Abstract
Although the benefits of breastfeeding are well‐documented, little is known about how best to encourage fathers to support breastfeeding. A quasi‐experimental study of a community‐based intervention was designed to examine whether health education to promote fathers' involvement in supporting women is associated with early initiation and exclusive breastfeeding practices. At baseline, 802 couples of fathers with pregnant wives from 12 to 27 weeks of gestational age were recruited to either the intervention group (n = 390) or a control group (n = 412) consisting of couples seeking care through routine maternal and child health services. Fathers in the intervention area received breastfeeding education and counselling services in health facilities and at home visits during the antenatal, delivery, and post‐partum periods. Peer education and social exchange concerning breastfeeding were organized in fathers' clubs. After 1 year of the intervention, mothers in the intervention group were more likely to initiate early breastfeeding 49.2 and 35.8% in the intervention and control group respectively, P < 0.001. At 1, 4, and 6 months after birth, 34.8, 18.7, and 1.9% of the mothers in the intervention group were exclusively breastfeeding their children because of birth, respectively, compared with 5.7, 4.0, and 0.0% of those in the control group (P < 0.001). Those practices were associated with the intervention in bivariate and multivariate logistic and Cox regression analyses. Intervention targeting fathers at antenatal and postnatal periods may positively influence the breastfeeding practices of mothers, and it should be an important component of breastfeeding programs.
Keywords: breastfeeding, fathers' involvement, Vietnam
Key messages.
Fathers can be involved in supporting breastfeeding during the antenatal, delivery, and postnatal period.
By mobilizing fathers' support for breastfeeding through an integrated community‐based educational intervention in Vietnam, we managed to make a positive association on early initiation and exclusive breastfeeding at 1, 4, and 6 months.
Father involvement could be addressed explicitly and possibly then considered as an additional component of the Ten Steps recommended by WHO on breastfeeding promotion.
1. INTRODUCTION
Breastfeeding is positively associated with health, survival, and development of the infant and the health of the mother (Victora et al., 2016). The rate of early initiation of breastfeeding and exclusive breastfeeding (EBF) of infants less than 6 months of age in lower‐middle income countries was only about 32 and 37%, respectively (Victora et al., 2016). In Vietnam, most mothers (98%) breastfeed their children, but the proportion of early initiation and EBF among children between 4 and 6 months is low and varies by geographical area, socioeconomic status, and maternal education (Thrive, 2012; Tuyen & Hop, 2012). Current review indicates breastfeeding is not only a woman's job (Rollins et al., 2016). It is affected by many individual factors including knowledge, education, workload, occupation (Dearden et al., 2002; Duong, Binns, & Lee, 2005), health of mother, method of delivery (Dearden et al., 2002; Forster, McLachlan, & Lumley, 2006; Prior et al., 2012), breastfeeding intention, and other factors (Meedya, Fahy, & Kable, 2010). Beyond individual factors, EBF is also influenced by family (Agunbiade & Ogunleye, 2012; Otoo, Lartey, & Perez‐Escamilla, 2009), community‐level factors such as peer group pressures and cultural perceptions (Cohen, Brown, Rivera, & Dewey, 1999; Fjeld et al., 2008), and societal level factors (Meedya et al., 2010; Morrow, 1996).
Fathers influence breastfeeding initiation, duration, and exclusivity (Bar‐Yam & Darby, 1997). They are considered a social support for their wife's breastfeeding (Hector, King, Webb, & Heywood, 2005; Meedya et al., 2010; Raj & Plicha, 1998) and a resource for child care and breastfeeding in the family (Clifford & McIntyre, 2008; Duong, Lee, & Binns, 2005). The role of fathers in supporting EBF has been included in the global strategy for breastfeeding promotion issued by the World Health Organization (WHO, 2003), but the role of father was not mentioned in the original Ten Steps to successful breastfeeding (WHO & UNICEF, 1989) or addressed explicitly in the revised version of the Ten Steps (WHO & UNICEF, 2018). Paternal intervention aims at strengthening breastfeeding knowledge, positive attitudes, and involvement of fathers in providing practical, physical, and emotional support to the mother, which may improve breastfeeding practices of the mother (Brown & Davies, 2014; Sherriff, Hall, & Panton, 2014).
A review of four controlled trials carried out in western hospital settings targeting fathers during antenatal and postnatal periods, showed different effects when applying breastfeeding educational interventions (mainly in the form of class and open discussion) (Mitchell‐Box & Braun, 2013). Some studies showed positive effects on early initiation of breastfeeding (Wolfberg et al., 2004) and exclusive breastfeeding at 4 (Susin & Giugliani, 2008b) and 6 months (Pisacane, Continisio, Aldinucci, D'Amora, & Continisio, 2005) Other studies showed negative or moderate effects on exclusive breastfeeding (Abbass‐Dick, Stern, Nelson, Watson, & Dennis, 2015; Maycock et al., 2013). Based on current literature, community‐based interventions have been widely and effectively used in promoting EBF (Haroon, Das, Salam, Imdad, & Bhutta, 2013; Sinha et al., 2015). Recently, results of a unique community‐based father intervention carried out in Vietnam showed that a combination of mass media approaches with group and individual education programs in commune health centres and counselling during home visits might increase the involvement of fathers in supporting breastfeeding and the proportion of early initiation and EBF at 1, 4, and 6 months (Bich et al., 2016; Bich & Cuong, 2017; Bich, Hoa, & Malqvist, 2014). In this study, the lack of information between intervention and control sites about the equivalence of breastfeeding practices at the baseline and the failure to establish a network of fathers with participation of local health workers and stakeholders may reduce the validity and sustainability of intervention on breastfeeding practices.
The aim of the current study was to evaluate an integrated community‐based educational intervention targeting fathers at antenatal, delivery, and postnatal periods for supporting breastfeeding practices in Vietnam. We hypothesized that after the intervention, the community under intervention will have higher proportions of women practicing early breastfeeding initiation and exclusive breastfeeding at 1, 4, and 6 months than women in the control community.
2. MATERIALS AND METHODS
2.1. Study design and settings
A quasi‐experimental study was conducted in two districts with equal population (about 130 thousand inhabitants) and socio‐economic development (Kim Thanh and Cam Giang) in Hai Duong province in northern Vietnam. In Kim Thanh district 12 communes and 1 township were selected by purposive sampling for intervention. Health care services in the intervention area are provided by 13 commune health centres, one district hospital, and one district prevention health centre. The Cam Giang district was chosen as a control site because it does not share a border with the Kim Thanh district. To ensure equalities of the intervention and control areas in terms of sample size and basic socioeconomic status, 11 communes and 1 township in Cam Giang were selected as control group. Health care services in these selected control area are also provided by 12 commune health centres, one district hospital, and one district prevention health centre. According to the routine district health reports and rapid assessment, the patterns of health care services regarding maternal and child health were similar between the two intervention and control districts. Based on the findings of an equivalent study (Bich & Thuy, 2017) carried out before baseline survey that recruited 128 and 113 of mother–infant dyads in the intervention and control sites to assess health and development of infants at 9 months and the breastfeeding practices of the mothers, the nutritional and development indicators of infants at 9 months of age (underweight, stunting and wasting, and development measured by using Ages & Stages Questionnaire 3), and 6‐month EBF rates were not significantly different between the two sites.
