Abstract
Background:
Pain and its consequences remain of concern, particularly in high-risk occupations such as the military. Alcohol is a legal and accessible means of self-medication, and risky alcohol use is associated with potentially serious consequences. This exploratory analysis aimed to better understand the association of selected pain diagnoses with risky alcohol use among soldiers returning from deployment.
Methods:
Analysis of data from active duty soldiers returning from Afghanistan or Iraq deployments in fiscal years 2008-2011 who completed Department of Defense health questionnaires after deployment (n= 267,100). Each questionnaire included self-reported alcohol consumption and items yielding AUDIT-C screening scores. Military Health System data were used to identify diagnoses of pain-related conditions.
Results:
About 70% of soldiers had none of the selected pain diagnoses either pre- or post-deployment. 10% had incident pain diagnoses (only post-deployment), 7% had persistent pain diagnoses (both pre- and post-deployment), and 13% had remitted pain diagnoses (only pre-deployment). On the AUDIT-C, 39% screened positive for at-risk drinking and 6% were likely to have severe alcohol problems. Half of the respondents reported any binge drinking; 20% at least monthly binge drinking. Logistic regression analyses found reduced odds of risky alcohol use post-deployment in association with incident and persistent pain diagnoses, compared to no pain diagnoses pre- or post-deployment.
Conclusions:
Pain diagnoses, binge drinking, and risky alcohol use were prevalent among this sample of Army soldiers. An inverse relationship was found between pain diagnosis (incident, persistent) and risky alcohol use post-deployment. Attention should continue to be paid to risky alcohol use in this population, yet these exploratory findings do not suggest that soldiers with the pain diagnoses used in this study are at greater risk. Combat exposure, traumatic brain injury, and psychological health were more important predictors, and should continue to warrant enhanced alcohol screening.
Keywords: military personnel, pain, alcohol drinking, alcohol-related disorders
INTRODUCTION
The presence of pain and its consequences remains a great concern. People in occupations such as the military or construction are at higher risk for painful injuries and conditions.1-3 Persistent pain that limits a military member’s ability to function in their job, or requires opioids, can be career-ending. To ensure force readiness, the Department of Defense (DoD) issued an instruction that military members who are non-deployable for 12 consecutive months because of pain or opioid prescriptions will be processed for military separation.4
People with pain have heightened use of alcohol and other substances; recent reviews consider causal mechanisms that include self-medication/negative reinforcement, stress responses, and analgesic properties of alcohol.5,6 The relationship between alcohol and pain may depend on prior levels of drinking or pain severity and/or interference.6,7 Further, pain and substance use disorders commonly co-occur.5,6,8 People with pain who have substance use disorders are at higher risk for relapse,9,10 and people with reduced pain after substance use treatment are less likely to relapse.8
To date, studies about alcohol and pain have focused on populations that that have low levels of baseline drinking, are in treatment for substance use disorders, or do not have chronic pain; little is known about whether pain drives alcohol use – risky or otherwise – in other populations.5,6,11 Earlier identification of potential alcohol problems that are related to pain would enable more effective interventions before the alcohol problems become severe.
Risky alcohol use is prevalent among military members.12,13 Since mandatory drug tests discourage the misuse of prescription pain relievers or illicit drug use, alcohol may be used to self-medicate for pain.14 It remains unknown whether risky alcohol use and alcohol-related problems, such as binge drinking, are more common among soldiers with pain than those without pain. If this proves true for military members, enhanced screening for alcohol problems and earlier interventions would be beneficial to reduce consequences of alcohol misuse for military members and military readiness.
This paper explored the following questions in a population of post-deployment soldiers: What is the association of pain-related diagnoses with 1) alcohol consumption, and 2) with binge drinking and risky drinking? These findings are intended to offer guidance regarding the risk for alcohol problems and the need for enhanced alcohol screening among soldiers with pain-related conditions.
METHODS
The Substance Use Psychological Injury Combat (SUPIC) study is a population-based, observational study of U.S. Army soldiers who returned from an Afghanistan or Iraq deployment. Data used for this study is from the cohort returning during fiscal years 2008-2011. The rationale, methods and sample are described elsewhere.15
Data Sources
Analyses relied on existing self-reported screening data (e.g., combat exposure, alcohol use) from the DoD’s post-deployment health surveillance program: (1) the Post-Deployment Health Assessment (PDHA) completed within 60 days of the end of deployment, and (2) the Post-Deployment Health Re-Assessment (PDHRA) completed on average 4.5 months post-deployment. Medical record diagnoses for pain-related conditions, pre-deployment alcohol use disorder, and filled opioid prescription medications were from the Military Health System Data Repository.
