Abstract
The provision of breast pumps is a potential strategy to increase breastfeeding duration. This trial compared the effectiveness and acceptability of two breast pumps in mothers exclusively breastfeeding (EBF) their healthy term infant. It also tested whether provision of pumps versus vouchers of equivalent value influenced breastfeeding or attainment of mothers' goals at 3 and 6 months. Mothers were randomised at 3‐ to 4‐week post‐partum (Beijing [n = 30], Moscow [n = 34], London [n = 45], New York [n = 3]) to groups A (Philips single‐electric pump, Natural bottle), B (Medela Swing single‐electric pump, Calma bottle), or C (Control; vouchers). At 6 weeks, group A and B mothers expressed for 10 min/breast; milk weight and opinions of pump/bottle were recorded. Feeding practices were assessed using questionnaires at 3 and 6 months. Milk weight/flow pattern did not differ between groups. Pump A scored significantly better for ease‐of‐use, cushion‐feel, need‐to‐lean‐forward, pleasant, comfort. At 3 and 6 months, %EBF or meeting their goal was not significantly different; (3 months: 86%, 85%, 84%; 6 months: 20%, 15%, 26%; meeting goal 24%, 17%, 27% for A, B, and C). Expressed breast milk (EBM) provision was higher in groups A and B (3 months: 76%, 76%, 24% (p < 0.001); 6 months: 83%, 87%, 32% (p < 0.001); and negatively predicted EBF at 6 months (OR no EBM 5.07, 95% CI [1.56, 16.5]). The pumps were equally effective for milk expression at 6 weeks. Pump provision did not significantly influence breastfeeding practices or attainment of goals but resulted in higher EBM provision, which was associated with lower EBF but not other breastfeeding categories at 6 months.
Keywords: breast pump, breastfeeding, efficacy, expressed milk, milk expression, randomised trial
Key messages.
Two single‐electric breast pumps with different design features showed similar efficacy, but there were differences in mothers' opinions for pump characteristics.
Breastfeeding practices at 6 months did not differ significantly between mothers who were exclusively breastfeeding their term infant at 3–4 weeks and randomised to receive a breast pump versus vouchers to an equivalent value.
Women randomised to receive a pump were significantly more likely to express milk and feed it to their infant than those randomised to receive a voucher.
Feeding expressed breast milk at 3 or 6 months was associated with reduced exclusive breastfeeding at 6 months but did not predict the likelihood of any breastfeeding at 6 months.
1. INTRODUCTION
Breastfeeding is an important public health intervention, with benefits for infants and mothers (Victora, Bahl, Barros, et al., 2016), and the potential for significant economic savings from even modest increases in prevalence and duration (Renfrew et al., 2012; Rollins, Bhandari, Hajeebhoy, et al., 2016). The World Health Organisation (WHO) recommends that mothers exclusively breastfeed (EBF) for the first 6 months of life (WHO, 2002). However, many mothers do not achieve this and even when initiation rates are high the proportion still breastfeeding often falls steeply over the first weeks post‐partum (RCPCH, 2017; Victora et al., 2016). Reasons why mothers do not follow or achieve breastfeeding recommendations are complex and differ among countries and regions but include concern about the adequacy of milk production, family and work commitments, night‐time waking, and feeling uncomfortable breastfeeding in public (RCPCH, 2017; Rollins et al., 2016; Victora et al., 2016).
One possible strategy to improve the provision of breast milk could be the increased use of expressed breast milk (EBM), to be given to the infant when breastfeeding is not possible or convenient. The prevalence of milk expression is not well documented but appears to vary between countries (Labiner‐Wolfe, Fein, Shealy, & Wang, 2008; Weisband, Keim, Keder, Geraghty, & Gallo, 2017; Win, Binns, Zhao, Scott, & Oddy, 2006). Reasons for expressing milk in mothers who deliver a healthy term infant broadly reflect short‐term issues such as difficulty establishing lactation or concerns about milk supply and longer‐term considerations including returning to work or “keeping up the milk supply” (Weisband et al., 2017; Win et al., 2006). The impact of milk expression on breastfeeding outcomes is unclear. A systematic review of incentives to promote breastfeeding (Moran et al., 2015) identified seven studies, namely, five randomised trials, evaluating the effect of breast pump provision alone or with other incentives, and effects on breastfeeding outcomes were inconsistent. Other studies examined associations between breast pump use and breastfeeding outcomes (Ahluwalia, Tessaro, Grummer‐Strawn, & MacGowan, 2000; Bream, Li, & Furman, 2017; Meehan et al., 2008; Schwartz et al., 2002; Win et al., 2006) with similarly mixed results, most likely reflecting differences in the study populations and underlying reasons for milk expression.
Several methods are available for milk expression, from hand expression to large dual‐electric breast pumps. Breast pump technology was historically based largely on suction, which may be unphysiological (Burton, Deng, MacDonald, & Fewtrell, 2013). Advances in pump technology have included the introduction of massage cushions in the pump insert which aim to mimic the compressive action of the infant during breastfeeding; a strategy shown to be effective and appreciated by mothers expressing milk for both preterm (Fewtrell, Lucas, Collier, Singhal, 2001; Burton et al., 2013) and term infants (Fewtrell, Lucas, Collier, Singhal, et al., 2001). Another development has been the introduction of two‐phase patterns of milk expression, with “let down” and “expression” phases to mimic an infant breastfeeding (Kent, Ramsay, Doherty, Larsson, & Hartmann, 2003). To our knowledge, although studies have examined the impact of breast pump design on short‐term milk production and maternal preference, no study has yet tested whether the use or design of a pump influences breastfeeding duration or attainment of the mother's own goals.
This randomised trial had two main aims. The first was to compare the effectiveness and acceptability of two modern single electric breast pumps with different design features in mothers breastfeeding their healthy term infant and the second aim was to test whether the provision of these pumps versus provision of vouchers to an equivalent monetary value influenced the likelihood of the mother breastfeeding at 3 and 6 months and attaining her own breastfeeding goals.
