Abstract
Breastfeeding confers multiple benefits for the health and development of very preterm infants, but there is scarce information on the duration of breastfeeding after discharge from the neonatal intensive care unit (NICU). We used data from the Effective Perinatal Intensive Care in Europe population‐based cohort of births below 32 weeks of gestation in 11 European countries in 2011–2012 to investigate breastfeeding continuation until 6 months. Clinical and sociodemographic characteristics were collected from obstetric and neonatal medical records as well as parental questionnaires at 2 years of corrected age. Among 3,217 ever‐breastfed infants, 34% were breastfeeding at 6 months of age (range across countries from 25% to 56%); younger and less educated mothers were more likely to stop before 6 months (adjusted relative risk [aRR] <25 years: 0.68, 95% CI [0.53, 0.88], vs. 25–34 years; lower secondary: 0.58, 95% CI [0.45, 0.76] vs. postgraduate education). Multiple birth, bronchopulmonary dysplasia (BPD), and several neonatal transfers reduced the probability of continuation but not low gestational age, fetal growth restriction, congenital anomalies, or severe neonatal morbidities. Among infants breastfeeding at discharge, mixed versus exclusive breast milk feeding at discharge was associated with stopping before 6 months: aRR = 0.60, 95% CI [0.48, 0.74]. Low breastfeeding continuation rates in this high‐risk population call for more support to breastfeeding mothers during and after the neonatal hospitalization, especially for families with low socio‐economic status, multiples, and infants with BPD. Promotion of exclusive breastfeeding in the NICU may constitute a lever for improving breastfeeding continuation after discharge.
Keywords: breast milk, breastfeeding, inverse probability weighting, neonatal intensive care, prematurity, very preterm infants
Key messages.
In this multiregional European cohort, one third of ever‐breastfed very preterm infants were breastfed at 6 months, varying from 25% (Portuguese and British regions) to 50% (Swedish and Danish regions).
The probability of being breastfed to 6 months was lower for infants with less educated mothers.
Neonatal factors associated with stopping were multiple birth, bronchopulmonary dysplasia, and multiple neonatal transfers but not low gestational age or other severe morbidities.
Continuation was more likely with exclusive, as opposed to mixed, breastfeeding.
Rates of breastfeeding continuation for very preterm babies in Europe fall short of international recommendations and are marked by strong social inequalities.
1. INTRODUCTION
Breast milk is considered the best food for newborns and infants, and the World Health Organization recommends exclusive breastfeeding until 6 months of age (Bernard et al., 2017; Edmond et al., 2006; Ip et al., 2007; Kramer & Kakuma, 2002). The nutritional and immunological benefits of breast milk are particularly important for very preterm infants born at less than 32 weeks of gestation who are at higher risk of infection and other health and developmental problems than term infants. (Lechner & Vohr, 2017; Vohr et al., 2007; Vohr et al., 2017). Breastfeeding a very preterm infant also reinforces the mother's caregiving role in the neonatal intensive care unit (NICU) and can promote bonding (Flacking, Ewald, Nyqvist, & Starrin, 2006; Ikonen, Paavilainen, & Kaunonen, 2015). However, breastfeeding a very preterm infant is challenging, requiring the mother to pump milk regularly until her child has acquired the capacity to suckle at the breast and posing multiple logistic challenges during the long neonatal hospitalization (Callen & Pinelli, 2005; Nye, 2008). Consequently, breastfeeding rates for very preterm infants are lower than for full‐term infants (Akerstrom, Asplund, & Norman, 2007; Flacking, Nyqvist, & Ewald, 2007; Merewood, Brooks, Bauchner, MacAuley, & Mehta, 2006).
Most research on breastfeeding very preterm infants has focused on breastfeeding initiation or at discharge from the NICU (Bonet et al., 2011; Lee & Gould, 2009; Sisk, Lovelady, Dillard, Gruber, & O'Shea, 2009; Zachariassen et al., 2010). These studies find that younger maternal age, being foreign‐born, and having a low educational level reduce the probability of breastfeeding at discharge home from hospital. The child's clinical characteristics are also important: Breastfeeding is less likely among multiples and infants with low gestational ages, fetal growth restriction, severe neonatal morbidities, and congenital anomalies.
Finally, breastfeeding support policies in the NICU, including having designated members to support mothers, having a Baby‐Friendly Hospital Initiative accreditation, and general cultural attitudes to breastfeeding also affect breastfeeding rates among very preterm infants (Bonet et al., 2015; Rodrigues, Severo, Zeitlin, & Barros, 2017; Santoro Junior & Martinez, 2007; Wilson et al., 2017).
We have less knowledge about factors that favour or hinder continued breastfeeding after discharge from the NICU. The same social and clinical characteristics that influence breastfeeding in the neonatal unit may affect continuation, but it is possible that salient factors differ. Social characteristics, for instance, may exert a stronger influence after the child returns home, whereas those related to care in the neonatal unit may have less impact. An understanding of the factors that promote continued breastfeeding is needed to develop effective postdischarge support and to prepare families at discharge for the difficulties they may face.
In this study, we sought to identify factors associated with breastfeeding continuation until 6 months of age among breastfed very preterm infants using data from a European multiregional population‐based study.
2. METHODS
2.1. Data source
This study uses data from the Effective Perinatal Intensive Care in Europe cohort, a population‐based cohort study including all stillbirths and live births born below 32 weeks of gestation in 19 regions from 11 European countries over a 12‐month period in 2011 and 2012 (Zeitlin et al., 2016). Participating countries (regions) were Belgium (Flanders), Denmark (Eastern region), Estonia (entire country), France (Burgundy, Ile‐de‐France, and the Northern region), Germany (Hesse and Saarland), Italy (Emilia‐Romagna, Lazio, and Marche), the Netherlands (Central and Eastern region), Poland (Wielkopolska), Portugal (Lisbon, Tagus Valley, and North region), Sweden (greater Stockholm area), and the United Kingdom (East Midlands, Northern, and Yorkshire and Humber regions). For the three French regions, data were collected as part of the French study EPIPAGE2, where inclusions lasted 6 months in 2011–2012 (Ancel et al., 2015).
Perinatal and maternal characteristics were abstracted from obstetrical and neonatal medical records using a pretested standardized questionnaire filled in by a trained health care professional. Data were collected until the infant's discharge home and included information on breastfeeding at discharge. At 2 years of corrected age, a questionnaire was sent to parents to collect information about maternal sociodemographic characteristics and the child's health and development. The 2‐year questionnaire included questions about whether the child was ever breastfed and the age of the child when breastfeeding was stopped.
2.2. Ethical approvals
Ethics approval and parental consent were obtained in each study region from regional and/or hospital ethics committees, as required by national legislation. The European study was also approved by the French Advisory Committee on Use of Health Data in Medical Research and the French National Commission for Data Protection and Liberties.
