Abstract
Adenocarcinoma of the bowel is a dreadful sequelae of inflammatory bowel disease that can be difficult to diagnose and has been shown to have poor prognosis. The diagnosis is often made on histopathological examination of the resected specimen for what is suspected to be an exacerbation of the underlying intestinal Crohn’s. A 39-year-old woman who was being treated for small bowel Crohn’s disease for 4 years presented with features of intermittent intestinal obstruction that was refractory to medical therapy. A contrast CT of the abdomen was suggestive of ileocaecal Crohn’s disease, and colonoscopy revealed a stricture at proximal transverse colon with multiple superficial ulcers. She underwent a mesentery sparing right hemicolectomy and had an uneventful recovery. The biopsy, however, was reported to be moderately differentiated adenocarcinoma stage T3N0 with a harvest of four pericolic nodes. Adjuvant chemotherapy was advised, which she deferred. Ten months later, she presented to the emergency room with features of intestinal obstruction. Contrast CT of the abdomen showed thickening at the anastomotic site with intestinal obstruction. On exploratory laparotomy, tumour recurrence was noted at the site of the anastomosis and diffuse peritoneal metastasis. A palliative diversion ileostomy was done due to inoperable obstructing disease. She was then given palliative therapy and subsequently succumbed to the illness. The inclusion of mesentery with the resected specimen in Crohn’s disease has been a debate over many years. Since the preoperative diagnosis of carcinoma of the bowel in Crohn’s disease is challenging, all ileocolic resections should be radical as done in oncological resections. This would yield better oncological safety and may improve survival rates.
Keywords: crohn's disease, colon cancer, gastrointestinal surgery, surgical oncology
Background
Over the last several years, adenocarcinoma of the bowel has been increasingly associated with inflammatory bowel disease as one of the complications. The first case of small bowel carcinoma in Crohn’s was reported by Ginzburg in 1956. The incidence has been on a steady rise since then, and the exact magnitude of the burden is impossible to determine.1 The relative risk of developing carcinoma of the bowel in patients with Crohn’s disease ranges from 6 to 320.1–3 Although the need to screen the patients with Crohn’s disease for carcinoma is well recognised, it is difficult to diagnose. Surgical interventions are done for what is believed to be an exacerbation or refractory to medical therapy.4 Unfortunately, the diagnosis is often made on histopathology of the resected specimen. The main debate in surgical resection of Crohn’s is whether the mesentery should be included as part of the specimen.4
In this case report, we describe a middle-aged woman with Crohn’s disease who underwent a conservative right hemicolectomy for a suspected exacerbation with ileocaecal intestinal obstruction. The histopathology was however conclusive of adenocarcinoma. She had a local recurrence and peritoneal metastasis within a year after the surgery. We believe that inadequate radicality and lymphadenectomy during the index operation led to the recurrence and dissemination of cancer. The clinical details, investigations and treatment have been described with a relevant review of the literature.
Case presentation
A 39-year-old woman with no known comorbid illnesses presented with complaints of recurrent abdominal pain and vomiting associated with loss of weight and appetite. She was diagnosed to have Crohn’s disease 4 years before this presentation in another centre for which she was being treated with mesalazine 1.2 g twice daily. She had recurrent episodes of abdominal pain, which was intermittent colicky in nature and was confined around the umbilicus. She also had multiple episodes of bilious vomiting. There was no history of jaundice, haematemesis, melena or bleeding per rectum. She had undergone an open appendicectomy at 14 years of age. There were no similar complaints, and there was no history of colorectal or urogynaecological malignancy in her family.
On examination, the vital parameters were within normal limits. Her general physical examination was unremarkable. On examination of the abdomen, there was mild distention, and fullness was noted over the right lumbar region. In the umbilical and right lumbar regions, there was an intraperitoneal mass palpable, which was tender and was firm to hard in consistency. Her bowel sounds were exaggerated, and the digital rectal examination was normal.