2. METHODS
Exclusively breastfeeding mothers were recruited 3‐ to 4‐week post‐partum from four sites (London [UK], Moscow [Russia], Beijing [China], and New York [USA]). In the United Kingdom, mothers were recruited from local mother and baby groups, using flyers and via word of mouth, while in the United States, Russia, and China they were recruited from maternity/baby clinics. Mothers were eligible if they (a) had a healthy, term singleton infant (birthweight > 2.5 kg, ≥37‐week gestation); (b) were EBF and willing to be randomised to receive a pump or to continue breastfeeding without using a pump; (c) were not using a pump regularly; and (d) could speak and write in English, Russian, or Mandarin. Enrolment and randomisation were performed in the clinic or during a home visit. Mothers were randomised to one of three groups: (a) Group A; Philips single electric Comfort breast pump with Natural bottle (Philips Consumer Lifestyle, Amsterdam, The Netherlands); (b) Group B; Medela Swing single electric pump with Calma bottle (Medela AG, Baar, Switzerland); (c) Group C; Babycare vouchers to the value of the breast pump/bottle combination. Pump A has a 5‐petal massage cushion to reduce reliance on vacuum and compact expression funnel to minimise the need to lean forward; it also allows flexibility of suction and rate. Pump B has a two‐phase expression system with a “light and fast” initiation phase and a “slower and deeper” extraction phase. A bottle and teat was included in the pack with the pump. The nurse explained to mothers in Groups A and B how to use and clean the pump, optimise milk expression, and store breast milk safely. Apart from the physiological test at 5/6 weeks and familiarising themselves with the pump beforehand, it was entirely the mother's choice whether she expressed milk and/or used the study bottle. If a mother used another pump, she was asked to record this with the reason for her decision. Study literature was translated into Russian or Mandarin and back‐translated by a second person to check for consistency of meaning.
Baseline data were collected on socio‐economic status, pregnancy and delivery, infant health, and feeding. Mothers were asked to indicate their personal goals for EBF and any breastfeeding in months, using questions from the Infant Feeding Practices Study (Centers for Disease Control & Prevention, 2009).
The study was registered with http://clinicaltrials.gov (NCT02128295; April 2014) and approved by the research ethics committee in each site (UK—UCL Research Ethics Committee, ref: 5645/001 12.8.14; USA—North Shore LIJ, Office of the Human Research Protection Program, ref: 14‐325B 25.9.14; Russia—Local Ethics Committee, ref:35–04/15.04.14; China: Local Institutional Approval). All participants gave written informed consent.
The primary hypotheses were that (a) milk weight produced at 1‐min intervals and total weight produced in 20 min at 5‐ to 6‐week post‐partum would be greater for mothers using pump A than pump B; and (b) mothers using pump A would award higher scores for a pump characteristics than those using pump B. The primary outcome measures were the weight of milk expressed in a 20 minute period at 5–6 weeks, and the mothers' opinions of the breast pump. Secondary hypotheses were (a) a greater proportion of mothers using pump A would be EBF, partially breastfeeding and/or providing breast milk at 3 and 6 months and would achieve their breastfeeding goals, compared with those using pump B; (b) the proportion of mothers in group A who were breastfeeding and achieving their goals would not differ from a control group of mothers who did not receive a breast pump; (c) mothers would give higher scores for characteristics of feeding bottle A than bottle B, if used. Secondary outcome measures were infant feeding practices reported at 3 and 6 months of age and opinions of the bottle if used. The hypotheses were based on the fact that Pump A combines two features previously shown to improve outcomes (a compression cushion and flexibility of speed and suction) whereas Pump B has one feature (flexibility of speed and suction) and on data from previous studies in which Pump A and bottle A received higher scores for certain characteristics (Fewtrell, Lucas, Collier, Singhal, et al., 2001; Burton, Kennedy, et al., 2013; Fewtrell, Lucas, Collier, & Lucas, 2001); Fewtrell, Kennedy, Nicholl, Khakoo, & Lucas, 2012).
2.1. Measurement of primary outcome measures at 5‐ to 6‐week visit
Mothers from groups A and B took part in the physiology study, conducted in the subject's home (United Kingdom and Russia) or clinic (United States and China) as close to 11 am as possible and, where feasible, at least 2 hr after the last feed. Mothers expressed milk for up to 20 min (10 min/breast), and the weight of milk was recorded by the research nurse at 1‐min intervals, by placing a different bottle under the pump outflow for each 1‐min period. The time and side of the last breast feed was noted.
Mothers provided their opinion about the pump (comfort, ease of use, how pleasant to use, suction, speed of milk flow, assembly, cleaning, leakage and overall opinion) using a 10‐cm visual analogue scale (VAS).
2.2. Measurement of secondary outcome measures at 3 and 6 month follow‐up
At 3 and 6 months, mothers completed questionnaires reporting infant feeding in the last 7 days. Questionnaires were sent to the mother in the week before their infant reached 3 or 6 months. Categories at 3 months were EBF, mainly breastfeeding (BF) with <1 formula‐feed (FF) per day, mainly BF with at least 1 FF per day, mainly FF with at least 1 BF per day, mainly FF with <1 BF per day, exclusively FF. At 6 months, there were additional categories for BF or FF with solid foods or other drinks. Separate questions asked when solid foods and/or infant formula had first been given (<22 weeks, 22–24 weeks, 24–25 weeks, not started). Breast pump and bottle use in the past 7 days were recorded as not used, once, twice, three to five times, six to seven times. Opinions of the study pump and bottle (if used) were recorded as strongly agree/agree, neither agree nor disagree, and strongly disagree/disagree with a series of statements. This method was used rather than a VAS to facilitate completion online; SurveyMonkey was used in the United Kingdom, whereas questionnaires were sent by e‐mail or post in the other centres. Mothers received a £15 (or equivalent) Babycare voucher on completion of the questionnaires.
2.3. Randomisation and blinding
The randomisation schedule was computer‐generated in randomised blocks of 3 and 6, stratified by site and parity; assignments were prepared by a team member with no subject contact and kept in sealed, opaque envelopes. After confirming eligibility and obtaining written informed consent, the research nurse opened the next randomisation envelope in sequence and provided the pump or vouchers according to the assigned group. It was not possible to blind mothers or research nurses to pump allocation, but data analyses for primary outcomes were performed blind to randomised group.
2.4. Statistics
A sample size of 64 per group for the primary analysis (comparison between randomised pump groups) at 6 weeks was estimated to provide 80% power to detect relevant differences in milk production and pump characteristics at p < 0.05, based on a combination of data from previous studies (Fewtrell, Lucas, Collier, Singhal, et al., 2001; Fewtrell, Lucas, Collier, & Lucas, 2001) and consumer data, although none of the available data were directly applicable to the planned study as different breast pumps were used under different circumstances. To allow for drop‐outs and subjects who did not comply with the protocol, we planned to recruit 228 subjects (76 per group) between the four participating centres (51 from Russia, 45 from China, 54 from the United States, 78 from the United Kingdom).
