Abstract
Global evidence demonstrates that adherence to the Baby Friendly Initiative (BFI) has a positive impact on multiple child health outcomes, including breastfeeding initiation and duration up to 1 year post‐partum. However, it is currently unclear whether these findings extend to specific countries with resource‐rich environments. This mixed‐methods systematic review aims to (a) examine the impact of BFI implementation (hospital and community) on maternal and infant health outcomes in the United Kingdom (UK) and (b) explore the experiences and views of women receiving BFI‐compliant care in the UK. Two authors independently extracted data including study design, participants, and results. There is no UK data available relating to wider maternal or infant health outcomes. Two quantitative studies indicate that Baby Friendly Hospital Initiative implementation has a positive impact on breastfeeding outcomes up to 1 week post‐partum but this is not sustained. There was also some evidence for the positive impact of individual steps of Baby Friendly Community Initiative (n = 3) on breastfeeding up to 8 weeks post‐partum. Future work is needed to confirm whether BFI (hospital and community) is effective in supporting longer term breastfeeding and wider maternal and infant health outcomes in the UK. A meta‐synthesis of five qualitative studies found that support from health professionals is highly influential to women's experiences of BFI‐compliant care, but current delivery of BFI may promote unrealistic expectations of breastfeeding, not meet women's individual needs, and foster negative emotional experiences. These findings reinforce conclusions that the current approach to BFI needs to be situationally modified in resource‐rich settings.
Keywords: Baby Friendly Initiative, breastfeeding, health, infant, maternal, UK
Key messages.
There is insufficient evidence to draw firm conclusions about the impact of BFI implementation on maternal and infant health outcomes in the UK. There is no data available relating to wider physical maternal or infant health outcomes.
Two quantitative studies indicate that BFHI implementation has a positive impact on breastfeeding to one week but this is not sustained. No evaluation of the full BFCI programme is available.
A meta‐synthesis finds that support is highly influential to women's experiences of BFI‐compliant care, but current provision may promote unrealistic expectations of breastfeeding, not meet women's individual needs, and foster negative emotional experiences. A mixed‐methods synthesis demonstrates that infant feeding support provided in BFI‐accredited settings should be regular, personal, and practical.
1. INTRODUCTION
Breastfeeding has major long‐term positive effects on the health, nutrition, and development of the child and on women's physical and mental health (Dennis & McQueen, 2009; Fallon, Groves, Halford, Bennett, & Harrold, 2016; Victora et al., 2016). The World Health Organisation (WHO) recommends breastfeeding initiation within an hour after birth, exclusive breastfeeding for the first 6 months of life, followed by the introduction of complementary foods alongside continued breastfeeding until the child is at least 2 years old (WHO, 2015).
To achieve these benefits for all mothers and infants, an ongoing global strategy for breastfeeding protection, promotion, and support has been in position for over 25 years (WHO & UNICEF, 1990). Its principal aim is to create a global environment that empowers women to breastfeed. The Baby Friendly Hospital Initiative (BFHI) was launched by WHO and UNICEF in 1991 to assist in the implementation of this aim by improving breastfeeding initiation, duration, and exclusivity within hospitals and maternity units. To receive BFHI accreditation, maternity units must restrict the use of breast milk substitutes in accordance with the International Code of Marketing of Breast‐milk Substitutes and implement 10 specific interventions to support successful breastfeeding (UNICEF, 2018a; Table 1). Since the inception of BFHI, more than 15,000 facilities in 152 countries have been awarded Baby Friendly status (UNICEF, 2016; WHO, 2018). The initiative has now been expanded to include community services, with a dedicated 7‐point plan (Table 2) to enable improved practice in community health care, in order to support sustained breastfeeding in line with WHO recommendations (UNICEF, 2017).
Table 1.
Ten steps to successful breastfeeding
| Every facility providing maternity services and care for newborn infants should |
| 1a. Comply fully with the International Code of Marketing of Breast‐milk Substitutes and relevant World Health Assembly resolutions; |
| 1b. Have a written infant feeding policy that is routinely communicated to staff and parents; |
| 1c. Establish ongoing monitoring and data‐management systems; |
| 2. Ensure that staff have sufficient knowledge, competence, and skills to support breastfeeding; |
| 3. Discuss the importance and management of breastfeeding with pregnant women and their families; |
| 4. Facilitate immediate and uninterrupted skin‐to‐skin contact and support mothers to initiate breastfeeding as soon as possible after birth; |
| 5. Support mothers to initiate and maintain breastfeeding and manage common difficulties; |
| 6. Do not provide breastfed newborns any food or fluids other than breast milk, unless medically indicated; |
| 7. Enable mothers and their infants to remain together and practice rooming in 24 hr a day; |
| 8. Support mothers to recognise and respond to their infant's cues for feeding; |
| 9. Counsel mothers on the use and risks of feeding bottles, teats, and pacifiers; |
| 10. Coordinate discharge so that parents and their infants have timely access to ongoing support and care. |
Source: Ten Steps to Successful Breastfeeding (revised 2018).
Table 2.
BFI—7‐point plan for sustaining breastfeeding in the community
| 1. Have a written breastfeeding policy that is routinely communicated to all health care staff |
| 2. Train all staff involved in the care of mothers and babies in the skills necessary to implement the policy |
| 3. Inform all pregnant women about the benefits and management of breastfeeding |
| 4. Support mothers to initiate and maintain breastfeeding |
| 5. Encourage exclusive and continued breastfeeding, with appropriately timed introduction of complementary foods |
| 6. Provide a welcoming atmosphere for breastfeeding families. |
| 7. Promote cooperation between health care staff, breastfeeding support groups, and the local community |
Note. BFI: Baby Friendly Initiative.
Source: UNICEF (2017) Baby Friendly 7 Point Plan.
Despite these extensive efforts, globally, less than 40% of infants aged less than 6 months of age are exclusively breastfed (Victora et al., 2016). Higher income countries have even shorter exclusive breastfeeding durations, and the UK has one of the lowest rates in the world (less than 1% at 6 months; Mcandrew et al., 2012; Victora et al., 2016). This leaves breastfeeding rates far below international targets and the large majority of infants still receiving some formula milk in the first 6 months of life. In terms of policy and investment, commitment to breastfeeding is in “a state of fatigue” (Victora et al., 2016, p. 491), which warrants reviews of current practice.
Only one systematic review has examined the impact of BFHI on breastfeeding and child health outcomes, both globally and specific to the United States (US) (Pérez‐Escamilla, Martinez, & Segura‐Pérez, 2016). Global evidence supported the conclusion that adherence to BFHI steps had a positive impact on multiple child health outcomes, including breastfeeding initiation and duration up to 1 year post‐partum. However, the U.S. BFHI evidence only demonstrated improvements in breastfeeding up to 6 weeks, and these were not sustained. It is currently unclear whether these findings extend to other countries with resource‐rich environments. Additionally, Perez‐Escamilla et al. (2016) noted that community support was vital for long‐term sustainability of breastfeeding outcomes, but no review has yet examined the impact of community BFI (BFCI) implementation.
Both qualitative and quantitative studies in resource‐rich settings indicate that the current approach to infant feeding promotion and support may be related to negative emotional and practical experiences in new mothers (Fallon et al., 2016; Knaak, 2006; Lee, 2007; Schmied, Beake, Sheehan, McCourt, & Dykes, 2011; Spencer, Greatrex‐White, & Fraser, 2015). However, these studies do not specify whether the populations were drawn from BFI‐accredited settings. It is important to consider whether BFI has implications that extend beyond breastfeeding outcomes yet there has been no review of literature that explores the experiences of women receiving infant feeding care under a BFI framework. A synthesis of available qualitative literature may provide important additional insights.
Comparable with the rationale for Perez‐Escamilla et al. (2016) review, the UK is currently undergoing major legislation and policy decisions in relation to breastfeeding promotion and support (All Party Parliamentary Group, 2016; Royal College of Midwives, 2018). A review of current provision specific to the UK has not yet been conducted. This will provide a valuable evidence synthesis to inform consultations and future research. This mixed‐methods systematic review aims to (a) examine the impact of BFI implementation (hospital and community) on maternal and infant health outcomes in the UK and (b) explore the experiences and views of women receiving BFI‐compliant care in the UK.
2. METHOD
A protocol was developed based initially on the work of Perez‐Escamilla et al. (2016) but with the inclusion of information relevant to the qualitative component of the review. In order to directly address the research questions, the search strategy (Table 3) and eligibility criteria (Table 4) for studies to be included in the review were designed in line with PICOS criteria (population, intervention, comparator, outcomes, study design and setting; Sayers, 2008).
Table 3.
PICOS search strategy
| Search no. | PICOS component | Search terms (search function OR) |
|---|---|---|
| 1 | Population | women, mother, maternal, pregnan($), post‐partum, infant, child, baby |
| 2 | Intervention | Baby Friendly Initiative, Baby friendly Hospital Initiative, BFI, BFHI, 10 steps, |
| N/A | Comparator | N/A |
| 3 | Outcomes | Depression, depress($), anxiety, anxi($), quality of life, QOL distress, stress, well‐being, mental health, mental illness, obes($), diet, eat, feeding style, complementary feeding, morbidity, disease, illness, mortality |
| 4 | Study design and setting | [Any design] UK, England, Northern Ireland, Wales, Scotland |
Note. BFI: Baby Friendly Initiative; BFHI: Baby Friendly Hospital Initiative; PICOS: population, intervention, comparator, outcomes, study design and setting. 1 AND 2 AND 3 AND 4. Limits: UK, since 1991.
Table 4.
Inclusion and exclusion criteria
| Inclusion criteria |
|
|
|
|
|
|
| Exclusion criteria |
|
|
|
|
|
|
Note. BFI: Baby Friendly Initiative.
2.1. Eligibility criteria
Published studies using any methodology (qualitative, quantitative, and mixed) were eligible if they collected data relating to the implementation of BFI (full and/or partial accreditation, or implementation of any of the 10 steps) and any maternal and infant physical and mental health outcomes. Health outcomes examined were kept deliberately broad in an attempt to capture the impact of BFI implementation on both infant feeding and wider physical and mental health (see Table 3). Studies that explored the experiences and views of women receiving BFI compliant care were also eligible (a BFI hospital or community setting had to be explicitly detailed in the paper). All studies that included women who were pregnant or had children under the age of two conducted in a UK setting were considered. Studies published before the introduction of BFI (i.e., <1991) were not deemed eligible.
