Abstract
Heart failure (HF) with preserved ejection fraction (HFpEF) is the most common form of HF in patients older than 65 years. Among elderly women living in the community, HFpEF comprises nearly 90% of incident HF cases. The health and economic impact of HFpEF is at least as great as that of HF with reduced ejection fraction (HFrEF), with similar severity of acute hospitalization rates and substantial mortality. Despite the importance of HFpEF, our understanding of its pathophysiology is incomplete, and optimal treatment remains largely undefined. Unlike the management of HFrEF, there is a paucity of large evidence-based trials demonstrating morbidity and mortality benefit for the treatment of HFpEF. The agents tested in trials to date, which were based upon an incomplete understanding of the pathophysiology of HFpEF, have not been positive. There is an urgent need to understand HFpEF pathophysiology as well as focus on developing novel therapeutic targets.
Keywords: Heart failure, Preserved ejection fraction, Management
Introduction
Heart failure (HF) with preserved ejection fraction (HFpEF) is the most common form of HF in patients older than 65 years.1 Among elderly women living in the community, HFpEF comprises nearly 90% of incident HF cases.2 The health and economic impact of HFpEF is at least as great as that of HF with reduced ejection fraction (HFrEF), with similar severity of acute hospitalization rates, and substantial mortality.3;4 Despite the importance of HFpEF, our understanding of its pathophysiology is incomplete and optimal treatment remains largely undefined. There is an urgent need to focus on drug and device development for HFpEF as well as to understand HFpEF pathophysiology. Here, we provide an overview of emerging treatments that are being tested in clinical trials in humans and novel therapeutic targets that may arise from advances in understanding pathophysiology of HFpEF.
Epidemiology of HFpEF
HFpEF is the predominant form of HF in older adults, increasing in prevalence as the population ages. In contrast to HFrEF, the prevalence of HFpEF is increasing and its prognosis is worsening.3 By 2020, the relative prevalence of HFpEF and HFrEF are predicted to be 69% and 31% turning HFpEF into the most common HF phenotype (Table 1).5 In westernized countries, HFpEF patients are older, predominantly female,1 and with a high prevalence of hypertension (HTN), obesity, diabetes, and atrial fibrillation (AF).1;6–10 The combined mortality and readmission rates 60–90 days post-discharge are comparable for HFrEF (36.1%) and HFpEF (35.3%).8 Non-cardiovascular hospital readmissions and mortality are more frequent in HFpEF than in HFrEF and the number of co-morbidities correlate with increased all-cause hospitalization and mortality.11
Table 1.
Epidemiology of HFpEF
| Prevalence | 40–71% (1.1–5.5% of the general population)1;3;155 |
| Incidence | 52.3% ( 2008–2010), decreased from 56.9% from 2004–2007156 |
| All-cause Mortality | In –hospital : 3–6.5%8;157;158
Short -term (30–90 days) : 5–9.5% 6;8 Long term (5 years)mortality : 55–74%159–161 Annual mortality rate from 3.5 to 15%52–54 |
| Overall mortality related to non-cardiovascular causes | 30–49%52;54;159;160 |
| One-year rate of readmission | 13.5%6 |
| Combined mortality and readmission rates at 60–90 days | 35.3%8 |
| One-year combined death and readmission for HF | 31.1%6 |
| Long term HF readmission | Increased from 33–39%3 |
| 5-year health care cost | $ 32 5807 |
HFpEF=heart failure with preserved ejection fraction; HF=heart failure
Brief introduction to pathophysiology of HFpEF
One of the most commonly cited mechanisms of HFpEF is left ventricular (LV) diastolic dysfunction consisting of abnormal LV active relaxation as well as increased LV passive stiffness.12 Myocardial stiffness is not just related to cardiomyocyte stiffness but also to extracellular matrix changes, which in turn are determined by the amount of collagen and the extent of collagen cross-linking.13 In HFpEF patients, excessive collagen type I deposition may result from an imbalance between exaggerated synthesis and depressed degradation and decreased matrix degradation because of down regulation of matrix metalloproteinases (MMPs) and up regulation of tissue inhibitors of matrix metalloproteinases (TIMPs).14;15 In addition, increases cardiac myocyte stiffness in HFpEF appears mediated in part by hypophosphorylation of titin, related to cyclic guanosine monophosphate (GMP) deficiency from increased nitroso- oxidative stress.13
Significant LV hypertrophy was previously thought to be a uniform characteristic of HFpEF. However, some HFpEF patients have concentric remodeling without hypertrophy or even normal LV geometry.16–18 In addition, the magnitude of increase in fibrosis in HFpEF patients appears modest.19 Data from multiple sources indicate that even in well-characterized, symptomatic HFpEF, many patients do not have echo-Doppler indexes of diastolic dysfunction, at least at rest, that differ greatly from that expected based on age and comorbidities.20;21 Our recent understanding of HFpEF indicates that abnormalities of intrinsic diastolic function are important, other factors contribute significantly as well.
Several studies from both animals and humans showed that additional mechanisms play important roles, such as LV systolic dysfunction,17;22;23 impaired systolic reserve in both LV and right ventricle (RV),24 autonomic dysfunction,25 cardiac aging,26;27 neuroendocrine dysfunction,28;29 left atrial (LA) dysfunction, impaired resting pulmonary arterial (PA) and RV function, abnormal PA vasodilatory reserve as well as abnormal RV-PA coupling,24;30–32 impaired heart rate (HR) recovery and chronotropic incompetence (CI),25;25;33 abnormal ventricular vascular coupling,16;34reduced vasodilator reserves25;33 and altered pulmonary function and gas exchange including low diffusion capacity.35;36
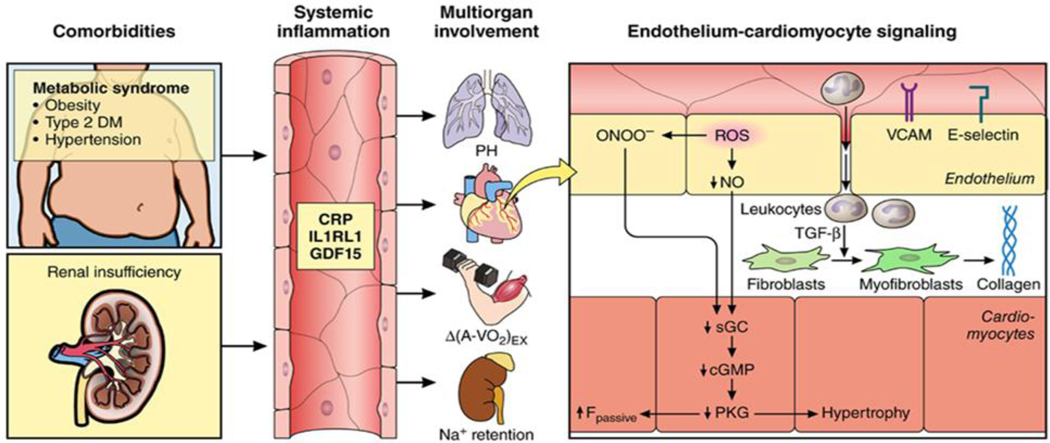
Recently the concept of HFpEF has evolved from a ‘cardio-centric’ model to a syndrome that may involve multiple cardiovascular and non-cardiovascular mechanisms. Findings to date indicate important contributions from skeletal muscle dysfunction,37–39 pulmonary and renal dysfunction1;2;40 and multiple comorbidities11 including obesity, HTN, diabetes, AF and anemia. Paulus and Tschope proposed that comorbidities and especially obesity induce a systemic inflammatory state, which induces oxidative stress in the coronary microvascular endothelium (Figure 1).This reduces myocardial nitric oxide (NO) bioavailability and leads to reduced protein kinase G (PKG) activity in cardiomyocytes, which therefore become stiff and hypertrophied.13 This is further exacerbated by cardiac aging which is associated with a systemic proinflammatory state, increasing cytokines levels,41–43 that may lead to functional declines in multiple organs.44 The impact of multiple comorbidities typical of older HFpEF patients further promotes phenotypic heterogeneity and multi-factorial pathophysiology. Although this complexity presents challenges, it also presents opportunities for advancing our understanding and provides potentially novel therapeutic targets. In this review, we mainly focus on current and potential novel treatments for HFpEF in relation to evolving key concepts.
Figure 1.
Systemic and myocardial signaling in HFpEF. Comorbidities induce systemic inflammation, evident from elevated plasma levels of inflammatory biomarkers such as soluble interleukin 1 receptor-like 1 (IL1RL1), C-reactive protein (CRP), and growth differentiation factor 15 (GDF15). Chronic inflammation affects the lungs, myocardium, skeletal muscle, and kidneys leading to diverse HFpEF phenotypes with variable involvement of pulmonary hypertension (PH), ocardia re ode in , de icient s e eta usc e ox en extraction (ΔA-Vo2) during exercise (Ex), and renal Na+ retention. Myocardial remodeling and dysfunction begins with coronary endothelial microvascular inflammation manifest from endothelial expression of adhesion molecules such as vascular cell adhesion molecule (VCAM) and E-Selectin. Expression of adhesion molecules attracts infiltrating leukocytes secreting transforming growth actor β (TGF-β), w ic con erts ibrob asts to o ibrob asts wit en anced interstitia co a en deposition. Endothelial inflammation also results in the presence of reactive oxygen species (ROS), reduced nitric oxide (NO) bioavailability, and production of peroxynitrite (ONOO–). This reduces soluble guanylate cyclase (sGC) activity, cyclic guanosine monophosphate (cGMP) content, and the favorable effects of protein kinase G (PKG) on cardiomyocyte stiffness and hypertrophy. HFpEF indicates heart failure with preserved ejection fraction. Reproduced from Circulation with permission. Circulation. 2016; 134:73–90.
Management
Current guidelines
Current guidelines for the management of HFpEF recommend management of volume status with appropriate diuretic dosing, control of blood pressure (BP), management of comorbidities, and dietary education.45 The 2013 American College of Cardiology Foundation/American Heart Association (ACCF/AHA) HF guidelines indicate that systolic and diastolic HTN should be controlled in accordance with published clinical practice guidelines to prevent morbidity and diuretics should be used to relieve symptoms due to volume overload (Class I with level of evidence B).45 ACCF/AHA HF guidelines support the use of beta-blockers, angiotensin converting enzyme inhibitor (ACEI), and angiotensin receptor blockers (ARBs) for HTN (IIa recommendation, level of evidence C) and recommend ARBs be considered to decrease hospitalizations (IIb recommendation).45 Beta-blockers are recommended for HFpEF patients with a history of myocardial infarction (MI), HTN, or AF. The European Society of Cardiology (ESC) guidelines have similar recommendations.46
Pharmacological interventions
Traditional pharmacotherapies: What is the evidence?