2.3. Study population
Our study population includes all infants followed up at 2 years of corrected age who were ever breastfed and for whom breastfeeding status at 6 months was available. Infants born in one of the regions, Northern UK, were excluded because of concern about selection bias among responders due to a very low response rate (<35%). Of 6,410 infants surviving to discharge in the 18 remaining regions, 26 died before 2 years of age. Of the 6,384 eligible infants for follow‐up at 2 years, questionnaires were returned for 4,321 (67.7%). Follow‐up rates differed between the regions: ranging from 47.2% in Belgium to 97.9% in Estonia. Among these infants, 951 were never breastfed (22.0%) and 153 (3.5%) had missing information on breastfeeding status at 6 months. The sample for this study therefore comprised 3,217 ever‐breastfed infants (Figure 1).
Figure 1.
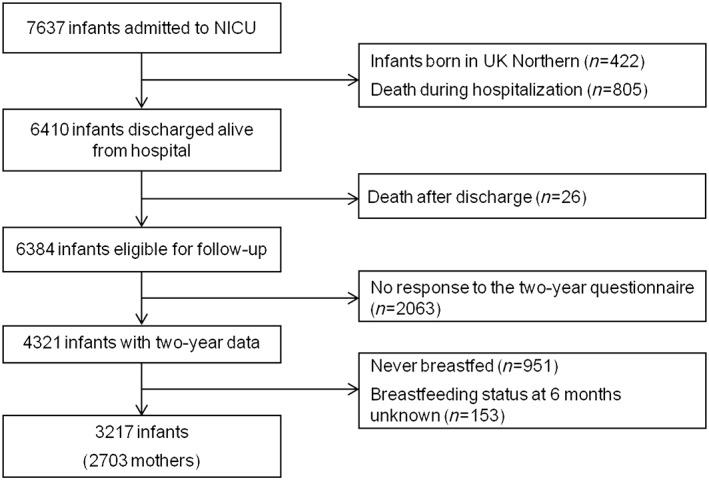
Flow‐chart of study cohort
2.4. Outcomes
First, infants were considered to have ever been breastfed if the answer was yes to the question “Was your child breast fed” in the parental questionnaire at 2 years.
The primary outcome was whether the child was breastfed until at least 6 months of chronological age. Information on exclusive (only breast milk) and mixed (breast milk and formula) feeding, and on whether the child was feeding directly at the breast or received breast milk using a cup or a bottle was collected at discharge but not at 2 years.
Infants were considered to be breastfed until at least 6 months if mothers reported an age when breastfeeding was stopped that was greater or equal to 6 months. In few cases, the mother stated that she had breastfed but did not provide information on when she stopped. If the infant was not breastfed at discharge, as indicated in the medical notes, and was discharged home before 6 months of age, we considered that the infant was not breastfed at 6 months.
2.5. Sociodemographic and infant health characteristics
We investigated maternal sociodemographic variables that were found in previous studies to affect breastfeeding initiation and breastfeeding in the NICU, including level of education, which was categorized in four groups according to the International Standard Classification of Education 2011 (Schneider), age in years, country of birth (Europe or other country), parity, and type of pregnancy (single or multiple). Infant characteristics were gestational age, whether the child had a severe neonatal morbidity diagnosed before discharge home—including intraventricular haemorrhage Papille's grades III or IV, cystic periventricular leukomalacia, retinopathy of prematurity III to V, necrotizing enterocolitis, and bronchopulmonary dysplasia (BPD), defined as respiratory support or oxygen at 36 weeks post menstrual age (Bonamy et al., 2017). We also included information on whether the infant was small for gestational age (<10th percentile) using intrauterine curves (Zeitlin et al., 2017), had any surgery, or was transferred during neonatal care. Finally for the subset of children who were no longer breastfed after discharge, we created a variable to describe their feeding status at discharge (receiving exclusive breast milk at the breast, exclusive breast milk but not from the breast, mixed feeding (breast milk and formula) with breast milk from the breast, mixed feeding with breast milk not from the breast). Missing data were low for maternal and neonatal variables (< 2%) and 2.5% for mother's education level. Missing data were excluded in multivariable models.
2.6. Analysis strategy
We first compared the characteristics of responders and nonresponders with the 2‐year questionnaire. We used the Wald test from logistic regressions adjusting for region to take into consideration differences in the response rates by region (Table S1). To take into consideration potential biases due to nonresponse, we used the inverse probability weighting method (Cole & Hernan, 2008). This method involves assigning a weight that is inversely proportional to the probability of response for each subject based on demographic, social, and medical characteristics; the weight was computed using the complete sample of eligible infants (n = 6,384). Probabilities were predicted using a logistic regression model with follow‐up status at 2 years (yes or no) as the outcome. All demographic and health variables associated with nonresponse were included in this regression (maternal age, parity, pregnancy and neonatal characteristics of care, breastfeeding at discharge, and region, as shown in Table S1). Missing data from variables included in this regression model were imputed with chained equations. Data were assumed to be missing at random. All results presented in this study are based on weighted data.
We then described rates of breastfeeding continuation for each covariable in our study sample of ever‐breastfed infants and used generalized linear multilevel regression models with a Poisson distribution and robust standard errors. This model makes it possible to estimate covariate adjusted risk ratios for binary outcomes (Zou & Donner, 2013). We used multilevel models to take into account the hierarchical structure of our data (infants within countries) and the nonindependence of observations within countries. Risk ratios were preferred to odds ratios as breastfeeding continuation at 6 months is not a rare event and our data study used a cohort design. In order to assess the potential impact of mode of feeding at discharge on breastfeeding continuation, we ran a second model using the subpopulation of infants breastfed at discharge, that is, excluding infants who stopped breast milk feedings before discharge. Finally, to estimate the impact of maternal and infant characteristics on country specific rates of breastfeeding continuation, we computed adjusted rates based on our final model in the overall sample and compared these with unadjusted rates.
We also carried out two sensitivity analyses. We first compared weighted with unweighted models to assess the impact of considering bias due to nonresponse. Second, we examined the potential impact of multiple births with a model using mothers (as opposed to babies) as our level of observation. In this model, a mother of multiples was considered to breastfeed until 6 months if at least one of her infants continued to this age. Variables describing neonatal risk factors (BPD, surgery, SGA, and morbidity) were considered present if at least one infant was affected.
All statistical analyses were performed using STATA V.14.
3. RESULTS
Table 1 describes the maternal and neonatal characteristics of our sample of ever‐breastfed infants included in the 2 years follow‐up. Both the unweighted and weighted distributions of maternal and neonatal characteristics are shown. As seen by the changes in proportions after weighting, taking into consideration nonresponders led to slightly higher proportions of mothers born outside of Europe, multipara, and multiples. The other variables had very similar overall distributions.
Table 1.