2.2. Search strategy
Scoping searches aided shaping of the resulting search strategy displayed in Table 3, which was then applied to the following databases: Web of Science, PubMed, and EBSCO. Study selection was conducted by the review authors (V. F. and A. C.) including initial screening of titles and abstracts, then following the removal of duplicates, full‐text eligibility checks against full inclusion criteria. Boolean operators were applied to blend the keywords, and truncation was used to retrieve variants of each keyword. Reference lists of all full‐texts identified were hand searched to identify any further studies eligible for inclusion alongside correspondence to authors where necessary. Searches were conducted between June and August 2017. J. H. independently assessed 10% of studies identified following title and abstract screening to enable reliability checking of full‐text eligibility assessments. Agreement obtained between reviewers was 100%. Figure 1 provides a PRISMA flow diagram displaying the full study selection process.
Figure 1.

PRISMA flow diagram demonstrating N for each stage of the screening process
2.3. Data extraction
A bespoke data extraction table was created to accommodate the range of study designs included in the review and was tailored to the review aims. These data, extracted by two authors (50% each by V. F. and A. C.), included the following components: study aim, design, sample details, health measure, variables controlled for, other data collected, and summary of findings. The third author (J. H.) reviewed all data extraction independently. For quality appraisal of included studies, existing Critical Appraisal Skills Programme (CASP) checklists were used (CASP UK, 2017). The CASP cohort and qualitative study checklists were used in their existing forms, and for intervention and cross‐sectional study designs, an adapted version of the CASP cohort study checklist was used (available upon request from the authors). Two authors (V. F. and A. C.) independently completed a quality appraisal checklist for all included studies so that interrater reliability could be obtained for each criterion. Kappa agreement was moderate for qualitative studies (0.49) and substantial for quantitative studies (0.64). All remaining disagreements were subsequently resolved via discussion with the third author (J. H.). The results of the quality assessment were used to generate methodological discussion within and across studies in the results and discussion (Tables 5, 6, 7, 8).
Table 5.
Quality appraisal summary of five included qualitative studies
| CASP criteria | Met the criteria? (f) | ||
|---|---|---|---|
| Yes | Can't Tell | No | |
| Q1. Was there a clear statement of the aims of the research? | 5 | ||
| Q2. Is a qualitative methodology approach appropriate? | 5 | ||
| Q3. Was the research design appropriate to address the aims of the research? | 1 | 4 | |
| Q4. Was the recruitment strategy appropriate to the aims of the research? | 4 | 1 | |
| Q5. Was the data collected in a way that addressed the research issue? | 2 | 3 | |
| Q6. Has the relationship between researcher and participants been adequately considered? | 1 | 3 | 1 |
| Q7. Have ethical issues been taken into consideration? | 5 | ||
| Q8. Was the data analysis sufficiently rigorous? | 3 | 2 | |
| Q9. Is there a clear statement of findings? | 4 | 1 | |
| Q10. Is the research valuable? | 5 | ||
Note. CASP: Critical Appraisal Skills Programme. Q10. Adapted from free text response “How valuable is the research?”
Table 6.
Quality appraisal summary of two included quantitative cohort studies
| CASP criteria | Met the criteria? (f) | ||
|---|---|---|---|
| Yes | Can't Tell | No | |
| Q1. Did the study address a clearly focused issue? | 2 | ||
| Q2. Was the cohort recruited in an acceptable way? | 2 | ||
| Q3. Was the exposure accurately measured to minimise bias? | 2 | ||
| Q4. Was the outcome accurately measured to minimise bias? | 2 | ||
| Q5a. Have the authors identified all important confounding factors? | 2 | ||
| Q5b. Have they taken account of the confounding factors in the design and/or analysis? | 2 | ||
| Q9. Do you believe the results? | 2 | ||
Note. CASP: Critical Appraisal Skills Programme.
Table 7.
Quality appraisal summary of one included quantitative cross sectional study
| CASP criteria | Met the criteria? (f) | ||
|---|---|---|---|
| Yes | Can't Tell | No | |
| Q1. Did the study address a clearly focused issue? | 1 | ||
| Q2. Was the sample recruited in an acceptable way? | 1 | ||
| Q3. Was the outcome accurately measured to minimise bias? | 1 | ||
| Q4a. Have the authors identified all important confounding factors? | 1 | ||
| Q4b. Have they taken account of the confounding factors in the design and/or analysis? | 1 | ||
| Q7. Do you believe the results? | 1 | ||
Note. CASP: Critical Appraisal Skills Programme.
Table 8.
Quality appraisal summary of three included quantitative intervention studies
| CASP criteria | Met the criteria? (f) | ||
|---|---|---|---|
| Yes | Can't Tell | No | |
| Q1. Did the study address a clearly focused issue? | 2 | 1 | |
| Q2. Was the sample recruited in an acceptable way? | 1.5 | 1.5 | |
| Q3. Was the outcome accurately measured to minimise bias? | 1.5 | 1.5 | |
| Q4a. Have the authors identified all important confounding factors? | 3 | ||
| Q4b. Have they taken account of the confounding factors in the design and/or analysis | 3 | ||
| Q5a. Was the follow up of subjects complete enough? | 0.5 | 2 | 0.5 |
| Q5b. Was the follow up of subjects long enough? | 3 | ||
| Q7. Do you believe the results? | 3 | ||
| Q11. Is the intervention described adequately to enable replication? | 1 | 1 | 1 |
Note. CASP: Critical Appraisal Skills Programme. Ingram et al. (2011) had two outcomes, so 0.5 points was awarded per outcome per criteria
2.4. Analysis
Due to the wide variety of study designs and outcome measures in the quantitative studies in this review, a narrative synthesis was conducted in order to synthesise the findings. Data were synthesised according to hospital or community BFI implementation. For included qualitative studies, a thematic synthesis adopting an inductive thematic analysis approach was used to synthesise findings (Braun & Clarke, 2006; Thomas & Harden, 2008). This process involved data familiarisation by reading and rereading included study results sections; coding of study data to identify patterns relevant to the research questions across studies (direct coding of both the text describing studies' findings and illustrative verbatim or written participant quotes within papers occurred); and finally theme and subtheme structure generation (including organisation of data within an analysis document using Microsoft Word, continual reorganisation of coding into emerging themes, and theme and subtheme title generation). A mixed‐methods synthesis of qualitative and quantitative studies was then conducted using Harden and Thomas's (2005) approach. The qualitative synthesis allowed recommendations to be made based on women's own experiences of BFI‐compliant care. These recommendations were then juxtaposed against the quantitative evidence. Three questions guided this analysis: “What quantitative evidence overlaps with recommendations derived from women's views and experiences?”; “Which recommendations have yet to be addressed by quantitative research?”; and “Do those quantitative studies that overlap with recommendations show larger statistical effects and/or explain heterogeneity?” Matches, mismatches, and gaps were identified. Gaps were used as a basis for recommending what kinds of research need to be developed and tested in the future in the discussion.
3. RESULTS
The search strategy identified 193 studies (Figure 1), of which 11 offered information that addressed the research questions and met full‐text criteria (see Table 9). Those included were published between 2002 and 2015. Six studies were conducted in England, four took place in Scotland, and one covered the whole of the UK. Six used quantitative designs and included intervention studies (n = 3), cohort studies (n = 2), and a cross‐sectional observational study (n = 1). Quantitative sample sizes ranged between 141 and 464,266 (overall sample N = 489,555). Five were qualitative designs and included interview studies (n = 3) and mixed‐focus group/interview studies (n = 2). Qualitative samples sizes were between 15 and 72 (N = 214).
Table 9.
