Abstract
Background
Trunk block technique has been used in postoperative analgesia for patients undergoing surgery, specifically, transversus abdominis plane block (TAPB) and quadratus lumborum block (QLB) have been proved effective. The purpose of this meta-analysis is to evaluate the effects of TAPB and QLB in postoperative analgesia.
Methods
Online databases, including MEDLINE, EMBASE, Cochrane Library (&Trail), Web of Science, CNKI, Wanfang and QVIP were applied to collect the randomized controlled trials (RCTs) from inception to Dec. 9th, 2019. Twenty-two studies were finally included containing 777 patients in the TAPB group and 783 cases in QLB group. RCTs comparing TAPB and QLB in postoperative analgesia were included in this meta-analysis. The indicators including total analgesia consumption postoperatively, operative time, duration of anesthesia, visual analogue scale (VAS) score at 24 h postoperatively, duration of postoperative analgesia, the number of patients requiring analgesia postoperatively and adverse reactions were analyzed.
Results
our findings showed that morphine consumption (mg) (WMD = 3.893, 95%CI: 2.053 to 5.733, P < 0.001), fentanyl consumption (μg) (WMD = 23.815, 95%CI: 15.521 to 32.109, P < 0.001), VAS score at 24 h postoperatively (WMD = 0.459, 95%CI: 0.118 to 0.801, P = 0.008), the number of patients requiring analgesia postoperatively (WMD = 3.893, 95%CI: 2.053 to 5.733, P < 0.001), and the incidence of dizziness (WMD = 2.691, 95%CI: 1.653 to 4.382, P < 0.001) in TAPB group were higher than in QLB group.
Conclusions
QLB is superior to TAPB in reducing morphine consumption, fentanyl consumption, VAS score at 24 h postoperatively, the number of patients requiring analgesia postoperatively, and the incidence of dizziness.
Keywords: Transversus abdominis plane block, Quadratus lumborum block, Postoperative analgesia, Outcomes
Background
Postoperative pain, including acute postoperative pain and persistent chronic postoperative pain, remains a main clinical problem. Without timely and effective treatment, acute postoperative pain can turn into persistent chronic postoperative pain [1]. Previous studies showed that 10–50% of patients undergoing surgery suffered from postoperative pain lasting more than 1 month, and 2–10% of these patients continued to experience moderate to severe chronic pain. Furthermore, inadequate postoperative analgesia continues to occur despite advances in analgesia techniques [2, 3]. Inadequate management of postoperative pain can lead to serious consequences, such as poor immediate postoperative effect, prolonged stay and/or hospital readmission, poor patient satisfaction, increased burden on patients and health systems [3, 4]. Therefore, effective prevention and control of postoperative pain is of great significance.
Multimodal analgesia technique has been widely applied in postoperative analgesia [3, 5]. Truncal block, including transversus abdominis plane block (TAPB), quadratus lumborum block (QLB), rectus sheath block and hernia block, plays important roles in multimodal analgesia [6, 7]. TAPB involves injecting local anesthetic into the plane between the transverse abdominis and the internal oblique, it can block the sensory nerve supply to the anterior abdominal wall by deposition of local anesthetics and has shown promising in managing postoperative pain [8–10]. QLB, similar to TAPB, was first introduced as a different form of TAPB in 2007 [11]. It is also known as an interfascial plane block because it involves injecting local anesthetics into the thoracolumbar fascia which is different from TAPB. QLB can result in a widespread sensory suppression via a wide distribution of local anesthetics, and has been increasingly used for postoperative analgesia [11–14].
In recent years, many randomized controlled trials (RCTs) have been conducted to compare the effects of TAPB and QLB in postoperative analgesia [6, 15–18]. However, the results of outcomes of postoperative analgesia were inconsistent. In the current study, we aimed to compare the efficacy of TAPB versus QLB in postoperative analgesia based on RCT articles with a meta-analysis. The indicators for this meta-analysis included total analgesia consumption postoperatively, operative time, duration of anesthesia, visual analogue scale (VAS) score at 24 h postoperatively, duration of postoperative analgesia, the number of patients requiring analgesia postoperatively and adverse reactions.
Methods
Search strategy
The literatures were retrieved from MEDLINE, EMBASE, Cochrane Library (&Trail), Web of Science, CNKI, Wanfang and QVIP the deadline for searching documents was Dec. 9th, 2019. The index words for searching literatures as follows: ‘transversus abdominis’ OR ‘transversus abdominis plane block’ OR ‘transverse abdominis’ OR ‘transverse abdominis plane block’ OR ‘TAP’ OR ‘TAP block’ OR ‘TAPB’ AND ‘quadratus lumborum’ OR ‘quadratus lumborum block’ OR ‘quadrate lumborum’ OR ‘quadrate lumborum block’ OR ‘QL’ OR ‘QL block’ OR ‘QLB’.
Inclusion and exclusion criteria
Inclusion criteria: (1) RCTs; (2) comparison of TAPB and QLB in postoperative analgesia; (3) English and Chinese literatures; (4) outcome indicators: total analgesia consumption postoperatively, operative time, duration of anesthesia, VAS score at 24 h postoperatively, duration of postoperative analgesia, the number of patients requiring analgesia postoperatively and adverse reactions.
Exclusion criteria: (1) reviews, meta-analyses, conference articles and letters; (2) animal experiments; (3) repetitive studies; (4) articles that cannot extract the valid data.
Methodological quality appraisal
The studies were screened independently by two researchers Y Wang and X Wang. In the event of disagreements, a third party (K Zhang) would participate in the discussion. The modified Jadad scale (Table 1) was applied to evaluate the quality of literatures. The scale was divided into 7 points, 1–3 were defined as low quality, and 4–7 were defined as high quality.
Table 1.