Targeting the renin–angiotensin–aldosterone system (RAAS)
ACE inhibitors and ARBs:
Targeting the RAAS pathways has long been considered a logical intervention for HFpEF, based on animal models as well as human hypertensives without HF and its link to LV hypertrophy, interstitial fibrosis and fluid imbalance.47–50 Angiotensin II promotes LV hypertrophy and fibrosis, both of which are contributors to HFpEF, as well as vasoconstriction and vascular remodeling.51 By blocking the formation of angiotensin II, ACE inhibitors are a potential target for HFpEF treatment. Similarly ARBs exert their effect further downstream and block the association of angiotensin II with its receptor.
Table 2 summarizes the important randomized trials. Of the three large randomized trials of ACEI/ARB performed to date in HFpEF, only the CHARM-Preserved study found nominal benefit for candesartan in reducing HF hospitalizations over three years of follow-up.52–54 However, most importantly, none of the trials showed benefit for their pre-planned primary endpoints.52–54 Kitzman et al showed no improvement in exercise capacity or quality of life with enalapril.55 In a small study of 74 elderly patients with HFpEF, quinapril failed to demonstrate improvement in exercise tolerance, quality of life, or hospitalizations.56
Table 2.
Summary of important randomized trials
| First Author/Trial (Ref.#) | Intervention | HFpEF Patient Type | Primary Endpoint | Trial Result |
|---|---|---|---|---|
| CHARM-Preserved 52 | Candesartan | ≥ 18 s/NYHA c ass II–IV HF | CV death or HF admission | Fewer HF admissions |
| The PEP-CHF 53 | Perindopril | ≥70 s/dia nosis o HF and treated with diuretics and an Echo-DD | All-cause mortality and HF admission | Fewer HF admissions |
| I-PRESERVE54 | Irbesartan | ≥ 60 s/ ospita ized or HF during the previous 6 months and have current NYHA class II-IV symptoms | Death from any cause or hospitalization for a CV cause | Neutral |
| Kitzman et al.55 | Enalapril | Elderly(70±1 ys), predominant female (80%) with compensated HF | Peak VO2 and 6 MWD | Neutral |
| TOPCAT60 | Spironolactone | ≥ 50 s, S pto atic HF. Patients had a h/o HF hospitalization within previous 12 months and elevated BNP within 60 days before randomization | CV death or aborted cardiac arrest, HF hospitalization | Neutral |
| Aldo-DHF57 | Spironolactone | ≥ 50 s a bu ator patients/NYHA class II–III symptoms, grade1 DD and normal or near-normal BNP levels | Peak VO2, c an e in E/e’ | Neutral |
| RAAM-PEF58 | Eplerenone | Elderly, symptomatic NYHA class II/III, increased BNP within 60 days | 6MWD | Neutral |
| J DHF63 | Carvedilol (lowdose) | ≥ 20 ys/ambulatory patients with NYHA class II–III symptoms, grade I DD, and normal or near-normal BNP levels | Death or HF hospitalization | Neutral |
| ELANDD64 | Nebivolol | ≥ 40 s/ a bu ator patients with NYHA class II–III symptoms, grade I DD, and normal or near-normal BNP levels | 6 MWD | Neutral |
| NEAT-HFPEFtrial68 | Isosorbide Mononitrate | ≥ 50 s/ a bu ator HF patients, prior hospitalization for HF within 12 months or increased invasively measured LV filling pressure or elevated BNP or echo-DD | Daily activity level, 6MWD | Neutral |
| RELAX68;84 | Sildenafil | capacity | Peak VO2 | Neutral |
| DILATE −190 | Riociguat | ≥ 18 s/ stab e s pto atic HF, ean PAP≥ 25 o Hg and PCWP > 15 mm of Hg | Change in mean PAP | Neutral |
| Little et al99 | Alagebrium chloride | > 65 ys , stable ambulatory NYHA class II/III | Peak VO2 | Neutral |
| RALI-DHF98 | Ranolazine | NYHA class II–III HF, Echo-DD, NT-pro BNP > 220 p / , restin L EDP ≥ 18 mm of Hg | LVEDP, PCWP | Some improvement in hemodynamics |
| Zile et al101 | Sitaxsentan | NYHA class II–III HF, Echo-DD | Change in treadmill exercise time | Positive |
| PARAMOUNT 71 | LCZ696(ARNI) | ≥ 40 s/NYHA c ass II–III HF, NT-pro BNP > 400 pg/nl and be on a diuretic therapy | Change in NT-proBNP | Positive |
| Kosmala et al88 | Ivabradine | ≥ 50 s/ ambulatory patients with NYHA class II–III symptoms, grade I DD, and normal or near-normal BNP levels | Peak VO2, Pea E/e’ | Positive |
| Kitzman et al115 | Exercise training | ≥ 60 s/A bu ator HF patients with NYHA class II–III symptoms | Peak VO2 | Positive |
| Kitzman et al114 | Caloric restriction and exercise training | ≥ 60 s/A bu ator HF patients with NYHA class II–III symptoms | Peak VO2 and Quality of Life | Positive |
| CHAMPION147 | CardioMEMs sensor | ≥ 18 s, NYHA c ass III HF, hospitalization for HF in last 12 months, | HF hospitalization | Positive |
HFpEF = heart failure with preserved ejection fraction; NYHA= New York heart association; CV=cardiovascular; HF=heart failure; DD=diastolic dysfunction; VO2= oxygen consumption; MWD=minute walk distance; BNP=B-type natriuretic peptide; E= Mitra early diastolic velocity; e’=mitral annular velocity; ARNI = angiotensin receptor-neprilysin inhibitor; PAP=pulmonary artery pressure; PCWP=pulmonary capillary wedge pressure. LVEDP=left ventricular end diastolic pressure
Aldosterone antagonists:
Aldosterone can promote interstitial collagen deposition and fibrosis, leading to ventricular stiffness and its inhibition might be expected to reduce the ventricular-vascular stiffening and diastolic dysfunction. In Aldo-DHF, patients who received spironolactone 25 mg daily showed improved some measures of diastolic dysfunction but there was no improvement in exercise capacity, patient symptoms, or quality of life.57 The RAAM-PEF trial of 6 months treatment of eplerenone vs. placebo, showed reductions in circulating markers of collagen turnover and modest improvements in diastolic function.58 In addition to this, in the OPTIMIZE-HF registry, aldosterone antagonists had no effect on all-cause mortality or hospitalization.59 In the large TOPCAT trial, spironolactone failed to show statistically significant benefit for the clinical composite primary end -point. A modest decline in hospitalizations was observed.60 However, a post hoc regional analysis indicated that the cohort from the Americas most closely matched characteristics observed in other randomized trials and also appeared most responsive to spironolactone.61
Targeting the β-adrenergic stimulation pathways
Beta-blockers:
Slowing the HR should result in an increase in the diastolic filling period in an abnormally stiff LV, thus potentially allowing greater filling of LV. Although a small early study of propranolol suggested a reduction in total mortality when compared to no propranolol, the patient group was atypical in that all were selected to have prior MI and were mostly men, and he EF was as low as 40%.62 In addition, there was no significant difference in cardiac deaths between these groups. Both carvedilol (the J-DHF study) and nebivolol (ELANDD study) had neutral effects on their primary outcomes in HFpEF patients.63;64 In the OPTIMIZE-HF registry, discharge use of beta-blockers appeared to exert no effect on 1 year mortality or hospitalization rates of HFpEF patients.65
Calcium channel blockers:
In a small, early study of 20 men, verapamil showed improvement in baseline HF score, treadmill exercise capacity and LV peak filling rate from baseline compared to placebo;66 however this study is difficult to extrapolate to a general HFpEF population given its small sample size and entirely male population. Digoxin: In the Digitalis Interaction Group, a subgroup of 988 patients with EF > 45% was randomized to placebo or to digoxin. There were no significant reductions in the amount of hospitalizations or mortality secondary to HF, although trends towards decreased hospitalization and improved exercise tolerance were noted.67 Of note, the majority of HFpEF patients in the DIG trial had HF related to an ischemic etiology (56%), and as such, these results may not be applicable to typical HFpEF patients encountered in the community. Nitrates: In NEAT-HFpEF, isosorbide mononitrate did not improve 6 minute walk distance (MWD), quality-of-life scores, or NT-pro Btype natriuretic peptide (BNP) levels compared to placebo.68 Even though, this result may appear to speak against the importance of NO deficiency in HFpEF, there are number of caveats. Organic nitrates tonically release NO, so there is not targeted delivery at the time of greatest need. In addition, organic nitrates can have pharmacological tolerance and are associated with development of endothelial dysfunction. Two recently reported randomized studies showed that intravenous or inhaled sodium nitrite improved CO reserve, LV stroke work and biventricular filling pressures and PA pressures at rest and during exercise in HFpEF.69;70 Beneficial effects are thought to be related to enhanced production of NO by nitrites in the setting of tissue hypoxia and acidosis induced by exercise. These trials led to the launch of 2 clinical trials sponsored by the NHLBI (NCT02742129 and NCT02713126)
Why Did These Traditional Therapies Not Show Benefit in HFpEF?
To date, trials have largely targeted solely targets previously thought to be specific to and universally present in HFpEF, such as LVH, diastolic dysfunction, and other features. However more recent data have challenged these assumptions. In a recent PARAMOUNT trial of well characterized HFpEF patients, only 8% of patients had LVH at baseline and 50% had significant or severe diastolic function at rest.71 With treatment, even though there was a positive signal on BNP, there was no difference in LV mass. Similarly Maurer and colleagues found no significantly increased LV mass in older HFpEF patients compared to controls with HTN but not HF.40;72 This indicates LV hypertrophy may not be a universal aspect of HFpEF as previously assumed. Studies of patients with all the clinical hallmarks of HF and an EF>50% showed that many patients appear to have modest diastolic dysfunction under resting conditions.71;73 Most HFpEF trials measured diastolic or other cardiovascular measures at rest and not during exercise. This might help explain why agents that had a proven ability to ameliorate LV hypertrophy, fibrosis, and other cardiac abnormalities typically found in HFpEF have not led to positive outcomes.