Analyses were performed on an intention‐to‐treat basis. Comparisons between pump groups were made using t test, Mann–Whitney test, or chi‐square test as appropriate. Comparisons of infant feeding practices between the three randomised groups were made by analysis of variance (ANOVA) with post hoc pairwise testing (Dunnett test) if the ANOVA was significant, or where specified a priori. Data on the age at first introduction of solid foods and/or infant formula were recoded to a variable indicating EBF at 6 months (i.e., no solids or formula) as yes/no. Data for milk production at 1‐min intervals were analysed by repeated measures ANOVA. Predictors of milk production during the physiological test were examined using general linear models, including parity, study site, randomised pump and time since the last breastfeed. Predictors of EBF and any BF at 6 months were examined using logistic regression. Analyses were performed using SPSS version 24.
3. RESULTS
3.1. Study population
One hundred and seventy mothers were recruited from Beijing (n = 45), Moscow (n = 51), London (n = 68), and New York (n = 6; Figure 1). The target sample size was not achieved in the United States mainly due to mothers who either planned to use infant formula within the first few weeks or who did not attend appointments; or the U.K. site where recruitment was slower than anticipated. Sixty mothers were randomised to group A; 52 to group B; and 58 to group C, with no significant differences in baseline characteristics between groups (Table 1). However, differences in parity, maternal age, education, income, and ethnicity were apparent among study sites (Table S1).
Figure 1.
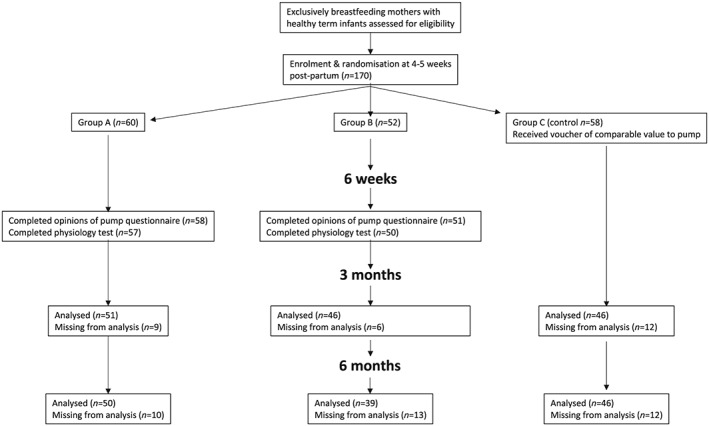
CONSORT flow diagram
Table 1.
Baseline characteristics by randomised group
| All subjects | Group A | Group B | Group C | |
|---|---|---|---|---|
| n | 170 | 60 | 52 | 58 |
| Birthweight (kg) (mean (SD)) | 3.47 (0.41) | 3.45 (0.39) | 3.43 (0.43) | 3.52 (0.42) |
| Gender | ||||
| Male | 88 | 32 | 23 | 33 |
| Female | 82 | 28 | 29 | 25 |
| Parity | ||||
| Primip | 105 | 37 | 33 | 35 |
| Multip | 65 | 23 | 19 | 23 |
| Delivery | ||||
| Vaginal | 136 | 51 | 43 | 42 |
| LSCS | 34 | 9 | 9 | 16 |
| Time after delivery when infant put to the breast | ||||
| Within 30 min | 81 | 35 | 24 | 22 |
| After 30 min | 89 | 25 | 28 | 36 |
| Maternal data | ||||
| Age (years) | 31.9 (4.5) | 32.8 (4.3) | 31.5 (4.5) | 31.5 (4.6) |
| Maternal education | ||||
| Years full‐time | 16.2 (3.4) | 16.5 (3.8) | 16.1 (2.9) | 15.9 (3.4) |
| Income pa1 | ||||
| Low (<£20 k) | 40 | 13 | 14 | 13 |
| Medium–low (<£30 k) | 44 | 15 | 10 | 19 |
| Medium–high (<£45 k) | 32 | 12 | 11 | 9 |
| High (>£45) | 54 | 20 | 17 | 17 |
| Maternal ethnicity | ||||
| White British/Europe | 86 | 36 | 27 | 24 |
| Chinese | 53 | 18 | 18 | 17 |
| All other groups | 24 | 6 | 6 | 12 |
3.2. Primary outcome measures at 5–6 weeks
3.2.1. Physiology study
One hundred and seven mothers (57/60 group A, 50/52 group B) completed the physiology study with no significant difference in time since last breastfeed between groups. Milk weight at 1‐min intervals, the total milk expressed from either breast (Table 2), and the pattern of milk production (Figure 2) did not differ according to the pump used, with or without adjustment for study site (data not shown). Mothers in Russia and China had later peak milk production than UK mothers (Figure S1).
Table 2.
Milk weight (g) at 1‐min intervals during milk expression according to randomised breast pump (median [25th and 75th percentiles])
| n | Pump A | n | Pump B | |
|---|---|---|---|---|
| Breast 1 | ||||
| 1 min | 57 | 6.2 (3.1, 10.5) | 50 | 6.6 (3.7, 14.7) |
| 2 min | 57 | 8.6 (4.5, 14.4) | 50 | 7.2 (4.4, 13.9) |
| 3 min | 57 | 8.5 (4.8, 14.9) | 50 | 8.4 (4.7, 14.6) |
| 4 min | 57 | 10.0 (4.5, 15.0) | 50 | 9.0 (4.1, 13.6) |
| 5 min | 56 | 9.2 (4.7, 14.8) | 60 | 8.1 (5.5, 13.0) |
| 6 min | 56 | 8.9 (4.3, 13.4) | 50 | 9.2 (4.3, 12.9) |
| 7 min | 56 | 8.6 (2.5, 11.7) | 49 | 7.9 (2.9, 12.1) |
| 8 min | 56 | 5.9 (2.1, 10.0) | 49 | 6.0 (2.9, 10.6) |
| 9 min | 55 | 4.3 (2.6, 9.7) | 48 | 4.2 (1.7, 8.9) |
| 10 min | 55 | 5.0 (2.6, 8.4) | 48 | 5.1 (2.5, 11.8) |
| Total side 1 | 57 | 83.3 (47.5, 115.2) | 50 | 71.1 (46.9, 124.6) |
| Breast 2 | ||||
| 1 min | 57 | 4.1 (2.5, 9.6) | 50 | 5.0 (2.5,9.1) |
| 2 min | 57 | 7.0 (3.4, 10.5) | 50 | 6.1 (3.3, 10.1) |
| 3 min | 57 | 5.2 (2.1, 11.2) | 50 | 6.1 (3.3, 11.1) |
| 4 min | 56 | 4.6 (2.2, 10.7) | 50 | 6.9 (3.7, 11.8) |
| 5 min | 56 | 4.6 (1.7, 10.3) | 50 | 6.1 (2.9, 9.7) |
| 6 min | 56 | 4.0 (0.8, 9.6) | 50 | 5.7 (2.3, 9.7) |
| 7 min | 55 | 3.5 (0.7, 9.2) | 50 | 5.2 (2.2, 9.2) |
| 8 min | 55 | 3.5 (0.6, 8.6) | 50 | 3.9 (1.8, 7.3) |
| 9 min | 55 | 2.4 (0.7, 6.0) | 50 | 3.1 (1.9, 6.4) |
| 10 min | 55 | 1.9 (0.7, 5.1) | 50 | 3.0 (1.3, 4.6) |
| Total side 2 | 57 | 43.6 (27.2, 75.5) | 50 | 50.0 (39.2, 72.5) |
Note. All comparisons p > 0.05.