2.2. Participants
The study subjects were expectant fathers and their pregnant wives whose pregnancies were from 12 to 27 weeks of gestation by March 21, 2013. The selected men had to live with their wives at home or maintain regular communication with them. Couples were excluded from the study or excluded from follow‐up if (a) the women were wrongly identified as pregnant or experienced a pregnancy loss (miscarriage, stillbirth, neonatal death) during the follow‐up period, or (b) the mother had serious medical problems and was unable to answer questions included in the study survey instruments, or (c) they were divorced or separated or migrated out of the study area during the intervention and assessment periods. Eligible women were selected by using lists of pregnant women managed and updated by the routine maternal and child health program available at commune health centres. This list was again updated by the village health workers to ensure all eligible pregnant women were recruited in the study to minimize potential selection bias (Bich et al., 2014). A complete sampling was carried out due to the small number of eligible pregnant women. As a result, a total of 390 couples was selected for the intervention site, and 412 couples selected for the control site from February 1, 2014, to March 2, 2014 (Figure 1).
Figure 1.
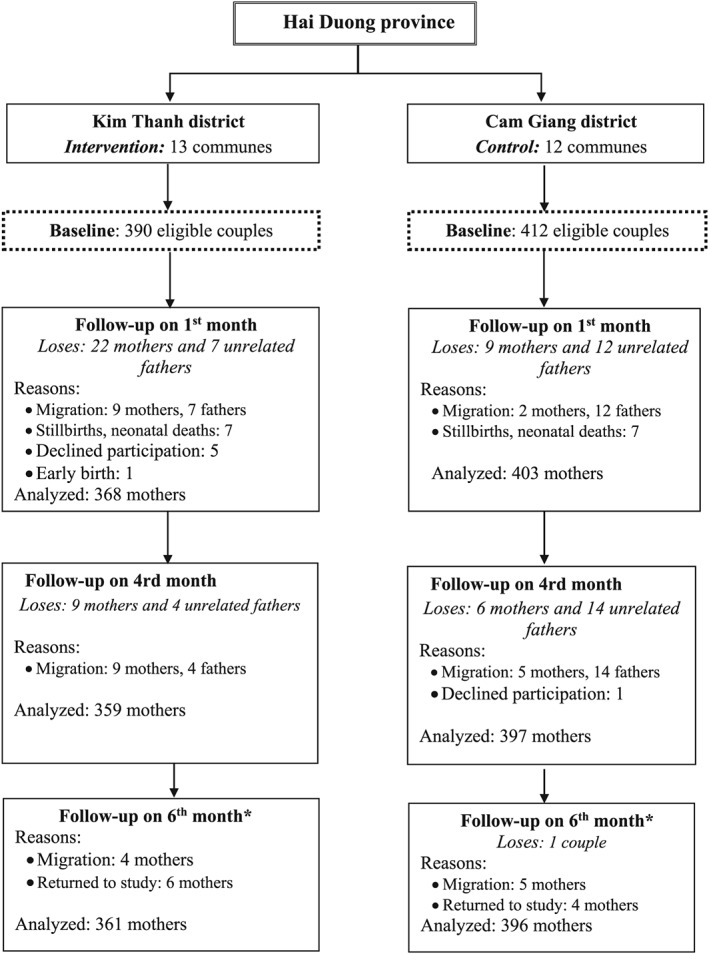
Flowchart of participants in an educational intervention study mobilizing fathers for better breastfeeding practices in Vietnam
2.3. Intervention design
This was a community‐based intervention integrated with routine health care services for women and children provided by local health staff within the Kim Thanh district health system service area. The intervention was carried out continuously during both antenatal and postnatal periods from May 1, 2014, to September 30, 2015. The intervention was designed based on social cognitive theory (Bandura, 1998) and theory of planned behavior (Ajzen, 1991). The intervention materials were adopted and updated from the breastfeeding promotion intervention strategy targeting fathers in Vietnam (Bich et al., 2014).
To train counsellors for the study, 10 district hospital midwives and 26 commune health workers and midwives were selected and trained in a 2‐day workshop to increase their knowledge about the benefits of breastfeeding and exclusive breastfeeding and to develop skills in large group and individual counselling. Activities carried out in the workshop were lectures, group discussions, role playing, and field practice with fathers who had characteristics similar to fathers whom they would provide consultation to in the intervention. Pre and post evaluation of participants was carried out to select the most capable candidates. After the 2‐day training, the successful participants participated in 3.5 months of field practice with similar fathers in another commune that was not selected for the study. In this practice period, the health workers had opportunities to obtain feedback from the trainers in the research team and from fathers so they could improve their counselling skills.
As shown in Table 1, the intervention package consisted of components including mass media communication; group health education and counselling; individual counselling; and social public activities. Through the communal loudspeaker system (aired twice every week), two separate breastfeeding promotional messages about the importance of exclusive breastfeeding and ways that fathers can support their wives' effort to breastfeed were made. Other health education materials included posters (in the commune health centre), flyers giveaways such as mugs and T‐shirts and father‐infant relationship calendars. The messages on the educational materials were designed to provide guidance for father to help them better understand and be motivated in supporting early initiation and exclusive breastfeeding. These materials were distributed to the fathers when they first agreed to participate in the study and came to health facilities.
Table 1.
Intervention components and activities implemented in intervention site at Kim Thanh district, Hai Duong province, Vietnam
| No | Intervention components and activities | Access results |
|---|---|---|
| 1 | Mass media communication from May 2014 to September 2015 | |
| • Two messages delivered via the communal speaker system. | • About 132 air times | |
| • 100% (368/368) fathers heard messages. | ||
| • Distribution of flyer, mugs, and T‐shirt and father–infant relationship calendar to fathers. | • 100% (368/368) fathers received all materials. | |
| • Putting motivational posters in health facilities to encourage fathers' involvement. | • All 13 commune health centres and district health facilities hung posters. | |
| 2 | Paternal group training and individual counselling at home visit from May 2014 to January 2015 | |
| • Group counselling and training for fathers at commune health centre | • 110 groups organized | |
| • 86.9% (339/390) fathers participated. | ||
| • Home visit: Individual counselling for fathers during last trimester | • 92.1% (359/390) fathers were consulted. | |
| • Individual counselling for fathers at delivery | • 51.6% (190/368) fathers | |
| • Home visit: Individual counselling for fathers at 7 days after birth | • 96.7% (356/368) fathers | |
| • Home visit: Individual counselling for fathers at 6 weeks | • 98.1% (361/368) fathers | |
| • Home visit: Individual counselling for fathers at 3.5 months | • 93.5% (344/368) fathers | |
| 3 | Fathers' Club and social event from September 2014 to June 2015 | |
| • Fathers'Clubs organized in 13 communes | • 45.7% (168/368) fathers in 13 clubs participated in club's activities | |
| • Fathers' contest “who love wives and children more” organized in March 2015. | • 38.7% (65/168) fathers participated in the contest's program | |
| • Contest's audience was 400 people | ||
| 4 | Organized fathers' group on Facebook from July 2015 | |
| • Activities were reviewed in 3 months (from July to September 2015) | • 153 members (fathers and health workers) | |
| • About 110 posts, 3000 views, and comments | ||
The group education and counselling sessions were monthly and lasted for 30 to 45 min. They were organized and provided by trained commune health workers at commune health centre when the couples came to receive antenatal and vaccination services. The materials used in group education and counselling were contained in a counselling manual designed for counsellors and other breastfeeding education materials. The first group counselling took place in May 2014 and ended on January 2015. The individual counselling was carried out at the time of the child's delivery in the district hospital or commune health centre and during four home visits (first visit at last trimester, second at the first week post‐partum, third at 6th week, and fourth at 3.5 months after birth.) Through counselling services, fathers discussed and were told about breastfeeding benefits and the specific activities they could do to support their wives during the antenatal, delivery, and post‐partum period.