Sample
From the SUPIC active duty cohort (n=434,986), we selected soldiers who completed the PDHA questionnaire that was matched to the index deployment and completed a follow-up PDHRA questionnaire (n=267,100). Description of this sample is available elsewhere.16
Variables
Alcohol Outcome Measures.
The PDHRA includes self-reported alcohol quantity and frequency questions: “How many drinks containing alcohol do you have on a typical day when you are drinking?” (1-2, 3-4, 5-6, 7-9, 10 or more), and, “How often do you have a drink containing alcohol?” (never, monthly or less, 2-4 times a month, 2-3 times a week, 4 or more times a week). The time frame for these items is not specified.
We adapted quantity-frequency (QF) measures from military and civilian literature,17-19 and created a self-reported alcohol consumption variable with 5 drinking categories: abstainer (no drinking days per month), light alcohol use (1-2 drinks per day, regardless of drinking frequency), moderate alcohol use (3-4 drinks per day, regardless of drinking frequency, or 5-6 drinks per day no more than 2-3 times per week), heavy-infrequent alcohol use (7 or more drinks per day, monthly or less), and heavy-frequent alcohol use (5-6 drinks per day, 4 or more times per week, or 7 or more drinks per day at least 2-4 times per month).
From the self-reported item, “How often do you have 6 or more drinks on one occasion?” (never, less than monthly, monthly, weekly, daily; not gender-specific), we created two dichotomous variables: any binge drinking and binge drinking at least monthly, each coded as 0=no (binge drinking or monthly binge drinking, respectively) and 1=yes.
Alcohol risk was measured from the AUDIT-C score items in the PDHRA.20-23 Two dichotomous measures were created, one for a positive screen for at-risk drinking (AUDIT-C ≥ 4 for men, ≥ 3 for women), and the other indicating a high likelihood for severe alcohol problems (AUDIT-C ≥ 8 for men or women).24 Each was coded as 0=no (not at-risk or severe) and 1=yes. By definition, “severe” on the AUDIT-C is a subset of “at-risk”.
Pain Measures.
We used a previously constructed pain-related diagnosis variable based on ICD-9 diagnostic codes from soldiers’ inpatient and outpatient claims for selected pain-related conditions (e.g., chronic pain, headache/migraine, back pain, nerve pain, unspecified joint pain, generalized pain, and cancer-related pain). Arthritis and some musculoskeletal pain-related diagnoses (e.g., shoulder) were excluded from this existing variable. A four-category variable was then created to indicate presence of pain diagnoses in the 1 year before and 90 days following deployment: no pain diagnosis (neither time period), remitted pain (presence of pain diagnoses before deployment, but not post-deployment), incident pain (presence of pain diagnoses post-deployment, but not before), and persistent pain (both before and post-deployment).
Covariates.
Demographic data (gender, race/ethnicity, marital status, age, education, and whether the soldier has dependent children) and military characteristics (rank/paygrade, any prior deployments, and length of the index deployment) were included.
Covariates from the PDHA included self-report about the index deployment (ever restricted to quarters or assigned light duty due to painful conditions; count (0 to 3) of combat exposures that were included on the PDHA [encountered dead bodies or seen people killed or wounded, engaged in direct combat where discharged a weapon, felt were in great danger of being killed]); positive screen for traumatic brain injury (TBI);16,25 poor physical health in the past 4 weeks; and positive screens for mental health problems in the past month (PTSD26-28 and depression29). We also included covariates indicating if a soldier had filled an opioid prescription in the 90 days post-deployment, or received an alcohol use disorder (AUD) diagnosis in the year prior to deployment. All covariates, with the exception of combat exposure, are dichotomous where 0=no (e.g., no positive PTSD screen) and 1=yes (e.g., positive PTSD screen).
Analyses
Analyses examined alcohol use measures from the PDHRA.16 We present univariate analyses to describe the sample overall, and bivariate analyses to examine the associations between the constructed pain variables and the alcohol measures. Logistic regression models examined the association of the pain variable on at-risk drinking, binge drinking at least monthly, severe alcohol problems, and heavy-frequent alcohol use, adjusting for covariates listed above. Analyses used SAS 9.3 (SAS Institute, Cary, NC). This study was approved by the Human Research Protection Programs at Brandeis University and the Office of the Assistant Secretary of Defense Health Affairs.