Figure 2.
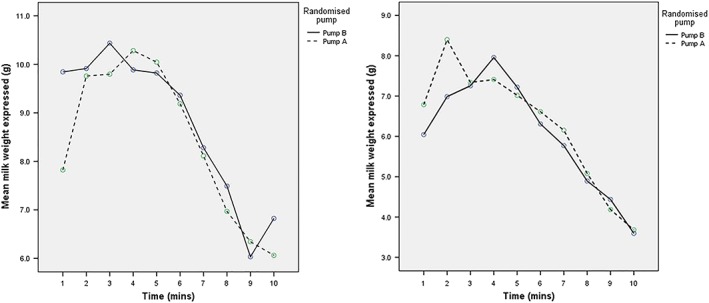
Mean milk weight at 1‐min intervals for breast 1 and breast 2 (estimated means from repeated measures analysis of variance) expressed over 10 min according to randomised pump for whole cohort
3.2.2. Opinions of breast pumps
One hundred and ten mothers (59 group A, 51 group B) completed the questionnaire. Pump A received significantly better (lower) scores for “ease of use” (median 1.3 (25th and 75th percentiles 0.7, 2.0) v 1.9 (0.9, 2.5), p = 0.02), “pleasant to use” (1.7 [0.9,2.7] v 2.3 [1.5, 4.0], p = 0.02), “feel of the pump insert” (1.95 [1.09, 3.07] v 2.71 [1.80, 4.39], p = 0.02), and “need to lean forward” (1.8 [0.8, 2.8] vs 6.1 [2.4, 8.7], p < 0.001). The score for comfort was also lower (better) for pump A (1.4 [0.6, 2.3] v 2.0 [0.8, 3.2, p = 0.051]). The pumps did not differ for overall opinion (1.6 [0.8, 2.6] v 2.2 [0.9, 3.5], p = 0.06). The results were unchanged after adjusting for study site (data not shown).
3.3. Secondary outcome measures at 3 and 6 months
At 3 months, of the 84% (142/170) of mothers who returned the questionnaire, the majority of mothers reported EBF (86% group A, 85% group B, 84% group C). The majority of noncompleters were from the United Kingdom (25/28). Participation at 3 months did not differ between randomised groups. Mothers who completed the questionnaire were younger (31.5 [4.3] vs. 34.1 [5.0] years) were less likely to have delivered by LSCS (17% vs. 36%, p = 0.01) and less likely to have a family income > £45 k pa (or local equivalent; 9% vs. 22%, p = 0.014) than noncompleters.
Eighty percent (135/170) of mothers completed the questionnaire at 6 months; the majority of noncompleters were from the United Kingdom (31/35). Participation at 6 months did not differ between randomised groups. Mothers who completed the questionnaire were more likely to have male infants (57% vs. 43%, p < 0.01) had fewer years in education (15.8 [3.5] years vs. 17.7 [2.7] years, p = 0.002) were less likely to have delivered by LSCS (16% vs. 34%, p = 0.01) and less likely to have a family income > £45 k pa (or local equivalent; 11% vs 21%, p = 0.008) than noncompleters. Parity and birthweight did not differ. By 6 months, three group A mothers and one group B mother reported using a different breast pump on at least one occasion, whereas six group C mothers reported having used a pump.
At 6 months, 20%, 15%, and 26% of mothers from groups A, B, and C, respectively, reported EBF over the last 7 days, with no significant difference between groups (Table 3 ). The proportion of infants who were BF with the addition of solid foods (BFCF) was 68%, 59%, and 85% for groups A, B, and C (p = 0.03; A vs. B, A vs. C not significant, B < C p < 0.05). The proportion of mothers EBF or BF with either solids or up to one bottle of formula per day (BFCFF) was 75%, 67%, and 85% for groups A, B, and C (not significant); whereas the proportion of mothers reporting “any breastfeeding” were 82%, 80%, and 87%, respectively (not significant). Only two mothers were exclusively formula feeding and 15 (five group B, six group A, and two group C) were formula feeding with complementary feeding. The proportions who reported no use of solids or formula by 26 weeks were 16%, 18%, and 26% for groups A, B, and C (p = 0.5). Discrepancies between this variable and “EBF in the past 7 days” were observed where mothers reported EBF but also reported introducing solid foods by 26 weeks (2, 1, and 2 in groups A, B, and C) or where they reported not EBF but also had not introduced solids or formula by 26 weeks (two group B, two group C). The latter discrepancy may be explained by the fact that a few mothers completed the questionnaire between 6 and 7 months so they may not have introduced solids or formula by 6 months despite no longer EBF when they completed the questionnaire. Excluding these four subjects, the EBF rate at 6 months was 20%, 16%, and 27% for groups A, B, and C, respectively (not significant). Assuming that these four subjects were EBF at 6 months, the rates were 20%, 21%, and 31% for groups A, B, and C, respectively (not significant). Rates of EBF at 6 months were not significantly different between the centres (Table S1).
Table 3.