The individual counselling was designed and implemented at delivery because the fathers often accompanied their wives to the district hospitals or commune health centres to give birth. On the very first days of having a new baby, the father was counselled about the importance of breast milk and exclusive breastfeeding. At delivery, a father–infant relationship calendar showing the development of infants during the first year (Month 1, Months 2–3, Months 4–6, Months 7–9, and Months 10–12) was also given to each father to use at home. By looking at the calendar, the father can learn more about how to help the infant fully develop through breastfeeding and by interacting with the infant.
Fathers' clubs were established in 13 communes and were operated by trained elected paternal leaders with support from commune health workers within the project timeline from September 2014 to June 2015 (10 months). These contacts continued with exchange activities operating through Facebook for a 3‐month period from July to September 2015. There were two kinds of club meetings including monthly meetings and unexpected meetings. The monthly meetings were organized by the paternal leader after consultation with other fathers concerning time, place, and topic of the meeting and in discussion with other members of the club management board including commune health worker and representatives of active social organization in the community. The unexpected meeting was organized based on the urgent needs and suggestions of any father in the club with the agreement of the club leader and some other fathers. For example, when fathers prepared for fathers' contest activities, they met more frequently in training meetings to be prepared for performance and activities demonstrated at the contest. The topics of the fathers' club were diversified including sharing experiences in supporting mothers to breastfeed exclusively and discussing approaches and tactics used to convince other family members to support EBF, vaccination, and child health issues and to prepare for other contest activities (taking EBF supporting photos, singing, and skits). Through club activities, fathers learned and shared experiences supporting exclusive breastfeeding, strengthening couples' relationships, and other child care issues. During the operation of the clubs, fathers in collaboration with commune health workers, local social associations, and authorities prepared and organized a public event entitled “Fathers' Contest‐ Who loves their wives and children more” to help mobilize community support, create social norms for involving fathers in exclusive breastfeeding, and reinforce the father's knowledge, attitudes, and behaviour. To be a contestant, a father was screened and trained in his commune by village and commune health workers. All targeted fathers and their families were invited to these events. On the basis of the score given by a jury, fathers who displayed knowledge and supported attitudes about breastfeeding and practice in taking care of their wives and small babies were recognized with awards and titles. This social behaviour change communication intervention was described in more detail elsewhere (Bich, 2017; Bich & Tuan, 2017) and in Figure 2.
Figure 2.
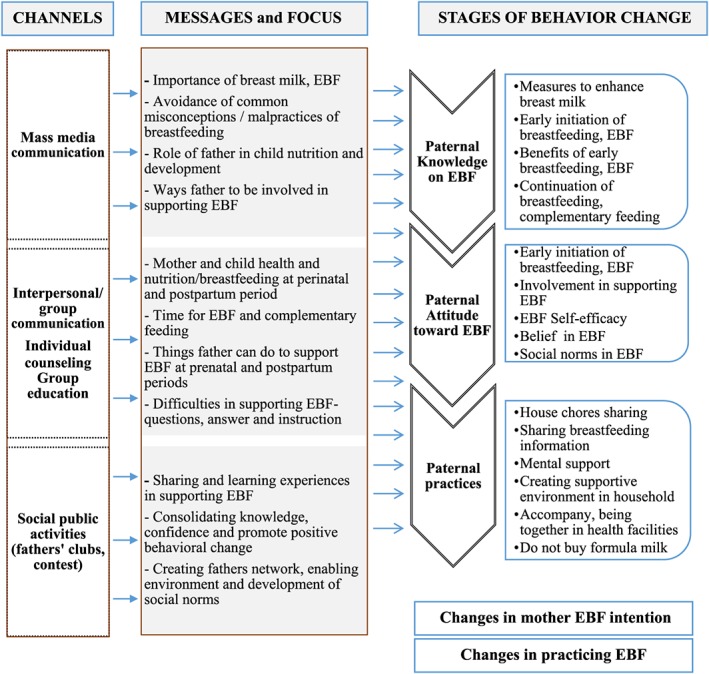
Schematic description of social behaviour change communication intervention to promote father involvement in supporting exclusive breastfeeding
In the control site (Cam Giang district), mothers and infants received routine maternal and child health services similar to that received by all mothers and infants in the intervention district. The usual care for mothers and infants includes regular periodic health and pregnancy check‐ups, counselling on newborn care and nutrition, vaccination, and other primary health care services. On some occasions, when they brought the children in for routine services at the commune health centre, fathers and grandparents accessed health educational materials.
2.4. Data collection
Basic socio‐demographic characteristics of the couples were collected at baseline through face‐to‐face structured interviews by an external independent data collection team blinded to the study hypotheses. These basic indicators included parental age, education, place of residence (rural vs. township), and family type (nuclear vs. extended). The economic status was defined as lower or higher than median of asset score developed from 13 asset items of the household including ownership of a colour TV, refrigerators/fridge, DVD player, TV digital driver, stereo sound system, radio, and other items. Occupation groupings were categorized as home‐based or close to home (farmer, housewife, small trader, and handicraftsman) or as not home‐based (government staff, workers, and driver.)
To evaluate the outcomes of intervention, all selected mothers were visited at the end of 1, 4, and 6 months post‐partum. At the first visit, the interviewer asked mothers about basic characteristics of the infants including gender, birth weight, type of delivery, and birth order of the infant. A structured questionnaire was used to assess the breastfeeding practices of mothers in the intervention and control groups including early initiation and exclusive breastfeeding, at 1, 4, and 6 months. This questionnaire was modified from tools used in a previous intervention measuring breastfeeding practices (Bich et al., 2014; Bich et al., 2016) by adding one more question to define time to event of stopping exclusivity. Definition of exclusive breastfeeding was based on the standards of the WHO (2010). Exclusive breastfeeding practices were identified from various methods including last week and since‐birth recalls when the infants were 1 month (30 ± 7 days), 4 months (120 ± 7 days), and 6 months (180 ± 7 days). Mothers were asked “From the time your baby was born was your baby fed anything other than breastmilk? The infant was identified as being exclusively breastfed since birth if the child was not given any water, liquids, solid, semi‐solid or soft foods since birth (Aarts et al., 2000; Bich et al., 2014; Bich et al., 2016). The duration of exclusive breastfeeding was identified by asking the mother to recall the time when mother stopped EBF with the child (time to event) by asking the mother “If your baby was given something other than breastmilk when was the first time your baby was given something other than breastmilk?”
Regarding “last week recall” of breastfeeding, the mothers were asked to recall feeding practice during the past week until the morning prior to the interview.
Information related to the knowledge, attitudes, and involvement in supporting EBF of the fathers as well as the intention of the mothers to EBF was also collected and presented in other papers (Bich, 2017; Bich & Tuan, 2017).
2.5. Statistical methods
EpiData and IBM SPSS Statistics 20 were used for data management and statistical analysis. The principle of intention‐to‐treat analysis and individual level data were used to measure overall intervention effect. Principal components and factor analysis were used to define household asset score. The Pearson's Chi‐square test was used to detect group differences (population basics at the baseline and intervention outcomes) between intervention and control groups. To estimate the crude odds ratio (OR), in case the original value in one cell was zero, a value of 0.5 was added to each of the four cells (Deeks & Higgins, 2010; Gerstman, 2003). Multivariate logistic regression was used to calculate odds ratios to measure the association between the intervention and control groups with regard to early initiation of breastfeeding and EBF at 1, 4, and 6 months. The effect of intervention was also studied by survival analysis. The duration of EBF (survival time) was the time when EBF was stopped or mother/father left the study site or due to infant's death. The Logrank and Breslow tests were used to assess the equality of the survival curves. Cox proportional hazards models were used to estimate the effect of intervention on cessation of EBF at 1, 4, and 6 months. The covariates included in the multivariate logistic and Cox regression model were five variables found significantly different at the baseline including residence, type of family, maternal education, father's occupation, household economics (Table 2), and type of delivery (potential confounding factor). A P value of <0.05 was considered significant.