Summary of studies included in the review
| Study ID (reference) | Study aim | Design | Sample (location, size, attrition) | Breastfeeding measure (time points) | Variables controlled for | Other data collected | Summary findings |
|---|---|---|---|---|---|---|---|
| Bartington, Griffiths, Tate, and Dezateux (2006). Are breastfeeding rates higher in Baby Friendly accredited maternity units in the UK? Int J Epi. 35: 1178–1186. | To examine whether mothers are more likely to start and continue to breastfeed if they delivered in a BFHI accredited unit | Cohort study |
Mother–infant pairs in UK including England, Wales, Scotland, Northern Ireland n = 18,819
n = 17,359 included in analysis (28% attrition) |
Breastfeeding initiation defined by two questions: “Did you ever try to breastfeed?” “How old was cohort child when s/he last had breastmilk?”a (1 month after birth) |
Planned pregnancy; antenatal class attendance; accompanied by significant other at delivery. Mode of delivery, admission to special or neonatal care; hospital stay duration. Country of residence, ward type, socio‐economic status, ethnicity, maternal age, education, parity, lone parent status. |
None |
Breastfeeding initiation:
Breastfeeding prevalence (at 1 month):
|
| Broadfoot, Britten, Tappin, and MacKenzie (2005). The Baby Friendly Hospital Initiative and breast feeding rates in Scotland. Arch Dis Child Fetal Neonatal Ed. 90: 114–116. | To examine the effect of the BFHI on breast feeding rates in Scotland. | Cohort study |
Mother–infant pairs in Scotland n = 464,246 n = 445,623 included in analysis (4% attrition) |
Breastfeeding rates recorded on Guthrie Screening card (7 days after birth, records collected 1995–2002) |
Mother's age Size of hospital Deprivation (Carstairs deprivation category) Mother's age |
None | Babies born in a hospital with the UK Baby Friendly Hospital Initiative standard award were 28% (OR = 1.28, 95% CI [1.24, 1.3], P < 0.001) more likely to be exclusively breast fed at 7 days of post‐natal age than those born in other maternity units after adjustment for mother's age, deprivation, hospital size, and year of birth. |
| Geddes (2012). Breastfeeding: How to increase prevalence. Nursing Times. 108: 32/32: 12–14 | To develop BFCI services (Steps 2 and 4) to improve breastfeeding prevalence | Intervention study | All new mothers in one London NHS trust | Trust breastfeeding rates at 6–8 weeks after birth (at start of intervention, 6 weeks and 9 months) | None |
Parent questionnaire; Parent focus group (6 months following intervention start) |
Breastfeeding prevalence at 6–8 weeks after birth:
Intervention was telephone support to mothers at 5–12 days after delivery; Band 4 NHS staff providing “support and advice on infant feeding.”a Questionnaire:
Focus group:
|
| Ingram, Johnson, and Greenwood (2002). Breastfeeding in Bristol: Teaching good positioning and support from fathers and families. Midwifery, 18: 87–101 | To determine whether a specific “hands‐off” breastfeeding technique, based on a BFI step, if taught to mothers in the immediate post‐natal period, improves their chances of breastfeeding successfully, and reduces the incidence of problems | Nonrandomised prospective cohort phased intervention study. | 1,400 South Bristol mothers who were breastfeeding on discharge from hospital. 390 of these mother were scored for efficiency of using the breastfeeding technique. | The “breastfeeding technique” comprises eight guidelines to enable mother's to position and attach their baby at the breast by themselves. Frequencies of exclusive and “any breastfeeding” at 2 and 6 weeks from questionnaires sent to mothers at home, and incidence of breastfeeding problems. | Phase of study in multivariate analysis | Partner encouragement, family encouragement, health professional encouragement, no dummy too much milk, enough support in hospital, no/poor advice | Significant increases were observed in the proportion of mothers exclusively breastfeeding at 2 weeks (P = 0.001) and 6 weeks (P = 0.02) and in “any breastfeeding” rates (P = 0.005) at 2 weeks after the technique intervention. The incidence of mothers feeling that they did “not have enough milk” (perceived milk insufficiency) decreased significantly after the breastfeeding technique had been taught (p = 0.02). Logistic regression analysis produced a model that showed that mothers with high scores for the “hands‐off” technique were significantly more likely to be breastfeeding at 6 weeks compared with those who did not use all the elements of the technique (OR 2.4; CI [1.3, 4.3]). |
| Ingram, Johnson, and Condon (2011). The effects of Baby Friendly Initiative training on breastfeeding rates and the breastfeeding attitudes, knowledge and self‐efficacy of community health‐care staff. Prim Health Care Res Dev, 12: 266–275 | Evaluate the effects of Baby Friendly Initiative (BFI) community training on breastfeeding rates, staff, and mothers in a large Primary Care Trust | Before‐and‐after study | Health visitors and nursery nurses who undertook BFI training in 2008, in England n = 141 (3‐day training) n = 137 evaluated the training; then n = 98 included in questionnaire analyses—30% attrition) |
Breast feeding rates collected by GPs (at 8‐week post‐natal check 2006 to 2009) Breastfeeding Self Efficacy Scale Short Form (Gregory, Penrose, Morrison, Dennis & MacArthur, 2018) via interviews with 101 mothers (2 months prestaff training and 6–9 months posttraining) |
None |
Staff breastfeeding attitudes and knowledge; Self‐efficacy tool (Administered immediately before training, 1 and 6 months posttraining) Semistructured interview with 35 staff (2–3 months after training) |
Breastfeeding rates at 8 weeks increased significantly overtime (P < 0.001): Odds ratios of any breastfeeding: 2006–1.0 2007–1.15 (95% CI [1.06, 1.25]) 2008 (training undertaken)—1.46 (95% CI [1.34, 1.58]) 2009–1.57 (95% CI [1.45, 1.69]) Odds ratios of any breastfeeding: 2006–1.0 2007–1.05 (95% CI [0.96, 1.14]) 2008 (training undertaken)—1.38 (95% CI [1.27, 1.50]) 2009–1.46 (95% CI [1.35, 1.59]) Mother's survey: No significant differences shown (authors suggest due to underpowered study). |
| Tappin, Britten, Broadfoot, and McInnes (2006). The effect of health visitors on breastfeeding in Glasgow. Int Breastf Journ, 1:11 | To document the health visitor role in a Glasgow community BFI setting and the effect it had on BF rates in 2000 | Cross‐sectional observational study | Health‐visitor infant pairs in Glasgow. 4,949 pairs recruited, n = 825 in analyses relevant to BFI community efficacy (full breakdown of attrition at all stages of study provided) | Breastfeeding data collected through the CHSPc first health visitor visit records showed 835/2,145 (38.9%) infants were breastfed at 10 days. These records were used to assess the effect of post‐natal intervention described by health visitors on the survival of breastfeeding to the second CHSP check scheduled at 6 weeks. | Adjustment was made for maternal age, smoking status, employment status, and DEPCAT (SES) | Feeding attitude of HV, HV using commercial company leaflets, BF support group availability to mothers (these did not directly align to the community BFI steps) |
HV training in the last 2 years (aligns with Point 2 of BFI community steps) Infants who were breastfed at the first routine health visitor contact after birth were nearly twice as likely to continue to be breastfeeding at the second routine contact if their health visitor had received training in breastfeeding support in the previous 2 years OR 1.56 (1.11, 2.21), AOR 1.74 (1.13, 2.68), P = 0.001
Post‐natal contact practiced by HV (aligns with Point 4) Weekly visits as a routine were associated with an increase in the proportion who stopped breastfeeding compared with contact initiated by the health visitor at least once during the first 6 weeks OR 0.58 (0.38, 0.89); AOR 0.55 [0.32, 0.94], P = 0.003. After further adjustment for training the association became nonsignificant (P = 0.07) |
| Hinliff‐Smith et al. (2014). Realities, difficulties, and outcomes for mothers choosing to breastfeed: Primigravid mothers experiences in the early postpartum period. Midwifery, 30:14–19 | To develop an understanding of primiparous women's experiences and challenges of breast feeding in the early post‐partum period at two BFI accredited hospitals | Qualitative phenomenology study with daily diaries and interviews |
n = 26 mothers in one of two BFI accredited hospitals in the East Midlands, UK
Daily diaries: n = 22
Interviews: n = 13 (9 completed a diary, 4 had not) |
Reported feeding at hospital discharge and at 6–8 weeks post‐partum | N/A |
Daily written diaries for 6 weeks from birth; Face‐to‐face interviews |
Descriptive statistics: Breast feeding at discharge = 18/26; at 6–8 weeks = 10/26 Artificial milk at discharge = 7/26; at 6–8 weeks = 16/26 Mixed at discharge = 1/26; at 6–8 weeks = 0/26
Emotional rollercoaster of infant feeding Maternal guilt, unpreparedness for breastfeeding, unrealistic expectations Professionals: notions of expertise, communication and impact Perceived power of “experts,” breastfeeding communication and support Dimensions of public feeding Feeding in front of family and relatives, using private facilities in public spaces, feeding “where ever and whenever” |
|
Hoddinott et al. (2012). A serial qualitative interview study of infant feeding experiences: idealism meets realism. BMJ Open. 2:1–14 |
To explore experiences of infant feeding in women and their partner's from pregnancy until 6 months after birth | Qualitative serial interview study |
72 of 541 (13%) pregnant women in Scotland (from two Health Boards implementing BFI) volunteered; 36 women and 37 significant others participated. |
None | N/A | Face‐to‐face and telephone interviews conducted every 4 weeks (total = 220 interviews) | Overarching theme: Clash between feeding idealism and reality experienced.
|
|
Lagan et al. (2014), “The midwives aren't allowed to tell you”: Perceived infant feeding policy restrictions in a formula feeding culture—The Feeding Your Baby Study. Midwifery. 20:49–55 |
To explore expectations and experiences of mothers in relation to infant feeding and identify how care could be improved in a Stage 2 BFI setting. | Qualitative interview and focus group study |
40 interviews and 7 focus groups (n = 38); Women in East Scotland with a range of breastfeeding experiences (breast fed; formula fed; breast then formula fed; concurrent breast and formula fed); 158 invited, 78 participated (49%) |
None | N/A | One‐to‐one semistructured interviews and focus groups with mothers (Thematic Analysis) |
One primary theme “Mixed and Missing Messages” emerged and contained four subthemes:
Women reported receiving contradicting information by staff; those given consistent advice reported more positive experiences; women highlighted the need for meaningful and practical feeding support)
Women who formula fed experienced a lack of support from staff compared with women who breast fed, they perceived a reluctance from staff to provide information about formula feeding causing alienation; women wanted more information shared on formula feeding
Women felt misled about the challenges of breast feeding leading to unrealistic expectations of breast feeding; pitfalls of formula feeding were unexplored; women who did not breast feed felt guilt and self‐blame due to the “breast is best” message
Women who intended to and did breast feed felt positive whereas those who intended to breast feed and did not felt surprised and distressed; type of care by staff dictated whether women felt supported or judged when transitioning from breast to formula |
| Thomson and Dykes (2011). Women's sense of coherence relating to their infant feeding experiences. Mat Child Nutr, 7:160–174 | To explore women's experiences, perceptions, and opinions of infant feeding using Antonovsky's Sense of Coherence theory | Qualitative interview study embedded within an evaluation study of the implementation of BFI Community Award | 15 women (under 12 months PP) recruited by HP engaged in the BFI evaluation in two primary care trusts in North West England | Semistructured interview incorporating questions within the BFI audit tools for bottle feeding and breastfeeding mothers as well as open‐ended questions to uncover attitudes and meanings. | N/A | None |
Where is the choice?—lack of info about FF, dogmatic approach to BF, BF aids encouraged against WHO guidance Targeting the information—a one size fits all approach to information provision The need for consistency—inconsistencies in feeding information and support
Benefits and barriers to peer support—access to peer support helped sustain BF, unconventional BF methods viewed as a barrier to accessing peer support The value of time and accessibility of support—marked lack of time and support by HP on post‐natal ward, much better support at home Manhandling of women's breasts—babies forced to the breast by HP against mothers will Personal support systems—level of emotional and practical support provided by partner, family, and friends. Partner sharing responsibility The birth experience—medicalised, traumatic birth influences BF experience, lack of skin‐to‐skin a barrier in such births
Theoretical versus embodied knowledge—discrepancies between expectation of BF experience and reality of it. Emotionality of infant feeing—a desire to BF for health benefits and bonding. Positive emotions such as love and determination among women who successfully BF, negative emotions such as guilt and remorse among women who did not. Encouraging and not dissuading—some women found encouragement of the value and benefits of BF essential, others felt pressure when receiving them. Media messages and public BF—negative media images and info about BF and personal difficulties BF in front of other people |
| Thomson, Ebisch‐Burton, and Flacking (2015). Shame if you do—shame if you don't women's experiences of infant feeding. Mat Child Nutr, 11: 33–46 | To explore mother's experiences, opinions, and perceptions of infant feeding within two PCTs implementing BFI community award using Lazare's categories of shame | Qualitative interview and focus group study (framework analysis) | Sixty‐three women took part in seven focus groups (n = 33) and 28 individual interviews (two interviews involved two participants). Recruited from two north‐west England PCTs | Semistructured interview guide designed to elicit women's current infant feeding status, intentions and motivations regarding infant feeding and barriers and facilitators to support | N/A | None |
Infant feeding as a shame inducing event Women experienced a sense of feeling out of control and dependent on others through insufficient information and lacking or inappropriate infant feeding support. When infant feeding methods were not as intended, this could lead to feelings of incompetence, inadequacy, and inferiority. Medicalisation of infant feeding creates experiences that render the method a “disease.” Feeding choices internalised as either failure (in those that cannot) and morally or socially unacceptable (for those who do). Infant feeding implicitly associated with “good” mothers and babies Vulnerability of the mother Mothers (particularly primiparous) often felt overwhelmed by new motherhood, exacerbated by difficult births. Unaware of what support was needed until faced with reality of motherhood. Many women felt expected or pressured to BF, which was viewed as an additional burden. Exposure of women's bodies and infant feeding methods Accounts of manhandling and objectification of breasts indicted intense distress and humiliation. In BF women, real or perceived negative reactions to public BF from others led to withdrawal. Judgement was also identified among non‐BF women, often from HP. Those FF were felt to be deviants and felt fear around informing HP of their feeding method. Perceived conspiracy of silence among HP through them not discussing or offering support for formula milk. Undermining and inadequate support Shame experienced by BF and non‐BF mothers when undermining or inadequate support received. Support needs not met for those BF. Marginalisation through a lack of support for FF women. Restrictions on FF info and advice left women dejected and isolated. Perceptions of inadequate mothering Non‐BF mothers felt that pro‐BF discourse and negative verbal responses from others made them feel second best and a bad mother who was denying and depriving their child. Reactions from HP in non‐BF women led to inadequacy and defectiveness. Non‐BF women experienced guilt and shame and subsequent morbidity in the infant for BF cessation. BF women described themselves as mean or selfish for not allowing others to help. |
Note. BFHI: Baby Friendly Hospital Initiative; BF: breastfeeding; FF: formula feeding; HP: health professional; CHSP: Child Health Surveillance Programme.