Breastfeeding practices at 3 and 6 months by randomised group (n [%])
| Group A | Group B | Group C | p (Chi‐square) three groups | A vs. B | A vs. C | B vs. C | |
|---|---|---|---|---|---|---|---|
| 3 months (n = 142) | n = 51 | n = 46 | n = 45 | ||||
| EBF | 44 (86) | 39 (85) | 38 (84) | 0.96 | 1.0 | 1.0 | 1.0 |
| Mainly BF (with 1FF) | 46 (90) | 41 (86) | 40 (89) | 0.98 | 1.0 | 1.0 | 1.0 |
| Provided EBM | 37 (73) | 35 (76) | 11 (24) | <0.001 | 0.82 | <0.001 | <0.001 |
| 6 months (n = 135) | n = 50 | n = 39 | n = 46 | ||||
| EBF | 10 (20) | 6 (15) | 12 (26) | 0.47 | 0.78 | 0.61 | 0.30 |
| Mainly EBF (with 1FF) | 13 (26) | 9 (23) | 12 (26) | 0.94 | 0.81 | 1.0 | 0.81 |
| BFCF | 34 (68) | 23 (59 | 39 (85) | 0.03 | 0.51 | 0.06 | 0.013 |
| BFCFFF | 37 (74) | 26 (67) | 39 (85) | 0.15 | 0.5 | 0.22 | 0.07 |
| Any breastfeeding | 41 (82) | 31 (80) | 40 (86) | 0.64 | |||
| Provided EBM | 39 (83) | 34 (87) | 13 (32) | <0.001 | ns | <0.001 | <0.001 |
| Reported no introduction of solid foods or infant formula by 26 weeks | 8 (16) | 7 (18) | 12 (26) | 0.5 | 1.0 | 0.32 | 0.40 |
3.3.1. Use of pumps and provision of EBM
At 3 months, 68% group A and 73% group B mothers were using their pump at least once a week, with 63% and 62% also using their study bottle. The proportion giving EBM to their infant did not differ between pump groups (76% group A, 76% group B, p = 0.9); however, only 24% of control mothers had provided EBM at 3 months (p < 0.001 for three‐way comparison; Table 3). Significantly fewer mothers in Russia (37%) were giving their infants EBM compared with either mothers in the United Kingdom (71%) or China (71%), p < 0.01.
At 6 months, there were no significant differences between groups in the proportions using their pump daily (group A 20% vs. group B 36%, p = 0.09) or weekly (group A 62% vs. group B 77%, p = 0.22) or in those using the study bottle. The proportion of mothers who had fed EBM to their infants was still significantly lower in group C (83% group A, 87% group B, 32% group C, p < 0.001).
3.3.2. Attainment of breastfeeding goals at 6 months
At baseline, 127/165 (77%) mothers aimed to EBF for 6 months; this goal did not differ significantly by randomised group (80% group A, 73% group B, 78% control, p = 0.62). Data for five mothers were excluded as they gave the same value for both duration of EBF and any breastfeeding or implausible values. Of 148 mothers who answered the further question: “when do you plan to stop breastfeeding your baby?,” 82% said at or beyond 12 months.
One hundred and thirty two mothers provided data on breastfeeding goals and on infant feeding at 6 months; 100/132 (76%) aimed to EBF for 6 months. The proportion of mothers who attained their goal of EBF for 6 months was 24%, 17%, and 27% for groups A, B, and C, respectively (not significant). Results for BFCF and BFCFF at 6 months were also not significantly different between groups (BFCF 63%, 69%, and 89%; BFCFFF 71%, 79%, and 88%). Conversely, 5/32 (16%) mothers who planned to EBF for <6 months reported they were EBF at 6 months.
3.3.3. Opinions of bottles
Forty‐one group A and 52 group B mothers had used the study bottle and completed the 6‐week questionnaire. Bottle A scored more highly (lower score) for cleaning (1.89 [25th and 75th percentiles 0.6, 2.3] v 2.0 [1.2, 3.4] p = 0.04); leakage (1.0 [0.5, 2.2] v 2.5 [1.0, 4.6] p = 0.001; shape of teat (2.6 [1.4, 3.9] v 3.8 [2.0, 5.1] p = 0.01); and overall opinion (2.3 [0.9, 3.4] v 3.2 [1.8, 6.2] p = 0.09). At 3 months, significantly more mothers using Bottle A agreed or strongly agreed that it was easy to clean compared with those using bottle B (88% vs. 54%, p = 0.001). At 6 months, more group A mothers agreed the bottle was easy to clean (97% vs. 70% group B, p = 0.01) and that they liked the bottle (100% vs. 86%, p = 0.04).
3.4. Predictors of the amount of milk expressed in the physiology test
The total milk expressed was predicted by the time since the last feed (0.58 g more per minute, p = 0.002), parity (adjusted mean for primips 128.7 g vs. multips 173.9 g, p = 0.002), and study site (China adjusted mean 120.8 g, United Kingdom 140.3 g, Russia 192.8 g, p < 0.001) but not by randomised pump group (group A 153.6 g, group B 149.0 g, p = 0.7). The model predicted 40% of the variance in milk weight. Breast pump opinions scores were not significant predictors of milk production.
3.5. Predictors of EBF and any BF at 6 months
Parity, centre, randomised group, maternal age, years of maternal education, pump opinion scores, and use of EBM at 3 and 6 months were investigated as potential predictors of EBF or any BF at 6 months in 135 mothers for whom this outcome was available. Provision of EBM at either 3 or 6 months was the only significant predictor; mothers who reported giving EBM to their infant were significantly less likely to report EBF at 6 months (OR of EBF at 6 months if no EBM given by 3 months 4.03 (95% CI [1.23, 13.2], Nagelkerke R 2 0.18) and if no EBM given by 6 months 5.07 (95% CI [1.56, 16.5], Nagelkerke R 2 0.20). The effect remained after adjusting for the mother's initial goal for EBF. By contrast, none of these factors, including provision of EBM, were significant predictors of other breastfeeding outcomes (any BF, BFCF, or BFCFFF) at 6 months.
4. DISCUSSION
The first aim of our study was to test the efficacy and acceptability of two single electric breast pumps with different design features. We found no difference in the total amount of milk expressed or pattern of milk flow at 5‐ to 6‐week post‐partum. More milk was expressed by multiparous women and also when there was a longer time interval since the last feed, consistent with our previous study in term mothers (Fewtrell, Lucas, Collier, & Lucas, 2001). Interestingly, study site was also a significant predictor of the amount of milk expressed during the test, with Russian mothers expressing most milk and Chinese mothers the least, even after adjusting for parity. The explanation for this is unclear, although we cannot rule out differences in the way the physiology test was conducted in the different sites which may have influenced the time to milk ejection, despite our best efforts at training and standardisation of the process.
Mothers who used pump A awarded significantly more favourable scores for certain pump characteristics—ease of use, how pleasant the pump was to use, comfort, feel of the pump insert, and the need to lean forward—compared with mothers who used pump B, similar to findings in previous trials using manual or electric versions of these pumps in mothers of both preterm and term infants (Fewtrell, Lucas, Collier, Singhal, et al., 2001; Burton, Kennedy, et al., 2013; Fewtrell, Lucas, Collier, & Lucas, 2001). In mothers expressing milk for their preterm infant, we found that the score awarded for comfort of the pump on Day 10 was a significant predictor of total milk volume expressed whereas the infant was hospitalised (Burton, Kennedy, et al., 2013). However, in the current trial, opinions of the pump did not predict the amount of milk expressed, albeit on a single occasion at 5–6 weeks, nor breastfeeding practices at 6 months. Furthermore, use of the pumps did not differ between groups and similarly small numbers of mothers in each group changed to an alternative pump.