Chronotropic incompetence, abnormally low HR at peak exercise, is perhaps the most consistently reported cardiac abnormality during exercise in HFpEF.25;74;75 In addition, there is a high prevalence of CI in HFpEF, and limitations in chronotropic reserve might be a key factor to reduce CO and exercise capacity.75;76 In some studies, CI is the only mechanism accounting for reduced CO during exercise in HFpEF and the primary or sole cardiac contributor to exercise intolerance.77 β-Blockers may result in pharmacologically induced CI and obscure identification of an underlying intrinsic abnormality in neural balance.78 In addition, unfavorable effect of beta-blockers on chronic obstructive pulmonary disease and diabetes could complicate the overall effect of these drugs in HFpEF patients with such conditions.79–81
The neutral outcomes were often attributed to patient recruitment with inclusion of many HFrEF or non-cardiac patients or nonadherence to diagnostic guidelines.13 For example, in TOPCAT trial, neutral outcome in the overall population has been attributed to aberrant patient enrollment in Russia/Republic of Georgia rather than to inefficacy of spironolactone.61 Recently evidence indicates that HFpEF is a systemic disorder, in addition to the heart, and also involves important contributions from peripheral abnormalities of vascular and skeletal muscle function that have not been addressed in trials to date. Perhaps most prominently, HFpEF is strongly influenced by aging, a progressive process affecting all organ systems, including the heart and arterial system, those most implicated in HFpEF. Aging and the associated comorbidities may initiate and/or aggravate chronic systemic inflammation that may affect myocardial remodeling and dysfunction in HFpEF through a signaling cascade, which begins with coronary microvascular endothelial dysfunction (Figure 1).13;82 Finally, multiple comorbidities, including non-cardiovascular co-morbidities, may play a much greater role in the development of symptoms and treatment response than previously recognized.
Novel pharmacotherapies (Summarized in Table 2)
Sildenafil is an inhibitor of phosphodiesterase-5 that increases cGMP levels by blocking catabolism, thus augmenting PKG activity in multiple organs relevant to HF. Increased availability of cGMP could provide benefits for both vascular and myocardial remodeling, including attenuating hypertrophy, fibrosis, and impaired cardiac relaxation.83 In the RELAX trial, sildenafil did not improve 6 MWD or quality of life, and was associated with modest worsening of renal function and increases in neurohormone levels.84 In a small trial of patients with HFpEF and PA systolic pressure (PASP) >40 mmHg sildenafil group demonstrated improvements in PASP and vasomotility, RV function and dimension, LV relaxation and distensibility.85 Another small, single-center trial examined the use of sildenafil in 52 patients with pulmonary hypertension due to HFpEF. There was no significant difference in mean PA pressure at 12 weeks, as well as other hemodynamic parameters included pulmonary arterial wedge pressure, CO and peak oxygen consumption (VO2).86 Neprilysin inhibitors: Neprilysin is a zincdependent metalloprotease that degrades biologically active natriuretic peptides and does not affect the biologically inactive NTproBNP.71 LCZ696 is a new combination drug of the angiotensin II type-1 receptor blocker valsartan and the neprilysin inhibitor prodrug AHU377. This dual combination exerts a powerful vasodilatory and natriuresis effect by blocking angiotensin II activity on the one hand, although augmenting plasma levels of natriuretic peptides, such as BNP, on the other. In PARAMOUNT study, the LCZ696 group had significantly lower NT-pro BNP levels and at 36 weeks, decreased LA size and showed a trend toward improved functional class.71 The promising findings of this phase-2 study led to an ongoing large, multi-center trial, PARAGON, which is comparing LCZ696 to valsartan in patients with HFpEF with the primary composite outcome of cardiovascular death or first hospitalization for HF. The estimated completion date for this trial is May 2019 (ClinicalTrials.gov NCT01920711). Ivabradine is a selective sinus node If sodium channel inhibitor that reduces HR without affecting contractility or lusiotropy. The theory that patients with HFpEF may have detrimental effects from high HR rate during exercise due to reduced time for diastolic filling has led to interest in ivabradine for HFpEF. In a diabetic mouse model of HFpEF, ivabradine reduced aortic stiffness and fibrosis and improved LV contractility and diastolic function.87 In a seven-day study, ivabradine increased peak VO2 and reduced exercise E/e’ ratio in 61 patients with HFpEF.88 However in contrast, a short term, placebo-controlled, randomized, crossover study found that 2 weeks of HR reduction with ivabradine in patients with HFpEF almost uniformly exacerbated already abnormal exercise physiology.89 To study the impact of restoring normal HR response during exercise in patients with HFpEF and CI, an ongoing trial RateAdaptive Atrial Pacing in Diastolic HF (NCT02145351) is underway. Riociguat is a soluble guanylate cyclase stimulator that targets the NO-soluble guanylate cyclase–cyclic guanosine monophosphate signaling pathway. As shown in Table 1, the DILATE-1 study failed to show any impact on the primary end -point.90 There is an ongoing trial examining the use of another oral guanylate cyclase stimulator, vericiguat, in patients with HFpEF (BAY1021189). Statins: By blocking the activity of several guanosine triphosphate binding proteins and inhibiting some of the inflammatory processes described above, statins can suppress LV hypertrophy and decrease collagen synthesis in experimental models.91;92 Even though observational data in HFpEF patients suggest a mortality benefit with use of HMG-Co-A reductase inhibitors, despite neutral outcomes in HFrEF patients, definitive trials have not been performed and might be difficult given existing wide-spread use of statins for multiple indications in many HFpEF patients.93;94 In a recent prospective study of HFpEF patients, statin use was associated with a higher rate of 1-year survival compared with those who were not treated. 95 A recent meta-analysis suggested a potential mortality benefit with statin.96 Ranolazine blocks inward sodium current, promotes Ca2+ extrusion through the Na+/Ca2+ exchanger and thereby improve diastolic tension and relaxation. The RALI-DHF study showed improvement in some measures of hemodynamics but no improvement in relaxation parameters.97;98 Alagebrium (ALT-711): A small open-label study found that administration of ALT-711 that breaks glucose crosslinks was associated with slightly reduced LV mass and improved diastolic filling, however, there were no changes in the primary outcomes.99 Anakinra: IL-1 (alpha) and IL-1 (beta) are potent proinflammatory cytokines implicated in adverse ventricular–vascular remodeling.100 IL-1 blockade with anakinra for 14 days significantly reduced the systemic inflammatory response and improved aerobic exercise capacity in patients with HFpEF and elevated plasma CRP levels. Sitaxsentan: In a moderate sized trial of 6-months treatment with sitaxsentan, a selective endothelin type A receptor antagonist appeared to provide a modest increase in treadmill exercise time.101 Empagliflozin, an inhibitor of sodium-glucose cotransporters type 2 (SGLT2), was shown to reduce HF admissions in patients with type 2 diabetes and high cardiovascular risk, with a consistent benefit in patients with and without baseline HF. HF admission was a secondary outcome of the trial, and it is unknown what proportion of HF events were HFpEF vs HFrEF.102 The ongoing CANDLE trial in patients with type 2 diabetes and chronic HF (Both HFpEF and HFrEF) is evaluating the clinical safety and efficacy on HF outcomes of another SGLT2 inhibitor, canagliflozin, in comparison with glimepiride. Other trials are also in planning, including the HF-PRESERVED trial which will evaluate the effect of dapagliflozin on biomarkers, symptoms, and functional status in HFpEF patients with type 2 diabetes or pre-diabetes.103 Long-term therapy with elamipretide(MTP-131), a novel mitochondria-targeting peptide, improves LV systolic function, normalizes plasma biomarkers, and reverses mitochondrial abnormalities in LV myocardium of dogs with advanced HF.104
Currently a phase I trial is evaluating the safety and tolerability of MTP-131 in mid to moderate HF patients (NCT02388464). A recent prospective human study demonstrated that pulmonary vasodilation, enhanced reductions in PA resistance and greater increase in PA compliance with dobutamine (a beta 2 agonist).30 Based on this finding, a randomized controlled trial (BEAT HFpEF: NCT02885636) is currently using inhaled beta-adrenergic agonists (Albeuterol) to treat pulmonary vascular disease in HFpEF. Two classic medications, nifedipine and isosorbide dinitrate/hydralazine (HISDN), are currently being tested for their potential benefit to HFpEF patients (NCT01157481 and NCT01516346). Preclinical data showed HISDN improved diastolic function, exercise capacity and reduced soluble vascular cell adhesion molecule 1 levels in mice, but there were no reductions in LV hypertrophy, cardiac fibrosis, or pulmonary congestion.105 Recently, exciting studies have revealed that microRNAs (miRNA)-34a might have an important role in cardiac aging via effects on apoptosis, DNA damage, and telomere shortening.106 The strategy of replacement of miRNAs of interest or of blockade of potentially harmful miRNAs (anti-MIRs) is currently being tested in pre-clinical studies.106 Endothelial NO synthase activators were studied in the DAHL salt–sensitive rat model of HFpEF. Diastolic dysfunction was reduced, as were both cardiac hypertrophy and fibrosis.107 In mice, aging is associated with increased MMP-9 levels that precede the development of diastolic dysfunction. Based on results in mice, there is strong rationale for evaluating MMP-9 selective inhibition in animal models of HFpEF.108 However, developments of these agents have proven difficult.
Non-pharmacological Strategies
Revascularization
Myocardial ischemia acutely causes both systolic and diastolic dysfunction and may contribute to abnormal cardiovascular reserve with stress.75 So it would seem that revascularization would be beneficial in patients with HFpEF who have underlying ischemic heart disease. Few larger retrospective studies showed CAD is common in patients with HFpEF and is associated with increased risk of cardiovascular death, especially sudden death.109;110 Complete revascularization lowered mortality and improved the systolic function in this cohort.109 An autopsy study recently showed epicardial CAD was frequent and extensive in HFpEF.21 However, retrospective data suggest that clinically evident, acute coronary ischemia may not be the key trigger for acute decompensation in HFpEF, and that the EF does not decline during an acute episode,111 and that are vascularizing epicardial coronary stenoses has little effect on preventing the recurrence of acute HFpEF.112 Although prospective data are relatively modest, the ACCF/AHA guideline recommends revascularization in HFpEF (IIa). Given the paucity of effective treatments for HFpEF, prospective trials are urgently needed to determine the optimal evaluation and management of CAD in HFpEF.