The second here question had the optional response of “never took breastmilk” and a selection of age categories.
Accredited hospitals [full BFI accreditation], Certified hospitals [commitment to BFI]; Neither award [not participating in BFI].
Child Health Surveillance Programme.
3.1. Narrative synthesis of quantitative studies (n = 6)
All studies included reported the impact of UK‐BFI implementation on breastfeeding outcomes. No data were available for other maternal and infant health outcomes. Some studies reported multiple breastfeeding outcomes yielding 13 different analyses. Multivariate analyses were given reporting precedence over bivariate techniques. In studies that did not use multivariate analyses, bivariate analyses were reported instead. Where bivariate analyses were not available, raw percentages were reported.
3.1.1. The impact of BFHI implementation on breastfeeding outcomes
Study quality
Three studies (two cohort and one intervention) yielding nine analyses examined the impact of BFHI implementation on breastfeeding outcomes (Bartington et al., 2006; Broadfoot et al., 2005; Ingram et al., 2002). The cohort studies had high recruitment rates and addressed a range of potential confounders (Bartington et al., 2006; Broadfoot et al., 2005). Key quality issues affecting these studies were potential recall bias (Bartington et al., 2006), lack of adjustment for covariates (Ingram et al., 2002), and unclear measurement of breastfeeding outcomes (Broadfoot et al., 2005).
Studies' description and findings
Two cohort studies found a positive impact of full accreditation on very early breastfeeding outcomes (Bartington et al., 2006; Broadfoot et al., 2005). Bartington et al. (2006) examined 18,819 UK mother–infant pairs and found that mothers who delivered in a fully accredited hospital were 10% more likely to initiate breastfeeding than those who delivered in a unit not participating in BFI (adjusted risk ratio [ARR]: 1.10; 95% CI [1.05, 1.15]). However, breastfeeding initiation was not significantly different when compared with units with a certificate of commitment. Furthermore, when examining any breastfeeding at 1 month, there was no impact of accreditation or certification when compared with units with neither award. Broadfoot et al. (2005) recruited 464,246 mother–infant pairs in Scotland between 1995 and 2002 and found that babies born in a hospital with the UK‐standard award were 28% more likely to be exclusively breastfed at 7 days of post‐natal age than those born in units not participating in BFHI (adjusted odds ratio [AOR]: 1.28; 95% CI [1.24, 1.31]). Furthermore, those delivering in a unit with a certificate of commitment were 4% more likely to be exclusively breastfeeding at 7 days than those delivering in units not participating (odds ratio [OR]: 1.04; 95% CI [1.02, 1.06]).
One English intervention study also found positive effects of BFHI implementation on later breastfeeding outcomes. Ingram et al. (2002) determined whether a specific “hands‐off” breastfeeding technique, based on Step 5 of BFHI improved mother's chances of breastfeeding successfully and reduced the incidence of breastfeeding problems. The intervention comprised eight guidelines to enable mothers to position and attach their baby at the breast by themselves. Significant bivariate increases were observed in the proportion of mothers exclusively breastfeeding at 2 weeks (P = 0.001) and 6 weeks (P = 0.02) and in any breastfeeding rates (P = 0.005) at 2 weeks after the technique intervention. Any breastfeeding at 6 weeks was not significantly different compared with preintervention. The incidence of perceived milk insufficiency also decreased significantly after the breastfeeding technique had been taught (P = 0.02). Finally, logistic regression analysis demonstrated that women with high compliance to the technique (seven or eight steps or more) were significantly more likely to be breastfeeding at 6 weeks compared with those with low compliance (OR 2.37; CI [1.30, 4.31]).
Summary
Based on two studies, there is some evidence for the impact of full BFHI accreditation on very early breastfeeding rates (birth to 7 days) but this is not sustained at 1 month. There is also weak statistical evidence for the implementation of Step 5 of the BFHI on breastfeeding outcomes at 2 and 6 weeks based on one study.
3.1.2. The impact of BFCI implementation on breastfeeding outcomes
Study quality
Three studies (two interventions and one cross‐sectional observational) yielding four analyses examined the impact of BFCI implementation on breastfeeding outcomes (Geddes, 2012; Ingram et al., 2011; Tappin et al., 2006). Two studies had low statistical quality, failing to adjust for a range of confounders (Ingram et al., 2011) or providing no inferential statistics (Geddes, 2012). Tappin et al. (2006) also lacked sampling representativeness and provided incomplete information on breastfeeding data.
Studies' description and findings
All three studies reported a positive effect of BFCI implementation on any breastfeeding outcomes at 6–8 weeks (Geddes, 2012; Ingram et al., 2011). An intervention study in a London primary care trust (PCT) aimed to develop services and improve breastfeeding outcomes by offering in‐house BFI breastfeeding management training to staff followed by telephone support to mothers at 5–12 days after delivery in line with Steps 2 and 4 of BFCI (Geddes, 2012). Any breastfeeding prevalence at 6–8 weeks after birth rose from 60.5% at baseline to 61.6% 6 weeks postintervention. Additional increases in any breastfeeding prevalence at 6–8 weeks were also noted 9 months after the intervention started (from 61.6% to 67.5%).
Ingram et al. (2011) evaluated the effects of BFCI training (Step 2) between 2006 and 2009 on breastfeeding rates at 8 weeks and breastfeeding self‐efficacy at 6–9 months. One hundred forty‐one health visitors in a large PCT in Bristol undertook the training and breastfeeding data (any and exclusive) were routinely collected by General Practitioners (GPs) to allow annual comparisons. Bivariate regression analyses demonstrated that any breastfeeding rose steadily from 2006 (pretraining) with significant increases in 2007 (OR: 1.15; 95% CI [1.06, 1.25]), 2008 (OR: 1.46; 95% CI [1.34, 1.58]), and 2009 (OR: 1.57; 95% CI [1.4, 1.69]). Exclusive breastfeeding rates did not improve from 2006 to 2007 (OR: 1.05; 95% CI [0.96, 1.14]) but significantly increased in 2008 (OR: 1.38; 95% CI [1.27, 1.50]) and 2009 (OR: 1.46; 95% CI [1.35, 1.59]). Maternal breastfeeding self‐efficacy scores were not significantly different before (n = 42) and after (n = 59) staff training, although the authors suggest that this was due to a lack of power.
Finally, a Scottish cross‐sectional observational study of 4,949 health visitor–infant pairs examined the health visitor role in a Glasgow BFCI setting and the effect it had on breastfeeding rates in 2000 (Tappin et al., 2006). Child Health Surveillance Programme first health visitor visit records showed 835/2,145 (38.9%) infants were breastfed at 10 days. These records were used to assess the effect of post‐natal intervention described by health visitors on the survival of breastfeeding to the second Child Health Surveillance check scheduled at 6 weeks. Infants who were breastfed at the first routine health visitor contact after birth were nearly twice as likely to continue to be breastfeeding at the second routine contact if their health visitor had received training (BFCI Step 2) in breastfeeding support in the previous 2 years (AOR: 1.74; 95% CI [1.13, 2.68]). Weekly visits as a routine (BFCI Step 4) were also associated with a decrease in the proportion who stopped breastfeeding compared with contact initiated by the health visitor at least once during the first 6 weeks (AOR: 0.55; 95% CI [0.32, 0.94]). However, after further adjustment for training, the association became nonsignificant.
Summary
Based on all three studies, there is some evidence that implementation of Step 2 (staff training) and Step 4 (supporting mothers to initiate and maintain breastfeeding) of community BFCI guidance improves breastfeeding rates at 6–8 weeks.