Breastfeeding continuation at 6 months among ever‐breastfed infants, according to maternal and neonatal characteristics
| Infants (N) | Unweighted (%) | Weighted (%) | Breastfed until 6 months weighted rates (%) | Unadjusted RR [95% CI] | |
|---|---|---|---|---|---|
| TOTAL | 3217 | 34.4 | |||
| Maternal age (years) | |||||
| <25 | 351 | 10.9 | 11.0 | 20.9 | 0.60 [0.48–0.75] |
| 25–34 | 1925 | 60.0 | 60.0 | 34.7 | Ref. |
| ≥35 | 934 | 29.1 | 29.0 | 37.6 | 1.08 [0.97–1.21] |
| Mother's country of birth | |||||
| Europe | 2716 | 85.6 | 84.4 | 31.8 | Ref. |
| Other | 457 | 14.4 | 15.6 | 45.8 | 1.44 [1.28–1.63] |
| Mother's educational level | |||||
| Lower secondary | 426 | 13.6 | 13.6 | 25.3 | 0.52 [0.53–0.64] |
| Upper secondary | 1265 | 40.3 | 40.4 | 29.9 | 0.61 [0.54–0.69] |
| Bachelor degree or less | 846 | 27.0 | 28.0 | 34.9 | 0.72 [0.63–0.82] |
| Master/doctoral degree | 598 | 19.1 | 18.1 | 48.6 | Ref. |
| Parity | |||||
| 0 | 2012 | 63.1 | 59.8 | 34.2 | Ref. |
| 1 | 754 | 23.6 | 24.2 | 35.1 | 1.03 [0.91–1.16] |
| 2 or more | 424 | 13.3 | 16.0 | 31.1 | 0.91 [0.77–1.07] |
| Type of pregnancy | |||||
| Singleton | 2201 | 68.4 | 66.6 | 37.2 | Ref. |
| Multiple | 1016 | 31.6 | 33.4 | 27.7 | 0.74 [0.66–0.83] |
| Gestational age (weeks) | |||||
| 23–25 | 227 | 7.1 | 7.2 | 35.8 | 1.10 [0.91–1.34] |
| 26–27 | 544 | 16.9 | 16.1 | 39.9 | 1.23 [1.08–1.40] |
| 28–29 | 648 | 26.9 | 27.0 | 33.0 | 1.02 [0.90–1.15] |
| 30–31 | 1582 | 49.1 | 49.7 | 32.4 | Ref. |
| SGA | |||||
| <10th percentile | 1035 | 32.2 | 32.0 | 34.7 | 1.03 [0.93–1.15] |
| ≥10 | 2182 | 67.8 | 68.0 | 33.7 | Ref. |
| Severe neonatal morbiditya | |||||
| No | 2866 | 90.9 | 90.5 | 34.3 | Ref. |
| Yes | 286 | 9.1 | 9.5 | 34.0 | 0.99 [0.83–1.18] |
| Bronchopulmonary dysplasiab | |||||
| No | 2777 | 88.0 | 87.2 | 34.8 | Ref. |
| Yes | 380 | 12.0 | 12.8 | 29.1 | 0.84 [0.71–0.99] |
| Surgeryc | |||||
| No | 2919 | 90.7 | 91.1 | 33.4 | Ref. |
| Yes | 298 | 9.3 | 8.9 | 40.4 | 1.21 [1.04–1.41] |
| Transfer during neonatal care | |||||
| 0 | 1923 | 59.8 | 60.2 | 35.9 | Ref. |
| 1 | 891 | 27.7 | 27.7 | 32.6 | 0.91 [0.81–1.02] |
| 2 or more | 403 | 12.5 | 12.1 | 28.0 | 0.78 [0.65–0.93] |
| Breastfeeding at discharge | |||||
| Exclusive at breast | 865 | 29.5 | 29.0 | 56.8 | ‐ |
| Exclusive not at breast | 305 | 10.4 | 9.4 | 44.4 | ‐ |
| Mixed at breast | 796 | 27.2 | 27.4 | 31.0 | ‐ |
| Mixed not at breast | 464 | 15.9 | 14.1 | 24.9 | ‐ |
| Not breastfeeding at discharge | 498 | 17.0 | 20.0 | 0.0 | ‐ |
| Countryd | |||||
| Belgium (Flanders) | 245 | 7.6 | 10.3 | 30.6 | 0.85 [0.71–1.02] |
| Denmark (eastern region) | 170 | 5.3 | 5.7 | 48.8 | 1.36 [1.17–1.59] |
| Estonia (entire country) | 119 | 3.7 | 2.6 | 37.0 | 1.03 [0.83–1.28] |
| France (Burgundy, Ile‐de‐France, and the northern region) | 526 | 16.4 | 12.3 | 36.2 | 1.01 [0.90–1.13] |
| Germany (Hesse and Saarland) | 316 | 9.8 | 9.6 | 41.1 | 1.15 [1.01–1.31] |
| Italy (Emilia‐Romagna, Lazio and Marche) | 545 | 16.9 | 14.8 | 31.9 | 0.89 [0.79–1.01] |
| The Netherlands (central and eastern region) | 199 | 6.2 | 5.9 | 33.8 | 0.94 [0.79–1.13] |
| Poland (Wielkopolska) | 129 | 4.0 | 3.3 | 38.2 | 1.07 [0.81–1.37] |
| Portugal (Lisbon, Tagus Valley, and north region) | 344 | 10.7 | 10.6 | 25.0 | 0.70 [0.58–0.83] |
| Sweden (greater Stockholm area) | 152 | 4.7 | 4.7 | 52.5 | 1.47 [1.26–1.71] |
| UK (east midlands and Yorkshire & Humber regions) | 472 | 14.7 | 20.3 | 28.1 | 0.78 [0.68–0.91] |
Note. Ref.: reference; RR: risk ratio—95% CI: confidence intervals.
Included retinopathy of prematurity, intraventricular haemorrhage, periventricular leukomalacia and necrotizing enterocolitis.
Oxygen dependence or ventilation at 36 weeks of gestational age.
During neonatal hospitalization.
Sample average was used as reference for deriving risk ratio for each region.
About 11% of infants had a mother aged less than 25 years of age and 29% had a mother 35 years or older; about 60% were first‐born children. Mothers were mainly born in Europe; almost 14% had only lower secondary education, whereas 18% had a master or doctoral degree. About one quarter of infants were born before 28 weeks of GA, with 7% at <26 weeks GA; 67% were from singleton pregnancies. About one in 10 had a severe neonatal morbidity, not including BPD, and 13% had BPD. Forty percent of children were transferred at least once during their neonatal hospitalization. At discharge, breastfeeding had already been discontinued for 20% of ever‐breastfed infants, whereas 38% were exclusively receiving breast milk and 42% breast milk and formula.
Overall, 34.4% were still breastfed at 6 months of age. In univariate comparisons, also shown in Table 1, maternal characteristics associated with breastfeeding continuation were maternal age (mothers under 25 were more likely to stop before 6 months), being born outside of Europe and higher maternal education. Parity was not associated with breastfeeding continuation. Children from multiple pregnancies, with BPD and who were transferred two or more times were less likely to be breastfed at 6 months. Having had surgery and being born at 26 and 27 weeks of gestational age compared with being born at 30 or 31 weeks were associated with continued breastfeeding. Infants who were exclusively breastfed at the breast at discharge were more likely to continue to 6 months, 56.8%, versus 24.9% for those receiving breast milk not at the breast and formula.