RESULTS
Sample Characteristics
The sample was mostly male (90.1%), approximately half were white (53.3%), with a mean age of 26.9 years old. About two-thirds (62.5%) were married and 44.7% had at least one dependent child. Over 12% reported being restricted to quarters or light duty due to pain during the index deployment, 59% had no combat exposure during the index deployment, just over 7% screened positive for a TBI, and almost 11% filled an opioid prescription in the 90 days post-deployment (Table 1).
Table 1.
Military, Deployment and Post-Deployment Characteristics, Active Duty Soldiers, FY2008-2011
| N | % | |
|---|---|---|
| TOTAL | 267,100 | 100.0 |
| Military | ||
| Rank/paygrade | ||
| Junior enlisted | 149,185 | 55.9 |
| Senior enlisted | 83,041 | 31.1 |
| Officer | 34,874 | 13.1 |
| Any prior deployment | 120,790 | 45.2 |
| Length of index deployment (months) | 267,100 | 12.0 (mean) |
| Deployment variables* | ||
| Restricted to quarters or light duty for pain | 33,481 | 12.5 |
| Combat exposure (count) | ||
| None | 156,901 | 58.7 |
| One | 58,048 | 21.7 |
| Two | 32,284 | 12.1 |
| Three | 19,867 | 7.4 |
| TBI during deployment, positive screen | 19,240 | 7.2 |
| Post-deployment variables* | ||
| Poor physical health past month | 29,832 | 11.2 |
| PTSD past month, positive screen | 14,295 | 5.4 |
| Depression past month, positive PHQ-2 screen | 20,103 | 7.5 |
| Filled opioid prescription 0-90 days post-deployment** | 28,839 | 10.8 |
Self-reported, from Post-Deployment Health Assessment, conducted within 60 days of the end of deployment
From pharmacy claims data
Pain Diagnoses and Alcohol Consumption
Overall, 70.3% of the sample had none of the selected pain diagnoses during the pre- or post-deployment time periods (Table 2). Nearly 7% had persistent pain diagnoses, 10.2% had incident pain diagnoses, and 12.9% had remitted pre-deployment pain diagnoses.
Table 2:
Post-Deployment Alcohol Use and Risky Use by Pain Category, Active Duty Soldiers, FY 2008-2011
| % of All Soldiers | |||||||
|---|---|---|---|---|---|---|---|
| Pain Category | |||||||
| N | Total | No Pain | Remitted | Incident | Persistent | p | |
| N | 267,100 | 267,100 | 187,693 | 34,389 | 27,242 | 17,776 | |
| % | 100.0 | 100.0 | 70.3 | 12.9 | 10.2 | 6.7 | |
| % of Soldiers by Pain Category | |||||||
| % | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | ||
| Drinking category* | 250,032 | ||||||
| Abstainer | 18.9 | 18.7 | 19.2 | 19.0 | 20.8 | <.0001 | |
| Light | 41.3 | 40.9 | 42.1 | 41.6 | 43.2 | ||
| Moderate | 34.0 | 34.6 | 33.2 | 33.2 | 30.6 | ||
| Heavy-Infrequent | 0.6 | 0.5 | 0.5 | 0.7 | 0.7 | ||
| Heavy-Frequent | 5.3 | 5.3 | 5.0 | 5.5 | 4.7 | ||
| Binge drinking** | 267,100 | ||||||
| Any binge | 49.8 | 50.4 | 48.2 | 50.1 | 45.9 | <.0001 | |
| At least monthly | 19.8 | 20.1 | 18.7 | 20.1 | 17.8 | <.0001 | |
| AUDIT-C*** | 267,100 | ||||||
| At-risk | 38.8 | 39.1 | 38.2 | 39.2 | 36.5 | <.0001 | |
| Severe | 6.0 | 6.1 | 5.8 | 6.5 | 5.6 | <.0001 | |
Data are self-reported from Post-Deployment Health Reassessment (PDHRA), conducted on average 5 months following end of deployment.
Drinking category based on typical alcohol quantity and frequency;
Binge drinking defined as 6 or more drinks on one occasion;
"At risk" = AUDIT-C score or 4 or higher for males, 3 or higher for females; "Severe" = AUDIT-C score of 8 or higher regardless of gender.
Most soldiers were light (41.3%) or moderate (34.0%) drinkers (Table 2). The minority were abstainers (18.9%), and the remainder were heavy drinkers (5.3% heavy-frequent and 0.6% heavy-infrequent). Half of soldiers reported any binge drinking at the level of 6+ drinks on one occasion, and about 20% reported binge drinking at least monthly. The AUDIT-C score indicated that 38.8% of soldiers screened positive for at-risk drinking, and 6.0% were likely to have severe alcohol problems.
