Abstract
Synthesis of effects of infant feeding interventions to prevent childhood obesity is limited by outcome measurement and reporting heterogeneity. Core outcome sets (COSs) represent standardised approaches to outcome selection and reporting. The aim of this review is to identify feeding outcomes used in infant feeding studies to inform an infant feeding COS for obesity prevention interventions. The databases EMBASE, Medline, CINAHL, CENTRAL, and PsycINFO searched from inception to February 2017. Studies eligible for inclusion must examine any infant feeding outcome in children ≤1 year. Feeding outcomes include those measured using self‐report and/or observational methods and include dietary intake, parent–child interaction, and parental beliefs, among others. Data were extracted using a standardised data extraction form. Outcomes were assigned to outcome domains using an inductive, iterative process with a multidisciplinary team. We identified 82 unique outcomes, representing nine outcome domains. Outcome domains were “breast and formula feeding,” “introduction of solids,” “parent feeding practices and styles,” “parent knowledge and beliefs,” “practical feeding,” “food environment,” “dietary intake,” “perceptions of infant behaviour and preferences,” and “child weight outcomes.” Heterogeneity in definition and frequency of outcomes was noted in reviewed studies. “Introduction of solids” (59.5%) and “breastfeeding duration” (55.5%) were the most frequently reported outcomes. Infant feeding studies focus predominantly on consumption of milks and solids and infant weight. Less focus is given to modifiable parental and environmental factors. An infant feeding COS can minimise heterogeneity in selection and reporting of infant feeding outcomes for childhood obesity prevention interventions.
Keywords: “childhood obesity”, “complementary feeding”, “core outcome set”, “food and nutrient Intake”, “infant feeding”, nutrition
Key messages.
There is considerable heterogeneity in infant feeding outcomes in the extant literature.
The most commonly examined infant feeding outcomes are “introduction of solids” and “breastfeeding duration.”
Greater attention needs to be given to modifiable parental behavioural and environmental outcomes.
Development of a standardised core outcome set of infant feeding outcomes for childhood obesity prevention interventions is essential to effectively synthesise and interpret effects of childhood obesity prevention interventions.
1. INTRODUCTION
Childhood obesity is a significant risk factor for diabetes (Bacha & Gidding, 2016), respiratory problems (Mohanan, Tapp, McWilliams, & Dulin, 2014), cardiovascular dysfunction (Cote, Harris, Panagiotopoulos, Sandor, & Devlin, 2013), and poor psychological health (Beck, 2016). Childhood obesity also tracks to adulthood, leading to an increased risk of later morbidity and mortality (Maffeis & Tato, 2001). Recent evidence suggests that despite some stabilisation of childhood obesity, rates remain high (Ogden et al., 2016). A recent examination of eight European countries identified that rates of obesity among children under 10 years were 7% (Ahrens et al., 2014). American data indicate that 9.4% of children aged 2–6 years, and 19.6% of children aged 6–11 years, were obese in 2013–2014 (Ogden et al., 2016).
Early infant feeding practices are associated with increased risk of childhood obesity. For instance, earlier introduction of solids (Pearce & Langley‐Evans, 2013), shorter duration of breastfeeding (Modrek et al., 2017), poor dietary intake (Pearce & Langley‐Evans, 2013), and nonresponsive parent–infant feeding interactions (DiSantis, Hodges, Johnson, & Fisher, 2011) are implicated in the development and maintenance of childhood obesity. The first 2 years of life represent a critical window for establishing healthy feeding behaviours and infant dietary habits (Woo Baidal et al., 2016). During the first 12 months specifically, infants undergo rapid developmental changes and concurrently changing feeding needs (Brown & Lee, 2011; Taylor et al., 2017). Although feeding of breast and formula milk has been widely studied and consistently associated with later child weight outcomes, including risk of later child obesity (Modrek et al., 2017), there is also increasing empirical focus on complementary feeding in the aetiology of obesity (DiSantis et al., 2011; Pearce & Langley‐Evans, 2013;Woo Baidal et al., 2016). This is because the transition to complementary foods that occurs during the weaning period in the first year demonstrates important associations with later weight and dietary patterns (Brown & Lee, 2011; Taylor et al., 2017). Thus, complementary feeding can be seen as a distinct and important behavioural domain for obesity prevention.
As a result, there is increased research interest in developing and evaluating complementary infant feeding interventions in the first year to prevent childhood obesity (Redsell et al., 2016). Recent reviews of infant complementary feeding interventions highlight inconsistent or minimal effects on feeding practices, dietary intakes, or weight outcomes (Blake‐Lamb et al., 2016; Matvienko‐Sikar et al., 2017; Redsell et al., 2016; Reilly, Martin, & Hughes, 2017). One potential reason for inconsistencies across trials may relate to heterogeneity in outcome reporting, definition, and measurement (Matvienko‐Sikar et al., 2017). Lack of standardisation of infant complementary feeding outcomes limits synthesis and comparison of infant feeding intervention effects and impairs evaluation and examination of the mechanisms of change underpinning childhood obesity prevention interventions (Matvienko‐Sikar et al., 2017).
Core outcomes sets (COSs) are standardised sets of outcomes, developed to improve outcome selection and measurement for specific health topics (Williamson et al., 2012). COSs are defined as the “minimum that should be measured and reported in all clinical trials of a specific condition and could also be suitable for use in other types of research and clinical audit” (Clarke, 2007). Development of a COS does not therefore restrict studies to only examining these outcomes but represents the minimum outcome set to collect and report (Williamson et al., 2017). Development of COS is supported by the Core Outcome Measures in Effectiveness Trials (COMET) initiative, with guidance recently published in the COMET handbook version 1 (Williamson et al., 2017). COS development typically follows three interrelated consecutive stages: a systematic review to identify all existing outcomes; a Delphi survey to identify and prioritise important outcomes for inclusion in the COS; and an in‐person consensus meeting of relevant stakeholders to achieve consensus on the most essential outcomes for inclusion in a COS for a specific health topic. This process focuses on what to measure rather than how outcomes should be measured and involves multiple stakeholder perspectives to achieve consensus on the COS.
Development of a COS for trials of infant feeding interventions for prevention of childhood obesity is timely and crucial (Matvienko‐Sikar et al., 2017). This is particularly evident in light of the importance of initiation and maintenance of healthy early feeding practices in the first year of life and the increased empirical focus on intervention delivery during this period. Given the increasing focus on complementary feeding particularly, which moves beyond a focus on breastfeeding only, development of a COS in the area of complementary feeding is warranted. Inclusion of standardised outcomes across trials will facilitate improved synthesis and comparison of intervention effects to better determine the most effective approaches to improving infant feeding practices and/or preventing childhood obesity. The first stage in development of such a COS is identifying potentially relevant outcomes from the extant literature (Matvienko‐Sikar et al., 2017; Williamson et al., 2017). This paper reports a systematic review of the extant feeding literature of infants up to 1 year to identify all potential infant feeding outcomes for inclusion in a COS of interventions to prevent childhood obesity. A secondary aim is to examine heterogeneity of outcome reporting across studies.
2. METHODS
This review was performed and reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses guidelines for systematic reviews (Moher, Liberati, Tetzlaff, Altman, & Grp, 2009). The protocol for this systematic review is registered on PROSPERO, registration number: CRD42017055608. This COS project is registered on the COMET database, and further details are available at http://www.comet-initiative.org. The protocol for development of this COS is published (Matvienko‐Sikar et al., 2017).
2.1. Eligibility of studies
2.1.1. Inclusion criteria
Studies examining at least one infant feeding outcome in children up to 1 year of age were eligible for inclusion. Feeding outcomes were defined as any feeding‐related outcome measured up to 1 year of age. Outcomes measured using self‐report and observational methods were eligible, including outcomes such as dietary intake, parent–child interaction, milk and solids consumption, and parental beliefs, among others. Types of studies included in the current review were not limited to obesity‐focused examinations. This is because the authors acknowledge that suitable outcomes for trials of obesity prevention interventions may arise from existing research that is not obesity focused. Studies were not therefore required to be trials of infant feeding interventions and could include observational, quasi‐experimental, and randomised control trial designs.
2.1.2. Exclusion criteria
The following types of studies were not eligible for exclusion: Studies only examining outcomes in children over 1 year of age; studies involving children with malnutrition or ongoing medical conditions related to feeding; studies focusing on dental caries. Studies focusing on breastfeeding only were also excluded as the authors acknowledge such studies may require a dedicated breastfeeding‐specific COS. There were no restrictions on child sex or ethnicity, but the search was limited to literature published in English, and grey literature was not examined.
