% CI [31.9, 78.91]; Pereira‐Santos et al., 2017). Another recent study conducted with secondary data from recent national surveys revealed a stagnation in the prevalence of EBF at the sixth month of the child's life between 2006 and 2013, remaining at 36.6% (Boccolini, de Moraes Mello Boccolini, Monteiro, Venâncio, & Giugliani, 2017). This prevalence is similar to low‐ and middle‐income countries, where only 37% of children under 6 months are estimated to receive EBF. The situation is even worse in high‐income countries (Victora et al., 2016).
Because of the importance of EBF during the first 6 months of the child's life for the health of both mother and child, in the short and long term (American Academy of Pediatrics, 2012; Victora et al., 2016), and because of the lack of progress in this practice in the last decade, effective actions need to be identified that encourage mothers to give EBF for longer periods.
Studies have shown that the support offered to mothers after hospital discharge can be decisive for the establishment of breastfeeding and the improvement of breastfeeding rates (Fu et al., 2014; Harari et al., 2018; Patel & Patel, 2016). The use of new technologies related to the Internet can also help mothers during this period (Ahmed, Roumani, Szucs, Zhang, & King, 2016; Giglia, Cox, Zhao, & Binns, 2015).
In this context, the objective of this study was to evaluate the effectiveness of a participatory intervention promoted by health professionals on the duration of EBF during the first six months of the child's life using an online social network.
2. METHODS
2.1. Study design and participants
This study is a single‐blind, randomized clinical trial with the parallel follow‐up of two groups consisting of mother–child pairings assisted in the maternity ward of the Hospital Universitário Lauro Wanderley (HULW), a hospital that is part of the Baby‐friendly Hospital Initiative and located in the city of Joao Pessoa‐PB, in the northeast region of Brazil. The intervention of this clinical trial was performed through a participatory strategy on an online social network. The study lasted 12 months, beginning in August 2016.
The mothers included in the study gave birth during the recruitment period, between August 2016 and February 2017, were over 18 years of age, knew how to read and write, used the online social network Facebook, and were discharged from the hospital together with their child. The exclusion criteria of the study were mothers who distanced themselves from their child for any reason throughout the study; who were HIV seropositive or had any other diseases that contraindicated breastfeeding; and who gave premature birth with infants with low birth weight, twins, or with congenital problems that prevented or hindered suckling at the breast.
2.2. Calculation of the sample size
The following factors were considered to calculate the sample: the last available estimate of the prevalence of EBF in children younger than 6 months in the city of João Pessoa, which was 39.1% in the year 2008 (Venancio et al., 2010), a significance level of 5%, a test's power of 80%, and an increase of 20% in the prevalence of EBF in the intervention group (IG). Based on these parameters, it is estimated that 107 mother–child pairings would be necessary in each group, intervention and control (Dean, Sullivan, & Soe, 2013). Fifteen percent were added to the original estimate to account for the possible losses in follow‐up, reaching a total of 246 mother–child pairings.
The final clinical trial was composed of 251 mother–child pairings, 123 in the IG and 128 in the control group (CG).
2.3. Research team
The research team was made up of academics of the nutrition, nursing, social work, and psychology courses (n = 18), nutritionists (n = 5), paediatricians (n = 2), and supervising professors (n = 2) of the Universidade Federal da Paraíba, João Pessoa, Brazil. Two nutritionists of this team were responsible for coordinating the project. The training of the team took place from March to July 2016, ensuring a training of at least 20 hr on all data collection procedures and the research logistics.
2.4. Resources and techniques used in the research
2.4.1. Phone interviews
Phone calls were carried out monthly during the 6 months post‐partum to collect the necessary data through interviews with the women who participated in this study.
The calls were made from an exclusive mobile phone number associated with the study so the mothers could identify the number whenever they received the monthly calls.
2.4.2. Booklet on the breastfeeding practice
The educational part of the study was performed with the aid of a booklet with information on breastfeeding developed by the research team and based on the official recommendations of the Brazilian Ministry of Health and the World Health Organization (Ministério da Saúde, 2015a, 2015c; World Health Organization, 2009). The messages were illustrated, direct and easy to read and understand. All mothers received the same booklet after birth while they were still in the maternity ward in order to provide the same information to the CG and IG.
The booklet was drafted collectively in the period from January to July 2016 by a multidisciplinary team of 30 people, the participants of the project's team.
By consensus, 24 topics were selected to make up the booklet (Table 1). The final content of each topic was exhaustively discussed, and the entire team was trained to advise the mothers on these matters. A specialist in graphic arts made the final artwork of the booklet.
Table 1.
Subjects of the booklet published on the online social network in accordance with the week of follow‐up of the mothers in the intervention group
| Week of follow‐up | Subjects |
|---|---|
| 1st week | Milk let‐down |
| 2nd week | Benefits of breastfeeding |
| 3rd week | The importance of exclusive breastfeeding until the sixth month |
| 4th week | Correct latching |
| 5th week | Why artificial teats, bottles and pacifiers should be avoided? |
| 6th week | Breastfeeding positions |
| 7th week | Time and duration of the feedings |
| 8th week | Production and aspects of breast milk |
| 9th week | What to do to have a lot of milk? |
| 10th week | Escape from the myths |
| 11th week | Caring for your breasts |
| 12th week | Clogged milk and mastitis |
| 13th week | Candidiasis, fissures or cracks |
| 14th week | Milking the milk |
| 15th week | Preserving the milk after milking |
| 16th week | Human milk banks |
| 17th week | What does breast milk contain? |
| 18th week | The nutrition of the mother |
| 19th week | Maternal diet and milk production |
| 20th week | Until when should you breastfeed? |
| 21st week | When can the baby eat other foods? |
| 22nd week | The importance of complementary food |
| 23rd week | How should the complementary feeding be done? |
| 24th week | Responsible feeding |
2.4.3. Participative methodology on the online social network
The IG was included in a closed group called Projeto Amamenta Mamãe (Mama Breastfeeding Project) on the online social network Facebook (https://www.facebook.com/groups/279662129036687/), ensuring the privacy of participants and of all their posts or comments.
The intervention was structured in a pedagogical manner, collaborating in the critical and reflective construction of the content made available on the network, based on the topics of the booklet, and it lasted 24 weeks for each mother.