Rates of breastfeeding continuation varied significantly by country of birth: from 25.0% in Portugal to 52.5% in Sweden. As shown in Figure 2, in addition to overall continuation rates, the proportion of infants who stopped breastfeeding during the neonatal hospitalization differed across countries, with a range from 10.7% in Poland, 11.0% in Estonia, or 11.4% in Italy to 25.8% in UK.
Figure 2.
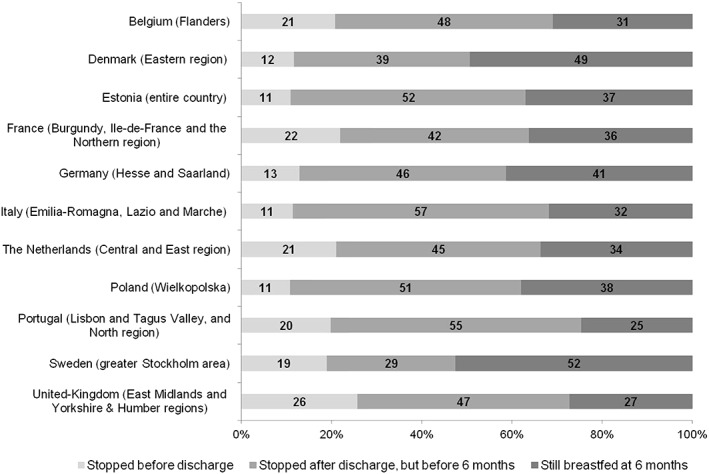
Distribution of infants by country according to the moment that breastfeeding was stopped
In the adjusted model conducted on the overall sample, presented in Table 2, most of the associations observed in Table 1 persisted. Infants with mothers less than 25 years of age were 30% less likely to be breastfed than infants with older mothers (aRR = 0.68 [0.53–0.88]), whereas educational level had a strong linear effect. Mothers born out of Europe were more likely to continue breastfeeding until 6 months (aRR = 1.47 [1.26–1.71]). Estimated relative risks for neonatal factors were similar in multivariable models.
Table 2.
Maternal and neonatal characteristics associated with breast milk feeding continuation until 6 months among all ever‐breastfed infants and among infants still breastfeeding at discharge
| Model 1 all ever‐breastfed infants | Model 2 infants breastfed at discharge | |||
|---|---|---|---|---|
| Adjusted RR | 95% CI | Adjusted RR | 95% CI | |
| Maternal age (years) | ||||
| <25 | 0.68 | 0.53–0.88 | 0.92 | 0.77.–1.09 |
| 25–34 | 1.00 | Ref. | 1.00 | Ref. |
| ≥35 | 1.11 | 0.94–1.30 | 1.13 | 0.97–1.32 |
| Mother born outside of Europe | 1.47 | 1.26–1.71 | 1.44 | 1.29–1.62 |
| Mother's educational level | ||||
| Lower secondary | 0.58 | 0.45–0.76 | 0.65 | 0.49–0.85 |
| Upper secondary | 0.67 | 0.55–0.82 | 0.74 | 0.62–0.87 |
| Bachelor degree or less | 0.85 | 0.70–1.02 | 0.86 | 0.74–0.99 |
| Master/doctoral degree | 1.00 | Ref. | 1.00 | Ref. |
| Parity | ||||
| 0 | 1.00 | Ref. | 1.00 | Ref. |
| 1 | 0.97 | 0.86–1.10 | 0.91 | 0.82–1.01 |
| 2 or more | 0.83 | 0.64–1.07 | 0.99 | 0.81–1.20 |
| Type of pregnancy (multiple) | 0.69 | 0.58–0.81 | 0.80 | 0.70–0.91 |
| Gestational age (weeks) | ||||
| 23–25 | 1.06 | 0.86–1.32 | 1.31 | 1.07–1.60 |
| 26–27 | 1.20 | 1.02–1.41 | 1.29 | 1.11–1.50 |
| 28–29 | 0.99 | 0.88–1.11 | 1.06 | 0.92–1.22 |
| 30–31 | 1.00 | Ref. | 1.00 | Ref. |
| SGA (<10th percentile) | 1.04 | 0.97–1.12 | 1.10 | 1.01–1.18 |
| Severe neonatal morbiditya | 0.95 | 0.76–1.18 | 0.93 | 0.72–1.19 |
| Bronchopulmonary dysplasiab | 0.83 | 0.73‐0.94 | 0.97 | 0.84–1.12 |
| Surgeryc | 1.21 | 1.05‐1.41 | 1.17 | 0.97–1.42 |
| Transfers during neonatal care | ||||
| 0 | 1.00 | Ref. | 1.00 | Ref. |
| 1 | 0.92 | 0.78–1.09 | 0.89 | 0.79–1.00 |
| 2 or more | 0.83 | 0.67–1.03 | 0.84 | 0.72–0.99 |
| Breastfeeding at discharge | ||||
| Exclusive feeding at breast | ‐ | ‐ | 1.00 | Ref. |
| Exclusive feeding not at breast | ‐ | ‐ | 0.86 | 0.71–1.05 |
| Mixed feeding at breast | ‐ | ‐ | 0.60 | 0.48–0.74 |
| Mixed feeding not at breast | ‐ | ‐ | 0.46 | 0.31–0.69 |
Note. aRR: adjusted risk ratio for all variables in the table; Ref.: reference.
Included retinopathy of prematurity, intraventricular haemorrhage, periventricular leukomalacia and necrotizing enterocolitis.
Oxygen dependence or ventilation at 36 weeks of gestational age.
During neonatal hospitalization.
In the second model which focused on the sample of infants still breastfed at discharge, we found that receiving formula at discharge was associated with a significantly lower probability of breastfeeding continuation until 6 months, for those feeding directly at the breast (aRR = 0.60 [0.48–0.74]) as well as those not feeding directly at the breast (aRR = 0.46 [0.31–0.69]). In the subpopulation of infants breastfed at discharge, young maternal age and BPD were no longer associated with breastfeeding continuation, even when feeding status at discharge was not present in the model (results not shown). Additional sensitivity analyses found that results of the final model were similar without weights (Table S2). When models were run using mothers, instead of infants, as the unit of observations, results were also similar (Table S3).
Maternal and neonatal characteristics explained only a small proportion of the difference between countries, as shown in Figure 3 which compares breastfeeding continuation to 6 months before and after adjustment. However, differences in population characteristics affected rankings in some countries. For instance, if maternal and infant characteristics were the same across all countries, Sweden would have lower rates (52% to 46%) and higher rates would be observed in Estonia (37 to 39%) and in the UK (28 to 31%).
Figure 3.