The modified Jaded Scale
| Classification | Score | Description |
|---|---|---|
| Randomization | ||
| Inappropriate | 0 | Semi-randomized or quasi-randomized trials |
| Unclear | 1 | Randomized trials without describing methods for generating random sequences |
| Appropriate | 2 | Random sequences produced by a computer or a random number table |
| Allocation concealment | ||
| Inappropriate | 0 | Regular grouping |
| Unclear | 1 | Only use of a random number table or other random assignment scheme |
| Appropriate | 2 | A method for assigning sequences without prediction |
| Blinding | ||
| Inappropriate | 0 | Use of double blindness without an appropriate method |
| Unclear | 1 | Only mention of double blindness |
| Appropriate | 2 | A description of the specific and appropriate method of double blindness |
| Withdrawals or dropouts | ||
| No | 0 | No description of withdrawal or dropouts |
| Yes | 1 | A description of withdrawal or dropouts |
Statistical analysis
Heterogeneity test was conducted for each indicator and measured by statistics of I2, with I2 > 50% indicating significant heterogeneity. If I2 > 50%, a random effects model was used; if I2 < 50%, the fixed effects model was applied, and the heterogeneity was assessed. The software Stata 15.0 (Stata Corporation, College Station, TX, USA) was used for statistical analysis, effect index relative risk (RR) was used for enumeration data and weighted mean difference (WMD) for measurement data. P < 0.05 was considered statistically significant.
Results
Included studies
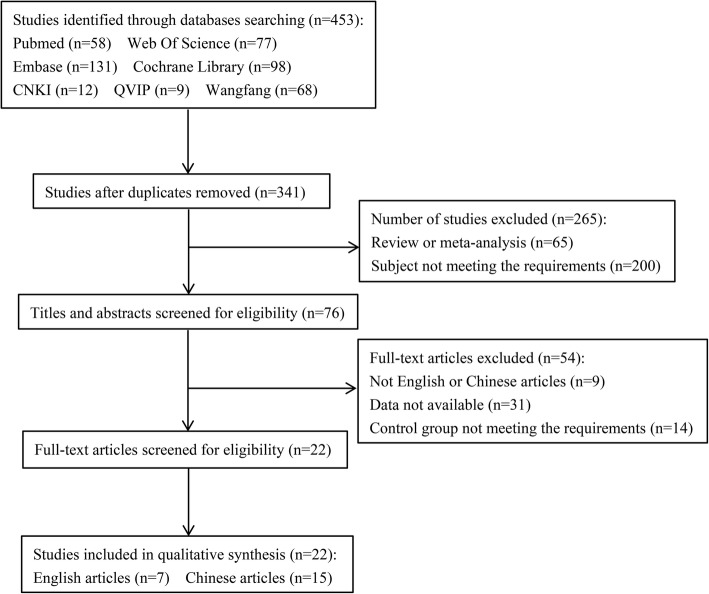
According to the search strategy, literature searches via the databases identified 453 articles. Following removing duplicates, screening titles or abstracts, and after assessing the full texts of relevant studies, 22 articles [6, 15–35] were finally included containing 777 patients in the TAPB group and 783 cases in QLB group (Table 2 and Fig. 1).
Table 2.
Characteristics of studies included in meta-analysis
| Author | Year | Country | Score | Treatment | TAPB_n (M/F) | TAPB_age# (years) | QLB_n (M/F) | QLB_age# (years) | Quality | Outcomes |
|---|---|---|---|---|---|---|---|---|---|---|
| Baytar | 2019 | Turkey | 4 | TAPB vs QLB | 53 (11/42) | 48.12 ± 12.42 | 54 (15/39) | 46.42 ± 16.57 | HQ | b f g |
| Yousef | 2018 | Egypt | 5 | TAPB vs QLB | 30 (0/30) | 50.70 ± 6.8 | 30 (0/30) | 56.5 ± 6.97 | HQ | a b c d e f |
| Kumar | 2018 | India | 4 | TAPB vs QLB | 35 (15/20) | 38.34 ± 11.59 | 35 (15/19) | 39.20 ± 11.64 | HQ | a b d f |
| Öksüz | 2017 | Turkey | 3 | TAPB vs QLB | 25 (21/4) | 3.02 ± 1.82 | 25 (21/4) | 3.13 ± 0.20 | LQ | e f |
| Blanco | 2016 | Arab | 3 | TAPB vs QLB | 38 (0/38) | NA | 38 (0/38) | NA | LQ | a |
| Verma | 2019 | India | 6 | TAPB vs QLB | 30 (0/30) | 28 ± 3 | 30 (0/30) | 30 ± 3 | HQ | b d f |
| Ipek | 2019 | Turkey | 3 | TAPB vs QLB | 29 (19/10) | 4.16 ± 2.55 | 35 (28/7) | 3.89 ± 3.26 | LQ | e f g |
| Shan | 2019 | China | 3 | TAPB vs QLB | 30 (0/30) | 30 ± 3 | 30 (0/30) | 29 ± 6 | LQ | c f |
| Deng | 2019 | China | 6 | TAPB vs QLB | 34 (12/22) | 53.5 ± 10.6 | 34 (14/20) | 51.1 ± 13.8 | HQ | b c f |
| Fu | 2019 | China | 4 | TAPB vs QLB | 30 (NA) | 71.8 ± 5.8 | 30 (NA) | 72.2 ± 6.9 | HQ | b f |
| Han | 2017 | China | 4 | TAPB vs QLB | 38 (24/14) | 27.8 ± 3.9 | 39 (20/19) | 26.3 ± 3.2 | HQ | b c f |
| He | 2018 | China | 2 | TAPB vs QLB | 36 (20/16) | 67.3 ± 2.3 | 36 (19/17) | 67.7 ± 2.1 | LQ | e f |
| Li G | 2018 | China | 5 | TAPB vs QLB | 40 (0/40) | 31 ± 4 | 40 (0/40) | 30 ± 5 | HQ | b c f |
| Li N | 2019 | China | 3 | TAPB vs QLB | 30 (0/30) | 42.10 ± 5.26 | 30 (0/30) | 41.07 ± 4.75 | LQ | b e f |
| Ma | 2019 | China | 3 | TAPB vs QLB | 30 (17/13) | 55. 2 ± 4. 4 | 30 (16/14) | 53.1 ± 4.6 | LQ | e |