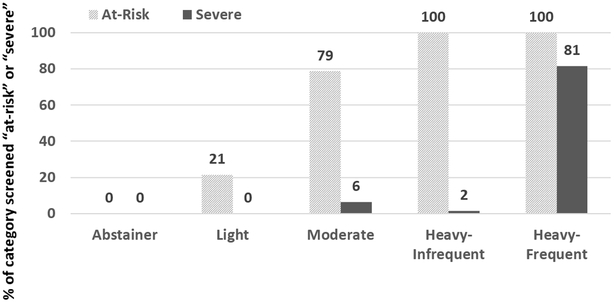
Figure 1 illustrates how the AUDIT-C variables relate to the created alcohol consumption variable. As shown, they do not fully coincide. Moderate drinkers are also at-risk on the AUDIT-C nearly 80% of the time, but rarely considered severe on the AUDIT-C. In particular, the heavy-infrequent drinkers were always at-risk on the AUDIT-C but rarely at a severe level, whereas the heavy-frequent drinkers were always at-risk on the AUDIT-C and 80% screened positive at the severe level.
Figure 1. % with Positive Screens on the AUDIT-C (“at-risk” or “severe”) for each Alcohol Consumption Category, Active Duty Soldiers, FY2008-2011.
Hatched columns represent the proportion of soldiers in each alcohol consumption category who screened positive for at-risk drinking (e.g., 79% of moderate drinkers screened as at-risk). Solid columns represent the proportion of soldiers in each alcohol consumption category who screened positive for severe alcohol problems (e.g., 6% of moderate drinkers screened as severe).
Bivariate analyses indicated significant differences in the alcohol measures by pain category (Table 2). Soldiers with no pain diagnosis in either time period and soldiers with post-deployment incident pain diagnoses had the highest rates of heavy-frequent drinking, binge or monthly binge drinking, and at-risk or severe AUDIT-C scores. Soldiers with persistent pain diagnoses were most likely to abstain from alcohol or be light drinkers, and least likely to be heavy drinkers, have any binge or monthly binge drinking, or have at-risk or severe AUDIT-C scores.
Likelihood of Risky Alcohol Use
Logistic regression results show that, controlling for other variables, soldiers with incident or persistent pain diagnoses had lower odds of risky alcohol use indicators at the post-deployment re-assessment than soldiers with no pain diagnosis at either time period (Table 3). More specifically, soldiers with persistent pain diagnoses were less likely to have an at-risk AUDIT-C score (adjusted odds ratio [AOR] 0.92, 95% confidence interval [CI] 0.89-0.95, p<.0001), binge monthly (AOR 0.91, 95% CI 0.87-0.95, p<.0001), have a severe AUDIT-C score (AOR 0.89, 95% CI 0.83-0.96, p=.002), or be heavy-frequent drinkers (AOR 0.89, 95% CI 0.82-0.96, p=.002) than soldiers with no pain diagnosis at either time period.
Table 3.
Likelihood of Risky Alcohol Use, Active Duty Solders, FY2008-2011
| Alcohol Outcomes, Post-Deployment* | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| At Risk (AUDIT-C) | Binge (6+) monthly | Severe (AUDIT-C) | Heavy-Frequent Drinking | |||||||||||||
| AOR | Lower CI |
Upper CI |
p | AOR | Lower CI |
Upper CI |
p | AOR | Lower CI |
Upper CI |
p | AOR | Lower CI |
Upper CI |
p | |
| N | ||||||||||||||||
| Pain Category [ref=none] | ||||||||||||||||
| Remitted | 1.00 | 0.98 | 1.03 | 0.852 | 0.98 | 0.95 | 1.01 | 0.167 | 1.01 | 0.96 | 1.06 | 0.786 | 0.99 | 0.94 | 1.05 | 0.713 |
| Incident | 0.97 | 0.94 | 0.99 | 0.010 | 0.94 | 0.91 | 0.98 | 0.001 | 0.95 | 0.90 | 1.00 | 0.061 | 0.93 | 0.88 | 0.99 | 0.021 |
| Persistent | 0.92 | 0.89 | 0.95 | <.0001 | 0.91 | 0.87 | 0.95 | <.0001 | 0.89 | 0.83 | 0.96 | 0.002 | 0.89 | 0.82 | 0.96 | 0.002 |
| Year before Deployment | ||||||||||||||||
| Any alcohol diagnosis** | 1.46 | 1.39 | 1.53 | <.0001 | 1.54 | 1.45 | 1.62 | <.0001 | 1.65 | 1.53 | 1.79 | <.0001 | 1.70 | 1.57 | 1.85 | <.0001 |