The second aim of our trial was to evaluate the impact of providing a breast pump on subsequent breastfeeding practices and the attainment of the mother's own goals. All mothers were EBF at the time of enrolment and the rates of EBF plus other categories of breastfeeding at 3 and 6 months were higher for the study population than reported for the general population in each country. However, there was no significant difference in breastfeeding practices between the two pump groups and the control group who received vouchers. For each outcome, there was a trend towards higher values for the control group but this did not reach significance with the exception of BF with solid foods, where the rate was significantly higher for the control group compared to group B. At baseline, 77% of mothers stated their aim was to EBF for 6 months. This was achieved by 23%, whereas 73% were EBF with the addition of solid foods, with no difference between groups. Our findings suggest that the provision of a breast pump to mothers who have already established EBF neither increases nor decreases the likelihood of the mother breastfeeding at 6 months or, importantly, meeting her own breastfeeding goals. However, our study was not powered to detect differences in this outcome and a larger study would be required to exclude a smaller effect size.
Previous randomised trials investigating the effect of the provision of breast pumps on breastfeeding were conducted in the United States, and the results were inconclusive (Bliss, Wilkie, Acredolo, Berman, & Tebb, 1997; Dungy, Christensen‐Szalanski, Losch, & Russell, 1992; Hayes et al., 2008; Rasmussen, Dieterich, Zelek, Altabet, & Kjolhede, 2011; Sciacca, Phipps, Dube, & Ratliff, 1995). The greatest positive impact of pump provision, as part of a discharge pack, was reported when the comparator was a pack containing infant formula which itself had a negative effect on breastfeeding (Dungy et al., 1992), although this effect was not seen in a larger RCT with similar interventions (Bliss et al., 1997). Sciacca et al. (1995) randomised 68 low‐income mothers to receive “prizes,” including pumps, versus usual care, and low value gifts, and reported significantly higher proportions breastfeeding in the intervention group at 2, 6, and 12 weeks. Other trials compared electric versus manual pumps (Hayes et al., 2008) or the use of electric pumps, manual pumps, or no pump in obese mothers (Rasmussen et al., 2011) and reported no effect on breastfeeding. None of these trials is directly comparable with ours, particularly because our intervention started once breastfeeding had been established rather than in the early post‐partum period.
Although breastfeeding practices did not differ between groups, we found that the provision of a breast pump significantly increased the likelihood of the mother expressing and providing EBM to her infant at both 3 and 6 months, compared with mothers randomised to receive vouchers. Furthermore, after adjusting for potential confounders, the provision of EBM at both ages was associated with lower EBF at 6 months, although it had no impact on any other category of breastfeeding. The randomised groups did not differ in baseline characteristics or breastfeeding goals, suggesting that the availability of the pump in itself encouraged mothers to express and provide EBM. Both breast pumps came packaged with a bottle and teat and we cannot therefore determine which component of the intervention was responsible for the observed effect. However, we did not consider it practical to provide a breast pump without the bottle because this is attached to the pump during milk expression. Furthermore, becasue the majority of mothers use a bottle and teat to feed EBM to their term infant (UK Infant Feeding Survey, 2010), removing the teat from the pack was not considered to represent a “real life” scenario.
Previous studies have reported on associations between milk expression and breastfeeding practices with mixed results, most likely reflecting differences in study populations. Win et al. (2006) reported that Australian mothers who expressed were significantly less likely to stop breastfeeding before 6 months than those who had never expressed. Bream, Li, and Furman (2017) conducted a chart review in 487 predominantly African American women who were eligible to receive a free pump under the Affordable Care Act. EBF at 2 months was similar in mothers with or without a breast pump (19.4% vs. 16.3%), but breastfeeding was significantly lower (31.4 vs. 46.9%, p = 0.004) and provision of EBM higher (16.6% vs. 8.2%, p = 0.02) in women who used a pump. Pang et al. (2017) found no difference in the likelihood of full breastfeeding at 3 months between mothers who fed directly at the breast and those who combined direct breastfeeding with EBM, among 541 mothers in Singapore. Schwartz et al. (2002) reported that milk expression before 3 weeks was a positive predictor of breastfeeding termination by 12 weeks in U.S. mothers, whereas expression after 3 weeks was associated with a greater likelihood of continuation. These findings may relate to the different reasons for milk expression at different post‐natal stages as highlighted by Weisband et al. (2017), who performed a cross‐sectional study before discharge from hospital in 100 U.S. mothers planning to breastfeed for at least 6 months; 98% planned to use a pump and 29% had already started. Those who started early reported pumping to increase their milk supply or to overcome latching difficulties, whereas for the whole cohort, the most common reason given was “to keep up the milk supply.” Our study intentionally started once breastfeeding had been established to avoid any interference with this process, so it is most likely that our mothers were pumping to maintain their milk supply or to provide milk for use when they were absent, either related to work or for social reasons.
We also addressed the method used to administer EBM to the infant. Although some mothers prefer to feed EBM using a cup, the majority who provide EBM for their term infant choose to use a bottle; 92% in a 2010 U.K. survey (UK Infant Feeding Survey, 2010). We previously demonstrated that the design of a feeding bottle can significantly affect infant behaviour, including fussing (Fewtrell et al., 2012) and colic (Lucas & James‐Roberts, 1998; Lucas & St James‐Roberts, 1994), which might theoretically influence the likelihood of the mother continuing to provide EBM. However, although mothers in group A awarded significantly better scores for a number of characteristics at 6 weeks, 3 and 6 months, these differences did not influence the provision of EBM or the proportion of mothers using the bottle.
4.1. Strengths and limitations
The major strength of our study is its experimental design and the inclusion of a control group who received a voucher of equivalent monetary value to the breast pumps, which allowed us to explore causal relationships between the intervention and breastfeeding outcomes, including maternal goals. Another strength is the inclusion of infants from four countries with significant cultural differences in infant feeding and care, including two where traditional confinement periods are commonly observed. Interestingly, despite differences in baseline characteristics, the findings for all outcomes with respect to randomised groups were similar across study sites, and adjusting primary and secondary outcome analyses for study site did not alter the results, suggesting they are generalizable to women who have established EBF at 3‐ to 4‐week post‐partum.