Table 2.
Characteristics of the couples at baseline and children at 1 month in the intervention group (n = 368) and control group (n = 403) in Hai Duong province, Vietnam
| Basic characteristics | Study sites | Total | P value | |
|---|---|---|---|---|
| Intervention n = 390 (%) | Control n = 412 (%) | |||
| Residence | ||||
| Rural | 364 (93.3) | 351 (85.2) | 715 (89.0) | <0.001 |
| Township | 26 (6.7) | 61 (14.8) | 87 (11.0) | |
| Household economics | ||||
| Lower (50% below median) | 248 (63.6) | 149 (36.2) | 397 (49.5) | <0.001 |
| Higher (50% above the median) | 142 (36.4) | 263 (63.8) | 405 (50.5) | |
| Paternal education | ||||
| Less than high school | 190 (48.7) | 173 (42.0) | 363 (45.3) | 0.06 |
| High school and above | 200 (51.3) | 239 (58.8) | 439 (54.7) | |
| Paternal occupation | ||||
| Close to home | 150 (38.5) | 211 (51.2) | 361 (45.0) | <0.001 |
| Not close to home | 240 (61.5) | 201 (48.8) | 441 (55.0) | |
| Maternal education | ||||
| Less than high school | 187 (47.9) | 150 (36.4) | 337 (42.0) | 0.001 |
| High school and above | 203 (52.1) | 262 (63.6) | 465 (58.0) | |
| Maternal occupation | ||||
| Close to home | 129 (33.1) | 134 (32.5) | 263 (32.8) | 0.87 |
| Not close to home | 261 (66.9) | 278 (67.5) | 539 (67.2) | |
| Family type | ||||
| Nuclear | 171 (43.8) | 151 (36.7) | 322 (40.1) | 0.04 |
| Extended | 219 (56.2) | 261 (63.3) | 480 (59.9) | |
| Child characterictics | n = 368 (%) | n = 403 (%) | Total | P value |
| Child birth weight (gram) | ||||
| Low birth weight (<2500 g) | 11 (3.0) | 16 (4.0) | 27 (3.5) | 0.46 |
| Normal birth weight (≥2500 g) | 357 (97.0) | 387 (96.0) | 744 (96.5) | |
| Child birth order | ||||
| First born | 143 (38.9) | 168 (41.7) | 311 (40.3) | 0.42 |
| Second and higher | 225 (61.1) | 235 (58.3) | 460 (59.7) | |
| Type of delivery | ||||
| Caesarean section | 143 (38.9) | 153 (38.0) | 296 (38.4) | 0.80 |
| Vaginal | 225 (61.1) | 250 (62.0) | 475 (61.6) | |
| Child gender | ||||
| Female | 167 (45.4) | 187 (46.4) | 354 (45.9) | 0.77 |
| Male | 201 (54.6) | 216 (53.6) | 417 (54.1) | |
Note. Chi‐square tests performed to assess differences between intervention and control groups.
Ethical approval for this study was obtained from the Institutional Review Board of the Hanoi School of Public Health and Brock University. Written signed informed consent was obtained from all fathers and mothers.
3. RESULTS
At baseline, 390 and 412 eligible couples were in the intervention and control areas, respectively. After 6 months of follow‐up, 18 mothers in the intervention and 8 mothers in the control area were lost due to outmigration; 21 mothers (13 from intervention and 8 from control area) were not contacted due to stillbirths, neonatal deaths, or refusals. This left 368, 359, and 361 mothers in the intervention group and 403, 397, and 396 in the control group who were eligible for data collection at 1, 4, and 6 months, respectively (Figure 1). There were no statistical differences between the two groups of couples lost to follow up as related to basic demographic indicators including household economic status, age of the fathers, and education or occupation of parents.
Table 2 shows at baseline that households in the intervention group were more likely to be a nuclear family, located in a rural area, and having lower economic status. In the intervention group, fathers were more likely to work not close to home (as they were government staff, workers, and drivers), and mothers were more likely to have lower level of education. Also presented in Table 2, the characteristics of infants in the intervention and control groups regarding birth weight, birth order, type of delivery, and gender were similar (P > 0.05).
3.1. Exposure to the intervention
Table 1 shows intervention activities implemented during the first year of intervention. A total of 132 air times were provided for launching two educational messages during the first year of the intervention. All fathers in the intervention group indicated that they were aware of the messages. There were 110 group counselling sessions carried out in 13 commune health centers, with a total of 339 participants in total. At the time of delivery, 190 fathers were provided individual counselling. Almost all eligible fathers (366) received individual counselling services through 1,432 home visits by commune health workers (about 4 visits on average per father). There were 360 fathers involved in activities of the “Fathers' Clubs” established in 13 communes. At the “Fathers' Contest,” five fathers representing each commune participated and performed in front of audience of about 400 people consisting of local fathers, health workers and district authorities, and representatives of social and international organizations (Table 1).
3.2. Impact of intervention on breastfeeding practices
Table 3 shows the relationship between the intervention and early initiation of breastfeeding and EBF. The proportion of mothers living in the intervention area‐initiated breastfeeding within 1 hr after delivery was higher compared with those living in the control area (48.6 vs. 35.7%, P < 0.001). In the intervention site, at 1 month, based on since‐birth recall, 34.8% of the infants were breastfed exclusively, with the percentage falling to 18.7% at 4 months and 1.9% at 6 months. In the control site, only 5.7% of the infants were breastfed exclusively at 1 month, with this percentage falling to 4.0 and 0.0% at 4 and 6 months, respectively. The EBF practices at 4 and 6 months were also significantly higher in the intervention site based on last week recall method.
Table 3.
Breastfeeding practices by different recall methods between intervention and control in Hai Duong province, Vietnam
| Intervention | Control | |||||
|---|---|---|---|---|---|---|
| n = 368 (%) | n = 403 (%) | |||||
| Breastfeeding status | n | n | Total | P‐value | ||
| Early initiation of breastfeeding | 368 | 179 (48.6) | 403 | 144 (35.7) | 323 (41.9) | < 0.001 |
| 1‐month breastfeeding | 368 | 403 | ||||
| Since birth recall | 128 (34.8) | 23 (5.7) | 151 (19.6) | <0.001 | ||
| 4‐month breastfeeding | 359 | 397 | ||||
| Since birth recall | 67 (18.7) | 16 (4.0) | 83 (11.0) | <0.001 | ||
| Last week recall | 139 (38.7) | 120 (30.2) | 259 (34.3) | 0.014 | ||
| 6‐month breastfeeding | 361 | 396 | ||||
| Since birth recall | 7 (1.9) | 0 (0.0) | 7 (0.9) | 0.005 | ||
| Last week recall | 15 (4.2) | 0 (0.0) | 15 (2.0) | <0.001 | ||
Note. Chi‐square tests performed to assess differences between intervention and control groups.