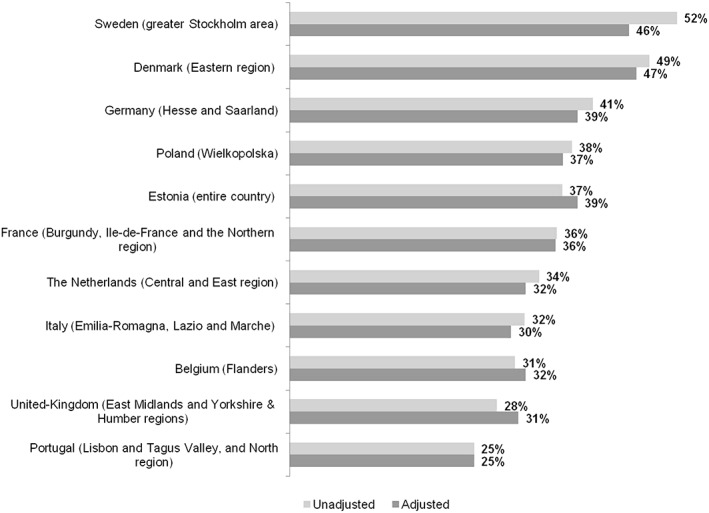
Percent breastfeeding at 6 months among breastfed very preterm infants by country
4. DISCUSSION
Among very preterm infants who were breastfed after birth, only 34.4% were breastfed up until 6 months, although breastfeeding continuation rates varied across countries. Lower rates were observed in regions from Portugal and the UK and higher rates in those from Sweden and Denmark, but even in the countries with higher rates, only about half of infants who started breastfeeding continued to 6 months of age. Most infants stopped breastfeeding after discharge from hospital, but in some countries up to one quarter of children had stopped before discharge. A low maternal educational level was a key risk factor for stopping breastfeeding. In contrast, women born outside of Europe breastfed longer. Infants from multiple pregnancies were also less likely to continue breastfeeding until 6 months. Two neonatal factors negatively affected continuation: BPD and multiple neonatal transfers, whereas other neonatal risk factors, such as severe neonatal morbidities and small for gestational age, found in previous research to negatively impact initiation of breastfeeding, were not associated with or favoured continuation. Finally, infants receiving breast milk and formula at discharge were half as likely to be breastfed to 6 months as those receiving only breast milk.
4.1. Strengths and limitations
The main strengths of this study are the large multicountry population‐based sample with data collected at birth and at 2 years using common, pretested protocols. It is therefore possible to estimate and to compare breastfeeding continuation rates until 6 months using the same methodology across a range of sociocultural contexts in Europe. This is important as previous studies have employed varying definitions, making international comparisons difficult (Rodrigues et al., 2018). The availability of data on many perinatal and socio‐economic characteristics allowed us to consider multiple risk factors found to be of importance for breastfeeding initiation in previous studies. Finally, the majority of previous studies had smaller, more selected samples, being principally from single centres (Flacking, Wallin, & Ewald, 2007; Morag et al., 2016; Rodrigues et al., 2018).
Our study also has some limitations. About 32% of the infants discharged alive were not followed‐up at 2 years corrected age. Infants whose parents answered the questionnaire at 2 years were more frequently breastfed at discharge from hospital. However, we were able to compare responders with nonresponders and took into consideration potential selection biases by using inverse probability weighting methods. Sensitivity analyses showed that results were not substantially affected by weighting for nonresponse. We also did not have information regarding exclusive breastfeeding after discharge, support after discharge, and the reasons for weaning. The duration of breastfeeding was collected retrospectively when the child was 2 years of age, and this may lead to some misclassification bias, although studies find good validity of maternal recall of breastfeeding duration (Amissah, Kancherla, Ko, & Li, 2017; Li, Scanlon, & Serdula, 2005). Finally, some important factors that might affect postdischarge decisions were not collected, including maternal smoking status which has been found to affect decisions to continue breastfeeding (Callen & Pinelli, 2005; Killersreiter, Grimmer, Buhrer, Dudenhausen, & Obladen, 2001).
4.2. Comparison with other findings and interpretation
Some of the maternal and neonatal characteristics that we found to be associated with continuation have been noted in smaller single‐centre studies. In one single‐centre study of 225 very preterm infants in Sweden, Flacking et al. (2007) reported that mothers with low socio‐economic level were less likely to continue breastfeeding until 6 months. In general, maternal social status has been found to negatively impact on breastfeeding—including breastfeeding initiation in very preterm infants as well as among term infants (Flacking et al., 2007; Forster, McLachlan, & Lumley, 2006; Herich et al., 2017; Li, Darling, Maurice, Barker, & Grummer‐Strawn, 2005; Scott & Binns, 1999). Previous studies have also observed that few neonatal morbidities impact on breastfeeding continuation. In an Israeli study including 181 very preterm infants, neonatal morbidities did not affect breastfeeding continuation between 6 weeks postdischarge and 6 months corrected age (Morag et al., 2016). In fact, cessation of breastfeeding before 6 months corrected age was more frequent for infants born at higher gestational age over 28 weeks (Morag et al., 2016). We also found that infants born below 28 weeks were more likely to be breastfed until 6 months compared with infants born at 30–31 weeks. One hypothesis for this finding is that motivation for breastfeeding may be increased for mothers with a particularly fragile infant; further, as initiation of breastfeeding is more challenging for these infants—as witnessed by the body of literature linking low gestational age to a reduced probability of breastfeeding (Lee & Gould, 2009)—less motivated mothers may be discouraged at the onset. Another hypothesis is that these mothers receive more support and attention from hospital staff because of their child's high‐risk health status.
In contrast with other neonatal morbidities, BPD did affect continuation. BPD affects suck–swallow respiration coordination, and these infants may face sucking difficulties. Infants with BPD also have poor feeding endurance and performance (Mizuno et al., 2007). These difficulties could make continued breastfeeding more challenging. Rehospitalizations in the first year of life are also more than twice as frequent among infants with BPD compared with other very preterm infants and this may interfere with breastfeeding continuation (Smith et al., 2004). We found, however, that the relation with BPD was no longer significant among the subsample of infants breastfed at discharge, suggesting that this factor may hinder continuation during the neonatal hospitalization. A better understanding of this negative relationship could lead to targeted interventions to help breastfeeding mothers of infants with BPD. This is important as BPD is an independent risk factor for poor longer term health and development (Arnaud et al., 2007).
We also found that multiple neonatal transfers were associated with an increased risk of stopping breastfeeding before 6 months. This result could be explained by the discontinuity in information provided or practices across different NICUs leading to confusion or lack of support. The absence of common beliefs and practices within the NICU has been identified as an obstacle at the unit level to successful breastfeeding promotion (Bonet et al., 2015). The variation in the proportion of infants who stopped breastfeeding while still in hospital illustrates that neonatal unit policies can impact on continuation. In a previous qualitative study on breastfeeding with neonatal unit staff in several regions participating in the Effective Perinatal Intensive Care in Europe project, UK participants suggested that discharge policies may discourage continued breastfeeding when formula feeding is perceived to facilitate earlier discharge (Bonet et al., 2015). Other unit policies have been found to affect breastfeeding at discharge in our cohort, including the presence of dedicated personnel for breastfeeding support in the Portuguese regions (Rodrigues et al., 2017) and the baby‐friendly hospital initiative in the overall sample (Wilson et al., 2017). Kangaroo Care has been found to be positively associated with breastfeeding duration in other studies (Flacking, Ewald, & Wallin, 2011). Our finding that exclusive as opposed to mixed breastfeeding at discharge was strongly related to the probability of continuation points to a modifiable practice that likely reflects unit policies, as rates of mixed versus exclusive feeding at discharge vary widely across Europe (Wilson et al., 2017). In contrast, we did not find that direct feeding from the breast had a significant impact on continuation, unlike a study conducted in one single‐centre in Israel on 162 mothers of very preterm infants (Pinchevski‐Kadir et al., 2017).