| Ren | 2018 | China | 3 | TAPB vs QLB | 82 (44/38) | 45.7 ± 15.2 | 78 (40/38) | 46.3 ± 15.1 | LQ | b c |
| Xia | 2018 | China | 4 | TAPB vs QLB | 30 (15/15) | 48 ± 8 | 30 (12/18) | 46 ± 11 | HQ | f |
| Yang | 2019 | China | 3 | TAPB vs QLB | 30 (0/30) | NA | 30 (0/30) | NA | LQ | a b |
| Yang | 2019 | China | 5 | TAPB vs QLB | 30 (0/30) | 38.5 ± 14.8 | 30 (0/30) | 43.9 ± 15.04 | HQ | b c e f |
| Ye | 2019 | China | 4 | TAPB vs QLB | 28 (12/16) | 48.9 ± 2.1 | 30 (14/16) | 50.3 ± 2.8 | HQ | c f |
| Zhu | 2019 | China | 3 | TAPB vs QLB | 39 (20/19) | 68.8 ± 3.4 | 39 (18/21) | 69.1 ± 3.2 | LQ | e f |
| Zhu | 2018 | China | 3 | TAPB vs QLB | 30 (0/30) | 52 ± 6 | 30 (0/30) | 51 ± 7 | LQ | b e f |
#: mean ± standard deviation
TAPB transversus abdominis plane block, QLB quadratus lumborum block, VAS visual analog scale, HQ high-quality, LQ low-quality, NA unavailable
a: morphine consumption; b: VAS score at 24 h postoperatively; c: fentanyl consumption; d: duration of postoperative analgesia; e: the number of patients requiring analgesia postoperatively; f: operative time; g: duration of anesthesia
Fig. 1.
Flow chart of the review process
Overall meta-analysis
As shown in Table 3, our findings showed that morphine consumption (mg) (WMD = 3.893, 95%CI: 2.053 to 5.733, P < 0.001), fentanyl consumption (μg) (WMD = 23.815, 95%CI: 15.521 to 32.109, P < 0.001), VAS score at 24 h postoperatively (WMD = 0.459, 95%CI: 0.118 to 0.801, P = 0.008), the number of patients requiring analgesia postoperatively (WMD = 3.893, 95%CI: 2.053 to 5.733, P < 0.001), and the incidence of dizziness (RR = 2.691, 95%CI: 1.653 to 4.382, P < 0.001) in TAPB group were higher than in QLB group. No significant differences were observed between the two groups regarding the operative time (min) (P = 0.573), duration of anesthesia (min) (P = 0.733), duration of postoperative analgesia (h) (P = 0.258), and nausea and vomiting (P = 0.141).
Table 3.
Overall results of the meta-analysis
| Outcomes | WMD/RR (95%CI) | P | I2 |
|---|---|---|---|
| Morphine consumption (mg) | |||
| Overall | 3.893 (2.053, 5.733) | < 0.001 | 72.7 |
| Operation types | |||
| Abdominal surgery | 2.400 (1.825, 2.975) | < 0.001 | NA |
| Pelvic surgery | 4.731 (2.634, 6.829) | < 0.001 | 44.5 |
| Quality | |||
| High-quality | 3.205 (1.283, 5.127) | 0.001 | 76.2 |
| Low-quality | 6.443 (0.098, 12.788) | 0.047 | 72.2 |
| Fentanyl consumption (μg) | |||
| Overall | 23.815 (15.521, 32.109) | < 0.001 | 96.0 |
| Operation types | |||
| Abdominal surgery | 14.077 (7.412, 20.742) | < 0.001 | 92.3 |
| Pelvic surgery | 34.808 (14.079, 55.537) | 0.001 | 96.5 |
| Quality | |||
| High-quality | 26.576 (13.594, 39.558) | < 0.001 | 96.9 |
| Low-quality | 16.264 (7.527, 25.000) | < 0.001 | 73.3 |
| Operative time | |||
| Overall | 0.324 (−0.805, 1.454) | 0.573 | 0.0 |
| Duration of anesthesia (min) | |||
| Overall | -2.139 (−14.423, 10.146) | 0.733 | 80.8 |
| VAS score at 24 h postoperatively | |||
| Overall | 0.459 (0.118, 0.801) | 0.008 | 94.8 |
| Operation types | |||
| Abdominal surgery | 0.224 (−0.033, 0.480) | 0.088 | 80.1 |
| Pelvic surgery | 0.671 (0.103, 1.240) | 0.021 | 95.4 |
| Quality | |||
| High-quality | 0.576 (0.048, 1.104) | 0.032 | 96.3 |
| Low-quality | 0.218 (−0.019, 0.455) | 0.071 | 66.1 |
| Duration of postoperative analgesia | |||
| Overall | -21.882 (−59.774, 16.010) | 0.258 | 100.0 |
| Operation types | |||
| Abdominal surgery | -3.400 (−4.038, −2.762) | < 0.001 | NA |
| Pelvic surgery | −31.125 (−78.851, 16.600) | 0.201 | 100.0 |
| Number of patients requiring analgesia postoperatively | |||
| Overall | 2.618 (2.040, 3.361) | < 0.001 | 13.2 |
| Adverse reactions | |||