| Deployment** | ||||||||||||||||
| Assigned to quarters for pain | 1.08 | 1.05 | 1.10 | <.0001 | 1.02 | 0.99 | 1.06 | 0.132 | 1.02 | 0.97 | 1.07 | 0.520 | 1.01 | 0.95 | 1.06 | 0.856 |
| Combat exposure [ref=none] | ||||||||||||||||
| One | 1.16 | 1.13 | 1.18 | <.0001 | 1.18 | 1.15 | 1.21 | <.0001 | 1.20 | 1.16 | 1.25 | <.0001 | 1.19 | 1.13 | 1.24 | <.0001 |
| Two | 1.25 | 1.22 | 1.29 | <.0001 | 1.28 | 1.24 | 1.32 | <.0001 | 1.41 | 1.35 | 1.48 | <.0001 | 1.37 | 1.30 | 1.45 | <.0001 |
| Three | 1.38 | 1.34 | 1.42 | <.0001 | 1.42 | 1.37 | 1.47 | <.0001 | 1.52 | 1.43 | 1.61 | <.0001 | 1.54 | 1.45 | 1.64 | <.0001 |
| Post-Deployment*** | ||||||||||||||||
| PTSD past mo, positive screen | 1.11 | 1.07 | 1.15 | <.0001 | 1.19 | 1.14 | 1.25 | <.0001 | 1.29 | 1.21 | 1.37 | <.0001 | 1.27 | 1.18 | 1.36 | <.0001 |
| Depression (PHQ-2) past mo, pos screen | 1.29 | 1.25 | 1.33 | <.0001 | 1.39 | 1.34 | 1.44 | <.0001 | 1.67 | 1.59 | 1.76 | <.0001 | 1.59 | 1.50 | 1.68 | <.0001 |
| Poor physical health past mo | 1.09 | 1.06 | 1.12 | <.0001 | 1.20 | 1.16 | 1.24 | <.0001 | 1.40 | 1.33 | 1.46 | <.0001 | 1.37 | 1.30 | 1.45 | <.0001 |
| TBI, positive screen | 1.11 | 1.07 | 1.14 | <.0001 | 1.15 | 1.11 | 1.20 | <.0001 | 1.16 | 1.10 | 1.23 | <.0001 | 1.15 | 1.08 | 1.22 | <.0001 |
| 0-90 Days Post-D'eployment | ||||||||||||||||
| Any opioid precription fill | 0.97 | 0.95 | 1.00 | 0.049 | 1.01 | 0.98 | 1.04 | 0.575 | 1.05 | 0.99 | 1.10 | 0.086 | 1.04 | 0.98 | 1.10 | 0.185 |
AOR = Adjusted Odds Ratio CI = 95% Confidence Interval, upper and lower limits
Alcohol outcomes from Post-Deployment Health Re-Assessment, conducted on average 5 months post-deployment. All models control for gender, race/ethnicity, marital status, dependent children, military rank/paygrade, length of index deployment, and days since deployment;
From pharmacy claims data;
Self reported from the Post Deployment Health Assessment, conducted within 60 days of the end of deployment
Soldiers with incident pain diagnoses were less likely to have at-risk AUDIT-C scores (AOR 0.97, 95% CI 0.94-0.99, p=.010), binge monthly (AOR 0.94, 95% CI 0.91-0.98, p<.0001), or be heavy-frequent drinkers (AOR 0.93, 95% CI 0.88-0.99, p=.021) than soldiers with no pain diagnoses at either time period. Severe AUDIT-C scores (AOR 0.95, 95% CI 0.90-1.00, p=.061) trended in the same direction.
Soldiers with remitted pain were not significantly different than soldiers with no pain on any of the problem alcohol indicators.
Soldiers who had a prior AUD diagnosis were significantly more likely to report problem alcohol indicators than soldiers without a prior AUD diagnosis. Soldiers who were assigned to quarters for pain were more likely to have an at-risk AUDIT-C score than soldiers who were not (AOR 1.08, 95% CI 1.05-1.10, p<.0001), but otherwise were not significantly different on the other alcohol measures. The more combat exposures reported, the greater the likelihood of each risky alcohol indicator, and the same was true for the presence of positive screens for PTSD, depression, TBI, or poor physical health in the past month. Having filled an opioid prescription in the 90 days post-deployment was associated with lower at-risk AUDIT-C scores but was not significantly associated with other alcohol indicators.