2.5. Pilot study
A pilot study was performed with a duration of 2 months with the participation of 20 mother–child pairings, with 10 pairings assigned to each group (intervention and control) to test and evaluate all methodological procedures of the study. The recruitment occurred in the maternity ward of the HULW and the follow‐up time was 1 month. The mothers who participated in this step were not included in the final study.
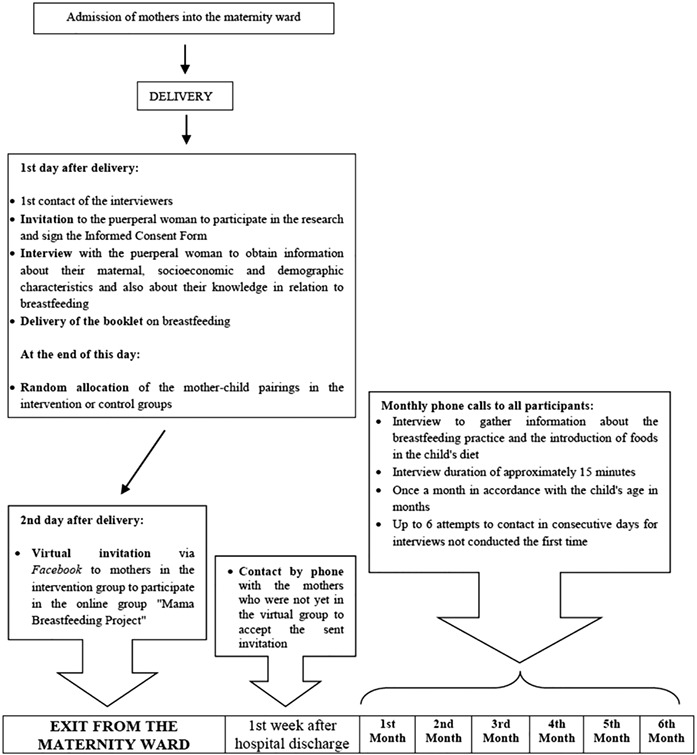
2.6. Recruitment and follow‐up of the mother–child pairings
The recruitment of the mother–child pairings and the development of all data collection procedures were done by the academics of the project team, under the supervision of the medical professionals and nutritionists of the HULW (Appendix A).
All women admitted at the maternity ward of the HULW were registered sequentially through a form developed for the recruitment. The inclusion criteria related to the mother were recorded at admission and those of the babies were checked immediately after birth.
Women who met the inclusion criteria and agreed to participate in the study were interviewed at the ward on the day following the baby's birth, in order to obtain information on the maternal, socio‐economic and demographic characteristics of the mother–child pairing, and their knowledge about breastfeeding. In addition, health and obstetric data were collected from the medical records, record books, or the prenatal care card.
During their stay at the hospital, the mothers received routine guidance from the care team about breastfeeding and the general care for the newborn, in addition to being assisted in accordance with their needs, as is usually done in public health services in Brazil. They also received the booklet on the practice of breastfeeding with explanations according to their questions and demands.
At the end of each day, one nutritionist of the project team performed the random assignment of the mother–child pairing in the CG or IG based on a list of random, binary numbers drawn up before the beginning of the study, using the function “random between 0 and 1” of the Microsoft Excel software. The correspondence of the recruitment order with the order of the numbers from the predefined list determined in which group the woman would be assigned, with the value “0” being assigned to the CG and “1” to the IG, characterizing a simple randomization. The academics who performed the recruitment did not participate in the assignment process of the women into groups, and the nutritionist who performed the assignment had no knowledge of or contact with the mothers during the recruitment stage. The participant mothers were not aware that there were two groups in the study and also did not know to which group they had been assigned.
The inclusion of the mothers in the IG in the closed online social network group was done on the day following the recruitment, before the discharge from the maternity ward, which occurred 48 hr after childbirth. Each woman received a virtual invitation that she should accept to allow her inclusion in that group.
Phone calls were made to each mother who still had not accepted the invitation to this group 1 week after hospital discharge in an attempt to convince her to accept the invitation. Eleven mothers did not accept the invitation. The recruitment happened until the sample size for the study was reached.
All of the mother–child pairings were followed monthly until the sixth month post‐partum after hospital discharge through phone calls with a duration of approximately 15 min. Information was collected on breastfeeding and the introduction of complementary foods referring to the previous day in order to identify the status of breastfeeding.
The phone interviews were scheduled in advance, and up to six contact attempts were made on consecutive days before the information was considered as lost. A contact was once again attempted in the following month for the mothers who had not been contacted in the previous month. If successful, these cases were not counted as losses.
The coordinators of the project reviewed the data collection forms obtained with the phone interviews, checking the answers according to the validation rules built into the questionnaire itself.
The IG of this study was followed after hospital discharge for a period of 6 months in a closed group of the online social network. The women were tagged in a post of the group, corresponding to a topic of the booklet, once each week, according to the week of entry into the group (Table 1). The post had messages of encouragement and clarification. A conversation was promoted through this tagging, which encouraged the mothers to raise doubts, comment on something, or share their experiences on the specific topic of the poster or another topic that could be important for them at that time. Each tag or participation in the group generated an automatic and immediate notification on the personal profile of each woman, enabling communication in real time.
The messages were monitored by the project team, which accompanied each view by the women, and when this did not happen in up to 5 days, a private message was sent by the same online social network inviting the woman to view that particular post.
The control of entries, taggings, and views of the mothers was performed with the aid of online applications: electronic spreadsheets and schedules, shared between the researchers and monitored daily by the coordinators of the project. Each mother was registered in the spreadsheet with the data for her identification, date of entry and registration for participation in the group. The registration in the schedule for the tagging of the mothers in the posters was performed immediately after the entry of the mother in the group.
The questions and demands of the mothers were answered virtually by the research team and supervised by the coordinators of the project. All the answers were given as soon as possible after the question was made by the woman. The project team also established an active communication among its members through the exchange of instant messages in an exclusive online group for the discussion and guidance of unique and appropriate responses.
2.7. Study variables
The maternal, socio‐economic, and characteristics of the population were described through the women's age, maternal schooling in years of study, marital status (living with or without partner), occupation (paid work or does not work outside the home), home ownership, and per capita income.