| Dizziness | |||
| Overall | 2.691 (1.653, 4.382) | < 0.001 | 0.0 |
| Nausea and vomiting | |||
| Overall | 1.918 (0.805, 4.571) | 0.141 | 50.9 |
| Quality | |||
| High-quality | 4.100 (1.932, 8.699) | < 0.001 | 0.0 |
| Low-quality | 0.417 (0.054, 3.239) | 0.403 | 70.9 |
CI confidence interval, RR, risk ratio, WMD weighted mean difference, VAS visual analog scal, NA unavailable
Total analgesia consumption postoperatively
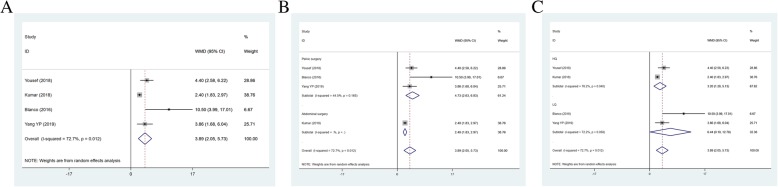
Total analgesia consumption postoperatively (mg) as an outcome was reported containing 4 studies (n = 266) on morphine consumption (mg) and 8 articles (n = 623) on fentanyl consumption (μg). Patients in TAPB group consumed more morphine than QLB group (WMD = 3.893, 95%CI: 2.053 to 5.733; P < 0.001) (Table 3 and Fig. 2a). Heterogeneity among the included studies was statistically significant (I2 = 72.7%). Subgroup analysis was performed to identify sources of heterogeneity. According to operation types and literature quality, there were significant differences in abdominal surgery (WMD = 2.400, 95%CI: 1.825 to 2.975, P < 0.001), pelvic surgery (WMD: 4.731, 95%CI: 2.634 to 6.829, P < 0.001), high-quality (WMD = 3.205, 95%CI: 1.283 to 5.127, P = 0.001) and low-quality (WMD = 6.443, 95%CI: 0.098 to 12.788, P = 0.047) between the two groups (Fig. 2b and c). The fentanyl consumption in TAPB group was higher than that in QLB group (WMD = 23.815, 95%CI: 15.521 to 32.109, P < 0.001) (Table 3 and Fig. 3a). We also found statistical differences in abdominal surgery (WMD = 14.077, 95%CI: 7.412 to 20.742, P < 0.001), pelvic surgery (WMD: 34.808, 95%CI: 14.079 to 55.537, P < 0.001), high-quality (WMD = 26.576, 95%CI: 13.594 to 39.558, P < 0.001) and low-quality (WMD = 16.264, 95%CI: 7.527 to 25.000, P < 0.001) between the two groups (Fig. 3b and c).
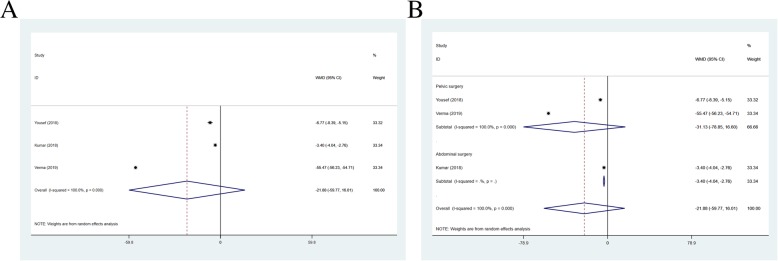
Fig. 2.
Forest plot for morphine consumption (a), operation types (b) and literature quality (c)
Fig. 3.
Forest plot for of fentanyl consumption (a), operation types (b) and literature quality (c)
Operative time
Eighteen articles (n = 1204) on operative time (min) were included containing 597 patients in TAPB group and 607 patients in QLB group. The operative time in TAPB group was similar to QLB group, with no significant differences (WMD = 0.324, 95%CI: − 0.805 to 1.454, P = 0.573).
Duration of anesthesia
The data of duration of anesthesia (min) as a clinical outcome was extracted from 2 articles including 171 cases. Duration of anesthesia in TAPB group was near to QLB group, with no significant differences (WMD = -2.139, 95%CI: − 14.423 to10.146, P = 0.733).
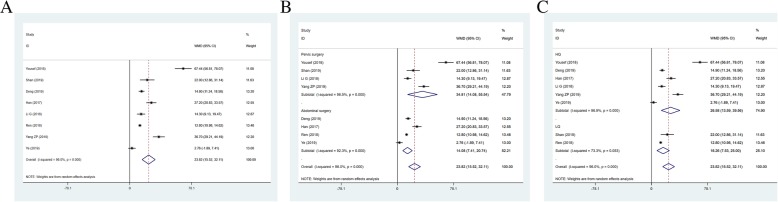
VAS score at 24 h postoperatively
Thirteen studies, including 982 patients, reported VAS score at 24 h postoperatively for pain as an outcome (I2 = 94.8%). The VAS score at 24 h postoperatively in TAPB group was higher than that in QLB group (WMD = 0.459, 95% CI: 0.118 to 0.801; P = 0.008) (Fig. 4a). The results of subgroup analysis showed statistical differences in pelvic surgery (WMD = 0.671, 95% CI: 0.103 to 1.240, P = 0.021) and high-quality (WMD = 0.576, 95% CI: 13.594 to 39.558, P < 0.001) (Fig. 4b and c).
Fig. 4.
Forest plot for VAS score at 24 h postoperatively (a), operation types (b) and literature quality (c)
Duration of postoperative analgesia
The duration of postoperative analgesia (h) was reported as an outcome in 3 studies (n = 190) (I2 = 100.00%). Duration of postoperative analgesia in TAPB group was shorter than QLB group (WMD = -21.882, 95% CI: − 59.774 to 16.010, P = 0.258) (Fig. 5a). The findings also showed differences in abdominal surgery (WMD = -3.400, 95% CI: − 4.038 to − 2.762, P < 0.001) (Fig. 5b).
Fig. 5.