DISCUSSION
The association between pain and risky alcohol use is essential to understand, particularly in a military population where there is a high prevalence of each. One concern is that people with pain might be self-medicating by using alcohol at higher rates, with the concomitant problems that often accompany excessive alcohol use. In contrast to that hypothesis, this study found that, when controlling for deployment experiences and comorbidities, the presence of incident or persistent pain diagnoses was associated with lower likelihood of alcohol problems as indicated by significantly reduced rates of heavy-frequent alcohol use or monthly binge drinking and of at-risk or severe AUDIT-C scores. Soldiers with remitted pain diagnoses were very similar to soldiers with no pain diagnoses regarding drinking patterns, suggesting that the relationships we found only hold while painful conditions are temporally close to the drinking behaviors being measured.
The negative effect of incident or persistent pain diagnoses on risky drinking was unexpected. Since we were able to control for opioid pain medications in the 90 days post-deployment, it is unlikely that this is due to an intentional decision to drink less because of pain medication. Some studies have suggested that pain could be increased in people who drink at higher levels.6 If so, those individuals might reduce their drinking to reduce their pain. Since our findings hold while controlling for alcohol use diagnoses, this may be a viable explanation. An alternative is that drinking is often a normative or recreational activity in military populations – serving as recreation, stress relief, and a way to build camaradierie13 – whereas people experiencing painful conditions may withdraw from activities.30 Future studies should examine our finding that suggests some level of protective effect regarding risky drinking among people with diagnoses of painful conditions.
Although the differences across groups were quite small, these findings do not suggest a need for enhanced alcohol screening or targeted alcohol interventions among soldiers with pain-related diagnoses. As discussed in the literature,13,24,31,32 risky alcohol use and indicators of alcohol problems are common in Army populations. Since unadjusted rates of risky alcohol use are similar among all four pain groups, while adjusted rates are significant for the incident and persistent groups, the significance must be largely attributable to these soldiers’ covariate values which would otherwise predict higher rates of risky alcohol use.
Similar to other studies, important predictors of problem alcohol indicators were related to combat and TBI exposure, and psychological health. 16,33,34 Further, these comorbidities had a stronger association with alcohol consumption than the presence or absence of pain-related diagnoses. It is unsurprising that these covariates might have stronger effects in soldiers with ongoing pain. These findings highlight the importance of universal screening and interventions to address risky drinking in Army soldiers, in particular in the context of psychological health.
This study has several limitations. The existing pain variable did not include all painful conditions, such as osteoarthritis and some musculoskeletal conditions, which were fairly rare in other analyses with this population. Cancer pain was included but is extremely rare in this sample. We could not include a measure of pain severity or functional limitations. With a large sample size, significant differences are not altogether surprising. However, except for the 3% difference in at-risk AUDIT-C scores among soldier with incident pain, all other significant effects are 5% or more. Effects of this size are commonly considered large enough to be worth noting.
Alcohol frequency and quantity were self-reported. The DoD binge drinking measure is 6 or more drinks regardless of gender, thus we underestimate binge drinking as commonly defined by the National Institute on Alcohol Abuse and Alcoholism and in the literature. This is particularly true for women, although they represent under 10% of the sample. Information on other drug use, another potential self-medication approach, was not available although illicit drug use is very low in the military.35 Study results may not be generalizable to military members from other U.S. military Services, National Guard or Reserve, or civilians.
With high rates of risky drinking across this sample, there could be a threshold effect, where we would not see any differences due to pain since the risky drinking rates are already more than we might expect. If our findings were not significant, the threshold effect might be of concern. However, we found a decreased likelihood of risky drinking, suggesting that a threshold does not play a role.
High levels of risky alcohol use remain of concern in populations such as the military, where pain is common. Yet, we did not find evidence of increased alcohol problems among soldiers with pain diagnoses, and pain may in fact be associated with fewer problems. We echo the call for increased attention to risky alcohol use among soldiers, but these findings do not indicate need for enhanced focus on soldiers with pain. Future studies should examine a broader range of painful conditions36 and other populations, both military and civilian. Further, the current context of the opioid epidemic and resulting reductions in use of prescription opioid medications suggest that replication of these findings in more recent populations would be valuable.
Acknowledgements:
We thank Beth Mohr Dana and Sue Lee for statistical programming. We acknowledge Kennell and Associates, Inc. for compiling the data files used in these analyses. Chester Buckenmaier, III, M.D., of the Uniformed Services University is the Department of Defense (DoD) data sponsor. Thomas V. Williams, Ph.D., formerly of the Defense Health Agency, was the data sponsor at the time these analyses were conducted. The Defense Health Agency’s Privacy and Civil Liberties Office provided access to DoD data. The opinions and assertions herein are those of the authors and do not necessarily reflect the official views of the DoD or the National Institutes of Health. Preliminary versions of these results were presented at the American Pain Society annual conference May 2016 and the Research Society on Alcoholism annual meeting May 2016.
