Dear Editor,
Currently, the whole world is grappling with the outbreak of COVID-19 pandemic. It is imperative to break the chains of transmission, which is the most effective way for a quick containing of spike in the accounting of COVID-19 cases. As one of the containment measures, household isolation is now becoming commonplace in many countries. However, we must be aware of its potentially adverse outcomes on COVID-19 patients and negative impacts on pandemic control. (See Fig. 1 ).
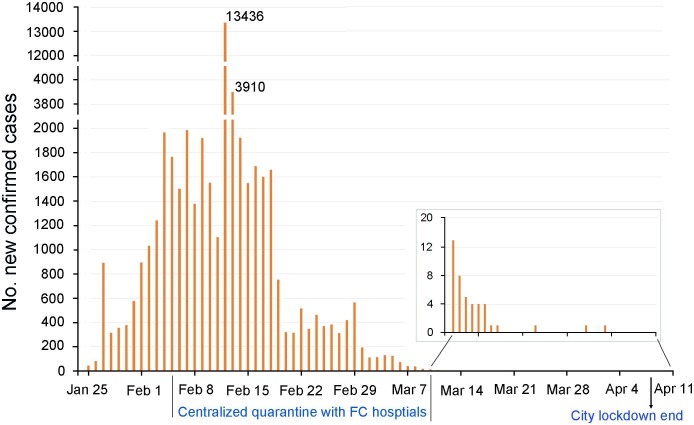
Fig. 1.
New confirmed COVID-19 cases in Wuhan from Jan 25 to April 11. The original data are from National Health Commission of the People's Republic of China (http://www.nhc.gov.cn/wjw/index.shtml) and Wuhan Municipal Health commission http://wjw.wuhan.gov.cn/). Although city lockdown and home quarantine was carried out from February 23, the number of new confirmed COVID cases per day continues to grow rapidly. However, this situation was clearly under control since the implementation of centralized isolation on February 5. Two weeks later, the vast majority of the first batch of isolated patients were discharged from Fangcang (FC) hospitals, correspondingly, the number of new cases began to drop sharply day by day. A significant increase of cases was observed on February 12, as the clinical diagnosis cases involved in the new confirmed cases.
Tension and anxiety—stimulated by a series factors such as strong infectiousness and high fatality of the disease, shortage of medical resources, and tons of negative and fake news, etc.—inevitably occur for COVID-19 patients once they get confirmed (Troyer et al., 2020). Worsening of conditions, such as fever, coughing and dyspnea, etc., exacerbates their panic, even worsened, haunting them in despair. The unavailability of appropriate place for isolation at home or improper control measures cause cross infection in family, which adds to their guilt. Also, a variety of iatrogenic tasks, including self-monitoring of temperature regularly, self-assessment of coughing and dyspnea, disinfection of living space and supplies, etc., increase anxiety and stress of the patients during home quarantine.
The above negative factors may spoil appetite and disrupt sleep of COVID-19 patients, even developing to anorexia and severe insomnia. These isolation-related stress reactions are bound to reduce immune function and delay the recovery. Especially for patients who are older than 65 years or with pre-existing conditions, such as depression, sleep disorders and cardio-pulmonary diseases, home isolation may increase the susceptibility to the inflammatory storm caused by COVID-19, potentially leading to a deterioration, or worse, the death (Sominsky et al., 2020).
Mechanismly, physical/objective social isolation has been recognized as a major risk factor for poor health, morbidity and mortality (Holt-Lunstad et al., 2015). Notably, there is considerable evidence for a close relationship between social isolation and inflammatory infection (Eisenberger et al., 2017). Social isolated loneliness is typically associated with higher levels of sympathetic nervous system activation and hypothalamic pituitary adrenocortical activity, subsequently causing overactivation of the inflammatory response (Smith et al., 2020).
Moreover, COVID-19 virus is highly infectious and has multiple transmission routes (Hindson, 2020), even medical personnel are vulnerable to be infected (Ferioli et al., 2020). Therefore, it is difficult to ensure that cluster infection does not occur in families during the isolation period for at least 2 weeks unless excellent infection control is implemented (Mao et al., 2020). This requires sufficient knowledge and proper measures, but for ordinary people and families, especially those living together in a narrow space, is obviously hard to meet, causing other family members to be infected. Subsequently, the asymptomatic carriers or infected individuals have not been diagnosed will become a key factor of community outbreak (Yu and Yang, 2020). A small portion of patients do not strictly adhere to stay at home, go shopping, exercise or other social activities, which brings high risk to other close contacts. The transmissions eventually lead to a surge of infections, which places huge pressure on city’s health-care system operating over its maximum capacity and soon overwhelmed (Kandel et al., 2020). Therefore, we consider that for newly confirmed COVID-19 patients, especially the elderly and those with pre-existing diseases, home isolation should be carefully chosen.