Table 4 presents the summaries of findings from crude and multivariate logistic regression analysis where the dependent variable was the early initiation of breastfeeding and EBF at 1, 4, and 6 months identified from since‐birth and last week recall methods. Based on multivariate analysis mothers in the intervention group were 1.7 times (OR 1.69; 95% CI [1.19, 2.41]) more likely to initiate early breastfeeding. Regarding breastfeeding practices, mothers in the intervention group were about 10 times (OR 10.15; 95% CI [6.06, 17.02]) and 7.5 times (OR 7.46; 95% CI [3.95, 14.11]) more likely to practice EBF from birth to 1 and 4 months than mothers in the control group. Because no study subjects were defined as EBF at 6 months in the control site, a value of 0.5 was added in each cell of the 2 × 2 table to calculate ORs as a measure of intervention effect. Based on this crude analysis, mothers in the intervention group were 17 times (95% CI [0.96, 294.8]) and 35.5 times (95% CI [2.1, 594.9]) as more likely to practice EBF than mothers in the control group, by since‐birth and last week recall methods, respectively.
Table 4.
Logistic regression analyses displaying crude and adjusted odds ratios for early initiation, exclusive breastfeeding at 1 month (n = 771), 4 months (n = 756), and 6 months (n = 761; adjusted for residence, type of family, maternal education, and father's occupation, household economics and type of delivery)
| Early initiation of breastfeeding | Yes n (%) | No n (%) | Crude OR | 95% CI | Adjusted OR | 95% CI |
|---|---|---|---|---|---|---|
| Control | 144 (35.7) | 259 (64.3) | 1 | 1 | ||
| n = 403 | ||||||
| Intervention | 179 (48.6) | 189 (51.4) | 1.70*** | 1.28‐2.27 | 1.69** | 1.19 – 2.41 |
| n = 368 | ||||||
| 1‐month EBF since birth recall | Yes | No | ||||
| n (%) | n (%) | |||||
| Control | 23 (5.7) | 380 (94.3) | 1 | 1 | ||
| n = 403 | ||||||
| Intervention | 128 (34.8) | 240 (65.2) | 8.81*** | 5.49‐14.13 | 10.15*** | 6.06‐17.02 |
| n = 368 | ||||||
| 4‐month EBF since birth recall | Yes | No | ||||
| n (%) | n (%) | |||||
| Control | 16 (4.0) | 381 (96.0) | 1 | 1 | ||
| n = 397 | ||||||
| Intervention | 67 (18.7) | 292 (81.3) | 5.56*** | 3.1‐9.63 | 7.46*** | 3.95‐14.11 |
| n = 359 | ||||||
| 4‐month last week recall | Yes | No | ||||
| n (%) | n (%) | |||||
| Control | 120 (30.2) | 277 (69.8) | 1 | 1 | ||
| n = 397 | ||||||
| Intervention | 139 (38.7) | 220 (61.3) | 1.46* | 1.10‐1.97 | 1.37 | 0.99–1.90 |
| n = 359 | ||||||
| 6‐month EBF since birth recall(*) | Yes | No | ||||
| n (%) | n (%) | |||||
| Control | 0.5 (0.13) | 396.5 (99.87) | 1 | |||
| n = 397 | ||||||
| Intervention | 7.5 (2.07) | 354.5 (97.93) | 16.78 | 0.96–294.8 | NA | NA |
| n = 362 | ||||||
| 6‐month last week recall(*) | Yes | No | ||||
| n (%) | n (%) | |||||
| Control | 0.5 (0.13) | 396.5 (99.87) | 1 | |||
| n = 397 | ||||||
| Intervention | 15.5 (4.4) | 346.5 (95.728) | 35.47*** | 2.1‐594.9 | NA | NA |
| n = 362 |
Note. OR: odds ratio.
P < 0.05;
P < 0.01;
P < 0.001;
0.5 was added to each cell to calculate crude ORs; NA: Not applicable.
Survival analysis was carried out to estimate the impact of intervention on EBF at 1, 4, and 6 months. Figure 3 presents the survival curve for EBF in the first 6 months for infants in the control and interventions groups. The rates of EBF were significantly greater in the intervention group (the results of Logrank and Breslow tests for comparisons at 4 and 6 months were <0.001.) As showed in Figure 3, the larger differences in EBF rates were found in the first 4 months after birth. At the end of 6 months, the reduction in EBF found in both the intervention and control groups was extremely small.
Figure 3.
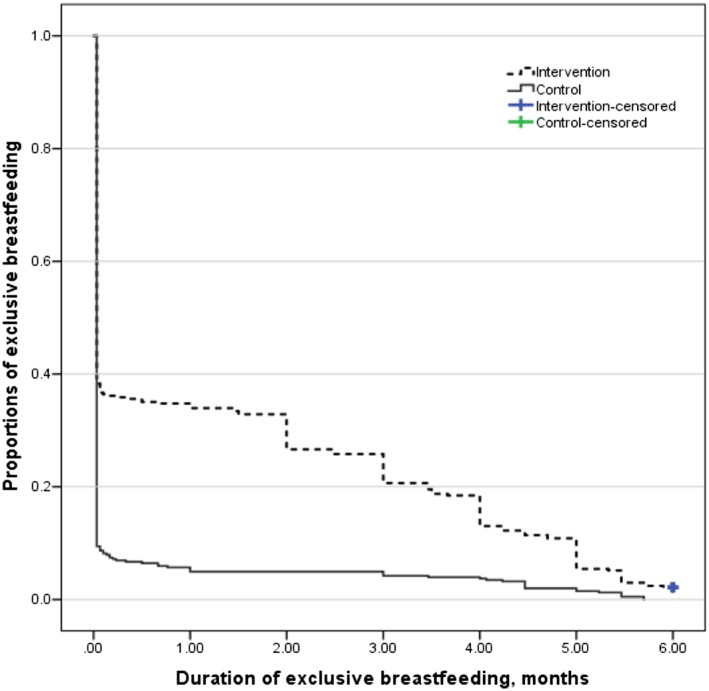
Kaplan–Meier curves of duration of exclusive breastfeeding in first 6 months after birth for intervention (n = 368, 7 mothers still practice exclusive breastfeeding) and control group (n = 403, 0 mothers practice exclusive breastfeeding)
Table 5 shows the impact of the intervention on EBF estimated by crude and adjusted hazard ratios (HR). The results of multivariate Cox regression indicate that the intervention has reduced by 35% the cessation of EBF in the first month (HR 0.65; CI 95% [0.54, 0.77]), by 33% (HR = 0.67; CI 95% [0.57, 0.79]), and 31% (HR = 0.69; CI 95% [0.59, 0.81]) in the first 4 and 6 months respectively.
Table 5.
Cox regression analyses displaying crude and adjusted hazard ratios for cessation of exclusive breastfeeding at 1, 4, and 6 months between intervention and control (adjusted for residence, type of family, maternal education, and father's occupation, household economics, and type of delivery)
| 1‐month exclusive breastfeeding | Crude HR | 95% CI | Adjusted HR | 95% CI |
|---|---|---|---|---|
| Control | 1 | 1 | ||
| n = 403 | ||||
| Intervention | 0.65*** | 0.55–0.76 | 0.65*** | 0.54–0.77 |
| n = 368 | ||||
| 4‐month exclusive breastfeeding | ||||
| Control | 1 | 1 | ||
| n = 403 | ||||
| Intervention | 0.68*** | 0.58–0.80 | 0.67*** | 0.57–0.79 |
| n = 368 | ||||
| 6‐month exclusive breastfeeding | ||||
| Control | 1 | 1 | ||
| n = 403 | ||||
| Intervention | 0.70*** | 0.60–0.81 | 0.69*** | 0.59–0.81 |
| n = 368 |
Note. HR: hazard ratio.