2.2. Search strategy
The following databases were searched from inception to February 2017: EMBASE, MEDLINE, CINAHL, the Cochrane Library, and PsychINFO. Search terms were required to be reported in the title, abstract, and/or study keyword and were modified for databases as needed: (“Infant” OR infancy OR “child” OR “children” OR “paediatric” OR “pediatric” OR “baby” OR “parent*” OR “parent*”) AND (“diet*” OR “feeding” OR “early feeding” OR “complementary feeding” OR “complementary food” OR “weaning” OR “feeding interaction*” OR “nutrition” OR “solid food” OR “first food” OR “responsive feed*” OR “anticipatory guid*” OR “baby led” OR “feed* practice*” OR “eating behav*” OR “food preference”) AND (“Randomised controlled trial*” OR “randomized controlled trial” OR “RCT*” OR “control* group” OR “controlled trial”) OR (“cohort” OR “observational” OR “pilot study” OR “case‐control study” OR “quasi‐experiment*”). Reference lists of identified articles were also examined.
2.3. Study selection and data extraction
All study titles, abstracts, and full texts were independently screened by two researchers (K. M. S. and N. McG.) against eligibility criteria. Any disagreements were discussed until resolved by consensus. Relevant study characteristics were independently extracted using a standardised data extraction form (see Data S1) by two researchers (N. McG. and C. G.). The data extraction file was developed for the purposes of this review and required data on paper characteristics, study characteristics, participant details, and outcomes examined. Data extraction for half of all studies was checked by a third researcher (K. M. S.). Data extracted included author, year of publication, study design, sample size, study setting, participant characteristics, study outcomes, and outcome measurement tool. Outcomes reported in the methods and/or results were included. As one aim of this review is to examine heterogeneity of outcome reporting, each article was treated as a unique study.
2.4. Quality assessment
Quality assessment of all included studies was conducted by one reviewer (C. G.), with a randomly selected 33% of these independently assessed by a second reviewer (K. M. S.). This was done to determine if study quality influenced frequency or heterogeneity of outcome reporting between or within studies. Quality was assessed using six items previously outlined in a COS for neonatal abstinence syndrome (Kelly et al., 2016). Items included assessing if primary and secondary outcomes are clearly stated and defined, if authors explain outcome selection, and whether methods were used to enhance quality of outcome measurement (Kelly et al., 2016).
2.5. Assessment of outcome reporting
All outcomes identified from data extraction were compiled into a long list of infant feeding outcomes. Based on previous evidence (Kapadia et al., 2015), it was expected that outcome terminology and assessment would vary. Outcomes determined to have similar definitions or themes were therefore merged. This was done via a consensus process with a group of researchers with experience and expertise in conducting infant feeding and childhood obesity research. The group comprised two health psychologists with experience in childhood obesity and of developing COSs (K. M. S. and M. B.), a developmental psychologist (C. H.), and a nutritionist (C. K.). A midwife with expertise in COS development and trials (D. D.) was also consulted during this process. Outcomes were initially grouped into outcome domains representing the overarching outcome area based on conceptual similarities of outcomes by K. M. S., with all outcome domains subsequently reviewed and discussed with M. B., C. K., and C. H.
Outcome matrices based on the Outcome Reporting Bias in Trials project outcome matrix (Kirkham et al., 2010), and as recommended by the COMET initiative (Williamson et al., 2017), were constructed to visually represent the frequency, consistency, and disparity of outcome reporting across studies. Individual matrices were created for each outcome domain. Each matrix included the outcome or outcome domain on the X axis and the reviewed studies reporting these on the Y axis. The frequency of reporting of individual outcomes was calculated for all studies in this review. The frequency with which overarching outcome domains were included in reporting across studies was also calculated; this was done by calculating the number of studies that reported outcomes that are grouped under each of the nine outcome domains.
3. RESULTS
The literature search identified 13,838 unique citations. Titles and abstracts of all articles were screened against inclusion criteria. Following this, full texts of 575 articles were evaluated against inclusion criteria; 126 articles were deemed eligible for inclusion in this review (see Figure 1).
Figure 1.
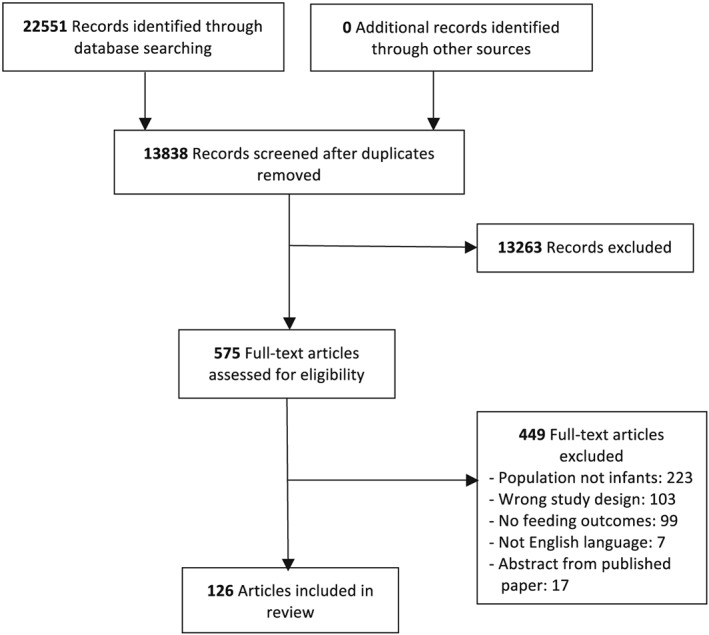
Systematic review flow chart
3.1. Study characteristics
Study characteristics are presented in Table 1. The majority of articles reported were longitudinal/cohort studies (n = 81); 27 were randomised controlled trials; 13 were cross‐sectional; 2 were repeated measure interventions; 1 was a case–control comparative study; 1 was a nonrandomised controlled trial; and 1 was a study protocol. Studies were conducted in the United States (25%), the United Kingdom (19%), and Australia (14%). The majority of studies (97.62%) were rated as being of high quality (see Table 1); thus, further sensitivity analyses related to study quality were not conducted.
Table 1.
Characteristics of included studies (n = 126)
| Study (Author, year) | Design | Study setting | Participants (n) | Child age at outcome assessment | Study focus | Quality of outcome reporting |
|---|---|---|---|---|---|---|
| Abdul Raheem et al., 2013 | Longitudinal | Maldives | 458 | 1, 3, and 6 months | Maternal depression, infant feeding, and growth | High |
| Abraham et al., 2012 | Longitudinal | Scotland | 4,493 | 9–12 months; 19–24 months | Infant feeding, eating patterns, and weight status | High |
| Andersen et al., 2015a | Longitudinal | Denmark | 513 | Birth and 9 months | Maternal obesity and offspring dietary patterns | High |
| Andersen et al., 2015b | Longitudinal | Denmark | 374 | 9 months | Infant dietary patterns | High |
| Ashman et al., 2016 | Longitudinal | Australia | 67 | 3, 6, 9, and 12 months | Dietary intake and anthropometric status of mothers and infants | High |
| Baird et al., 2008 | Longitudinal | UK | 1,740 | 6 and 12 months | Feeding, dietary patterns, and infant weight | High |
| Betoko et al., 2013 | Longitudinal | France | 1,004 | Birth, 4, 8, and 12 months | Infant feeding patterns | High |
| Binns et al., 2007 | Longitudinal | Australia | 453 | 12 months | Cow's milk consumption | High |
| Black et al., 2001 | RCT | USA | 181 | 3 months | Early complementary feeding | High |
| Bonuck et al., 2014 | RCT | USA | 464 | 12 months | Bottle use | High |
| Bonuck et. al, 2010 | Repeated measures intervention | USA | 299 | 12 and 24* months | Bottle weaning intervention and toddler overweight | High |
| Boudet‐Berquier et al., 2016 | Longitudinal | France | 2,732 | 12 months | Introduction of complementary foods | High |
| Braid et al., 2014 | Longitudinal | USA | 7,650 | 9 months | Early introduction of complementary foods in preterm infants | High |
| Brekke et al., 2007 | Longitudinal | Sweden | 10,762 | Birth and follow‐up at median 12 (SD 1.1) months | Consumption of high sugar, low nutrient foods | High |
| Brodribb et al., 2013 | Longitudinal | Queensland, Australia | 6,470 | 17 weeks/4 months | Introduction of solids and water | High |
| Bronte‐Tinkew et al., 2007 | Longitudinal | USA | 8,693 | 9 months | Food insecurity, toddlers' overweight (weight for length), physical health, and length for age | High |
| Brown et al., 2015 | Longitudinal | UK | 298 | 6–12 (M = 8.34 months), 18–24* months | Child satiety responsiveness | High |