Consideration of maternal and neonatal factors did not substantially reduce the wide differences observed between countries in our study. The reasons for these persistent large disparities are likely linked to unit policies, as discussed above, as well as the support and counselling available to mothers after their discharge from hospital; the importance of these latter factors, which we could not include in our study, was highlighted in the integrative review by Briere et al. on breastfeeding duration after NICU discharge (Briere, McGrath, Cong, & Cusson, 2014). Broader policies promoting breastfeeding in the general population as well as structural measures related to the duration of maternity leave or employment regulations that facilitate combining work with breastfeeding also differ across the countries in our sample, but further research is needed to understand their impact on breastfeeding continuation in this population (Bonet et al., 2015).
5. CONCLUSION
We found low breastfeeding continuation rates, marked by strong social inequalities, among very preterm infants in European regions. Given current international recommendations, knowledge about the positive effects of breastfeeding for child health and development and the need to address social inequalities in health, our results call for increased policy attention to the promotion of breastfeeding in this vulnerable population. Overall, a majority of ever‐breastfed infants were weaned after discharge, highlighting the importance of postdischarge counselling and support. However, more support in the neonatal unit could target discontinuation during the neonatal hospitalization, which occurred more frequently in some of the study regions. Our results also point to specific areas where changes to neonatal policies could improve breastfeeding continuation more generally, including management of intrafacility transfers, breastfeeding support to the mothers of multiples and infants with BPD and promotion of exclusive feeding. Given the marked differences in continuation by maternal education, understanding the specific obstacles faced by women from more disadvantaged families is needed to design interventions to mitigate these negative effects. Finally, our study has an encouraging message for parents and providers: once breastfeeding initiation is successful, infants at highest risk are not more likely to stop. Thus, while it may be harder to start breastfeeding infants born at very low gestational age or with severe neonatal morbidities, these obstacles appear to be overcome in the long‐run.
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
JZ had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design was done by JZ, BB, AKEB, LG, AvH, ESD, and MC. All authors (including authors listed in EPICE Research Group) contributed to the acquisition, analysis, or interpretation of data. The drafting of the manuscript was done by CB and JZ. Also, the statistical analysis was done by CB, AP, and JZ. Lastly, the critical revision of the manuscript for important intellectual content and approval of final version of the manuscript was done by all authors (including authors listed in EPICE Research Group).
Supporting information
Table S1: Comparison of proportions of children followed up at 2 years by maternal and neonatal characteristics and country, all infants eligible for follow‐up regardless of breastfeeding status
Table S2: Maternal and neonatal characteristics associated with breast milk feeding continuation until 6 months among all ever‐breastfed infants and among infants still breastfeeding at discharge – Unweighted models
Table S3: Maternal and neonatal characteristics associated with breast milk feeding continuation until 6 months among mothers of all ever breastfed infant and among mothers of infant still breastfeeding at discharge
ACKNOWLEDGMENTS
We would like to acknowledge the participation of the Departments of Obstetrics and Neonatology from the hospitals in the EPICE regions. Additional funding is acknowledged from the following regions: France (French Institute of Public Health Research/Institute of Public Health and its partners the French Health Ministry, the National Institute of Health and Medical Research, the National Institute of Cancer, and the National Solidarity Fund for Autonomy; grant ANR‐11‐EQPX‐0038 from the National Research Agency through the French Equipex Program of Investments in the Future; and the PremUp Foundation); Poland (2012‐2015 allocation of funds for international projects from the Polish Ministry of Science and Higher Education); Sweden (funding by a regional agreement on medical training and clinical research [ALF] between Stockholm County Council and Karolinska Institutet, and by the Department of Neonatal Medicine, Karolinska University Hospital); and United Kingdom (funding for the neonatal survey from Neonatal Networks for East Midlands and Yorkshire and Humber regions).
Epice (Effective Perinatal Intensive Care in Europe) Research Group: BELGIUM: Flanders (E Martens, G Martens, P Van Reempts); DENMARK: Eastern Region (K Boerch, A Hasselager, L Huusom, O Pryds, T Weber); ESTONIA (L Toome, H Varendi); FRANCE: Burgundy, Ile‐de France and Northern Region (PY Ancel, B Blondel, A Burguet, PH Jarreau, P Truffert); GERMANY: Hesse (RF Maier, B Misselwitz, S Schmidt), Saarland (L Gortner); ITALY: Emilia Romagna (D Baronciani, G Gargano), Lazio (R Agostino, D DiLallo, F Franco), Marche (V Carnielli), M Cuttini; NETHERLANDS: Eastern & Central (C Koopman‐Esseboom, A Van Heijst, J Nijman); POLAND: Wielkopolska (J Gadzinowski, J Mazela); PORTUGAL: Lisbon and Tagus Valley (LM Graça, MC Machado), Northern region (Carina Rodrigues, T Rodrigues), H Barros; SWEDEN: Stockholm (AK Bonamy, M Norman, E Wilson); UK: East Midlands and Yorkshire and Humber (E Boyle, ES Draper, BN Manktelow), Northern Region (AC Fenton, DWA Milligan); INSERM, Paris (J Zeitlin, M Bonet, A Piedvache).