3.2. Meta‐synthesis of qualitative studies (n = 5)
Three themes emerged from the meta‐synthesis of qualitative studies included in the review, which explored the experiences and views of women receiving BFI‐compliant care: (a) influential support from professionals, (b) unrealistic expectations causing unmet needs, and (c) emotional impact of care. These themes accounted for how women experienced infant feeding care and their views and beliefs around this. Each theme is presented below alongside illustrative quotes from included studies labelled to indicate the study and type of data presented (i.e., text or verbatim quote). Where verbatim quotes are used, the nonidentifying label used within the study it is derived from is used (e.g., unique ID number or pseudonym). Figure 1 provides a diagrammatic overview of the thematic structure.
3.2.1. Study quality
All studies had clearly defined aims and appropriate sampling methods and provided thick description of experiences, which is indicative of transferability (Hoddinott, Craig, Britten, & McInnes, 2012; Hinsliff‐Smith, Spencer, & Walsh, 2014; Lagan, Symon, Dalzell, & Whitford, 2014; Thomson & Dykes, 2011; Thomson et al., 2015). However, in some studies, the data analysis lacked information about procedures to ensure rigour (Thomson & Dykes, 2011; Thomson et al., 2015) and did not specify the relationship between the researcher and the participant (Hinsliff‐Smith et al., 2014; Thomson & Dykes, 2012; Thomson et al., 2015), which limits the credibility of findings.
3.3. Influential support from professionals
The type of care provided to women significantly affected their thoughts, emotions, and behaviours regarding feeding experiences. Whether it was the actions of health professionals, the information they provided, or their communication style, these factors played a role in how negative or positive women's subsequent perceptions of her feeding experiences were.
The nature and type of communication with health professionals was paramount to how they [the mothers] viewed their breast feeding abilities. (Hinsliff‐Smith_text)
3.3.1. Positive experiences of support
Women described some positive experiences regarding the support provided to them by health professionals. These experiences occurred when professionals provided care that reassured women, was family‐centred rather than fixed around feeding guidelines, and was practical in nature and consistent.
Women who experienced carers with good communication skills, consistent approaches to care and provision of practical support, reported that their overall experience was positive and supportive. (Lagan_text)
3.3.2. Negative experiences of support
Negative experiences were commonly reported and were believed to influence women's feeding self‐efficacy. Poor communication including judgemental language and criticism of feeding attempts accounted for some women's negative experiences; these exchanges often left women feeling reprimanded and inadequate.
One mother, who had been hand expressing and feeding this expressed breast milk to her infant from a bottle due to painful nipples, wrote in her diary after her first home visit from her health visitor: My health visitor told me off. She said I was confusing him [baby](P36diary) …. What these examples demonstrate is the potential to undermine and discourage mothers. New mothers appear particularly vulnerable to negative feedback. (Hinsliff‐Smith_text and quote)
The provision of inconsistent information was also a key factor leading women to feel unsupported. Women received conflicting advice regarding guidelines around breastfeeding duration, introduction of solid foods, or advice about use of bottles. Regardless of feeding method, women found that inconsistent advice left them feeling confused and demoralised. Unsupportive care often affected women and stayed with them creating distinctive memories that troubled them after these experiences had occurred. Both the poor communication and inconsistent advice received were attributed to the nature of care settings in some cases with rushed health professionals and continually changing care teams. This created a sense that women's feeding support needs were a burden to health professionals who were unable to provide the support they needed.
Families describe some healthcare professionals as lacking good communication skills and breastfeeding expertise and, above all, staff were seen to be “rushed off their feet,” leading women to feel “really bad” about asking for help, and feeling a “burden rather than a priority.” (Hoddinott _text)
3.3.3. Rigid and impersonal support
The delivery of feeding information also contributed to how supported women felt. Women highlighted that feeding information presented to them was often patronising or overly “rules‐based.” Women particularly disliked feeding education being so technical because it focused on feeding as a rigid and unnatural process, which challenged breastfeeding confidence.
Feeding education perceived as unrealistic, overly technical and rules based which undermines women's confidence. (Hoddinott_text)
Feeding information was often presented to women in an impersonal manner, described as a checklist, rather than tailored to families' needs. Women disliked this generic approach, wondered if this was again due to the busyness of care settings, and emphasised the desire for more individualised, personal care than they had received.
A number of the participants described a “one size fits all” approach to information provision rather than amended or adapted to their individual needs, and this related to time shortages. (Thomson & Dykes_text)
Women were clear that they would have preferred feeding information that was tailored and individualised to them, their family circumstances, and their specific needs.
As they [mothers] considered that “no two babies are the same,” a flexible, open and embodied approach was considered to be far more effective rather than a rigid “must do” approach. (Thomson & Dykes_text)
3.3.4. Practical advice needed post‐natally
Breastfeeding support directly after birth was also an area of unmet need. Women emphasised that they would have found it beneficial to receive practical feeding support in the early post‐natal period, for example, regarding positioning and the practicalities of breastfeeding. However, in one study, women highlighted that when they attempted to access this type of support on hospital wards, their support requests were unanswered.
A number of the mothers made reference to buzzing for assistance—but nobody came: X (health professional) said when she wakes up, buzz me, I buzzed for two hours and nobody came…. This presented a paradox in that, while women were being encouraged to stay in hospital to establish breastfeeding, they were not being provided with, or felt unable to access the necessary support for this to be achieved. (Thomson & Dykes_text and quote_Lorraine)
3.4. Unrealistic expectations causing unmet needs
The support provided to women by health professionals was directly reported to set up a large gap between women's expectations of breastfeeding and the reality of their experiences. This in turn identified a number of unmet needs. In general, women expected breastfeeding to be less challenging than their post‐natal experiences, and this therefore resulted in them being unprepared for breastfeeding difficulties, the cessation of breastfeeding, or the introduction of formula.
Although some women are happy with the breast feeding help available on postnatal wards, for most there is a large gap between antenatal ideals or expectations and the reality. (Hoddinott et al., text)
3.4.1. Breastfeeding as panacea
Unrealistic feeding expectations related strongly to breastfeeding being depicted as a panacea by women. In part, the manner in which feeding information had been delivered to women was seen as responsible. Feeding education classes solely focused on breastfeeding rather than incorporating alternative feeding methods were described as strict and even dogmatic in approach. This was combined with the presentation of breastfeeding in an exclusively positive manner (e.g., easy, natural, painless, and enjoyable). Women were also offered an abundance of breastfeeding support following discharge from hospital. In combination, this set women up to believe that breastfeeding was the only feeding option that would meet their needs. However, women reported real‐world experiences of breastfeeding being much more negative and encountering challenges that were unanticipated and surprising to them, including breastfeeding being exhausting, painful, demanding, and restrictive.
A number of the women had anticipated breastfeeding to be a pain‐free, straightforward and natural experience. However, the reality of breastfeeding was “tying,” “difficult,” “painful” and required women and babies to “learn together.” (Thomson & Dykes_text)
3.4.2. Unaddressed breastfeeding challenges
Unrealistic expectations often meant women were underprepared for managing common breastfeeding challenges. Particular difficulties were around cluster feeding, misperceptions about milk production, expressing practices, feeding in public, restrictions on daily functioning, tiredness, pain, and discomfort. For some women, this led them to believe that switching to formula was the only viable solution. In hindsight, women and their partners felt they would have been more able to deal with such challenges if feeding education had acknowledged these problems before they were occurring in practice.
If you had mums with babies coming along [to classes before birth] I'd be interested to see where difficulties lay so that I could be there to support and say, “well that's kind of normal” and “d'you remember that woman had that particular issue for a couple of months but then it kind of came good in the end?,” kind of thing. (Hoddinott et al., quote_ID 205—partner)
3.4.3. Withholding formula feeding information
In stark, contrast to the presentation of breastfeeding support, women felt that health professionals were withholding information about formula feeding. The withholding of information about alternative feeding methods led to a secretive culture around nonbreastfeeding practices. For example, health professionals were reported to share some formula feeding information covertly with women, and women themselves reported hiding bottles from health professionals for fear of stigmatisation. The pro breastfeeding discourse was therefore seen as unhelpful, leading women to feel anxious and uninformed by health professionals when it came to appropriate formula feeding information.
The perceived undesirable nature of their actions [not breastfeeding] was also reinforced by what women considered to be a “conspiracy” of silence among health professionals through them not discussing or offering support for bottle‐feeding. (Thomson_text)
3.4.4. Sense of cluelessness about formula feeding
Women also reported a total lack of understanding and preparedness about formula feeding. They were left unaware of the practicalities of how to formula feed and reported feeling clueless about feeding preparation, feeding amounts, and understanding feeding cues. This cluelessness led women to feel isolated and feeling like health professionals had turned their backs on them.
Some of the women who formula fed from the early post‐natal period or after a period of breastfeeding also reported marginalisation through a lack of support:
When you bottle‐feed you don't get as much help. I did try so hard [to breastfeed] I kept blaming myself that I couldn't do it. […] it was too painful and however much I tried I couldn't get him on, and wasn't feeding properly. […] But when you decide “I don't want to do it anymore,” it seems the support goes out the window. […] It did get me very down, it felt like they turned against me because I was bottle‐feeding. (Thomson_text and quote_Focus group 4)
3.5. Emotional impact of feeding care
3.5.1. Guilt
The studies in this review clearly indicated that the pro breastfeeding discourse in BFI settings perpetuated feelings of guilt in women who struggled to breast feed. They reported that this reinforced perceptions of failure in themselves and a sense of self‐blame and inadequacy as a parent. Specific elements of the discourse that enhanced maternal guilt included the overemphasis on breastfeeding being natural and easy, expectations that all mothers are capable of breastfeeding, framing breastfeeding as the “best” feeding method, anxiety about missing out on the health benefits of breastfeeding, and positioning nonbreastfeeding women as deviant or bad parents.
I felt so guilty and bad about giving up, but I just couldn't stand the pain. When I was in hospital I had to go and get my own bottles and make them up. I […] felt really frowned upon, and made to feel really bad. I was really frightened of saying “I don't want to.” I was in fear of telling the midwife. (Thomson_quote_Kryshia)
Internal feelings also perpetuated this guilt including women's personal desire to breastfeed, the loss of closeness with their child, and observing other mothers successfully breastfeeding. Together, these guilt‐inducing factors led women to feel shame and to come to believe they were inferior and inadequate parents. This not only led to negative perceptions of themselves, but one study identified that this impacted on women's overall well‐being and mental health.