Exercise Training (ET)
Exercise intolerance is the primary manifestation of chronic HFpEF, and key determinant of these patients reduced quality of life, and is therefore an important outcome in trials of HFpEF. ET has been shown to improve exercise intolerance in HF.113;114 Kitzman and colleagues found increased peak VO2, ventilatory anaerobic threshold, 6 MWD, and physical quality-of-life scores with exercise therapy in HFpEF .115 These results were confirmed in a subsequent multicenter, randomized trial of 3 months of combined ET and strength training in HFpEF patients.116 In a second, separate, randomized, attention-controlled, single- blind trial of 4 months upper and lower extremity endurance ET, Kitzman et al found a significant increase in peak VO2 without altering carotid arterial stiffness or brachial artery flow mediated dilation.117 Furthermore, Kitzman et al showed that strongest determinant of the severely reduced exercise capacity in HFpEF patients was reduced peak arterial-venous oxygen difference (A-VO2 Diff );118 peak AVO2 diff was higher after ET and was the primary contributor to improved peak VO2.77 Recently, Kitzman et al further extended these results by demonstrating that in obese older patients with HFpEF the addition of caloric restriction diet to endurance ET training was additive and produced a relatively large increase in peak VO2. The improvements in Peak VO2 were associated with in body composition, but not any echo-Doppler measure of resting LV structure or function.114 In a recent pilot study, 4 week o i -intensit inter a trainin si ni icant i pro ed pea o2 and left ventricular diastolic dysfunction in HFpEF patients.119 Taken together, ET is an effective non-pharmacologic therapy in clinically stable patients with HFpEF to improve exercise tolerance. A randomized multi-center study comparing three months supervised moderate intensity continuous training versus high intensity interval training versus a control group followed by nine months of telemedically monitored home-based training is under way.120
How did ET improve exercise intolerance in HFpEF patients? Several studies demonstrated that in HFpEF, pathologic elevations in filling pressures with impaired CO during exercise and were related to limitations in biventricular and pulmonary vascular reserve.24;121;122 Studies also demonstrated that inadequate CO relative to metabolic needs also contributes to exercise intolerance in HFpEF patients.123 However beneficial effects of ET certainly points through mechanisms independent of LV systolic or diastolic function. A majority of improvements in peak VO2 with ET was mediated by extra-cardiac factors such as improved arterial and skeletal muscle function.118 In fact, Kitzman et al. reported that older HFpEF patients have abnormal skeletal muscle oxygen utilization and that this is related to their severely reduced peak VO2. They also demonstrated that skeletal muscle oxidative capacity, mitochondrial content, and mitochondrial fusion were abnormal in older patients with HFpEF. 124;125 Similarly, Bhella et al. reported that elderly HFpEF patients have baseline impaired skeletal muscle oxidative metabolism, which can be favorably shifted by ET to more efficient muscle O2 utilization. Recently, Dhakal et al. using invasive hemodynamic monitoring during exercise; showed that oxygen extraction was significantly reduced in HFpEF and was a major contributor to reduced peak VO2.
Because exercise induced increases in LV filling pressure may also contribute significantly to exercise intolerance in in HFpEF, improvements in LV filling could also contribute to the benefit of ET. However, there are relatively few data in this regard. While, some studies have attributed this to exercise-induced favorable changes in LV function and CO, atrial reverse remodeling and improved LV diastolic function. 116;119;126 In addition, peak exercise HR reduced in these patients and ET reverses this CI.77;127 Fujimoto et al was the only study to measure invasively measured LV filling and diastolic LV function before and after ET in elderly HFpEF patients and found no improvements after a fully year of ET.128
Nutritional Strategies
In a recent proof-of-concept study, consumption of sodium-restricted DASH diet for 21 days in 13 hypertensive HFpEF patients resulted in improvement in relaxation and stiffness based measures of diastolic function and ventricular–vascular coupling ratio and decrease in arterial elastance.129;130 A recent study with a relatively small patient sample showed that one week of daily dosing with beet root juice (6.1 mmol inorganic nitrate) significantly improved submaximal aerobic endurance and blood pressure in elderly 20 HFpEF patients.131 Similarly, Zamani, et al found that a single dose of inorganic nitrate (NO3-rich beetroot juice: NO3−, 12.9 mmol) administered before exercise significantly improves peak VO2 in subjects with HFpEF by significant reduction in systemic vascular resistance, increase in CO at peak exercise, as well as an increase in the peak Vo2 at which ventilatory threshold occurred. They speculated that that NO3− improves exercise capacity in HFpEF by improving the peripheral response to exercise and by providing greater O2 delivery to exercising muscles.132 Recently Kitzman et al showed among obese older patients with clinically stable HFpEF, caloric restriction significantly improved exercise capacity and quality of life, and the effect was additive to ET.114
Miscellaneous:
Anemia is highly prevalent in HFpEF and carries a poor prognosis; leading to the hypothesis that epoeitin-alfa would improve submaximal exercise capacity and ventricular remodeling. However, in a well-designed randomized trial, after 24 weeks of therapy there was no change in 6-MWD or LV end diastolic volume.133 Injection of a myostatin-blocking antibody in mice with preexisting HF preserved muscle mass.134 Thus, myostatin inhibition might be a medically relevant avenue for the treatment of muscle wasting in HF. A number of clinical trials that target myostatin in older patients with sarcopenia associated with other chronic disorders are ongoing.
Managing common comorbidities
Both HFpEF and AF are inextricably linked, both to each other and to adverse cardiovascular outcomes.135;136 AF in HFpEF associated with impaired LV systolic, diastolic function and functional reserve, larger LA with poor LA function, more severe neurohumoral activation, and impaired exercise tolerance.136–139 The ACCF/AHA guidelines recommends management of AF for symptom control for HFpEF (Class IIa with level of evidence C). ESC guidelines support restoring sinus rhythm by cardioversion along with anticoagulation, although strong evidence is sparse.140 Catheter ablation of AF had limited long-term success in HFpEF.141 Further study is required to determine whether different rate control strategies or indeed, rhythm control in patients with HFpEF and AF may favorably affect exercise tolerance. HTN is the most prevalent risk factor for HF, and precedes the diagnosis of HF in 75–85% of persons who develop HF. In addition, HTN pathophysiology is closely linked to all key adverse outcomes in HF, including acute exacerbations, chronic symptoms, and mortality.2 Since myocardial perfusion depends on diastolic BP, intensive diastolic BP reduction could reduce myocardial perfusion, and promote myocardial ischemia, LV dilation, and subsequent HF. In addition, due to increased ventricular and arterial stiffening beyond that associated with aging and/or HTN, excessive reduction in BP with vasodilation in HFpEF could potentially offset any benefit from antagonism of pathologic neurohormonal activation.142;143 However despite controversies regarding potential adverse effects of intensive BP lowering, the recent SPRINT trial demonstrated that intensive systolic BP reduction significantly reduced the rate of development of acute decompensated HF.144 While it is uncertain what proportion of these HF events were HFpEF vs HFrEF, it is likely that HFpEF was well-represented.144 In addition it is worth noting that large outcome trials confirmed
ACEIs/ARBs and spironolactone to be safe and well tolerated in HFpEF. Obesity: Approximately 85% of elderly HFpEF patients are overweight or obese, and the HFpEF epidemic has largely paralleled the obesity epidemic. Approximately 85% of elderly HFpEF patients are overweight or obese, and the HFpEF epidemic has largely paralleled the obesity epidemic.145 Adiposityinduced inflammation has wide-ranging adverse effects, including endothelial dysfunction, capillary rarefaction, and mitochondrial dysfunction in both the cardiac and systemic vascular beds.146 Unfortunately, obesity has not only been overlooked as a potentially pivotal factor in HFpEF pathophysiology and treatment, it has been actively avoided.
Device Therapy
The CARDIOMEMS device is a wireless, implanted PA pressure monitor implanted in the distal PA during a right heart catheterization procedure. Patients transmit hemodynamic data daily using a wireless RF transmitter. The CHAMPION trial showed a significant reduction in HF hospitalizations.147 In HFpEF, CARDIOMEMS device reduced decompensation leading to hospitalization compared with standard HF management strategies.148
Given that rises in LA pressure and pulmonary venous congestion are shown to herald HF decompensation events in patients with HFpEF, creating a controlled left-to-right interatrial shunt to allow LA decompression could be a rational nonpharmacological strategy for alleviating symptoms in patients with HFpEF. Hemodynamic modelling based on clinical measurements suggested that an appropriately sized iatrogenic atrial septal defect could attenuate exercise-induced increases in LA pressure in patients with HFpEF.149 Subsequently, an open-label study demonstrated reductions in LA pressure during exercise with improvements in functional capacity and quality of life 6 months after implantation of this device.150 A prospective, multicenter, randomized, and single blinded trial is underway to confirm this finding (NCT02600234).
A trial testing potential benefit of Baroreflex activation therapy (BAT) for HFpEF, the HOPE4HF trial (a randomized outcomes trial designed to evaluate the clinical safety and efficacy of BAT in the HFpEF population: NCT00957073),151 is underway. A micro-ventricular assist device implanted (off pump) via a mini-thoracotomy, in a right subclavicular subcutaneous pocket (like a pacemaker) with drainage of blood from the LA and output it in the subclavian artery appears to interrupt the progressive hemodynamic deterioration in HFrEF.152 However its role in HFpEF is yet to be defined. In a recent cardiovascular simulation model of HFpEF, mechanical circulatory support significantly increased CO, provided a mild increase in BP, and markedly reduced pulmonary and LA pressures.153
Conclusions and Perspectives
HFpEF is the most common form of HF in patients older than 65 years. The ideal treatment modality for HFpEF should be one that is able to relieve symptom but also provide mortality and morbidity benefit. To date, there are no approved therapies available for reducing mortality or hospitalizations for these patients. The failure to develop successful therapies for the management of HFpEF may be because of the poor understanding of the pathophysiology of HFpEF, inadequate standardization of the HFpEF diagnosis, the lack of strict definition and inadequate differentiation of disease subtypes. In addition, HFpEF is likely a systemic syndrome, with multi-factorial pathophysiology, underlying age-related changes, frequent multiple chronic co-morbidities, multi-organ involvement, and clinical heterogeneity. These concepts have led to the proposal of key phenotypes in HFpEF, with each phenotype having somewhat distinct pathophysiological and treatment implications.154 Acknowledging these factors and the resulting key phenotypes in designing HFpEF trials could help achieve more homogenous study populations, and thereby better match underlying pathophysiology with proposed therapeutic mechanisms. New clinical trials that target underlying inflammation, oxidative stress, and aging-related dysfunction may prove to be particularly effective for HFpEF.
Acknowledgments
Supported in part by NIH grants R01AG18915 and P30AG12232, and by the Kermit Glenn Phillips endowment in cardiovascular medicine.
Potential Financial Conflicts of Interest:
Dr. Kitzman declares the following relationships: Consultant for Abbvie, Bayer, Merck, 3 Medtronic, GSK, Relypsa, Regeneron, Merck, Corvia Medical, and Actavis, research grant 4 funding from Novartis, and stock ownership in Gilead Sciences and Relypsa.