Bonnet C, Blondel B, Piedvache A, et al. Low breastfeeding continuation to 6 months for very preterm infants: A European multiregional cohort study. Matern Child Nutr. 2019;15:e12657 10.1111/mcn.12657
REFERENCES
- Akerstrom, S. , Asplund, I. , & Norman, M. (2007). Successful breastfeeding after discharge of preterm and sick newborn infants. Acta Paediatrica, 96(10), 1450–1454. 10.1111/j.1651-2227.2007.00502.x [DOI] [PubMed] [Google Scholar]
- Amissah, E. A. , Kancherla, V. , Ko, Y. A. , & Li, R. (2017). Validation study of maternal recall on breastfeeding duration 6 years after childbirth. Journal of Human Lactation, 33(2), 390–400. 10.1177/0890334417691506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ancel, P. Y. , Goffinet, F. , Group, E.‐W , Kuhn, P. , Langer, B. , Matis, J. , … Kaminski, M. (2015). Survival and morbidity of preterm children born at 22 through 34 weeks' gestation in France in 2011: Results of the EPIPAGE‐2 cohort study. JAMA Pediatrics, 169(3), 230–238. 10.1001/jamapediatrics.2014.3351 [DOI] [PubMed] [Google Scholar]
- Arnaud, C. , Daubisse‐Marliac, L. , White‐Koning, M. , Pierrat, V. , Larroque, B. , Grandjean, H. , … Kaminski, M. (2007). Prevalence and associated factors of minor neuromotor dysfunctions at age 5 years in prematurely born children: The EPIPAGE Study. Archives of Pediatrics & Adolescent Medicine, 161(11), 1053–1061. 10.1001/archpedi.161.11.1053 [DOI] [PubMed] [Google Scholar]
- Bernard, J. Y. , Armand, M. , Peyre, H. , Garcia, C. , Forhan, A. , De Agostini, M. , … Group, E. M.‐C. C. S (2017). Breastfeeding, polyunsaturated fatty acid levels in colostrum and child intelligence quotient at age 5‐6 years. The Journal of Pediatrics, 183, 43, e43–50. 10.1016/j.jpeds.2016.12.039 [DOI] [PubMed] [Google Scholar]
- Bonamy, A. , Zeitlin, J. , Piedvache, A. , Maier, R. , Heijst, A. , & Varendi, H. (2017). Wide variation in severe neonatal morbidity among very preterm infants in European regions. Archives of Disease in Childhood. Fetal and Neonatal Edition. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonet, M. , Blondel, B. , Agostino, R. , Combier, E. , Maier, R. F. , Cuttini, M. , … group, M. r (2011). Variations in breastfeeding rates for very preterm infants between regions and neonatal units in Europe: Results from the MOSAIC cohort. Archives of Disease in Childhood. Fetal and Neonatal Edition, 96(6), F450–F452. 10.1136/adc.2009.179564 [DOI] [PubMed] [Google Scholar]
- Bonet, M. , Forcella, E. , Blondel, B. , Draper, E. S. , Agostino, R. , Cuttini, M. , & Zeitlin, J. (2015). Approaches to supporting lactation and breastfeeding for very preterm infants in the NICU: A qualitative study in three European regions. BMJ Open, 5(6), e006973 10.1136/bmjopen-2014-006973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briere, C. E. , McGrath, J. , Cong, X. , & Cusson, R. (2014). An integrative review of factors that influence breastfeeding duration for premature infants after NICU hospitalization. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 43(3), 272–281. 10.1111/1552-6909.12297 [DOI] [PubMed] [Google Scholar]
- Callen, J. , & Pinelli, J. (2005). A review of the literature examining the benefits and challenges, incidence and duration, and barriers to breastfeeding in preterm infants. Advances in Neonatal Care, 5(2), 72–88. quiz 89‐92 [DOI] [PubMed] [Google Scholar]
- Cole, S. R. , & Hernan, M. A. (2008). Constructing inverse probability weights for marginal structural models. American Journal of Epidemiology, 168(6), 656–664. 10.1093/aje/kwn164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edmond, K. M. , Zandoh, C. , Quigley, M. A. , Amenga‐Etego, S. , Owusu‐Agyei, S. , & Kirkwood, B. R. (2006). Delayed breastfeeding initiation increases risk of neonatal mortality. Pediatrics, 117(3), e380–e386. 10.1542/peds.2005-1496 [DOI] [PubMed] [Google Scholar]
- Flacking, R. , Ewald, U. , Nyqvist, K. H. , & Starrin, B. (2006). Trustful bonds: A key to “becoming a mother” and to reciprocal breastfeeding. Stories of mothers of very preterm infants at a neonatal unit. Social Science & Medicine, 62(1), 70–80. 10.1016/j.socscimed.2005.05.026 [DOI] [PubMed] [Google Scholar]
- Flacking, R. , Ewald, U. , & Wallin, L. (2011). Positive effect of kangaroo mother care on long‐term breastfeeding in very preterm infants. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 40(2), 190–197. 10.1111/j.1552-6909.2011.01226.x [DOI] [PubMed] [Google Scholar]
- Flacking, R. , Nyqvist, K. H. , & Ewald, U. (2007). Effects of socioeconomic status on breastfeeding duration in mothers of preterm and term infants. European Journal of Public Health, 17(6), 579–584. 10.1093/eurpub/ckm019 [DOI] [PubMed] [Google Scholar]
- Flacking, R. , Wallin, L. , & Ewald, U. (2007). Perinatal and socioeconomic determinants of breastfeeding duration in very preterm infants. Acta Paediatrica, 96(8), 1126–1130. 10.1111/j.1651-2227.2007.00386.x [DOI] [PubMed] [Google Scholar]
- Forster, D. A. , McLachlan, H. L. , & Lumley, J. (2006). Factors associated with breastfeeding at six months postpartum in a group of Australian women. International Breastfeeding Journal, 1, 18 10.1186/1746-4358-1-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herich, L. C. , Cuttini, M. , Croci, I. , Franco, F. , Di Lallo, D. , Baronciani, D. , … Italian Effective Perinatal Intensive Care in Europe, N (2017). Maternal education is associated with disparities in breastfeeding at time of discharge but not at initiation of enteral feeding in the neonatal intensive care unit. The Journal of Pediatrics, 182(59–65), e57 10.1016/j.jpeds.2016.10.046 [DOI] [PubMed] [Google Scholar]
- Ikonen, R. , Paavilainen, E. , & Kaunonen, M. (2015). Preterm infants' mothers' experiences with milk expression and breastfeeding: An integrative review. Advances in Neonatal Care, 15(6), 394–406. 10.1097/ANC.0000000000000232 [DOI] [PubMed] [Google Scholar]
- Ip, S. , Chung, M. , Raman, G. , Chew, P. , Magula, N. , DeVine, D. , … Lau, J. (2007). Breastfeeding and maternal and infant health outcomes in developed countries. Evid Rep Technol Assess (Full Rep), 153, 1–186. [PMC free article] [PubMed] [Google Scholar]
- Killersreiter, B. , Grimmer, I. , Buhrer, C. , Dudenhausen, J. W. , & Obladen, M. (2001). Early cessation of breast milk feeding in very low birthweight infants. Early Human Development, 60(3), 193–205. [DOI] [PubMed] [Google Scholar]
- Kramer, M. S. , & Kakuma, R. (2002). Optimal duration of exclusive breastfeeding. Cochrane Database of Systematic Reviews, 1, CD003517 10.1002/14651858.CD003517 [DOI] [PubMed] [Google Scholar]
- Lechner, B. E. , & Vohr, B. R. (2017). Neurodevelopmental outcomes of preterm infants fed human milk: A systematic review. Clinics in Perinatology, 44(1), 69–83. 10.1016/j.clp.2016.11.004 [DOI] [PubMed] [Google Scholar]