Funding Details: This study was funded by the National Center for Complementary and Integrative Health (NCCIH; R01 AT008404), with support to develop the study cohort from the National Institute on Drug Abuse (NIDA; R01 DA030150). The funding agencies had no role in in study design, data collection, analysis or interpretation of data, writing or review of the manuscript, or decision to submit the manuscript for publication.
Footnotes
Declarations of Interest: The authors declare no conflicts of interest.
REFERENCES
- 1.Office of The Army Surgeon General. Pain Management Task Force: Providing a Standardized DoD and VHA Vision and Approach to Pain Management to Optimize the Care for Warriors and their Families. Final Report. 2010; http://www.dvcipm.org/site/assets/files/1070/pain-task-force-final-report-may-2010.pdf. Accessed March 2, 2019.
- 2.Gauntlett-Gilbert J, Wilson S. Veterans and chronic pain. Br J Pain. 2013;7(2):79–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guo H-R, Tanaka S, Halperin WE, Cameron LL. Back pain prevalence in US industry and estimates of lost workdays. Am J Public Health. 1999;89(7):1029–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Department of Defense. DoD Instruction 1332.45 Retention Determinations for Non-Deployable Service Members. In: Office of Under Secretary of Defense for Personnel and Readiness, http://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/133245p.pdf?ver=2018-08-01-143025-053; 2018.
- 5.Witkiewitz K, Vowles KE. Alcohol and opioid use, co-use, and chronic pain in the context of the opioid epidemic: A critical review. Alcohol Clin Exp Res. 2018;42(3):478–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zale EL, Maisto SA, Ditre JW. Interrelations between pain and alcohol: An integrative review. Clin Psychol Rev. 2015;37:57–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Davis AK, Walton MA, Bohnert KM, Bourque C, Ilgen MA. Factors associated with alcohol consumption among medical cannabis patients with chronic pain. Addictive Behav. 2018;77:166–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jakubczyk A, Ilgen MA, Kopera M, et al. Reductions in physical pain predict lower risk of relapse following alcohol treatment. Drug Alcohol Depend. 2016;158:167–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Witkiewitz K, Vowles KE, McCallion E, Frohe T, Kirouac M, Maisto SA. Pain as a predictor of heavy drinking and any drinking lapses in the COMBINE study and the UK Alcohol Treatment Trial. Addiction. 2015;110(8):1262–1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Larson MJ, Paasche-Orlow M, Cheng DM, Lloyd-Travaglini C, Saitz R, Samet JH. Persistent pain is associated with substance use after detoxification: a prospective cohort analysis. Addiction. 2007;102(5):752–760. [DOI] [PubMed] [Google Scholar]
- 11.Moskal D, Maisto SA, De Vita M, Ditre JW. Effects of experimental pain induction on alcohol urge, intention to consume alcohol, and alcohol demand. Exp Clin Psychopharmacol. 2018;26(1):65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bray RM, Pemberton MR, Lane ME, Hourani LL, Mattiko MJ, Babeu LA. Substance use and mental health trends among U.S. military active duty personnel: key findings from the 2008 DoD Health Behavior Survey. Mil Med. 2010;175(6):390–399. [DOI] [PubMed] [Google Scholar]
- 13.Institute of Medicine. Substance Use Disorders in the U.S. Armed Forces. Washington, DC: The National Academies Press, http://www.nap.edu/openbook.php?record_id=13441;2013. [Google Scholar]
- 14.Goebel JR, Compton P, Zubkoff L, et al. Prescription sharing, alcohol use, and street drug use to manage pain among veterans. J Pain Symptom Manage. 2011. [DOI] [PubMed] [Google Scholar]
- 15.Larson M, Adams R, Mohr B, et al. Rationale and methods of the substance use and psychological injury combat study (SUPIC): A longitudinal study of Army service members returning from deployment in FY2008-2011. Substance Use & Misuse. 2013;48(10):863–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adams RS, Corrigan JD, Mohr BA, Williams TV, Larson MJ. Traumatic brain injury and post-deployment binge drinking among male and female Army active duty service members returning from Operation Enduring Freedom/Operation Iraqi Freedom. J Neurotrauma. 2017;34(7):1457–1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Breslow RA, Graubard BI. Prospective study of alcohol consumption in the United States: quantity, frequency, and cause-specific mortality. Alcohol Clin Exp Res. 2008;32(3):513–521. [DOI] [PubMed] [Google Scholar]