Dr. Upadhya has received research funding from Novarits and Corvia.
Reference List
- (1).Kitzman DW, Gardin JM, Gottdiener JS et al. Importance of heart failure with preserved systolic function in patients > or = 65 Years of Age. CHS Research Group. Cardiovascular Health Study. Am J Cardiol 2001;87:413–419. [DOI] [PubMed] [Google Scholar]
- (2).Gottdiener JS, Arnold AM, Aurigemma GP et al. Predictors of congestive heart failure in the elderly: the Cardiovascular Health Study. J Am Coll Cardiol 2000;35:1628–1637. [DOI] [PubMed] [Google Scholar]
- (3).Owan TE, Hodge DO, Herges RM, Jacobsen SJ, Roger VL, Redfield MM. Trends in prevalence and outcome of heart failure with preserved ejection fraction. N Engl J Med 2006;355:251–259. [DOI] [PubMed] [Google Scholar]
- (4).Dunlay SM, Redfield MM, Weston SA et al. Hospitalizations after heart failure diagnosis: a community perspective. J Am Coll Cardiol 2009;54:1695–1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (5).Steinberg BA, Zhao X, Heidenreich PA et al. Trends in Patients Hospitalized With Heart Failure and Preserved Left Ventricular Ejection Fraction: Prevalence, Therapies, and Outcomes. Circulation 2012;126:65–75. [DOI] [PubMed] [Google Scholar]
- (6).Bhatia RS, Tu JV, Lee DS et al. Outcome of heart failure with preserved ejection fraction in a population-based study. N Engl J Med 2006;355:260–269. [DOI] [PubMed] [Google Scholar]
- (7).Liao L, Jollis JG, Anstrom KJ et al. Costs for Heart Failure With Normal vs Reduced Ejection Fraction. Arch Intern Med 2006;166:112–118. [DOI] [PubMed] [Google Scholar]
- (8).Fonarow GC, Stough WG, Abraham WT et al. Characteristics, Treatments, and Outcomes of Patients With Preserved Systolic Function Hospitalized for Heart Failure: A Report From the OPTIMIZE-HF Registry. J Am Coll Cardiol 2007;50:768–777. [DOI] [PubMed] [Google Scholar]
- (9).Vasan RS, Larson MG, Benjamin EJ, Evans JC, Reiss CK, Levy D. Congestive heart failure in subjects with normal versus reduced left ventricular ejection fraction: prevalence and mortality in a population-based cohort. J Am Coll Cardiol 1999;33:19481955. [DOI] [PubMed] [Google Scholar]
- (10).Yancy C, Lopatin M, Stevenson L, De Marco T, Fonarow G, ADHERE Scientific Advisory Committee and Investigators. Clinical presentation, management, and in-hospital outcomes of patients admitted with acute decompensated heart failure with preserved systolic function: a report from the Acute Decompensated Heart Failure National Registry (ADHERE) Database. J Am Coll Cardiol 2006;47:76–84. [DOI] [PubMed] [Google Scholar]
- (11).Ather S, Chan W, Bozkurt B et al. Impact of Noncardiac Comorbidities on Morbidity and Mortality in a Predominantly Male Population With Heart Failure and Preserved Versus Reduced Ejection Fraction. J Am Coll Cardiol 2012;59:998–1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).Zile MR, Baicu CF, Gaasch WH. Diastolic heart failure--abnormalities in active relaxation and passive stiffness of the left ventricle. N Engl J Med 2004;350:1953–1959. [DOI] [PubMed] [Google Scholar]
- (13).Paulus W, Tschope C. A Novel Paradigm for Heart Failure with Preserved Ejection Fraction: Comorbidities Drive Myocardial Dysfunction and Remodeling Through Coronary Microvascular Endothelial Inflammation. J Am Coll Cardiol 2013;62:263–271. [DOI] [PubMed] [Google Scholar]
- (14).Weber K, Brilla C, Janicki J. Myocardial fibrosis: functional significance and regulatory factors. Cardiovasc Res 1993;27:341–348. [DOI] [PubMed] [Google Scholar]
- (15).Ahmed SH, Clark LL, Pennington WR et al. Matrix Metalloproteinases/Tissue Inhibitors of Metalloproteinases: Relationship Between Changes in Proteolytic Determinants of Matrix Composition and Structural, Functional, and Clinical Manifestations of Hypertensive Heart Disease. Circulation 2006;113:2089–2096. [DOI] [PubMed] [Google Scholar]
- (16).Lam CSP, Roger VrL, Rodeheffer RJ et al. Cardiac Structure and VentricularGÇôVascular Function in Persons With Heart Failure and Preserved Ejection Fraction From Olmsted County, Minnesota. Circulation 2007;115:1982–1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (17).Borlaug BA, Lam CSP, Roger VL, Rodeheffer RJ, Redfield MM. Contractility and Ventricular Systolic Stiffening in Hypertensive Heart Disease: Insights Into the Pathogenesis of Heart Failure With Preserved Ejection Fraction. J Am Coll Cardiol 2009;54:410–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (18).Zile MR, Gottdiener JS, Hetzel SJ et al. Prevalence and Significance of Alterations in Cardiac Structure and Function in Patients With Heart Failure and a Preserved Ejection Fraction. Circulation 2011;124:2491–2501. [DOI] [PubMed] [Google Scholar]
- (19).Su MY, Lin LY, Tseng YH et al. CMR-verified diffuse myocardial fibrosis is associated with diastolic dysfunction in HFpEF. JACC Cardiovasc Imaging 2014;7:991–997. [DOI] [PubMed] [Google Scholar]
- (20).Kitzman DW, Upadhya B, Vasu S. What the dead can teach the living: the systemic nature of heart failure with preserved ejection fraction. Circulation 2015;131:522–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (21).Mohammed SF, Hussain S, Mirzoyev SA, Edwards WD, Maleszewski JJ, Redfield MM. Coronary microvascular rarefaction and myocardial fibrosis in heart failure with preserved ejection fraction. Circulation 2015;131:550–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Yip GW, Zhang Q, Xie JM et al. Resting global and regional left ventricular contractility in patients with heart failure and normal ejection fraction: insights from speckle-tracking echocardiography. Heart 2011;97:287–294. [DOI] [PubMed] [Google Scholar]
- (23).Kraigher-Krainer E, Shah AM, Gupta DK et al. Impaired systolic function by strain imaging in heart failure with preserved ejection fraction. J Am Coll Cardiol 2014;63:446456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (24).Borlaug BA, Kane GC, Melenovsky V, Olson TP. Abnormal right ventricular-pulmonary artery coupling with exercise in heart failure with preserved ejection fraction. Eur Heart J 2016; 14; 37:3293–3302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (25).Borlaug BA, Melenovsky V, Russell SD et al. Impaired Chronotropic and Vasodilator Reserves Limit Exercise Capacity in Patients With Heart Failure and a Preserved Ejection Fraction. Circulation 2006;114:2138–2147. [DOI] [PubMed] [Google Scholar]
- (26).Lakatta EG, Levy D. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part II: the aging heart in health: links to heart disease. Circulation 2003;107:346–354. [DOI] [PubMed] [Google Scholar]
- (27).Kitzman DW, Taffet G. Effects of aging on cardiovascular structure and function In: Halter JB, Ouslander JG, Tinetti ME, Studenski SA, High KP, Asthana S, eds. Hazzard’s Geriatric Medicine and Gerontology. 6th ed New York: McGraw Hill; 2009;883–895. [Google Scholar]
- (28).Kitzman DW, Little WC, Brubaker PH et al. Pathophysiological characterization of isolated diastolic heart failure in comparison to systolic heart failure. JAMA 2002;288:2144–2150. [DOI] [PubMed] [Google Scholar]
- (29).Clarkson PB, Wheeldon NM, MacFadyen RJ, Pringle SD, MacDonald TM. Effects of brain natriuretic peptide on exercise hemodynamics and neurohormones in isolated diatsolic heart failure. Circulation 1996;93:2037–2042. [DOI] [PubMed] [Google Scholar]
- (30).Andersen MJ, Hwang SJ, Kane GC et al. Enhanced pulmonary vasodilator reserve and abnormal right ventricular: pulmonary artery coupling in heart failure with preserved ejection fraction. Circ Heart Fail 2015;8:542–550. [DOI] [PubMed] [Google Scholar]
- (31).Melenovsky V, Hwang S, Lin G, Redfield M, Borlaug B. Right heart dysfunction in heart failure with preserved ejection fraction. Eur Heart J 2014;35:3452–3462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (32).Mohammed SF, Hussain I, Abou Ezzeddine OF et al. Right ventricular function in heart failure with preserved ejection fraction: a community-based study. Circulation 2014;130:2310–2320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (33).Phan T, Shivu G, Weaver R, Ahmed I, Frenneaux M. Impaired heart rate recovery and chronotropic incompetence in patients with heart failure with preserved ejection fraction. Circ Heart Fail 2010;3:29–34. [DOI] [PubMed] [Google Scholar]
- (34).Redfield MM, Jacobsen SJ, Borlaug BA, Rodeheffer R, Kass DA. Age- and genderrelated ventricular-vascular stiffening: a community-based study. Circulation 2005;112:2254–2262. [DOI] [PubMed] [Google Scholar]
- (35).Olson TP, Johnson BD, Borlaug BA. Impaired Pulmonary Diffusion in Heart Failure With Preserved Ejection Fraction. JACC Heart Fail 2016;4:490–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (36).Hoeper MM, Meyer K, Rademacher J, Fuge J, Welte T, Olsson KM. Diffusion Capacity and Mortality in Patients With Pulmonary Hypertension Due to Heart Failure With Preserved Ejection Fraction . JACC Heart Fail 2016;4:441–449. [DOI] [PubMed] [Google Scholar]
- (37).Bhella PS, Prasad A, Heinicke K et al. Abnormal haemodynamic response to exercise in heart failure with preserved ejection fraction. Eur J Heart Fail 2011;13:1296–1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (38).Nicklas B, Leng I, Delbono O et al. Relationship of physical function to vastus lateralis capillary density and metabolic enzyme activity in elderly men and women. Aging Clin Exp Res 2008;20:302–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (39).Haykowsky MJ, Brubaker PH, Morgan TM, Kritchevsky SB, Eggebeen J, Kitzman DW. Impaired aerobic capacity and physical functional performance in older heart failure patients with preserved ejection fraction: role of lean body mass. J Gerontol A Biol Sci Med Sci 2013;68:968–975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (40).Maurer MS, Burkhoff D, Fried LP, Gottdiener J, King DL, Kitzman DW. Ventricular Structure and Function in Hypertensive Participants With Heart Failure and a Normal Ejection Fraction: The Cardiovascular Health Study. J Am Coll Cardiol 2007;49:972–981. [DOI] [PubMed] [Google Scholar]