Our study also has a number of limitations. We did not adjust our sample size for multiple outcomes nor apply any statistical adjustment for multiple testing, and this should be considered when interpreting the findings, particularly as we did not meet our planned target. Our study population consisted of mothers who were EBF at enrolment and the findings cannot therefore be generalised to all mothers and infants in those settings, for example, groups with low breastfeeding rates where provision of a pump early in the post‐partum period might be considered as an incentive for breastfeeding. Interestingly, a recent study in the United Kingdom that explored the views of pregnant women, new mothers, their significant others, and health care professionals about a range of potential incentives for increasing breastfeeding, reported that the provision of a free breast pump costing around £40 was considered the most acceptable option with 67.8% agreement (337/497; Crossland et al., 2016). However, their qualitative research found mixed views around issues including the monetary value of pumps, sharing the load, perceived benefits, perceived risks, and issues related to the timing of any intervention. We did not collect data on the mothers' reasons for expressing milk or their opinions about receiving a pump or vouchers, partly due to the language constraints. However, these are important issues to consider in future research as they may assist in better targeting the provision of breast pumps or other incentives to subgroups who may benefit most.
We paid careful attention when translating study documents into Mandarin and Russian, in particular asking bilingual colleagues to check that the wording of the questionnaires conveyed the same intended meaning in both languages. However, it is impossible to rule out discrepancies. We carefully defined infant feeding categories in the questionnaires but still found some inconsistencies in the responses, for example, to the questions asking about EBF versus those asking if other fluids or solid foods had been introduced. However, these occurred in all three groups, and we do not consider they would have systematically biased the findings. Furthermore, either excluding four subjects with a discrepancy in responses to the questions on EBF at 6 months and the introduction of solid foods or formula before 6 months, or including them as EBF at 6 months, did not alter the findings.
5. CONCLUSION
In this multicountry trial, we found similar efficacy for two single‐electric breast pumps with different design characteristics. Although one pump received better ratings for certain consumer characteristics, these did not predict the amount of milk expressed, use of the pump or breastfeeding practices. Provision of a breast pump to mothers who had already established EBF at 3‐ to 4‐week post‐partum did not significantly influence breastfeeding practices at 3 or 6 months. Mothers randomised to receive a pump were significantly more likely to express milk and to feed it to their infant and this was, in turn, associated with lower rates of EBF at 6 months, although there was no effect on other categories of breastfeeding. Future research should investigate the provision of breast pumps on breastfeeding outcomes in a larger sample, and also in different populations, including mothers from groups where breastfeeding rates are particularly low, as well as exploring mothers' opinions and motivations and the use of breast pumps as an incentive to promote breastfeeding.
CONFLICTS OF INTEREST
MF and KK receive an unrestricted research donation from Philips Avent. MF has lectured at scientific meetings organised by Prolacta Bioscience. RS has received research funding from Abbott nutrition and is a speaker for Prolacta Biosciences.
CONTRIBUTIONS
MF and KK were involved in the study concept and design. All the authors designed the protocol, translated the document, and collected the data. MF and KK analysed the data and drafted the manuscript. All the authors contributed to the critical input and revision of manuscript.
Supporting information
Figure S1. Milk weight (g) expressed at 1 minute intervals at 5–6 weeks, according to study site (Russia, China, UK) for i) First breast, ii) Second breast
Data S1 Supporting information
Data S2 Supporting information
Data S3 Supporting information
Data S4 Supporting information
Data S5 Supporting information
Data S6 Supporting information
Table S1. Baseline characteristics by study site
Table S2. Infant feeding at 3 and 6 months by study site
ACKNOWLEDGMENTS
The authors thank the mothers and infants who participated in the study and the research nurses who collected data (UK: Kim Lee Loh, China: Dong JQ, Russia: Nadezhda Stepanova).
Fewtrell M, Kennedy K, Lukoyanova O, et al. Short‐term efficacy of two breast pumps and impact on breastfeeding outcomes at 6 months in exclusively breastfeeding mothers: A randomised trial. Matern Child Nutr. 2019;15:e12779 10.1111/mcn.12779
REFERENCES
- Ahluwalia, I. B. , Tessaro, I. , Grummer‐Strawn, L. M. , MacGowan, C. , & Benton‐Davis, S. (2000). Georgia's breastfeeding promotion program for low‐income women. Pediatrics, 105(6), E85. [DOI] [PubMed] [Google Scholar]
- Bliss, M. C. , Wilkie, J. , Acredolo, C. , Berman, S. , & Tebb, K. P. (1997). The effect of discharge pack formula and breast pumps on breastfeeding duration and choice of infant feeding method. Birth, 24, 90–97. 10.1111/j.1523-536X.1997.tb00347.x [DOI] [PubMed] [Google Scholar]
- Bream, E. , Li, H. , & Furman, L. (2017). The effect of breast pump use on exclusive breastfeeding at 2 months postpartum in an inner‐city population. Breastfeeding Medicine, 12, 149–155. 10.1089/bfm.2016.0160 [DOI] [PubMed] [Google Scholar]
- Burton, P. , Deng, J. , MacDonald, D. , & Fewtrell, M. S. (2013). Real time 3D ultrasound imaging of infant tongue movements during breast feeding. Early Human Development, 89(9), 635–641. 10.1016/j.earlhumdev.2013.04.009 [DOI] [PubMed] [Google Scholar]
- Burton, P. , Kennedy, K. , Ahluwalia, J. S. , Nicholl, R. , Lucas, A. , & Fewtrell, M. S. (2013). Randomised trial comparing the effectiveness of 2 electric breast pumps in the NICU. Journal of Human Lactation, 29(3), 412–419. 10.1177/0890334413490995 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control & Prevention . (2009). Infant Feeding Practices Study II: The Questionnaires. Available at https:\\www.cdc.gov/ifps/questionnaires.html