Forest plot for duration of postoperative analgesia (a) and operation types (b)
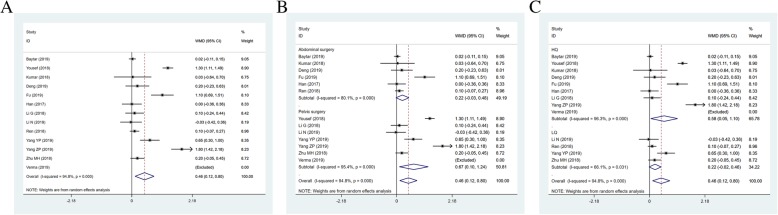
The number of patients requiring analgesia postoperatively
Nine studies (564 patients) on the number of patients requiring analgesia postoperatively were analyzed (I2 = 13.2%). The results founded that the number of patients requiring analgesia after surgery in TAPB group were higher than QLB group (RR = 2.618, 95% CI: 2.040 to 3.361, P < 0.001).
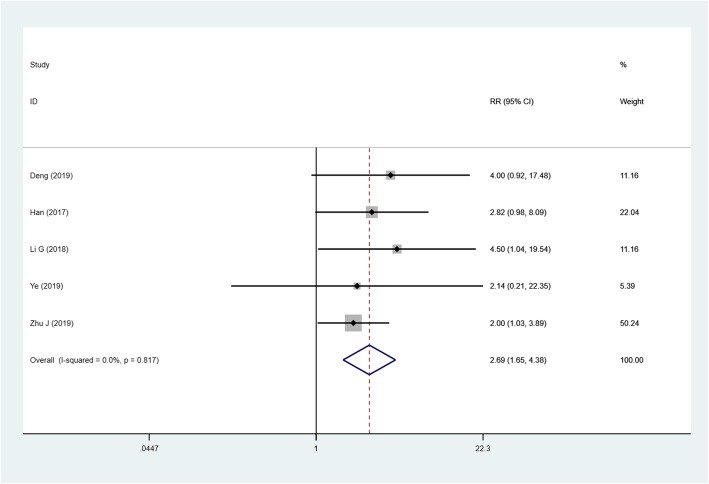
Adverse reactions
The incidence of dizziness in TAPB group from 5 articles was (n = 361) higher than that in QLB group (I2 = 0.0%, RR = 2.691, 95% CI: 1.653 to 4.382, P < 0.001) (Fig. 6). 8 studies (n = 535) on the incidence of nausea and vomiting were no differences between the two groups (I2 = 50.9%, RR = 1.918, 95% CI: 0.805 to 4.571, P = 0.141).
Fig. 6.
Forest plot for the incidence of dizziness
Publication bias
Publication bias was performed using Begg’ test. There were no distinct publication bias in morphine consumption (Z = 1.36, P = 0.174), operative time (Z = 1.17, P = 0.240), duration of anesthesia (Z = 1.00, P = 0.317), VAS score at 24 h postoperatively (Z = 1.10, P = 0.273), duration of postoperative analgesia (Z = -1.00, P = 0.317), the number of patients requiring analgesia postoperatively (Z = -0.42, P = 0.677), the incidence of dizziness (Z = 0.49, P = 0.624), and nausea and vomiting (Z = -0.12, P = 1.000), except fentanyl consumption (Z = 2.23, P = 0.026).
Discussion
Twenty-two studies [6, 15–20] on effects of TAPB vs. QLB in postoperative analgesia were included in this meta-analysis. Overall results showed that QLB showed more effective analgesia than TAPB in regards to morphine consumption, fentanyl consumption, VAS score at 24 h postoperatively, the number of patients requiring analgesia postoperatively, and the incidence of dizziness.
Pain was regarded as the fifth vital sign by the joint commission on accreditation of medical institutions (JCAHO) in 2000, ignoring pain management equals disrespecting human rights [36]. Postoperative pain is a major concern for patients and clinicians. Inadequate management of postoperative pain remains a common clinical problem worldwide [3, 4, 37]. TAPB has been described as a successful adjunct procedure for postoperative analgesia, however with some complications: failure of block, abdominal organ injury, nerve injury, vascular injury and so on [38–40]. Fortunately, the application of ultrasound can display injection point, the tap plane and the needle. With the guidance of ultrasound, the accuracy of puncture is improved, and the related complications are reduced [13, 41]. However, TAPB only blocks the anterolateral skin, muscles and parietal peritoneal sensory nerve fibers of the abdominal wall, and has no inhibitory effect on visceral pain [42]. QLB, as an effective and reliable option for relieving postoperative pain, is performed exclusively under the guidance of ultrasound, and the passage of the needle and the site of the local anesthetic application are far from the abdominal organs, great vessels and peritoneal cavity [43–47]. QLB can block the sympathetic nerves distributed between the thoracolumbar fascias. Some scholars suggested that QLB may alleviate the visceral pain to a certain extent [48]. Compared with TAPB, the drug diffusion range of QLB drugs was relatively wide, even reaching the paravertebral space of chests [49].
In this meta-analysis, VAS score at 24 h postoperatively of TAPB group was higher than that of QLB group, which may cause high consumption of analgesics. We also found that morphine and fentanyl consumption postoperatively in TAPB group were higher than QLB group. Similarly, a previous study showed that QLB type 1 significantly reduced morphine consumption up to postoperative 48 h [50]. Salama et al. found that QLB performed after cesarean section provided an ideal effect in reducing total postoperative morphine consumption [44]. The reason why the patients in TAPB group consumed more morphine than QLB group may be that TAPB only provides effective somatic analgesia, however poor effect in visceral analgesia [47]. Yousef reported that patients undergoing hysterectomy bilateral QLB provided more effective intraoperative and postoperative analgesia with less intraoperative fentanyl consumption and less postoperative morphine consumption compared with bilateral TAPB [18]. As we all know, morphine and fentanyl are common analgesic drugs for pain, and excessive use may cause several adverse reactions. Herein, it is significant for postoperative analgesia to explore an adjunct procedure that can reduce analgesia consumption.