- (41).Kalogeropoulos A, Georgiopoulou V, Psaty B et al. Inflammatory markers and incident heart failure risk in older adults: the Health ABC (Health, Aging, and Body Composition) study. J Am Coll Cardiol 2010;55:2129–2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (42).Matsubara J, Sugiyama S, Nozaki T et al. Pentraxin 3 Is a New Inflammatory Marker Correlated With Left Ventricular Diastolic Dysfunction and Heart Failure With Normal Ejection Fraction. J Am Coll Cardiol 2011;57:861–869. [DOI] [PubMed] [Google Scholar]
- (43).Collier P, Watson C, Voon V et al. Can emerging biomarkers of myocardial remodelling identify asymptomatic hypertensive patients at risk for diastolic dysfunction and diastolic heart failure? Eur J Heart Fail 2011;13:1087–1095. [DOI] [PubMed] [Google Scholar]
- (44).Franceschi C, Bonafe M, Valensin S et al. Inflamm-aging: An evolutionary perspective on immunosenescence. Ann N Y Acad Sci 2000;908:244–254. [DOI] [PubMed] [Google Scholar]
- (45).Yancy CW, Jessup M, Bozkurt B et al. 2013 ACCF/AHA Guideline for the management of heart-failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;62:e147e239. [DOI] [PubMed] [Google Scholar]
- (46).McMurray JJ, Adamopoulos S, Anker SD et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012;14:803–869. [DOI] [PubMed] [Google Scholar]
- (47).Groban L, Pailes NA, Bennett C et al. Growth Hormone Replacement Attenuates Diastolic Dysfunction and Cardiac Angiotensin II Expression in Senescent Rats. J Gerontol A Biol Sci Med Sci 2006;61:28–35. [DOI] [PubMed] [Google Scholar]
- (48).Groban L, Yamaleyeva LM, Westwood BM et al. Progressive diastolic dysfunction in the female mRen(2).Lewis Rat: Influence of salt and ovarian hormones. Gerontol B Physiol Sci Sco Sci 2008;63:3–11. [DOI] [PubMed] [Google Scholar]
- (49).Lasocki S, Iglarz M, Seince PF et al. Involvement of renin-angiotensin system in pressure-flow relationship: role of angiotensin-converting enzyme gene polymorphism. Anesthesiology 2002;96:271–275. [DOI] [PubMed] [Google Scholar]
- (50).Little WC, Wesley-Farrington DJ, Hoyle J et al. Effect of candesartan and verapamil on exercise tolerance in diastolic dysfunction. J Cardiovasc Pharmacol 2004;43:288–293. [DOI] [PubMed] [Google Scholar]
- (51).Wright JW, Mizutani S, Harding JW. Pathways involved in the transition from hypertension to hypertrophy to heart failure. Treatment strategies. Heart Fail Rev 2008;13:367–375. [DOI] [PubMed] [Google Scholar]
- (52).Yusuf S, Pfeffer MA, Swedberg K et al. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-Preserved Trial. Lancet 2003;362:777–781. [DOI] [PubMed] [Google Scholar]
- (53).Cleland JGF, Tendera M, Adamus J, Freemantle N, Polonski L, Taylor J. The perindopril in elderly people with chronic heart failure (PEP-CHF) study. Eur Heart J 2006;27:23382345. [DOI] [PubMed] [Google Scholar]
- (54).Massie BM, Carson PE, McMurray JJ et al. Irbesartan in Patients with Heart Failure and Preserved Ejection Fraction. N Engl J Med 2008;359:2456–2467. [DOI] [PubMed] [Google Scholar]
- (55).Kitzman DW, Hundley WG, Brubaker P, Stewart K, Little WC. A randomized, controlled, double-blinded trial of enalapril in older patients with heart failure and preserved ejection fraction; effects on exercise tolerance, and arterial distensibility. Circ Heart Fail 2010;3:477–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (56).Zi M, Carmichael N, Lye M. The effect of quinapril on functional status of elderly patients with diastolic heart failure. Cardiovasc Drugs Ther 2003;17:133–139. [DOI] [PubMed] [Google Scholar]
- (57).Edelmann F, Aldo-DHF investigators. Effect of spironolactone on diastolic function and exercise capacity in patients with heart failure with preserved ejection fraction: The aldodhf randomized controlled trial. JAMA 2013;309:781–791. [DOI] [PubMed] [Google Scholar]
- (58).Deswal A, Richardson P, Bozkurt B, Mann D. Results of the Randomized Aldosterone Antagonism in Heart Failure With Preserved Ejection Fraction Trial (RAAM-PEF). J Card Fail 2011;17:634–642. [DOI] [PubMed] [Google Scholar]
- (59).Patel K, Fonarow GC, Kitzman DW et al. Aldosterone antagonists and outcomes in realworld older patients with heart failure and preserved ejection fraction. JACC Heart Fail 2013;1:40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (60).Pitt B, Pfeffer M, Assmann S et al. Spironolactone for heart failure with preserved ejection fraction. N Engl J Med 2014;370:1383–1392. [DOI] [PubMed] [Google Scholar]
- (61).Pfeffer MA, Claggett B, Assmann SF et al. Regional variation in patients and outcomes in the treatment of preserved cardiac function heart failure with an Aldosterone Antagonist (TOPCAT) Trial. Circulation 2015;131:34–42. [DOI] [PubMed] [Google Scholar]
- (62).Aronow WS, Ahn C, Kronzon I. Effect of propranolol versus no propranolol on total mortality plus nonfatal myocardial infarction in older patients with prior myocardial infarction, congestive heart failure, and left ventricular ejection fraction > or = 40% treated with diuretics plus angiotensin-converting enzyme inhibitors. Am J Cardiol 1997;80:207–209. [DOI] [PubMed] [Google Scholar]
- (63).Yamamoto K, Origasa H, Hori M, J-DHF Investigators. Effects of carvedilol on heart failure with preserved ejection fraction: the Japanese Diastolic Heart Failure Study (JDHF). Eur J Heart Fail 2013;15:110–118. [DOI] [PubMed] [Google Scholar]
- (64).Conraads V, Metra M, Kamp O et al. Effects of the long-term administration of nebivolol on the clinical symptoms, exercise capacity, and left ventricular function of patients with diastolic dysfunction: results of the ELANDD study. Eur J Heart Fail 2012;14:219–225. [DOI] [PubMed] [Google Scholar]
- (65).Hernandez AF, Hammill BG, O’Connor CM, Schulman KA, Curtis LH, Fonarow GC. Clinical Effectiveness of Beta-Blockers in Heart Failure: Findings From the OPTIMIZE-HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure) Registry. J Am Coll Cardiol 2009;53:184–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (66).Setaro JF, Zaret BL, Schulman DS, Black HR. Usefulness of verapamil for congestive heart failure associated with abnormal left ventricular diastolic filling and normal left ventricular systolic performance. Am J Cardiol 1990;66:981–986. [DOI] [PubMed] [Google Scholar]
- (67).Ahmed A, Pitt B, Rahimtoola SH et al. Effects of digoxin at low serum concentrations on mortality and hospitalization in heart failure: A propensity-matched study of the DIG trial. Int J Cardiol 2008;123:138–146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (68).Redfield M, Anstrom K, Levine J et al. Isosorbide Mononitrate in Heart Failure with Preserved Ejection Fraction. N Engl J Med 2015;[Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (69).Borlaug BA, Melenovsky V, Koepp KE. Inhaled sodium nitrite improves rest and exercise hemodynamics in heart failure with preserved ejection fraction. Circ Res 2016;119:880886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (70).Borlaug BA, Koepp KE, Melenovsky V. Sodium nitrite improves exercise hemodynamics and ventricular performance in heart failure with preserved ejection fraction. J Am Coll Cardiol 2015;66:1672–1682. [DOI] [PubMed] [Google Scholar]
- (71).Solomon S, Zile M, Pieske B et al. The angiotensin receptor neprilysin inhibitor LCZ696 in heart failure with preserved ejection fraction: a phase 2 double-blind randomised controlled trial. The Lancet 2012;380:1387–1395. [DOI] [PubMed] [Google Scholar]
- (72).Solomon SD, Verma A, Desai A et al. Effect of Intensive Versus Standard Blood Pressure Lowering on Diastolic Function in Patients With Uncontrolled Hypertension and Diastolic Dysfunction. Hypertension 2010;55:241–248. [DOI] [PubMed] [Google Scholar]
- (73).Kitzman D, Upadhya B. Heart failure with preserved ejection fraction: a heterogenous disorder with multifactorial pathophysiology. J Am Coll Cardiol 2014;63:457–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (74).Brubaker PH, Joo KC, Stewart KP, Fray B, Moore B, Kitzman DW. Chronotropic incompetence and its contribution to exercise intolerance in older heart failure patients. J Cardiopulm Rehabil 2006;26:86–89. [DOI] [PubMed] [Google Scholar]
- (75).Borlaug BA, Olson TP, Lam CSP et al. Global Cardiovascular Reserve Dysfunction in Heart Failure With Preserved Ejection Fraction. J Am Coll Cardiol 2010;56:845–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (76).Phan TT, Abozguia K, Nallur Shivu G et al. Heart Failure With Preserved Ejection Fraction Is Characterized by Dynamic Impairment of Active Relaxation and Contraction of the Left Ventricle on Exercise and Associated With Myocardial Energy Deficiency. J Am Coll Cardiol 2009;54:402–409. [DOI] [PubMed] [Google Scholar]
- (77).Haykowsky MJ, Brubaker PH, Stewart KP, Morgan TM, Eggebeen J, Kitzman DW. Effect of endurance training on the determinants of peak exercise oxygen consumption in elderly patients with stable compensated heart failure and preserved ejection fraction. J Am Coll Cardiol 2012;60:120–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (78).Witte KK, Cleland J, Clark AL. Chronic heart failure, chronotropic incompetence, and the effects of beta blockers. Heart 2006;92:481–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (79).Hawkins NM, Petrie MC, MacDonald MR et al. Heart Failure and Chronic Obstructive Pulmonary Disease: The Quandary of Beta-Blockers and Beta-Agonists. J Am Coll Cardiol 2011;57:2127–2138. [DOI] [PubMed] [Google Scholar]
- (80).Bangalore S, Kumar S, Lobach I, Messerli FH. Blood pressure targets in subjects with type 2 diabetes mellitus/impaired fasting glucose: observations from traditional and bayesian random-effects meta-analyses of randomized trials. Circulation 2011;123:2799–2810. [DOI] [PubMed] [Google Scholar]