- Lee, H. C. , & Gould, J. B. (2009). Factors influencing breast milk versus formula feeding at discharge for very low birth weight infants in California. The Journal of Pediatrics, 155(5), 657–662. e1‐2. 10.1016/j.jpeds.2009.04.064 [DOI] [PubMed] [Google Scholar]
- Li, R. , Darling, N. , Maurice, E. , Barker, L. , & Grummer‐Strawn, L. M. (2005). Breastfeeding rates in the United States by characteristics of the child, mother, or family: The 2002 National Immunization Survey. Pediatrics, 115(1), e31–e37. 10.1542/peds.2004-0481 [DOI] [PubMed] [Google Scholar]
- Li, R. , Scanlon, K. S. , & Serdula, M. K. (2005). The validity and reliability of maternal recall of breastfeeding practice. Nutrition Reviews, 63(4), 103–110. [DOI] [PubMed] [Google Scholar]
- Merewood, A. , Brooks, D. , Bauchner, H. , MacAuley, L. , & Mehta, S. D. (2006). Maternal birthplace and breastfeeding initiation among term and preterm infants: A statewide assessment for Massachusetts. Pediatrics, 118(4), e1048–e1054. 10.1542/peds.2005-2637 [DOI] [PubMed] [Google Scholar]
- Mizuno, K. , Nishida, Y. , Taki, M. , Hibino, S. , Murase, M. , Sakurai, M. , & Itabashi, K. (2007). Infants with bronchopulmonary dysplasia suckle with weak pressures to maintain breathing during feeding. Pediatrics, 120(4), e1035–e1042. 10.1542/peds.2006-3567 [DOI] [PubMed] [Google Scholar]
- Morag, I. , Harel, T. , Leibovitch, L. , Simchen, M. J. , Maayan‐Metzger, A. , & Strauss, T. (2016). Factors associated with breast milk feeding of very preterm infants from birth to 6 months corrected age. Breastfeeding Medicine, 11, 138–143. 10.1089/bfm.2015.0161 [DOI] [PubMed] [Google Scholar]
- Nye, C. (2008). Transitioning premature infants from gavage to breast. Neonatal Network, 27(1), 7–13. 10.1891/0730-0832.27.1.7 [DOI] [PubMed] [Google Scholar]
- Pinchevski‐Kadir, S. , Shust‐Barequet, S. , Zajicek, M. , Leibovich, M. , Strauss, T. , Leibovitch, L. , & Morag, I. (2017). Direct feeding at the breast is associated with breast milk feeding duration among preterm infants. Nutrients, 9(11). 10.3390/nu9111202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues, C. , Severo, M. , Zeitlin, J. , & Barros, H. (2017). The type of feeding at discharge of very preterm infants: Neonatal intensive care units policies and practices make a difference. Breastfeeding Medicine, 13, 50–59. 10.1089/bfm.2017.0135 [DOI] [PubMed] [Google Scholar]
- Rodrigues, C. , Teixeira, R. , Fonseca, M. J. , Zeitlin, J. , Barros, H. , & Portuguese, E. N. (2018). Prevalence and duration of breast milk feeding in very preterm infants: A 3‐year follow‐up study and a systematic literature review. Paediatric and Perinatal Epidemiology, 32, 237–246. 10.1111/ppe.12457 [DOI] [PubMed] [Google Scholar]
- Santoro Junior, W. , & Martinez, F. E. (2007). Effect of intervention on the rates of breastfeeding of very low birth weight newborns. Jornal de Pediatria, 83(6), 541–546. 10.2223/JPED.1724 [DOI] [PubMed] [Google Scholar]
- Schneider, S. L. (2011). The international standard classification of education In Class and stratification analysis (pp. 365–379). [Google Scholar]
- Scott, J. A. , & Binns, C. W. (1999). Factors associated with the initiation and duration of breastfeeding: A review of the literature. Breastfeeding Review, 7(1), 5–16. [PubMed] [Google Scholar]
- Sisk, P. M. , Lovelady, C. A. , Dillard, R. G. , Gruber, K. J. , & O'Shea, T. M. (2009). Maternal and infant characteristics associated with human milk feeding in very low birth weight infants. Journal of Human Lactation, 25(4), 412–419. 10.1177/0890334409340776 [DOI] [PubMed] [Google Scholar]
- Smith, V. C. , Zupancic, J. A. , McCormick, M. C. , Croen, L. A. , Greene, J. , Escobar, G. J. , & Richardson, D. K. (2004). Rehospitalization in the first year of life among infants with bronchopulmonary dysplasia. The Journal of Pediatrics, 144(6), 799–803. 10.1016/j.jpeds.2004.03.026 [DOI] [PubMed] [Google Scholar]
- Vohr, B. , McGowan, E. , McKinley, L. , Tucker, R. , Keszler, L. , & Alksninis, B. (2017). Differential effects of the single‐family room neonatal intensive care unit on 18‐ to 24‐month bayley scores of preterm infants. The Journal of Pediatrics, 185(42–48), e41 10.1016/j.jpeds.2017.01.056 [DOI] [PubMed] [Google Scholar]
- Vohr, B. R. , Poindexter, B. B. , Dusick, A. M. , McKinley, L. T. , Higgins, R. D. , Langer, J. C. , … Human Development National Research, N (2007). Persistent beneficial effects of breast milk ingested in the neonatal intensive care unit on outcomes of extremely low birth weight infants at 30 months of age. Pediatrics, 120(4), e953–e959. 10.1542/peds.2006-3227 [DOI] [PubMed] [Google Scholar]
- Wilson, E. , Edstedt Bonamy, A. K. , Bonet, M. , Toome, L. , Rodrigues, C. , Howell, E. A. , … Group, E. R (2017). Room for improvement in breast milk feeding after very preterm birth in Europe: Results from the EPICE cohort. Maternal & Child Nutrition, 14 10.1111/mcn.12485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zachariassen, G. , Faerk, J. , Grytter, C. , Esberg, B. , Juvonen, P. , & Halken, S. (2010). Factors associated with successful establishment of breastfeeding in very preterm infants. Acta Paediatrica, 99(7), 1000–1004. 10.1111/j.1651-2227.2010.01721.x [DOI] [PubMed] [Google Scholar]
- Zeitlin, J. , Bonamy, A. E. , Piedvache, A. , Cuttini, M. , Barros, H. , Van Reempts, P. , … Group, E. R (2017). Variation in term birthweight across European countries affects the prevalence of small for gestational age among very preterm infants. Acta Paediatrica, 106(9), 1447–1455. 10.1111/apa.13899 [DOI] [PubMed] [Google Scholar]
- Zeitlin, J. , Manktelow, B. N. , Piedvache, A. , Cuttini, M. , Boyle, E. , van Heijst, A. , … Group, E. R (2016). Use of evidence based practices to improve survival without severe morbidity for very preterm infants: Results from the EPICE population based cohort. BMJ, 354, i2976 10.1136/bmj.i2976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zou, G. Y. , & Donner, A. (2013). Extension of the modified Poisson regression model to prospective studies with correlated binary data. Statistical Methods in Medical Research, 22(6), 661–670. 10.1177/0962280211427759 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1: Comparison of proportions of children followed up at 2 years by maternal and neonatal characteristics and country, all infants eligible for follow‐up regardless of breastfeeding status
Table S2: Maternal and neonatal characteristics associated with breast milk feeding continuation until 6 months among all ever‐breastfed infants and among infants still breastfeeding at discharge – Unweighted models
Table S3: Maternal and neonatal characteristics associated with breast milk feeding continuation until 6 months among mothers of all ever breastfed infant and among mothers of infant still breastfeeding at discharge