With respect to the health and obstetric conditions, the number of antenatal consultations, parity (primiparous or multiparous women), type of delivery (normal or caesarean), birth weight, and sex of the newborn were checked.
The practice of EBF (dependent variable) was verified on a monthly basis in accordance with the food consumption data of the newborn contained in the monthly telephone interview forms. The food consumption markers for children under 6 months proposed by the Ministry of Health (Ministério da Saúde, 2015b) were used to verify the foods consumed on the day before and the questions allowed for the evaluation of the breastfeeding practice and the early introduction of food. As such, the mother was first asked if the baby was being breastfed. If so, she was also asked if—in the last month—the baby consumed any other food besides breast milk (porridge, water, tea, cow's milk, infant formula, fruit juice, fruit, warm food, or other foods). If the child had consumed other food in the last month, then the same question was asked about the previous day. If the child was not being breastfed or received other foods during the month, then the date of the interview of the previous month was recorded as the date of weaning or of the interruption of EBF, respectively.
2.8. Data processing and analysis
The data were doubly entered into an electronic spreadsheet, and the answers were then validated with the use of the logical commands false (different values) or true (equal values). The statistical analyses were performed with the aid of the Stata/SE software, version 14.2. The continuous variables data were first submitted to the Kolmogorov–Smirnov statistical test to evaluate the normality of its distribution. The categorical variables were described through their absolute and relative frequencies and the continuous variables through their means and standard deviations or medians and percentiles, characterizing the IG and CG. The EBF proportions between the groups, at each month of follow‐up, were compared with Pearson's chi‐square test.
The median duration and the frequency of EBF were calculated for the total sample and for each group through survival analysis using the Kaplan–Meier technique. The event “interruption of exclusive breastfeeding” was considered when the mother introduced any food other than breast milk, at which point both the time and the age of the child on the date of the last phone call were recorded. The cases in which the child was still on EBF at the end of 6 months of follow‐up, and in which the child dropped out of follow‐up (loss to follow‐up) before the end of the study while still receiving EBF were censored. In these cases the child's age was recorded at either the end of follow‐up or at the time of the last registered phone contact. In those cases where the introduction of some food was already recorded at the first call, the time of EBF was considered as 1 day.
The survival curves for each group—control and intervention—were developed and the log‐rank test was used to check the difference between the curves, considering a significance level of 5%. In the cases where such a difference was found, the assumption of proportional hazards was tested throughout the observation period based on the analysis of the residuals (George, Seals, & Aban, 2014). The difference between the groups was tested with respect to the other study variables for the possible inclusion of any other variable in the regression model if a significant difference was found according to the chi‐square test. A semiparametric Cox regression model was built to estimate the effect of the intervention on the duration of EBF. This model estimates the hazard ratio of the early interruption of EBF in mothers who received the intervention as compared with the other mothers.
2.9. Ethical aspects
The project “Effects of an online social network on promoting and supporting breastfeeding” was approved by the Ethics in Human Research Committee at the HULW with a submission certificate for ethical consideration (Portuguese acronym CAAE) with the no. 54328116.8.0000.5183, and it was included in the universal registry of clinical trials (UTN: U1111‐1187‐6136) in the International Clinical Trials Registry Platform—ICTRP (http://www.who.int/ictrp/en/) of the World Health Organization through the Brazilian Registry of Clinical Trials. Furthermore, the study followed the CONSORT 2010 guideline (Consolidated Standards of Reporting Trials; Moher et al., 2010).
The mothers in the IG and CG were continuously informed about their and their children's health, food, and nutrition data. In the case of the detection of any nutritional disorder or health problem of the mother–child pairing, the woman was told to seek care at the basic health unit closest to her residence for the proper management of the problem.
3. RESULTS
Of the 768 mothers who were admitted in the maternity ward during the recruitment period, 251 met the inclusion criteria and agreed to participate in the study, of which 123 were assigned to the IG and 128 to the CG. There were no losses in either group in the first month of follow‐up. In the course of the 6 months of follow‐up, there were eight losses, seven in the IG and one in the CG. The main reason for these losses was the refusal of the participant to continue the study. All individuals were included in the analyses and censored at the time of loss of follow‐up (Figure 1).
Figure 1.
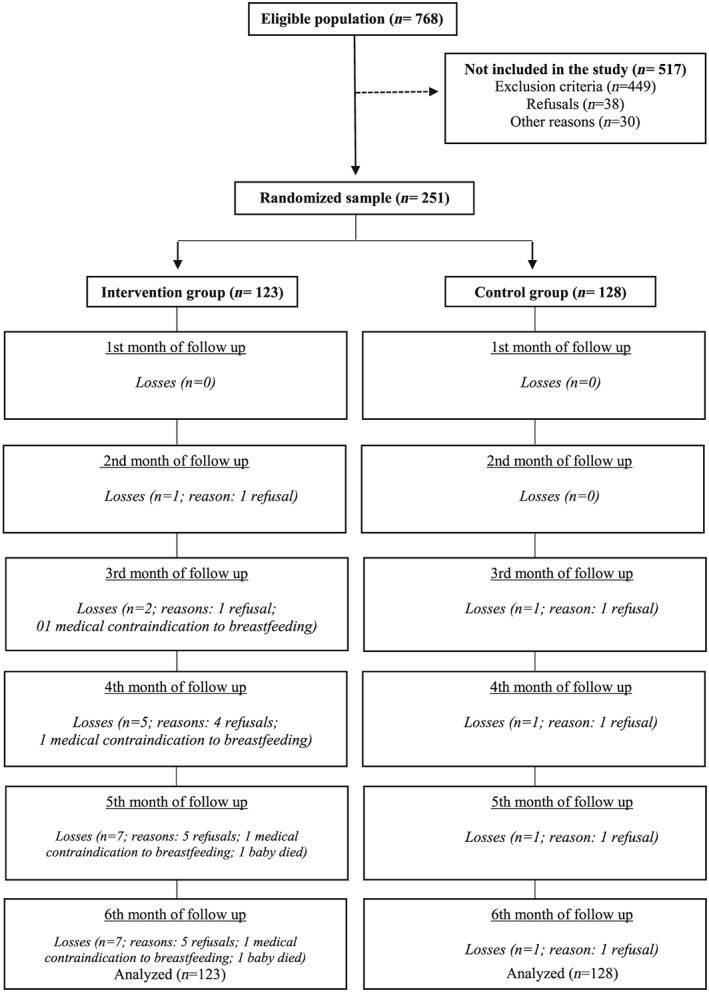
Flowchart of the randomized clinical trial
The maternal, socio‐economic, demographic, obstetric, and health characteristics of the mother–child pairing can be seen in Table 2. The number of prenatal consultations was the only variable with significant statistical difference between the groups. Most women were between 20 and 34 years of age (78% of the IG and 77.3% of the CG), had more than 11 years of schooling (73% of the IG and 72.4% of the CG), lived with a partner (88.6% of the IG and 88.3% of the CG), and in their own home (57.7% of the IG and 53.1% of the CG). As for the occupation of these women, 50.4% of the IG did not work outside of the home against 43% of the CG. With respect to the obstetric history, around half had already had another child (52.8% of the IG and 50% of the CG), more than half of the births were through caesarean section (52.8% of the IG and 61.7% of the CG), and the male sex was slightly more frequent in the newborns (51.2% of the IG and 53.1% of the CG). Most women went to more than six consultations during the prenatal care period (76.4% of the IG and 89.8% of the CG).