| Bruun et al., 2016 | Longitudinal | Denmark | 499 | 3 days to 16 weeks | Breastfeeding and introduction of complementary foods | High |
| Bryanton et al., 2007 | Longitudinal | Canada | 175 | 12 and 24 hr post‐partum and 1 month | Birth experience and post‐partum parenting including feeding | High |
| Cameron et al., 2014 | RCT | Australia | 389 | 4 months and 20* months | Effectiveness of INFANT trial on dietary intake | High |
| Cameron et al., 2015 | RCT | New Zealand | 802 | 4 months | Intervention effects on introduction of complementary foods | Moderate |
| Campbell et al., 2013 | RCT | Melbourne, Australia | 239 | 4, 9, and 20* months | Intervention effects on obesity risk behaviours and infant BMI | High |
| Carletti et al., 2017 | Longitudinal | Italy | 148 | 3, 6, 9, 12, 18*, 24*, and 36* months | Introduction of complementary foods | Low |
| Cartagena et al., 2016 | Cross‐sectional | USA | 62 | 4 and 12 months | Modifiable feeding practice by overweight status | High |
| Cassells et al., 2014 | RCT | Australia | 244 | 4 months | Maternal infant feeding practices and beliefs, and infant neophobia | High |
| Castro et al., 2015 | Cross‐sectional | Ireland | 11,134 | 17 weeks | Complementary feeding determinants | High |
| Chivers et al., 2010 | Longitudinal | Australia | 1,403 | 12 months (24* months and 36 months) | Body mass index, adiposity rebound, and infant feeding | High |
| Chu et al., 2012 | Longitudinal | Canada | 246 | 12 months | Maternal physical activity, infant feeding practices, and infant weight gain | High |
| Dancel et al., 2015 | Cross‐sectional | USA | 398 | 12 months | Acculturation and feeding styles | High |
| de Campora et al., 2016 | Longitudinal | Italy | 53 | 7 and 12 months | Emotional dysregulation and obesity risk | High |
| de Hoog et al., 2011 | Longitudinal | The Netherlands | 2,998 | 6 months | Infant feeding and ethnic differences in infant growth (including weight, length and weight‐for‐length during the first 6 months of life) | High |
| de Oliviera et al., 2012 | RCT | Brazil | 163 | 6 months | Prevention of early introduction to solids and nonbreast milk | High |
| Emmett et al., 2000 | Longitudinal | UK | 1,178 | 4 and 8 months | Drink consumption | High |
| Emmett et al., 2016 | Longitudinal | UK | n > 11,000 | 6 and 15* months | Dietary patterns during complementary feeding | High |
| Fairley et al., 2015 | Longitudinal | UK | 987 | 6, 12, and 24* months | Modifiable risk factors for obesity and BMI | High |
| Faith et al., 2006 | Cross‐sectional | USA | 971 | 7 and 12 months | Fruit juice consumption and adiposity gain | High |
| Farrow et al., 2006 | Cross‐sectional | UK | 69 | 6 months | Maternal feeding control and infant weight gain | High |
| Fildes et al., 2015a | Longitudinal | UK | 1,920 | 8 months | Parental control of infant feeding. Influence of infant weight, appetite, and feeding method | High |
| Fildes et al., 2015b | Cross‐sectional | UK, Greece, and Portugal | 139 | 1 month after introduction of solids | Increasing vegetable acceptance in infancy | High |
| Gatica et al., 2012 | Longitudinal | Brazil | 4,231 | 3, 12, 24*, 48* months | Food intake variations by SES and behavioural characteristics | High |
| Gondolf et al., 2012 | Cross‐sectional | Denmark | 312 | 9 months | Dietary habits of partly breastfed and completely weaned infants | High |
| Gooze et al., 2011 | Longitudinal | USA | 9,850 | 9 and 24* months | Prolonged bottle use and obesity risk | High |
| Griffiths et al., 2007 | Longitudinal | UK | 18,150 | 9 months | Ethnic variations in infant feeding practices | High |
| Griffiths et al., 2009 | Longitudinal | UK | 10,533 | 9 months | Infant feeding practices and weight gain | High |
| Grimm et al., 2014 | Longitudinal | USA | 1,078 | 10.5 months | Fruit and vegetable intake | High |
| Groner et al., 2009 | Protocol | USA | 34 | 12 months | Obesity prevention | High |
| Gross et al., 2016 | RCT | USA | 456 | 3 months | Obesity prevention intervention on infant feeding practices | High |
| Hamilton et al., 2011 | Longitudinal | Australia | 375 | 3 and 7 months | Decisions to introduce complementary feeding | High |
| Hampson et al., 2011 | Longitudinal | Norway | 37,919 | 6 months | Prenatal negative affectivity and food choices for infants | High |
| Hohman et al., 2017 | RCT | USA | 279 | Ages 3, 16, 28, and 40 weeks | Intervention effects on infant dietary patterns | High |
| Hoppe et al., 2004 | Longitudinal | The Netherlands | 142 | 9 months | Protein intake, body size, and body fat | High |
| Horodynski et al., 2015 | RCT | USA | 100 | 3 and 6 months | Intervention for obesity reduction | High |
| Howe et al., 2015 | Longitudinal | New Zealand | 687 | 3 months | Ethnic differences in obesity risk factors | High |
| Huh et al., 2011 | Longitudinal | USA | 847 | 6 months | Introduction of solids and obesity risk | High |
| Jacknowitz et al., 2007 | Longitudinal | USA | 5,276 | 9 months | WIC effects on infant feeding | High |
| Jiang et al., 2016 | Repeated measures intervention | China | 582 | 12 months | Intervention effects on BMI | High |
| Johnson et al., 1993 | RCT | Ireland | 262 | 12 months | Effects of child development programme | High |
| Kim & Peterson, 2008 | Cross‐sectional | USA | 8,150 | 9 months | Childcare effects on feeding practices and weight gain | High |
| Klingberg et al., 2016 | Longitudinal | Sweden | 9,727 | After birth, throughout first year, 12 months | Introduction of complementary foods | High |
| Koh et al., 2014 | Cross‐sectional | Australia | 277 | M = 27 weeks (SD = 3.2) | Maternal self‐efficacy and fruit and vegetable intake | High |
| Kronberg et al., 2014 | Cross‐sectional | Denmark | 4,503 | 6 months | Early introduction to solids | High |
| Kupers et al., 2015 | Longitudinal | The Netherlands | 2,475 | 1, 6, 12*, and 24* months | Infant weight gain | High |
| Lande et al., 2005 | Longitudinal | Norway | 1,825 | 6 and 12 months old | Birth size, feeding practices, and BMI | High |
| Launer et al., 1992 | Longitudinal | Israel | 318 | 6, 12, and 18* months | Maternal recall of feeding events | High |
| Layte et al., 2014 | Longitudinal | Ireland | 11,134 | Birth, 9 months old, and 3 years* old | SES and rapid infant growth | High |
| Lim et al., 2016 | Longitudinal | Singapore | 486 | 6, 9, and 12 months | Dietary pattern trajectory | High |
| Lin et al., 2013 | Longitudinal | Hong Kong | 3,390 | <3, 3–4, 5–6, 7–8, and >8 months | Timing of solid food introduction and obesity | High |
| Lindberg et al., 1996 | Case–control comparative study | Sweden | 48 | 5.3 +/− 1.99 months in nurse‐identified cases and 6 +/− 2.32 months in parent‐identified cases | Maternal infant interactions during food refusal | High |
| Llewellyn et. al., 2010 | Longitudinal | UK | 2,402 pairs (twins) | M = 8.2 (SD = 2.18) months | Appetitive traits that have been shown to be heritable later in childhood | High |
| Llewellyn et. al., 2012 | Longitudinal | UK | 2,402 pairs (twins) | M = 8.2 (SD = 2.18) months | Inheritable susceptibility to adiposity | High |
| Mihrshahi et al., 2011 | RCT | Australia | 612 | 4.3 ± 1.0 (months) | Intervention effects on rapid weight gain | High |
| Moschonis et al., 2013 | RCT | Greece, UK, and Portugal | 283 | 2 tests between 5 and 12 months | Intervention to increase vegetable liking and consumption | Low |
| Newby et al., 2014 | Longitudinal | Australia | 462 | 4 and 6 months | Introduction of complementary foods | High |
| O′ Donovan et al., 2015 | Longitudinal | Ireland | 823 | 2 days and 2, 6, and 12 months | Adherence with early infant feeding and complementary feeding guidelines | High |
| Okubo et al., 2015 | Longitudinal | UK | 1,018 | *Ages 6 and 12 months, and 3 and 6 years | Diet quality and adiposity | High |
| Oliveira et al., 2015 | Longitudinal | Portugal, UK, and France | 1,280 | 4*, 12, and 48 months | Birth weight and eating behaviours | High |