Many non‐breastfeeding women made self‐depreciating reflections on their characteristics and capabilities and blamed themselves for the negative health and emotional implications of their infant feeding method … I ended up suffering from quite severe postnatal depression, I have always wondered whether that was something to do with it, if I could have breastfed would it have happened. (Thomson_text and quote_Jill)
3.5.2. Pressure
Women described breastfeeding promotion as militant, which came across as pressurising rather than encouraging. Women wanted breastfeeding support to be more balanced and sensitive in approach. They disliked the tone being used to promote breastfeeding because it made them feel unequipped and unable to cope with this demand. The emotional impact of this was often negative.
Some women felt harassed and pressurised to breast feed by health professionals. The dissatisfaction with the “breast is best” message was evident. (Lagan_text)
As well as verbal pressure, physical pressure was noted by women via health professionals manhandling their breasts. Women often experienced these episodes as highly distressing. Women reported feeling embarrassed, upset, and uncomfortable with this. It also served to reduce women's confidence in breastfeeding rather than bolster it.
The one [midwife] who came pulled my gown down, plonked her on, didn't tell me what she was doing or anything, kept rubbing her head dead hard into my boob, made her latch on and then walked off. So I was like thank you, next time I will really know what to do, won't I. (Thomson_text and quote_Gail)
3.5.3. Positivity
In line with the advocation of breastfeeding, women reported positive emotions when they were able to breastfeed successfully. Women felt satisfied and happy when they were able to breastfeed, especially if they had intended to breastfeed before the birth of their child. Women also reported feeling positive about being able to overcome challenges of breastfeeding.
Women who had always intended to breast feed and managed to do so enjoyed their experience: I enjoyed the feeling of closeness once I'd got over the pain. (Lagan text and quote_EF)
Overcoming such challenges and successfully breastfeeding accounted for women therefore feeling a sense of achievement, and women reported that mastering this process demonstrated their determination and a sense of control over the early post‐natal period (Figure 2).
Figure 2.
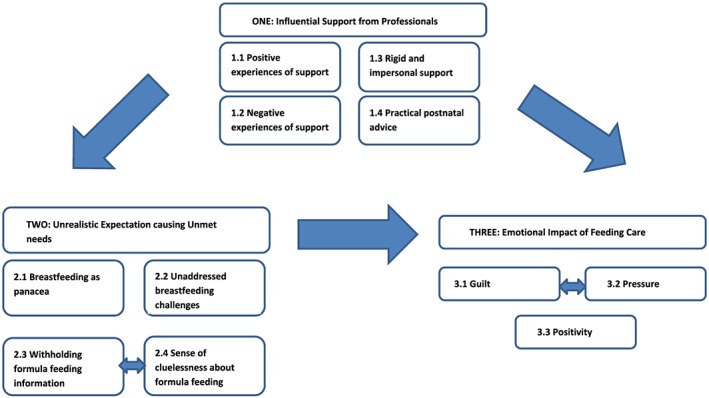
Thematic structure diagram demonstrating themes, subthemes, and interrelationships between themes
3.6. Mixed‐methods synthesis of all studies (n = 11)
The thematic synthesis provided three recommendations to be made based on women's own experiences of BFI‐compliant care. Quantitative evidence that supports or refutes each recommendation is provided.
-
1
Support provided in BFI settings should be regular in quantity, consistent in quality, personal, practical, and non‐judgemental
Overlapping supporting evidence was identified in Ingram et al. (2002), which used a practical “hands‐off” breastfeeding technique in a BFHI setting and found that women with high compliance were significantly more likely to be breastfeeding at 6 weeks. Perceptions of receiving “enough breastfeeding support” from hospital staff (rather than just help or advice) were also a factor in increasing breastfeeding continuation in this study. BFCI evidence also demonstrated that personal telephone support (Geddes, 2012) and an increase in regularity of visits (Ingram et al., 2011) as a routine were also associated with longer breastfeeding continuation. No comparisons of statistical effects were possible, and no refuting evidence was identified.
-
2
BFI‐compliant care should provide realistic expectations of breastfeeding and its associated challenges in pregnancy and the post‐partum and provide appropriate, timely information and support on formula feeding
No quantitative evidence examined expectations of breastfeeding in pregnancy or the post‐partum, and none measured formula feeding information and support provision. Breastfeeding self‐efficacy was examined by Ingram et al. (2011), which could be considered as a proxy for management of breastfeeding challenges. No significant differences were found when pre‐to‐post scores were compared, which refutes the recommendation; however, the authors suggest this was due to sampling issues.
-
3
Emotions associated with breastfeeding difficulties or cessation (i.e., guilt, shame, pressure) should be considered an important component of infant feeding support and not perpetuated by the promotion or support of breastfeeding
No quantitative evidence examined emotions associated with breastfeeding or the impact of the intervention on emotional outcomes.
4. DISCUSSION
4.1. Discussion of quantitative findings
The primary objective of this review was to examine the impact of BFI implementation on maternal and infant physical and mental health outcomes in the UK. Comparable with the US, there is currently no UK data available relating to wider physical maternal or infant health outcomes. Evidence from high‐quality randomised controlled trial (RCT) in middle‐income countries find that implementation of BFHI leads to multiple health benefits among infants and school‐aged children, including gastrointestinal infections, atopic eczema, IQ, and academic performance (Pérez‐Escamilla et al., 2016). Replication of these findings in the UK and US is necessary to establish generalisability in these settings. BFI was ultimately designed with the aim of supporting breastfeeding to enable better health outcomes for mothers and infants. There are differences in the magnitude of health benefits of breastfeeding according to country income (Victora et al., 2016); therefore, it is essential to have country‐specific evidence to understand whether its objectives are being met globally.
Six quantitative studies provided findings for breastfeeding outcomes (three hospital; three community). Both studies examining full BFHI accreditation indicate that full accreditation is associated with very short term (i.e., initiation and at 1 week), positive effects on breastfeeding (Bartington et al., 2006; Broadfoot et al., 2005). This resonates with global literature that finds BFHI is associated with positive short‐term outcomes (Pérez‐Escamilla et al., 2016) and although not directly attributable is consistent with a sharp increase in UK breastfeeding initiation rates since BFHI was introduced (Mcandrew et al., 2012). However, an increase in breastfeeding initiation in the hospital is a criterion for BFHI accreditation. Concluding that the intervention increases breastfeeding initiation implies that the intervention itself is also a measured outcome, which is circular logic (Howe‐Heyman & Lutenbacher, 2016). It is more important to consider the influence of BFHI on breastfeeding duration as this has the greatest influence on health outcomes.
In the only study available with a longer follow‐up period, these effects were not sustained for breastfeeding duration at 1 month, which conflicts with global evidence (Bartington et al., 2006). Similar findings were observed by Pérez‐Escamilla et al. (2016) in his synthesis of 13 U.S. studies, which in combination suggests that BFHI implementation in its current form may not influence longer term breastfeeding outcomes in high‐income settings like the US and UK. Barriers and determinants of breastfeeding behaviour differ according to income setting (Skouteris et al., 2017), which indicates a clear need for tailored breastfeeding promotion and support. Furthermore, breastfeeding rates differ significantly by country income, which signals the need to tailor breastfeeding support strategies to specific patterns recorded in each country (Victora et al., 2016). In high‐income settings, short breastfeeding durations pose a particular challenge (Victora et al., 2016), which indicate further need for BFHI to focus on strategies that support the long‐term sustainability of breastfeeding. Despite evidence from one other study for a specific step of BFHI on later positive breastfeeding outcomes (Ingram et al., 2002), there was no evidence available at all for accreditation status (i.e., adherence to all 10 steps) on later breastfeeding outcomes (i.e., >1 month). Given that the initiative is underpinned by the WHO/UNICEF recommendation of exclusive breastfeeding to 6 months, this is a concerning omission from the literature and indicates an urgent need for future research examining the impact of BFHI on later breastfeeding outcomes.
There were no studies examining the impact of full BFCI implementation (i.e., all 7 points) on breastfeeding outcomes. However, all three studies included in this review reported a positive effect of partial BFCI implementation (Step 2 staff training; Step 4 support initiation and maintenance of breastfeeding) on any breastfeeding outcomes at 6–8 weeks (Geddes, 2012; Ingram et al., 2011; Tappin et al., 2006). There is supporting global evidence that mandatory staff BFI training improves health professional's knowledge and attitudes of breastfeeding (Dagvadorj, Yourkavitch, & Lopes, 2017). Standards for achieving Step 4 include a full breastfeeding assessment alongside practical support about positioning, attachment, hand expressing, and continuation of breastfeeding when returning to work (UNICEF, 2017). There are particularly high rates of breastfeeding cessation between birth and 6 weeks in the UK (Mcandrew et al., 2012), and the current findings indicate that appropriate training and pragmatic community support may be helpful in minimising this risk. Perez‐Escamilla et al. (2016) also found that community support (BFHI Step 10) was crucial for the long‐term sustainability of breastfeeding. The evidence for individual steps of BFCI in resource‐rich settings is very limited but promising, and further research is essential to establish whether full community accreditation influences longer term breastfeeding outcomes in the UK.
4.2. Discussion of qualitative findings
Five qualitative studies examined the experiences of women experiencing BFI‐compliant care. The thematic synthesis identified that support was highly influential in mother's experiences and some positive experiences of support received in a BFI setting were identified, particularly for those who breastfed. However, this was very dependent on the nature of health communications and settings, and often, support was described as negative, with inconsistent advice, prescriptive information, and limited practical support in the hospital. Breastfeeding support services have previously been described as “along a continuum from authentic presence at one end, perceived as effective support, to disconnected encounters at the other, perceived as ineffective or even discouraging and counterproductive” (Schmied et al., 2011, p. 49). This resonates with the review findings and suggest inconsistencies in provision of care. The way in which BFI is interpreted and delivered by health professionals appears to be instrumental to how women experience BFI‐compliant care. Studies in the US and Australia have found that some health professionals view the steps as an imposition of women's choice, which supports the perceptions of prescriptive information noted by mothers in the current review (Schmied et al., 2014). Resistance and noncompliance from health professionals has also been identified in other work, which may affect consistency of BFI provision and experiences of care (Reddin, Pincombe, & Darbyshire, 2007; Schmied et al., 2014).