Investigations
Her routine blood tests were within normal limits (table 1). She underwent a colonoscopy, which revealed a stricture in the proximal transverse colon with a near-complete luminal compromise. There were a few superficial ulcers along the luminal opening, and the mucosa of the transverse colon was erythematous. The biopsy from the lesion was suggestive of a tubulovillous lesion with a high-grade dysplasia with background features suggestive of inflammatory bowel disease. A contrast-enhanced CT of the abdomen and pelvis was done, which showed a circumferential enhancing mural thickening of the terminal ileum and ileocaecal junction with surrounding fat stranding (figure 1). There was ahaustral ascending and transverse colon with mural thickening at the hepatic and splenic flexure. These features were also suggestive of inflammatory bowel disease.
Table 1.
Relevant laboratory investigations
| Tests | Results |
| Complete blood count | Hb: 10.8 g/dL, WBC: 8500/mm3, platelets: 3.23 L/mm3 |
| CRP | 6.05 mg/L (<6) |
| ESR | 38 at 60 min |
| Faecal calprotectin | 1829 µg/g (positive) |
| Albumin | 4.4 g/dL |
| CEA | 0.82 (<5) |
CEA, Carcinoembryonic antigen; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; Hb, Haemoglobin; WCC, white cell count.
Figure 1.
Circumferential mural thickening of terminal ileum with annular narrowing of ileocaecal junction and ahaustral ascending and transverse colon with mural thickening of hepatic and splenic flexure.
Treatment
After a discussion in the multidisciplinary inflammatory bowel disease meeting, she was planned for surgical intervention with suspicion of exacerbation of Crohn’s disease with recurrent intestinal obstruction.
Intraoperatively, there was an ileocaecal mass with obstruction and features of creeping fat over the transverse colon. The rest of the bowel and solid viscera were normal. A mesentery sparing right hemicolectomy was done by dividing the mesocolon close to the bowel with an inadequate lymph nodal harvest. As a result, the operation was not within the principles of oncological safety. An end to side ileocolic anastomosis was done. Postoperatively, she recovered well and was subsequently discharged in a stable condition.
To the surprise of the treating team, the biopsy of the specimen was reported to be moderately differentiated adenocarcinoma T3N0 with necrotising granulomatous inflammation. Only four pericolic lymph nodes were harvested that were free of tumour. After rediscussion in a multidisciplinary IBD meeting, she was offered adjuvant chemotherapy and to continue mesalazine since azathioprine was not recommended after the diagnosis of cancer.
Outcome and follow-up
The patient presented to the emergency department 10 months later with intestinal obstruction and after having defaulted the chemotherapy. A contrast CT of the abdomen showed features of recurrence at the anastomotic site and peritoneal disease (figure 2). She underwent an emergency exploratory laparotomy for persistent acute intestinal obstruction and was found to have inoperable hard mass at the site of the previous ileocolic anastomosis with multiple nodules over the small bowel mesentery, peritoneum and the liver. In view of the metastatic nature of the disease, a palliative loop ileostomy was done, and the patient was subsequently discharged. She was advised palliative chemotherapy with FOLFOX regimen, but she succumbed 3 months after discharge.