- (81).Bangalore S, Parkar S, Grossman E, Messerli FH. A meta-analysis of 94,492 patients with hypertension treated with beta blockers to determine the risk of new-onset diabetes mellitus. Am J Cardiol 2007;100:1254–1262. [DOI] [PubMed] [Google Scholar]
- (82).Franssen C, Chen S, Unger A et al. Myocardial Microvascular Inflammatory Endothelial Activation in Heart Failure With Preserved Ejection Fraction. JACC Heart Fail 2015;4:312–324. [DOI] [PubMed] [Google Scholar]
- (83).Kanwar M, Agarwal R, Barnes M et al. Role of phosphodiesterase-5 inhibitors in heart failure: emerging data and concepts. Curr Heart Fail Rep 2013;10:26–35. [DOI] [PubMed] [Google Scholar]
- (84).Redfield M, Chen H, Borlaug B et al. Effect of phosphodiesterase-5 inhibition on exercise capacity and clinical status in heart failure with preserved ejection fraction: A randomized clinical trial. JAMA 2013;309:1268–1277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (85).Guazzi M, Vicenzi M, Arena R, Guazzi MD. Pulmonary hypertension in heart failure with preserved ejection fraction: a target of phosphodiesterase-5 inhibition in a 1-year study. Circulation 2011;124:164–174. [DOI] [PubMed] [Google Scholar]
- (86).Hoendermis ES, Liu LC, Hummel YM et al. Effects of sildenafil on invasive haemodynamics and exercise capacity in heart failure patients with preserved ejection fraction and pulmonary hypertension: a randomized controlled trial. Eur Heart J 2015;36:2565–2573. [DOI] [PubMed] [Google Scholar]
- (87).Reil JC, Hohl M, Reil GH et al. Heart rate reduction by If-inhibition improves vascular stiffness and left ventricular systolic and diastolic function in a mouse model of heart failure with preserved ejection fraction. Eur Heart J 2013;34:2839–2849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (88).Kosmala W, Holland DJ, Rojek A, Wright L, Przewlocka-Kosmala M, Marwick TH. Effect of If-Channel Inhibition on Hemodynamic Status and Exercise Tolerance in Heart Failure With Preserved Ejection Fraction: A Randomized Trial. J Am Coll Cardiol 2013;62:13301338. [DOI] [PubMed] [Google Scholar]
- (89).Pal N, Sivaswamy N, Mahmod M et al. Effect of Selective Heart Rate Slowing in Heart Failure With Preserved Ejection Fraction. Circulation 2015;132:1719–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (90).Bonderman D, Pretsch I, Steringer-Mascherbauer R et al. Acute hemodynamic effects of riociguat in patients with pulmonary hypertension associated with diastolic heart failure (dilate-1): A randomized, double-blind, placebo-controlled, single-dose study. CHEST Journal 2014;146:1274–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (91).Hattori T, Shimokawa H, Higashi M et al. Long-term inhibition of Rho-kinase suppresses left ventricular remodeling after myocardial infarction in mice. Circulation 2004;109:22342239. [DOI] [PubMed] [Google Scholar]
- (92).Martin J, Denver R, Bailey M, Krum H. In vitro inhibitory effects of atorvastatin on cardiac fibroblasts: implications for ventricular remodelling. Clin Exp Pharmacol Physiol 2005;32:697–701. [DOI] [PubMed] [Google Scholar]
- (93).Fukuta H, Little W. Observational studies of statins in heart failure with preserved systolic function. Heart Fail Clin 2008;4:209–216. [DOI] [PubMed] [Google Scholar]
- (94).Fukuta H, Sane DC, Brucks S, Little WC. Statin Therapy May Be Associated With Lower Mortality in Patients With Diastolic Heart Failure: A Preliminary Report. Circulation 2005;112:357–363. [DOI] [PubMed] [Google Scholar]
- (95).Alehagen U, Benson L, Edner M, Dahlstrom U, Lund LH. Association between use of dtatins and mortality in patients with heart failure and ejection fraction of greater than or equal to 50. Circ Heart Fail 2015;8:862–870. [DOI] [PubMed] [Google Scholar]
- (96).Fukuta H, Goto T, Wakami K, Ohte N. The effect of statins on mortality in heart failure with preserved ejection fraction: a meta-analysis of propensity score analyses. Int J Cardiol 2016;214:301–306. [DOI] [PubMed] [Google Scholar]
- (97).Jacobshagen C, Belardinelli L, Hasenfuss G, Maier L. Ranolazine for the Treatment of Heart Failure With Preserved Ejection Fraction: Background, Aims, and Design of the RALI-DHF Study. Clin Cardiol 2011;34:426–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (98).Maier LS, Layug B, Karwatowska-Prokopczuk E et al. RAnoLazIne for the treatment of diastolic heart failure in patients with preserved ejection fraction: the RALI-DHF proof-ofconcept study. JACC Heart Fail 2013;1:115–122. [DOI] [PubMed] [Google Scholar]
- (99).Little WC, Zile MR, Kitzman DW, Hundley WG, O’Brien TX., deGroof RC. The Effect of Alagebrium Chloride (ALT-711), a Novel Glucose Cross-Link Breaker, in the Treatment of Elderly Patients with Diastolic Heart Failure. J Card Fail 2005;11:191–195. [DOI] [PubMed] [Google Scholar]
- (100).Bujak M, Frangogiannis NG. The role of IL-1 in the pathogenesis of heart disease. Arch Immunol Ther Exp (Warsz ) 2009;57:165–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (101).Zile MR, Bourge RC, Redfield MM, Zhou D, Baicu CF, Little WC. Randomized, double-blind, placebo-controlled study of sitaxsentan to improve impaired exercise tolerance in patients with heart failure and a preserved ejection fraction. JACC Heart Fail 2014;2:123–130. [DOI] [PubMed] [Google Scholar]
- (102).Fitchett D, Zinman B, Wanner C et al. Heart failure outcomes with empagliflozin in patients with type 2 diabetes at high cardiovascular risk: results of the EMPA-REG OUTCOME(R) trial. Eur Heart J 2016;37:1526–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (103).Tanaka A, Inoue T, Kitakaze M et al. Rationale and design of a randomized trial to test the safety and non-inferiority of canagliflozin in patients with diabetes with chronic heart failure: the CANDLE trial. Cardiovasc Diabetol 2016;15:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (104).Sabbah HN, Gupta RC, Kohli S, Wang M, Hachem S, Zhang K. Chronic therapy with Elamipretide (MTP-131), a novel mitochondria-targeting peptide, improves left ventricular and mitochondrial function in dogs with advanced heart failure. Circ Heart Fail 2016;9:e002206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (105).Wilson RM, De Silva DS, Sato K, Izumiya Y, Sam F. Effects of Fixed-Dose Isosorbide Dinitrate/Hydralazine on Diastolic Function and Exercise Capacity in HypertensionInduced Diastolic Heart Failure. Hypertension 2009;54:583–590. [DOI] [PubMed] [Google Scholar]
- (106).Boon RA, Iekushi K, Lechner S et al. MicroRNA-34a regulates cardiac ageing and function. Nature 2013;495:107–110. [DOI] [PubMed] [Google Scholar]
- (107).Westermann D, Riad A, Richter U et al. Enhancement of the endothelial NO synthase attenuates experimental diastolic heart failure. Basic Res Cardiol 2009;104:499–509. [DOI] [PubMed] [Google Scholar]
- (108).Chiao YA, Ramirez TA, Zamilpa R et al. Matrix metalloproteinase-9 deletion attenuates myocardial fibrosis and diastolic dysfunction in ageing mice. Cardiovasc Res 2012;96:444–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (109).Hwang SJ, Melenovsky V, Borlaug BA. Implications of coronary artery disease in heart failure with preserved ejection fraction. J Am Coll Cardiol 2014;63:2817–2827. [DOI] [PubMed] [Google Scholar]
- (110).Rusinaru D, Houpe D, Szymanski C, Levy F, Marechaux S, Tribouilloy C. Coronary artery disease and 10-year outcome after hospital admission for heart failure with preserved and with reduced ejection fraction. Eur J Heart Fail 2014;16:967–976. [DOI] [PubMed] [Google Scholar]
- (111).Gandhi SK, Powers JC, Nomeir AM et al. The pathogenesis of acute pulmonary edema associated with hypertension. N Engl J Med 2001;344:17–22. [DOI] [PubMed] [Google Scholar]
- (112).Kramer K, Kirkman P, Kitzman DW, Little WC. Flash pulmonary edema: Association with hypertension, reocurrence despite coronary revascularization. Am Heart J 2000;140:451–455. [DOI] [PubMed] [Google Scholar]
- (113).O’Connor CM, Whellan DJ, Lee KL et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 2009;301:1439–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (114).Kitzman DW, Brubaker P, Morgan T et al. Effect of caloric restriction or aerobic exercise training on peak oxygen consumption and quality of life in obese older patients with heart failure with preserved ejection fraction: a randomised clinical trial. JAMA 2016;315:36–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (115).Kitzman D, Brubaker P, Morgan T, Stewart K, Little W. Exercise training in older patients with heart failure and preserved ejection fraction. Circ Heart Fail 2010;3:659–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (116).Edelmann F, Gelbrich G, Dungen H et al. Exercise Training Improves Exercise Capacity and Diastolic Function in Patients With Heart Failure With Preserved Ejection Fraction: Results of the Ex-DHF (Exercise training in Diastolic Heart Failure) Pilot Study. J Am Coll Cardiol 2011;58:1780–1791. [DOI] [PubMed] [Google Scholar]
- (117).Kitzman DW, Brubaker PH, Herrington DM et al. Effect of endurance exercise training on endothelial function and arterial stiffness in older patients with heart failure and preserved ejection fraction: A randomized, controlled, single-blind trial. J Am Coll Cardiol 2013;62:584–592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (118).Haykowsky MJ, Brubaker PH, John JM, Stewart KP, Morgan TM, Kitzman DW. Determinants of Exercise Intolerance in Elderly Heart Failure Patients With Preserved Ejection Fraction. J Am Coll Cardiol 2011;58:265–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (119).Angadi SS, Mookadam F, Lee CD, Tucker WJ, Haykowsky MJ, Gaesser GA. Highintensity interval training vs. moderate-intensity continuous exercise training in heart failure with preserved ejection fraction: A pilot study. J Appl Physiol 2014;95:15–27. [DOI] [PubMed] [Google Scholar]
- (120).Suchy C, Massen L, Rognmo O et al. Optimising exercise training in prevention and treatment of diastolic heart failure (OptimEx-CLIN): rationale and design of a prospective, randomised, controlled trial. Eur J Prev Cardiol 2014;21:18–25. [DOI] [PubMed] [Google Scholar]
