Dear Editor,
At present, there is no effective drug against the present coronavirus disease 2019 (COVID-19) pandemic. It is known that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike protein binds to human angiotensin-converting enzyme 2 (ACE2), which acts as a receptor, and binding to ACE2 is crucial for the cellular entry of SARS-COV-2 [1]. Any drug that interrupts the binding of spike protein with the ACE2 receptor will be useful in the treatment of COVID-19.
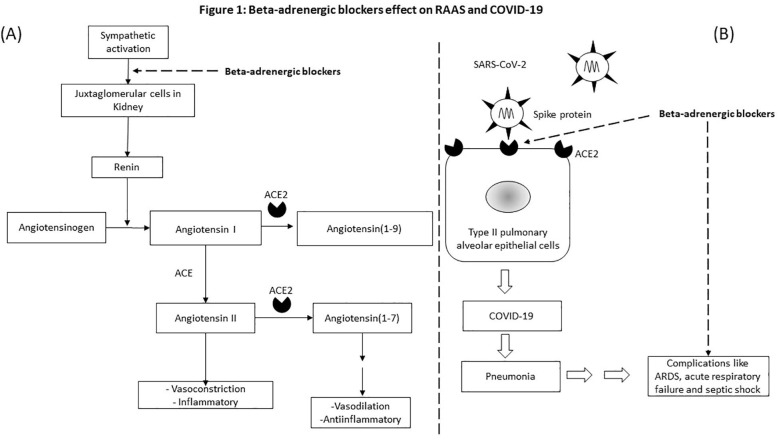
Renin-Angiotensin-Aldosterone System (RAAS) plays a crucial role in the regulation of blood pressure, sodium level, extracellular fluid volume, etc. Along with the classic pathway which produces effects like vasoconstriction and inflammation, one more pathway with opposing actions to classic pathway exist which produces effects like vasorelaxation and it is anti-inflammatory. Unlike the classic RAAS pathway which uses ACE, the vasorelaxation arm uses ACE2 [1].
It is known that COVID-19 patients exhibit pneumonia, and severe cases had complications like acute respiratory distress syndrome (ARDS), respiratory failure and septic shock which carries a high mortality rate [2]. Recent studies showed that beta-adrenergic blockers reduced the mortality in septic shock patients [3]. Beta-adrenergic blockers also showed beneficial effects in ARDS and respiratory failure patients [4], [5]. Beta-adrenergic blockers by its inhibitory action on the sympathetic system negatively regulate renin release by Juxtaglomerular (JG) cells in the kidney. A decrease in renin may reduce the activity in both arms of RAAS and may decrease ACE2, which may decrease the SARS-CoV-2 virus entry into the host cell.
Considering the potential role of beta-adrenergic blockers in decreasing the SARS-CoV-2 entry into the cells by downregulating ACE2 receptors, and its role in reducing the mortality in respiratory failure, ARDS and septic shock conditions, it may be a good candidate drug for treating COVID-19 patients (Fig. 1 ). I propose that beta-adrenergic blockers may be beneficial in COVID-19 patients with hypertension comorbidity, by regulation of blood pressure and decreasing SARS-CoV-2 cellular entry. In low doses, beta-adrenergic blockers may be beneficial in COVID-19 patients with normal blood pressure, as it may decrease the SARS-CoV-2 entry into the cell. I suggest doing a retrospective study on the COVID-19 patients, who were already on beta-adrenergic blockers for their previous cardiovascular illness and its effect on mortality. The proposed retrospective study will test the validity of the hypothesis and clarify the role of beta-adrenergic blockers in COVID-19 patients.
Fig. 1.
Beta-adrenergic blockers effect on RAAS and COVID-19. A) Beta-adrenergic blockers by its inhibitory action on the sympathetic system decrease the renin release by Juxtaglomerular (JG) cells in the Kidney. A decrease in renin may reduce the activity in both arms and may decrease ACE2 receptors. B) Decreased ACE2 receptors will affect the SARS-CoV-2 cellular entry and thereby reduce the viral infectivity. Beta-adrenergic blockers have been shown to reduce the mortality rate in ARDS, septic shock and respiratory failure. Beta-adrenergic blockers will be beneficial in COVID-19 patients in two ways, by reducing the SARS-CoV-2 virus cellular entry and by reducing the complications like ARDS, Septic shock and respiratory failure in severe cases.
Declaration of Competing Interest
The author has no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.mehy.2020.109809.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.Zhang H., Penninger J.M., Li Y., Zhong N., Slutsky A.S. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;3:1–5. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. The Lancet. 2020 doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tan K., Harazim M., Tang B., Mclean A., Nalos M. The association between premorbid beta blocker exposure and mortality in sepsis—a systematic review. Crit Care. 2019;23(1):298. doi: 10.1186/s13054-019-2562-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Qadi M.O., Kashyap R. A42 ARDS: risk, treatment, and outcomes: effect of chronic beta blockers use on sepsis-related acute respiratory distress syndrome. Am J Respir Crit Care Med. 2015;191:1. [Google Scholar]
- 5.Noveanu M., Breidthardt T., Reichlin T., Gayat E., Potocki M., Pargger H. Effect of oral beta-blocker on short and long-term mortality in patients with acute respiratory failure: results from the BASEL-II-ICU study. Crit Care. 2010;14(6):R198. doi: 10.1186/cc9317. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.