P < 0.001.
4. DISCUSSION
This study provides additional evidence that an integrated community‐based intervention directed at fathers may significantly improve early initiation and exclusivity of breastfeeding practices after delivery. Based on adjusted findings from multivariate logistic regression and Cox proportional hazards models, mothers in the intervention area whose husbands participated in the breastfeeding promotion program reported earlier initiation of breastfeeding and better EBF at 1, 4 and 6 months (by both since‐birth and last week recall method) than mothers in the control group.
The positive impact of the intervention on early initiation of breastfeeding was also found in a controlled trial testing the role of the father in supporting breastfeeding by providing breastfeeding education in antenatal class (Wolfberg et al., 2004) and in a quasi‐experimental study carried out with similar intervention strategy on getting father's involvement, in rural context of Vietnam (Bich et al., 2016). The current study found the same pattern of positive intervention effects on exclusive breastfeeding at 4 months as was reported from a Brazilian randomized controlled study carried out in 2008 (Susin & Giugliani, 2008a) and at 6 months in another controlled study carried out in Italy (Pisacane et al., 2005). In these two studies, couples were recruited after delivery and the intervention targeting fathers implemented during the post‐partum period and in a hospital setting. A similar positive impact of father's involvement on 4 and 6 months EBF in our study was also found in other quasi‐experimental studies carried out in Vietnam (Bich et al., 2014) and in China (Su & Ouyang, 2016). While other studies targeted and educated fathers through breastfeeding classes in hospital and clinic settings (Abbass‐Dick et al., 2015; Lovera, Sanderson, Bogle, & Vela Acosta, 2010; Maycock et al., 2013; Susin & Giugliani, 2008a; Wolfberg et al., 2004), in our community‐based study, in addition to educational and counselling activities at commune health centres and at home visits, fathers were also counselled at the delivery in the obstetric wards of district hospital when they accompanied their wives for the delivery. In our study, a father's network was established through activities of fathers' club established in 13 communes. The experience of father's involvement in supporting EBF was shared and encouraged through the club's social activities led by a paternal leader and supported by local stakeholders. Because more women in rural Vietnam deliver at the hospital rather than in the commune health centre, counselling for fathers at delivery in district hospitals helped to increase access of fathers to breastfeeding promotion.
In our study, a large sample size of 771 couples were recruited before the delivery and the intervention targeting fathers took place at antenatal, delivery, and post‐partum periods compared with previous intervention studies that had smaller sample sizes and were carried out in a short period of time either at the antenatal (Maycock et al., 2013) or post‐partum period (Abbass‐Dick et al., 2015; Lovera et al., 2010; Pisacane et al., 2005; Su & Ouyang, 2016; Susin & Giugliani, 2008a). Mothers were followed up and EBF statuses were defined at the end of 1, 4, and 6 months after delivery. It has previously been shown that mothers are able to recall breastfeeding practices accurately (Li, Scanlon, & Serdula, 2005).
Several studies have discussed the limitations of using populations of infants from 0 to 4 and 6 months and 24‐hour recall to estimate exclusive breastfeeding practices because it oftenoverestimates these indicators compared with since‐birth recall method (Aarts et al., 2000; Agampodi, Agampodi, & Silva, 2009). In our study, exclusivity of breastfeeding status was better identified because it was measured by more valid last‐week and since‐birth recall methods used in previous studies (Aarts et al., 2000; Bich et al., 2014) and denominators for estimation of proportions of exclusive breastfeeding at 1, 4, and 6 months were a unique population of infants that has been followed since birth.
This community‐based intervention study was designed and implemented based on social cognitive theory (Bandura, 1998; Bich, 2017) and theory of planned behaviors (Ajzen, 1991; Bich & Tuan, 2017). It applied the principles of the continuum of care (Kerber et al., 2007) to integrate into the primary peripheral health care system. Collaboration with Vietnamese stakeholders is highly recommended (Duong, Binns, & Lee, 2004; Kerber et al., 2007; Nguyen et al., 2013) for successful implementation to improve early initiation and EBF (Bich et al., 2014; Bich et al., 2016). The changes of the fathers' knowledge, attitude, and practices as well as the intention of the mother toward EBF may provide additional information on the ways the intervention effects mothers' breastfeeding practices (Bich, 2017; Bich & Tuan, 2017).
Although there is the risk that participants in the control group may have been exposed to some components of the intervention because the control district is in the same province as the intervention district, such cross‐contamination is unlikely because the two districts do not share a common border. In addition, there were no breastfeeding promotion programs carried out in Hai Duong province at the time of our intervention. Selection bias was not an issue because all eligible pregnant women, in both the intervention and control sites, were selected at the same time, by the same sampling procedure, and with high participation levels of 95%.
4.1. Limitations
There are limitations to the study that need to be mentioned. There were some differences regarding basic socioeconomic status found between the intervention and control groups at baseline. These differences were taken into account in both multivariate logistic and Cox regression analysis. The lack of data on breastfeeding practices of the same study subjects prior to the intervention in the two areas must also be taken into account when interpreting the results. However, based on the results of the survey carried out to assess the equivalence between the two sites, the proportions of early initiation and EFB prior to the initiation of the current study were not significantly different between intervention and control sites (Bich & Thuy, 2017). Although an independent team of data collectors used to evaluate breastfeeding practices was “blinded” to the study hypotheses, the exclusive breastfeeding practices reported by the mothers in the intervention site might still be overestimated by the public part of the intervention. Based on our supervision report, there was only about 50% of fathers received individual counselling at the time of delivery. We could not provide individual counselling for all fathers because mothers gave birth in other hospitals outside of the intervention district (at the provincial and central hospitals). In addition to that, the admission of the pregnant women at different times (night, weekend) did not always match with the time the counsellor was on duty.
The fathers were encouraged to organize club's activities in different locations (house of father's leader, commune health centre), at different times (evening, weekend) to get more involvement of the fathers. However, the participation rate was low, and this may be due to the fact that many of them having busy work schedules with occupations such as truck driver, construction worker, and worker in factories. Despite the fact that quasi‐experimental study designs do not allow for non‐random allocation of the study subjects to the intervention and control group, in the current study, the differences between the two groups were controlled during multivariate analysis. However, we were not being able to control for unobserved potential confounding factors that could have been controlled through randomization, and this may influence the validity of the intervention effect. In this study, we have used individual‐level data in the analysis, and this kind of analysis may ignore the effect of implicit clustering at the commune level. Such analysis may overestimate the precision of the intervention effect. However, the implicit clustering effect at commune level may not be a problem because all communes in the district are very homogenous in terms of ethnicity and socio‐economic development. Dose–response analysis and analysis of individual intervention components were not carried out because this was not an objective of the study and all the components were designed and implemented simultaneously during the intervention period. This study and current literature have provided evidence about the role of father in supporting mother's breastfeeding practices. In our opinion, at the global level, the role of father has not been taken into account properly even in the original (1989) and revised Ten Steps to Successful Breastfeeding (2018) recommended by the UNICEF and WHO (1989, 2018).