Table 2.
Maternal, socio‐economic, demographic, obstetric condition and health characteristics of the mother–child pairings for the intervention and control groups
| Variables | Intervention group (n = 123) | Control group (n = 128) | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Maternal, socio‐economic, and demographic characteristics | Age | ||||
| <20 years | 11 | 8.9 | 12 | 9.4 | |
| 20–34 years | 96 | 78.1 | 99 | 77.3 | |
| >35 years | 16 | 13.0 | 17 | 13.3 | |
| Median (p.25 and p.75) | 26 (22–32) | 27 (23–32) | |||
| Years of schooling | |||||
| ≤8 years | 14 | 11.5 | 13 | 10.2 | |
| 9–11 years | 19 | 15.6 | 22 | 17.3 | |
| ≥12 years | 89 | 73.0 | 92 | 72.4 | |
| Median (p.25 and p.75) | 12 (11–12) | 12 (10–13) | |||
| Lives with partner | |||||
| Yes | 109 | 88.6 | 113 | 88.3 | |
| No | 14 | 11.4 | 15 | 11.7 | |
| Occupation | |||||
| Paid work | 61 | 49.6 | 73 | 57.0 | |
| Does not work outside of home | 62 | 50.4 | 55 | 43.0 | |
| Own home | |||||
| Yes | 71 | 57.7 | 68 | 53.1 | |
| No | 52 | 42.3 | 60 | 46.9 | |
| Per capita income (R$) | |||||
| Median (p.25 and p.75) | 400 (293.3–586.7) | 352 (293.3–543.3) | |||
| Obstetric and health conditions | No. of prenatal consultations | ||||
| <6 | 29 | 23.6 | 13 | 10.2 | |
| ≥6 | 94 | 76.4 | 115 | 89.8 | |
| Median (p.25 and p.75) | 8 (6–9) | 9 (7–10) | |||
| Parity | |||||
| Primiparous | 58 | 47.2 | 64 | 50.0 | |
| 2 or more | 65 | 52.8 | 64 | 50.0 | |
| Type of delivery | |||||
| Normal | 58 | 47.2 | 49 | 38.3 | |
| Caesarean section | 65 | 52.8 | 79 | 61.7 | |
| Birth weight (g) | |||||
| Mean ± SD | 3,420.5 ± 441.2 | 3,444.8 ± 495.2 | |||
| Child's sex | |||||
| Female | 60 | 48.8 | 60 | 46.9 | |
| Male | 63 | 51.2 | 68 | 53.1 | |
Note. SD: standard deviation; p.25: 25 percentile; p.75: 5 percentile.
The EBF proportions during every month of follow‐up between the groups can be seen in Table 3. The IG had higher EBF percentages throughout the follow‐up period of the study as compared with the CG. These percentages underwent declines each month in both groups, and at the sixth month of follow‐up, the smallest proportions of EBF were observed in both groups, 33.3% in the IG versus 8.3% in the CG (P < 0.001).
Table 3.
Comparison of the exclusive breastfeeding proportions between the intervention and control group in the months of follow‐up of the mother–child pairings
| Follow‐up period | Exclusive breastfeeding | ||||
|---|---|---|---|---|---|
| Intervention group | Control group | P value | |||
| n | % | n | % | ||
| 1st month | 113 | 91.9 | 106 | 82.8 | 0.031 |
| 2nd month | 110 | 90.9 | 78 | 61.4 | 0.000 |
| 3rd month | 99 | 83.9 | 65 | 53.7 | 0.000 |
| 4th month | 80 | 69.6 | 41 | 33.9 | 0.000 |
| 5th month | 59 | 53.6 | 25 | 20.7 | 0.000 |
| 6th month | 38 | 33.3 | 10 | 8.3 | 0.000 |
The result of the survival analysis using the Kaplan–Meier technique estimated that the EBF median of the entire sample was 117 days (95% CI [101.5, 132.5]). When the time of EBF interruption in each group is analysed, one can see that the median EBF duration in the IG was 63 days longer than in the CG: 149 days for the IG (95% CI [129.6, 168.4]) versus 86 days for the CG (95% CI [64.9, 107.1]). This difference was statistically significant according to the log‐rank test, P < 0.0001.
Figure 2 shows the survival curves of the EBF duration time during the infants' first 6 months of life (n = 251, 191 events and 60 censored events). A proportional behaviour of the curves could be observed, with a sharp decline in the CG when compared with the IG. The semiparametric Cox regression model estimated the proportional hazard of the early interruption of EBF as hazard ratio: 0.38 (95% CI [0.28, 0.51], P < 0.0001), demonstrating that the intervention was a protective factor that reduced the early interruption rates of EBF during the first 6 months by 62% when compared with the CG. Considering a sample size of 251 cases with two groups of similar sizes, this effect has a test power equal to approximately 1.
Figure 2.