The findings also suggest that BFI settings may not achieve aspects of care that are important to women with unbalanced feeding education, unaddressed breastfeeding challenges, and insufficient formula feeding information creating a mismatch between the expectation and reality of infant feeding for women. The Royal College of Midwives (RCM) recommend that women should be at the centre of their own care with midwives providing balanced feeding information and promoting informed choice (RCM, 2018). Maternal perceptions of feeding education in a UK‐BFI setting conflict with this recommendation. They further this by stating that women who formula feed their infants need accessible evidence‐based information to enable them to do so safely, which is not reflected in the current findings. BFI recognises the importance of providing appropriate formula feeding information and advice in their guidance (UNICEF, 2010, 2018b), but the current review suggests that this is lacking at a grass‐roots level in UK settings. Acknowledgement within the 10 steps of how safe, responsive formula feeding can be achieved while maintaining compliance with the International Code of Marketing of Breast‐milk Substitutes may be a starting point.
Finally, the emotional impact of the feeding care received by women was identified. Although women who successfully managed to breastfeed reported positive emotions, those that did not commonly experienced feelings of guilt, which often arose as a result of the pro‐breastfeeding discourse. Verbal and physical pressure around breastfeeding was also experienced by both breastfeeding and non‐breastfeeding women. This supports other work that did not meet the inclusion criteria for this review and reinforces conclusions that the current approach to BFI needs to be situationally modified in resource‐rich settings (Fallon, Komninou, Bennett, Halford, & Harrold, 2017; Komninou, Fallon, Halford, & Harrold, 2017; Lee, 2007). Mothers in developing countries regularly experience poor sanitation and a lack of water, which means breastfeeding is vital to infant survival. Mothers in resource‐rich settings face different challenges such as meeting societal expectations, while managing multiple external demands, which may include breastfeeding. Although UK culture undoubtedly needs to change to remove structural barriers to breastfeeding, this is outside of maternal control (Brown, 2017). BFI needs to consider the specific needs of the UK population currently experiencing care underneath their initiative and adapt their steps and training in accordance with the cultural context. Maternal well‐being is important in the healthy development of early attachment relationships (Higgins, St, Roberts, Glover, & Taylor, 2013) and responsive parenting (Mertesacker, Bade, Haverkock, & Pauli‐Pott, 2004), and the available evidence is not conducive to BFI's aim of supporting a close mother–infant bond (UNICEF, 2018b).
4.3. Discussion of mixed methods synthesis
Although limited by a lack of complementary literature, the mixed‐methods synthesis allowed us to examine the extent to which the views of women had been addressed by the quantitative studies and offer ideas for future research based on the gaps identified. The only recommendation generated by thematic synthesis, which was supported quantitatively, was that infant feeding support provided in BFI‐accredited (hospital and community) settings should be regular in quantity, consistent in quality, personal, and practical. This was deemed important for both positive experiences of care and longer breastfeeding durations. The need for maternity units to be appropriately staffed has been highlighted as key in enabling appropriate and regular infant feeding support but lacking sufficient investment and difficult to combat (Royal College of Midwives, 2018). Government support is critical in enabling the design and implementation of breastfeeding intervention tailored to the needs of UK families. Policies are intended to be guidelines rather than tramlines, and it has been suggested both here and previously (Hoddinott et al., 2012; Lakshman, Ogilvie, & Ong, 2009) that a more flexible, individualised approach to the steps may be beneficial to both breastfeeding outcomes and maternal well‐being.
Based on the gaps identified by the other recommendations, some targeted suggestions for future research can be made. Prenatal interventions that emphasise the practical challenges of breastfeeding, rather than the promotion of health benefits, may minimise the expectation versus reality gap. Evaluation of how formula feeding guidance is interpreted and delivered by health professionals is also needed to understand how formula feeding women can be better supported. Studies examining implementation of BFI (hospital and community) should include outcome measures of maternal emotional well‐being to better understand the effects of the intervention on physical and mental health. Studies that include a qualitative component would be an excellent method of exploring the effect of BFI implementation on breastfeeding outcomes and experiences of care simultaneously. Finally, examining the effects of individual steps in these studies may isolate specific components of the model of care, which need adapting in UK settings.
4.4. Limitations
The quality of the research included in the review limits the ability to provide firm conclusions. None of the quantitative studies adjusted for a fully comprehensive range of confounders. In particular, control was lacking for breastfeeding intention and additional breastfeeding interventions that may have been running in parallel at the study sites, both of which likely influence breastfeeding behaviour (DiGirolamo, Thompson, Martorell, Fein, & Grummer‐Strawn, 2005; Linares, Rayens, Gomez, Gokun, & Dignan, 2014; Skouteris et al., 2017). In addition, only one before and after study described the BFI‐based intervention adequately enough to enable replication (Ingram et al., 2002). As noted by Perez‐Escamilla (2016), in his review of U.S. studies, RCTs and/or quasi‐experimental with a baseline equivalent parallel reference group need to be implemented in these settings to gain greater understanding of the impact of full BFI accreditation on breastfeeding and child health outcomes. Some of the qualitative research lacked information about procedures to ensure rigour in the data analysis (Thomson et al., 2015; Thomson & Dykes, 2011). In addition, one of the studies was published before 2012 (Thomson & Dykes, 2011). BFI has since been revised to include guidance on responsive formula feeding so the data may not reflect the experiences of women receiving care under current BFI standards.
In terms of review limitations, there is likely to be more published studies exploring women's experiences of care conducted in BFI settings but without specifying this detail in the manuscript. However, removing terms relating to BFI would have severely affected the sensitivity of the search strategy. Future infant feeding research conducted in UK hospital or community settings should specify whether this takes place at a BFI accredited site and at which stage of accreditation this is in order to expand the evidence base more rapidly. It is also unclear whether the qualitative findings are purely specific to BFI practices or UK maternity care in general as there was no evidence directly comparing BFI versus non‐BFI care. Finally, the Kappa agreement was only moderate for qualitative studies, which may indicate limitations with the CASP qualitative appraisal tool applied to the studies.
5. CONCLUSIONS
There is insufficient evidence to draw firm conclusions about the impact of BFI implementation on maternal and infant health outcomes in the UK. Available quantitative evidence indicates that BFHI implementation has a very short‐term positive impact on breastfeeding outcomes but this is not sustained. Individual steps of BFCI provide some evidence for the positive impact of staff training and pragmatic breastfeeding support on breastfeeding up to 8 weeks post‐partum, but no evaluation of the full programme has been published in the UK. Qualitative evidence finds that support from health professionals is highly influential, but current BFI provision may promote unrealistic expectations of breastfeeding, not meet women's individual needs, and foster negative emotional experiences. The mixed‐methods synthesis highlights the importance of regular, practical, and personal support for both breastfeeding and maternal well‐being. Future work is urgently needed to confirm whether BFI is effective in supporting longer term breastfeeding outcomes. Further evaluation of how BFI is experienced by those receiving and providing care under its guidelines in resource‐rich settings is also necessary, to ensure that while continuing to promote and support breastfeeding, the mental, emotional, and practical needs of all mothers are met.
CONFLICTS OF INTEREST
The authors have no conflicts of interest to disclose. The authors have no financial relationships relevant to this article to disclose.
CONTRIBUTIONS
VF conceptualized the review. JAH critically reviewed the protocol. VF and AC are responsible for the searches, quality assessment, and data extraction and for the data synthesis and interpretation. VF and AC drafted the initial manuscript. VF, JAH, and AC critically revised the article. VF, JAH, and AC approved the final version of the study to be published.
Fallon VM, Harrold JA, Chisholm A. The impact of the UK Baby Friendly Initiative on maternal and infant health outcomes: A mixed‐methods systematic review. Matern Child Nutr. 2019;15:e12778 10.1111/mcn.12778
Footnotes
Sample size from Geddes (2012) not included in this figure as not reported in the original paper.