The number of patients requiring analgesia postoperatively in QLB group was less than TAPB group. Zhu et al. [51] have studied the rate at patients who receive QLB requested analgesia postoperatively. They performed ultrasound-guided subcostal approach to QLB in an ipsilateral parasagittal oblique plane at the L1-L2 level on patients who underwent laparoscopic nephrectomy, and they reported that QLB was related with reducing rate of patients requiring rescue analgesia postoperatively. There were no significant differences in the operative time, duration of anesthesia, duration of postoperative analgesia, and nausea and vomiting between the two groups. The reasons may be less number of articles and small sample size included in this study. More high-quality studies with large samples are needed to further verify these results.
Because of representing the high level of evidences, the meta-analysis of RCTs can help patients, doctors and policy-makers to make decisions [52]. This meta-analysis was conducted to compare the effect of TAPB and QLB on postoperative analgesia based on RCT studies. However, several limitations of this study should be noted. First, heterogeneity existed in some measurements, and subgroup analyses failed to change the heterogeneity. Furthermore, there was a publication bias in fentanyl consumption, which may be attributed to the fact that the positive results were easy to publish, and only one English article and 2 low-quality studies were included in this meta-analysis. These factors mentioned above may affect our results. Therefore, the current results should be interpreted with caution.
Conclusions
In summary, compared with TAPB, QLB provided effective intraoperative and postoperative analgesia with less morphine consumption, less fentanyl consumption, lower VAS score at 24 h postoperatively, decreased number of patients requiring analgesia postoperatively, and reduced incidence of dizziness. In addition, QLB is comparable with TAPB as regards to operative time, duration of anesthesia, and the incidence of nausea and vomiting. More researches with well-designed and adequate sample size are required to confirm these findings.
Acknowledgements
Not applicable.
Abbreviations
- TAPB
Transversus abdominis plane block
- QLB
Quadratus lumborum block
- RCTs
Randomized controlled trials
- VAS
Visual analogue scale
- RR
Relative risk
- WMD
Weighted mean difference
- JCAHO
Joint commission on accreditation of medical institutions
Authors’ contributions
All authors conceived and designed the study. YQW and XJW participated in manuscript writing, data collection and data analysis. KYZ critically reviewed and edited the manuscript. All authors read and approved the final manuscript.
Funding
No funding.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yanqing Wang and Xiaojia Wang contributed equally to this work.
References
- 1.Lovich-Sapola J, Smith CE, Brandt CP. Postoperative pain control. Surg Clin N Am. 2015;95(2):301–318. doi: 10.1016/j.suc.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Grosu I, de Kock M. New concepts in acute pain management: strategies to prevent chronic postsurgical pain, opioid-induced hyperalgesia, and outcome measures. Anesthesiol Clin. 2011;29(2):311–327. doi: 10.1016/j.anclin.2011.04.001. [DOI] [PubMed] [Google Scholar]
- 3.Rawal N. Current issues in postoperative pain management. Eur J Anaesthesiol. 2016;33(3):160–171. doi: 10.1097/EJA.0000000000000366. [DOI] [PubMed] [Google Scholar]
- 4.Wu MS, Chen KH, Chen IF, Huang SK, Tzeng PC, Yeh ML, Lee FP, Lin JG, Chen C. The efficacy of acupuncture in post-operative pain management: a aystematic review and meta-analysis. PLoS One. 2016;11(3):e0150367. doi: 10.1371/journal.pone.0150367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chandon M, Bonnet A, Burg Y, Barnichon C, DesMesnards-Smaja V, Sitbon B, Foiret C, Dreyfus JF, Rahmani J, Laloe PA, et al. Ultrasound-guided transversus abdominis plane block versus continuous wound infusion for post-caesarean analgesia: a randomized trial. PLoS One. 2014;9(8):e103971. doi: 10.1371/journal.pone.0103971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oksuz G, Bilal B, Gurkan Y, Urfalioglu A, Arslan M, Gisi G, Oksuz H. Quadratus lumborum block versus transversus abdominis plane block in children undergoing low abdominal surgery: a randomized controlled trial. Reg Anesth Pain Med. 2017;42(5):674–679. doi: 10.1097/AAP.0000000000000645. [DOI] [PubMed] [Google Scholar]
- 7.Chakraborty A, Khemka R, Datta T. Ultrasound-guided truncal blocks: a new frontier in regional anaesthesia. Indian J anaesth. 2016;60(10):703–711. doi: 10.4103/0019-5049.191665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dal Moro F, Aiello L, Pavarin P, Zattoni F. Ultrasound-guided transversus abdominis plane block (US-TAPb) for robot-assisted radical prostatectomy: a novel '4-point' technique-results of a prospective, randomized study. J Robot Surg. 2019;13(1):147–151. doi: 10.1007/s11701-018-0858-6. [DOI] [PubMed] [Google Scholar]
- 9.Sun N, Wang S, Ma P, Liu S, Shao A, Xiong L. Postoperative analgesia by a transversus abdominis plane block using different concentrations of ropivacaine for abdominal surgery: a meta-analysis. Clin J Pain. 2017;33(9):853–863. doi: 10.1097/AJP.0000000000000468. [DOI] [PubMed] [Google Scholar]
- 10.Ghisi D, Fanelli A, Vianello F, Gardini M, Mensi G, La Colla L, Danelli G. Transversus abdominis plane block for postoperative analgesia in patients undergoing total laparoscopic hysterectomy: a randomized, controlled, observer-blinded trial. Anesth Analg. 2016;123(2):488–492. doi: 10.1213/ANE.0000000000001267. [DOI] [PubMed] [Google Scholar]