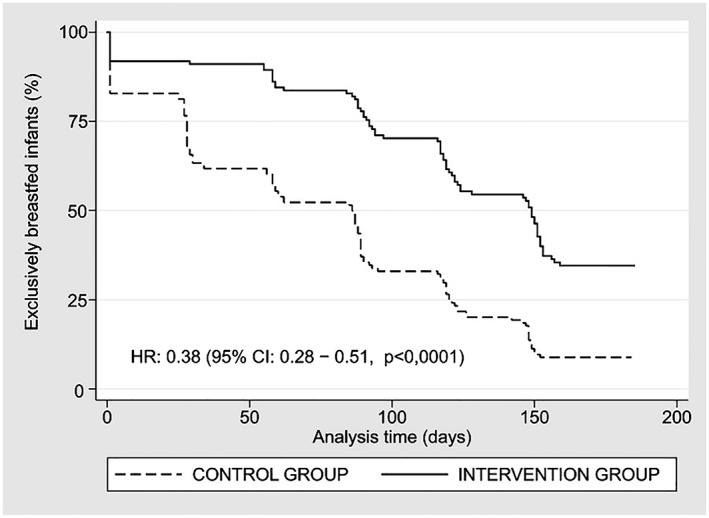
Survival curves of the duration of exclusive breastfeeding (EBF). HR: hazard ratio; CI: confidence interval; p = P value
4. DISCUSSION
The findings of this study strengthen the evidence that the appropriate promotion and support to puerperal women, at the appropriate time after hospital discharge, increase the EBF rates and durations.
The data from Brazil show that the practice of breastfeeding increased expressively between 1986 and 2006, after which the trend virtually stagnated, with a slight decline in the prevalence in the first months of a child's life, in contrast to a small increase after 18 months of age. The national health survey conducted in 2013 reported a prevalence of 36.6% and 52.1% for EBF at 6 months and total breastfeeding at 24 months of age, respectively (Boccolini et al., 2017). In the city of João Pessoa, the available data are from a survey carried out in 2008, in which a prevalence of 39.1% was observed for EBF at 6 months (Ministério da Saúde, 2009).
The results obtained in this study are from a longitudinal study with literate mothers coming from a hospital participating in the Baby‐friendly Hospital Initiative. Its estimates are therefore not comparable with those obtained in cross‐sectional studies. However, the results it found of 33.3% of children under 6 months of age receiving EBF are positive, especially when compared with the CG, but it is still short of the rate recommended by the World Health Organization (World Health Organization, 2003).
Some characteristics of the study population are widely described in the literature as protective factors for EBF (Boccolini, de Carvalho, & de Oliveira, 2015; Machado et al., 2014; Vieira et al., 2014; Warkentin, de Aguiar Carrazedo Taddei, de Jesus Viana, & Colugnati, 2013), including the age of the mothers with a predominance of the age cohort between 20 and 35 years, care in a hospital that is part of the Baby‐friendly Hospital Initiative, literacy of the mother with at least secondary education, mostly living with a partner in an own property and having been to an adequate number of prenatal care sessions with at least the minimum number of expected consultations. Even considering all these favourable characteristics and recognizing the similarity of the groups due to the randomization of the clinical trial, the median EBF time of the IG was higher than the CG, and this difference can be attributed exclusively to the participation of the mothers in the online social network using the proposed methodology and mediated by health professionals.
The puerperium is the period in which the main complications related to the establishment of breastfeeding happen, such as the difficulty of the baby to latch, pain in the breasts, cracked nipples, breast engorgement, sensation of insufficient milk, tiredness, among many other real possibilities (Li, Fein, Chen, & Grummer‐Strawn, 2008). During this period, women are known to face situations of emotional instability and insecurity, which may increase doubts, fears, and anxieties (Marques, Cotta, Botelho, et al., 2010; Marques, Cotta, Magalhães, et al., 2010). The lack of support or timely clarification brings with it the risk that the woman does not overcome these difficulties, thus compromising the breastfeeding process and leading to the early interruption of EBF or to full weaning (Brand, Kothari, & Stark, 2011).
The emotional support offered by health professionals and the promotion of the self‐confidence of the mother regarding her ability to breastfeed are important components for successful breastfeeding (Wood, Woods, Blackburn, & Sanders, 2016). The methodology adopted in the IG of this clinical trial used a participatory approach, exploring the educational context for the promotion of breastfeeding through the weekly publication of posters on topics relevant to the practice of breastfeeding, which encouraged conversations between members of the group and enabled the sharing of knowledge, the building of relationships, and the mutual identification of experiences and learnings.
Another important component was the immediate and appropriate support to help women overcome the difficulties they were experiencing and transmitting, in addition to the knowledge and messages of confidence and encouragement regarding their actual ability to face the challenges ahead of them. This component was always strengthened by the support of the group through the sharing of experiences, enabling the mothers to participate actively in this process and consequently to be better able to adhere and continue the EBF practice.
As such, the intervention of this study was based on a continuous interactive education process of groups involving participants in their real‐life situations and experiences, within their context and in accordance with their needs, always mediated by a health professionals trained for this task.
Breastfeeding support strategies that are geared to transmitting only technical‐scientific knowledge and do not address the subjectivities and realities of each woman are superficial, unsatisfactory for integral care and do not meet the diverse needs of these women, increasing their feelings of guilt and responsibility for the challenges faced in the breastfeeding period (Alves et al., 2017; de Almeida, de Araújo Barros Luz, & da Veiga Ued, 2015; Lima, dos Santos, Erdmann, & de Souza, 2018).
On the other hand, the experiences described in the literature confirm that intervention strategies based on the support to the breastfeeding woman, developed in a pedagogical and participatory manner by health professionals, stimulate the dialogue and interaction between the subjects (da Silva, de Lima, & Osório, 2016; Monte, Leal, & Pontes, 2013; Silva et al., 2016), and they also confirm that the timely support in the post‐partum period has a positive impact on the practice of EBF (Aksu, Küçük, & Düzgün, 2011; Fu et al., 2014; Kronborg, Vaeth, Olsen, Iversen, & Harder, 2007; Patel & Patel, 2016; Sheehan, Schmied, & Barclay, 2009).