REFERENCES
- All Party Parliamentary Group . (2016). Breastfeeding trends UK. Retrieved from https://ukbreastfeeding.org/category/all-party-parliamentary-group/
- Bartington, S. , Griffiths, L. J. , Tate, a. R. , & Dezateux, C. (2006). Are breastfeeding rates higher among mothers delivering in Baby Friendly accredited maternity units in the UK? International Journal of Epidemiology, 35(5), 1178–1186. 10.1093/ije/dyl155 [DOI] [PubMed] [Google Scholar]
- Braun, V. , & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- Broadfoot, M. , Britten, J. , Tappin, D. M. , & MacKenzie, J. M. (2005). The Baby Friendly Hospital Initiative and breast feeding rates in Scotland. Archives of Disease in Childhood. Fetal and Neonatal Edition, 90(2), F114–F116. 10.1136/adc.2003.041558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, A. (2017). Breastfeeding as a public health responsibility: A review of the evidence. Journal of Human Nutrition and Dietetics, 30, 759–770. 10.1111/jhn.12496 [DOI] [PubMed] [Google Scholar]
- Critical Appraisal Skills Programme UK . (2017). CASP checklists. Retrieved from http://www.casp-uk.net/casp-tools-checklists
- Dagvadorj, A. , Yourkavitch, J. , & Lopes, S. (2017). Health facility staff training for improving breastfeeding outcome: A systematic review for step 2 of the Baby‐Friendly Hospital Initiative. Breastfeeding Medicine, 12(9). 10.1089/bfm.2017.0040), 537–546. [DOI] [PubMed] [Google Scholar]
- Dennis, C.‐L. C.‐L. , & McQueen, K. (2009). The relationship between infant‐feeding outcomes and postpartum depression: A qualitative systematic review. Pediatrics, 123(4), e736–e751. 10.1542/peds.2008-1629 [DOI] [PubMed] [Google Scholar]
- DiGirolamo, A. , Thompson, N. , Martorell, R. , Fein, S. , & Grummer‐Strawn, L. (2005). Intention or experience? Predictors of continued breastfeeding. Health Education & Behavior, 32(2), 208–226. 10.1177/1090198104271971 [DOI] [PubMed] [Google Scholar]
- Fallon, V. , Groves, R. , Halford, J. C. G. , Bennett, K. , & Harrold, J. A. (2016). Postpartum anxiety and infant feeding outcomes: A systematic review. Journal of Human Lactation, 32(4), 750–758. [DOI] [PubMed] [Google Scholar]
- Fallon, V. , Komninou, S. , Bennett, K. M. , Halford, J. C. G. , & Harrold, J. A. (2017). The emotional and practical experiences of formula‐feeding mothers. Maternal & Child Nutrition, 13(4). 10.1111/mcn.12392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geddes, J. (2012). Breastfeeding: How to increase prevalence. Nursing Times, 108(32–33), 12–14. [PubMed] [Google Scholar]
- Gregory, A. , Penrose, K. , Morrison, C. , Dennis, C. L. , & MacArthur, C. (2018). Psychometric properties of the breastfeeding self‐efficacy scale‐short form in an ethnically diverse UK sample. Public Health Nursing, 25(3), 278–284. [DOI] [PubMed] [Google Scholar]
- Harden, A. , & Thomas, J. (2005). Methodological issues in combining diverse study types in systematic reviews. International Journal of Social Research Methodology, 8(3), 257–271. 10.1080/13645570500155078 [DOI] [Google Scholar]
- Higgins, M. O. , St, I. , Roberts, J. , Glover, V. , & Taylor, A. (2013). Mother‐child bonding at 1 year; associations with symptoms of postnatal depression and bonding in the first few weeks. Archives of Women's Mental Health, 16, 381–389. 10.1007/s00737-013-0354-y [DOI] [PubMed] [Google Scholar]
- Hinsliff‐Smith, K. , Spencer, R. , & Walsh, D. (2014). Realities, difficulties, and outcomes for mothers choosing to breastfeed. Primigravid mother's experiences in the early postpartum period (6‐8) weeks. Midwifery, 30, e14–e19. [DOI] [PubMed] [Google Scholar]
- Hoddinott, P. , Craig, L. C. A. , Britten, J. , & McInnes, R. M. (2012). A serial qualitative interview study of infant feeding experiences: Idealism meets realism. BMJ Open, 2(2), e000504 10.1136/bmjopen-2011-000504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe‐Heyman, A. , & Lutenbacher, M. (2016). The Baby‐Friendly Hospital Initiative as an intervention to improve breastfeeding rates: A review of the literature. Journal of Midwifery & Women's Health, 61, 77–102. 10.1111/jmwh.12376 [DOI] [PubMed] [Google Scholar]
- Ingram, J. , Johnson, D. , & Condon, L. (2011). The effects of Baby Friendly Initiative training on breastfeeding rates and the breastfeeding attitudes, knowledge and self‐efficacy of community health‐care staff. Primary Health Care Research & Development, 12(3), 266–275. 10.1017/S1463423610000423 [DOI] [PubMed] [Google Scholar]
- Ingram, J. , Johnson, D. , & Greenwood, R. (2002). Breastfeeding in Bristol: Teaching good positioning, and support from fathers and families. Midwifery, 18(2), 87–101. 10.1054/midw.2002.0308 [DOI] [PubMed] [Google Scholar]
- Knaak, S. (2006). The problem with breastfeeding discourse. Canadian Journal of Public Health, 97(5), 412–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Komninou, S. , Fallon, V. , Halford, J. C. G. , & Harrold, J. A. (2017). Differences in the emotional and practical experiences of exclusively breastfeeding and combination feeding mothers. Maternal & Child Nutrition, 13(3). 10.1111/mcn.12364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lagan, B. M. , Symon, A. , Dalzell, J. , & Whitford, S. (2014). “The midwives aren't allowed to tell you”: Perceived infant feeding policy restrictions in a formula feeding culture. The Feeding your Baby Study. Midwifery, 30, e49–e55. [DOI] [PubMed] [Google Scholar]
- Lakshman, R. , Ogilvie, D. , & Ong, K. K. (2009). Mothers' experiences of bottle‐feeding: A systematic review of qualitative and quantitative studies. Archives of Disease in Childhood, 94(8), 596–601. 10.1136/adc.2008.151910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, E. (2007). Health, morality, and infant feeding: British mothers' experiences of formula milk use in the early weeks. Sociology of Health & Illness, 29(7), 1075–1090. 10.1111/j.1467-9566.2007.01020.x [DOI] [PubMed] [Google Scholar]
- Linares, A. M. , Rayens, M. K. , Gomez, M. L. , Gokun, Y. , & Dignan, M. B. (2014). Intention to breastfeed as a predictor of initiation of exclusive breastfeeding in Hispanic Women. Journal of Immigrant and Minority Health, E‐pub. [DOI] [PubMed]
- Mcandrew, A. F. , Thompson, J. , Fellows, L. , Large, A. , Speed, M. , & Renfrew, M. J. (2012). Infant feeding survey 2010. The Health and Social Care Information Centre, 1–331. [Google Scholar]
- Mertesacker, B. , Bade, U. , Haverkock, A. , & Pauli‐Pott, U. (2004). Predicting maternal reactivity/sensitivity: The role of infant emotionality, maternal depressiveness/anxiety, and social support. Infant Mental Health Journal, 25(1), 47–61. 10.1002/imhj.10085 [DOI] [Google Scholar]
- Pérez‐Escamilla, R. , Martinez, J. L. , & Segura‐Pérez, S. (2016). Impact of the Baby‐friendly Hospital Initiative on breastfeeding and child health outcomes: A systematic review. Maternal & Child Nutrition, 12(3), 402–417. 10.1111/mcn.12294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddin, E. , Pincombe, J. , & Darbyshire, P. (2007). Passive resistance: Early experiences of midwifery students/graduates and the Baby Friendly Health Initiative 10 steps to successful breastfeeding. 10.1016/j.wombi.2007.04.003 [DOI] [PubMed]
- Royal College of Midwives (2018). Position statement infant feeding. Retrieved from https://www.rcm.org.uk/sites/default/files/Infant Feeding.pdf
- Sayers, A. (2008). Tips and tricks in performing a systematic review. British Journal of General Practice, 58(457), 136 10.3399/bjgp08X277168–13136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmied, V. , Beake, S. , Sheehan, A. , McCourt, C. , & Dykes, F. (2011). Women's perceptions and experiences of breastfeeding support: A meta‐synthesis. Birth, 38(1), 49–61. 10.1111/j.1523-536X.2010.00446.x [DOI] [PubMed] [Google Scholar]
- Schmied, V. , Thomson, G. , Byrom, A. , Burns, E. , Sheehan, A. , & Dykes, F. (2014). A meta‐ethnographic study of health care staff perceptions of the WHO/UNICEF Baby Friendly Health Initiative. Women and Birth, 27(4), 242–249. 10.1016/j.wombi.2014.05.005 [DOI] [PubMed] [Google Scholar]
- Skouteris, H. , Bailey, C. , Nagle, C. , Hauck, Y. , Bruce, L. , & Morris, H. (2017). Interventions designed to promote exclusive breastfeeding in high‐income countries: A systematic review update. Breastfeeding Medicine, 12(10), 604–614. 10.1089/bfm.2017.0065 [DOI] [PubMed] [Google Scholar]
- Spencer, R. , Greatrex‐White, S. , & Fraser, D. (2015). ‘I thought it would keep them all quiet’. Women's experiences of breastfeeding as illusions of compliance: An interpretive phenomenological study. Journal of Advanced Nursing, 71(5), 1076–1086. 10.1111/jan.12592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tappin, D. , Britten, J. , Broadfoot, M. , & McInnes, R. (2006). The effect of health visitors on breastfeeding in Glasgow. International Breastfeeding Journal, 1, 1–9. 10.1186/1746-4358-1-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas, J. , & Harden, A. (2008). Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Medical Research Methodology, 8, 45 10.1186/1471-2288-8-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson, G. , & Dykes, F. (2011). Women's sense of coherence related to their infant feeding experiences. Maternal & Child Nutrition, 7(2), 160–174. 10.1111/j.1740-8709.2010.00251.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson, G. , Ebisch‐Burton, K. , & Flacking, R. (2015). Shame if you do—shame if you don't: Women's experiences of infant feeding. Maternal & Child Nutrition, 11(1), 33–46. 10.1111/mcn.12148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . (2010). Bottle feeding FAQs. Retrieved September 26, 2015, from http://www.unicef.org.uk/BabyFriendly/Health-Professionals/going-baby-friendly/FAQs/Bottle-feeding-FAQ/
- UNICEF . (2016). The Baby‐Friendly Hospital Initiative. Retrieved from http://www.unicef.org/programme/breastfeeding/baby.htm
- UNICEF . (2017). Baby Friendly—7 point plan for sustaining breastfeeding in the community. Retrieved from https://www.unicef.org.uk/babyfriendly/wp-content/uploads/sites/2/2014/02/7_point_plan_community.pdf
- UNICEF . (2018a). Baby Friendy Hospital Initiative: Ten steps to successful breastfeeding. Retrieved from https://www.unicef.org/nutrition/index_breastfeeding-ten-steps.html
- UNICEF . (2018b). Responsive feeding: Supporting close relationships. Retrieved from https://www.unicef.org.uk/babyfriendly/baby-friendly-resources/relationship-building-resources/responsive-feeding-infosheet/
- Victora, C. G. , Bahl, R. , Barros, A. J. D. , França, G. V. A. , Horton, S. , Krasevec, J. , … Walker, N. (2016). Breastfeeding in the 21st century: Epidemiology, mechanisms, and lifelong effect. Lancet, 387, 475–490. 10.1016/S0140-6736(15)01024-7 [DOI] [PubMed] [Google Scholar]
- WHO . (2015). World Health Organisation Infant Feeding Recommendation. Retrieved September 1, 2015, from http://www.who.int/nutrition/topics/infantfeeding_recommendation/en/
- WHO . (2018). Baby Friendly Hospital Initiative. Retrieved October 24, 2018 from http://www.who.int/nutrition/topics/bfhi/en/
- WHO & UNICEF . (1990). Innocenti Declaration. Retrieved from https://www.unicef.org/programme/breastfeeding/innocenti.htm