| Park et al., 2014 | Longitudinal | USA | 1,333 | ∼3 weeks and 2, 3, 4, 5, 6, 7, 9, 10, and 12 months of age, and 6 years* | Influence of sugar‐sweetened beverage intake during infancy | High |
| Parkinson et al., 2009 | Longitudinal | UK | 583 | 6* weeks, 4, 8, 12, and 30 months, at 5–6 years | Infant appetite correlating with child eating behaviour | High |
| Paul et al., 2011 | RCT | USA | 160 | 2–3 weeks, 4–6 months, 1 year | Intervention to prevent obesity | High |
| Pimpin et al., 2016 | Longitudinal | UK | 2,154 |
Infant feeding data at M = 8 (SD = 2.2) Dietary data at 21 months Weight and height every 3 months, from birth to 5 years* |
Dietary protein intake, association with body mass index and in children up to 5 years of age | High |
| Pontin et al., 2007 | Longitudinal | UK | 11,490 | 4 weeks, 6 months, and 15* months | Breastfeeding pattern | High |
| Quah et al., 2015 | Longitudinal | Singapore | 210 | Ages 3, 6, 9, 12, 15*, 18*, and 24* months | Appetitive traits, body mass index, and weight gain | High |
| Quah et al., 2016 | Longitudinal | Singapore | 1,237 | At birth, data from 0 to 6 months, and 15 months* | Maternal feeding beliefs and practices | High |
| Qiu et al., 2008 | Longitudinal | China | 1,520 | 1, 3, and 6 months | Infant feeding practices | High |
| Reat et al., 2015 | Cross‐sectional | USA | 196 | M = 11.4 (SD = 5.6) months | Dietary intake and feeding practices | High |
| Rebhan et al., 2009 | Longitudinal | Germany | 3,103 | 6 days and 2, 4, 6, and 9 months | Infant feeding practices | High |
| Rifas‐Shiman et al., 2011 | Longitudinal | USA | 837 | 6 months, 1 year, and 3* years | Maternal feeding restriction, and childhood obesity | High |
| Robinson et al., 2009 | Longitudinal | UK | 536 | 6 and 12 months | Infant feeding practice, body composition in childhood | High |
| Schack Nielsen et al., 2010 | Longitudinal | Denmark | 5,068 | 1 year | Complementary feeding protect against adult overweight | High |
| Schroeder et al., 2015 | RCT | USA | 278 | 1–24* months (monthly), 3, 4, and 5 years old* | Intervention on early obesity prevention | High |
| Scott et al., 2009 | Longitudinal | Australia | 519 | 4, 10, 16, 22, 32, 40, and 52 weeks post‐partum | Early introduction of solid foods in infants | High |
| Scott et al., 2015 | Longitudinal | Australia | 303 | Birth, 6, 12, 18, and 26 weeks post‐partum | Introduction of complementary foods | High |
| Spence et al., 2013 | RCT | Australia | 528 | 4–19* months approximately | Intervention's impact on diet quality in early childhood | High |
| Spence et al., 2014 | RCT | Australia | 528 | 4–19* months approximately | Intervention (InFANT) to improve child diet quality | High |
| Tang et al., 2015 | Longitudinal | China | 695 | 1, 3, and 6 months post‐partum | Early introduction of complementary feeding | High |
| Tarrant et al., 2010 | Longitudinal | Ireland | 401 | 6 weeks and 6 months | Weaning practices | High |
| Taveras et al., 2010 | Longitudinal | USA | 1,826 | First and second trimester, few days after birth, 6 months, and 1, 2*, 3*, and 4* years | Racial/ethnic differences in early‐life risk factors for childhood obesity | High |
| Taveras et al., 2011 | Nonrandomised controlled trial | USA | 80 | 6 months | Feasibility of intervention to improve nutrition and physical activity behaviours of mothers and infants | High |
| Thompson et al., 2013a | Longitudinal | USA | 217 | 3, 6, 9, 12, and 18* months of age | Pressuring and restrictive feeding styles, infant feeding and size (African American) | High |
| Thompson et al., 2013b | Longitudinal | USA | 217 | 3, 6, 9, 12, and 18* months of age | Period of infant feeding for the development of disparities in obesity | High |
| Thorisdottir et al., 2011 | Longitudinal | Iceland | 141 | 6, 9, and 12 months | Nutrition and iron status following a revision in infant dietary recommendations, and its association with diet and growth | High |
| Timby et al., 2014 | RCT | Sweden | 213 | <2, 4, 6, and 12 months | Parental feeding control in relation to feeding mode and growth pattern during infancy | High |
| Toh et al., 2016 | Longitudinal | Singapore | 842 | 9 and 12 months | Infant feeding practices (Asian longitudinal) | High |
| Vail et al., 2015 | Longitudinal | UK | 571 | At birth, 3 and 12 months | Age at weaning and infant growth | High |
| Van Der Merwe et al., 2015 | Cross‐sectional | South Africa | 435 | Ranged from 1 day to 5 months | Infant feeding practices | High |
| Van Jaarsveld et al., 2011 | Longitudinal | UK | 2402 pairs of twins | 3, 9, and 15* months | Appetitive traits and weight gain in infancy | High |
| van Jaarsveld et al., 2014 | Longitudinal | UK | 800 | Mean (SD) age was 8.2 (2.2) months | Appetite and growth among siblings | High |
| van Rossem et al., 2013 | Longitudinal | The Netherlands | 3,184 |
Infant feeding outcomes at 12 months Anthropometric outcomes at 1, 2, 3, 4, 6, 11, 14*, 18*, 24*, 30*, 36*, and 45* |
Weight change before and after the introduction of solids | High |
| Vitolo et al., 2012 | RCT | Brazil | 363 | 6 and 16* months | Intervention: maternal dietary counselling, consumption of energy‐dense foods among infants | High |
| Vitolo et al., 2014 | RCT | Brazil | 619 | 6–9 months | Intervention: child feeding training programme for primary health care professionals | High |
| Wasser et al., 2011 | Longitudinal | USA | 217 | 3, 6, 9, 12, and 18 months* | “Fussy” infants and complementary foods before 4 months of age | High |
| Wasser et al., 2013 | Longitudinal | USA | 217 | 3, 6, 9, 12, and 18 months* | Nonmaternal involvement in feeding and dietary intakes among infants and toddlers | High |
| Watt et al., 2009 | RCT | UK | 212 | Approximately 10 weeks, and subsequently 12 and 18* months old | Social support intervention on infant feeding practices | High |
| Wen et al., 2009 | RCT | Australia | 56 | 1, 3, 5, 9, and 12 months | Feasibility of addressing risk factors for childhood obesity through an intervention | High |
| Wen et al., 2011 | RCT | Australia | 258 | 6 and 12 months | Intervention on infant feeding practices and “tummy time” | High |
| Wen et al., 2012 | RCT | Australia | 497 | 6, 12, and 24* months | Intervention on children's BMI at Age 2 | High |
| Woo et al., 2013 | Longitudinal | China, Mexico, and USA | 324 | Weekly between 2 and 52 weeks | Infant feeding practices and anthropometry at age 1 year | High |
| Woo et al., 2015 | Longitudinal | China, Mexico, and USA | 324 | Weekly between 2 and 52 weeks | Infant complementary diet diversity | High |
| Wright et al., 2004 | Longitudinal | UK | 707 | 6 weeks and 4, 8, and 12 months | Early weaning | High |
| Yin et al., 2013 | RCT | USA | 844 | M = 2.1 (SD 0.4) months | Parent health literacy and “obesogenic” infant care behaviours | High |
| Yuan et al., 2016a | Longitudinal | France | 268 | 1–12 months of age, monthly 7‐day food record | Infant dietary exposures to sweetness and fattiness during the first year of life and feeding practices | High |
| Yuan et al., 2016b | Longitudinal | France | 1,142 | 4, 8, and 12 months | Early determinants of food liking among 5‐year‐old children | High |
| Zhang et al., 2009 | RCT | China | 599 | 2–4, 6, 9, 12, 15*, and 18* months of age | Intervention to improve child feeding practices and growth in rural China | High |
| Zhang et al., 2013 | RCT | China | 599 | 2–4 and 10–11 months | Intervention on infant feeding | High |
| Zheng et al., 2015 | Longitudinal | China | 40,510 | 1, 3, and 6 months and 4–5 years* | Complementary feeding and childhood adiposity in preschool‐aged children | High |
| Ziol‐Guest et al., 2010 | Cross‐sectional | USA | 4,450 | 9 months | First‐ and second‐trimester WIC participation and breastfeeding rates and cow's milk introduction during infancy | High |
Note. BMI: body mass index; InFANT: infant feeding activity and nutrition trial; SES: socio‐economic status; WIC: women, infants, and children programme; RCT: randomised controlled trial.