Centralized isolation is recommended, because it is not only convenient to get timely treatment and intervention of COVID-19 patients when the disease deteriorates, but also helps to cut off transfection effectively. Notably, Makeshift (Fangcang, FC) hospitals, usually transformed from gymnasiums, exhibition center, factory facilities is an effective alternative to home isolation. FC hospitals, with high mobility, less environmental requirements, and rapid deployment, fill the gaps and in short terms, relieve the pressure of designated medical institutions. FC quarantine minimizes the spread size of COVID-19 among family and community and has been proved in effectively fighting against COVID-19 pandemic in Wuhan, China (Pan et al., 2020). Notably, a FC hospital is far more than a hospital simply for physical isolation or mere treatment either. Instead, it builds a small society with enriched environment to maintain the health status of COVID-19 patients, thus promoting their rehabilitation and preventing the deterioration comparing to home isolation (Chen et al., 2020). It will help to save medical resources in the region and even the whole country. Centralized quarantine mode of FG hospitals might also have long-term effects on the prevention and treatment of post-traumatic stress disorder, however, it remains to be verified in the future.
Presently, an increasing number of countries and regions are constructing or have put into use FC hospitals in response to COVID-19 crisis. Yet, considering the differences in management system, culture and living habits among countries and regions, it is necessary to make deliberate decisions on quarantine strategies according to local conditions.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bbi.2020.05.009.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Chen S., Zhang Z., Yang J., Wang J., Zhai X., Barnighausen T., Wang C. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395:1305–1314. doi: 10.1016/S0140-6736(20)30744-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberger N.I., Moieni M., Inagaki T.K., Muscatell K.A., Irwin M.R. In Sickness and in Health: The Co-Regulation of Inflammation and Social Behavior. Neuropsychopharmacology. 2017;42:242–253. doi: 10.1038/npp.2016.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferioli M., Cisternino C., Leo V., Pisani L., Palange P., Nava S. Protecting healthcare workers from SARS-CoV-2 infection: practical indications. Eur. Respir. Rev. 2020;29(155) doi: 10.1183/16000617.0068-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindson J. COVID-19: faecal-oral transmission? Nat. Rev. Gastroenterol. Hepatol. 2020 doi: 10.1038/s41575-020-0295-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J., Smith T.B., Baker M., Harris T., Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect. Psychol. Sci. 2015;10:227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- Kandel N., Chungong S., Omaar A., Xing J. Health security capacities in the context of COVID-19 outbreak: an analysis of International Health Regulations annual report data from 182 countries. Lancet. 2020;395:1047–1053. doi: 10.1016/S0140-6736(20)30553-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mao Z.Q., Wan R., He L.Y., Hu Y.C., Chen W. The enlightenment from two cases of asymptomatic infection with SARS-CoV-2: is it safe after 14 days of isolation? Int J Infect Dis. 2020 doi: 10.1016/j.ijid.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pan A., Liu L., Wang C., Guo H., Hao X., Wang Q., Huang J., He N., Yu H., Lin X., Wei S., Wu T. Association of Public Health Interventions With the Epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.6130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith K.J., Gavey S., Riddell N.E., Kontari P., Victor C. The association between loneliness, social isolation and inflammation: A systematic review and meta-analysis. Neurosci. Biobehav. Rev. 2020;112:519–541. doi: 10.1016/j.neubiorev.2020.02.002. [DOI] [PubMed] [Google Scholar]
- Sominsky L., Walker D.W., Spencer S.J. One size does not fit all - Patterns of vulnerability and resilience in the COVID-19 pandemic and why heterogeneity ofdisease matters. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Troyer E.A., Kohn J.N., Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu, X., Yang, R., COVID-19 transmission through asymptomatic carriers is a challenge to containment. Influenza and Other Respiratory Viruses n/a (n/a). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.