- 11.Yuan Q, Cui X, Fei Y, Xu Z, Huang Y. Transmuscular quadratus lumborum block versus thoracic paravertebral block for acute pain and quality of recovery after laparoscopic renal surgery: study protocol for a randomized controlled trial. Trials. 2019;20(1):276. doi: 10.1186/s13063-019-3359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bjelland TW, Yates TGR, Fagerland MW, Froyen JK, Lysebraten KR, Spreng UJ. Quadratus lumborum block for postoperative analgesia after full abdominoplasty: a randomized controlled trial. Scand J Pain. 2019;19(4):671–8. [DOI] [PubMed]
- 13.Bak H, Bang S, Yoo S, Kim S, Lee SY. Continuous quadratus lumborum block as part of multimodal analgesia after total hip arthroplasty: a case report. Korean J Anesthesiol. 2020;73(2):158–62. [DOI] [PMC free article] [PubMed]
- 14.Dhanjal S, Tonder S. Quadratus Lumborum block. In: StatPearls. Edn. Treasure Island (FL): StatPearls Publishing StatPearls Publishing LLC; 2019. [PubMed] [Google Scholar]
- 15.Kumar GD, Gnanasekar N, Kurhekar P, Prasad TK. A comparative study of transversus abdominis plane block versus quadratus lumborum block for postoperative analgesia following lower abdominal surgeries: a prospective double-blinded study. Anesth Essays Res. 2018;12(4):919–923. doi: 10.4103/aer.AER_158_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baytar C, Yilmaz C, Karasu D, Topal S. Comparison of ultrasound-guided subcostal transversus abdominis plane block and quadratus lumborum block in laparoscopic cholecystectomy: a prospective, randomized, controlled clinical ptudy. Pain Res Manag. 2019;2019:2815301. doi: 10.1155/2019/2815301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blanco R, Ansari T, Riad W, Shetty N. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg Anesth Pain Med. 2016;41(6):757–762. doi: 10.1097/AAP.0000000000000495. [DOI] [PubMed] [Google Scholar]
- 18.Yousef NK. Quadratus lumborum block versus transversus abdominis plane block in patients undergoing total abdominal hysterectomy: a randomized prospective controlled trial. Anesth Essays Res. 2018;12(3):742–747. doi: 10.4103/aer.AER_108_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Verma K, Malawat A, Jethava D, Jethava DD. Comparison of transversus abdominis plane block and quadratus lumborum block for post-caesarean section analgesia: a randomised clinical trial. Indian J Anaesth. 2019;63(10):820–826. doi: 10.4103/ija.IJA_61_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ipek CB, Kara D, Yilmaz S, Yesiltas S, Esen A, Dooply S, Karaaslan K, Turkoz A. Comparison of ultrasound-guided transversus abdominis plane block, quadratus lumborum block, and caudal epidural block for perioperative analgesia in pediatric lower abdominal surgery. Turk J Med Sci. 2019;49(5):1395–1402. doi: 10.3906/sag-1812-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shan T, Bao HG. Efficiency of ultrasound-guided quadratus lumborum block for postoperative analgesia in puerperants underwent cesarean section. Jiangsu Med J. 2019;45(7):704–706. [Google Scholar]
- 22.Zheng W: Application of quaratus lumborum block versus transversus abdominis plane block on enhanced recovery after laparoscopic radical resection of colorectal cancer. Master. Nanchang University; 2019.
- 23.Ma CZ, Chen QY, Lin ZX, Zhang CC, Zhang Z. Effect of ultrasound-guided quadratus lumborum block for peritoneal dialysis catheter placement. J Clin Anesthesiol. 2019;35(10):961–964. [Google Scholar]
- 24.Fu K, Wei JY, Zhou FF, Hu QH. Comparison for the analgesic effect after inguinal herniorrhaphy in the elderly. Jiangxi Med J. 2019;54(5):551–553. [Google Scholar]
- 25.Han B, Wang B, He AP. Comparison of ultrasound-guided quadratus lumborum block and transversus abdominis plane block combined with patient controlled intravenous analgesia with sufentanil on post-operation analgesia after appendectomy. J Clin Anesthesiol. 2017;33(10):984–986. [Google Scholar]
- 26.Ye P, Lin YL, Liu YJ, Yu ZG. Comparison of analgesia effects between ultrasound-guided quadratus lumborum block and transversus abdominis plane block with assistance of patient controlled intravenous analgesia after laparoscopic cholecystectomy. J Trauma Emerg. 2019;7(2):93–97. doi: 10.29252/beat-070201. [DOI] [Google Scholar]
- 27.Yang ZP, Zhao WB. Effects of ultrasound-guided quadrate lumbar block and transverse abdominal block on postoperative analgesia of gynecological tumors. Sichuan Med J. 2019;40(6):566–570. [Google Scholar]
- 28.Zhu J, Ma JL, Gao YP. Effect of low back quadratus block and transverse abdominis block on postoperative analgesia in elderly patients undergoing radical gastrectomy. Guizhou Med J. 2019;43(9):1368–1371. [Google Scholar]
- 29.Li N, Yue XQ. Analgesia effect study of ultrasound-guided lumbar quadratus block after laparoscopic myomectomy. Smart Healthcare. 2019;5(9):102–105. [Google Scholar]
- 30.Yang YP, Sun ZP, Xu JJ. Comparison of analgesic effect of dexmedetomidine combined with different nerve block pathways after cesarean section. Zhejiang Med J. 2019;21(9):1275–1276. [Google Scholar]
- 31.Xia ZY, Bu HL, Wang ZF, Wang ZY, Zhang W. Efficiency of ultrasound-guided quadratus lumborum block for analgesia after laparoscopic cholecystectomy. Clin J Anesthesiol. 2018;38(8):950–952. [Google Scholar]
- 32.Ren BL, Feng AM, Qiao YS, Wang JW, Lu XH. Comparison of the analegesic effect between quadratus lumborum block and transversus abdominis plane block in laparoscopic operation. J Xinxiang Med Univ. 2018;35(8):719–721. [Google Scholar]