3.2. Study outcomes
Two hundred and thirty‐six outcomes were initially identified (see Data S2). Following review of outcomes and merging of outcomes with similar definitions, 82 unique outcome terms were identified across 126 studies. Outcomes were merged based on similarities in definitions/themes. The 82 outcomes were then grouped into nine outcome domains. These are “breastfeeding and formula feeding,” “introduction of solids,” “parent feeding practices and styles,” “parent knowledge and beliefs,” “practical feeding,” “food environment,” “dietary intake,” “perceptions of infant behaviour and preferences,” and “child weight outcomes.” Individual outcomes are presented in their respective outcome domains in Table 2.
Table 2.
Outcome domains and outcomes
| Outcome | Outcome definition |
|---|---|
| Domain 1. Breastfeeding and formula feeding (n = 15) | |
| Breastfeeding duration | The length of time mothers breastfeed their infants. This can include the length of time mothers exclusively breastfed their infants or the length of time before mothers ceased all breastfeeding |
| Breastfeeding intentions | Parental intentions to initiate breastfeeding and/or intentions relating to duration of breastfeeding |
| Breastfeeding initiation | Whether mothers began breastfeeding their infant, regardless of duration of breastfeeding |
| Breastfeeding frequency | How often infants are breastfed |
| Breastfeeding intensity | How often and for how long the infant is breastfed |
| Exclusive breastfeeding | Feeding the infant only breast milk, without introducing solids or formula |
| Duration of exclusive breastfeeding | The length of time mothers only breastfeed their infants |
| Feeding method (breast milk, formula, solids, and combination) | The method by which the infant is fed. This can include single feeding approaches or a combination of feeding approaches |
| Timing of introduction to formula | The infants age when formula was introduced. This can include combination feeding of breast and formula milk |
| Formula feeding | Whether the infant ever consumed formula milk, rather than routine consumption of formula milk |
| Bottle/formula feeding frequency | How often infants are fed formula milk by bottle |
| Amount/volume formula consumed | The quantity of formula milk consumed |
| Duration of infant formula feeding | The length of time infants consumed formula milk |
| Type of formula fed | The type of formula provided to infants (e.g., early baby and hungry baby) |
| Number of feeds per day of either breastfeeding or formula | The frequency of any milk feeds per day |
| Domain 2. Introduction of solids (n = 6) | |
| Timing of introduction of solids | The infant's age when solids were introduced to the diet. Solids are considered any food or liquid substance, other than breast milk or formula milk |
| Intended age of solids introduction | Parental intentions to introduce solid foods at a certain age. This can be in line with feeding recommendations or not |
| Timing of introduction of certain foods | The infant's age when individual foods and/or liquids were introduced to the diet. These can include overarching food groups (e.g., vegetables) or specific foods within those groups (e.g., carrot, potato, and broccoli) |
| Timing cow's milk introduced | The age at which infants began consuming cow's milk |
| Timing nonmilk drink introduced | The age at which infants began consuming nonmilk drinks |
| Adding solids to bottle | Including solids, such as cereals, to the infant's bottle |
| Domain 3. Parents feeding practices and styles (n = 16) | |
| Instrumental feeding | Using incentives or rewards, such as other preferred foods, to encourage consumption of foods |
| Emotional feeding | Using food to regulate a child's emotions, for instance, giving the child food in response to distress |
| Feeding to soothe | Use of food to prevent or stop infant from crying |
| Restriction | Limiting the child's access to foods. Caregivers can restrict for health or weight control purposes. For instance, restricting “unhealthy” foods or restricting the amount a child eats |
| Pressure | Pressuring or cajoling the child to eat more at mealtimes. For instance, insisting the child finishes everything on their plate |
| Modelling | Caregivers acting as models of eating that children learn to emulate. Caregivers who engage in healthy appropriate eating behaviours serve as positive models; caregivers who engage in unhealthy eating behaviours serve as negative models |
| Parent control | Guiding children's eating by exerting control, such as restricting how much their child eats or putting pressure on the child to eat more |
| Feeding to schedule | Caregivers allowing the infant to eat whenever they want or only providing food for the infant at set times |
| Parent–infant interaction during feeding | How parents and infants interact during feeding, can include responsiveness of both, including feeding behaviours and responses to reactions |
| Satiety and hunger responsiveness | Caregiver's awareness and attention to infant cues for hunger or fullness, and the initiation and termination of feeding in response to those cues |
| Laissez faire feeding style | Not setting limits on quality or quantity of foods infants consume, while showing little interaction with the infant during feeding |
| Indulgent feeding | Not setting limits on quality or quantity of foods infants consume, while also being highly involved with feeding |
| Authoritative feeding | Feeding style that is characterised by high parental demandingness and high responsiveness |
| Authoritarian feeding | Feeding style that is characterised by high parental demandingness and low responsiveness |
| Responsive infant feeding | Infant feeding in which the parent is aware of and responds in a timely and appropriate manner to infant cues and needs |
| Bottle to bed | Allowing the infant to take the bottle while laying down in their bed or cot and bottle‐feed themselves to relaxation/rest |
| Domain 4. Parent knowledge and beliefs (n = 9) | |
| Parent's feeding intentions | Parents intentions to feed the infant in a certain way, this can be in line with infant feeding recommendations or not |
| Maternal feeding self‐efficacy | The degree to which the caregiver perceives themselves capable of the necessary tasks involved in infant feeding |
| Knowing what foods should be offered/avoided | Caregiver knowledge of what foods should be offered to infants and what foods should be avoided during early feeding |
| Knowledge about how to offer complimentary foods | Caregiver knowledge of the appropriate ways to feed infants complimentary foods |
| Perceived behavioural control about introducing solids | Caregiver's perceived ease of introducing solid foods to the infant's diet |
| Perceptions of child weight | Parents perceptions of the child's weight |
| Weight concern | Caregiver's concerns about the child's risk of being overweight or underweight |
| Concern about eating | Caregiver's concern that the infant is not getting enough to eat or is eating too much |
| Perceived responsibility | Caregivers' perceptions of their responsibility for child feeding, including responsibility for feeding in general, portion size, and the types of foods consumed |
| Domain 5. Practical feeding (n = 2) | |
| Self or assisted feeding | Whether the child self‐feeds (finger foods or spoon use) or is assisted in feeding by the caregiver (spoon fed). This relates to all feeding occasions rather than just introduction of solids |
| Beverage container use | Whether the child drinks from a bottle, “sippy‐cup,” or cup, which is developmentally appropriate for their age |
| Domain 6. Food environment (n = 3) | |
| Feeding environment | The environment in which feeding takes place. This includes, but is not limited to, communication with the infant, sitting down to eat with the infant, and turning off the television during feeding |
| Offering healthy foods | Availability and provision of healthy foods to infant |
| Infant consuming family foods | Whether the infant is fed common family foods that are consumed by all members of the family, or if the food is prepared specially for the infant and differs from the family meal/foods |
| Domain 7. Dietary intake (n = 16) | |
| Types of food consumed | Relates to the different types of foodstuffs infants consume. This can include ever feeding, and/or the quantity of foods consumed, ranging from fruits and vegetables to sweet and savoury snacks |
| Energy/nutrient intakes | Intake of different nutrients, protein, energy, fat, and so forth |
| Portion size | The size or amount of food provided to infants |
| Consumption of new foods | Infant consumption of new foods |
| Type of first food | The type of solid infants were first introduced to |
| Offering age appropriate foods and beverages | Whether the foods and beverages provided to infants are developmentally appropriate |
| Ready‐made food consumption | Infant consumption of commercial baby food; this includes pre‐packaged, ready‐made, or shop‐bought foods. These foods can include cereals, fruit, vegetables, fish, meat, sweets, and desserts |
| Food variety | Infant consumption of a varied diet |
| Frequency of solid food consumption | How often infants consume solid foods, including main meals and snacks |
| Home‐made food consumption | Infant consumption of food prepared by caregiver. This can include the type of food prepared by caregiver for infant |
| Texture of foods consumed | Texture of foods provided to infants (pureed and lumpy), can include whether the texture is developmentally appropriate for infant age |
| Type of milk consumed | Infant consumption of different types of milk, including full‐fat cow's milk, low‐fat cow's milk, soya milk, and goat's milk. This does not include formula milk |
| Type of “other drinks” consumed | Infant consumption of a range of nonmilk drinks. These include water, sugar‐sweetened beverages, herbal drinks, tea/coffee, and warm drinks (other than tea or coffee) |
| Frequency of sugar‐sweetened beverage consumption | How often infants consume sugar‐sweetened beverages |
| Food/feeding preparation method | The methods by which infant foods are prepared |
|
Supplement intake (e.g., vitamins/minerals/probiotics) |
Infant consumption of vitamins and minerals |
| Domain 8. Perceptions of infant behaviours and preferences (n = 12) | |
| Infant appetite | Infant's perceived appetite |
| Food preferences | Perceptions of the infant's liking of established or newly introduced foods |
| Infant food responsiveness | The infant's desire to eat in response to food stimuli, regardless of how hungry they are |
| Infant enjoyment of food | Perceptions of how much the child enjoys eating and is interested in food |
| Infant satiety responsiveness | The infant's ability to regulate their intake based on their own fullness |
| Infant slowness in eating | The speed at which the child eats |
| Infant food fussiness | Whether the infant is seen as being a “picky eater” and highly selective about the foods that are consumed |
| Child willingness to try new foods | Perceptions of child's aversion to novel foods |
| Food refusal | Perceptions of infants refusal of any foods offered, not limited to new foods |
| Ease of feeding | How easy the infant is perceived to be to feed |
| Desire for drinks | How often the child is perceived to want a drink such as water, breast milk, formula milk, or other |
| Emotional eating |
The infant eating more (overeating) or less (under‐eating) in response to emotional states |
| Domain 9. Child weight‐related outcomes (n = 3) | |
| Weight | Including infant's weight, and weight for age and length |
| Body fat | Includes BMI and skinfold thicknesses |
| Length | Includes infant length and length for age |
Note. BMI: body mass index.