- (121).Maeder MT, Thompson BR, Brunner-La Rocca H-P, Kaye DM. Hemodynamic Basis of Exercise Limitation in Patients With Heart Failure and Normal Ejection. J Am Coll Cardiol 2010;56:855–863. [DOI] [PubMed] [Google Scholar]
- (122).Borlaug BA, Nishimura RA, Sorajja P, Lam CSP, Redfield MM. Exercise Hemodynamics Enhance Diagnosis of Early Heart Failure with Preserved Ejection Fraction. Circ Heart Fail 2010;3:588–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (123).Abudiab MM, Redfield MM, Melenovsky V et al. Cardiac output response to exercise in relation to metabolic demand in heart failure with preserved ejection fraction. Eur J Heart Fail 2013;15:776–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (124).Kitzman DW, Nicklas B, Kraus WE et al. Skeletal muscle abnormalities and exercise intolerance in older patients with heart failure and preserved ejection fraction. Am J Physiol Heart Circ Physiol 2014;306:H1364–1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (125).Molina AJ, Bharadwaj MS, Van Horn C et al. Skeletal Muscle Mitochondrial Content, Oxidative Capacity, and Mfn2 Expression Are Reduced in Older Patients With Heart Failure and Preserved Ejection Fraction and Are Related to Exercise Intolerance. JACC Heart Fail 2016;4:636–645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (126).Hambrecht R, Gielen S, Linke A et al. Effects of exercise training on left ventricular function and peripheral resistance in patients with chronic heart failure. JAMA 2000;283:3095–3101. [DOI] [PubMed] [Google Scholar]
- (127).Ahmed A, Zile MR, Rich MW et al. Hospitalizations Due to Unstable Angina Pectoris in Diastolic and Systolic Heart Failure. Am J Cardiol 2007;99:460–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (128).Fujimoto N, Prasad A, Hastings JL et al. Cardiovascular effects of 1 year of progressive endurance exercise training in patients with heart failure with preserved ejection fraction. Am Heart J 2012;164:869–877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (129).Hummel S, Seymour E, Brook R et al. Low-sodium dietary approaches to stop hypertension diet reduces blood pressure, arterial stiffness, and oxidative stress in hypertensive heart failure with preserved ejection fraction. Hypertension 2012;60:12001206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (130).Hummel S, Seymour E, Brook R et al. Low-sodium DASH diet improves diastolic function and ventricular-arterial coupling in hypertensive heart failure with preserved ejection fraction. Circ Heart Fail 2013; November; 6:1165–71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- (131).Eggebeen J, Kim-Shapiro DB, Haykowsky MJ et al. One week of daily dosing with beetroot juice improves submaximal endurance and blood pressure in older patients with Heart Faliure and Preserved Ejection Fraction. JACC Heart Fail 2015;4:428–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (132).Zamani P, Rawat D, Shiva-Kumar P et al. Effect of inorganic nitrate on exercise capacity in heart failure with preserved ejection fraction. Circulation 2015;131:371–380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (133).Maurer MS, Teruya S, Chakraborty B, Helmke S, Mancini D. Treating Anemia in Older Adults with Heart Failure with a Preserved Ejection Fraction (HFPEF) with Epoetin Alfa: Single Blind Randomized Clinical Trial of Safety and Efficacy. Circ Heart Fail 2013;6:254–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (134).Heineke J, Auger-Messier M, Xu J et al. Genetic deletion of myostatin from the heart prevents skeletal muscle atrophy in heart failure. Circulation 2010;121:419–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (135).Vermond RA, Geelhoed B, Verweij N et al. Incidence of atrial fibrillation and relationship with cardiovascular events, heart failure, and mortality: a community-based study from the Netherlands. J Am Coll Cardiol 2015;66:1000–1007. [DOI] [PubMed] [Google Scholar]
- (136).Chamberlain AM, Redfield MM, Alonso A, Weston SA, Roger VL. Atrial fibrillation and mortality in heart failure: a community study. Circ Heart Fail 2011;4:740–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (137).Zakeri R, Borlaug BA, McNulty SE et al. Impact of atrial fibrillation on exercise capacity in heart failure with preserved ejection fraction: a RELAX trial ancillary study. Circ Heart Fail 2014;7:123–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (138).Lam CS, Rienstra M, Tay WT et al. Atrial fibrillation in heart failure with preserved ejection fraction: association with exercise capacity, left ventricular filling pressures, natriuretic peptides, and left atrial volume. JACC: Heart Failure 2017; 5:92–98. [DOI] [PubMed] [Google Scholar]
- (139).Melenovsky V, Hwang SJ, Redfield MM, Zakeri R, Lin G, Borlaug BA. Left atrial remodeling and function in advanced heart failure with preserved or reduced ejection fraction. Circ Heart Fail 2015; 8:295–303 [DOI] [PubMed] [Google Scholar]
- (140).Ponikowski P, Voors AA, Anker SD et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2016;18:891–975. [DOI] [PubMed] [Google Scholar]
- (141).Machino-Ohtsuka T, Seo Y, Ishizu T et al. Efficacy, safety, and outcomes of catheter ablation of atrial fibrillation in patients with heart failure with preserved ejection fraction. J Am Coll Cardiol 2013;62:1857–1865. [DOI] [PubMed] [Google Scholar]
- (142).Kawaguchi M, Hay I, Fetics B, Kass DA. Combined Ventricular Systolic and Arterial Stiffening in Patients With Heart Failure and Preserved Ejection Fraction. Circulation 2003;107:714–720. [DOI] [PubMed] [Google Scholar]
- (143).Schwartzenberg S, Redfield MM, From AM, Sorajja P, Nishimura RA, Borlaug BA. Effects of Vasodilation in Heart Failure With Preserved or Reduced Ejection Fraction: Implications of Distinct Pathophysiologies on Response to Therapy. J Am Coll Cardiol 2012;59:442–451. [DOI] [PubMed] [Google Scholar]
- (144).Wright JT Jr, Williamson JD, Whelton PK et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med 2015;373:2103–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (145).Ndumele CE, Coresh J, Lazo M et al. Obesity, subclinical myocardial injury, and incident heart failure. JACC Heart Fail 2014;2:600–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (146).Kitzman DW, Shah SJ. The HFpEF Obesity Phenotype: The Elephant in the Room. J Am Coll Cardiol 2016;68:200–203. [DOI] [PubMed] [Google Scholar]
- (147).Abraham WT, Adamson PB, Bourge RC et al. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: a randomised controlled trial. Lancet 2011;377:658666. [DOI] [PubMed] [Google Scholar]
- (148).Adamson PB, Abraham WT, Bourge RC et al. Wireless pulmonary artery pressure monitoring guides management to reduce decompensation in heart failure with preserved ejection fraction. Circ Heart Fail 2014;7:935–944. [DOI] [PubMed] [Google Scholar]
- (149).Kaye D, Shah SJ, Borlaug BA et al. Effects of an interatrial shunt on rest and exercise hemodynamics: results of a computer simulation in heart failure. J Card Fail 2014;20:212–221. [DOI] [PubMed] [Google Scholar]
- (150).Hasenfuss G, Hayward C, Burkhoff D et al. A transcatheter intracardiac shunt device for heart failure with preserved ejection fraction (REDUCE LAP-HF): a multicentre, openlabel, single-arm, phase 1 trial. Lancet 2016;387:1298–1304. [DOI] [PubMed] [Google Scholar]
- (151).Georgakopoulos D, Little WC, Abraham WT, Weaver FA, Zile MR. Chronic baroreflex activation: a potential therapeutic approach to heart failure with preserved ejection fraction. J Card Fail 2011;17:167–178. [DOI] [PubMed] [Google Scholar]
- (152).Meyns B, Klotz S, Simon A et al. Proof of concept: hemodynamic response to long-term partial ventricular support with the synergy pocket micro-pump. J Am Coll Cardiol 2009;54:79–86. [DOI] [PubMed] [Google Scholar]
- (153).Burkhoff D, Maurer MS, Joseph SM et al. Left atrial decompression pump for severe heart failure with preserved ejection fraction: theoretical and clinical considerations. JACC Heart Fail 2015;3:275–282. [DOI] [PubMed] [Google Scholar]
- (154).Shah SJ, Kitzman DW, Borlaug BA et al. Phenotype-Specific Treatment of Heart Failure With Preserved Ejection Fraction: A Multiorgan Roadmap. Circulation 2016;134:73–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (155).Redfield MM, Jacobsen SJ, Burnett JC Jr., Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: appreciating the scope of the heart failure epidemic. JAMA 2003;289:194–202. [DOI] [PubMed] [Google Scholar]
- (156).Gerber Y, Weston SA, Redfield MM et al. A contemporary appraisal of the heart failure epidemic in olmsted county, minnesota, 2000 to 2010. JAMA Intern Med 2015;175:9961004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (157).Perez de Isla L, Zamorano J, Hernandez N et al. Prognostic factors and predictors of in-hospital mortality of patients with heart failure with preserved left ventricular ejection fraction. J Cardiovasc Med (Hagerstown ) 2008;9:1011–1015. [DOI] [PubMed] [Google Scholar]
- (158).Tsuchihashi-Makaya M, Hamaguchi S, Kinugawa S et al. Characteristics and outcomes of hospitalized patients with heart failure and reduced vs preserved ejection fraction. Circ J 2009;73:1893–1900. [DOI] [PubMed] [Google Scholar]
- (159).Henkel D, Redfield M, Weston S, Gerber Y, Roger V. Death in heart failure. Circ Heart Fail 2008;1:91–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (160).Tribouilloy C, Rusinaru D, Mahjoub Hf et al. Prognosis of heart failure with preserved ejection fraction: a 5 year prospective population-based study. Eur Heart J 2008;29:339347. [DOI] [PubMed] [Google Scholar]
- (161).Lee DS, Gona P, Vasan RS et al. Relation of Disease Pathogenesis and Risk Factors to Heart Failure With Preserved or Reduced Ejection Fraction: Insights From the Framingham Heart Study of the National Heart, Lung, and Blood Institute. Circulation 2009;119:3070–3077. [DOI] [PMC free article] [PubMed] [Google Scholar]