The use of mobile technologies and the Internet are viable, innovative, easy, accessible, and increasingly popular options (World Health Organization, 2011). In the case of breastfeeding women, these technologies are offering information and support through the formation of networks of people, promoting breastfeeding, especially EBF (Ahmed et al., 2016; Prates et al., 2015; Thomas & Shaikh, 2012). In practice, this form of interaction can help overcome difficulties and alleviate maternal worries, in addition to assisting in the sharing of knowledge and experiences, making post‐natal assistance more effective and humane (Ahmed et al., 2016; Harari et al., 2018; Thomas & Shaikh, 2012; World Health Organization, 2011).
Our study also corroborates the literature by demonstrating that the support offered in the online social network can help to alleviate the concerns of breastfeeding women (Wagner, Chantry, Dewey, & Nommsen‐Rivers, 2013); that the online social networks enable improvements in the communication between the professionals and lactating women, effectively strengthening the breastfeeding practice (Asiodu, Waters, Dailey, Lee, & Lyndon, 2015; Tomfohrde & Reinke, 2016); and, finally, that this tool overcomes the difficulties arising from the lack of time and resources to support breastfeeding women (Brown, Raynor, & Lee, 2011).
The intervention in this study does not require costly technologies or large investments in infrastructure. However, it does demand training and organization of the health care team for the online monitoring. In terms of equipment, only those already used by a large part of the population are required, that is, mobile phones connected to the Internet. As such, it is an initiative that can be replicated in other maternity wards in Brazil or other countries. For the health of the population, this intervention can have a big impact on improving breastfeeding indicators, which in turn triggers the positive effects of this practice already described in the scientific literature (American Academy of Pediatrics, 2012; Victora et al., 2016).
Even though the difficulty to access the internet may be a limitation for the multiplication of online social network groups mediated by health professionals for the promotion and support to breastfeeding, especially in poor populations, the expansion of the use of virtual communication technologies is inevitable. It should be noted that the expansion of connections through mobile devices—both for the sending of instant messages and the use of social networks—is a basic capability required for the implementation of this intervention (Brazilian Internet Steering Committee, 2017).
One limitation of this randomized study was that the research team knew which participants were included in each group. The study could not be double‐blind because of the health professionals' need for communication, both over the phone with all women, and through the virtual online social network with the women in the IG.
Another limitation involved not being able to obtain the exact date of the interruption of EBF, with the date of the phone contact of the month prior to the introduction of foods in the diet of the child being considered. The interruption of EBF may therefore have been underestimated—and not overestimated—by a maximum of 30 days. However, this lack of an accurate date also avoided false results regarding the success of the intervention.
The results of this randomized clinical trial make it possible to conclude that participatory and continuous strategies using innovative technologies, such as online social networks mediated by health professionals for the promotion and support to breastfeeding, can have a positive impact on the prevalence and duration of breastfeeding. This methodology to promote and support breastfeeding in the post‐natal period strengthens the tenth step for the success of breastfeeding in the Baby‐friendly Hospital Initiative (World Health Organization & UNICEF, 2009). New strategies and local subjects can further leverage this model for the use of online social networks according to the social and cultural characteristics and needs of the target population, always respecting the rights of women and infants. Longer lasting interventions are more effective in increasing the duration of EBF (Skouteris et al., 2014). Periods longer than 6 months of follow‐up can therefore also be adopted.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
DSC, MMO, and RPdTV conceived and designed the study. DSC and RPdTV analysed and interpreted the data. DSC and CSC assisted in the literature research and drafted the manuscript. All the authors contributed to the writing of the manuscript and critically reviewed its content and approved the final version submitted for publication.
ACKNOWLEDGMENTS
The authors would like to thank the students and the health professionals for their continuous support and active participation throughout the research.
APPENDIX A. FLOW DIAGRAM OF THE CONTACT STEPS BETWEEN RESEARCHERS AND RESEARCH PARTICIPANTS
Cavalcanti DS, Cabral CS, de Toledo Vianna RP, Osório MM. Online participatory intervention to promote and support exclusive breastfeeding: Randomized clinical trial. Matern Child Nutr. 2019;15:e12806 10.1111/mcn.12806
REFERENCES
- Ahmed, A. H. , Roumani, A. M. , Szucs, K. , Zhang, L. , & King, D. (2016). The effect of interactive web‐based monitoring on breastfeeding exclusivity, intensity, and duration in healthy term infants after hospital discharge. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 45(2), 143–154. 10.1016/j.jogn.2015.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aksu, H. , Küçük, M. , & Düzgün, G. (2011). The effect of postnatal breastfeeding education/support offered at home 3 days after delivery on breastfeeding duration and knowledge: A randomized trial. The Journal of Maternal‐Fetal & Neonatal Medicine, 24(2), 354–361. 10.3109/14767058.2010.497569 [DOI] [PubMed] [Google Scholar]
- Alves, T. , de Carvalho, J. B. L. , Cavalcante, R. D. , Teixeira, G. A. , da Silva, F. C. B. , de Oliveira, A. M. , & dos S. Silva, G. W. (2017). Influences of non‐accession to exclusive breastfeeding: Understanding of feminine subjectivity. International Archives of Medicine, 10, 1–9. [Google Scholar]
- American Academy of Pediatrics (2012). Breastfeeding and the use of human milk: Policy statement. Pediatrics, 129(3), e827–e841. 10.1542/peds.2011-3552 [DOI] [PubMed] [Google Scholar]
- Asiodu, I. V. , Waters, C. M. , Dailey, D. E. , Lee, K. A. , & Lyndon, A. (2015). Breastfeeding and use of social media among first‐time African American mothers. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 44(2), 268–278. 10.1111/1552-6909.12552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boccolini, C. S. , de Carvalho, M. L. , & de Oliveira, M. I. C. (2015). Factors associated with exclusive breastfeeding in the first six months of life in Brazil: A systematic review. Revista de Saúde Pública, 49, 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boccolini, C. S. , de Moraes Mello Boccolini, P. , Monteiro, F. R. , Venâncio, S. I. , & Giugliani, E. R. J. (2017). Breastfeeding indicators trends in Brazil for three decades. Revista de Saúde Pública, 51, 108 10.11606/S1518-8787.2017051000029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand, E. , Kothari, C. , & Stark, M. A. (2011). Factors related to breastfeeding discontinuation between hospital discharge and 2 weeks postpartum. The Journal of Perinatal Education, 20(1), 36–44. 10.1891/1058-1243.20.1.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brazilian Internet Steering Committee (2017). Survey on the use of information and communication technologies in Brazilian households: ICT households 2016. São Paulo: Núcleo de Informação e Coordenação do Ponto BR. [Google Scholar]
- Brown, A. , Raynor, P. , & Lee, M. (2011). Healthcare professionals' and mothers' perceptions of factors that influence decisions to breastfeed or formula feed infants: A comparative study. Journal of Advanced Nursing, 67(9), 1993–2003. 10.1111/j.1365-2648.2011.05647.x [DOI] [PubMed] [Google Scholar]
- da Silva, E. P. , de Lima, R. T. , & Osório, M. M. (2016). Impact of educational strategies in low‐risk prenatal care: Systematic review of randomized clinical trials. Ciência & Saúde Coletiva, 21(9), 2935–2948. 10.1590/1413-81232015219.01602015 [DOI] [PubMed] [Google Scholar]
- de Almeida, J. M. , de Araújo Barros Luz, S. , & da Veiga Ued, F. (2015). Support of breastfeeding by health professionals: Integrative review of the literature. Revista Paulista de Pediatria, 33(3), 355–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dean, A. , Sullivan, K. , & Soe, M . (2013). OpenEpi: Open source epidemiologic statistics for public health, version 3.01. http://www.OpenEpi.com.