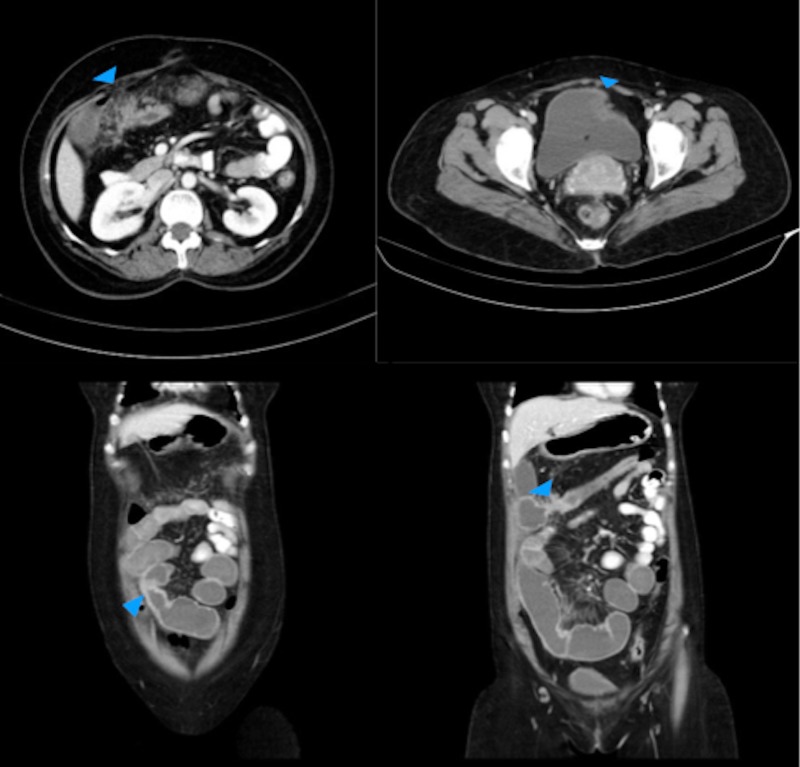
Figure 2.
Postoperative right hemicolectomy with thickening at the site of anastomosis, pericolic nodular fat stranding involving the omentum and mesentery, peritoneal thickening in the pouch of Douglas and anterior wall of rectum.
Discussion
The prognosis of intestinal carcinoma occurring from an underlying Crohn’s disease has been noted to be poorer than the de novo carcinomas.5 The diagnosis is often challenging as they present at a younger age and are more diffuse and distally located. Almost two-thirds of the patients present with intestinal obstruction that can masquerade as an exacerbation of Crohn’s disease.1 Fifty-nine to seventy per cent of the carcinomas are incidentally detected during histopathological examination of the resected surgical specimens.1 Two-year survival rates were abysmal and was found to be as low as 27%, which may be attributed to non-adherence to principles of oncological safety during the surgery and poorly differentiated grade of cancers.5 6
The treatment of choice is radical resection of the involved segment of the bowel including the corresponding mesentery and lymph nodes. The main dilemma during the operation for ileocolic Crohn’s disease when the diagnosis of carcinoma is uncertain is whether the mesentery should be included in the resected specimen. The recent advances conclude that the surgical recurrence in Crohn’s disease is significantly less when mesentery is excised.7 8 However, the decision to proceed with bowel resection including the mesentery in the surgical specimen should be balanced carefully considering difficulty in haemostasis due to severe mesenteric disease resulting in thickened or friable mesentery.
While many studies support the inclusion of mesentery in resections for Crohn’s disease, some suggest that the mesenteric changes like fat wrapping are immunologically protective.9 10 If this is true, then radical resection of mesentery could lead to poor clinical outcomes. On the contrary, excision of the mesentery results in a better lymphadenectomy, which finally reduces immunological inputs and improved postoperative outcomes.11 This debate does not arise when the diagnosis of carcinoma is made before surgical resection. However, the challenge lies when the diagnosis is uncertain, or surgical intervention is planned for a suspected exacerbation of Crohn’s disease.12 There is an ongoing international multicentre randomised clinical trial comparing mesenteric excision surgery versus conservative limited resection in Crohn’s disease, which hopefully would address the issue of radicality of bowel resection in Crohn’s disease.13 The intraoperative findings are seldom helpful in differentiating a carcinoma from the features of Crohn’s disease. Our patient underwent a right hemicolectomy for a suspected exacerbation of Crohn’s disease involving the ileocaecal region with no features suspicious of a malignancy intraoperatively. Hence, a mesentery-sparing ileocolic resection was performed, which resulted in a less radical resection and inadequate lymph nodal clearance. Consequently, there was local disease recurrence and peritoneal metastasis within a year. Although lack of adjuvant chemotherapy could have contributed to the recurrence, the fact that the surgical resection was not oncologically adequate cannot be disregarded.
Learning points.