3.2.1. Frequency of outcome domains
The most frequently reported outcome domain was “breastfeeding and formula feeding,” which was reported in 82.5% (n = 104) of reviewed studies. “Introduction of solids” outcomes were reported in 64.3% (n = 81) of studies, and “dietary intake” outcomes were reported in 52.4% (n = 66) of studies. “Child weight‐related outcomes” were reported in 50.8% (n = 64) of studies. “Practical feeding” and “food environment” were the least commonly reported outcome domains, reported in only 5.5% (n = 7) and 6.3% (n = 8) of studies, respectively. See Figure 2 for frequency of all outcome domains; see Data S3 for matrix representing frequency of outcome domain reporting within and across studies.
Figure 2.
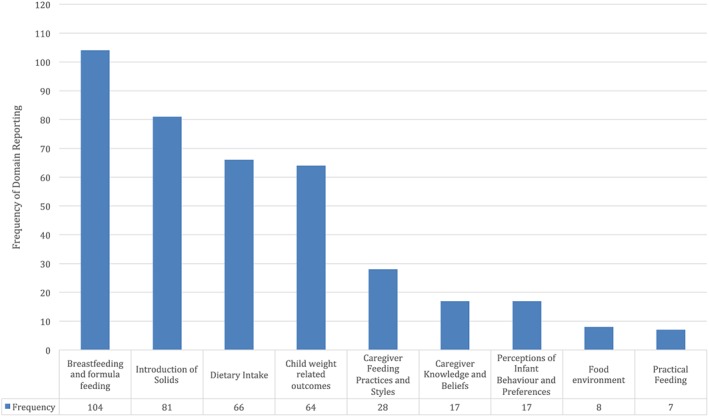
Reporting of outcome domains in reviewed studies
3.2.2. Frequency of outcomes
Frequencies of outcomes within each outcome domain, and across all reviewed studies, are presented in Data S4. Across all outcome domains, the most frequently reported outcome was timing of introduction of solids, which was reported in 59.5% (n = 75) of reviewed studies. This was followed by breastfeeding duration (55.5%, n = 70), infant weight (38.1%), and types of food consumed (34.9%, n = 44). Of the two most frequently reported outcomes, 39.7% of studies reported both outcomes in the same paper. Only 4.8% of studies reported the four most common infant feeding outcomes together. A number of outcomes were reported in one study only: infant desire for drinks; infant emotional eating; portion size; supplement intake; feeding intentions; perceived behavioural control of introduction to solids; weight concern; concern about eating; emotional feeding; feeding to soothe; modelling; authoritative feeding; and authoritarian feeding.
4. DISCUSSION
This review examined reporting of infant feeding outcomes from 126 papers related to feeding of infants up to 1 year of age. The findings indicate a considerable degree of heterogeneity in reporting of core outcome domains and of individual infant feeding‐related outcomes. Study outcomes predominantly focus on the areas of breastfeeding and formula feeding, child weight‐related outcomes, introduction of solids, and dietary intake. Less attention is given to parents' feeding practices and styles and parents' knowledge and beliefs. Outcomes relating to the food environment, practical feeding, and perceptions of infant behaviour and preferences are further under‐represented. Differences in terminology and reporting of individual outcomes highlight that the same or similar outcomes are often reported differently across studies. Inconsistency in outcome selection and reporting limits synthesis and comparison across studies (Williamson et al., 2017) and hinders the development and evaluation of childhood obesity prevention efforts.
The four most common outcome domains identified in the current review (“breastfeeding and formula feeding,” “introduction of solids,” “dietary intake,” and “child weight‐related outcomes”) were unsurprising in the context of childhood obesity prevention. Over two fifths of all reviewed studies included outcomes assigned to the “breastfeeding and formula feeding” outcome domain, suggesting that this is a core aspect of infant feeding in the first year of life. This is interesting given that this review excluded studies with a breastfeeding only focus, further indicating the importance of this domain in any examination of early child feeding. This is unsurprising in light of consistent evidence linking factors such as breastfeeding (Modrek et al., 2017) and type of formula consumption (Koletzko et al., 2009; Weber et al., 2014) to later child weight status. Outcomes within the “child weight‐related outcomes” domain, child weight (Institute of Medicine (U.S.), Committee on Obesity Prevention Policies for Young Children, Birch, Burns, Parker, & Institute of Medicine (U.S.), 2011), and weight trajectories (Baird et al., 2005; Institute of Medicine (U.S.), Committee on Obesity Prevention Policies for Young Children, et al., 2011; Woo Baidal et al., 2016) are also consistently associated with risk of later childhood obesity. Outcomes within the “introduction of solids” domain, such as the timing of introduction of foods and beverages other than breast or formula milk, are also associated with risk of later childhood obesity (Weng, Redsell, Swift, Yang, & Glazebrook, 2012). Similarly, outcomes within the “dietary intake” domain, including types and amounts of foods consumed, demonstrate associations with childhood obesity, although a recent review has identified inconsistencies across findings. (Matvienko‐Sikar et al., 2018).
The domains of “parent feeding knowledge and beliefs” and “parent feeding practices and styles” were reported less frequently. This suggests that less consideration is given to parent‐related factors when examining infant feeding overall. “Feeding practices and styles” include responsive and nonresponsive feeding behaviours, such as parent awareness and attention to satiety and hunger responsiveness and pressure to eat. Such outcomes are particularly important for examinations of infant feeding interventions because they reflect modifiable behaviours that are consistently associated with infant feeding and weight outcomes (DiSantis et al., 2011; Hurley, Cross, & Hughes, 2011; O'Malley et al., 2015). Recent reviews have shown that interventions incorporating responsive feeding components demonstrate greater benefits for some feeding and weight outcomes than interventions without this focus (Matvienko‐Sikar; Redsell et al., 2016). What parents know and believe about how, what, and when to feed is also important in terms of improving infant feeding. Parents' perceived self‐efficacy around infant feeding (Campbell, Hesketh, Silverii, & Abbott, 2010) will also influence when and how different feeding behaviours occur. These outcome domains are therefore important to consider in feeding and obesity prevention research because many behavioural infant feeding interventions operate on an assumption that modifying such outcomes leads to effects for child weight outcomes. By not assessing these outcomes, important information on the mechanisms of change of infant feeding interventions may be missed, further limiting development of efficacious obesity prevention interventions.
Outcomes categorised under the perceptions of infant behaviour and preferences domain are under‐represented across trials. These outcomes are important because of the bidirectional nature of the parent–infant feeding relationship, whereby parents engage in feeding behaviours based on infant reactions and/or perceived temperament (Jansen et al., 2017). As noted in a recent examination of parents' feeding responses to fussy eating, this bidirectional relationship can result in poorer child feeding outcomes (Jansen et al., 2017). For instance, pressuring a child to eat may lead to problematic food avoidant behaviours (Jansen et al., 2017). It is important to note that a number of outcomes within this domain come from the Child Eating Behaviour Questionnaire (Wardle, Guthrie, Sanderson, & Rapoport, 2001). Thus, under‐representation of this outcome domain in the current review may reflect less frequent use of this questionnaire in infant feeding examinations, rather than reduced importance of this domain.
Under‐representation of the “food environment” and “practical feeding” outcome domains may reflect a greater focus in the literature on individual‐level factors related to infants and/or parents than on environmental factors. More recently, there has been greater attention paid to broader environmental factors, and this recent focus is not reflected in all studies included in this review. The food environment relates to the environment in which feeding takes place and the types of food provided/available within this environment. Exposure to obesogenic environments is associated with poorer dietary intake and weight outcomes in older children (Schrempft, van Jaarsveld, Fisher, & Wardle, 2015), and such outcomes warrant further examination in infancy. “Practical feeding” relates to beverage container use and the child's self‐feeding behaviours. In the first year of life, these factors may be of less importance to weight outcomes than, for instance, between 1 and 2 years of age (Woo Baidal et al., 2016), thus explaining infrequent reporting here.