- Fu, I. C. Y. , Fong, D. Y. T. , Heys, M. , Lee, I. L. Y. , Sham, A. , & Tarrant, M. (2014). Professional breastfeeding support for first‐time mothers: A multicentre cluster randomised controlled trial. BJOG : An International Journal of Obstetrics and Gynaecology, 121(13), 1673–1683. 10.1111/1471-0528.12884 [DOI] [PubMed] [Google Scholar]
- George, B. , Seals, S. , & Aban, I. (2014). Survival analysis and regression models. Journal of Nuclear Cardiology, 21(4), 686–694. 10.1007/s12350-014-9908-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giglia, R. , Cox, K. , Zhao, Y. , & Binns, C. W. (2015). Exclusive breastfeeding increased by an internet intervention. Breastfeeding Medicine, 10(1), 20–25. 10.1089/bfm.2014.0093 [DOI] [PubMed] [Google Scholar]
- Harari, N. , Rosenthal, M. S. , Bozzi, V. , Goeschel, L. , Jayewickreme, T. , Onyebeke, C. , … Perez‐Escamilla, R. (2018). Feasibility and acceptability of a text message intervention used as an adjunct tool by WIC breastfeeding peer counsellors: The LATCH pilot. Maternal & Child Nutrition, 14(1), e12488 10.1111/mcn.12488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronborg, H. , Vaeth, M. , Olsen, J. , Iversen, L. , & Harder, I. (2007). Effect of early postnatal breastfeeding support: A cluster‐randomized community based trial. Acta Paediatrica, 96(7), 1064–1070. 10.1111/j.1651-2227.2007.00341.x [DOI] [PubMed] [Google Scholar]
- Li, R. , Fein, S. B. , Chen, J. , & Grummer‐Strawn, L. M. (2008). Why mothers stop breastfeeding: Mothers' self‐reported reasons for stopping during the first year. Pediatrics, 122(Suppl 2), S69–S76. 10.1542/peds.2008-1315i [DOI] [PubMed] [Google Scholar]
- Lima, S. P. , dos Santos, E. K. A. , Erdmann, A. L. , & de Souza, A. I. J. (2018). Unveiling the lived experience meaning of being a woman breastfeeding with puerperal complications. Texto & Contexto ‐ Enfermagem, 27(1), e0880016. [Google Scholar]
- Machado, M. C. M. , Assis, K. F. , de Cássia Carvalho Oliveira, F. , Ribeiro, A. Q. , Araújo, R. M. A. , Cury, A. F. , … do Carmo Castro Franceschini, S. (2014). Determinants of the exclusive breastfeeding abandonment: Psychosocial factors. Revista de Saúde Pública, 48(6), 985–994. 10.1590/S0034-8910.2014048005340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques, E. S. , Cotta, R. M. M. , Botelho, M. I. V. , do Carmo Castro Franceschini, S. , Araújo, R. M. A. , & Lopes, L. L. (2010). Social network: Revealing the nursing mother social affairs. Physis: Revista de Saúde Coletiva, 20(1), 261–281. 10.1590/S0103-73312010000100014 [DOI] [Google Scholar]
- Marques, E. S. , Cotta, R. M. M. , Magalhães, K. A. , da Rocha Sant'Ana, L. F. , Gomes, A. P. , & Siqueira‐Batista, R. (2010). The influence of the social net of lactating mothers in the breastfeeding: The strategic role of the relatives and professionals of health. Ciência & Saúde Coletiva, 15, 1391–1400. 10.1590/S1413-81232010000700049 [DOI] [PubMed] [Google Scholar]
- Ministério da Saúde (2009). II Pesquisa de prevalência de aleitamento materno nas capitais brasileiras e Distrito Federal. Brasília: Ministério da Saúde. [Google Scholar]
- Ministério da Saúde (2015a). Cartilha para a mulher trabalhadora que amamenta (2nd ed.). Brasília: Ministério da Saúde. [Google Scholar]
- Ministério da Saúde (2015b). Orientações para avaliação de marcadores de consumo alimentar na atenção básica. Brasília: Ministério da Saúde. [Google Scholar]
- Ministério da Saúde (2015c). Saúde da criança: Aleitamento materno e alimentação complementar (2nd ed.). Brasília: Ministério da Saúde. [Google Scholar]
- Moher, D. , Hopewell, S. , Schulz, K. F. , Montori, V. , Gøtzsche, P. C. , Devereaux, P. J. , … Altman, D. G. (2010). CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. BMJ, 340, c869 10.1136/bmj.c869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monte, G. C. S. B. , Leal, L. P. , & Pontes, C. M. (2013). Social support networks for breastfeeding women. Cogitare Enfermagem, 18(1), 148–155. [Google Scholar]
- Müller, F. S. , Rea, M. F. , & Monteiro, N. R. (2014). Iniciativa Mundial Sobre Tendências Do Aleitamento Materno (WBTi). São Paulo: IBFAN Brasil. [Google Scholar]
- Patel, S. , & Patel, S. (2016). The effectiveness of lactation consultants and lactation counselors on breastfeeding outcomes. Journal of Human Lactation, 32(3), 530–541. 10.1177/0890334415618668 [DOI] [PubMed] [Google Scholar]
- Pereira‐Santos, M. , de Sousa Santana, M. , Oliveira, D. S. , Filho, N. , Aleixo, R. , Lisboa, C. S. , … Oliveira, A. M. (2017). Prevalence and associated factors for early interruption of exclusive breastfeeding: Meta‐analysis on Brazilian epidemiological studies. Revista Brasileira de Saúde Materno Infantil, 17(1), 59–67. 10.1590/1806-93042017000100004 [DOI] [Google Scholar]