- 18.Stahre M, Naimi T, Brewer R, Holt J. Measuring average alcohol consumption: the impact of including binge drinks in quantity-frequency calculations. Addiction. 2006;101(12):1711–1718. [DOI] [PubMed] [Google Scholar]
- 19.Bray RM, Pemberton MR, Hourani LL, et al. Department of Defense Survey of Health Related Behaviors among Active Duty Military Personnel. Research Triangle Institute;2009. [Google Scholar]
- 20.Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alc Clin Exp Res. 2007;31(7):1208–1217. [DOI] [PubMed] [Google Scholar]
- 21.Bradley KA, Williams EC, Achtmeyer CE, et al. Measuring performance of brief alcohol counseling in medical settings: A review of the options and lessons from the Veterans Affairs (VA) health care system. Subst Abuse. 2007;28(4):133–149. [DOI] [PubMed] [Google Scholar]
- 22.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA, et al. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Arch Intern Med. 1998;158(16):1789–1795. [DOI] [PubMed] [Google Scholar]
- 23.Crawford EF, Fulton JJ, Swinkels CM, Beckham JC, V.A. Mid-Atlantic MIRECC OEF/OIF Registry Workgroup, Calhoun PS. Diagnostic efficiency of the AUDIT-C in U.S. veterans with military service since September 11, 2001. Drug Alcohol Depend. 2013;132(1-2):101–106. [DOI] [PubMed] [Google Scholar]
- 24.Larson MJ, Mohr BA, Adams RS, Wooten NR, Williams TV. Missed opportunity for alcohol problem prevention among army active duty service members postdeployment. Am J Public Health. 2014;104(8):1402–1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kay T, Harrington DE, Adams R, et al. Definition of mild traumatic brain injury. J Head Trauma Rehabil. 1993;8(3):86–87. [Google Scholar]
- 26.Calhoun PS, McDonald SD, Guerra VS, Eggleston AM, Beckham JC, Straits-Troster K. Clinical utility of the Primary Care-PTSD Screen among U.S. veterans who served since September 11, 2001. Psychiatry Res. 2010;178(2):330–335. [DOI] [PubMed] [Google Scholar]
- 27.Prins A, Ouimette P, Kimerling R, et al. The Primary Care PTSD screen (PC-PTSD): Development and operating characteristics. Prim Care Psychiatr. 2003;9(4):151–151. [Google Scholar]
- 28.Bliese PD, Wright KM, Adler AB, Cabrera O, Castro CA, Hoge CW. Validating the Primary Care Posttraumatic Stress Disorder Screen and the Posttraumatic Stress Disorder Checklist with soldiers returning from combat. J Consult Clin Psychol. 2008;76(2):272–281. [DOI] [PubMed] [Google Scholar]
- 29.Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2 - Validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. [DOI] [PubMed] [Google Scholar]
- 30.Institute of Medicine. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, D.C.: National Academies Press; 2011. [PubMed] [Google Scholar]
- 31.Larson MJ, Wooten NR, Adams RS, Merrick EL. Military combat deployments and substance use: Review and future directions. J Soc Work Pract Addict. 2012;12(1):6–27. PMCID: PMC3321386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Santiago PN, Wilk JE, Milliken CS, Castro CA, Engel CC, Hoge CW. Screening for alcohol misuse and alcohol-related behaviors among combat veterans. Psychiatr Serv. 2010;61(6):575–581. [DOI] [PubMed] [Google Scholar]
- 33.Adams RS, Larson MJ, Corrigan JD, et al. Combat-acquired traumatic brain injury, posttraumatic stress disorder, and their relative associations with postdeployment binge drinking. J Head Trauma Rehabil. 2016;31(1):13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spera C, Thomas RK, Barlas F, Szoc R, Cambridge MH. Relationship of military deployment recency, frequency, duration, and combat exposure to alcohol use in the Air Force. J Stud Alc Drugs. 2011;72(1):5–14. [DOI] [PubMed] [Google Scholar]
- 35.Larson MJ, Mohr BA, Jeffery DD, Adams RS, Williams TV. Predictors of positive illicit drug tests after OEF/OIF deployment among army enlisted service members. Mil Med. 2016;181(4):334–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Reif S, Adams RS, Ritter GA, Williams TV, Larson MJ. Prevalence of pain diagnoses and burden of pain among active duty soldiers, FY2012. Mil Med. 2018;183(9-10):e330–e337. [DOI] [PMC free article] [PubMed] [Google Scholar]