The observed inconsistencies in outcome definitions and reporting have important implications for childhood obesity prevention, particularly trials of infant feeding interventions conducted with infants under 1 year. Lack of standardisation of outcomes facilitates a continuation of heterogeneity in the literature on infant feeding approaches to obesity prevention. This limits synthesis of trial outcomes and robust evaluation of the effects and mechanisms of change underpinning childhood obesity prevention interventions (Matvienko‐Sikar). Without standardisation of outcomes, an effective and efficient approach to developing, implementing, and evaluating infant feeding interventions for childhood obesity prevention cannot be conducted. This heterogeneity therefore provides a robust rationale for the development of a COS for trials of infant feeding interventions for infants up to 1 year, of which this review forms the first part (Matvienko‐Sikar et al., 2017).
4.1. Strengths and limitations
This review had a number of strengths, including use of the established Preferred Reporting Items for Systematic Reviews and Meta‐Analyses systematic review methodology (Moher et al., 2009) and the COMET initiative guidelines (Williamson et al., 2017). As such, the authors are confident that all relevant papers were identified for the current review; this was further strengthened by the lack of restriction on date of publication. Inclusion of infant feeding studies that are not explicitly weight focused in the current review is also a strength as it facilitated evaluation and examination of all reported infant feeding outcomes. It is possible that important outcomes may be overlooked in trials of obesity prevention interventions and this may contribute to inconsistencies observed in intervention effects (Matvienko‐Sikar et al., 2017; Redsell et al., 2016).
Inductive generation of outcome domains could be considered a limitation of this review. Previous reviews (Kapadia et al., 2015) have utilised standardised approaches to categorising outcomes, such as the Outcome Measures in Rheumatology (OMERACT) filter (Boers et al., 2014) to assign individual outcomes to a number of prespecified key domains. The inclusion of a multidisciplinary team in this outcome synthesis process provides confidence in the outcomes and outcome domains presented in this review however. This review does not address outcome measurement instruments used to examine individual outcomes or outcome domains, as has been done in other reviews of children with neurodisabilities (Kapadia et al., 2015). Examination of outcome measurement instruments provides further insight into heterogeneity of outcome evaluation and also facilitates identification of potentially useful outcome tools. However, it is advised by the COMET initiative (Williamson et al., 2017) and the consensus‐based standards for the selection of health measurement instruments (Prinsen et al., 2016) initiative to first establish what to measure; only when this is done should measurements, or the how to measure, be examined.
4.2. Future research
The findings of the current review highlight a significant need for standardisation of infant feeding outcomes for trials of obesity prevention interventions in children up to 1 year. Doing so will facilitate improved evaluation of existing interventions and development of more robust and effective interventions to prevent childhood obesity in the future. Given the current high rates of childhood obesity (Ogden et al., 2016), development, implementation, and evaluation of effective obesity prevention interventions is crucial.
This review represents the first stage in development of an infant feeding COS for childhood obesity prevention interventions (Matvienko‐Sikar et al., 2017). The 82 outcomes identified in this review will form the basis for the development of the COS. As outlined in the COMET handbook version 1.0, the next stage is to engage in a consensus process with expert stakeholders to elicit views about important outcomes for COS inclusion (Williamson et al., 2017). This will be conducted as an online Delphi survey with stakeholder groups including parents, health care professionals, and researchers. The identified outcomes and outcome domains will be used in this process to prioritise outcomes for the COS. This will be followed by a nominal group consensus meeting to achieve consensus on outcomes for inclusion in the COS (Matvienko‐Sikar et al., 2017). The final COS will present a standardised list of outcomes to guide research and practice in infant feeding childhood obesity prevention.
5. CONCLUSIONS
This review identified nine domains of 82 infant feeding outcomes from 126 studies. There was considerable heterogeneity and inconsistencies in outcome selection and reporting. Current outcome reporting focuses predominantly on early consumption of milks and solids and infant weight. Less focus is given to important modifiable parental feeding practices and styles. Similarly, there is proportionally little attention given to environmental factors relating to infant feeding. These results provide a robust foundation for the development of an infant feeding COS for childhood obesity prevention interventions for children up to 1 year.
CONFLICTS OF INTEREST
The authors have no conflicts of interest relevant to this article to disclose.
CONTRIBUTIONS
KM‐S conceptualised the review, developed the review protocol, synthesised outcomes, conducted analyses, and drafted the manuscript. CG conducted searches and quality assessment, conducted analyses, and made significant contributions to reviewing and revising the manuscript. NM conducted searches and made significant contributions to reviewing and revising the manuscript. ET contributed to drafting the review protocol and substantially contributed to reviewing and revising the manuscript. MB, CK, CH, and DD contributed to analyses and substantially contributed to drafting, reviewing, and revising the manuscript. PMK advised on all aspects of the review and made significant contributions to reviewing and revising the manuscript.
Supporting information
Data S1: Supporting Information
Data S2: Supporting Information
Data S3. Frequency of outcome domain reporting in all studies (shaded boxes represent outcomes reported)
Data S4. Frequency of Outcome Reporting
Supporting Info
ACKNOWLEDGMENTS
The authors would like to thank those authors of the original papers who provided information where requested.
Matvienko‐Sikar K, Griffin C, McGrath N, et al. Developing a core outcome set for childhood obesity prevention: A systematic review. Matern Child Nutr. 2019;15:e12680 10.1111/mcn.12680
REFERENCES
- Ahrens, W. , Pigeot, I. , Pohlabeln, H. , De Henauw, S. , Lissner, L. , Molnar, D. , … Consortium, I. (2014). Prevalence of overweight and obesity in European children below the age of 10. International Journal of Obesity, 38, S99–S107. 10.1038/ijo.2014.140 [DOI] [PubMed] [Google Scholar]
- Bacha, F. , & Gidding, S. S. (2016). Cardiac abnormalities in youth with obesity and type 2 diabetes. Current Diabetes Reports, 16(7). doi: ARTN), 62 10.1007/s11892-016-0750-6 [DOI] [PubMed] [Google Scholar]
- Baird, J. , Fisher, D. , Lucas, P. , Kleijnen, J. , Roberts, H. , & Law, C. (2005). Being big or growing fast: Systematic review of size and growth in infancy and later obesity. British Medical Journal, 331(7522), 929–931. 10.1136/bmj.38586.411273.E0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, A. R. (2016). Psychosocial aspects of obesity. NASN School Nurse, 31(1), 23–27. 10.1177/1942602X15619756 [DOI] [PubMed] [Google Scholar]
- Blake‐Lamb, T. L. , Locks, L. M. , Perkins, M. E. , Woo Baidal, J. A. , Cheng, E. R. , & Taveras, E. M. (2016). Interventions for childhood obesity in the first 1,000 days a systematic review. American Journal of Preventive Medicine, 50(6), 780–789. 10.1016/j.amepre.2015.11.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boers, M. , Kirwan, J. R. , Wells, G. , Beaton, D. , Gossec, L. , d'Agostino, M. A. , … Tugwell, P. (2014). Developing core outcome measurement sets for clinical trials: OMERACT filter 2.0. Journal of Clinical Epidemiology, 67(7), 745–753. 10.1016/j.jclinepi.2013.11.013 [DOI] [PubMed] [Google Scholar]
- Brown, A. , & Lee, M. (2011). Maternal child‐feeding style during the weaning period: Association with infant weight and maternal eating style. Eating Behaviors, 12(2), 108–111. 10.1016/j.eatbeh.2011.01.002 [DOI] [PubMed] [Google Scholar]
- Campbell, K. , Hesketh, K. , Silverii, A. , & Abbott, G. (2010). Maternal self‐efficacy regarding children's eating and sedentary behaviours in the early years: Associations with children's food intake and sedentary behaviours. International Journal of Pediatric Obesity, 5(6), 501–508. 10.3109/17477161003777425 [DOI] [PubMed] [Google Scholar]