- Pérez‐Escamilla, R. , Curry, L. , Minhas, D. , Taylor, L. , & Bradley, E. (2012). Scaling up of breastfeeding promotion programs in low‐ and middle‐income countries: The “breastfeeding gear” model. Advances in Nutrition, 3(6), 790–800. 10.3945/an.112.002873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pittas, T. M. , & Dri, C. F. (2017). The dialog between health and foreign policy in Brazilian cooperation in human milk banks. Ciência & Saúde Coletiva, 22(7), 2277–2286. 10.1590/1413-81232017227.02832017 [DOI] [PubMed] [Google Scholar]
- Prates, L. A. , Schmalfuss, J. M. , Lipinski, J. M. , Prates, L. A. , Schmalfuss, J. M. , & Lipinski, J. M. (2015). Social support network of post‐partum mothers in the practice of breastfeeding. Escola Anna Nery, 19(2), 310–315. [Google Scholar]
- Sheehan, A. , Schmied, V. , & Barclay, L. (2009). Women's experiences of infant feeding support in the first 6 weeks post‐birth. Maternal & Child Nutrition, 5(2), 138–150. 10.1111/j.1740-8709.2008.00163.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva, A. C. , Freitas, L. M. C. , de Feritas Maia, J. A. , Granja, M. M. F. , Dodt, R. C. M. , & Chaves, E. M. C. (2016). Technologies in breastfeeding: An integrative review. Revista Brasileira Em Promoção da Saúde, 29(3), 439–446. [Google Scholar]
- Skouteris, H. , Nagle, C. , Fowler, M. , Kent, B. , Sahota, P. , & Morris, H. (2014). Interventions designed to promote exclusive breastfeeding in high‐income countries: A systematic review. Breastfeeding Medicine, 9(3), 113–127. 10.1089/bfm.2013.0081 [DOI] [PubMed] [Google Scholar]
- Sousa, A. F. , Claro, M. D. , Sousa, A. L. , Lima, L. H. , & Santana, A. G. (2015). Advances and challenges of breastfeeding in Brazil: An integrative review. Revista Brasileira Em Promoção da Saúde, 28(3), 434–442. [Google Scholar]
- Thomas, J. R. , & Shaikh, U. (2012). Use of electronic communication by physician breastfeeding experts for support of the breastfeeding mother. Breastfeeding Medicine, 7(6), 393–396. 10.1089/bfm.2011.0133 [DOI] [PubMed] [Google Scholar]
- Tomfohrde, O. J. , & Reinke, J. S. (2016). Breastfeeding mothers' use of technology while breastfeeding. Computers in Human Behavior, 64(Suppl C), 556–561. 10.1016/j.chb.2016.07.057 [DOI] [Google Scholar]
- Venancio, S. I. , Escuder, M. M. L. , Saldiva, S. R. D. M. , & Giugliani, E. R. J. (2010). Breastfeeding practice in the Brazilian capital cities and the Federal District: Current status and advances. Jornal de Pediatria, 86(4), 317–324. 10.2223/JPED.2016 [DOI] [PubMed] [Google Scholar]
- Venancio, S. I. , & Monteiro, C. A. (1998). Breast‐feeding trends between 1970 and 1980 in Brazil. Revista Brasileira de Epidemiologia, 1(1), 40–49. 10.1590/S1415-790X1998000100005 [DOI] [Google Scholar]
- Victora, C. G. , Bahl, R. , Barros, A. J. D. , França, G. V. A. , Horton, S. , Krasevec, J. , … Rollins, N. C. (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. The Lancet, 387(10017), 475–490. 10.1016/S0140-6736(15)01024-7 [DOI] [PubMed] [Google Scholar]
- Vieira, T. O. , Vieira, G. O. , de Oliveira, N. F. , Mendes, C. M. C. , Giugliani, E. R. J. , & Silva, L. R. (2014). Duration of exclusive breastfeeding in a Brazilian population: New determinants in a cohort study. BMC Pregnancy and Childbirth, 14, 175 10.1186/1471-2393-14-175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner, E. A. , Chantry, C. J. , Dewey, K. G. , & Nommsen‐Rivers, L. A. (2013). Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics, 132(4), e865–e875. 10.1542/peds.2013-0724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warkentin, S. , de Aguiar Carrazedo Taddei, J. A. , de Jesus Viana, K. , & Colugnati, F. A. B. (2013). Exclusive breastfeeding duration and determinants among Brazilian children under two years of age. Revista de Nutrição, 26(3), 259–269. 10.1590/S1415-52732013000300001 [DOI] [Google Scholar]
- Wood, N. K. , Woods, N. F. , Blackburn, S. T. , & Sanders, E. A. (2016). Interventions that enhance breastfeeding initiation, duration, and exclusivity: A systematic review. MCN: The American Journal of Maternal/Child Nursing, 41(5), 299–307. 10.1097/NMC.0000000000000264 [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2003). Infant and young child feeding: A tool for assessing national practices, policies and programmes. Geneva, Switzerland: WHO. [Google Scholar]
- World Health Organization (2009). Infant and young child feeding: Model chapter for textbooks for medical students and allied health professionals. Geneva, Switzerland: WHO. [PubMed] [Google Scholar]
- World Health Organization (2011). mHealth: New horizons for health through mobile technologies (Vol. 3). Geneva, Switzerland: WHO. [Google Scholar]
- World Health Organization, & UNICEF (2009). Baby‐friendly hospital initiative: Revised, updated and expanded for integrated care. Geneva, Switzerland: WHO. [PubMed] [Google Scholar]