Adenocarcinoma of the bowel is a rare but undeniable complication of Crohn’s disease and has a poorer prognosis compared with de novo adenocarcinoma of the bowel.
The diagnosis is challenging preoperatively and is often made after histopathological examination of the resected specimen.
Inadequate radical bowel resection and lymph nodal clearance of ileocolic disease in the background of Crohn’s disease may be associated with disease recurrence.
Mesentery sparing bowel resection should be avoided in Crohn’s disease even if the suspicion of malignancy is low.
A radical bowel resection results in better oncological outcome and should be the standard of care.
Footnotes
Contributors: GV and AKD identified the complexity of the case and need for reporting. RD and GV were involved in the preparation of the manuscript and review of the literature. DRK contributed in providing the appropriate radiological images and reporting of the same.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Parental/guardian consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Cahill C, Gordon PH, Petrucci A, et al. Small bowel adenocarcinoma and Crohn's disease: any further ahead than 50 years ago? World J Gastroenterol 2014;20:11486–95. 10.3748/wjg.v20.i33.11486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ribeiro MB, Greenstein AJ, Heimann TM, et al. Adenocarcinoma of the small intestine in Crohn's disease. Surg Gynecol Obstet 1991;173:343–9. [PubMed] [Google Scholar]
- 3.von Roon AC, Reese G, Teare J, et al. The risk of cancer in patients with Crohn's disease. Dis Colon Rectum 2007;50:839–55. 10.1007/s10350-006-0848-z [DOI] [PubMed] [Google Scholar]
- 4.Greenstein AJ. Cancer in inflammatory bowel disease. Mt Sinai J Med 2000;67:227–40. [PubMed] [Google Scholar]
- 5.Kerber GW, Frank PH. Carcinoma of the small intestine and colon as a complication of Crohn disease: radiologic manifestations. Radiology 1984;150:639–45. 10.1148/radiology.150.3.6695061 [DOI] [PubMed] [Google Scholar]
- 6.Dossett LA, White LM, Welch DC, et al. Small bowel adenocarcinoma complicating Crohn's disease: case series and review of the literature. Am Surg 2007;73:1181–7. [PubMed] [Google Scholar]
- 7.Coffey JC, O'Leary DP. The mesentery: structure, function, and role in disease. Lancet Gastroenterol Hepatol 2016;1:238–47. 10.1016/S2468-1253(16)30026-7 [DOI] [PubMed] [Google Scholar]
- 8.Coffey JC, Dockery P. Colorectal cancer: surgery for colorectal cancer - standardization required. Nat Rev Gastroenterol Hepatol 2016;13:256–7. 10.1038/nrgastro.2016.40 [DOI] [PubMed] [Google Scholar]
- 9.Olivier I, Théodorou V, Valet P, et al. Is Crohn's creeping fat an adipose tissue? Inflamm Bowel Dis 2011;17:747–57. 10.1002/ibd.21413 [DOI] [PubMed] [Google Scholar]
- 10.Rodrigues VS, Milanski M, Fagundes JJ, et al. Serum levels and mesenteric fat tissue expression of adiponectin and leptin in patients with Crohn's disease. Clin Exp Immunol 2012;170:358–64. 10.1111/j.1365-2249.2012.04660.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Coffey CJ, Kiernan MG, Sahebally SM, et al. Inclusion of the mesentery in ileocolic resection for Crohn’s disease is associated with reduced surgical recurrence. J Crohn’s Colitis 2018;12:1139–50. 10.1093/ecco-jcc/jjx187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feldstein RC, Sood S, Katz S. Small bowel adenocarcinoma in Crohn's disease. Inflamm Bowel Dis 2008;14:1154–7. 10.1002/ibd.20393 [DOI] [PubMed] [Google Scholar]
- 13.Li Y, Mohan H, Lan N, et al. Mesenteric excision surgery or conservative limited resection in Crohn’s disease: study protocol for an international, multicenter, randomized controlled trial. Trials 2020;21 10.1186/s13063-020-4105-x [DOI] [PMC free article] [PubMed] [Google Scholar]