- Crossland, N. , Thomson, G. , Morgan, H. , MacLennan, G. , Campbell, M. , Dykes, F. , & Hoddinott, P. (2016). Breast pumps as an incentive for breastfeeding: A mixed methods study of acceptability. Maternal & Child Nutrition, 12, 726–739. 10.1111/mcn.12346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dungy, C. I. , Christensen‐Szalanski, J. , Losch, M. , & Russell, D. (1992). Effect of discharge samples on duration of breast‐feeding. Pediatrics, 90, 233–237. [PubMed] [Google Scholar]
- Fewtrell, M. S. , Lucas, P. , Collier, S. , Singhal, A. , Ahluwalia, J. S. , & Lucas, A. (2001). Randomised trial comparing the efficacy of a novel manual breast pump with a standard electric breast pump in mothers who delivered preterm infants. Pediatrics, 107, 1291–1297. 10.1542/peds.107.6.1291 [DOI] [PubMed] [Google Scholar]
- Fewtrell, M. , Lucas, P. , Collier, S. , & Lucas, A. (2001). Randomised study comparing the efficacy of a novel manual breast pump with a mini‐electric breast pump in mothers of term infants. Journal of Human Lactation, 7(2), 126–131. [DOI] [PubMed] [Google Scholar]
- Fewtrell, M. S. , Kennedy, K. , Nicholl, R. , Khakoo, A. , & Lucas, A. (2012). Infant feeding bottle design, growth and behaviour: Results from a randomised trial. BMC Research Notes, 5, 150 10.1186/1756-0500-5-150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes, D. K. , Prince, C. B. , Espinueva, V. , Fuddy, L. J. , Li, R. , & Grummer‐Strawn, L. M. (2008). Comparison of manual and electric breast pumps among WIC women returning to work or school in Hawaii. Breastfeeding Medicine, 3, 3–10. 10.1089/bfm.2007.0022 [DOI] [PubMed] [Google Scholar]
- Kent, J. C. , Ramsay, D. T. , Doherty, D. , Larsson, M. , & Hartmann, P. E. (2003). Response of breasts to different stimulation patterns of an electric breast pump. Journal of Human Lactation, 19, 179–186. 10.1177/0890334403252473 [DOI] [PubMed] [Google Scholar]
- Labiner‐Wolfe, J. , Fein, S. B. , Shealy, K. R. , & Wang, C. (2008). Prevalence of breast milk expression and associated factors. Pediatrics, 122, S63–S68. 10.1542/peds.2008-1315h [DOI] [PubMed] [Google Scholar]
- Lucas, A. , & James‐Roberts, I. (1998). Crying, fussing and colic behaviour in breast‐and bottle‐fed infants. Early Human Development, 53(1), 9–18. 10.1016/S0378-3782(98)00032-2 [DOI] [PubMed] [Google Scholar]
- Lucas A, St James‐Roberts I. Colic, Crying Fussing and Feeding. Ross 1994: Paediatric Research Conference, USA.
- Meehan, K. , Harrison, G. G. , Afifi, A. A. , Nickel, N. , Jenks, E. , & Ramirez, A. (2008). The association between an electric pump loan program and the timing of requests for formula by working mothers in WIC. Journal of Human Lactation, 24, 150–158. 10.1177/0890334408316081 [DOI] [PubMed] [Google Scholar]
- Moran, V. H. , Morgan, H. , Rothnie, K. , MacLennan, G. , Stewart, F. , Thomson, G. , … Hoddinott, P. (2015). Incentives to promote breastfeeding: A systematic review. Pediatrics, e687, 135. [DOI] [PubMed] [Google Scholar]
- Pang, W. W. , Bernard, J. Y. , Thavamani, G. , Chan, Y. H. , Fok, D. , Soh, S. E. , … Chong, Y. S. (2017). Direct vs. expressed breast milk feeding: Relation to duration of breastfeeding. Nutrients, 9, E547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Position Statement: Breastfeeding in the UK . Royal College of Paediatrics and Child Health, August (2017). https://www.rcpch.ac.uk/system/files/protected/news/ WEBSITE%20FINAL%20Breastfeeding%20Position%20Statement%20280717_0.pdf
- Rasmussen, K. M. , Dieterich, C. M. , Zelek, S. T. , Altabet, J. D. , & Kjolhede, C. L. (2011). Interventions to increase the duration of breastfeeding in obese mothers: The Bassett Improving Breastfeeding Study. Breastfeeding Medicine, 6, 69–75. 10.1089/bfm.2010.0014 [DOI] [PubMed] [Google Scholar]
- Renfrew M, Pokhrel, S. , Quigley, M. , McCormick, F. , Fox‐Rushby, J. , Dodds, R. , … Williams, A. (2012). Preventing disease and saving resources: The potential contribution of increasing breastfeeding rates in the UK. http://www.unicef.org.uk/Documents/Baby_Friendly/Research/Preventing_disease_saving_resources.pdf2010 IFS2. [DOI] [PubMed]
- Rollins, N. C. , Bhandari, N. , Hajeebhoy, N. , Horton, S. , Lutter, C. K. , Martines, J. C. , … on behalf of The Lancet Breastfeeding Series Group . (2016). Why invest, and what it will take to improve breastfeeding practices? Lancet, 387, 491–504. 10.1016/S0140-6736(15)01044-2 [DOI] [PubMed] [Google Scholar]
- Schwartz, K. , D'Arcy, H. J. , Gillespie, B. , Bobo, J. , Longeway, M. , & Foxman, B. (2002). Factors associated with weaning in the first 3 months postpartum. The Journal of Family Practice, 51, 439–444. [PubMed] [Google Scholar]
- Sciacca, J. P. , Phipps, B. L. , Dube, D. A. , & Ratliff, M. I. (1995). Influences on breast‐feeding by lower‐income women: An incentive‐based, partner‐supported educational program. Journal of the American Dietetic Association, 95, 323–328. 10.1016/S0002-8223(95)00083-6 [DOI] [PubMed] [Google Scholar]
- UK Infant Feeding Survey . (2010). http://data.gov.uk/dataset/infant-feeding-survey-2010
- Victora, C. G. , Bahl, R. , Barros, A. J. D. , … for The Lancet Breastfeeding Series Group . (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet, 387, 475–490. 10.1016/S0140-6736(15)01024-7 [DOI] [PubMed] [Google Scholar]
- Weisband, Y. L. , Keim, S. A. , Keder, L. M. , Geraghty, S. R. , & Gallo, M. F. (2017). Early breast milk pumping intention among postpartum women. Breastfeeding Medicine, 12, 28–32. 10.1089/bfm.2016.0142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Win, N. N. , Binns, C. W. , Zhao, Y. , Scott, J. A. , & Oddy, W. A. (2006). Breastfeeding duration in mothers who express milk: A cohort study. International Breastfeeding Journal, 1, 28 10.1186/1746-4358-1-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) , 55th World Health Assembly. Infant and young child nutrition. World Health Organization, (2002) (WHA55.25). http://apps.who.int/gb/archive/pdf_files/WHA55/ewha5525.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Milk weight (g) expressed at 1 minute intervals at 5–6 weeks, according to study site (Russia, China, UK) for i) First breast, ii) Second breast
Data S1 Supporting information
Data S2 Supporting information
Data S3 Supporting information
Data S4 Supporting information
Data S5 Supporting information
Data S6 Supporting information
Table S1. Baseline characteristics by study site
Table S2. Infant feeding at 3 and 6 months by study site