5. CONCLUSIONS
Despite some limitations of quasi‐experimental design, we believe that the intervention to involve fathers in breastfeeding promotion has added additional positive evidence on the effects of the intervention on early initiation of breastfeeding and EBF rates at 1, 4, and 6 months. To get fathers involved, the issue of socio‐economical, cultural, and political context should be thoughtfully understood and taken into account during designing and implementation of the intervention. The replication of the model in other settings should consider the capacity and function of health workers at the peripheral level and consider issues involving the social network of fathers and barriers that fathers need to overcome to be effectively become involved in child care. Fathers can be directly engaged at district hospitals, at commune health centres, and at home where participation in social events supporting breastfeeding and in fathers' groups is promoted to sustain their continued involvement. We suggest a future study of cluster randomized controlled trials together with multilevel analysis to come up with more valid measures of fathers' involvement. Father's involvement could be explicitly addressed and possibly then considered as an additional component of the Ten Steps recommended by WHO on breastfeeding promotion. Responsible government agencies (Ministry of Health, National Institute of Nutrition) and committed NGOs (UNICEF, WHO, and others) could consider integrating breastfeeding counselling for fathers in existing maternal and child health services at commune health centres and in hospital maternity wards.
CONFLICTS OF INTERESTS
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
THB acted as principal investigator of the study. THB developed the study design together with DHTP and analysed data together with TKL. THB produced the first draft of the article. All authors were involved in the writing of the manuscript and have approved the final version for publication.
ACKNOWLEDGEMENTS
This study was supported by Grand Challenges Canada. We would like to thank Dr. Lynn Rempel and Dr. John Rempel, the research team, and the fathers, mothers, infants, and health care workers at the Kim Thanh and Cam Giang health centres for their collaboration in this study. We would also like to thank Professor Philip Nasca for his kind support on reviewing and English editing of the manuscript.
Bich TH, Long TK, Hoa DP. Community‐based father education intervention on breastfeeding practice—Results of a quasi‐experimental study. Matern Child Nutr. 2019;15(S1):e12705 10.1111/mcn.12705
REFERENCES
- Aarts, C. , Kylberg, E. , Honell, A. , Hofvander, Y. , Gebre‐Medhin, M. , & Greiner, T. (2000). How exclusive is exclusive breastfeeding? A comparison of data since birth with current status data. International Journal of Epidemiology, 29, 1041–1046. 10.1093/ije/29.6.1041 [DOI] [PubMed] [Google Scholar]
- Abbass‐Dick, J. , Stern, S. , Nelson, L. , Watson, W. , & Dennis, C. (2015). Coparenting breastfeeding support and exclusive breastfeeding: A randomized controlled trial. Pediatrics, 135, 102–110. 10.1542/peds.2014-1416 [DOI] [PubMed] [Google Scholar]
- Agampodi, S. , Agampodi, T. , & Silva, A. (2009). Exclusive breastfeeding in Sri Lanka: Problems of interpretation of reported rates. International Breastfeeding Journal, 4, 14 10.1186/1746-4358-4-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agunbiade, M. O. , & Ogunleye, O. V. (2012). Constraints to exclusive breastfeeding practice among breastfeeding mothers in Southwest Nigeria: Implications for scaling up. International Breastfeeding Journal, 7, 5 10.1186/1746-4358-7-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajzen, I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179–211. 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- Bandura, A. (1998). Health promotion from the perspective of social cognitive theory. Psychology and Health, 13, 623–649. 10.1080/08870449808407422 [DOI] [Google Scholar]
- Bar‐Yam, B. , & Darby, L. (1997). Fathers and breastfeeding: A review of literature. Journal of Human Lactation, 13, 45–50. 10.1177/089033449701300116 [DOI] [PubMed] [Google Scholar]
- Bich, T. (2017). Changes of knowledge, attitude and practice of fathers regarding supporting six months exclusive breastfeeding: Results of a community based intervention applying social cognitive theory. Journal of Health and Development Studies, 1, 19–28. [Google Scholar]
- Bich, T. , & Cuong, N. (2017). Changes in knowledge, attitude and involvement of fathers in supporting exclusive breastfeeding: A community based intervention study in a rural area of Vietnam. International Journal of Public Health, 62, 17–26. 10.1007/s00038-016-0882-0 [DOI] [PubMed] [Google Scholar]
- Bich, T. , Hoa, D. , Ha, N. , Vui, L. , Nghia, D. , & Målqvist, M. (2016). Father's involvement and its effect on early breastfeeding practices in Viet Nam. Maternal & Child Nutrition, 12, 768–777. 10.1111/mcn.12207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bich, T. , Hoa, D. , & Malqvist, M. (2014). Fathers as supporters for improved exclusive breastfeeding in Viet Nam. Maternal and Child Health Journal, 18, 1444–1453. 10.1007/s10995-013-1384-9 [DOI] [PubMed] [Google Scholar]
- Bich, T. , & Thuy, H. (2017). Relationship between exclusive breastfeeding and infant development at 9 months: Results of a cross‐sectional study in Hai Duong province. Journal of Health and Development Studies, 2, 81–90. [Google Scholar]
- Bich, T. , & Tuan, D. (2017). Intention and practice of exclusive breastfeeding for the first six months: The results of a community‐based intervention targeting fathers applying theory of planned behavior. Journal of Health and Development Studies, 1, 29–37. [Google Scholar]
- Brown, A. , & Davies, R. (2014). Fathers' experiences of supporting breastfeeding: Challenges for breastfeeding promotion and education. Maternal & Child Nutrition, 10, 510–526. 10.1111/mcn.12129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clifford, J. , & McIntyre, E. (2008). Who supports breastfeeding? Breastfeeding Review, 16, 9–19. [PubMed] [Google Scholar]
- Cohen, R. J. , Brown, K. H. , Rivera, L. L. , & Dewey, K. G. (1999). Promoting exclusive breastfeeding for 4‐6 months in Honduras: Attitudes of mothers and barriers to compliance. Journal of Human Lactation, 15, 9–18. 10.1177/089033449901500107 [DOI] [PubMed] [Google Scholar]
- Dearden, K. , Quan, L. , Do, M. , Marsh, D. , Pachón, H. , Schroeder, D. , & Lang, T. T. (2002). Work outside the home is the primary barrier to exclusive breastfeeding in rural Viet Nam: Insights from mothers who exclusively breastfed and worked. Food and Nutrition Bulletin, 23, 101–108. [PubMed] [Google Scholar]
- Deeks, J. , & Higgins, J. (2010). Statistical algorithms in review. Manager, 5. [Google Scholar]
- Duong, D. , Binns, C. , & Lee, A. (2004). Breast‐feeding initiation and exclusive breast‐feeding in rural Vietnam. Public Health Nutrition, 7, 795–799. [DOI] [PubMed] [Google Scholar]
- Duong, D. V. , Binns, C. , & Lee, A. H. (2005). Introduction of complementary food to infant within the first six months postpartum in rural Viet Nam. Acta Paediatrica, 94, 1714–1720. 10.1080/08035250510042906 [DOI] [PubMed] [Google Scholar]