- Clarke, M. (2007). Standardising outcomes for clinical trials and systematic reviews. Trials, 8 10.1186/1745-6215-8-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cote, A. T. , Harris, K. C. , Panagiotopoulos, C. , Sandor, G. G. S. , & Devlin, A. M. (2013). Childhood obesity and cardiovascular dysfunction. Journal of the American College of Cardiology, 62(15), 1309–1319. 10.1016/j.jacc.2013.07.042 [DOI] [PubMed] [Google Scholar]
- DiSantis, K. I. , Hodges, E. A. , Johnson, S. L. , & Fisher, J. O. (2011). The role of responsive feeding in overweight during infancy and toddlerhood: A systematic review. International Journal of Obesity, 35(4), 480–492. 10.1038/ijo.2011.3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley, K. M. , Cross, M. B. , & Hughes, S. O. (2011). A systematic review of responsive feeding and child obesity in high‐income countries. Journal of Nutrition, 141(3), 495–501. 10.3945/jn.110.130047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (U.S.), Committee on Obesity Prevention Policies for Young Children , Birch, L. L. , Burns, A. C. , Parker, L. , & Institute of Medicine (U.S.) (2011). Early childhood obesity prevention policies. Washington, D.C: National Academies Press. [Google Scholar]
- Jansen, P. W. , de Barse, L. M. , Jaddoe, V. W. V. , Verhulst, F. C. , Franco, O. H. , & Tiemeier, H. (2017). Bi‐directional associations between child fussy eating and parents' pressure to eat: Who influences whom? Physiology & Behavior, 176, 101–106. 10.1016/j.physbeh.2017.02.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapadia, M. Z. , Balasingham, C. , Cohen, E. , Mahant, S. , Nelson, K. , Maguire, J. L. , … Offringa, M. (2015). Development of a core set of outcomes in children with severe neurodisability and feeding tune dependency: A systematic review. Trials, 16 10.1186/1745-6215-16-S3-P9 [DOI] [Google Scholar]
- Kelly, L. E. , Jansson, L. M. , Moulsdale, W. , Pereira, J. , Simpson, S. , Guttman, A. , … Offringa, M. (2016). A core outcome set for neonatal abstinence syndrome: Study protocol for a systematic review, parent interviews and a Delphi survey. Trials, 17, ARTN 536. 10.1186/s13063-016-1666-9 17, 536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkham, J. J. , Dwan, K. M. , Altman, D. G. , Gamble, C. , Dodd, S. , Smyth, R. , & Williamson, P. R. (2010). The impact of outcome reporting bias in randomised controlled trials on a cohort of systematic reviews. BMJ, 340, c365 10.1136/bmj.c365 [DOI] [PubMed] [Google Scholar]
- Koletzko, B. , von Kries, R. , Closa, R. , Escribano, J. , Scaglioni, S. , Giovannini, M. , … Trial, E. C. O. (2009). Lower protein in infant formula is associated with lower weight up to age 2 y: A randomized clinical trial. American Journal of Clinical Nutrition, 89(6), 1836–1845. 10.3945/ajcn.2008.27091 [DOI] [PubMed] [Google Scholar]
- Maffeis, C. , & Tato, L. (2001). Long‐term effects of childhood obesity on morbidity and mortality. Hormone Research, 55(Suppl 1), 42, 63462–45. [DOI] [PubMed] [Google Scholar]
- Matvienko‐Sikar, K. , Byrne, M. , Kelly, C. , Toomey, E. , Hennessy, M. , Devane, D. , … Kearney, P. M. (2017). Development of an infant feeding core outcome set for childhood obesity interventions: Study protocol. Trials, 18(1), 463 10.1186/s13063-017-2180-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matvienko‐Sikar, K. , Toomey, E. , Delaney, L. , Harrington, J. , & Kearney, P. M. (2018). ‘Effects of healthcare professional delivered early feeding interventions on feeding practices and dietary intake: A systematic review’. Appetite, 123(1), 56–71. [DOI] [PubMed] [Google Scholar]
- Modrek, S. , Basu, S. , Harding, M. , White, J. S. , Bartick, M. C. , Rodriguez, E. , & Rosenberg, K. D. (2017). Does breastfeeding duration decrease child obesity? An instrumental variables analysis. Pediatric Obesity, 12(4), 304–311. 10.1111/ijpo.12143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohanan, S. , Tapp, H. , McWilliams, A. , & Dulin, M. (2014). Obesity and asthma: Pathophysiology and implications for diagnosis and management in primary care. Experimental Biology and Medicine, 239(11), 1531–1540. 10.1177/1535370214525302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher, D. , Liberati, A. , Tetzlaff, J. , Altman, D. G. , & Grp, P. (2009). Preferred reporting items for systematic reviews and meta‐analyses: The PRISMA statement. PLoS Medicine, 6(7). doi: ARTN), e1000097 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogden, C. L. , Carroll, M. D. , Lawman, H. G. , Fryar, C. D. , Kruszon‐Moran, D. , Kit, B. K. , & Flegal, K. M. (2016). Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA, 315(21), 2292–2299. 10.1001/jama.2016.6361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Malley, C. , Mazarello Paes, V. , Hesketh, K. , Moore, H. J. , Ong, K. , Van Sluijs, E. , … Summerbell, C. D. (2015). Systematic review on the determinants of fruit and vegetable consumption in young children (aged 0–6). Obesity Facts, 8, 70–272. 10.1159/000382140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce, J. , & Langley‐Evans, S. C. (2013). The types of food introduced during complementary feeding and risk of childhood obesity: A systematic review. International Journal of Obesity, 37(4), 477–485. 10.1038/ijo.2013.8 [DOI] [PubMed] [Google Scholar]
- Prinsen, C. A. C. , Vohra, S. , Rose, M. R. , Boers, M. , Tugwell, P. , Clarke, M. , … Terwee, C. B. (2016). How to select outcome measurement instruments for outcomes included in a “Core Outcome Set”—A practical guideline. Trials, 17. doi: ARTN 449. 10.1186/s13063-016-1555-2, 449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redsell, S. A. , Edmonds, B. , Swift, J. A. , Siriwardena, A. N. , Weng, S. , Nathan, D. , & Glazebrook, C. (2016). Systematic review of randomised controlled trials of interventions that aim to reduce the risk, either directly or indirectly, of overweight and obesity in infancy and early childhood. Maternal & Child Nutrition, 12(1), 24–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reilly, J. J. , Martin, A. , & Hughes, A. R. (2017). Early‐life obesity prevention: Critique of intervention trials during the first one thousand days. Current Obesity Reports, 6(2), 127–133. 10.1007/s13679-017-0255-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schrempft, S. , van Jaarsveld, C. H. M. , Fisher, A. , & Wardle, J. (2015). The obesogenic quality of the home environment: Associations with diet, physical activity, TV viewing, and BMI in preschool children. PLoS One, 10(8). doi: ARTN), e0134490 10.1371/journal.pone.0134490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor, R. W. , Iosua, E. , Heath, A.‐L. M. , Gray, A. R. , Taylor, B. J. , Lawrence, J. A. , … Galland, B. (2017). Eating frequency in relation to BMI in very young children: A longitudinal analysis. Public Health Nutrition, 20, 1–8. 10.1017/S1368980017000143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardle, J. , Guthrie, C. A. , Sanderson, S. , & Rapoport, L. (2001). Development of the children's eating behaviour questionnaire. Journal of Child Psychology and Psychiatry, 42(7), 963–970. 10.1111/1469-7610.00792 [DOI] [PubMed] [Google Scholar]
- Weber, M. , Grote, V. , Closa‐Monasterolo, R. , Escribano, J. , Langhendries, J. P. , Dain, E. , … S, E. C. O. T (2014). Lower protein content in infant formula reduces BMI and obesity risk at school age: Follow‐up of a randomized trial. American Journal of Clinical Nutrition, 99(5), 1041–1051. 10.3945/ajcn.113.064071 [DOI] [PubMed] [Google Scholar]
- Weng, S. F. , Redsell, S. A. , Swift, J. A. , Yang, M. , & Glazebrook, C. P. (2012). Systematic review and meta‐analyses of risk factors for childhood overweight identifiable during infancy. Archives of Disease in Childhood, 97(12), 1019–1026. 10.1136/archdischild-2012-302263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson, P. R. , Altman, D. G. , Bagley, H. , Barnes, K. L. , Blazeby, J. M. , Brookes, S. T. , … Young, B. (2017). The COMET handbook: Version 1.0. Trials, 18. ARTN 280.10.1186/s13063‐017‐1978‐4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson, P. R. , Altman, D. G. , Blazeby, J. M. , Clarke, M. , Devane, D. , Gargon, E. , & Tugwell, P. (2012). Developing core outcome sets for clinical trials: Issues to consider. Trials, 13(1), 1–8. 10.1186/1745-6215-13-132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woo Baidal, J. A. , Locks, L. M. , Cheng, E. R. , Blake‐Lamb, T. L. , Perkins, M. E. , & Taveras, E. M. (2016). Risk factors for childhood obesity in the first 1,000 days: A systematic review. American Journal of Preventive Medicine, 50(6), 761–779. 10.1016/j.amepre.2015.11.012 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1: Supporting Information
Data S2: Supporting Information
Data S3. Frequency of outcome domain reporting in all studies (shaded boxes represent outcomes reported)
Data S4. Frequency of Outcome Reporting
Supporting Info