- 33.Zhu MH, Tang Y, Xu Q, Qin Q. Chen Y: quadratus lumborum block versus transversus abdominis plane block for analgesia after total abdominal hysterectomy. Int J Anesth Resus. 2018;39(8):741–745. [Google Scholar]
- 34.He WQ, Li YS, Zhang XH, Yi B, Lu KZ. Comparison of quadratus lumborum block and transversus abdominis plane block for postoperative analgesia in elderly patients undergoing abdominal surgery. Clin J Anesthesiol. 2018;38(1):40–43. [Google Scholar]
- 35.Li G, Mamat R, Gai DX. Postoperative analgesia efficacy of quadratus lumborum block versus transversus abdominis plane block in patients undergoing caesarean section. Int J Anesth Resus. 2018;39(4):338–340. [Google Scholar]
- 36.White PF, Kehlet H. Improving pain management: are we jumping from the frying pan into the fire? Anesth Analg. 2007;105(1):10–12. doi: 10.1213/01.ane.0000268392.05157.a8. [DOI] [PubMed] [Google Scholar]
- 37.Mahama F, Ninnoni JPK. Assessment and management of postoperative pain among nurses at a resource-constraint teaching hospital in Ghana. Nurs Res Pract. 2019;2019:9091467. doi: 10.1155/2019/9091467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Baeriswyl M, Zeiter F, Piubellini D, Kirkham KR, Albrecht E. The analgesic efficacy of transverse abdominis plane block versus epidural analgesia: a systematic review with meta-analysis. Medicine. 2018;97(26):e11261. doi: 10.1097/MD.0000000000011261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Soltani Mohammadi S, Dabir A, Shoeibi G: Efficacy of transversus abdominis plane block for acute postoperative pain relief in kidney recipients: a double-blinded clinical trial. Pain Med (Malden, Mass) 2014, 15(3):460–464. [DOI] [PubMed]
- 40.Baker BW, Villadiego LG, Lake YN, Amin Y, Timmins AE, Swaim LS, Ashton DW. Transversus abdominis plane block with liposomal bupivacaine for pain control after cesarean delivery: a retrospective chart review. J Pain Res. 2018;11:3109–3116. doi: 10.2147/JPR.S184279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jin Y, Li Y, Zhu S, Zhu G, Yu M. Comparison of ultrasound-guided iliohypogastric/ilioinguinal nerve block and transversus abdominis plane block for analgesia after cesarean section: a retrospective propensity match study. Exp Ther Med. 2019;18(1):289–295. doi: 10.3892/etm.2019.7540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kargar R, Minas V, Gorgin-Karaji A, Shadjoo K, Padmehr R, Mohazzab A, Enzevaei A, Samimi-Sadeh S, Kamali K, Khazali S. Transversus abdominis plane block under laparoscopic guide versus port-site local anaesthetic infiltration in laparoscopic excision of endometriosis: a double-blind randomised placebo-controlled trial. BJOG. 2019;126(5):647–654. doi: 10.1111/1471-0528.15502. [DOI] [PubMed] [Google Scholar]
- 43.Murouchi T, Iwasaki S, Yamakage M. Quadratus lumborum block: analgesic effects and chronological ropivacaine concentrations after laparoscopic surgery. Reg Anesth Pain Med. 2016;41(2):146–150. doi: 10.1097/AAP.0000000000000349. [DOI] [PubMed] [Google Scholar]
- 44.Salama ER. Ultrasound-guided bilateral quadratus lumborum block vs. intrathecal morphine for postoperative analgesia after cesarean section: a randomised controlled trial. Korean J Anesthesiol. 2020;73(2):121–8. [DOI] [PMC free article] [PubMed]
- 45.Zhu Q, Li L, Yang Z, Shen J, Zhu R, Wen Y, Cai W, Liu L. Ultrasound guided continuous Quadratus Lumborum block hastened recovery in patients undergoing open liver resection: a randomized controlled, open-label trial. BMC Anesthesiol. 2019;19(1):23. doi: 10.1186/s12871-019-0692-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ueshima H, Hiroshi O. Intermittent bilateral anterior sub-costal quadratus lumborum block for effective analgesia in lower abdominal surgery. J Clin Anesth. 2017;43:65. doi: 10.1016/j.jclinane.2017.09.018. [DOI] [PubMed] [Google Scholar]
- 47.Akerman M, Pejcic N, Velickovic I. A review of the quadratus lumborum block and ERAS. Front Med (Lausanne) 2018;5:44. doi: 10.3389/fmed.2018.00044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Putzu M, Gambaretti E, Rizzo F, Latronico N. Postoperative analgesia for laparotomic surgery provided by bilateral single-shot quadratus lumborum block. Minerva Anestesiol. 2018;84(10):1231–1232. doi: 10.23736/S0375-9393.18.12777-5. [DOI] [PubMed] [Google Scholar]
- 49.Hussein MM. Ultrasound-guided quadratus lumborum block in pediatrics: trans-muscular versus intra-muscular approach. J Anesth. 2018;32(6):850–855. doi: 10.1007/s00540-018-2563-z. [DOI] [PubMed] [Google Scholar]
- 50.Mieszkowski MM, Mayzner-Zawadzka E, Tuyakov B, Mieszkowska M, Zukowski M, Wasniewski T, Onichimowski D. Evaluation of the effectiveness of the quadratus lumborum block type I using ropivacaine in postoperative analgesia after a cesarean section - a controlled clinical study. Ginekol Pol. 2018;89(2):89–96. doi: 10.5603/GP.a2018.0015. [DOI] [PubMed] [Google Scholar]
- 51.Zhu M, Qi Y, He H, Lou J, Pei Q, Mei Y. Analgesic effect of the ultrasound-guided subcostal approach to transmuscular quadratus lumborum block in patients undergoing laparoscopic nephrectomy: a randomized controlled trial. BMC Anesthesiol. 2019;19(1):154. doi: 10.1186/s12871-019-0825-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Young D. Policymakers, experts review evidence-based medicine. Am J Health Syst Pharm. 2005;62(4):342–343. doi: 10.1093/ajhp/62.4.342. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.