- Duong, D. V. , Lee, A. H. , & Binns, C. W. (2005). Determinants of breast‐feeding within the first 6 months post‐partum in rural Vietnam. Journal of Paediatrics and Child Health, 41, 338–343. 10.1111/j.1440-1754.2005.00627.x [DOI] [PubMed] [Google Scholar]
- Fjeld, E. , Siziya, S. , Katepa‐Bwalya, M. , Kankasa, C. , Moland, K. , & Tylleskär, T. (2008). No sister, the breast alone is not enough for my baby a qualitative assessment of potentials and barriers in the promotion of exclusive breastfeeding in southern Zambia. International Breastfeeding Journal, 3, 26 10.1186/1746-4358-3-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forster, D. , McLachlan, H. , & Lumley, J. (2006). Factors associated with breastfeeding at six months postpartum in a group of Australian women. International Breastfeeding Journal, 1, 18 10.1186/1746-4358-1-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstman, B. (2003). Epidemiology kept simple: An introduction to traditional and modern epidemiology (Second edition ed.)John Wiley & Sons, Inc. [Google Scholar]
- Haroon, S. , Das, J. , Salam, R. , Imdad, A. , & Bhutta, Z. (2013). Breastfeeding promotion interventions and breastfeeding practices: A systematic review. BMC Public Health, 13, S20 10.1186/1471-2458-13-S3-S20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hector, D. , King, L. , Webb, K. , & Heywood, P. (2005). Factors affecting breastfeeding practices: Applying a conceptual framework. New South Wales Public Health Bulletin 2005 Mar‐Apr, 16(3–4), 52–55. [DOI] [PubMed] [Google Scholar]
- Kerber, K. , de Graft‐Johnson, J. , Bhutta, Z. , Okong, P. , Starrs, A. , & Lawn, J. (2007). Continuum of care for maternal, newborn, and child health: From slogan to service delivery. Lancet, 370, 1358–1369. 10.1016/S0140-6736(07)61578-5 [DOI] [PubMed] [Google Scholar]
- Li, R. , Scanlon, K. S. , & Serdula, M. K. (2005). The validity and reliability of maternal recall of breastfeeding practice. Nutrition Reviews, 63, 103–110. 10.1111/j.1753-4887.2005.tb00128.x [DOI] [PubMed] [Google Scholar]
- Lovera, D. , Sanderson, M. , Bogle, M. L. , & Vela Acosta, M. (2010). Evaluation of a breastfeeding peer support program for fathers of Hispanic participants in a Texas special supplemental nutrition program for women, infants, and children. Journal of the American Dietetic Association, 110, 1696–1702. 10.1016/j.jada.2010.08.001 [DOI] [PubMed] [Google Scholar]
- Maycock, B. , Binns, C. , Dhaliwal, S. , Tohotoa, J. , Hauck, Y. , Burns, S. , et al. (2013). Education and support for fathers improves breastfeeding rates: A randomized controlled trial. Journal of Human Lactation, 29, 484–490. 10.1177/0890334413484387 [DOI] [PubMed] [Google Scholar]
- Meedya, S. , Fahy, K. , & Kable, A. (2010). Factors that positively influence breastfeeding duration to 6 months: A literature review. Women and Birth, 23, 135–145. 10.1016/j.wombi.2010.02.002 [DOI] [PubMed] [Google Scholar]
- Mitchell‐Box, K. , & Braun, K. (2013). Impact of male‐partner‐focused interventions on breastfeeding initiation, exclusivity, and continuation. Journal of Human Lactation, 24, 473–479. [DOI] [PubMed] [Google Scholar]
- Morrow, M. (1996). Breastfeeding in Vietnam: Poverty, tradition, and economic transition. Journal of Human Lactation, 12, 97–103. 10.1177/089033449601200211 [DOI] [PubMed] [Google Scholar]
- Nguyen, P. , Keithly, S. , Nguyen, N. , Nguyen, T. , Tran, L. , & Hajeebhoy, N. (2013). Prelacteal feeding practices in Vietnam: Challenges and associated factors. BMC Public Health, 13, 932 10.1186/1471-2458-13-932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otoo, G. E. , Lartey, A. A. , & Perez‐Escamilla, R. (2009). Perceived incentives and barriers to exclusive breastfeeding among periurban Ghanaian women. Journal of Human Lactation, 25, 34–41. 10.1177/0890334408325072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pisacane, A. , Continisio, G. , Aldinucci, M. , D'Amora, S. , & Continisio, P. (2005). A controlled trial of the father's role in breastfeeding promotion. Pediatrics, 116, 494–498. [DOI] [PubMed] [Google Scholar]
- Prior, E. , Santhakumaran, S. , Gale, C. , Philipps, L. H. , Modi, N. , & Hyde, M. J. (2012). Breastfeeding after cesarean delivery: A systematic review and meta‐analysis of world literature. The American Journal of Clinical Nutrition, 95, 1113–1135. 10.3945/ajcn.111.030254 [DOI] [PubMed] [Google Scholar]
- Raj, V. , & Plicha, S. (1998). The role of social support in breastfeeding promotion: A Literature Review. Journal of Human Lactation, 14, 41–45. 10.1177/089033449801400114 [DOI] [PubMed] [Google Scholar]
- Rollins, N. C. , Bhandari, N. , Hajeebhoy, N. , Horton, S. , Lutter, C. K. , Martines, J. C. , … Victora, C. G. (2016). Why invest, and what it will take to improve breastfeeding practices? Lancet, 387, 491–504. 10.1016/S0140-6736(15)01044-2 [DOI] [PubMed] [Google Scholar]
- Sherriff, N. , Hall, V. , & Panton, C. (2014). Engaging and supporting fathers to promote breast feeding: A concept analysis. Midwifery, 30, 667–677. 10.1016/j.midw.2013.07.014 [DOI] [PubMed] [Google Scholar]
- Sinha, B. , Chowdhury, R. , Sankar, M. , Martines, J. , Taneja, S. , Mazumder, S. , … Bhandari, N. (2015). Interventions to improve breastfeeding outcomes: A systematic review and meta‐analysis. Acta Paediatrica, 104, 114–134. 10.1111/apa.13127 [DOI] [PubMed] [Google Scholar]
- Su, M. , & Ouyang, Y. (2016). Father's role in breastfeeding promotion: Lessons from a quasi‐experimental trial in China. Breastfeeding Medicine, 11, 144–149. 10.1089/bfm.2015.0144 [DOI] [PubMed] [Google Scholar]
- Susin, L. , & Giugliani, E. (2008a). Inclusion of fathers in an intervention to promote breastfeeding: Impact on breastfeeding rates. Journal of Human Lactation, 24, 386–392. 10.1177/0890334408323545 [DOI] [PubMed] [Google Scholar]
- Susin, L. , & Giugliani, E. (2008b). Inclusion of fathers in an intervention to promote breastfeeding: Impact on breastfeeding rates. Journal of Human Lactation, 24. [DOI] [PubMed] [Google Scholar]
- Thrive, A . (2012). Formative research on infant and young child feeding in Viet Nam: Phase 1 summary report. Alive & Thrive, Ha Noi ‐ Viet Nam.
- Tuyen, L. , & Hop, L. (2012). General nutrition survey 2009–2010. Medical publishing house, Ha Noi.
- Victora, C. G. , Bahl, R. , Barros, A. J. D. , França, G. V. A. , Horton, S. , Krasevec, J. , … Rollins, N. C. (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. The Lancet, 387, 475–490. 10.1016/S0140-6736(15)01024-7 [DOI] [PubMed] [Google Scholar]
- WHO (2003). Global strategy for infant and young child feeding. World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland
- WHO (2010). Indicators for assessing infant and young child feeding practices part 3: Country profiles. World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland
- WHO & UNICEF . (1989). Protecting, promoting and supporting breast‐feeding: The special role of maternity services. Geneva: World Health Organization. [Google Scholar]
- WHO & UNICEF . (2018). Implementation guidance: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services—The revised baby‐friendly hospital initiative. Geneva: World Health Organization. [PubMed] [Google Scholar]
- Wolfberg, A. , Michels, K. , Shields, W. , O'Campo, P. , Bronner, Y. , & Bienstock, J. (2004). Dads as breastfeeding advocates: Results from a randomized controlled trial of an educational intervention. American Journal of Obstetrics and Gynecology, 191, 708–712. 10.1016/j.ajog.2004.05.019 [DOI] [PubMed] [Google Scholar]


